Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Diagrams / tables | Pathophysiology / etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Molecular / cytogenetics description | Differential diagnosisCite this page: Bychkov A. Ectopic thyroid tissue. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidheterotopic.html. Accessed April 25th, 2024.
Definition / general
- Developmental abnormality characterized by the presence of thyroid tissue in any location other than its normal anatomic position
- First well documented case was reported by Hickman in 1869 (AMA Arch Otolaryngol 1953;57:60)
Terminology
- Synonyms:
- Heterotopic thyroid, accessory thyroid, aberrant thyroid rests, choristoma
- Wolfler gland (cervical accessory thyroid), struma cordis (cardiac thyroid)
- Types:
- Sole / total ectopia vs. accessory thyroid (partial, associated with orthotopic thyroid)
- Single or multiple (dual, triple, etc.)
- Gross vs. microscopic
- True vs. mimickers (metastasis, parasitic nodule, see Differential Diagnosis)
Epidemiology
- The most frequent form of thyroid dysgenesis, accounting for ~50% of cases (Endocr Rev 2004;25:722)
- Several hundred cases of ectopic thyroid have been reported
- Prevalence in general population is 1 per 100,000 to 300,000 people
- Prevalence in population with thyroid disease is 1 per 4,000 to 8,000 (Thyroid 2007;17:1117); however intense imaging screening yields up to 2% of ectopic thyroid in patients with thyroid disease (Arch Endocrinol Metab 2015;60:231)
- Autopsy studies suggest that 7 - 10% of adults may have remnants of thyroid tissue along the path of thyroid descent (J Pathol 1970;102:239)
- F:M = 3 - 4:1
- May occur at any age, from 5 months to eighth decade but is most common at younger ages (Hormones (Athens) 2011;10:261)
Sites
- The target area for thyroid heterotopia lies along the track of medial anlage descent between the base of tongue and the normal thyroid location; a wider region can be defined as the Wolfler area, spanning from the edges of the mandible through the neck to the aortic arch (Nikiforov: Diagnostic Pathology and Molecular Genetics of the Thyroid, 2nd Edition, 2012)
- Sites in descending order of frequency:
- Lingual thyroid is the most common type, accounting for up to 90% of the cases
- Often found within thyroglossal duct cysts (25 - 65%, more sections yield higher percentage)
- Neck midline organs (larynx and trachea) and superior mediastinum
- Benign thyroid follicles occur in perithyroid soft tissue and muscles (often around isthmus), which are silent and harmless (Hum Pathol 1988;19:689)
- Nonmidline sites, including salivary glands, retropharyngeal space, cervical lymph nodes and branchial cleft cysts
- Distant sites are rare (categorized in Case reports)
- Thyroid tissue in ovary (struma ovarii) represents a component of teratoma, sometimes in the absence of other tissues (monodermal teratoma)
Pathophysiology / etiology
