Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Agarwal S. Hashimoto thyroiditis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidhashimotosthyroiditis.html. Accessed December 21st, 2024.
Definition / general
- Prototype of autoimmune disease presenting with goiter, elevated circulating antithyroid antibodies, often with hypothyroidism
- Histopathologically diffuse lymphoplasmacytic infiltration, lymphoid follicle formation, follicular atrophy, oncocytic metaplasia and fibrosis
- First described in 1912 by Dr. Hakaru Hashimoto, who called it struma lymphomatosa (Thyroid 2013;23:142)
Essential features
- Most common cause of hypothyroidism in iodine sufficient areas
- Infiltration of thyroid parenchyma by mononuclear cells, lymphoid follicles with germinal centers, oncocytic cells lining residual thyroid follicles, fibrosis
Terminology
- Also known as Hashimoto disease, struma lymphomatosa, chronic lymphocytic thyroiditis, goitrous thyroiditis, lymphadenoid goitre
- Hashitoxicosis: transient thyrotoxicosis due to follicle destruction in Hashimoto thyroiditis
ICD coding
- ICD-10: E06.3 - autoimmune thyroiditis
Epidemiology
- Incidence per year 0.3 - 1.5/1,000 (Best Pract Res Clin Endocrinol Metab 2019;33:101367)
