Table of Contents
Definition / general | Physiology | Clinical features | Case reports | Microscopic (histologic) images | Positive stains | Electron microscopy description | Electron microscopy images | VideosCite this page: Islam S. Histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidhistology.html. Accessed December 22nd, 2024.
Definition / general
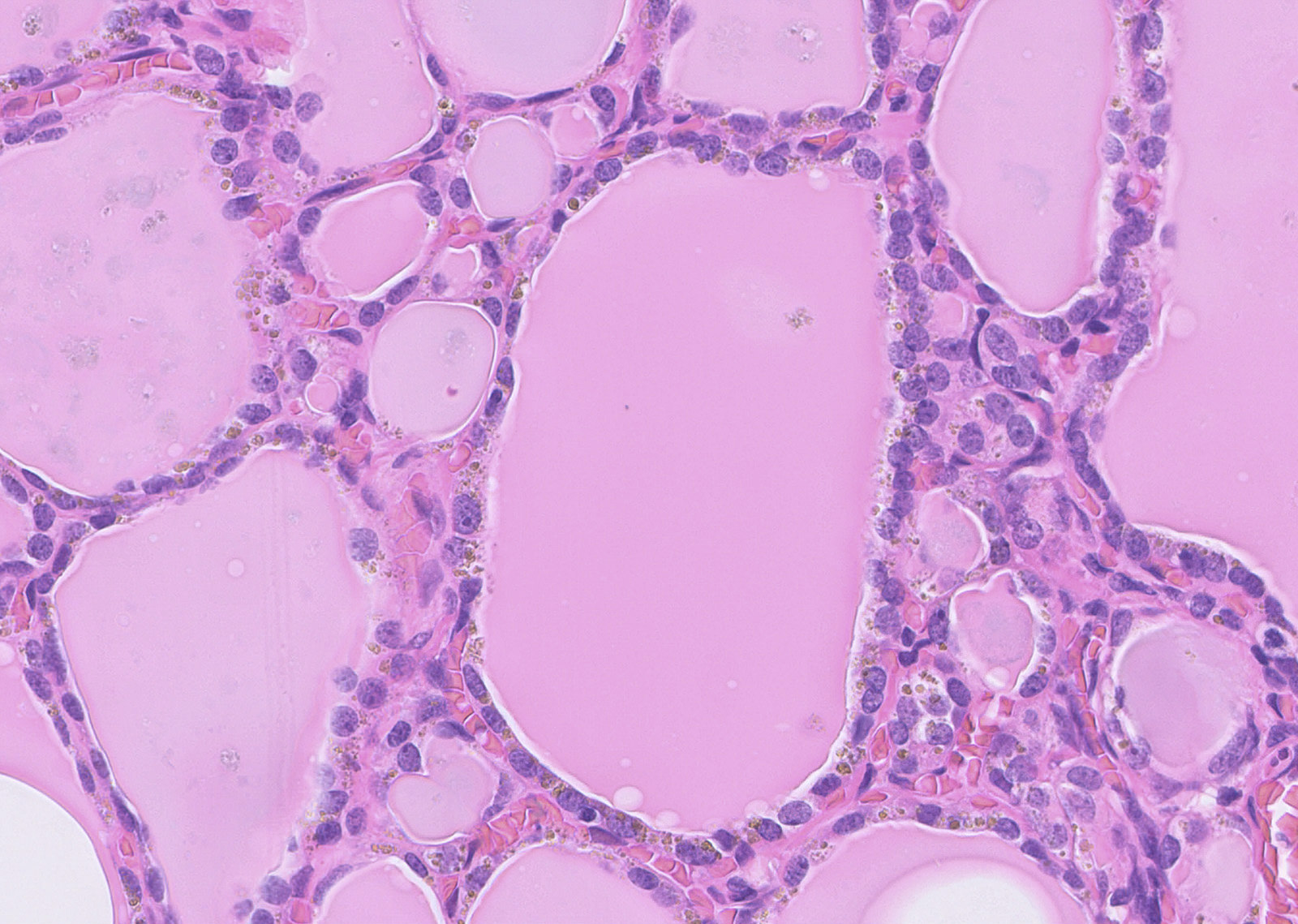
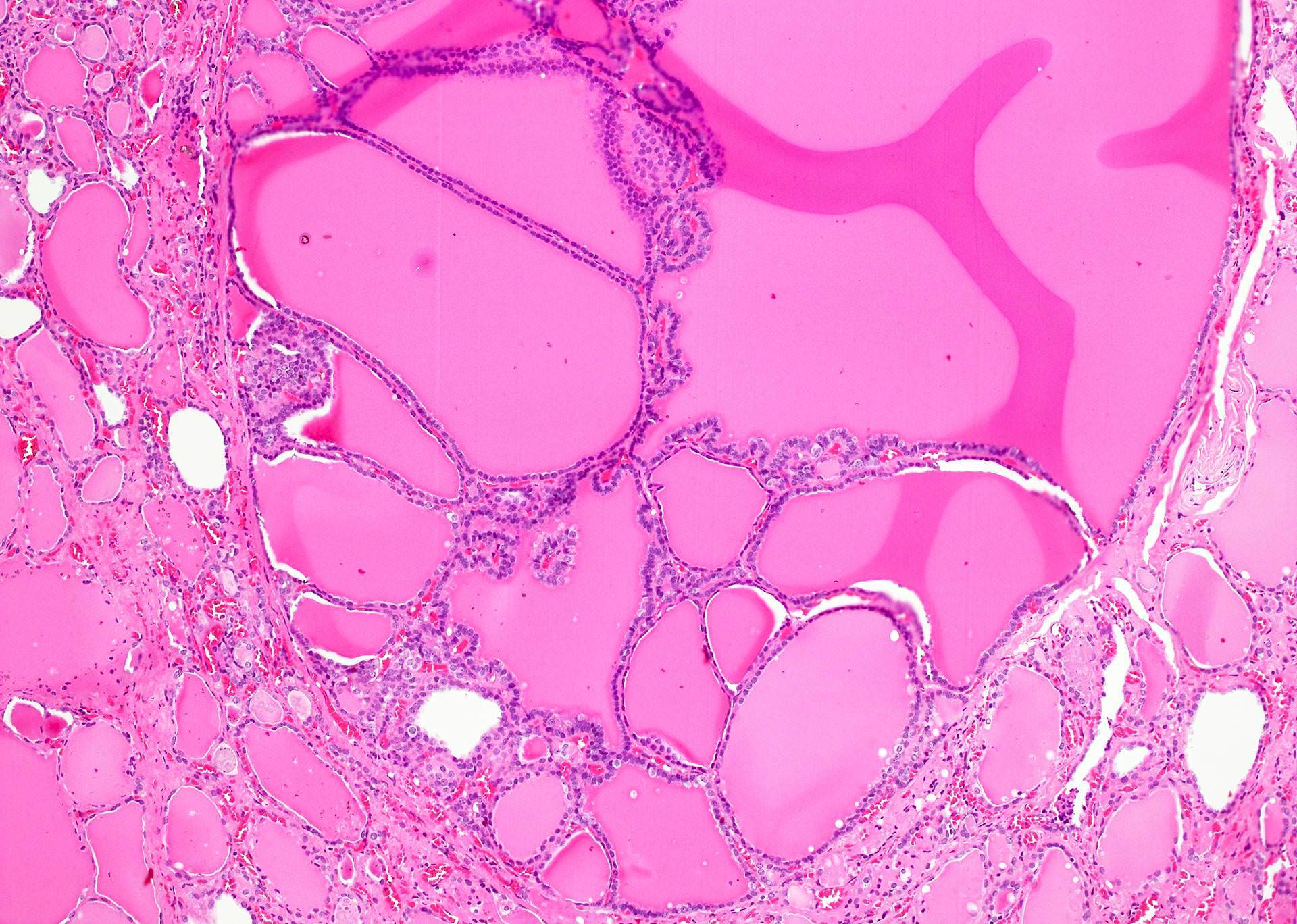
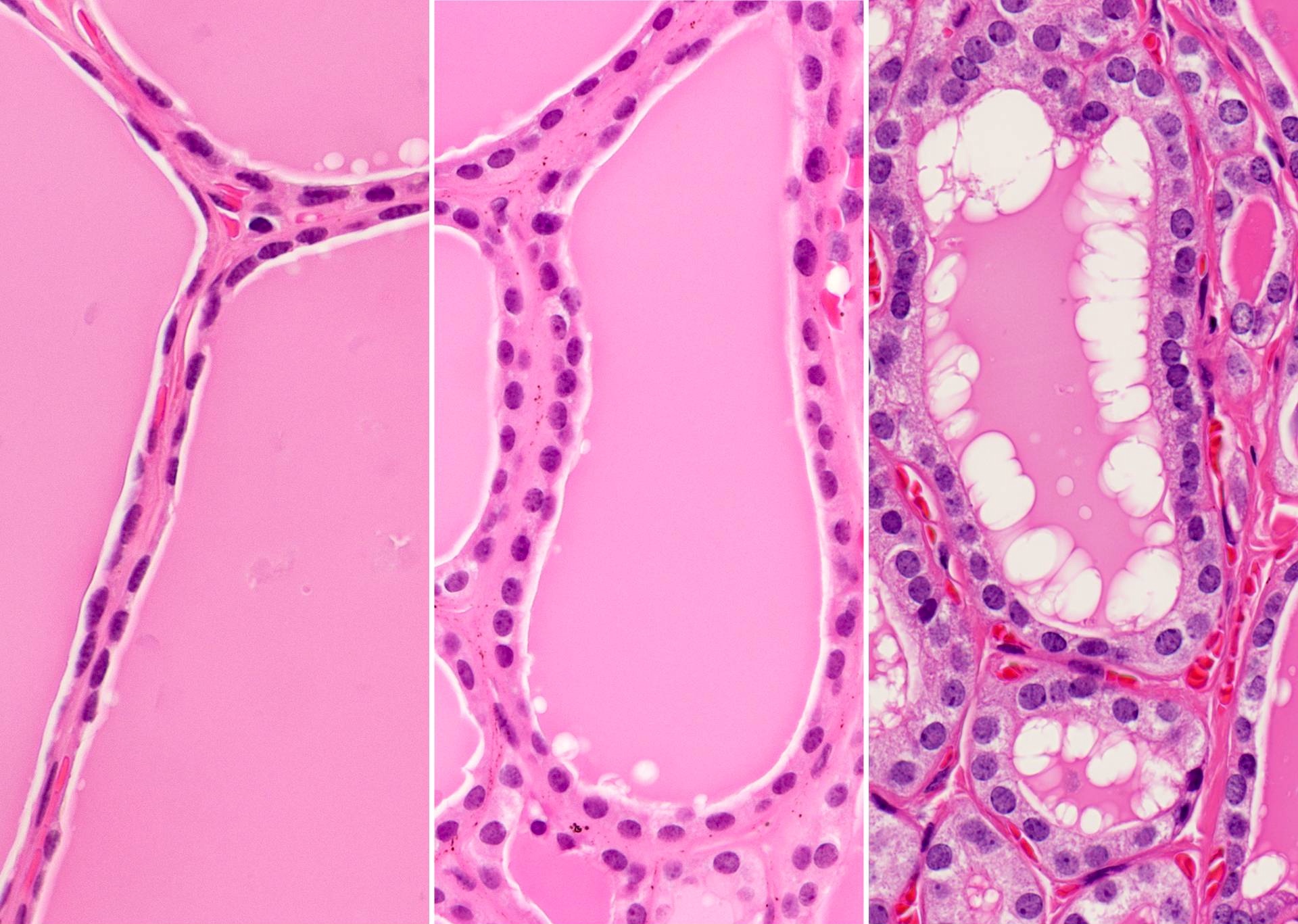
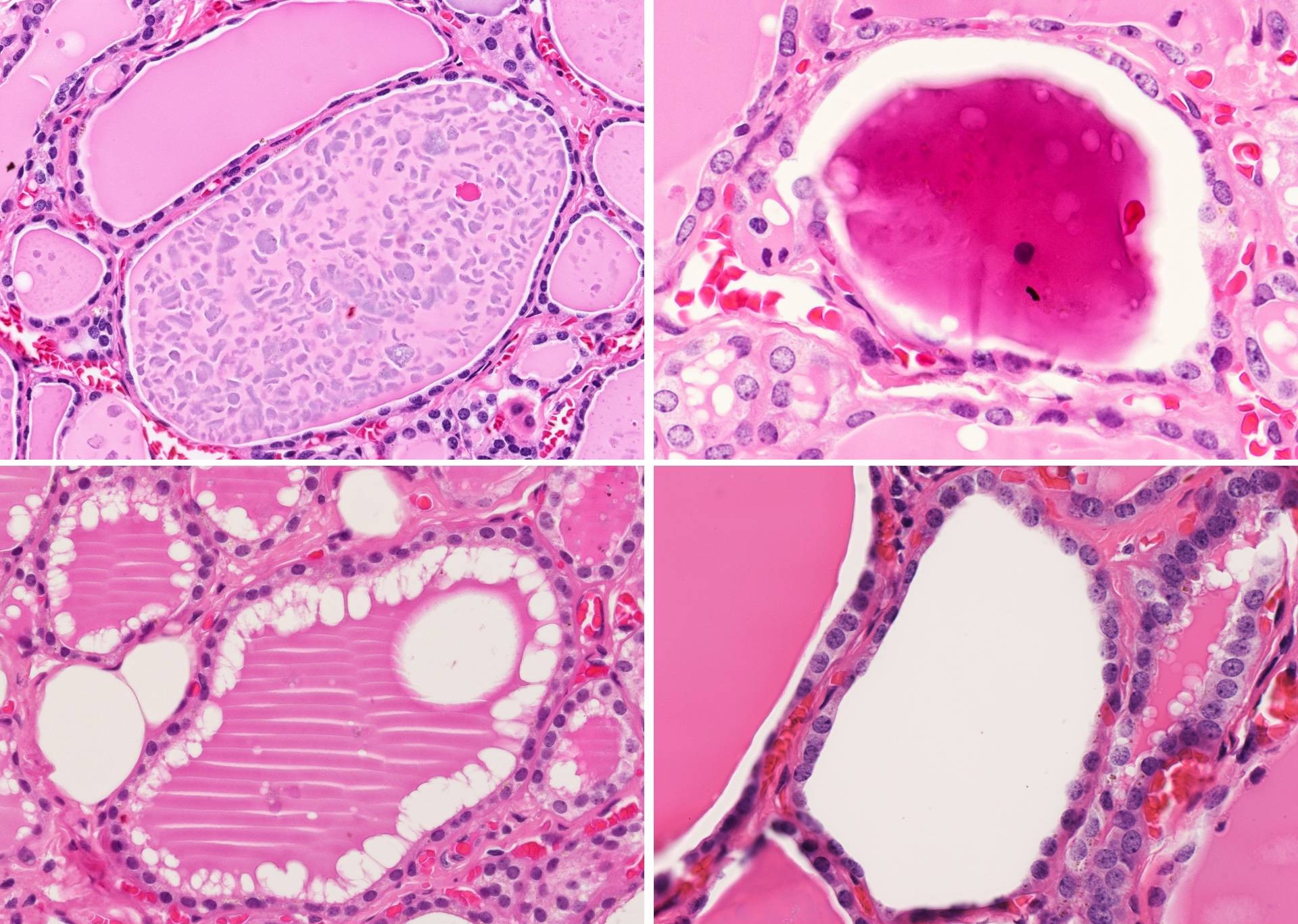
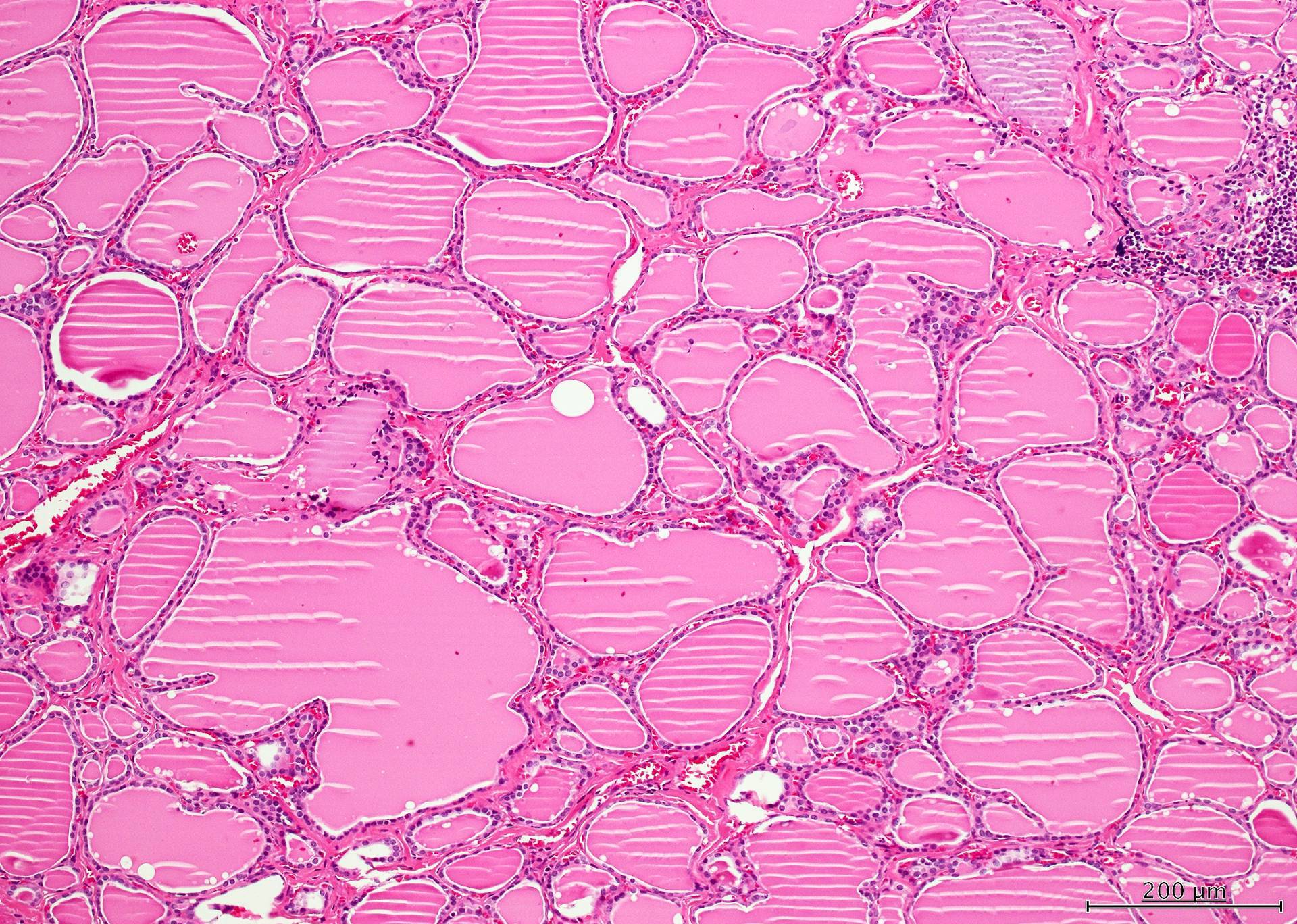
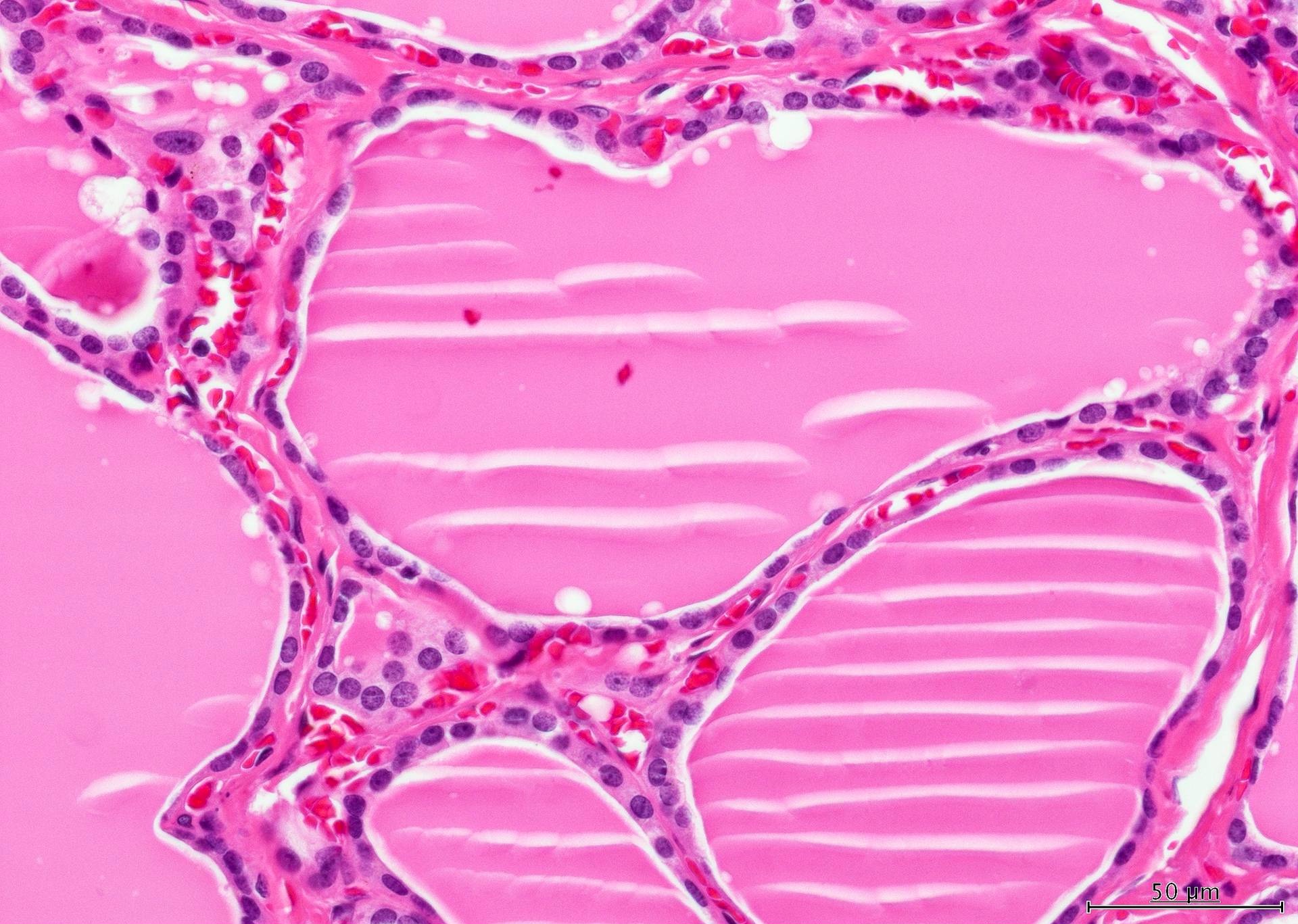
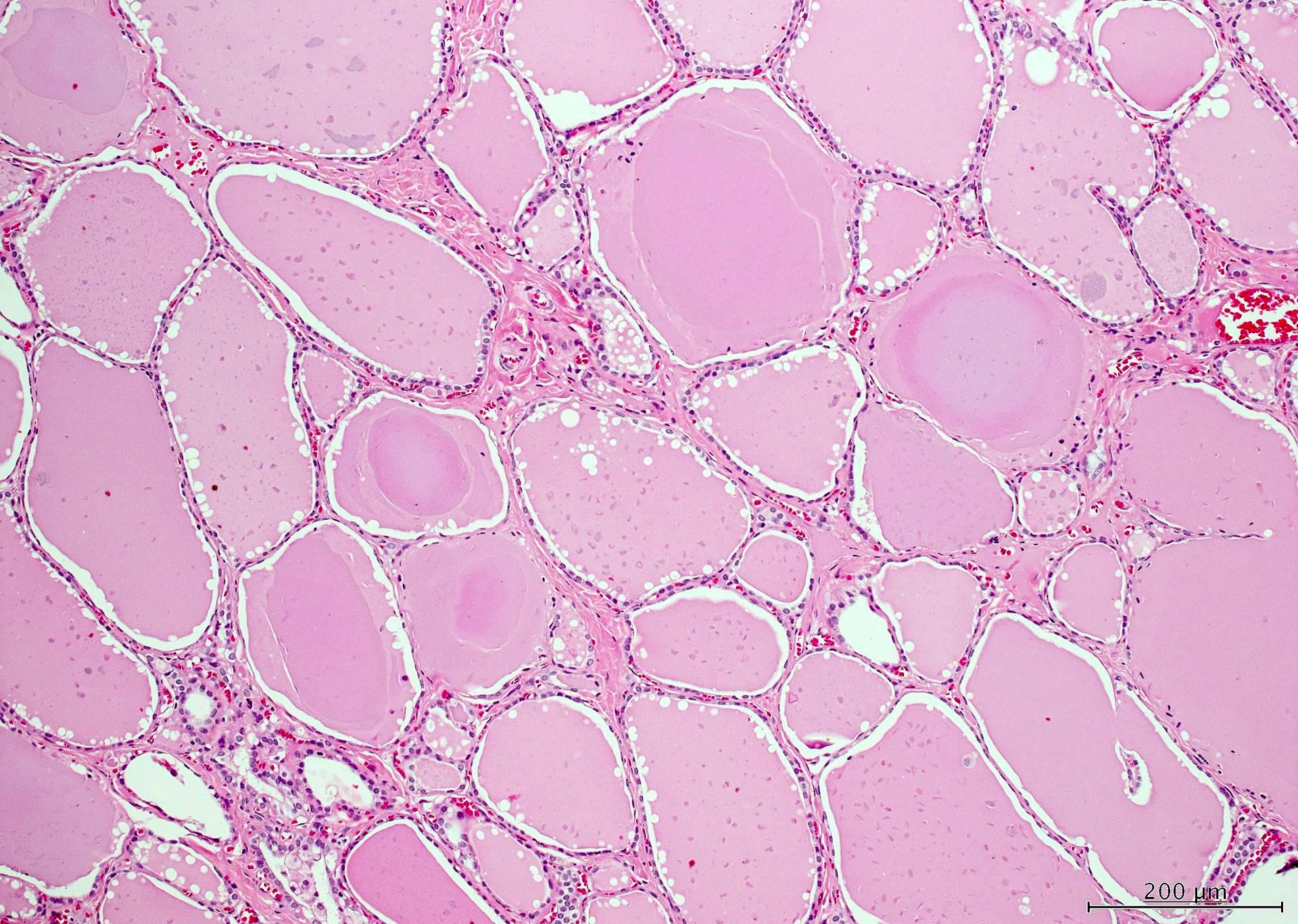
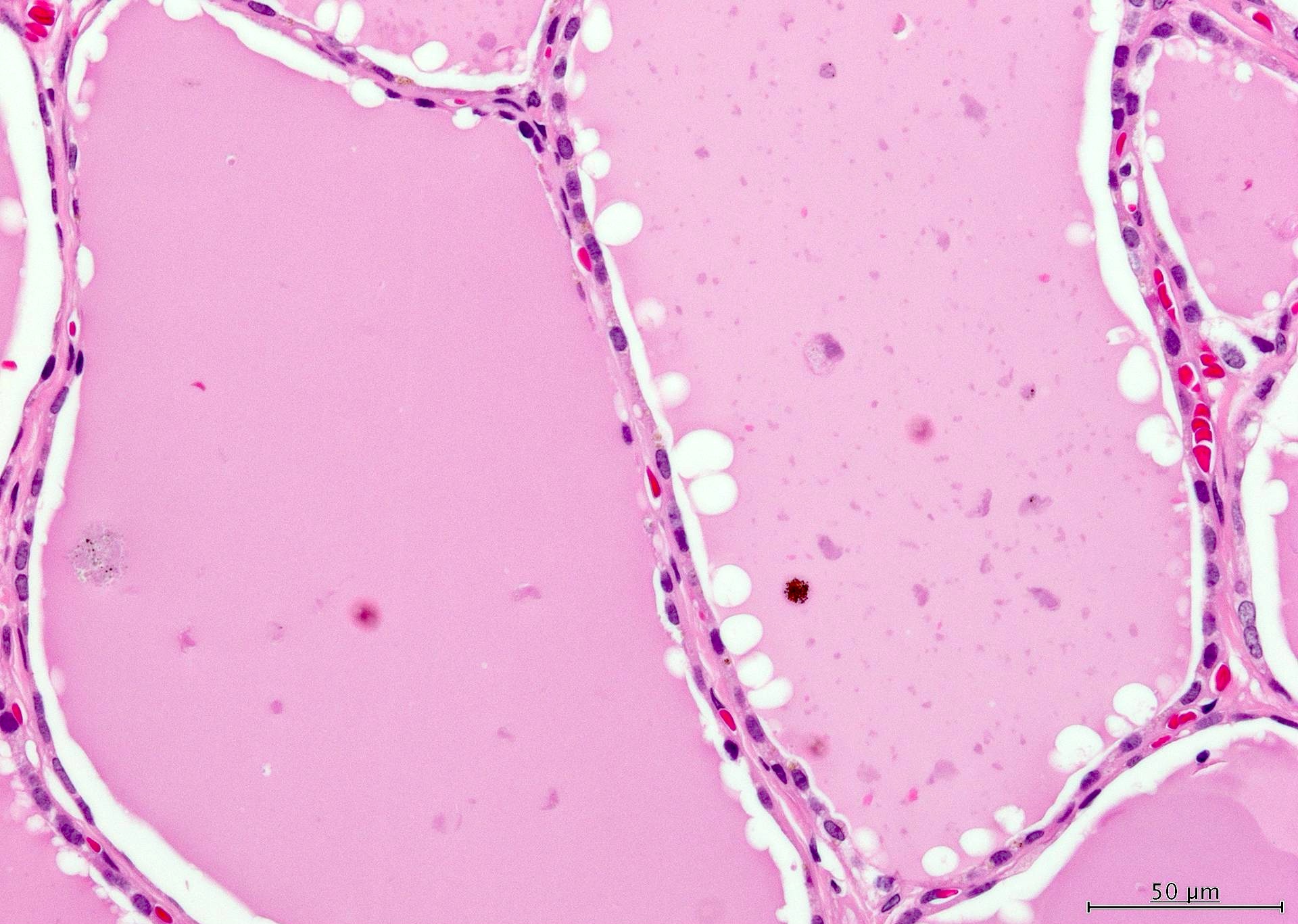
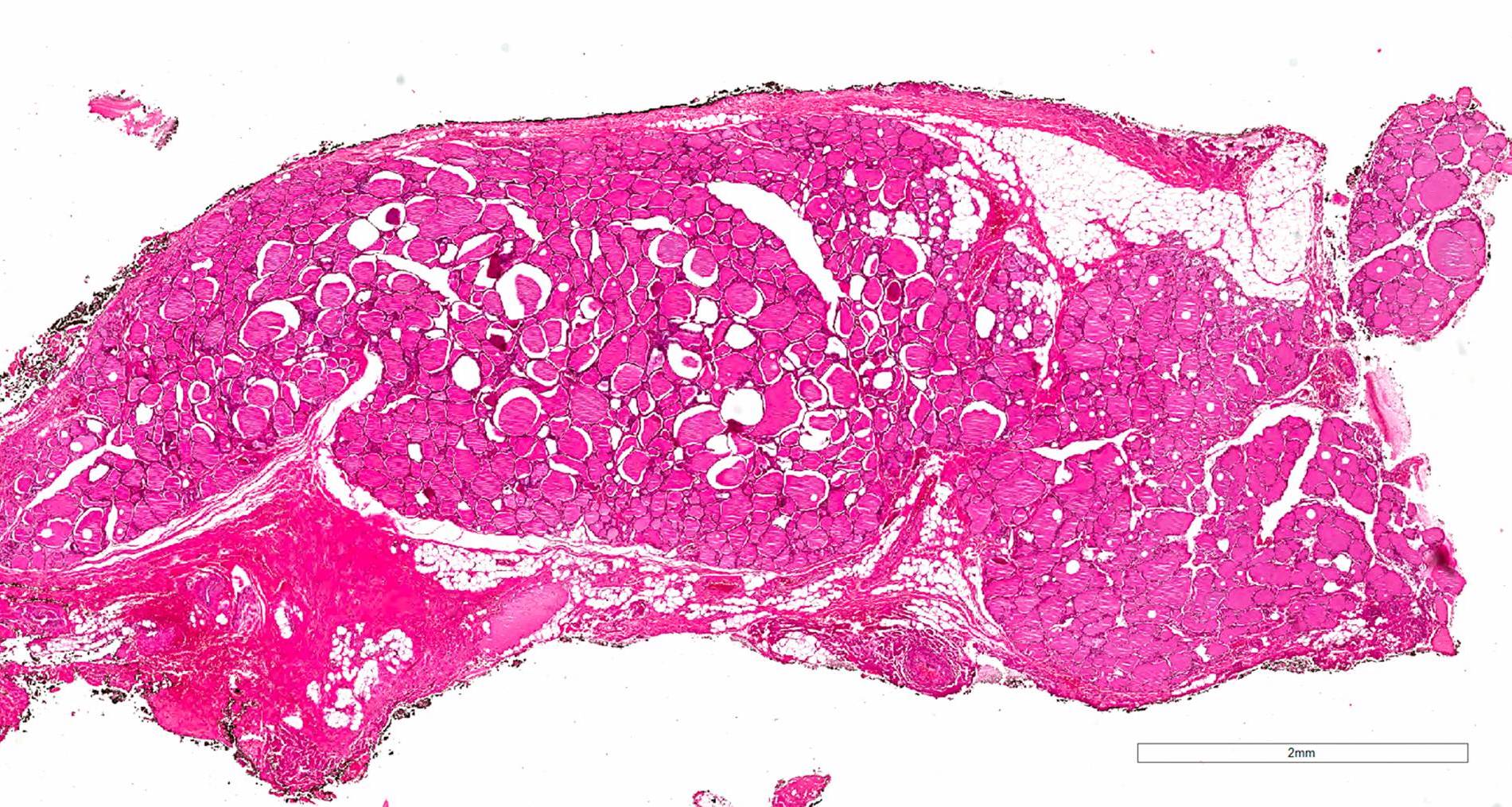
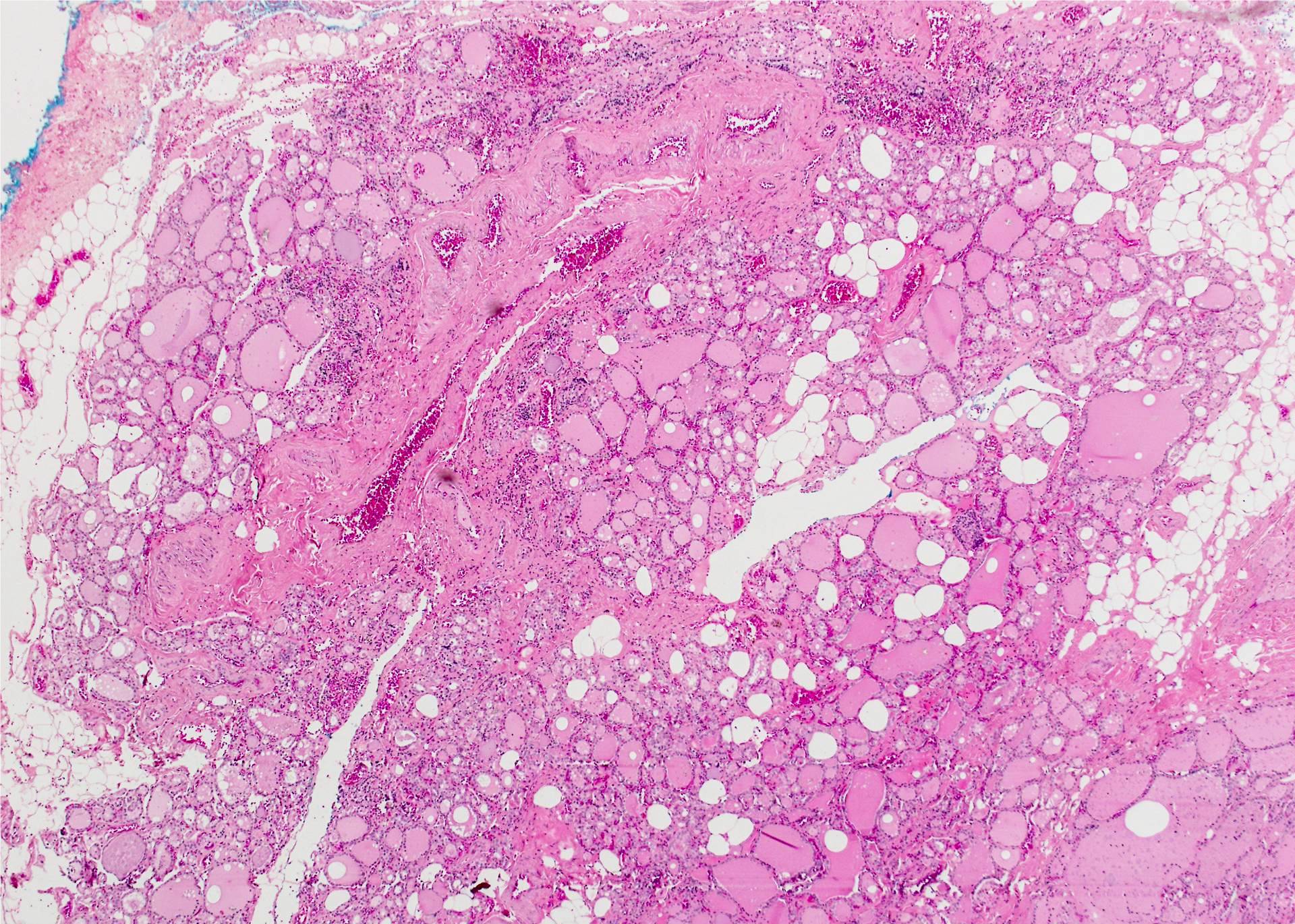
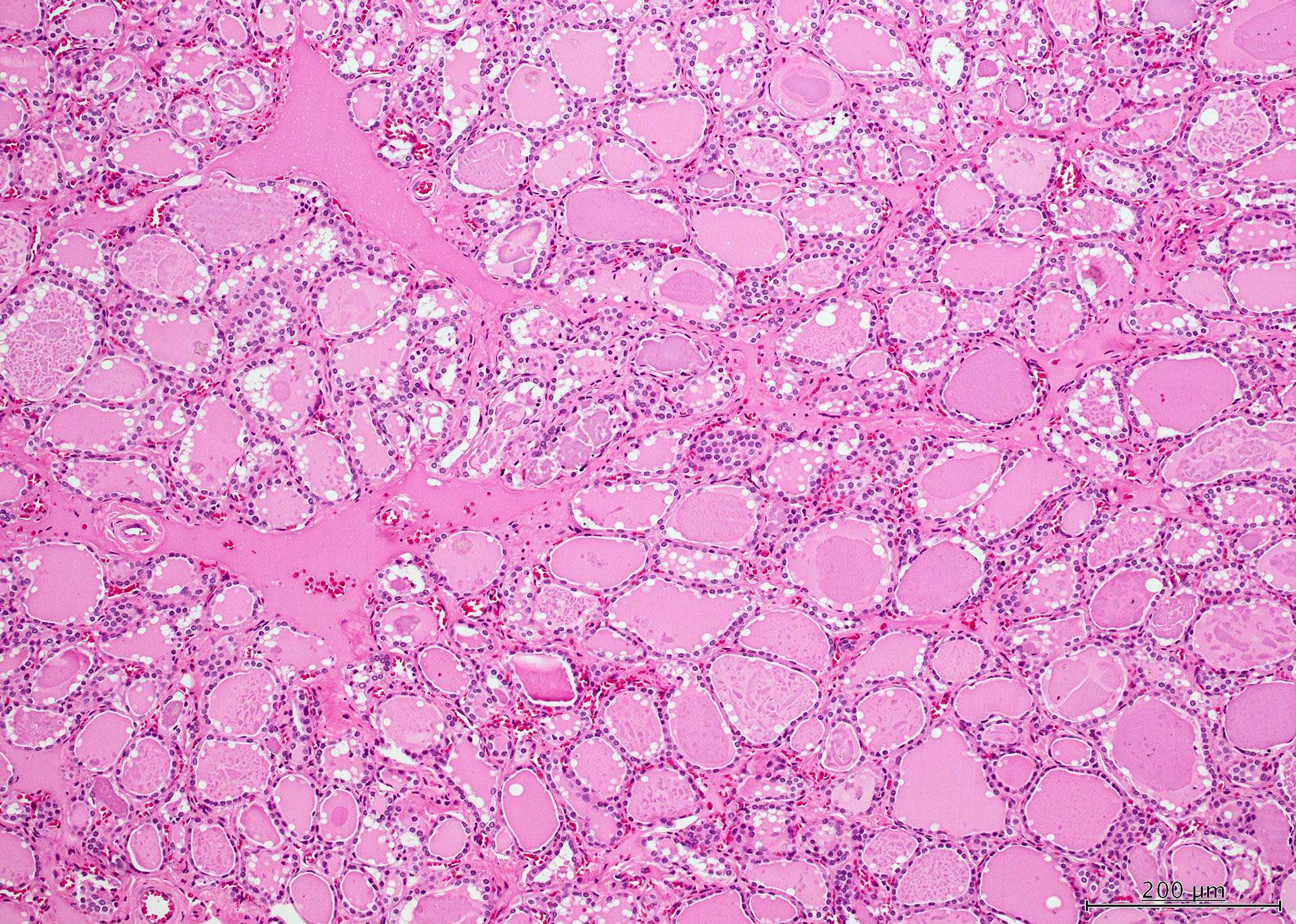
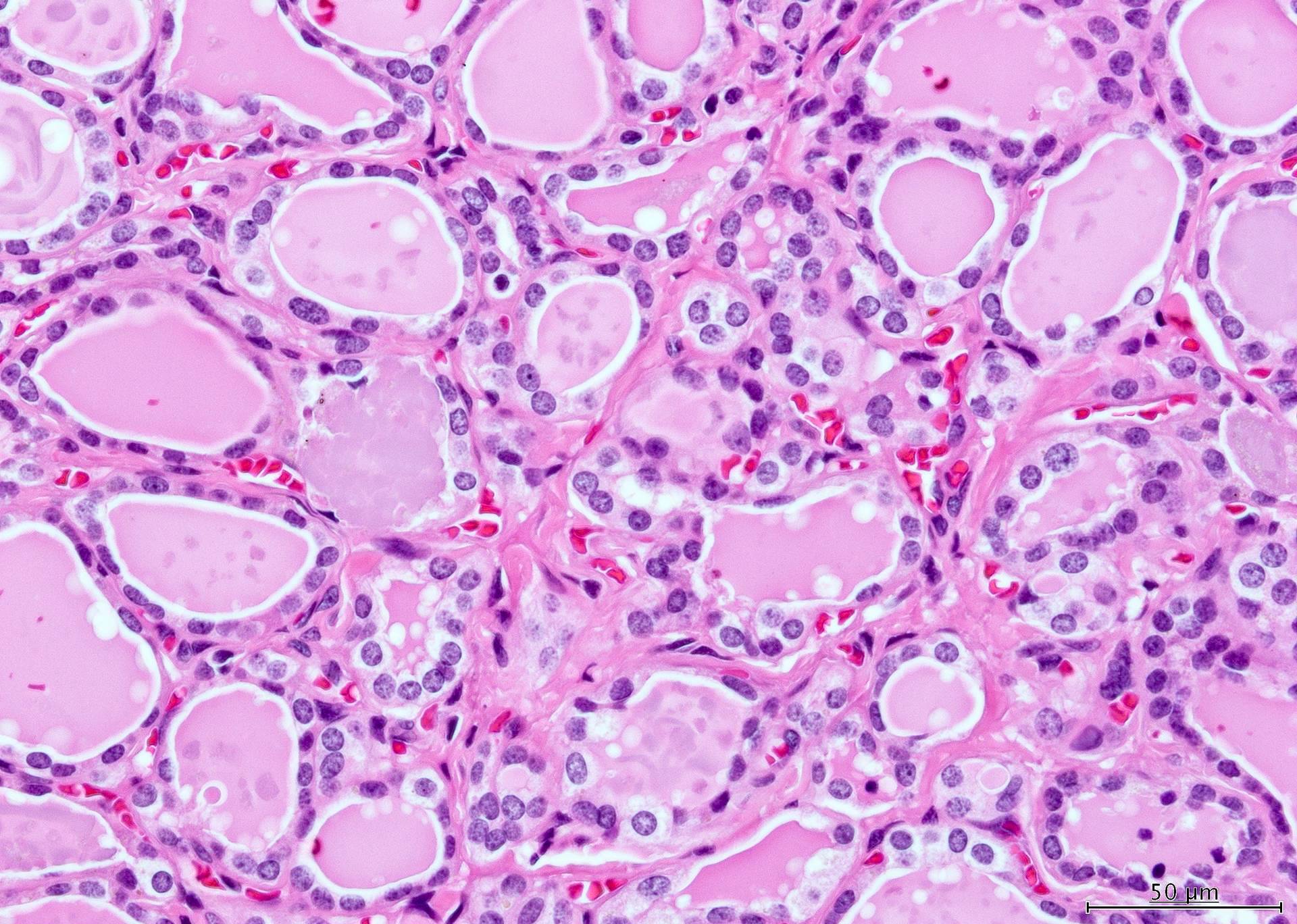
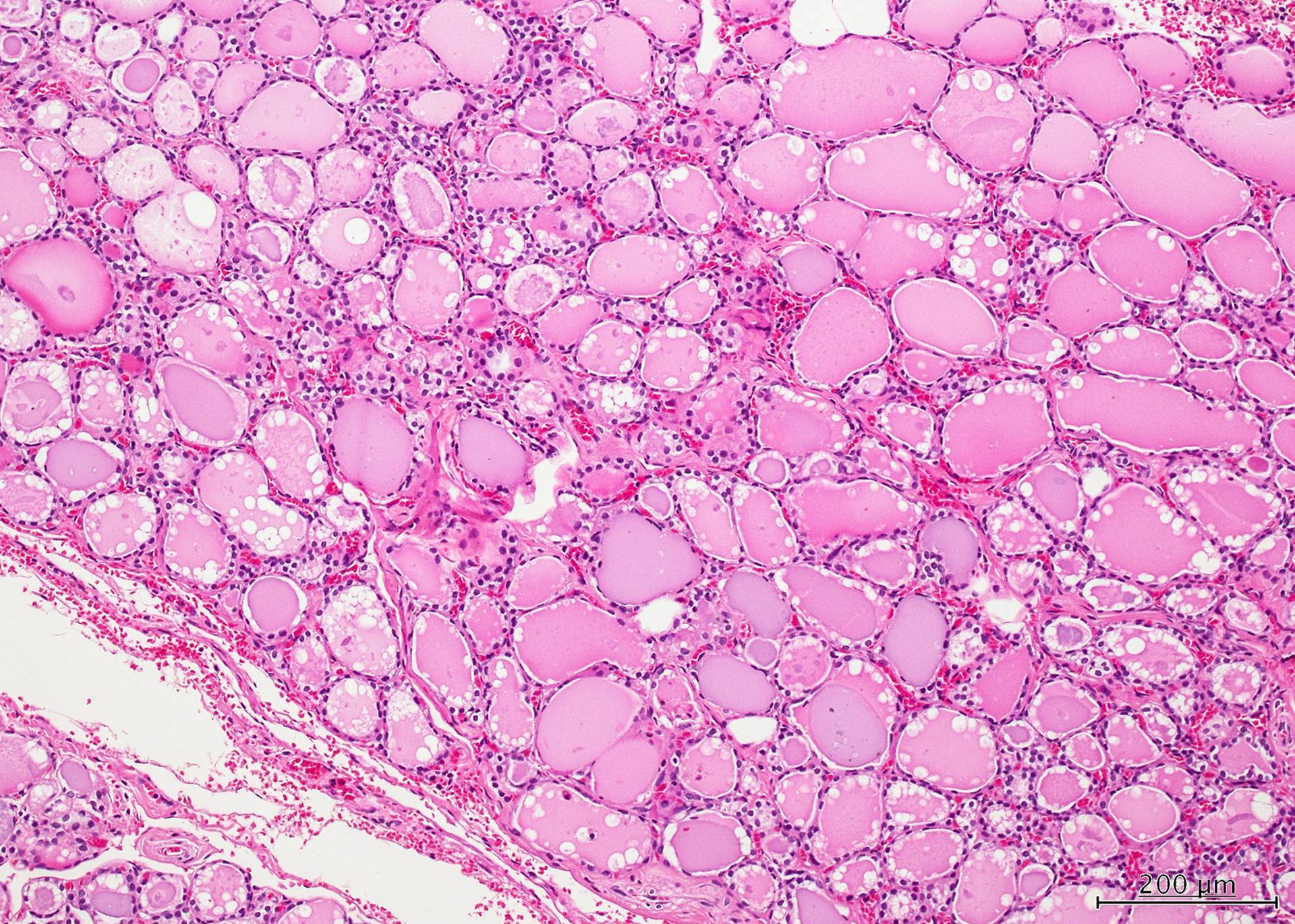
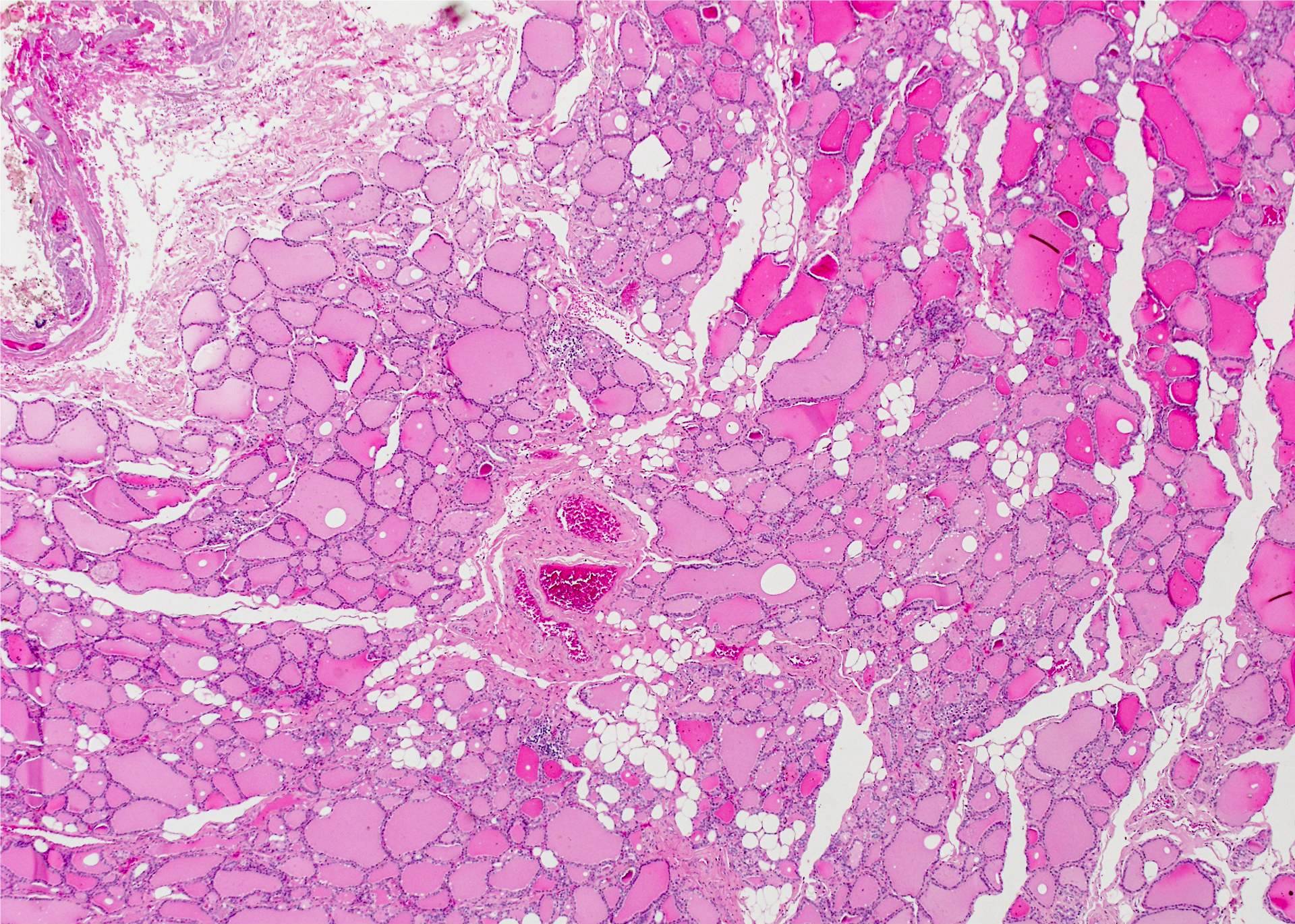