- Thyroid anlages may descend too slow or fast and develop ectopia above or below normal thyroid position
- Heart, large vessels and thymus originate very close to the primordial thyroid and attachment of thyroid tissue may occur before their caudal migration
- Developmental anomalies of the foregut may explain ectopia in the thorax and upper gastrointestinal tract (Nikiforov: Diagnostic Pathology and Molecular Genetics of the Thyroid, 2nd Edition, 2012)
- Aberrant thyroid tissue in the submandibular and lateral neck regions could originate from a defective lateral thyroid component that cannot migrate and fuse with the median thyroid anlage (Endocr Rev 2004;25:722)
- Heterotopic differentiation (heteroplasia, transdifferentiation) of uncommitted endodermal cells may hypothetically explain the presence of ectopic thyroid tissues in distant locations (Thyroid 2003;13:503)
- Mutation in the genes of thyroid specific transcription factors TTF1, TTF2 (FOXE1) and PAX8 may be involved in abnormal migration of the thyroid, as shown in animals (Nat Genet 1998;19:395)
- However, no mutation in known genes has so far been associated with the human ectopic thyroid
- Rarely, familial thyroid heterotopia occurs (Thyroid 1992;2:325)
Clinical features
- Most cases are asymptomatic, and detected incidentally
- Symptoms are usually related to size / location of heterotopia and associated thyroid dysfunction
- Ectopic thyroid is commonly detected during puberty and pregnancy, when increased levels of thyrotropin stimulates enlargement of the ectopic thyroid tissue (Hormones (Athens) 2011;10:261)
- This enlargement may manifest with compression (airway obstruction) or swelling (neck mass) symptoms
- Heterotopia due to aberrant migration has inadequate blood supply and is not able to release sufficient amount of hormones (Development 2006;133:3797)
- Presentation with features of hypothyroidism occurs often in children (Laryngoscope 2008;118:1174)
- Hyperthyroidism arising from ectopic thyroid tissue is rare (Thyroid 2000;10:363)
- Ectopic thyroid tissue may be the only functioning thyroid tissue in ~50% of cases, particularly with lingual and cervical heterotopia (Eur J Endocrinol 2011;165:375)
- Heterotopic thyroid may have the same diseases as eutopic thyroid gland, including:
- Nodular goiter (Hormones (Athens) 2009;8:150) but most mediastinal goiters are actually parasitic nodules and not ectopic thyroid tissue
- Inflammatory diseases, e.g. Hashimoto thyroiditis (Otolaryngol Head Neck Surg 2001;125:274) and Graves disease (Endocr J 1999;46:731)
- Neoplasms, both benign (AJR Am J Roentgenol 2008;190:W161) and malignant (J Clin Endocrinol Metab 2011;96:2684), with a frequency comparable to orthotopic thyroid tumors (Thyroid 2015;25:1050)
Diagnosis
- Thyroid cancer metastases should always be considered and excluded before accepting the diagnosis of ectopic thyroid
- Imaging:
- Radionuclide imaging with technetium-99m pertechnetate, iodine-131 or iodine-123
- CT and MRI