- 30 - 50 years (Maedica (Bucur) 2019;14:98)
- F:M = 3 - 12:1 (Autoimmun Rev 2014;13:391)
- 3:1 for IgG4 related variant
- 5:1 for Hashitoxicosis form
- 6:1 for juvenile variant
- 10:1 for fibrous variant
- 12:1 for classic variant
- Polymorphisms associated with other autoimmune diseases in 20% of cases
Pathophysiology
- Breakdown of immune tolerance (Best Pract Res Clin Endocrinol Metab 2019;33:101367)
- Genetic susceptibility
- Familial aggregation
- Polymorphisms in human leukocyte antigen (HLA) genes
- Polymorphisms in genes involved in immune regulation, including cytotoxic T lymphocyte associated antigen 4 (CTLA4), protein tyrosine phosphatase 22 (PTPN22) and interlukin 2 receptor α chain (IL2RA)
- Environmental factors (Autoimmun Rev 2014;13:391)
- Smoking has a protective effect
- Increased dietary iodine is associated with increased incidence
- Polymorphisms
- Decrease in Tregs
- Genetic susceptibility
- Autoantibodies against thyroglobulin, thyroid peroxidase (TPO) and antithyroid stimulating hormone (TSH) receptor
- CD8+ T cell mediated cytotoxicity, cytokine mediated cell death and antibody dependent cell mediated cytotoxicity
Etiology
- Multifactorial; immunological, genetic and environmental