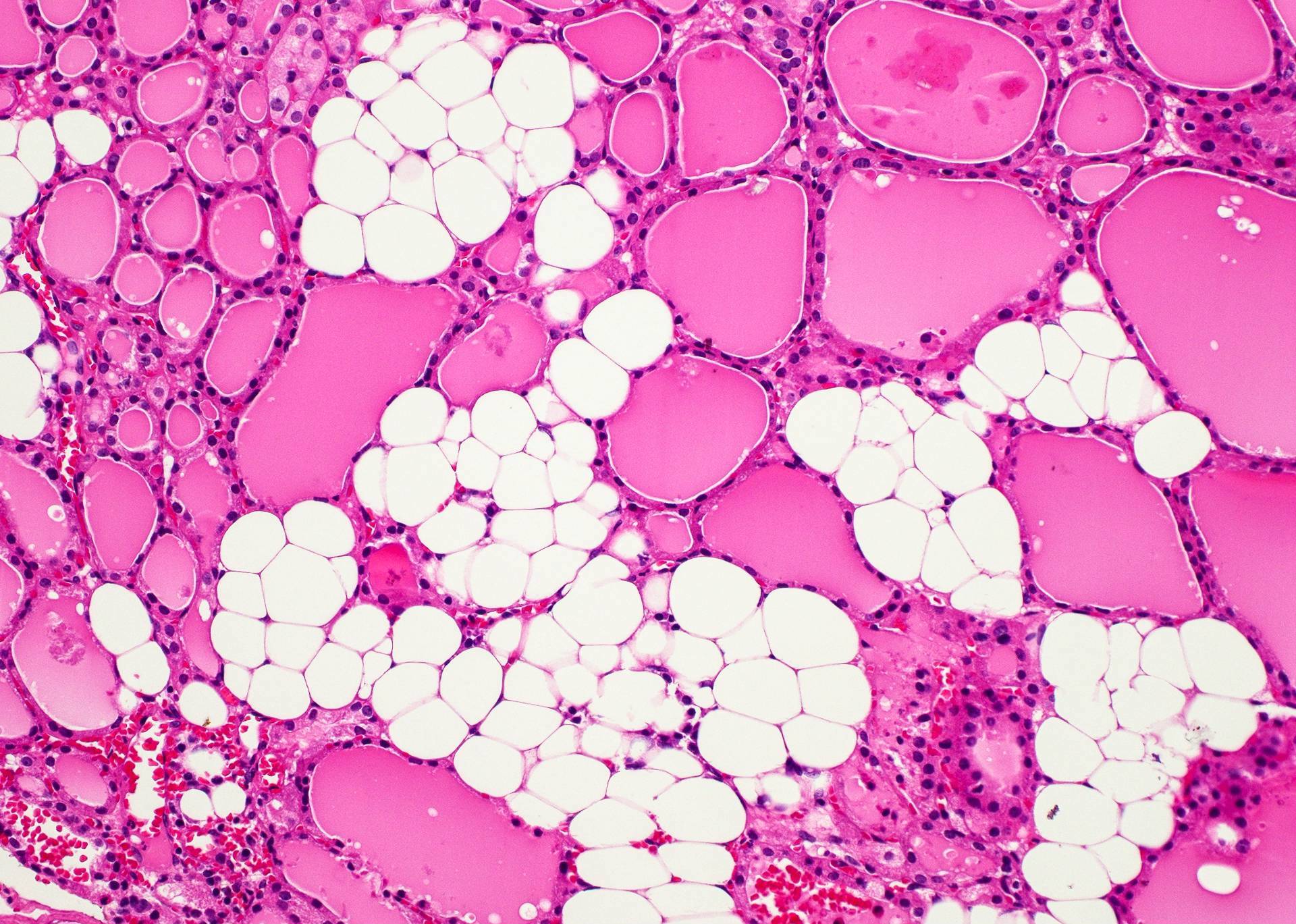
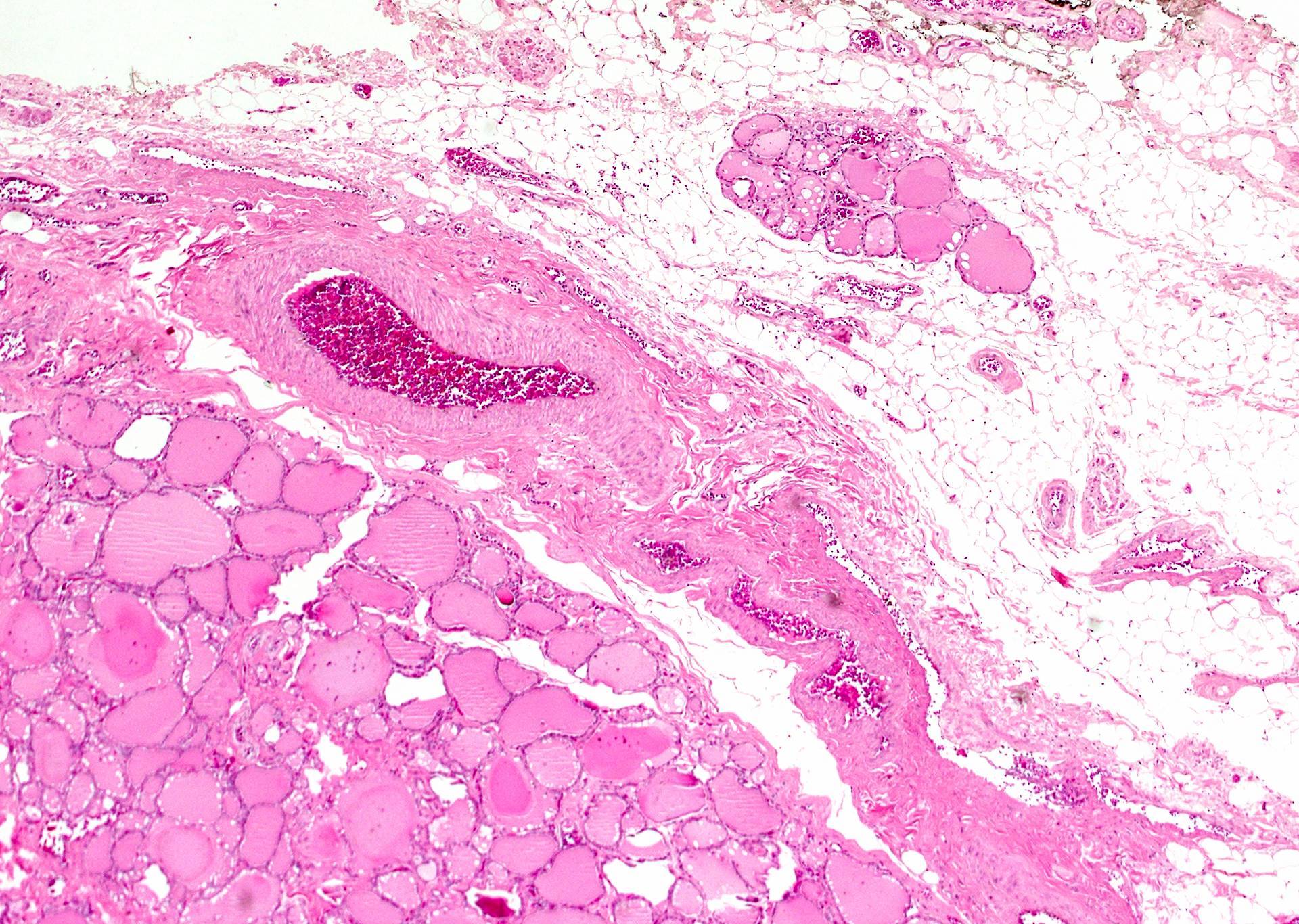
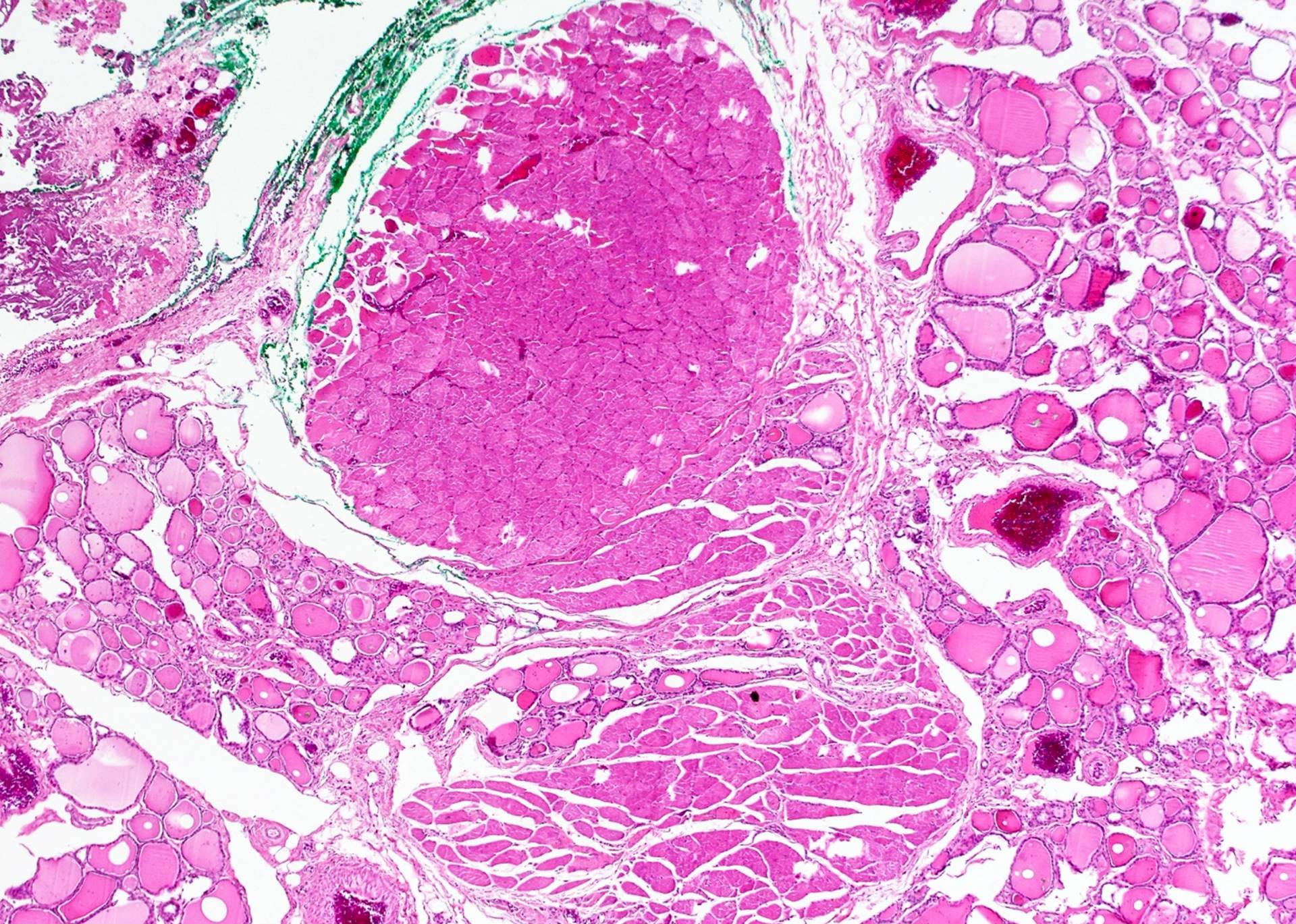
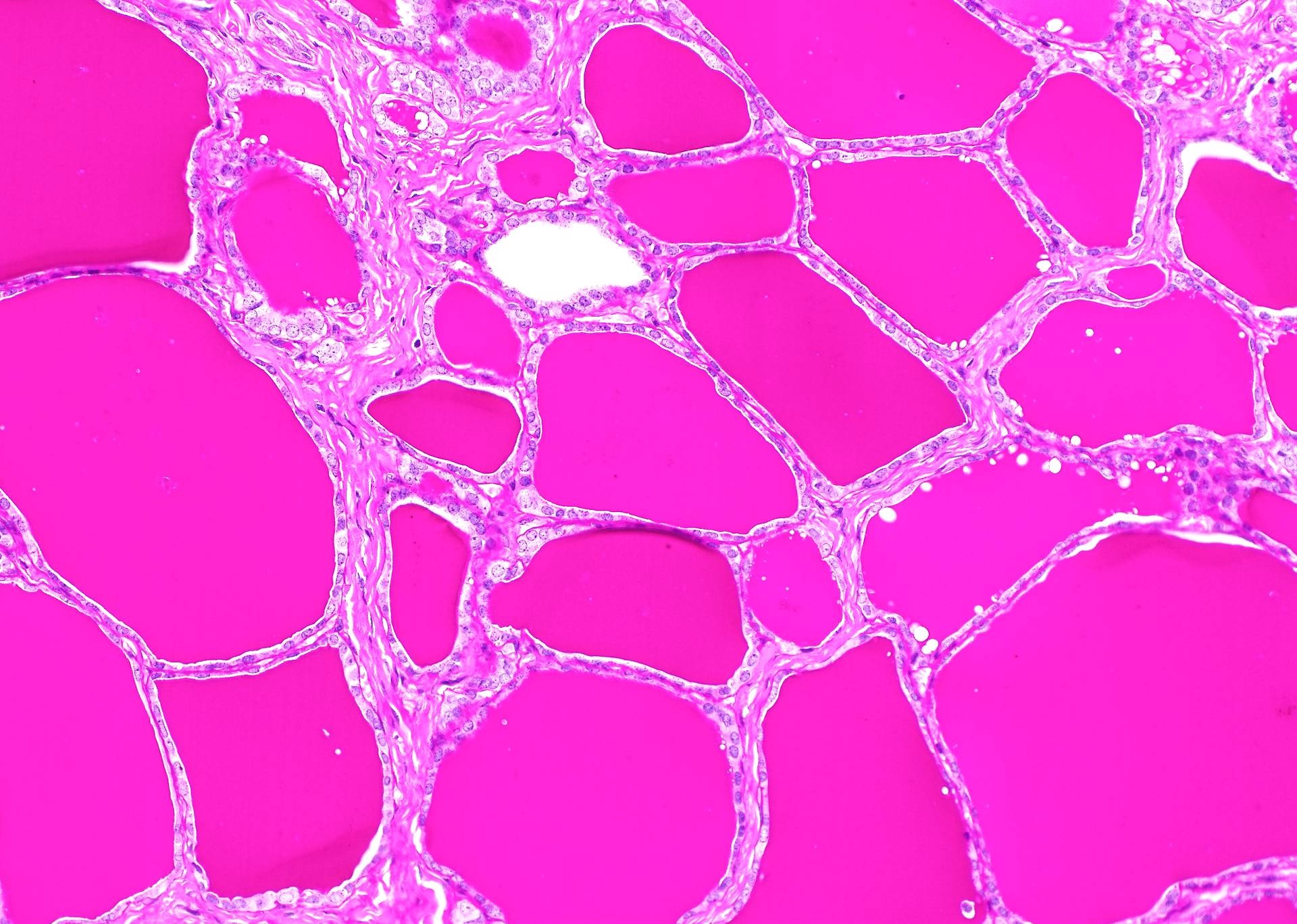
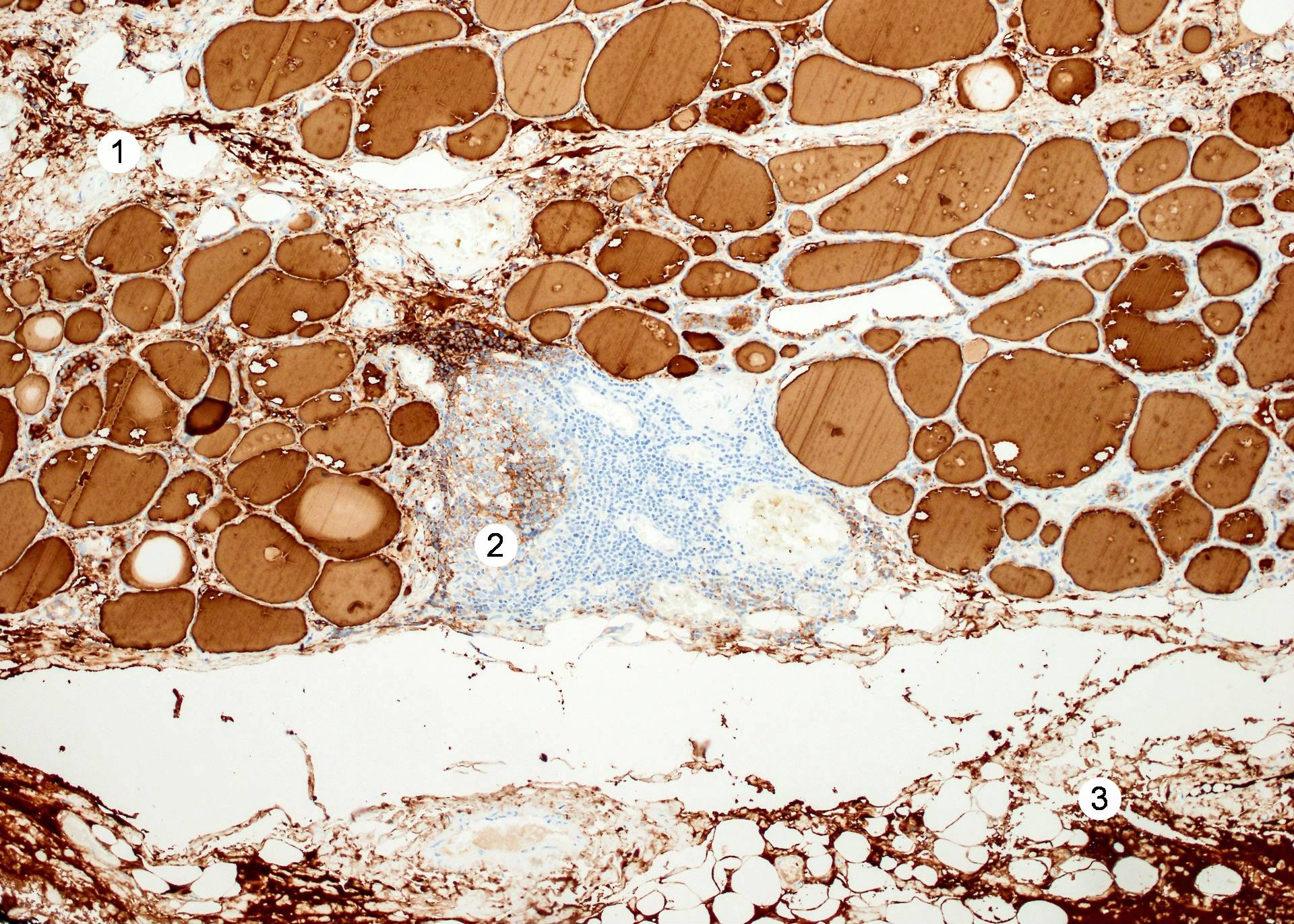
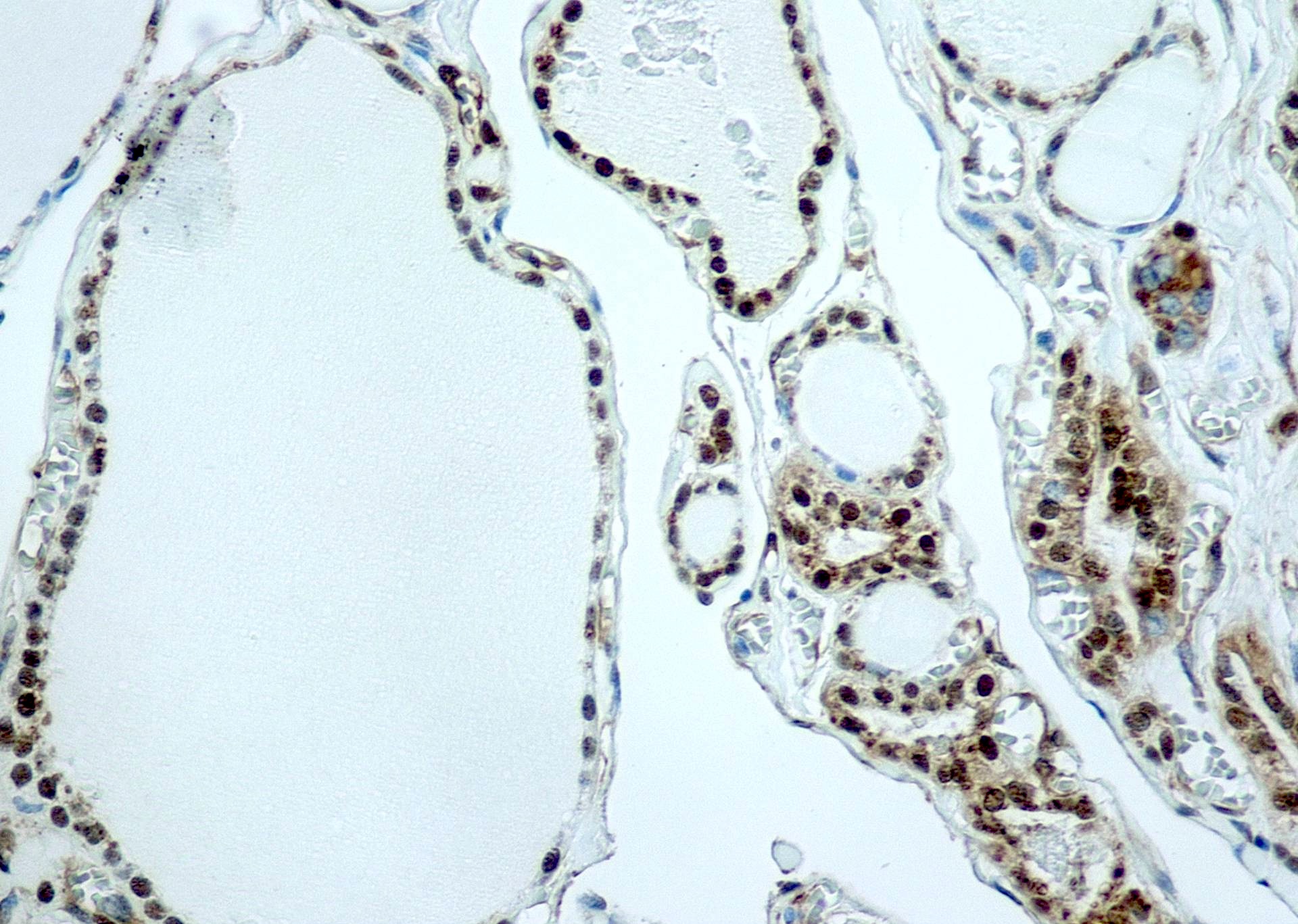
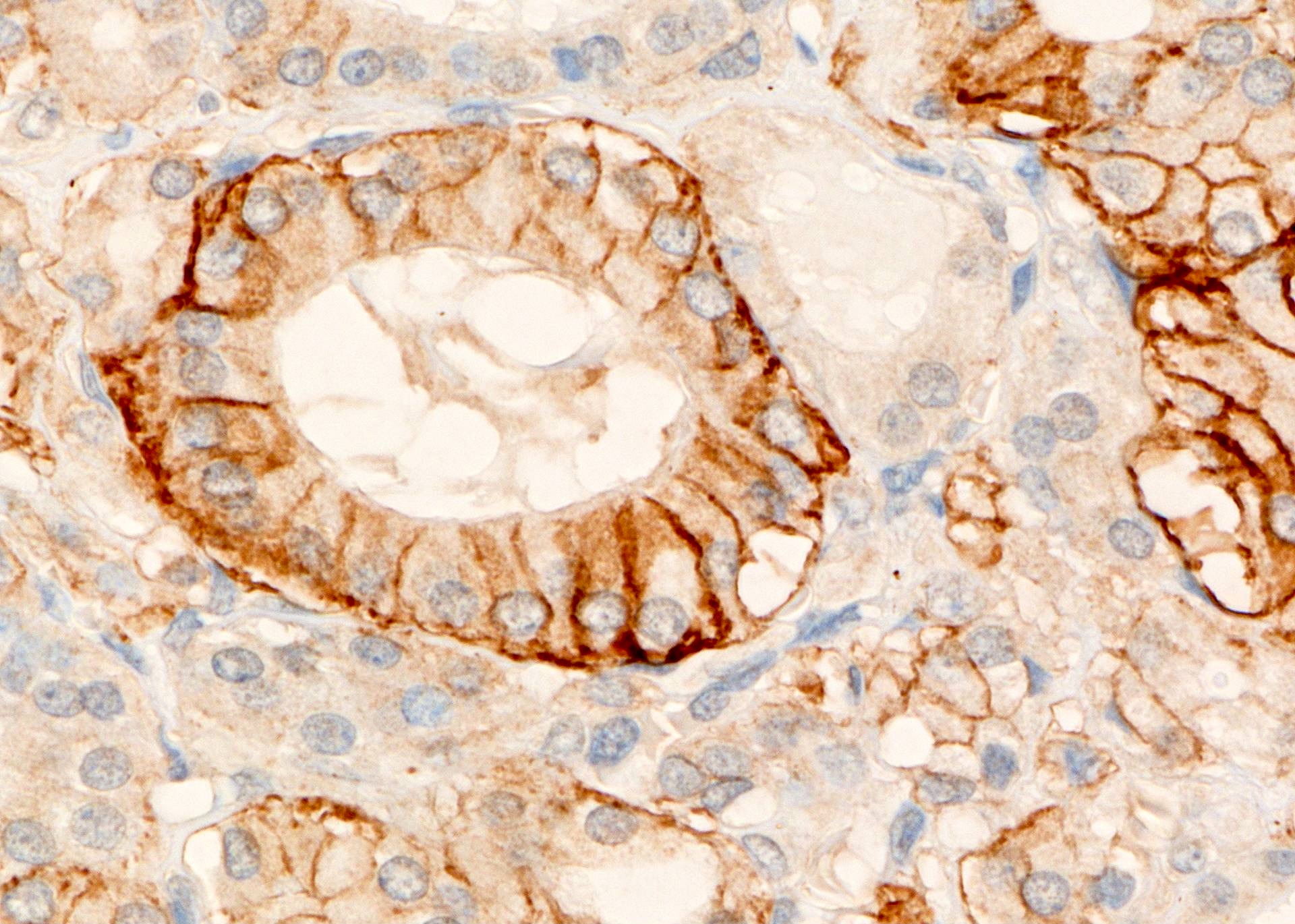
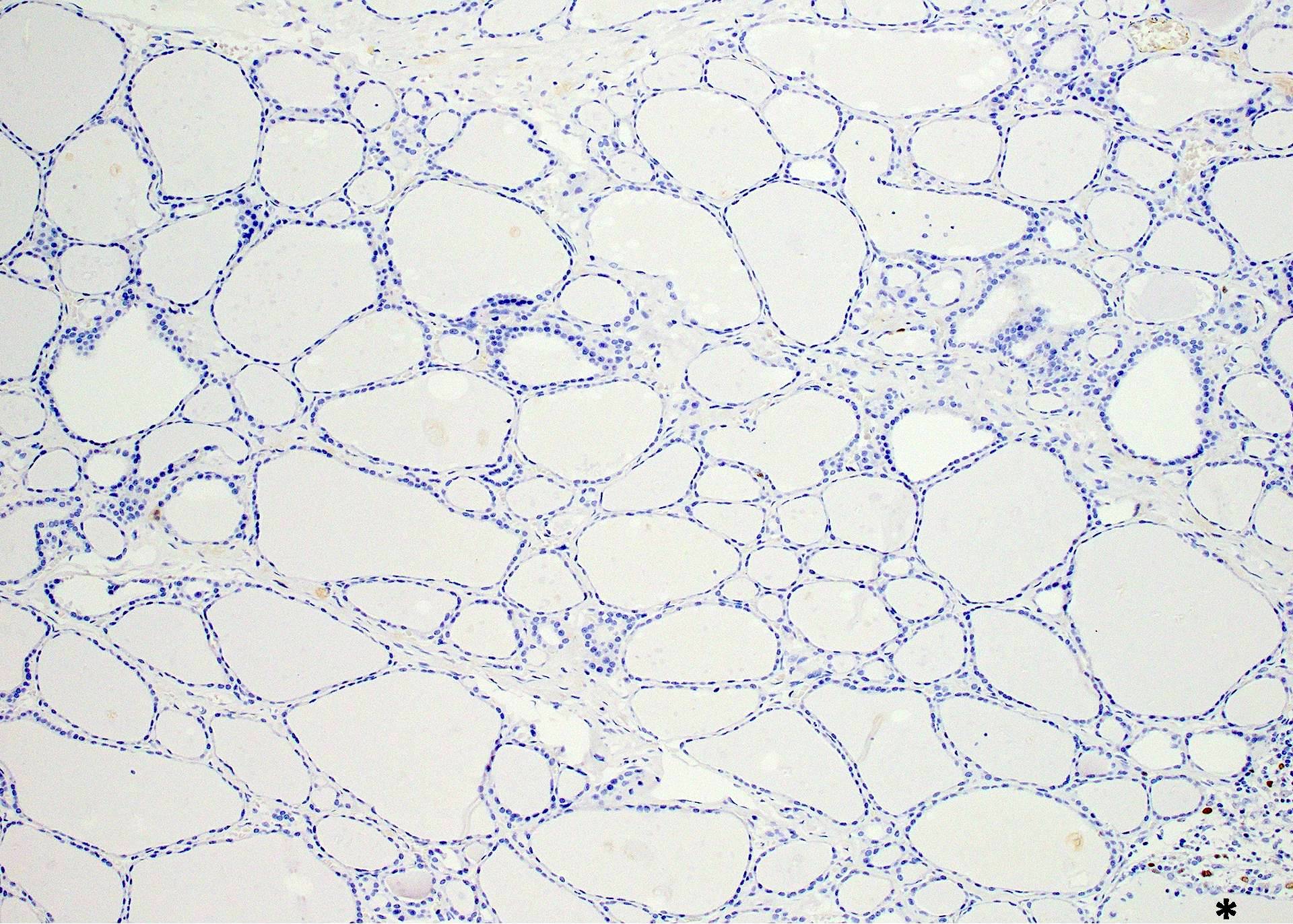
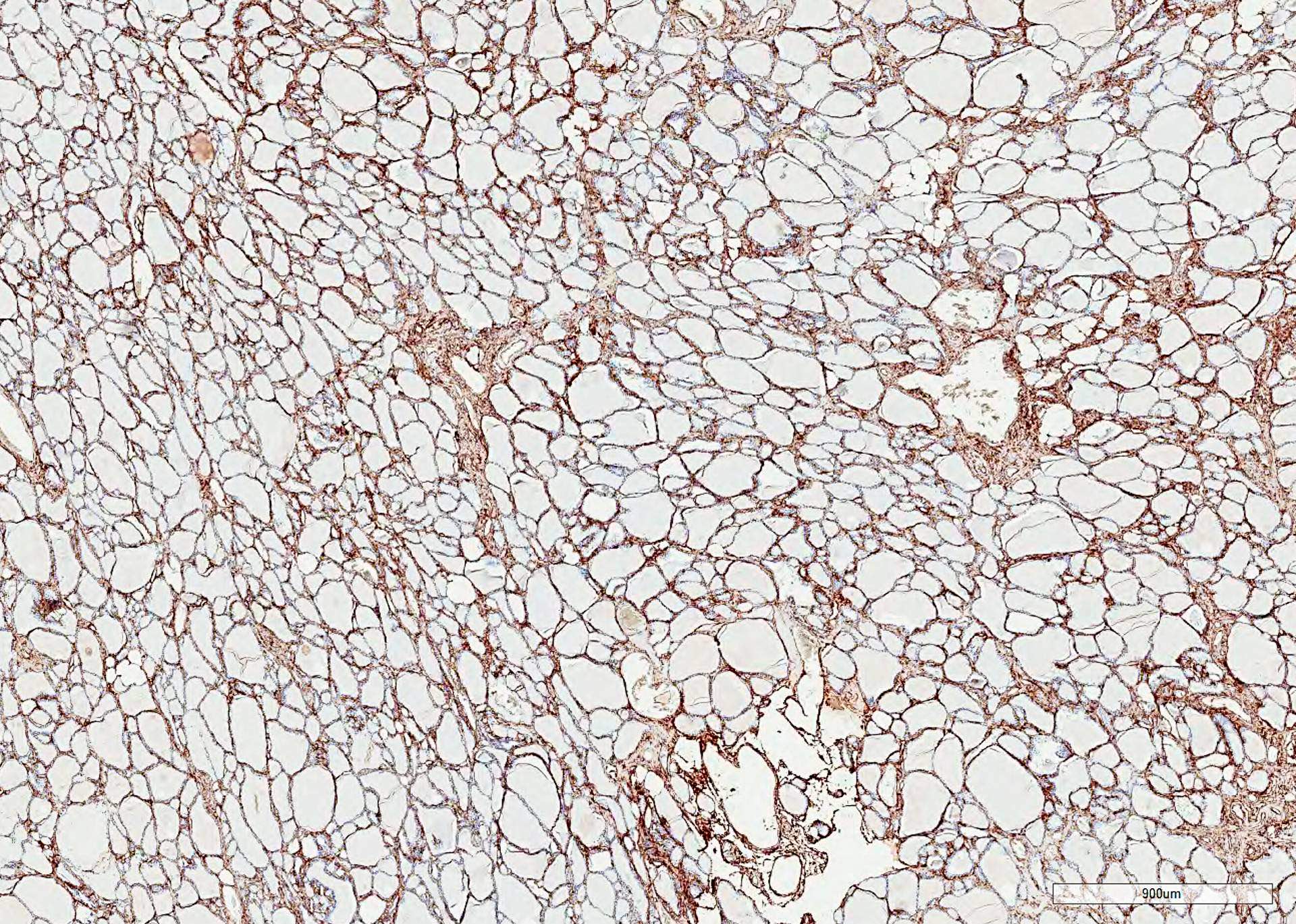
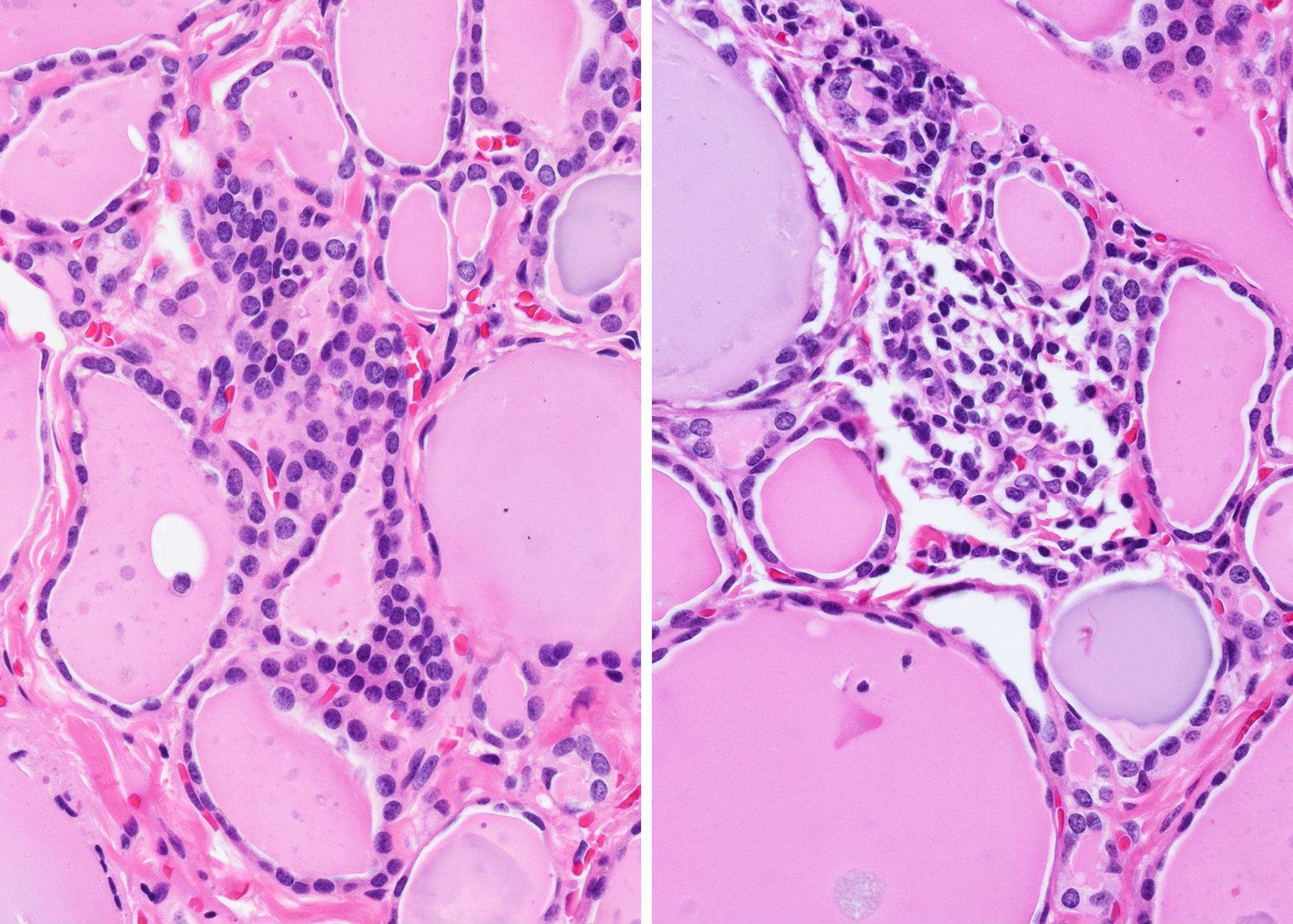
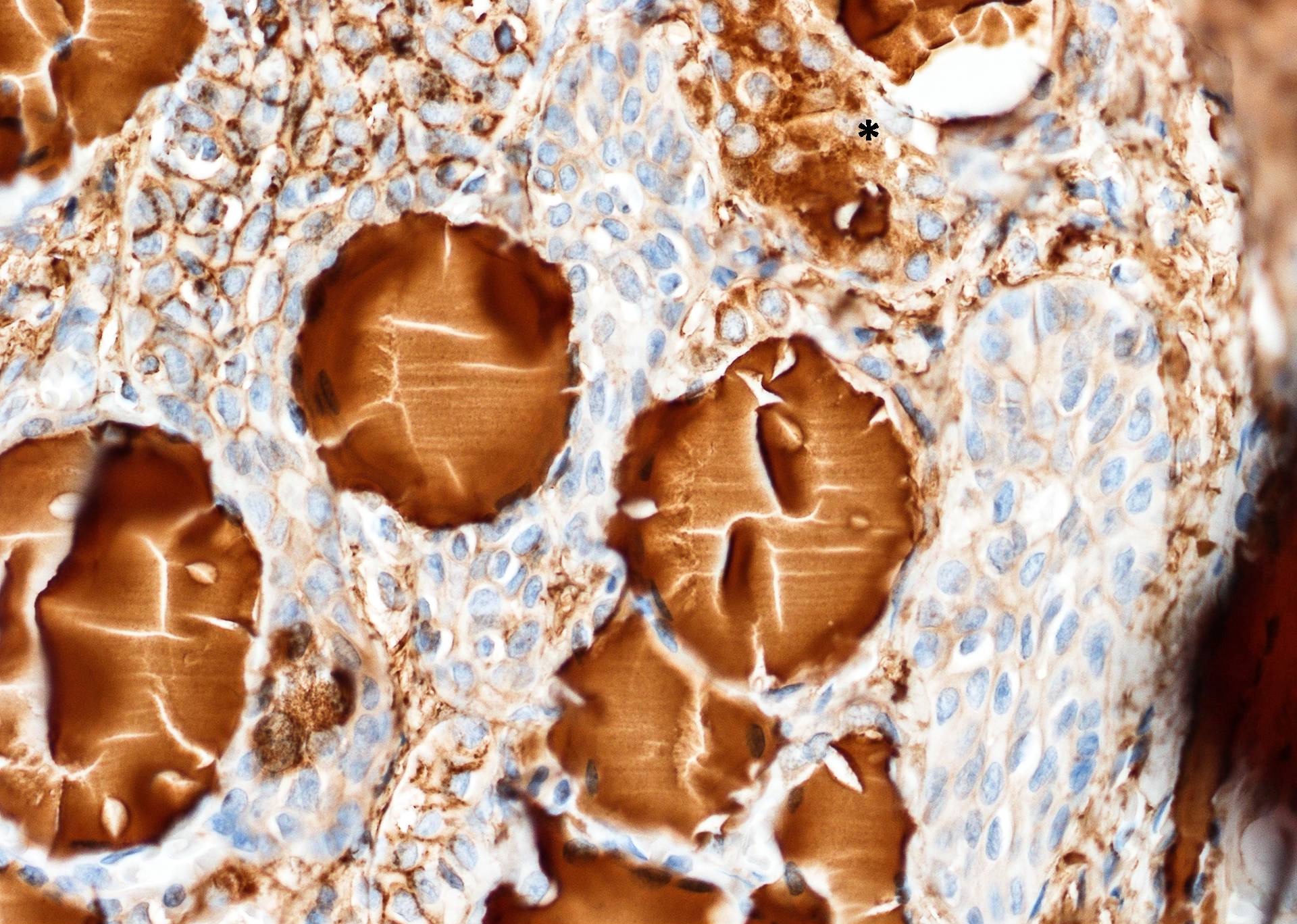
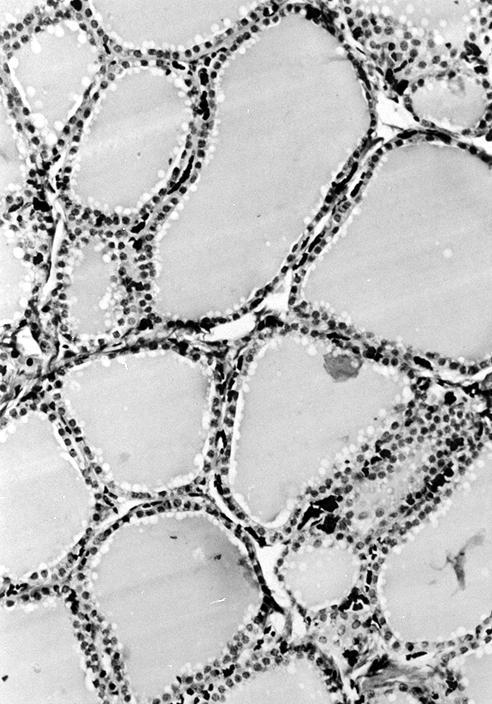
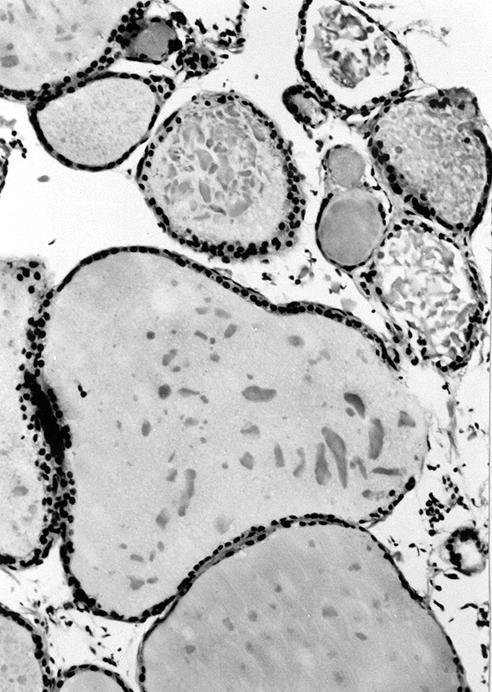
- Divided into lobules of 20 - 40 round to oval follicles, each 50 - 500 microns, with a single layer of cuboidal to low columnar epithelium
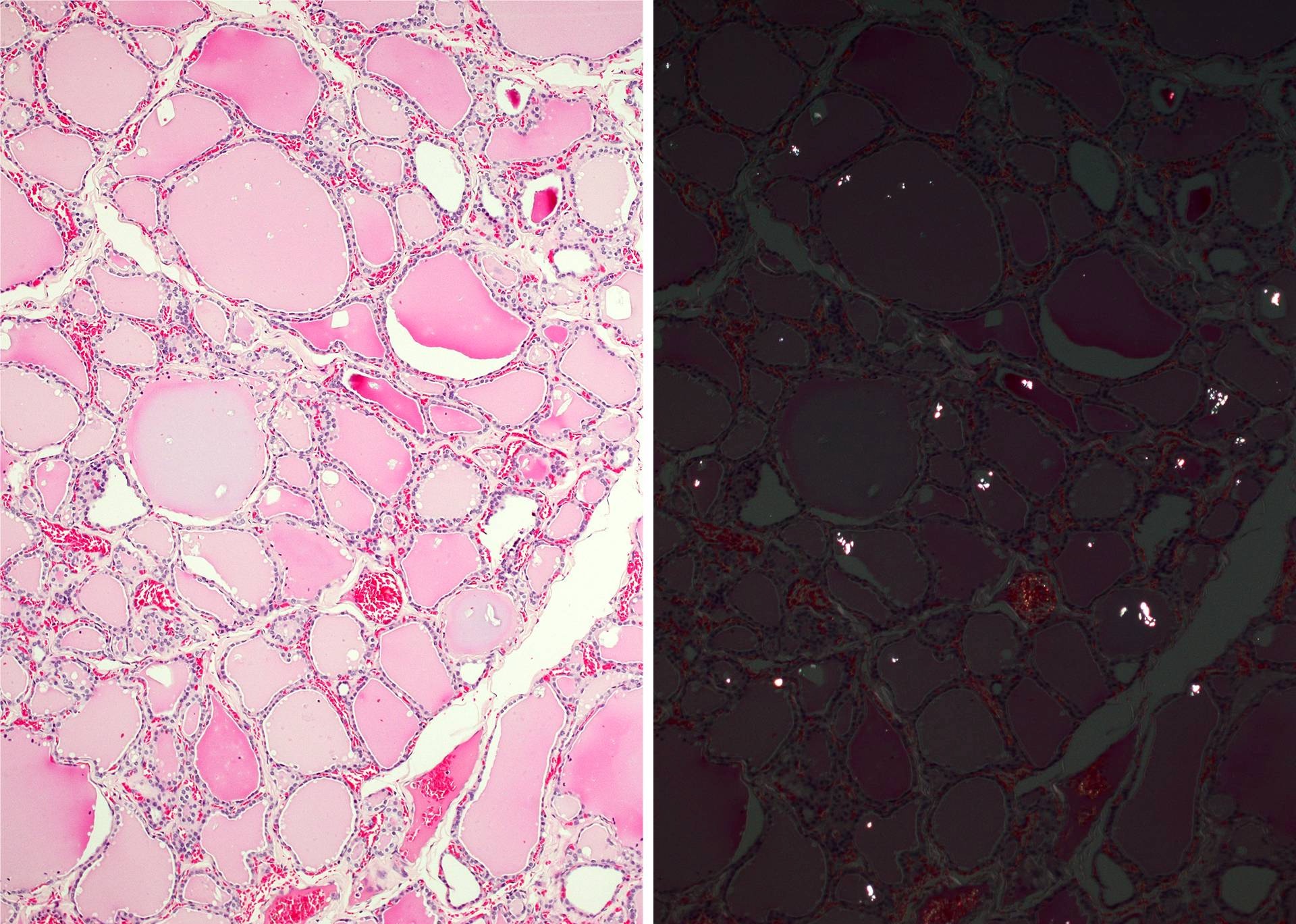
- Lumen contains colloid, which is scalloped and pale in follicles with active secretory activity, densely eosinophilic in inactive follicles and more flocculent ("like a clump or tuft of wool") and basophilic in elderly