- Ultrasonography with color Doppler
- FNA
Laboratory
- Hypothyroidism (low T3 and T4, high TSH) occurs frequently
- The inability to image the normal gland combined with a normal serum thyroglobulin may suggest an ectopic thyroid
Radiology description
- Scintigraphy: radioisotope tracer uptake in the area other than normal thyroid location (background from salivary glands should be considered)
- Ectopic thyroid tissue has a characteristic uniform high attenuation on non contrast CT, while on MRI it shows an elevated signal on T1 and T2 weighted images compared with the surrounding musculature (Int J Surg 2014;12:S3)
- Sonography: echotexture of thyroid tissue; usually isoechogenic, with regular margins, rare cystic degeneration, and without calcification (Arch Endocrinol Metab 2015;60:231)
Radiology images
Prognostic factors
- Prognosis is good: there is a very low chance of recurrence after surgical excision
Case reports
- Lingual
- Neck:
- 32 year old man with supraclavicular thyroid tissue (Internet J Surg 2007;13(1))
- 32 year old woman with parotid gland tissue (Singapore Med J 2004;45:437)
- 33 year old pregnant woman with intratracheal ectopic thyroid tissue with adenomatous hyperplasia (AJR Am J Roentgenol 2008;190:W161)
- 35 year old woman with cutaneous thyroid tissue (J Cutan Pathol 2004;31:195)
- 36 year old woman with thyroid papillary carcinoma arising in ectopic thyroid tissue within a neck branchial cyst (World J Surg Oncol 2006;4:24)
- 40 year old man with intratracheal ectopic thyroid tissue (Ear Nose Throat J 2007;86:406)
- 59 year old woman with intralaryngeal thyroid (Otolaryngol Pol 2014;68:46)
- 61 year old woman with ectopic thyroid gland in the mandible (J Oral Maxillofac Surg 2012;70:363)
- 64 year old woman with ectopic thyroid tissue surrounding laryngeal nerve (Int J Clin Exp Pathol 2014;7:5313)
- 65 year old woman with thyroid tissue in submandibular and infrahyoid region (Eurasian J Med 2014;46:216)
- Mediastinum and thorax:
- 33 year old woman with intracardiac ectopic thyroid adenoma (Interact Cardiovasc Thorac Surg 2009;8:587)
- 42 year old woman with ectopic thyroid gland on the ascending aorta (Surg Today 2007;37:486)
- 46 year old woman with intracardiac ectopic thyroid mass (Interact Cardiovasc Thorac Surg 2013;17:903)
- 51 year old man with intrapericardial ectopic thyroid (Int J Cardiol 2012;158:e55)
- 61 year old woman with ectopic thyroid mass in the heart (Lancet 2012;379:1762)
- 65 year old man with mediastinal ectopic thyroid (Korean J Intern Med 2013;28:361)
- 66 year old woman with ectopic thyroid tissue in the lateral chest wall (Acta Cytol 2009;53:313)
- 74 year old man with ectopic thyroid tissue in posterior mediastinum (Cases J 2008;1:53)
- 74 year old woman with intracardiac ectopic thyroid mass (Eur J Echocardiogr 2009;10:704)
- 77 year old man with ectopic thyroid of the lung (Pathologica 2010;102:102)
- Two cases in anterior mediastinum (J Bras Pneumol 2009;35:383)