Clinical features
- Painless enlargement of thyroid gland
- Majority (75%) are euthyroid (Autoimmun Rev 2014;13:391)
- Progressively increasing hypothyroidism
- May have an initial transient phase of hyperthyroidism
- May coexist with other autoimmune diseases, like type 1 diabetes mellitus, Addison disease, systemic lupus erythematosus, Sjögren syndrome, pernicious anemia, myasthenia gravis, vitiligo, celiac disease, chronic active hepatitis
- Increased risk of primary thyroid lymphoma and papillary thyroid carcinoma (PTC) (Front Oncol 2017;7:53, Endocr Pathol 2021;32:368)
- 6 clinicopathologic forms: classic, fibrous variant, IgG4 related variant, juvenile form, Hashitoxicosis and painless (or silent) thyroiditis (Autoimmun Rev 2014;13:391)
- Idiopathic myxedema in older patients with fibrous variant
- Juvenile variant: < 18 years of age, (mean age of 11 years); usually asymptomatic thyroid swelling
- Hashitoxicosis variant: initial hyperthyroid phase similar to Graves disease, followed by hypothyroidism
- Painless thyroiditis: sporadic or (more commonly) postpartum (within 12 months of delivery); usually self limited
Diagnosis
- Diagnostic workup is similar to any thyroid swelling
- Thyroid function test