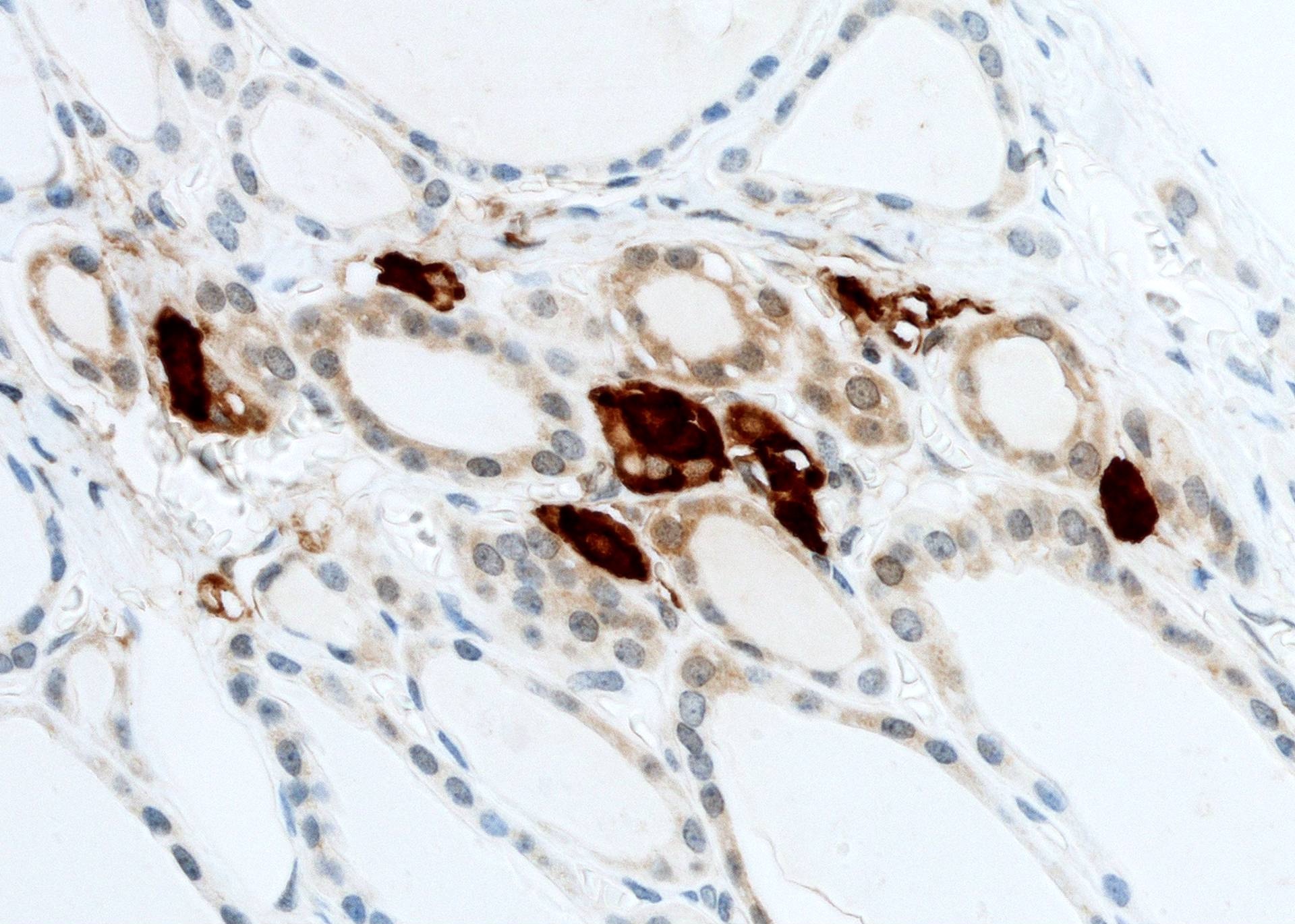
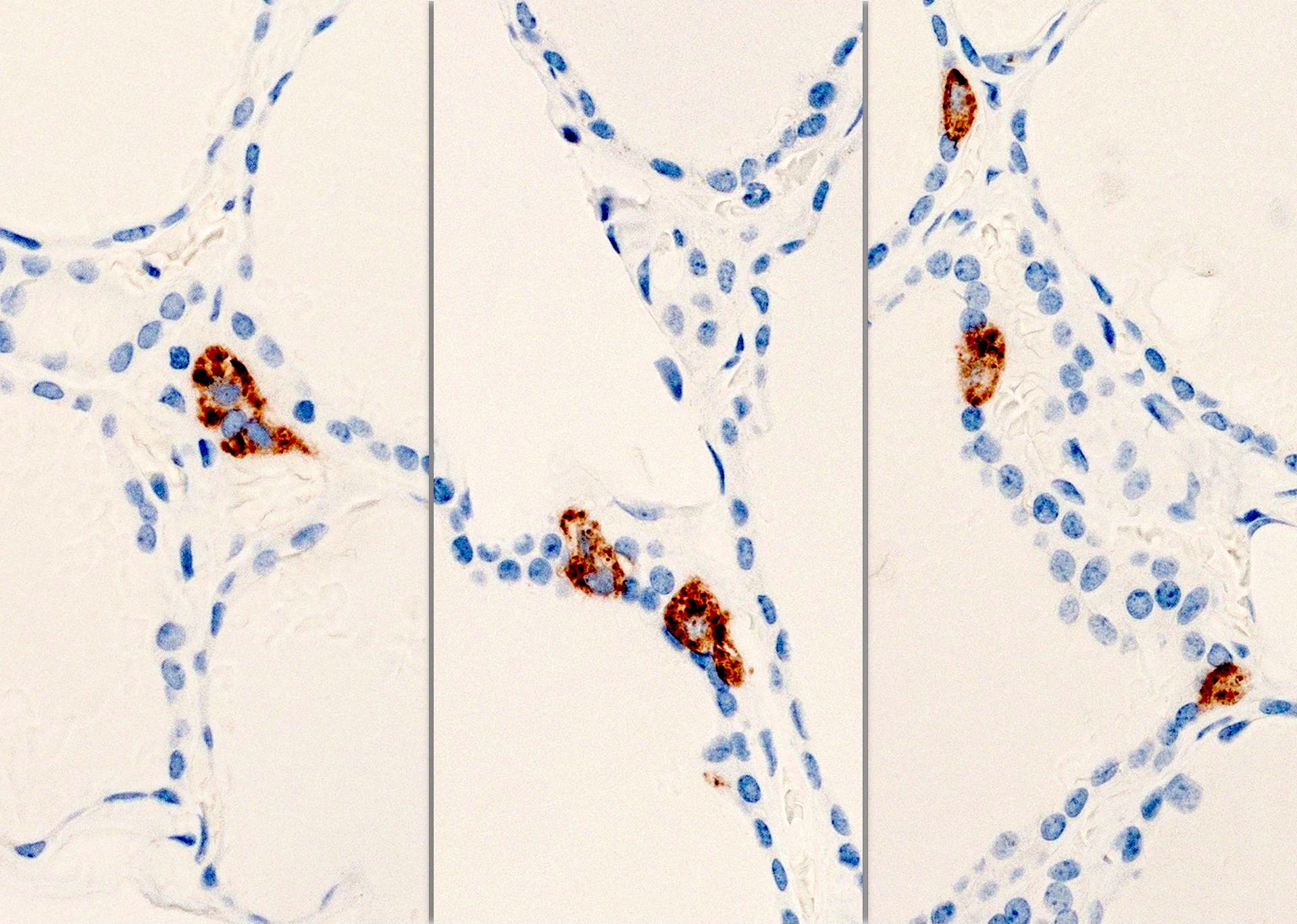
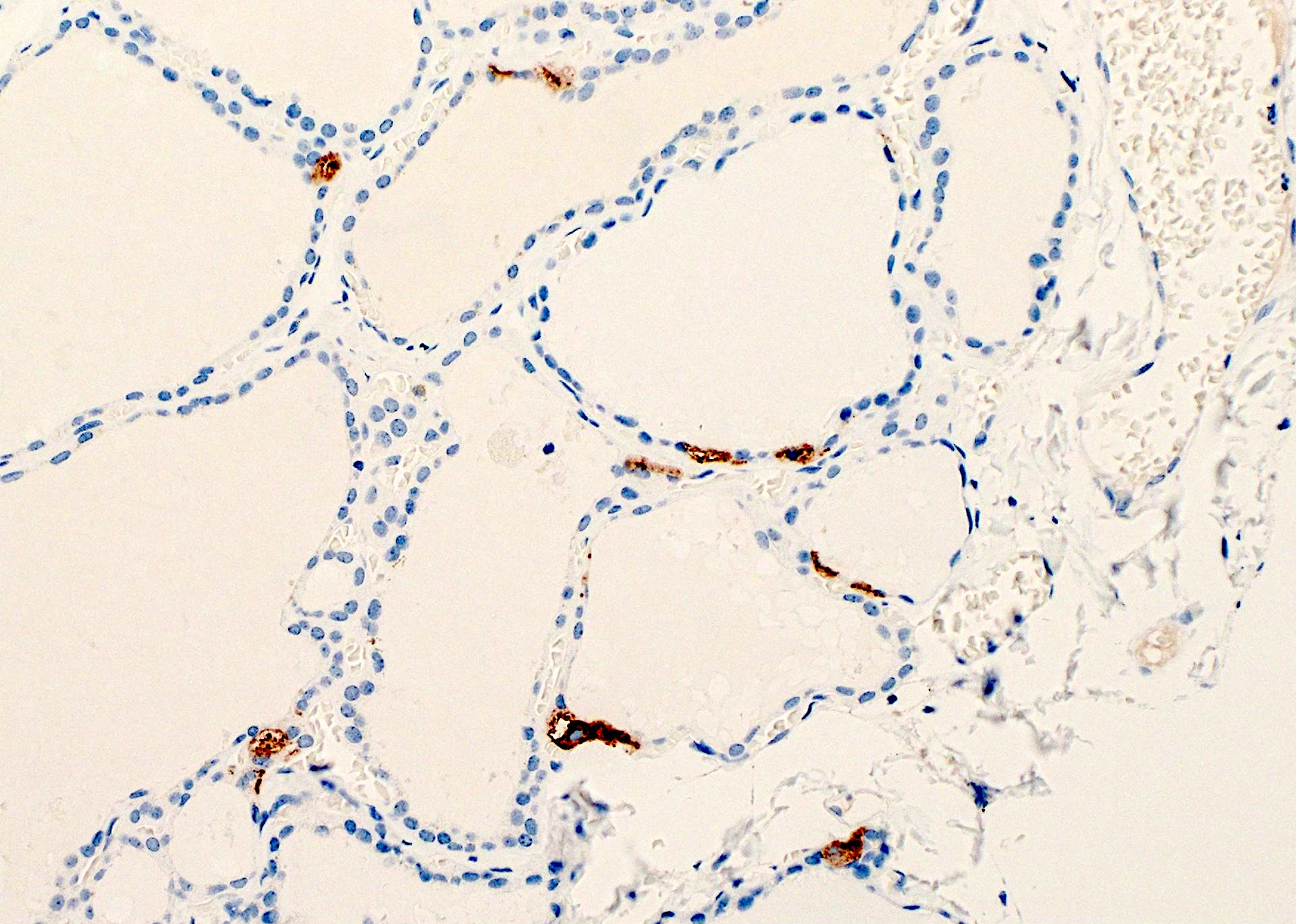
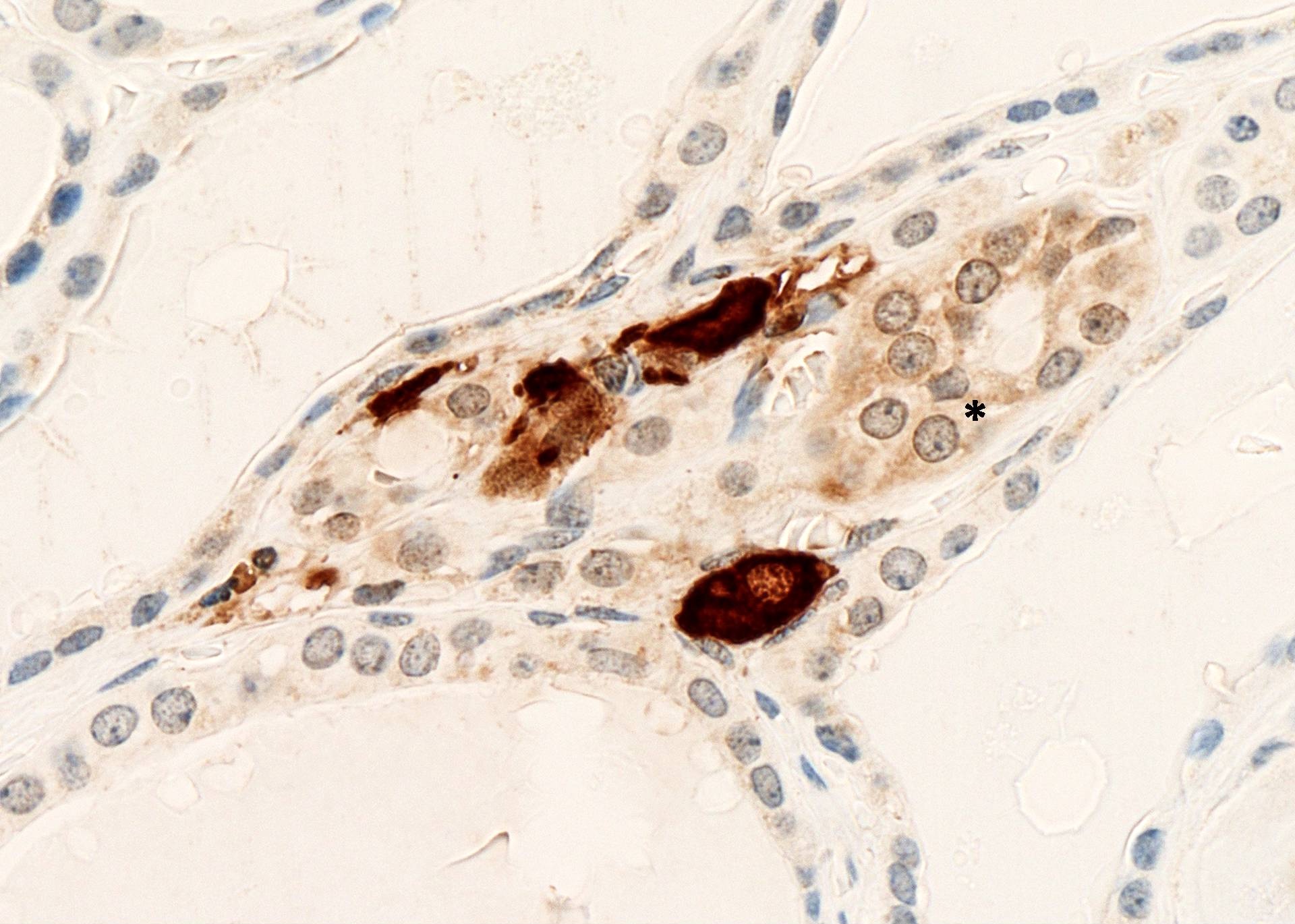
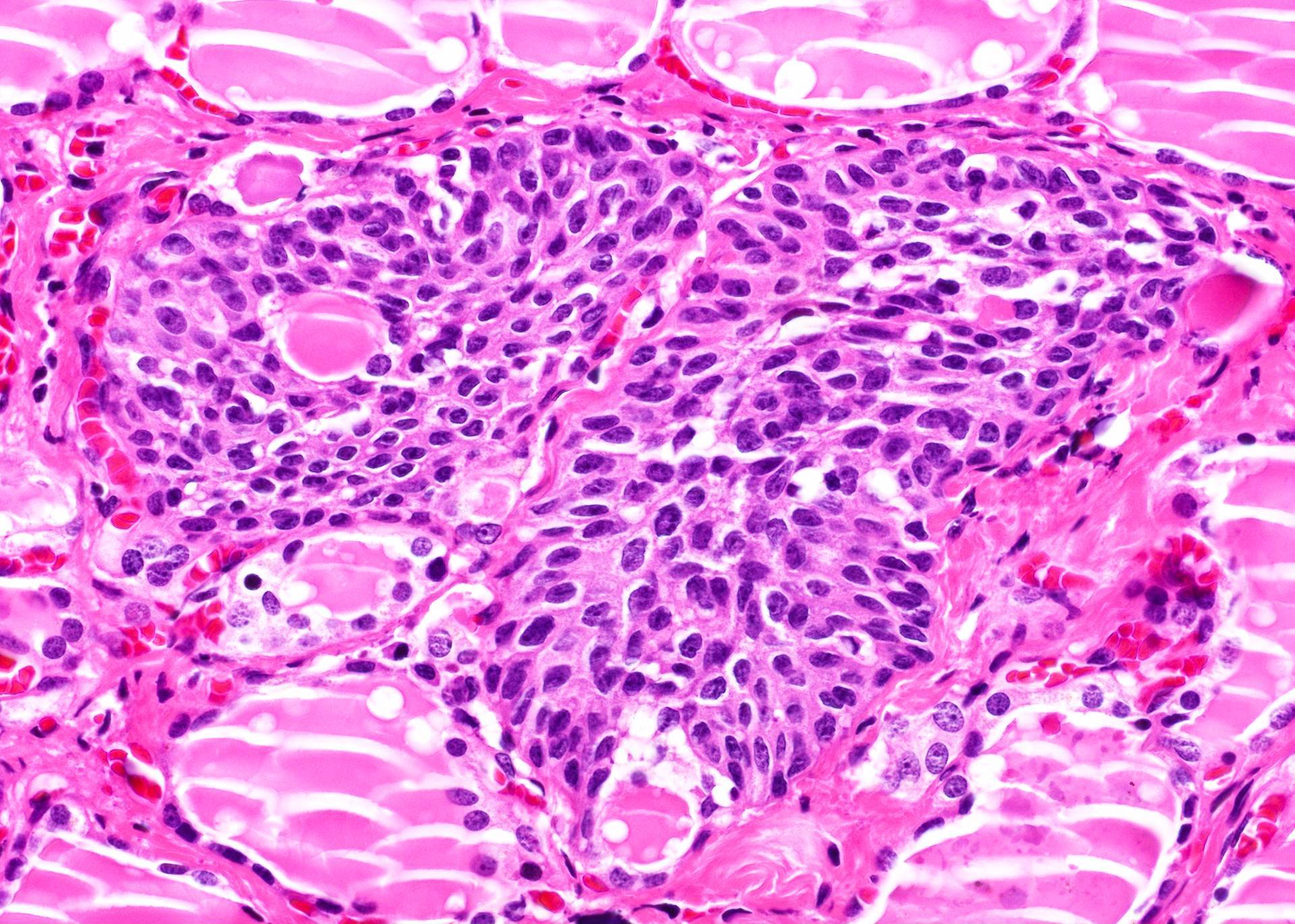
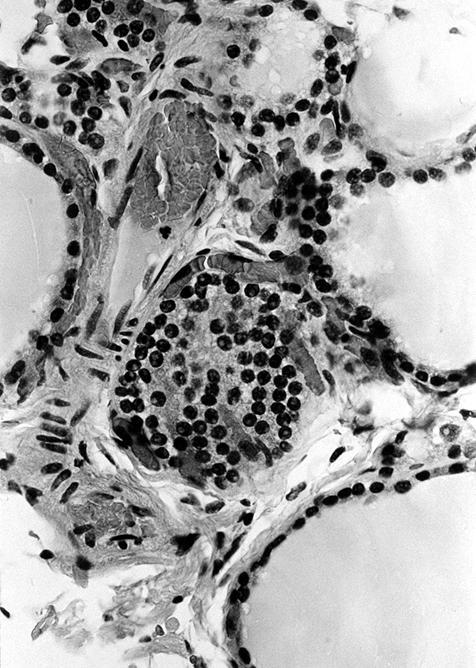
- Stroma contains C cells, formerly called parafollicular cells (actually are intrafollicular), derived from neural crest
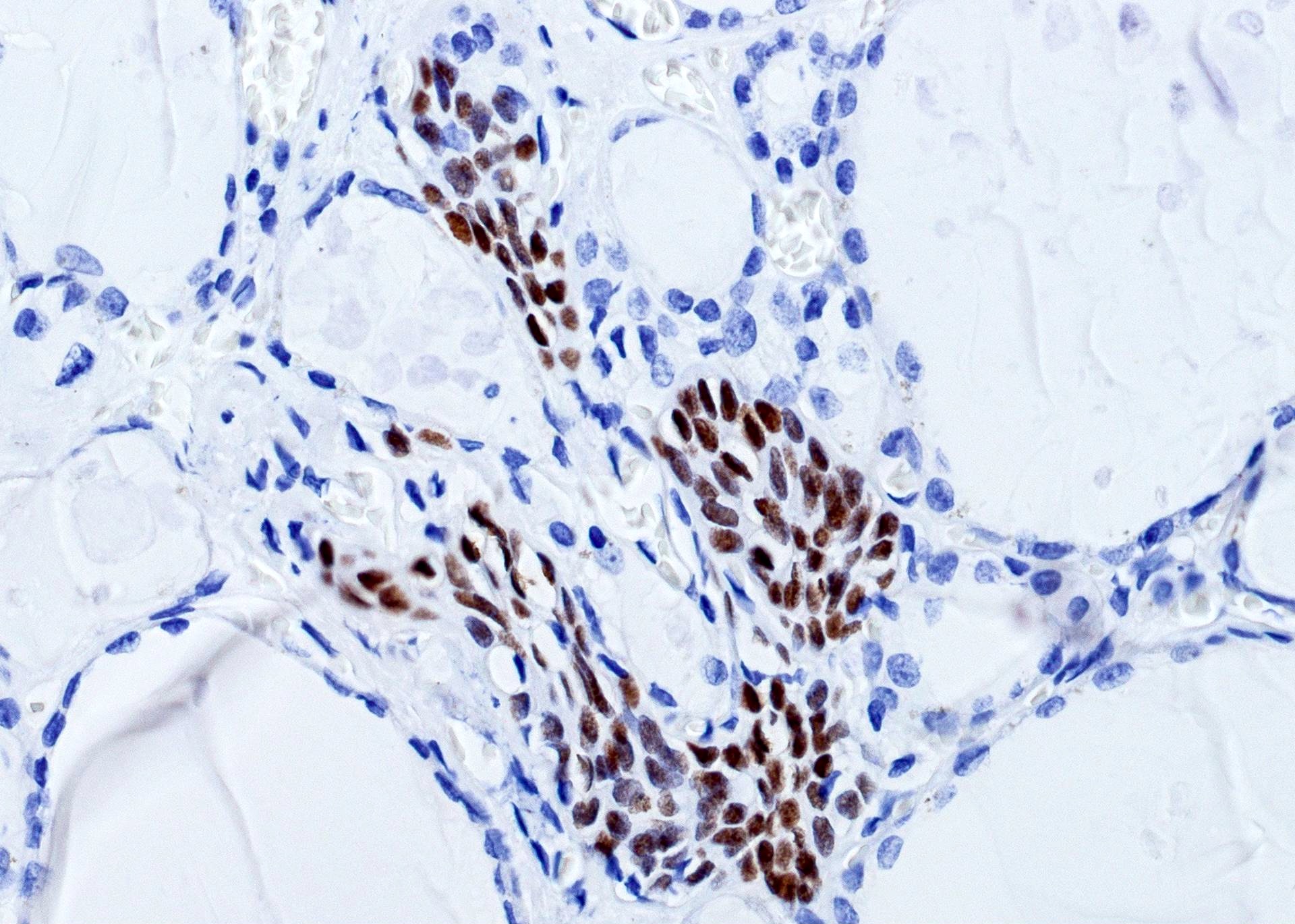
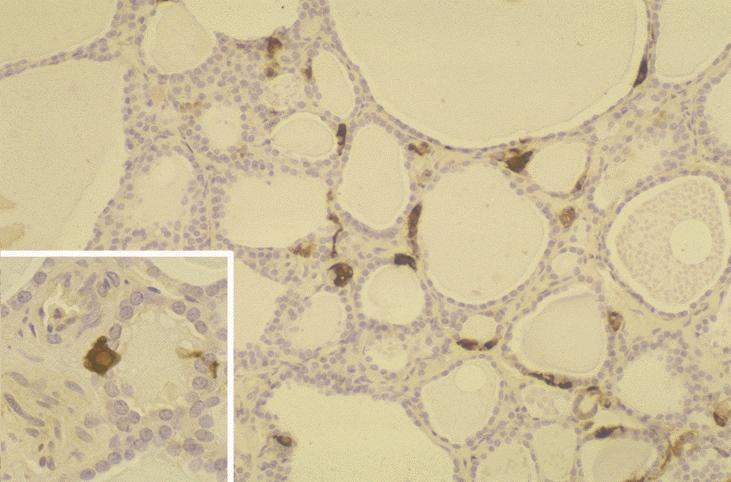
- C cells represent 0.1% of gland, produce calcitonin, are present in middle and upper third of lateral lobes along central axes, are not present in extreme upper and lower poles or in isthmus
- Usually 10 C cells per low power field in adults
- C cells are more numerous in neonates, decrease in adults, increase and appear as nodular aggregates after age 60 years
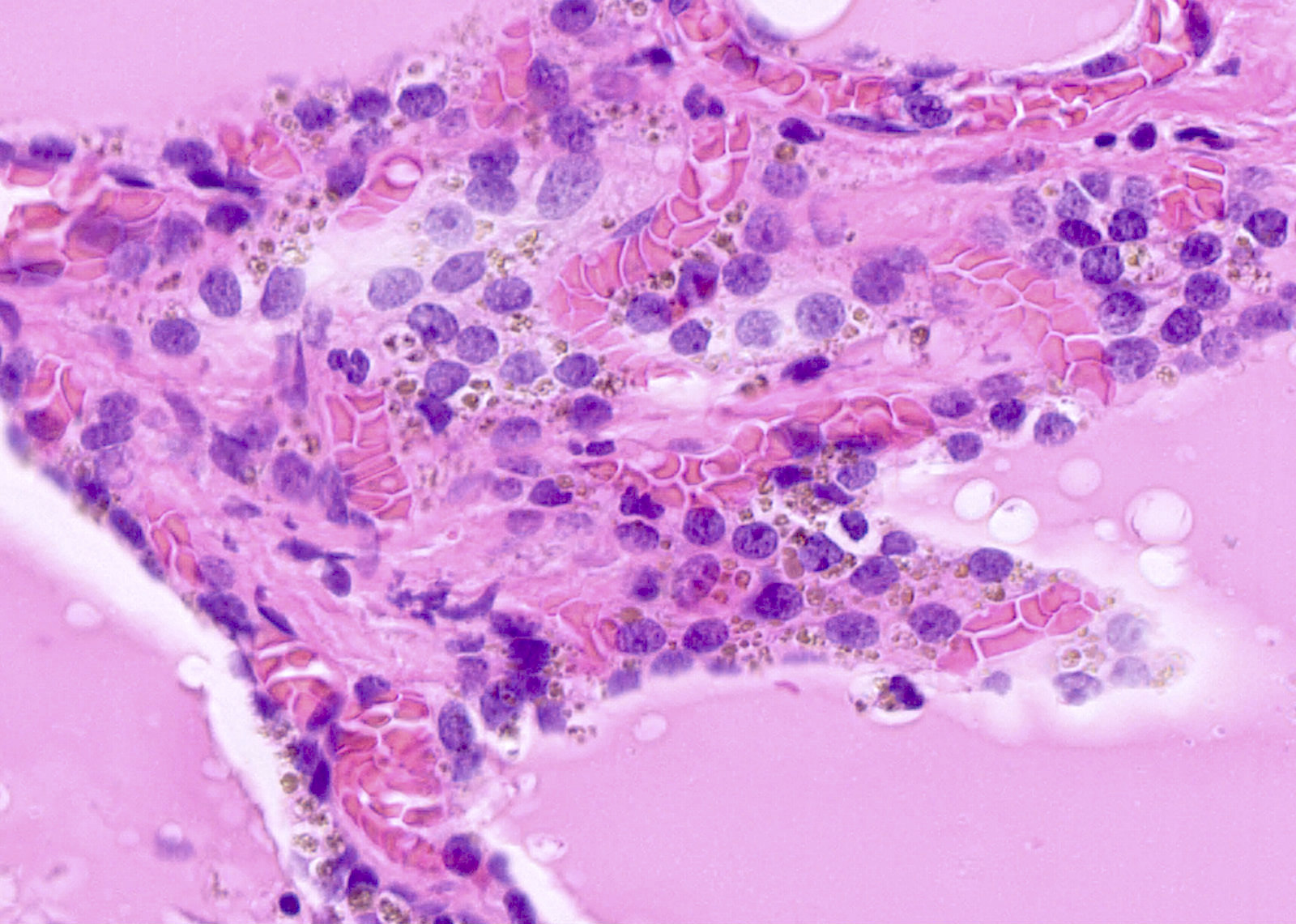
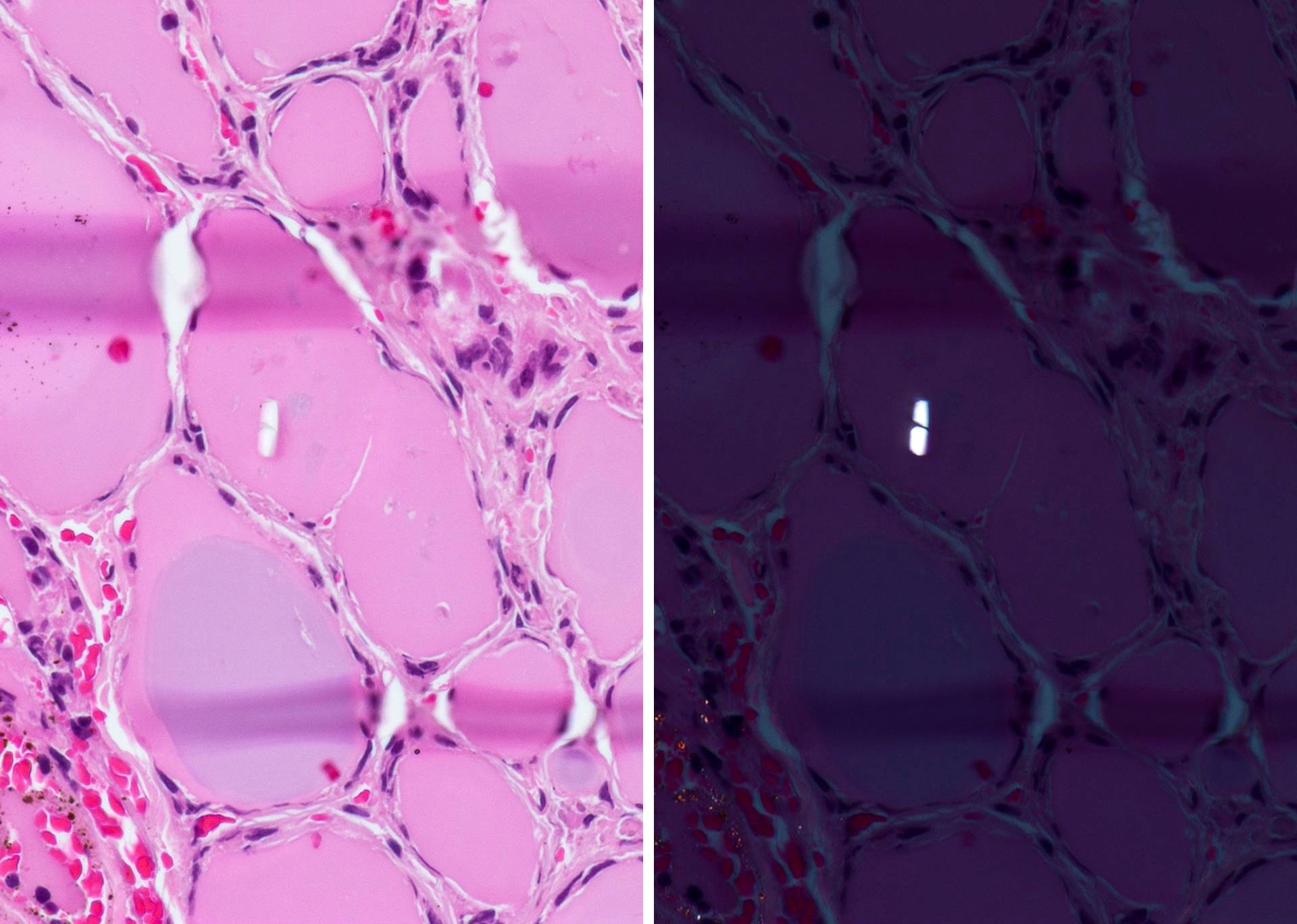
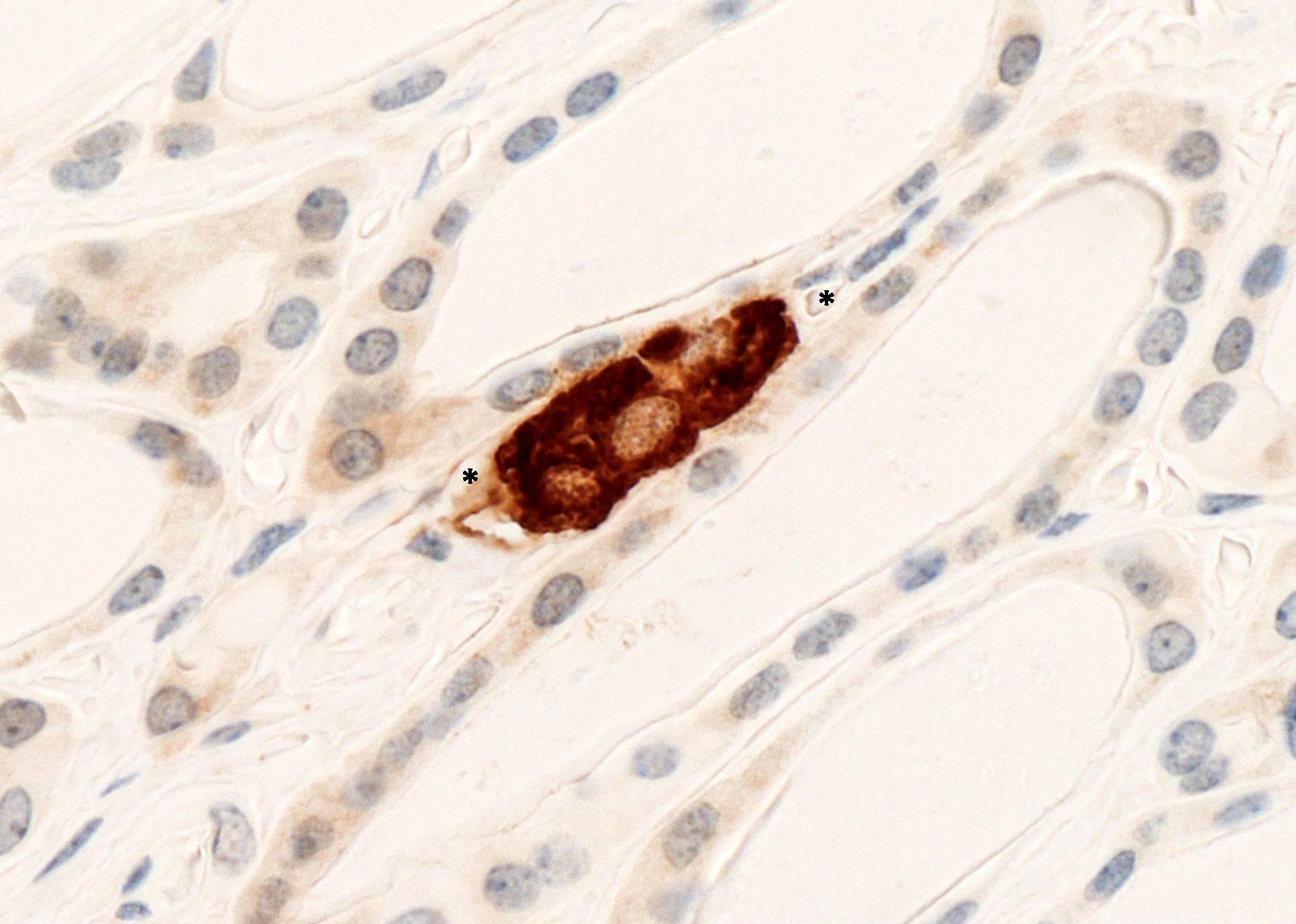