- Subdiaphragmatic:
- Fetus with heterotopic thyroid tissue at the porta hepatis (Virchows Arch 2000;436:498)
- 16 year old girl with gastric heterotopia containing thyroid tissue (J Pediatr Gastroenterol Nutr 2007;45:484)
- 29 year old woman with ectopic thyroid tissue in gallbladder (Endocr Pathol 2010;21:263)
- 32 year old woman and 51 year old woman with ectopic thyroid tissue in the adrenal gland (Int J Surg Pathol 2015;23:170, Endocr Pathol 2014;25:353)
- 45 year old woman with ectopic thyroid tissue in the uterus (Acta Obstet Gynecol Scand 2005;84:201)
- 50 year old woman with ectopic thyroid tissue in the pancreas (Surg Today 1999;29:472)
- 54 year old woman with adrenal mass (BMC Urol 2006;6:18)
- 63 year old man with thyroid follicles in the submucosa of the duodenum (Virchows Arch A Pathol Anat Histopathol 1991;418:547)
- 71 year old woman with liver mass (Clin Gastroenterol Hepatol 2012;10:xxx)
- Female with thyroid and parathyroid glands in the vaginal wall (Am J Clin Pathol 1973;59:503)
- Two cases in adrenal gland (Hum Pathol 1999;30:105)
- Other unique sites:
- 15 year old boy with ectopic thyroid tissue in the iris (Arch Ophthalmol 2006;124:1497)
- 19 year old woman with thyroid nodule of the breast (Breast J 2016;22:240)
- 43 year old woman with thyroid tissue in the axilla (Thyroid 2005;15:1095)
- Two cases of thyroid tissue in pituitary (Chin Med J (Engl) 2015;128:3389)
- Multiple sites:
- 5 year old girl with dual ectopic thyroid (Iran J Radiol 2011;8:29)
- 10 year old girl with triple ectopic thyroid (Thyroid Disorders Ther 2013;2:126)
- 16 year old girl with triple ectopic thyroid (Med J Armed Forces India 2012;68:173)
- 17 year old girl with dual ectopic thyroid (J Thyroid Res 2011;2011:159703)
- 37 year old woman with adenomatous hyperplasia arising from dual ectopic thyroid (Clin Exp Otorhinolaryngol 2009;2:155)
- 42 year old woman with triple ectopic thyroid (Indian J Endocrinol Metab 2014;18:238)
Treatment
- Asymptomatic euthyroid patients do not usually require therapy but are kept under observation
- Mild hypothyroidism is corrected by thyroid hormones
- Radioiodine ablation is indicated for patients who are symptomatic or unresponsive to medical treatment (BMJ Case Rep 2015 Aug 3; 2015)
- Surgical excision is indicated for severe obstructive symptoms, bleeding, ulceration, cystic degeneration or malignancy (Thyroid 2007;17:1117)
- It is important to determine the presence of an orthotopic thyroid gland before removing ectopic tissue to avoid hypothyroidism, because the ectopic gland may be the only functional thyroid (Hormones (Athens) 2011;10:261)
- Autotransplantation may help retain some degree of thyroid function
Gross description
- Average size of manifested lesion is 2 - 4 cm, range is 0.2 - 7.3 cm (Int J Clin Exp Pathol 2014;7:5313, J Thorac Dis 2014;6:E39)
- Often encapsulated, can be cystic
- Cut surface resembles normal thyroid parenchyma (brownish red)
Gross images