- Serum antithyroid antibody levels
- Ultrasound neck
- Fine needle aspiration cytology (FNAC) if thyroid nodule present
- References: J Endocrinol Invest 2021;44:883, Autoimmun Rev 2020;19:102649
Laboratory
- Deranged thyroid function tests
- Elevated levels of TSH, with normal or low serum thyroid hormones (T3,T4)
- Decreased TSH, with normal or increased serum T3,T4
- Elevated serum antithyroid antibodies
- Antithyroglobulin
- Anti-TPO
- Anti-TSH receptor
- References: J Endocrinol Invest 2021;44:883, Autoimmun Rev 2020;19:102649
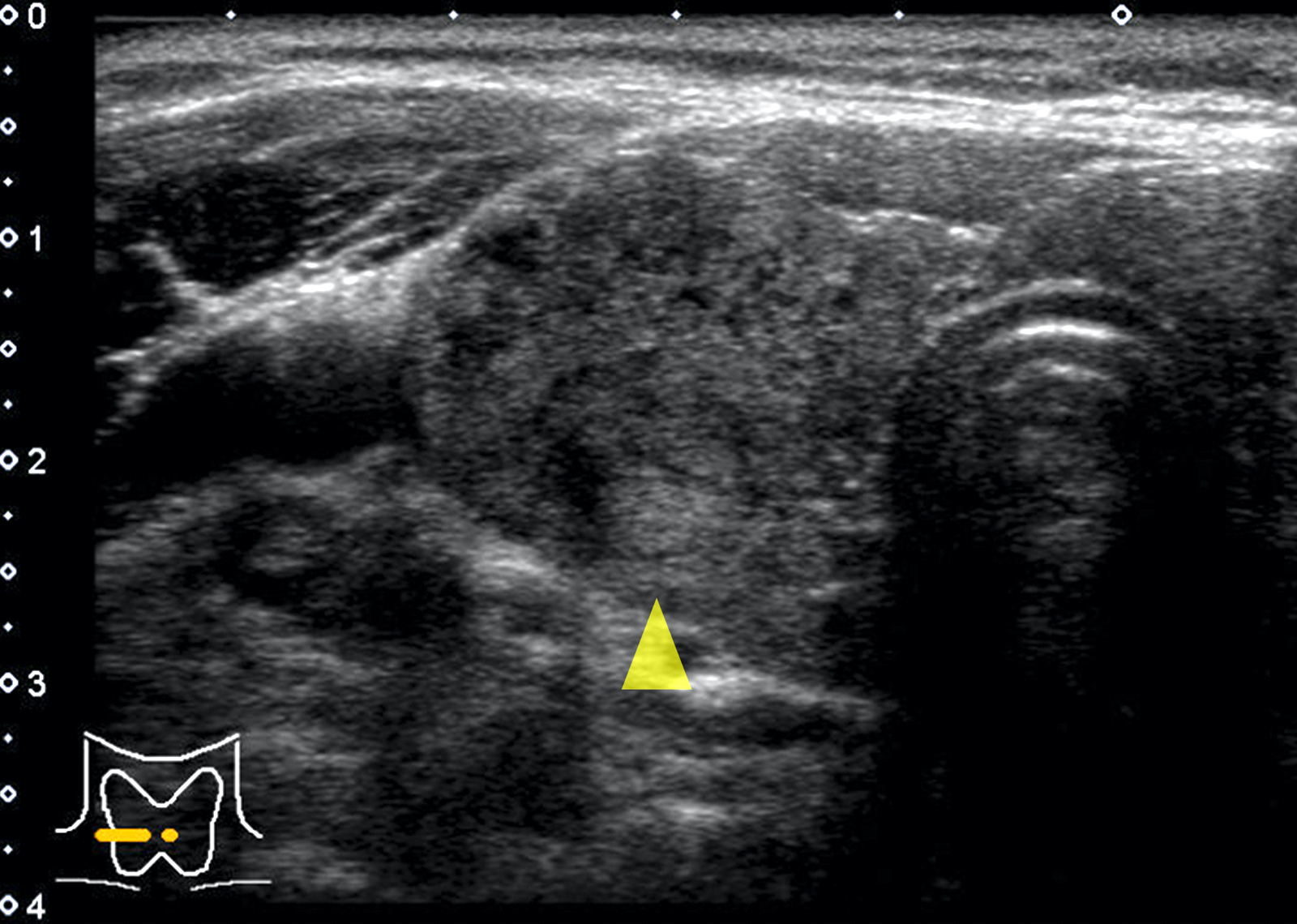
Radiology description
- Sonography: diffusely enlarged thyroid gland; diffusely heterogeneous, coarse and hypoechogenic parenchyma with micronodular pattern (Eur J Endocrinol 2019;181:539, AJR Am J Roentgenol 2010;195:208)
- IgG4 related variant: more marked hypoechogenicity (Autoimmun Rev 2014;13:391)
- Fibrous variant: hypoechogenicity along with prominent nodularity of the parenchyma
Radiology images
Prognostic factors
- IgG4 related variant shows a more aggressive clinical course, with more severe and treatment resistant hypothyroidism (Autoimmun Rev 2014;13:391)
Case reports
- 24 year old woman with Hashimoto thyroiditis associated with inflammatory myopathy (Pathology 2017;49:97)