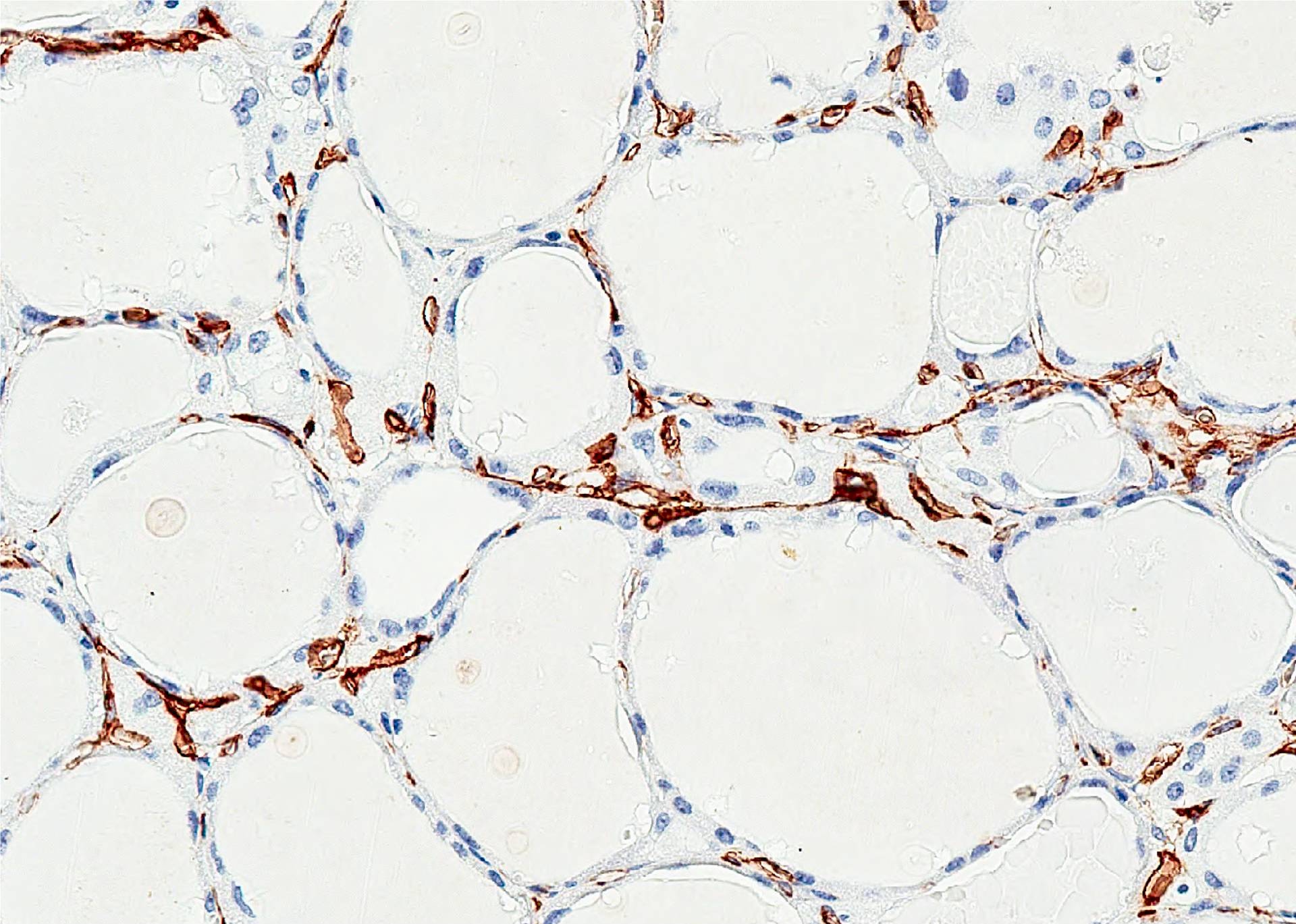
- C cells have pale / clear cytoplasm, oval nuclei, difficult to identify with H&E, use calcitonin stain
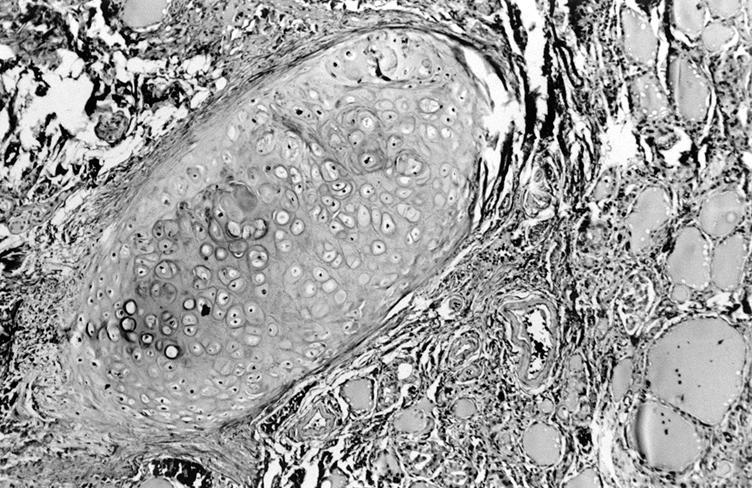
- Sanderson polsters: collections of small follicles projecting into lumen of large actively secreting follicles; may resemble papillary carcinoma
- Oncocytes (Hürthle cells, oxyphilic cells, Ashkenazy cells): large cells with abundant deeply eosinophilic granular cytoplasm and numerous mitochondria
Physiology
- Purpose of thyroid gland is to produce T4 and T3, which regulate metabolism, increase protein synthesis and increase oxygen consumption in all cells in body; T4 and T3 are also important for growth and development, and maturation of peripheral and central nervous system
- Hypothalamus releases thyroid releasing factor (TRF) into hypothalamic-pituitary portal blood circulation, which travels to pituitary, which releases thyroid stimulating hormone (TSH) into blood