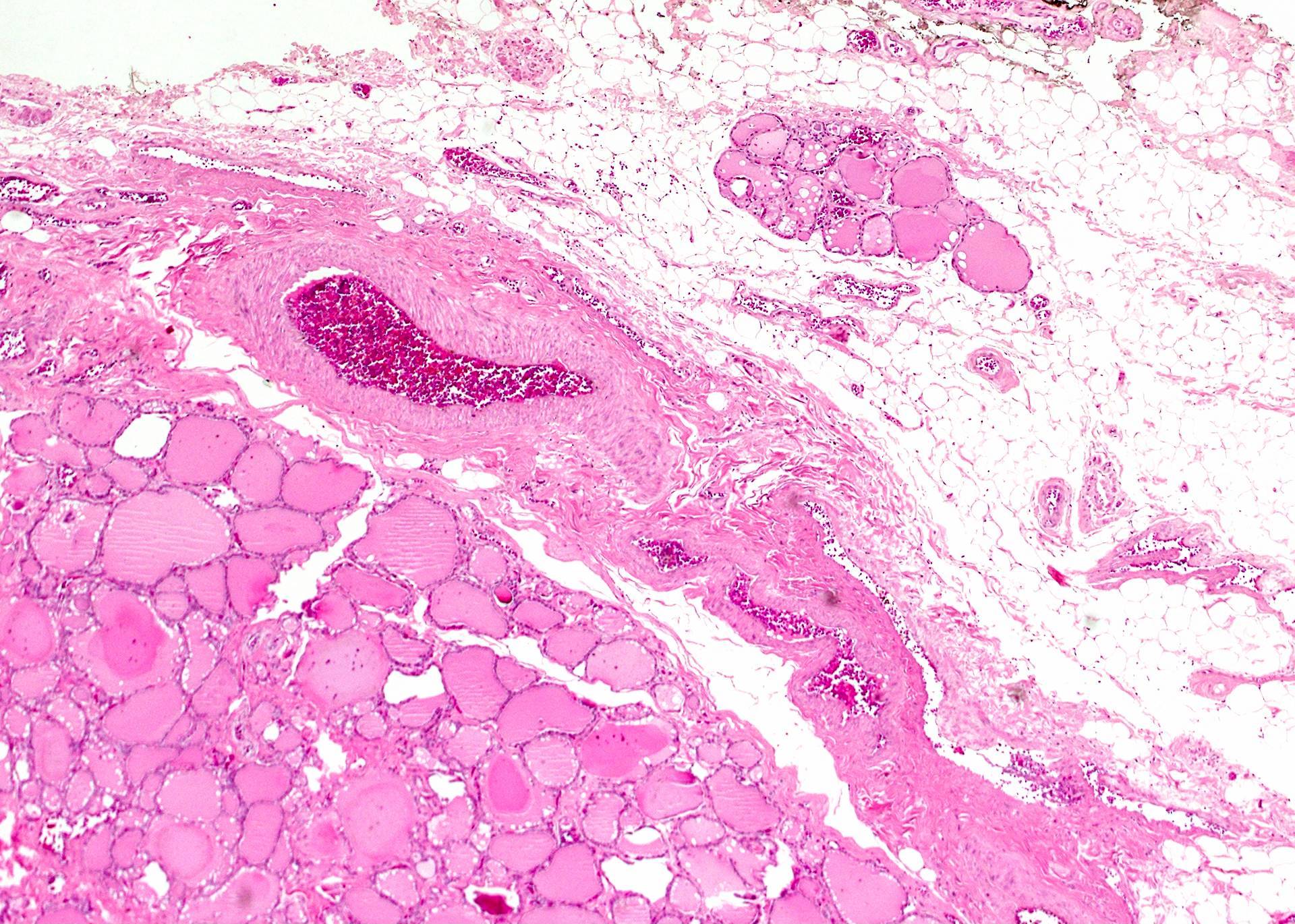
Microscopic (histologic) description
- The same histological appearance as the orthotopic thyroid tissue, composed of colloid filled follicles
- Signs of hyperplasia or thyroiditis in relevant clinical situations
- Ectopic thyroid tissue showing cytologic or histologic features of thyroid carcinoma should be considered as metastases until proven otherwise, although there are several reports of tumors arising de novo in ectopic thyroid (Thyroid 2007;17:603):
- Follicular adenoma (J Med Case Rep 2014;8:270)
- Follicular carcinoma (Am J Clin Pathol 1987;87:776)
- Classic variant of papillary thyroid carcinoma (BMJ Case Rep. 2012 Jul 9;2012)
- Follicular variant of papillary thyroid carcinoma (Ear Nose Throat J 2009;88:E7)
- Hurthle cell carcinoma (Acta Cytol 1983;27:188)
- Medullary thyroid carcinoma (Singapore Med J 2008;49:251)
- Poorly differentiated thyroid carcinoma (Endocr Pathol 2002;13:353)
- Anaplastic carcinoma (BMJ Case Rep 2010 Aug 31; 2010)
- Teratoma (Anal Quant Cytol Histol 2009;31:233)
- B cell lymphoma (Acta Chir Belg 2009;109:802)
Microscopic (histologic) images
Cytology description
- Microfollicular aggregates and colloid (IRCMJ 2009;11:100)
- Additional findings may reflect pathological conditions of thyroid tissue, e.g. abundant lymphocytes (thyroiditis) or atypical cells with nuclear grooves and inclusions (papillary carcinoma)
Positive stains
- Immunophenotype of thyroid tissue: thyroglobulin, TTF1 in follicular cells, and calcitonin in C cells (J Clin Endocrinol Metab 2012;97:951)
Molecular / cytogenetics description
- Absence of thyroid cancer related molecular alterations (BRAFV600E, N-RAS, H-RAS, K-RAS) in benign appearing ectopic thyroid tissue (Int J Surg Pathol 2015;23:170)
Differential diagnosis
- If any morphologic signs of malignancy are identified, then diagnosis is metastatic papillary thyroid carcinoma until proven otherwise
- Clues to malignancy: classic architectural and cytomorphologic features of papillary carcinoma, with fibrotic response (desmoplasia) of surrounding tissue
- Features against malignancy: separate blood supply of the ectopic gland from extracervical vessels, no personal history of malignancy, and normal or absent orthotopic thyroid with no history of surgery (Ann Thorac Cardiovasc Surg 2007;13:122)
- Metastasis from ectopic thyroid carcinoma may also be considered
- Benign mimickers of thyroid ectopia:
- Cystically dilated nonthyroid glands with flattened epithelium and inspissated secretions
- Parasitic nodule
- Mechanical implantation outside gland due to surgery or trauma: history of neck surgery
- Retrosternal goiter
- Teratoma with thyroid component
- Differential diagnosis in rare sites depends on the location
- Accidental finding of thyroid follicles in unusual site may pose a concern about specimen contamination by tissue from an unrelated case ("floater"), which can be resolved by genetic fingerprinting (Hum Pathol 2007;38:378)