- 28 year old woman with RET / PTC1 rearrangement in Hashimoto thyroiditis and in associated papillary thyroid carcinoma and hyalinizing trabecular adenoma (AJSP Reviews & Reports 2019;24:13)
- 31 year old man with Hashimoto thyroiditis presented with myxedema psychosis (J Am Osteopath Assoc 2017;117:50)
- 41 year old woman with hypothyroidism and multinodular goiter (Arch Pathol Lab Med 2003;127:e253)
- 43 year old woman with coexisting affective psychosis and brain perfusion abnormalities (Clin Pract Epidemiol Ment Health 2007;3:31)
- 46 year old woman with thyroid adenoma and Hashimoto thyroiditis (Rom J Morphol Embryol 2017;58:241)
- 52 year old woman with Hashimoto thyroiditis involving ectopic cervical thyroid tissue (Head Neck Pathol 2021;15:328)
Treatment
- Thyroid hormone replacement if hypothyroid
- Subtotal thyroidectomy to relieve compression symptoms (Best Pract Res Clin Endocrinol Metab 2019;33:101367)
- Hemitotal or subtotal thyroidectomy in case of oncocytic cell neoplasm or suspicious for malignancy cytology
- Short course glucocorticoids in IgG4 related variant (Autoimmun Rev 2014;13:391)
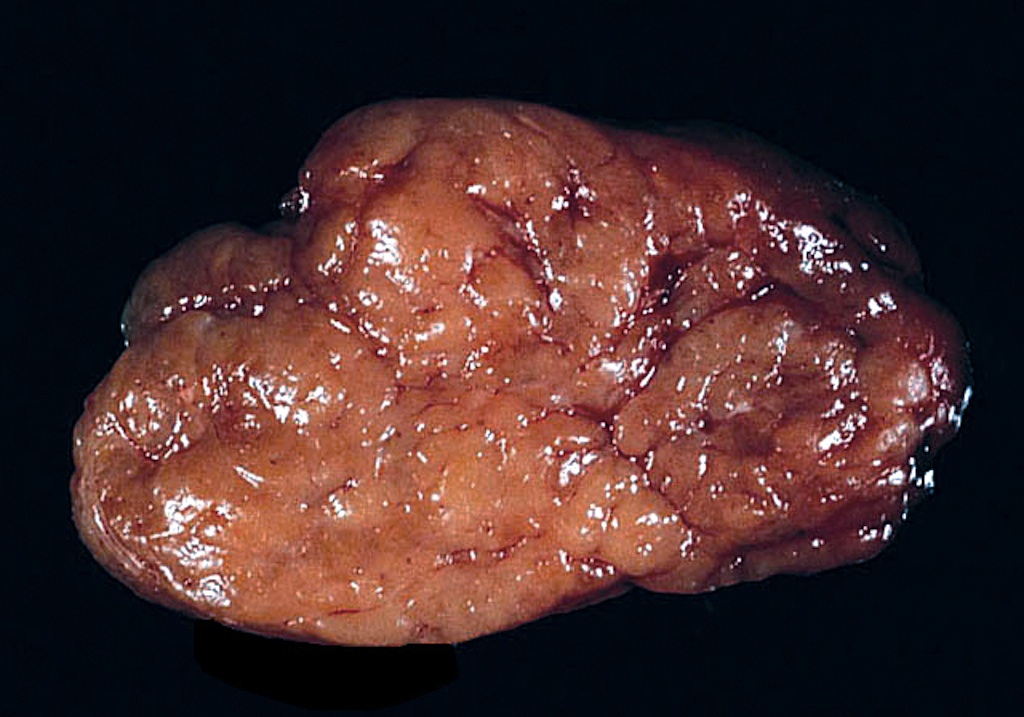
Gross description