- Follicular cells normally synthesize thyroglobulin and secrete it into follicular lumen
- Thyroid peroxidase, found in apical membrane of thyroid follicular cells, catalyzes iodination of tyrosine residues on thyroglobulin molecule and coupling of iodotyrosyl residues to form T4 (thyroxine) and T3, which are still bound to thyroglobulin, making them inactive; they are then stored as colloid
- In response to TSH, follicular cells pinocytose colloid, release the thyroglobulin, and secrete now active T4 and T3 into bloodstream
- Body needs 100 mg of iodide per day from diet to synthesize adequate T4; iodide uptake is mediated by human sodium iodide symporter, then oxidized to iodine by iodide peroxidase, which binds to tyrosine
- Most T4 / T3 is reversibly bound to thyroid binding globulin, which maintains levels within narrow limits
- Free T4 / T3 enters cells, binds to nuclear receptors, increases protein synthesis and catabolism of carbohydrates and fats (basal metabolic rate)
- Decreased serum T4 / T3 stimulates release of TRF and TSH via negative feedback regulation; elevated levels have opposite effect
- Chronically stimulated (hyperplastic) follicular cells are tall and columnar, may be papillary
- C cells secrete calcitonin, which lowers serum calcium by promoting bone absorption of calcium and inhibiting bone resorption by osteoclasts; in humans, has only a minor role in calcium homeostasis
- Major role of calcitonin may be to protect skeleton during periods of calcitonin stress, such as growth, pregnancy and lactation
- Goitrogens: suppress T4 / T3 synthesis by interfering with iodide uptake or other parts of biochemical pathways, causing an increased TSH, which causes goiter (enlargement of thyroid gland); examples include propylthiouracil, which inhibits oxidation of iodide and blocks T4 / T3 production; iodides in large doses, which inhibit thyroglobulin proteolysis; vegetables such as cabbage, turnips and cassava
- References: Nussey: Endocrinology, 2001, Wikipedia: Thyroid Hormones [Accessed 19 July 2018]
Clinical features
- Adipose metaplasia (mature adipose tissue between follicles or near capsule)
- Intrathyroidal cartilage, skeletal muscle or salivary gland
- Melanosis of follicular cells in old age (pigment granules also contain colloid, Ultrastruct Pathol 1998;22:401); see also Black thyroid
- Calcification is associated with vessels in elderly, has no laminations (in contrast to psammoma bodies)
- Squamous metaplasia is rare in normal thyroid, more common in thyroid disorders
Case reports
- 67 year old woman with thyroid nodule with adipose metaplasia in a nodular goiter (Indian J Pathol Microbiol 2007;50:369)
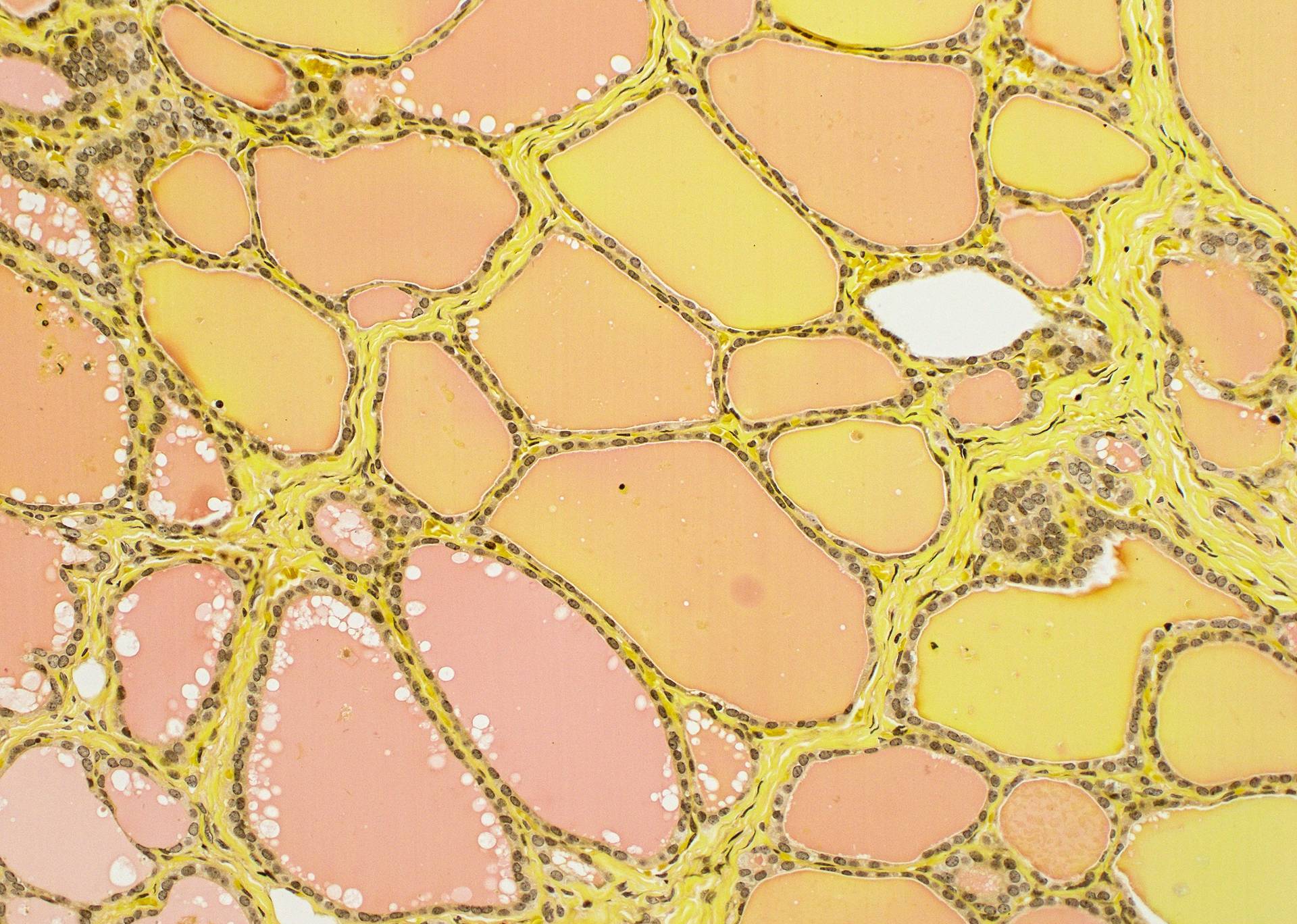
Microscopic (histologic) images
Contributed by Andrey Bychkov, M.D., Ph.D.