- Diffuse symmetric enlargement of thyroid gland; occasionally asymmetric enlargement or nodular
- Cut surface: pale, yellow-tan, firm, nodular; resembles lymph nodes
- May be fibrotic and atrophied
Gross images
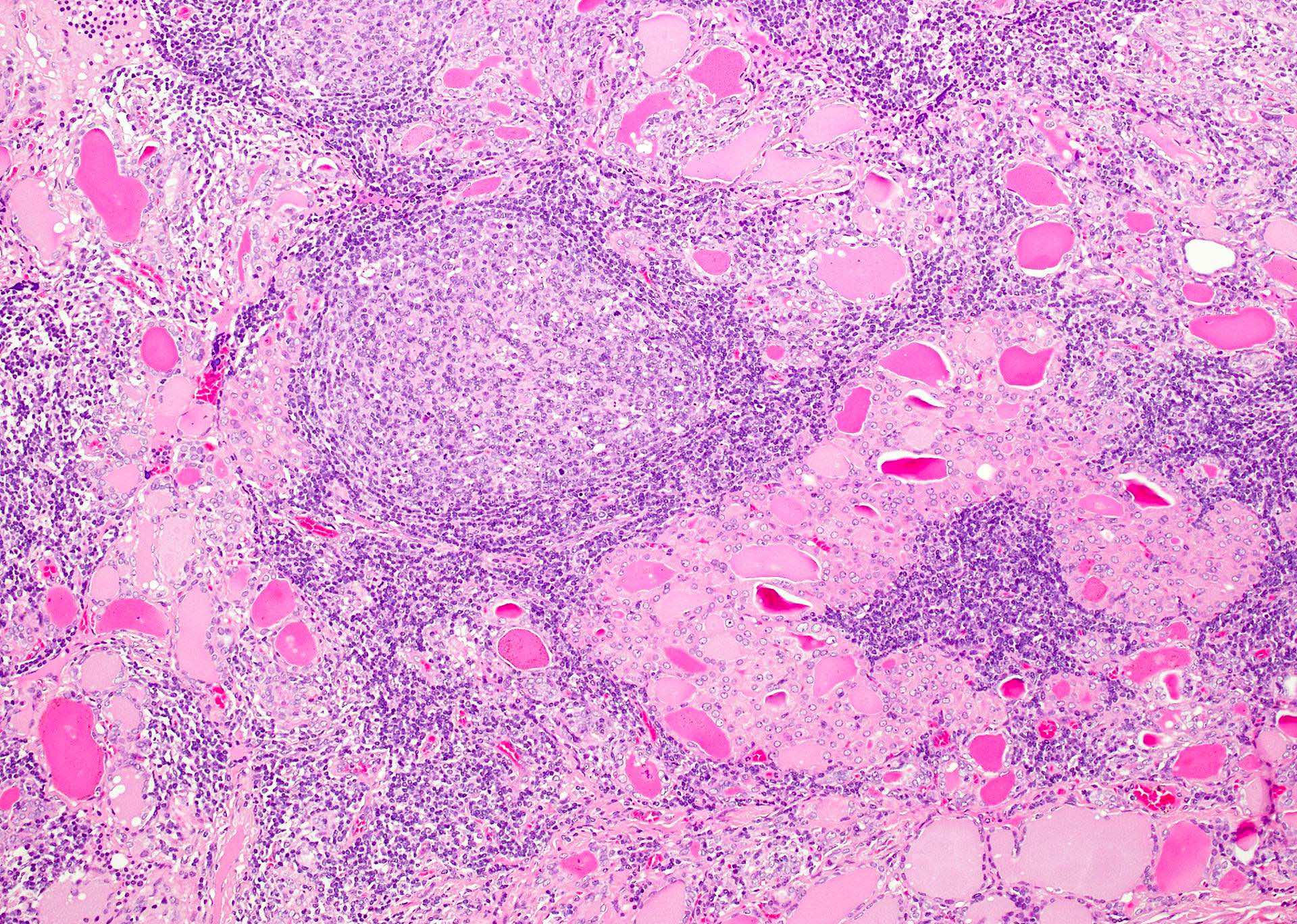
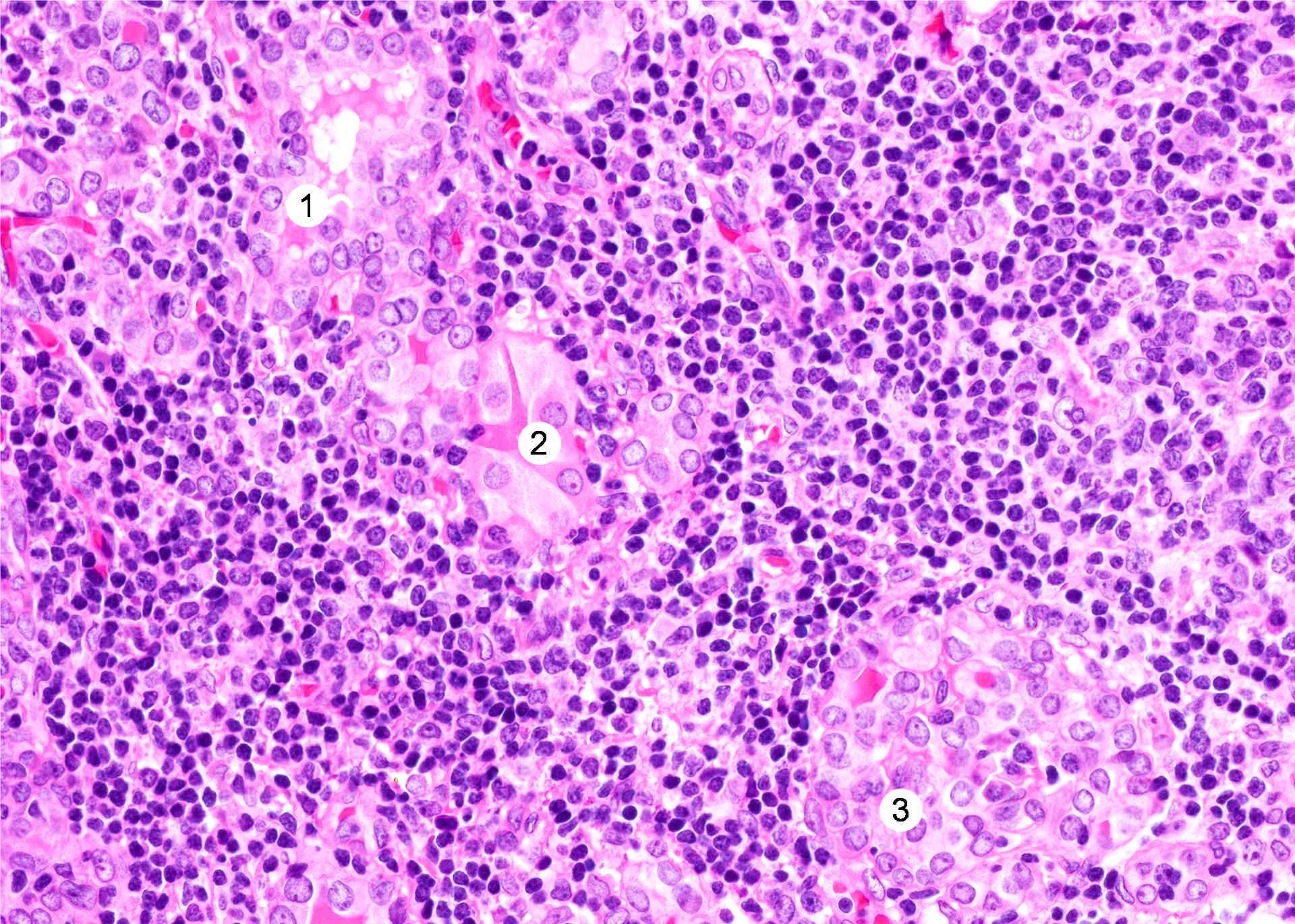
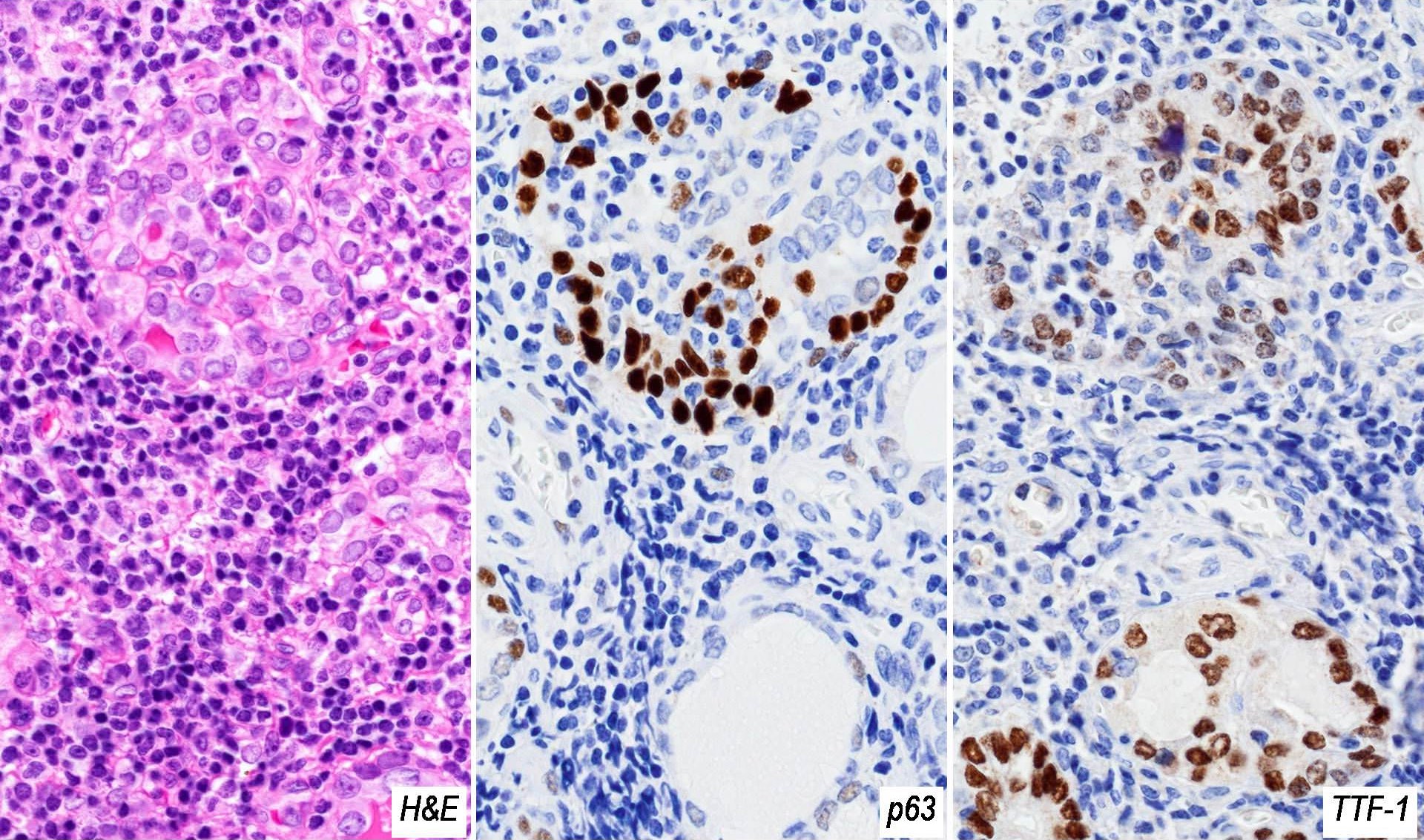
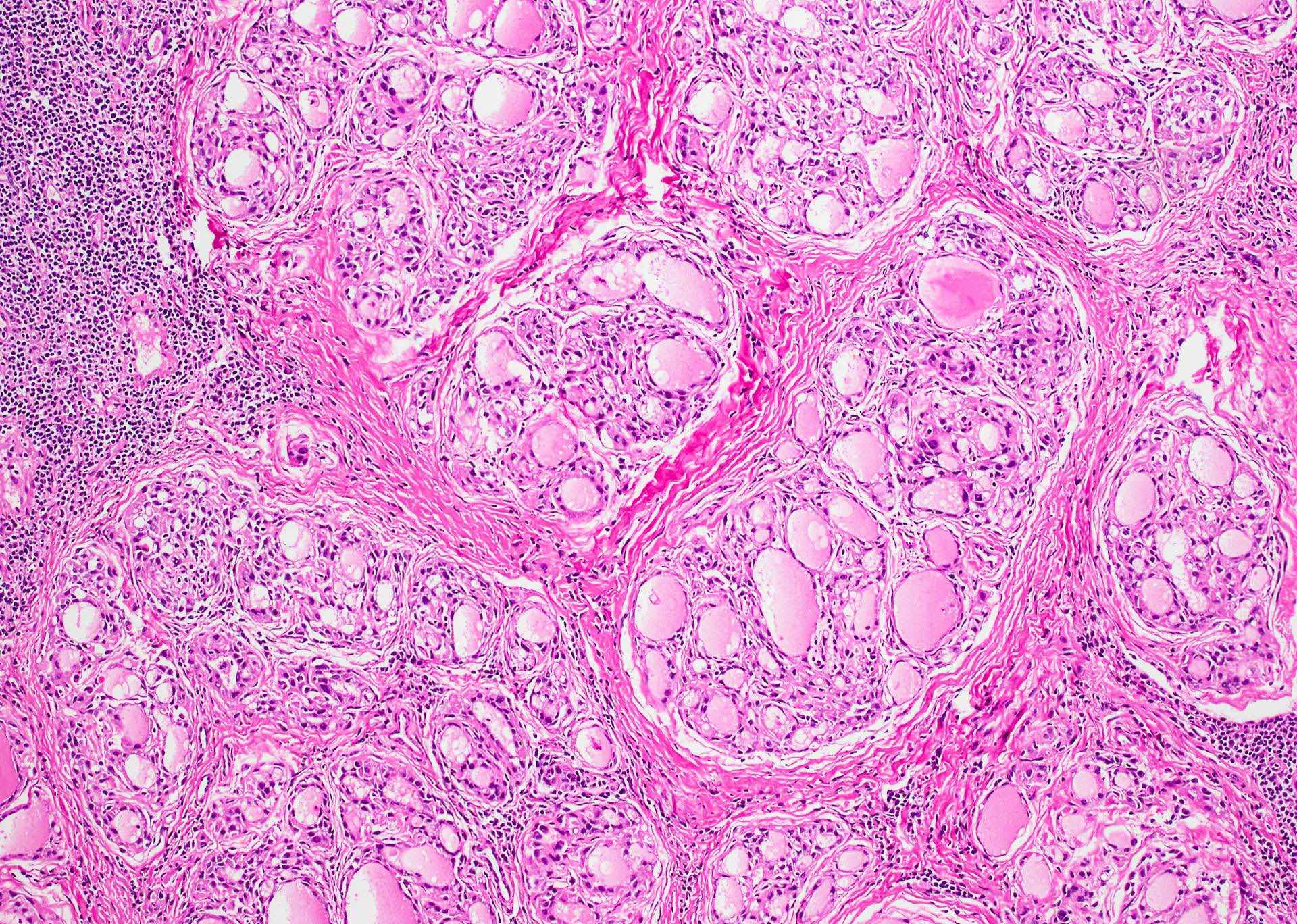
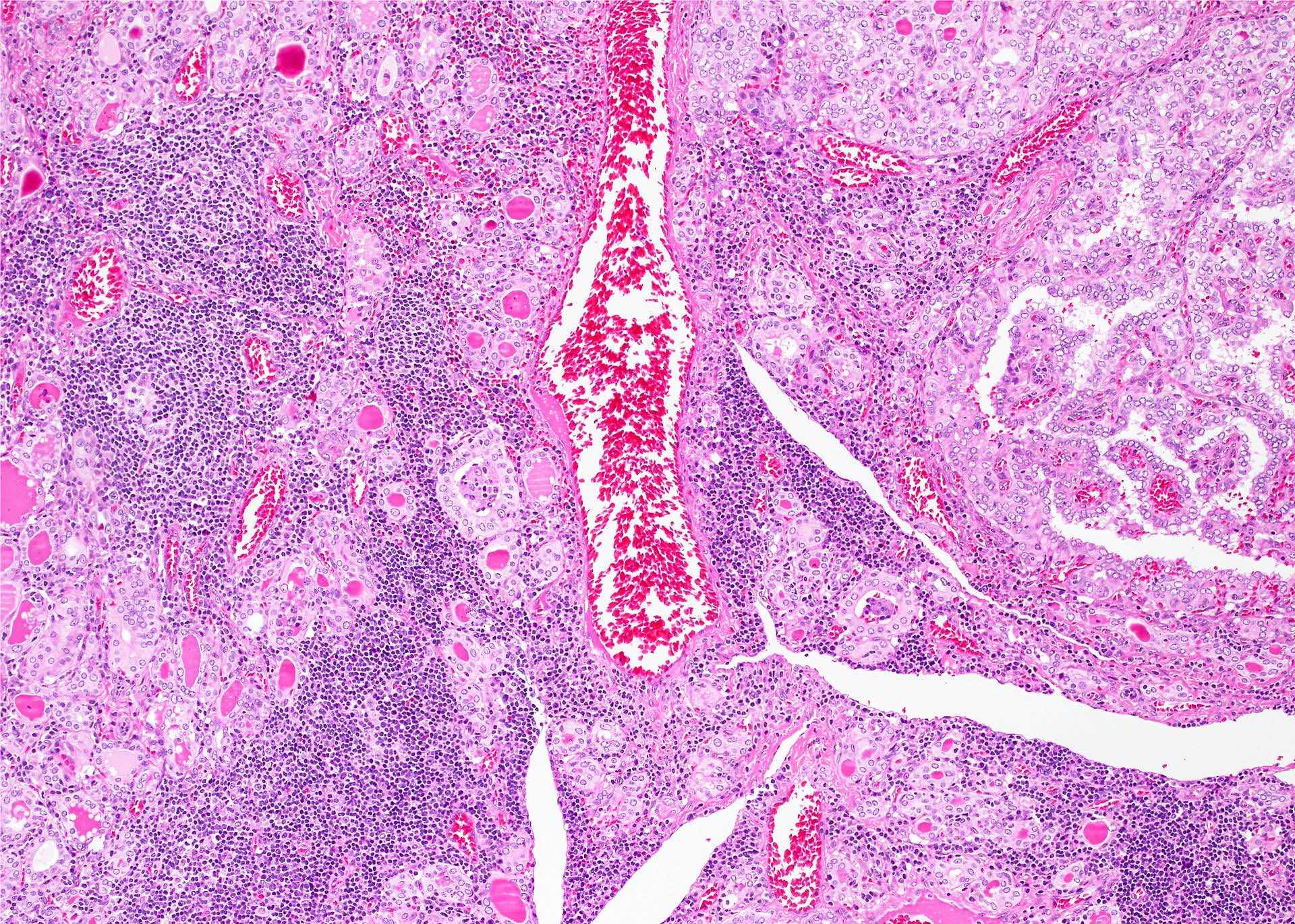
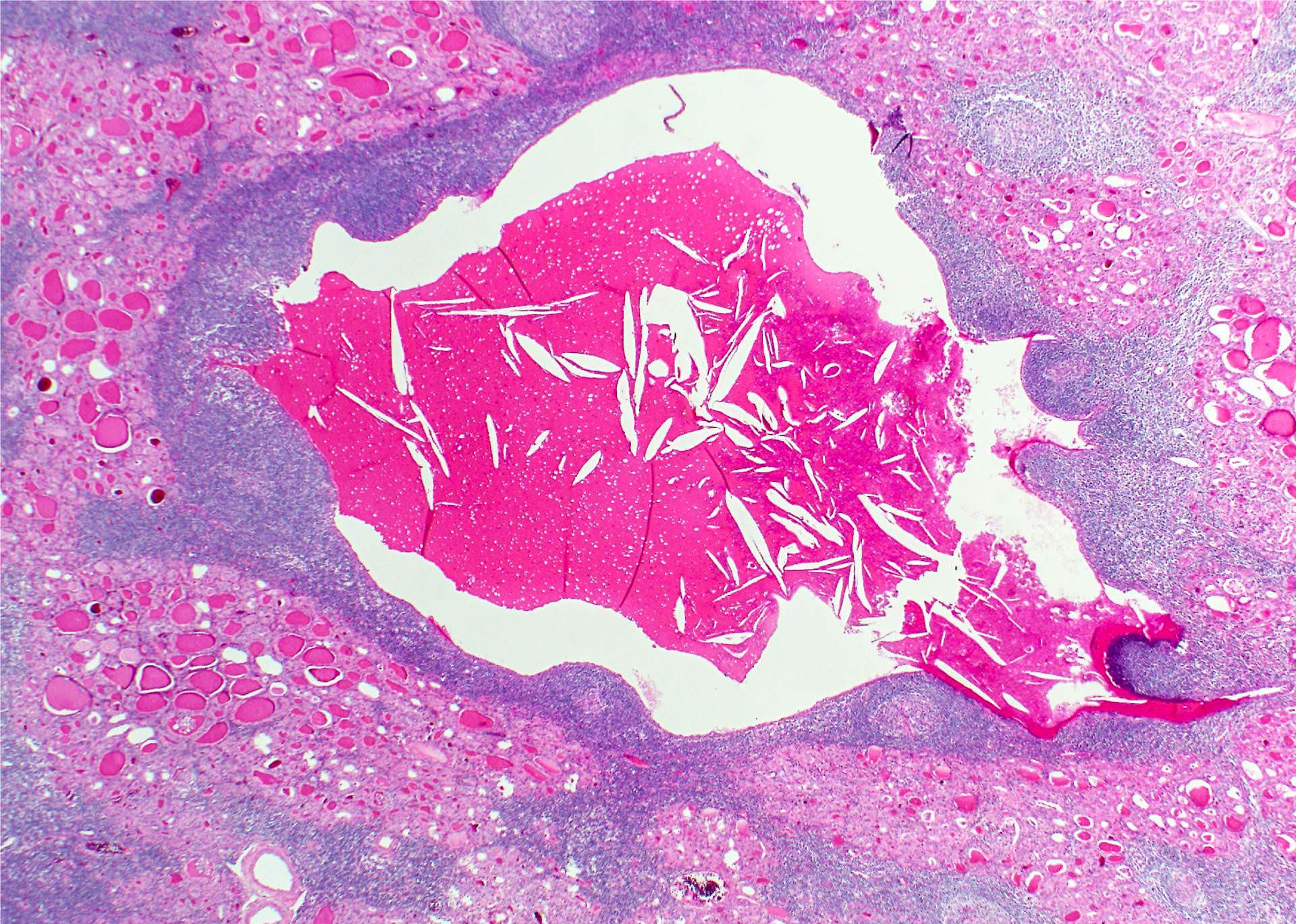
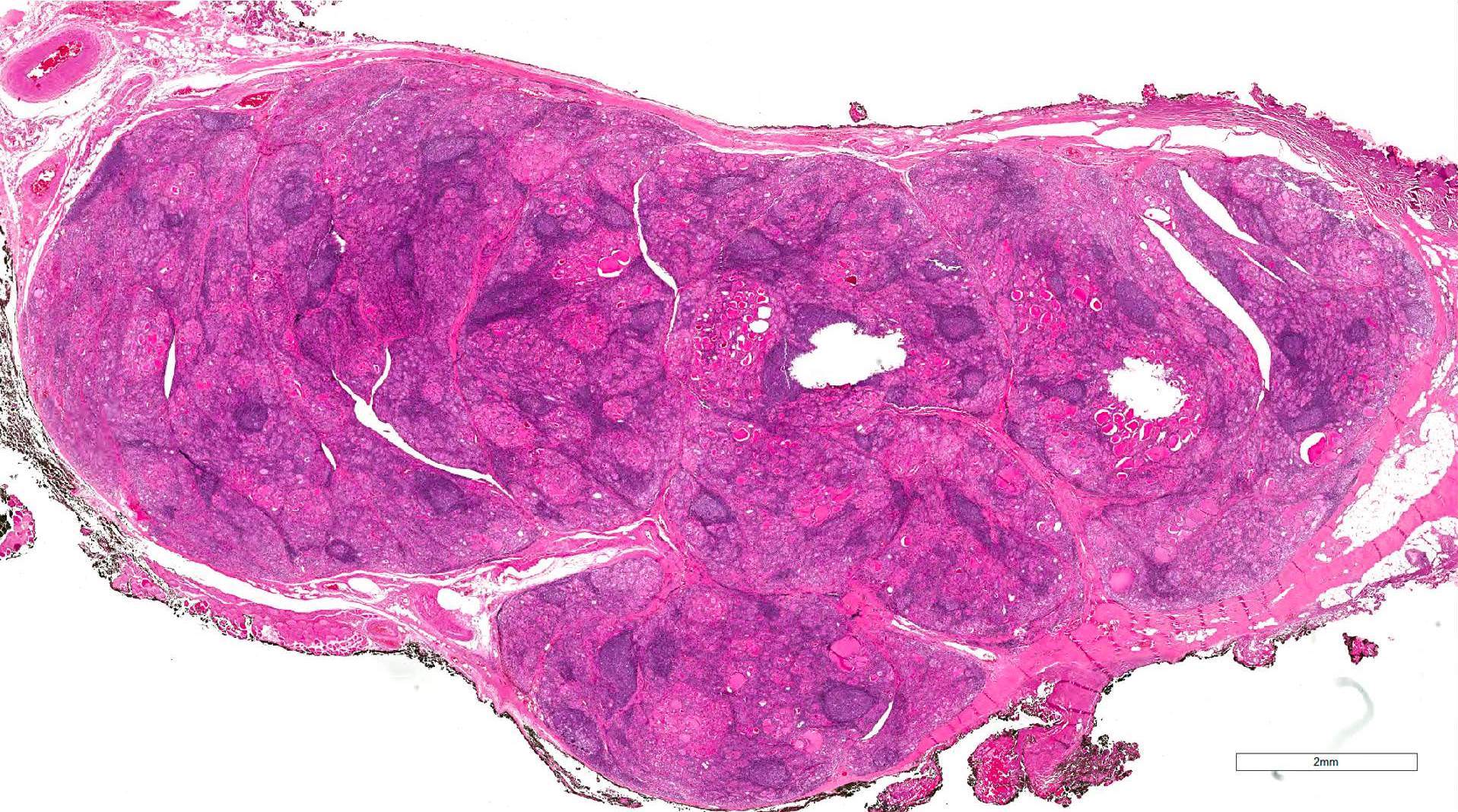
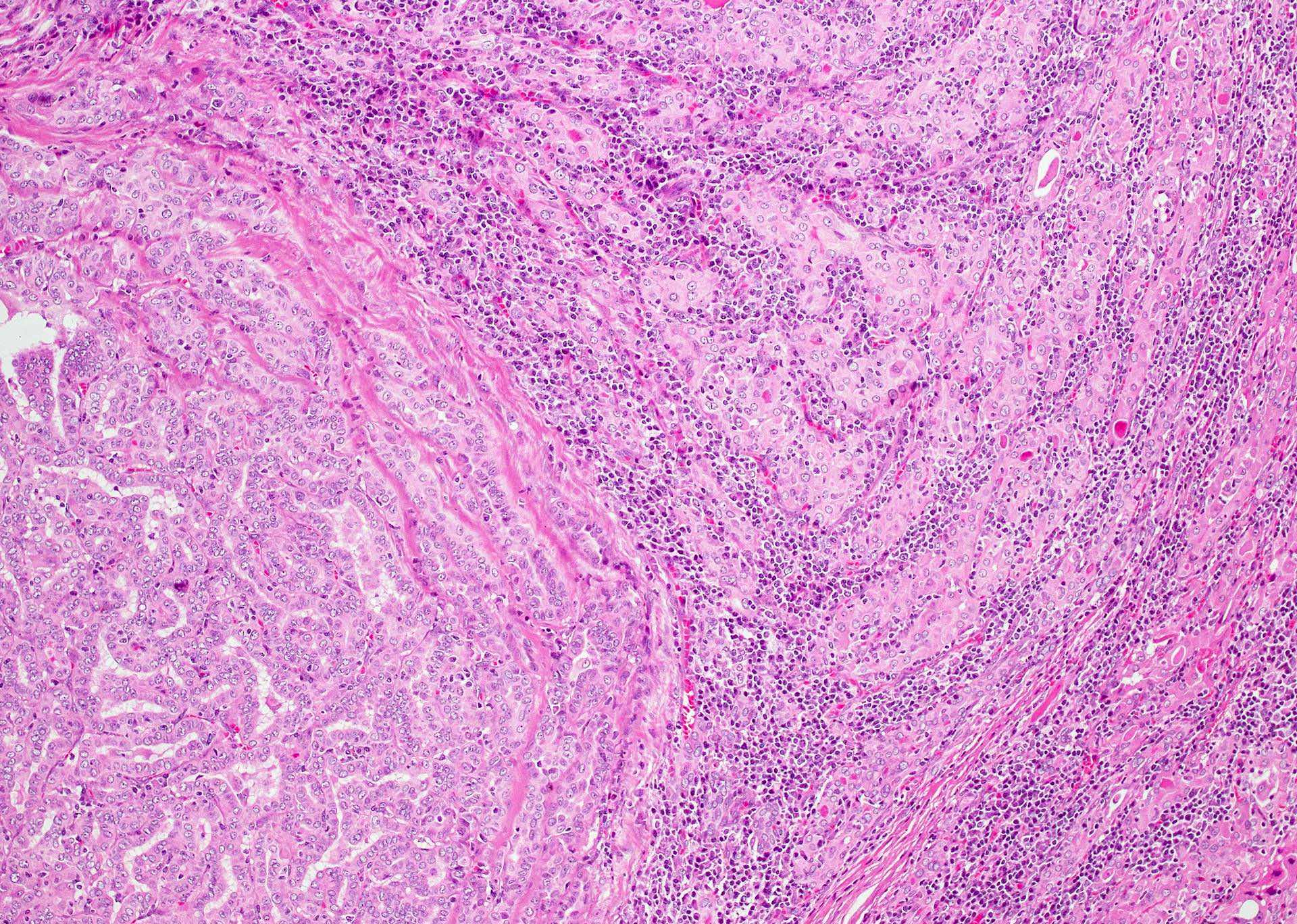
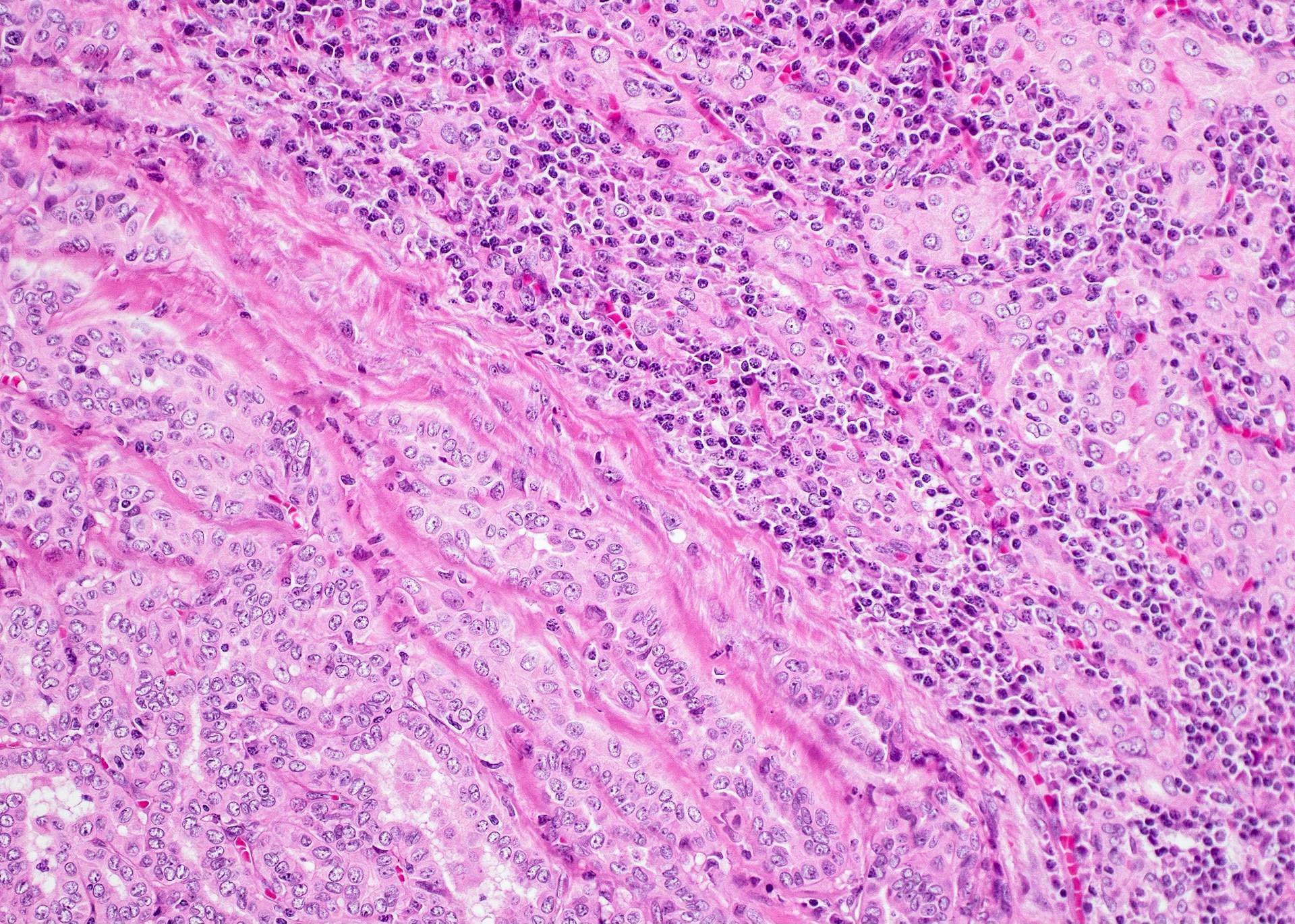
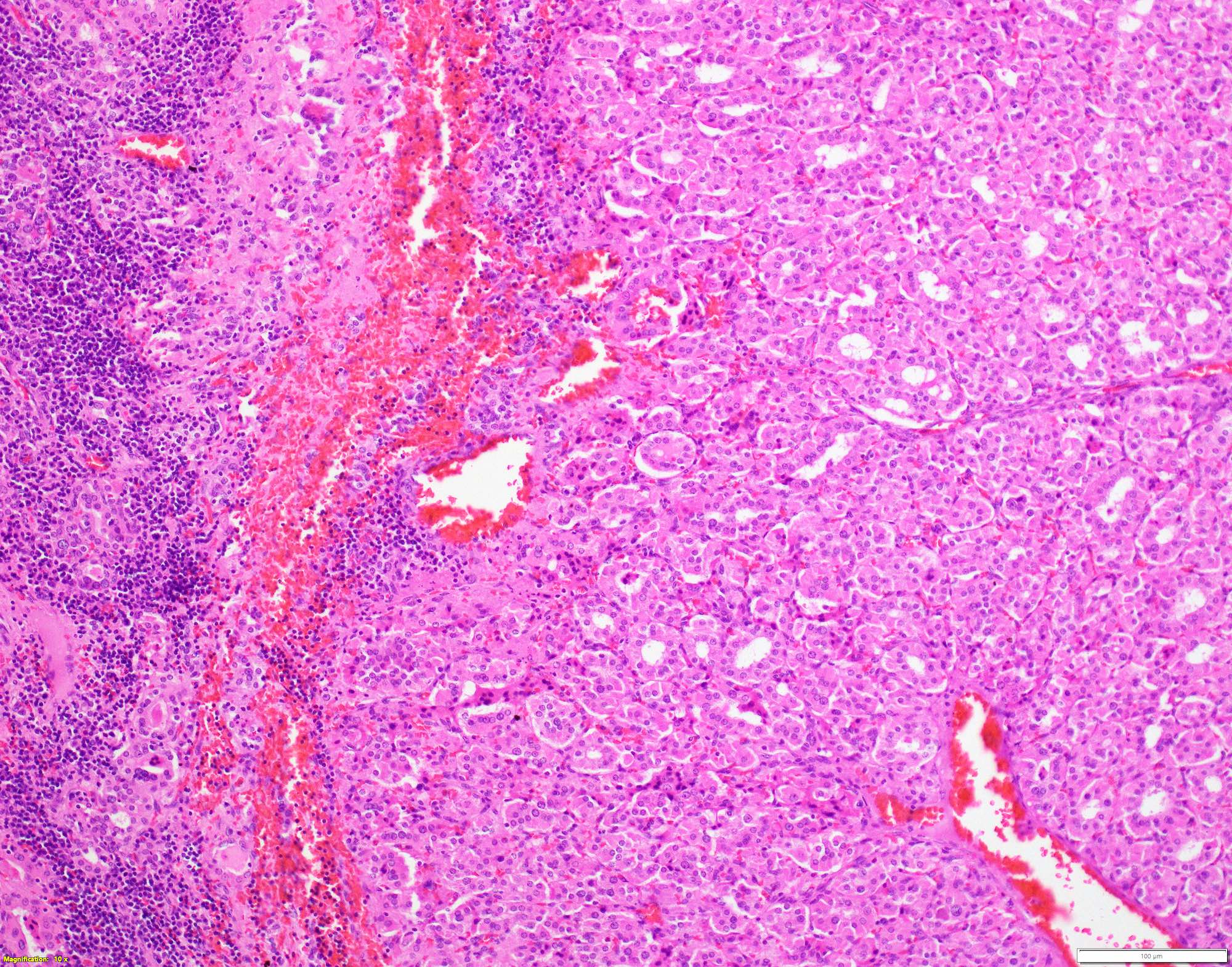
Microscopic (histologic) description
- Classic form: diffuse infiltration of thyroid parenchyma with lymphocytes and plasma cells; lymphoid follicle formation with germinal centers (Best Pract Res Clin Endocrinol Metab 2019;33:101367)
- Polymorphic lymphocytic infiltrate, predominantly T cells
- Thyroid follicular destruction
- Atrophic thyroid follicles; many lined by oncocytic cells / oncocytes having abundant granular eosinophilic cytoplasm; rarely squamous metaplasia
- Later fibrosis and nodularity (Virchows Arch 2013;462:557)
- Fibrous (or fibrosing) variant: extensive keloid-like fibrosis of thyroid parenchyma, fibrous septa divide the parenchyma into lobules, mononuclear cell infiltration, lymphoid follicles, thyroid follicular atrophy, oncocytic cell and squamous metaplasia (Autoimmun Rev 2014;13:391)
- IgG4 related variant: dense lymphoplasmacytic infiltrate, enriched in IgG4 producing plasma cells (> 20 cells per high power field); interstitial fibrosis; often associated with obliterative phlebitis (Autoimmun Rev 2014;13:391)
- Juvenile thyroiditis, Hashitoxicosis and painless thyroiditis: rare / absent germinal center formation and follicular atrophy, follicular cell hyperplasia, less pronounced oncocytic cell metaplasia and fibrosis (Autoimmun Rev 2014;13:391)
- Variable atypia of follicular cells and oncocytic cells, may mimic and act as a precursor (limited evidence) of papillary thyroid carcinoma (Endocr Pathol 2021;32:368)
- Squamous metaplasia of follicular epithelium can be confused with solid cell nests (J Clin Endocrinol Metab 2012;97:2209)
- May be associated with colloid goiter, follicular neoplasm, oncocytic cell neoplasm, papillary thyroid carcinoma and primary thyroid lymphoma (Acta Cytol 2009;53:507, Front Oncol 2017;7:53)
Microscopic (histologic) images
Contributed by Andrey Bychkov, M.D., Ph.D. and Shipra Agarwal, M.D.