AFIP images
Images hosted on other servers:
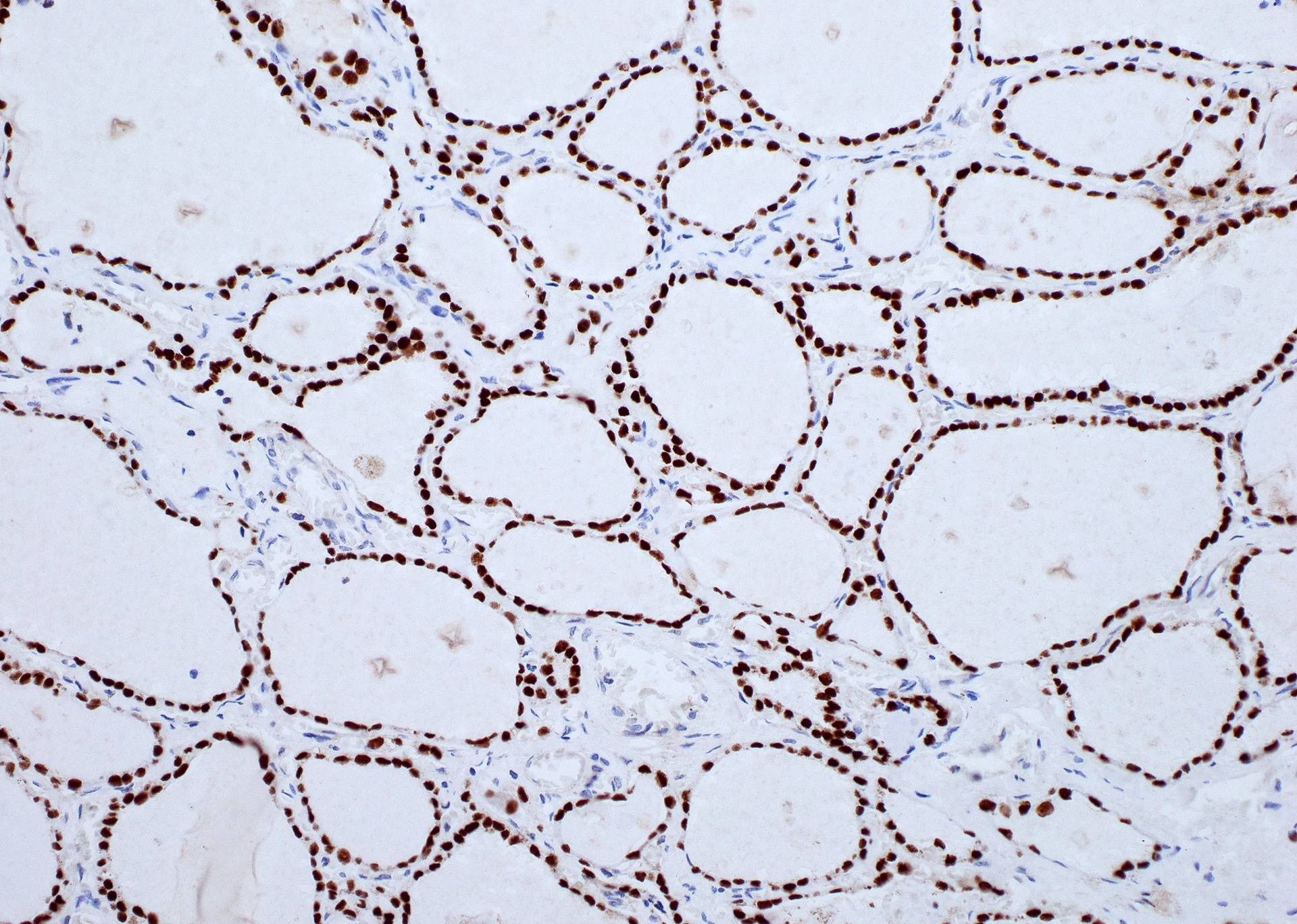
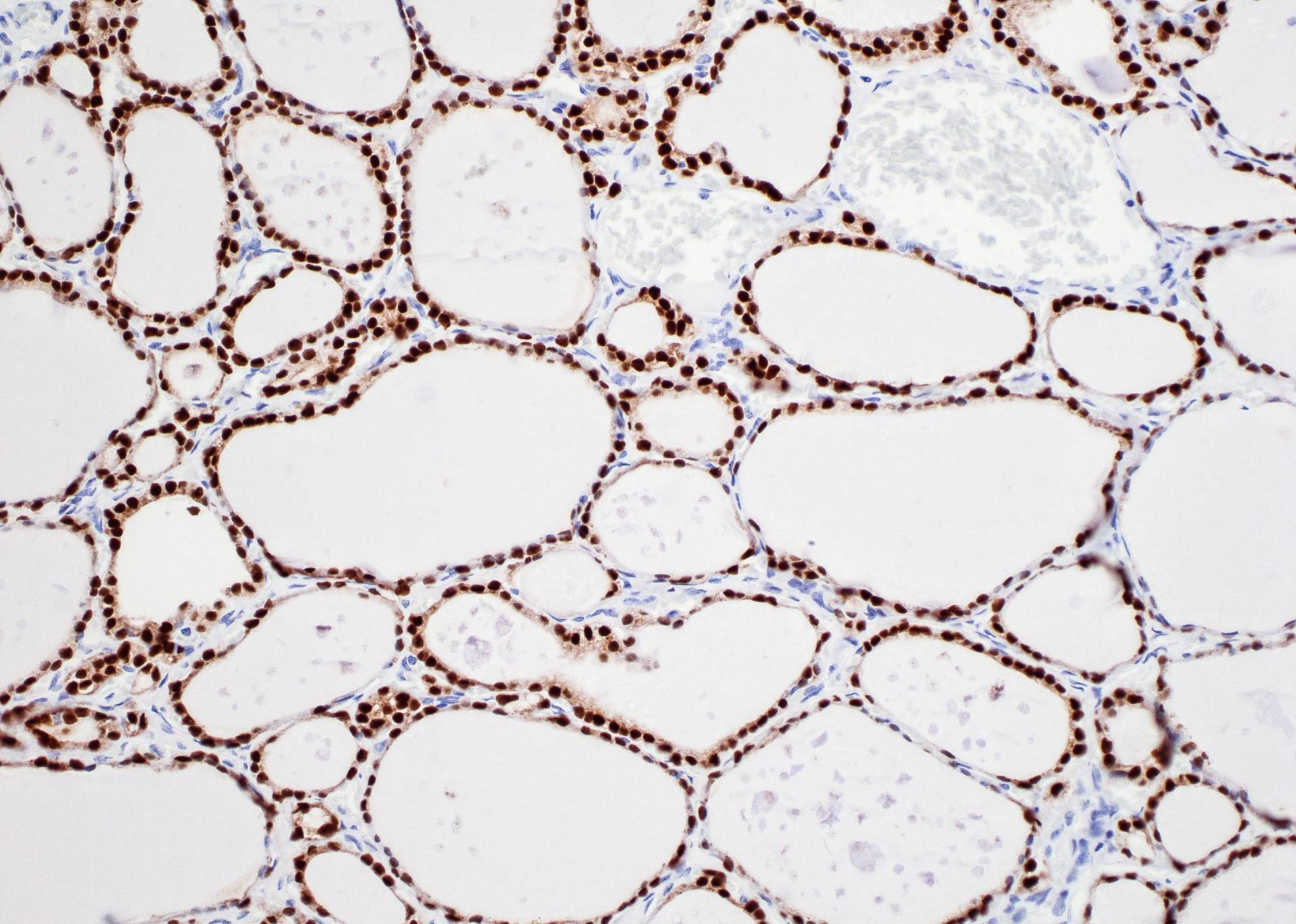
Positive stains
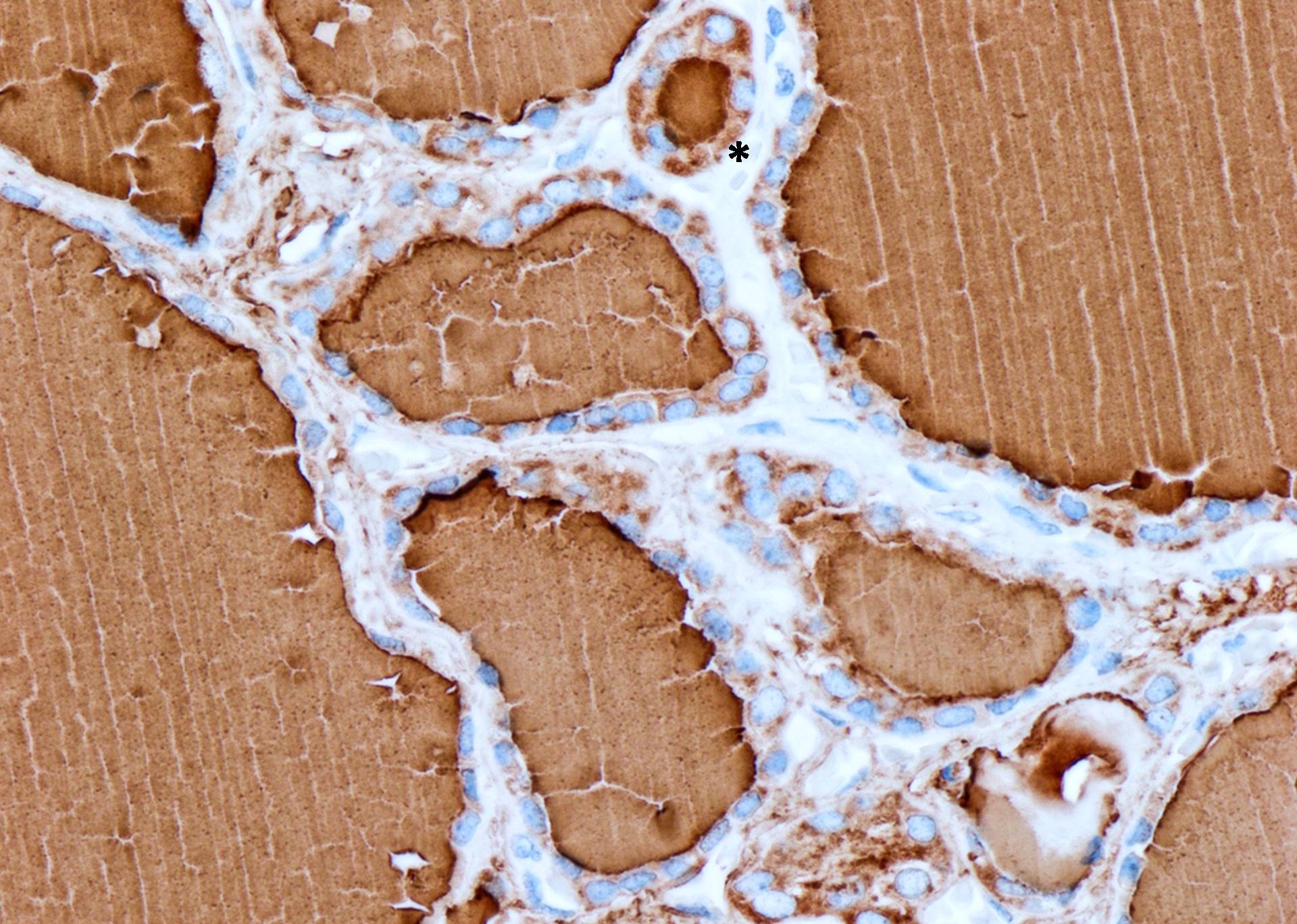
- Follicular cells: thyroglobulin (very specific, weaker staining in oncocytic cells), TTF1, low molecular weight keratin; also EMA, vimentin, T3 (triiodothyronine), T4 (thyroxine), ER beta (not alpha), PgR
- Note: thyroglobulin may leak out of follicular cells and create false positivity in adjacent cells
- Colloid: thyroglobulin, Alcian blue, PAS, T3, T4
- C cells: calcitonin, calcitonin gene related peptide (CGRP), neuron specific enolase, chromogranin A, synaptophysin, CEA, somatostatin; C cells are metachromatic with toluidine blue; C cells are NEGATIVE for thyroglobulin
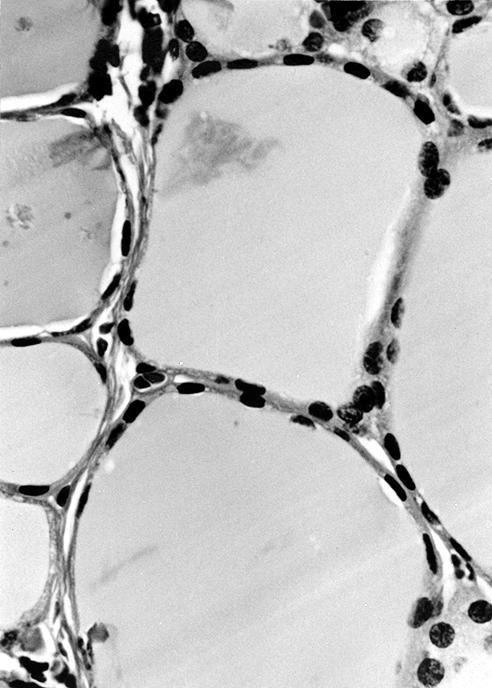
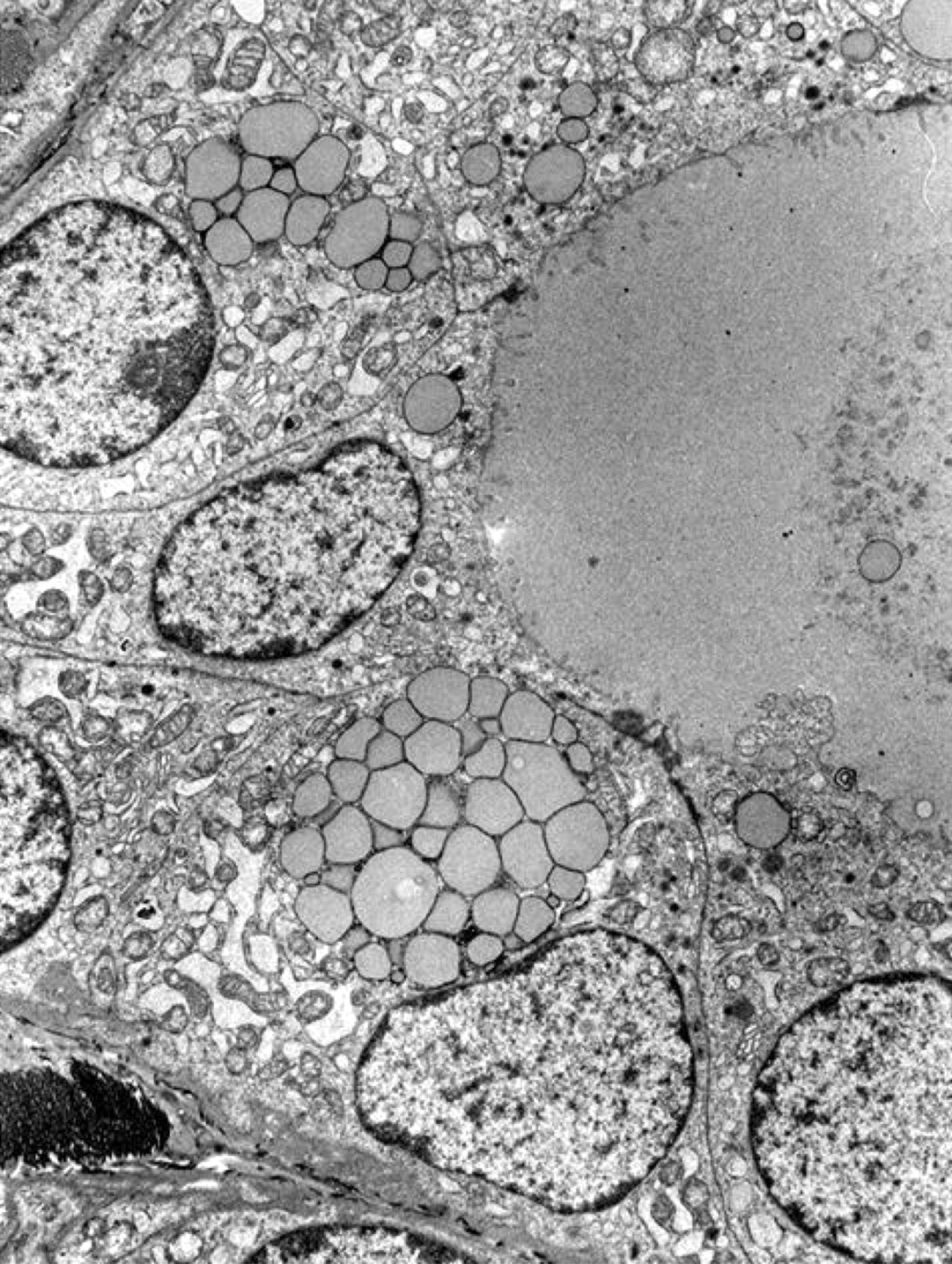
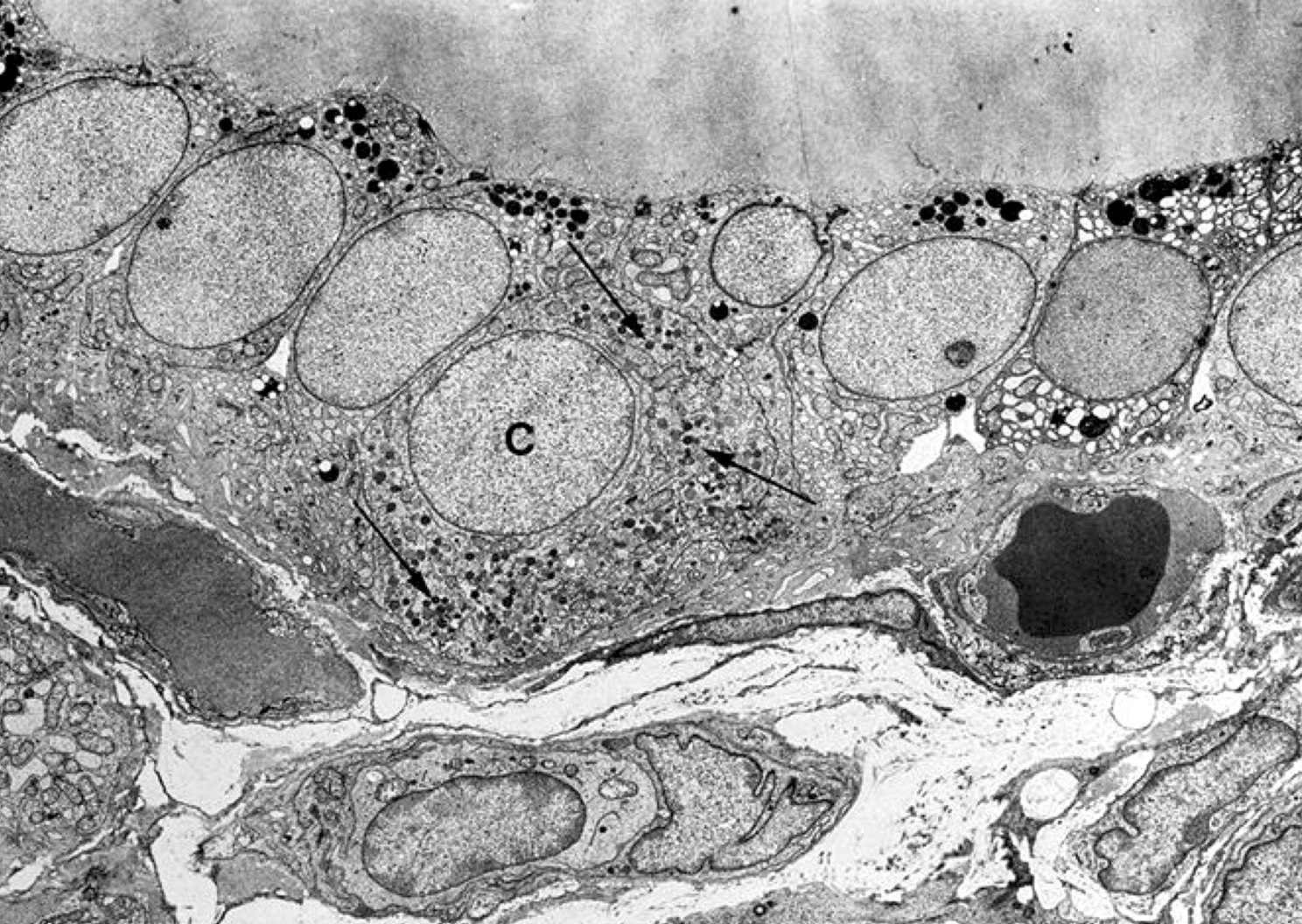
Electron microscopy description
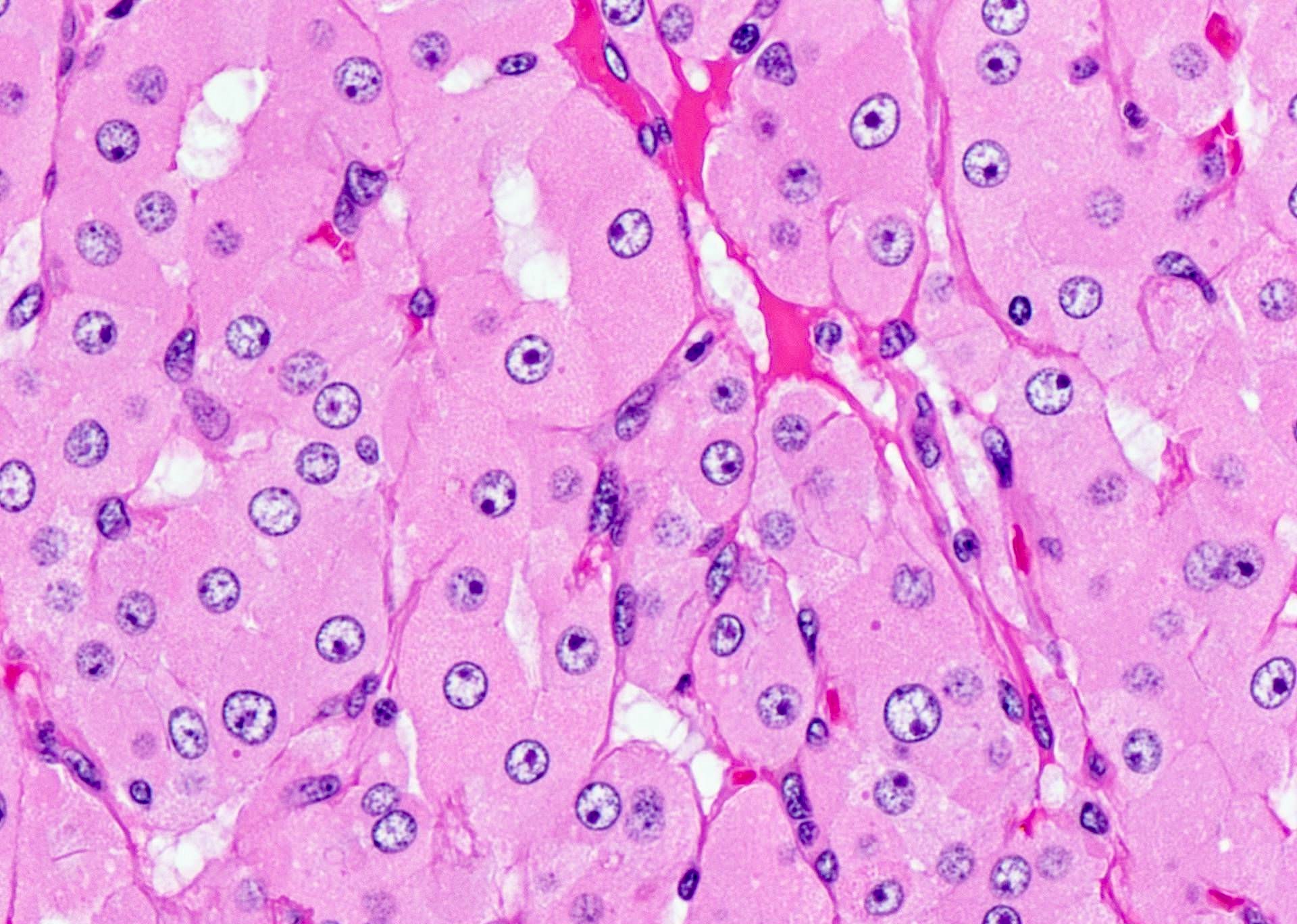
- Follicular cells: abundant granular endoplasmic reticulum, well developed Golgi, prominent lysosomes, luminal (apical) microvilli, well developed desmosomes with terminal bars between cells, small mitochondria, may contain lipofuscin; nuclei are round with homogeneous chromatin
- C cells: intrafollicular (separated from thyroid interstitium by follicular basal lamina), numerous dense core neurosecretory granules (type I are 280 nm, moderately electron dense and present in most C cells; type II are 130 nm, more electron dense and rare)
Electron microscopy images
Videos
By John R. Minarcik, M.D.