Virtual slides
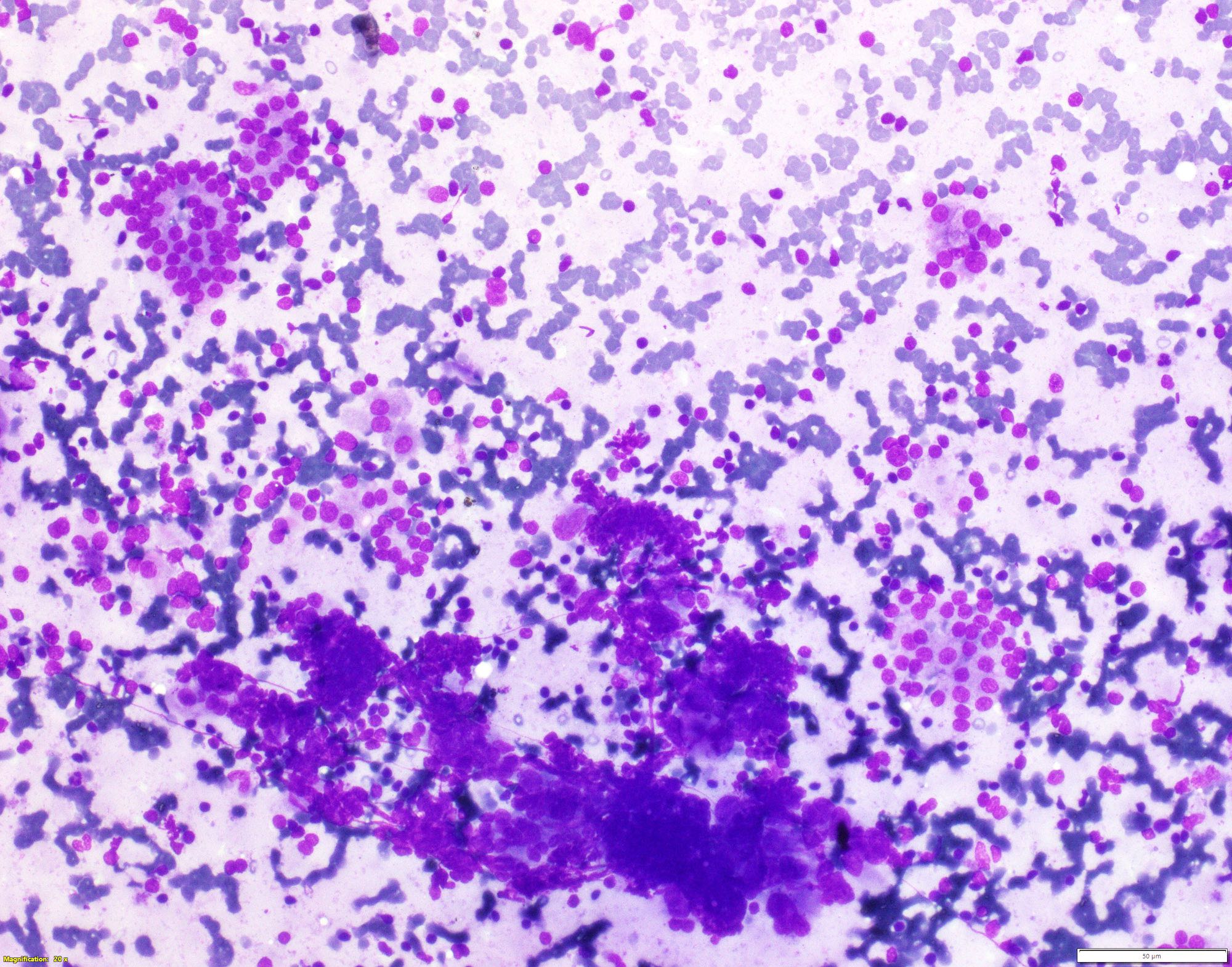
Cytology description
- Moderately or highly cellular aspirate
- Inflammatory infiltrate
- Variable number of lymphocytes in different stages of development (Cureus 2019;11:e5851, J Thyroid Res 2018;2018:5246516)
- Lymphocytes infiltrating follicular epithelial cells
- Lymphoglandular bodies (Acta Cytol 2009;53:507)
- Plasma cells
- Can grade based on lymphocytic infiltration from 0 to 3+ (see Diagrams / tables) but does not correlate with clinical, biochemical, radionuclide and ultrasonographic parameters (Cytojournal 2007;4:10, J Cytol 2016;33:145)
- Aggregates of oncocytic cells / oncocytes
- Crushed cells, lymphoid tangles
- Absent or scant colloid
- Mild anisonucleosis, giant cells, macrophages, epithelioid cells, eosinophils, fire flares
- Usually Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) category II; can be TBSRTC III / IV / V
Cytology images
Contributed by Shipra Agarwal, M.D. and Ayana Suzuki, C.T.
Images hosted on other servers:
Positive stains
- High molecular weight keratin, p63 (Hum Pathol 2003;34:764)
- May have elevated kappa/lambda ratio (Am J Clin Pathol 2006;125:42)
- Mixture of T and B cells (Indian J Pathol Microbiol 2011;54:464)
- HBME-1, cytokeratin 19, cyclin D1, galectin3: variable positivity in case of atypia (Virchows Arch 2013;462:557, Endocr Pathol 2021;32:368)
Electron microscopy description
- Oncocytic cells have numerous large mitochondria
Molecular / cytogenetics description
- Polyclonal (Hum Pathol 1988;19:1444, Indian J Pathol Microbiol 2011;54:464)
- No mutations, gene fusions (previously reported RET / PTC rearrangements were erroneous)
Videos
Thyroid: compare and contrast
Histopathology thyroid: Hashimoto thyroiditis
Sample pathology report
- Thyroid, total thyroidectomy:
- Hashimoto thyroiditis
Differential diagnosis
- Chronic (focal) lymphocytic thyroiditis:
- Incidental detection of focal aggregates of lymphocytes, with or without germinal center formation, in thyroid parenchyma
- Absent or limited oncocytic metaplasia
- Follicular atrophy and fibrosis
- Usually absent clinical and laboratory indicators of autoimmune thyroid disease
- Riedel thyroiditis:
- Hard fixed mass simulating thyroid carcinoma
- Active fibroblastic proliferation; storiform fibrosis
- Inflammation and fibrosis extends beyond the thyroid capsule into perithyroidal tissues
- Associated with fibroinflammatory lesions in other sites
- MALT lymphoma:
- Age: > 60 years
- Rapid increase in size of thyroid swelling, hard swelling
- Clonal proliferation of B cells, confirmed on immunostaining and flow cytometry
- Destructive lymphoepithelial lesions (Rom J Morphol Embryol 2017;58:731)
- Oncocytic cell neoplasms:
- Well circumscribed lesion within an echonormal background
- Composed mainly of oncocytic cells without (or with minimal) mononuclear cell infiltration (Rom J Morphol Embryol 2017;58:731)
- Papillary carcinoma:
- Presence of true papillae, more well developed and diffuse nuclear features, infiltrative borders
- Lithium intake:
- Significant clinical history; shows similar morphologic findings (Hum Pathol 1983;14:737)
Board review style question #1
Which of the following is true regarding the thyroid lesion shown above?
- Fibrosis extends into perithyroidal soft tissues
- Increased risk of follicular thyroid carcinoma
- Increased risk of medullary thyroid carcinoma
- Increased risk of primary thyroid lymphoma
- Shows monoclonal lymphoid cell proliferation
Board review style answer #1
D. Increased risk of primary thyroid lymphoma. Answer A is incorrect because unlike Riedel thyroiditis, in which the fibrosis extends into perithyroidal soft tissues, it is limited to the thyroid gland in Hashimoto thyroiditis. Answers B and C are incorrect because Hashimoto thyroiditis predisposes to papillary thyroid carcinoma and primary thyroid lymphoma. Answer E is incorrect because Hashimoto thyroiditis is characterized by a polyclonal lymphocytic infiltration of the thyroid parenchyma.
Comment Here
Reference: Hashimoto thyroiditis
Comment Here
Reference: Hashimoto thyroiditis
Board review style question #2
Which of the following is true about Hashimoto thyroiditis?
- Common in iodine deficient areas
- Mononuclear cell infiltration of the thyroid parenchyma
- More common in males
- Not a familial disease
- Usually presents with hyperthyroidism
Board review style answer #2
B. Mononuclear cell infiltration of the thyroid parenchyma. Histological examination in Hashimoto thyroiditis reveals a mononuclear cell infiltration of the thyroid parenchyma, composed of lymphocytes and plasma cells. Answer A is incorrect because Hashimoto thyroiditis is the most common cause of hypothyroidism in iodine sufficient areas. Answers C and D are incorrect because the disease shows a female preponderance and is often familial. Answer E is incorrect because the patients usually present with painless diffuse thyroid swelling and are mostly euthyroid.
Comment Here
Reference: Hashimoto thyroiditis
Comment Here
Reference: Hashimoto thyroiditis