Table of Contents
Definition / general | Essential features | Key features to report for Thyroid Cancer | Diagrams / tables | Microscopic (histologic) images | Videos | Sample of case summary | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Bychkov A. Features to report. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidfeatures.html. Accessed December 22nd, 2024.
Definition / general
- Protocols for histopathology reporting of thyroid cancer are issued by U.S. College of American Pathologists / CAP (CAP: Protocol for the Examination of Specimens From Patients With Carcinomas of the Thyroid Gland [Accessed 31 October 2018]), U.K. Royal College of Pathologists / RCPath (rcpath.org: Dataset for thyroid cancer histopathology reports [Accessed 31 October 2018]), The Royal College of Pathologists of Australasia / RCPA (CAP: Thyroid cancer structured reporting protocol 1st Edition 2011 [Accessed 31 October 2018]) and other expert societies
- CAP provides the most comprehensive and regularly updated protocol for the examination of specimens from patients with carcinomas of the thyroid gland
- Synoptic reporting considers a use of structured checklists to produce more complete and standardized medical reports
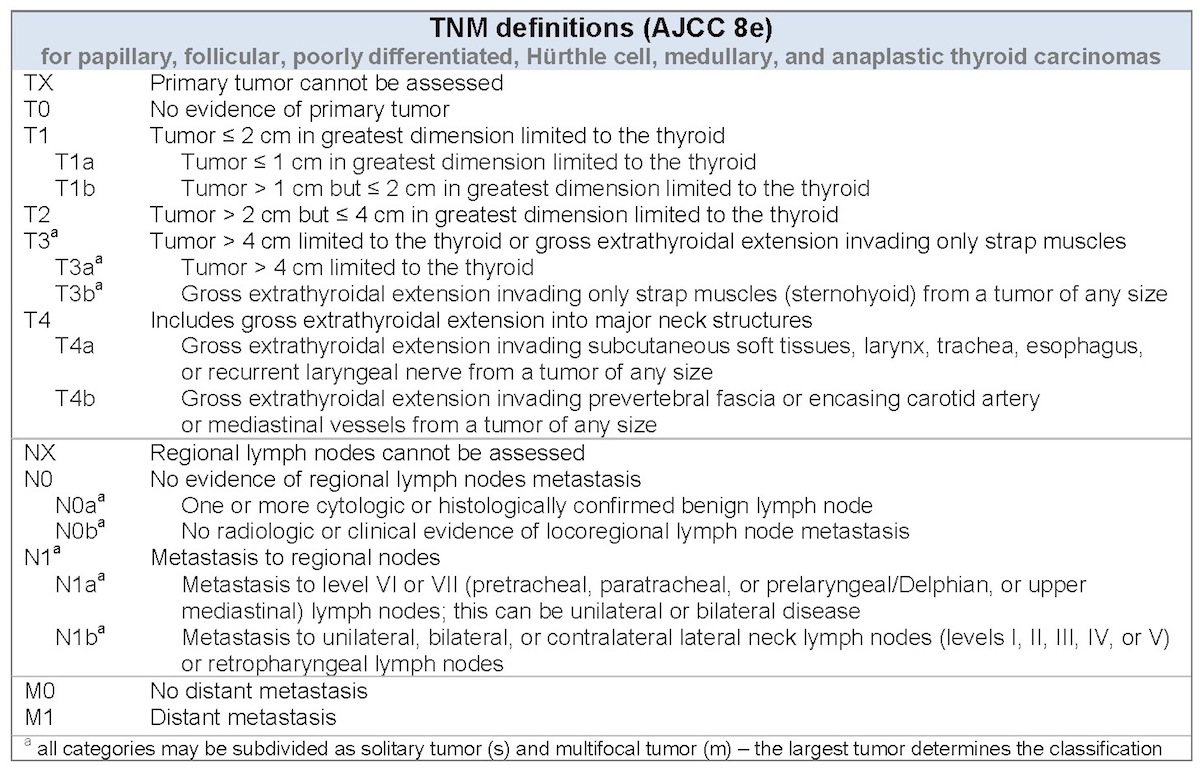
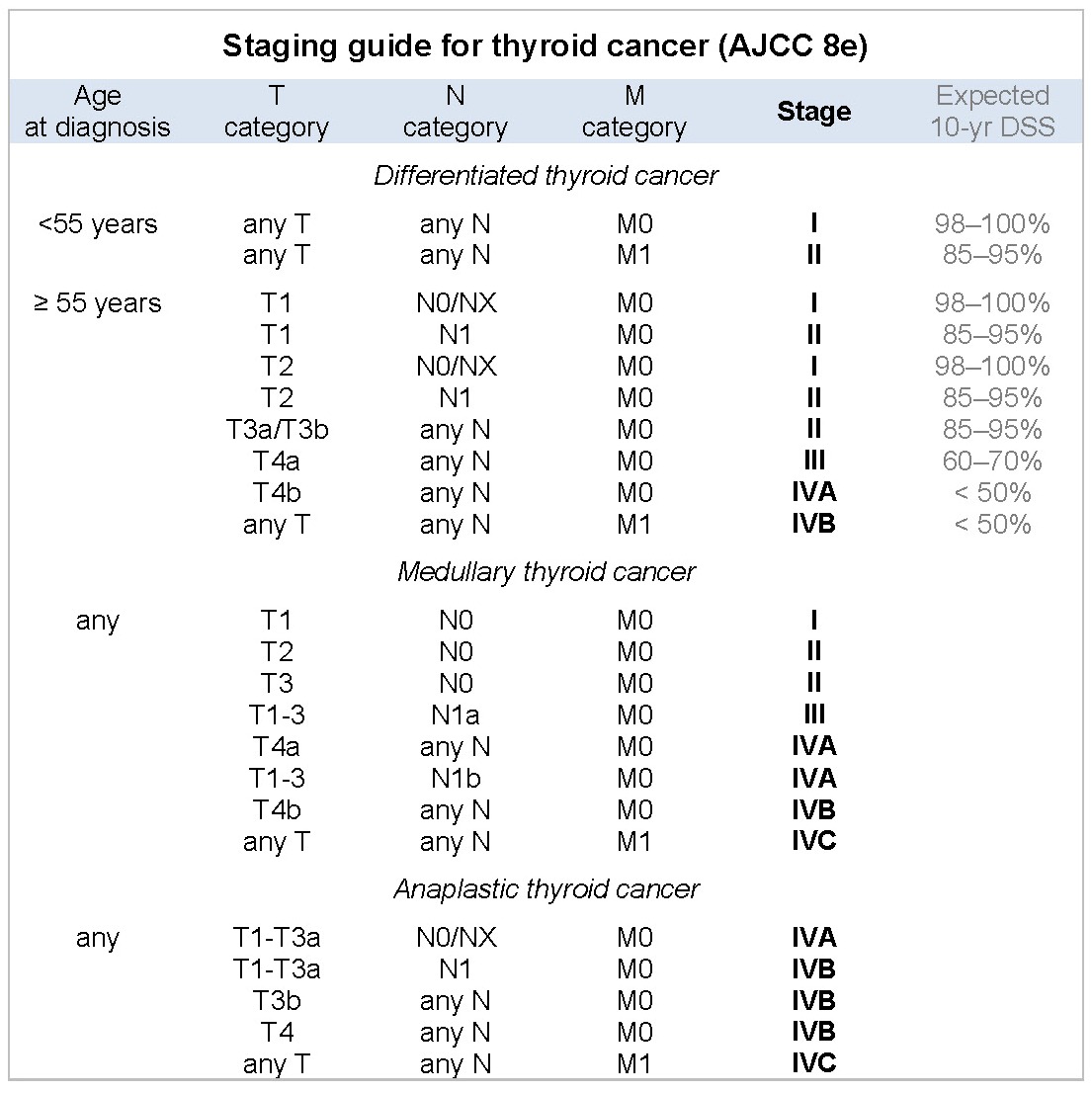
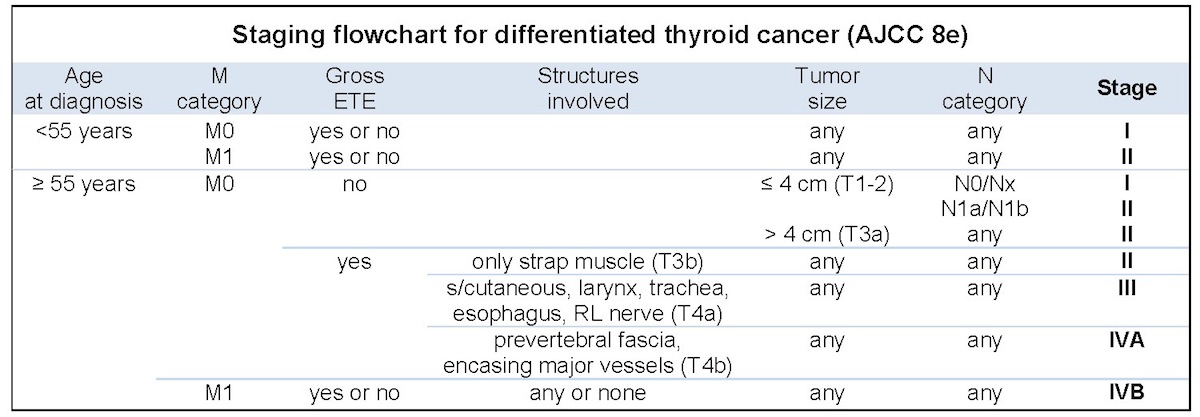
- Reporting protocol is aimed to supply clinicians with information required for cancer staging (AJCC / TNM), initial risk stratification (American Thyroid Association / ATA) and treatment decisions, e.g. necessity of additional surgery (completion thyroidectomy) and radioactive iodine / RAI ablation (see Diagrams / tables below)
Essential features
- Mandatory features to report (by CAP): procedure, tumor focality, tumor site, tumor size, histologic type, margins, angioinvasion, lymphatic invasion, extrathyroidal extension; number of lymph nodes examined and involved, size of the largest metastatic deposit, extranodal extension; pTNM
- Important for cancer staging (AJCC / TNM), initial risk stratification (ATA) and treatment decision
Key features to report for Thyroid Cancer
- Procedure
- Lobectomy
- Hemithyroidectomy: lobe with isthmus
- Subtotal thyroidectomy: small portion of uninvolved thyroid gland is left to preserve endocrine function
- Total thyroidectomy: entire gland, including posterior capsule, is removed
- Completion thyroidectomy
- Tumor focality
- Unifocal
- Multifocal
- CAP note:
- In multifocal cancers the protocol is applicable to the dominant excised tumor, which is defined as the most aggressive tumor - often but not necessarily the largest tumor
- If the second tumor is clinically relevant (e.g. medullary carcinoma in case of papillary carcinoma), a second report can be generated
- Comment:
- Multiple foci, whether minute or large, ipsi- or contralateral, can be either independent tumors or may result from intrathyroid spread of index tumor, which is difficult to distinguish (Endocr Pathol 2012;23:101)
- Tumor site (laterality)
- Right lobe
- Left lobe
- Isthmus
- Pyramidal lobe
- Tumor size
- Greatest dimension, in centimeters
- CAP note: additional dimensions are optional
- Comment:
- Papillary cancers ≤ 1 cm and > 4 cm are associated with excellent and worse prognosis, respectively
- Follicular cancer ≥ 3.5 cm has adverse prognosis
- Average tumor size in Western practice is 2.5 cm, number of subcentimeter cancers is growing (from 20 - 30% in the USA to 80% in Korea) (J Endocrinol Invest 2017;40:683)
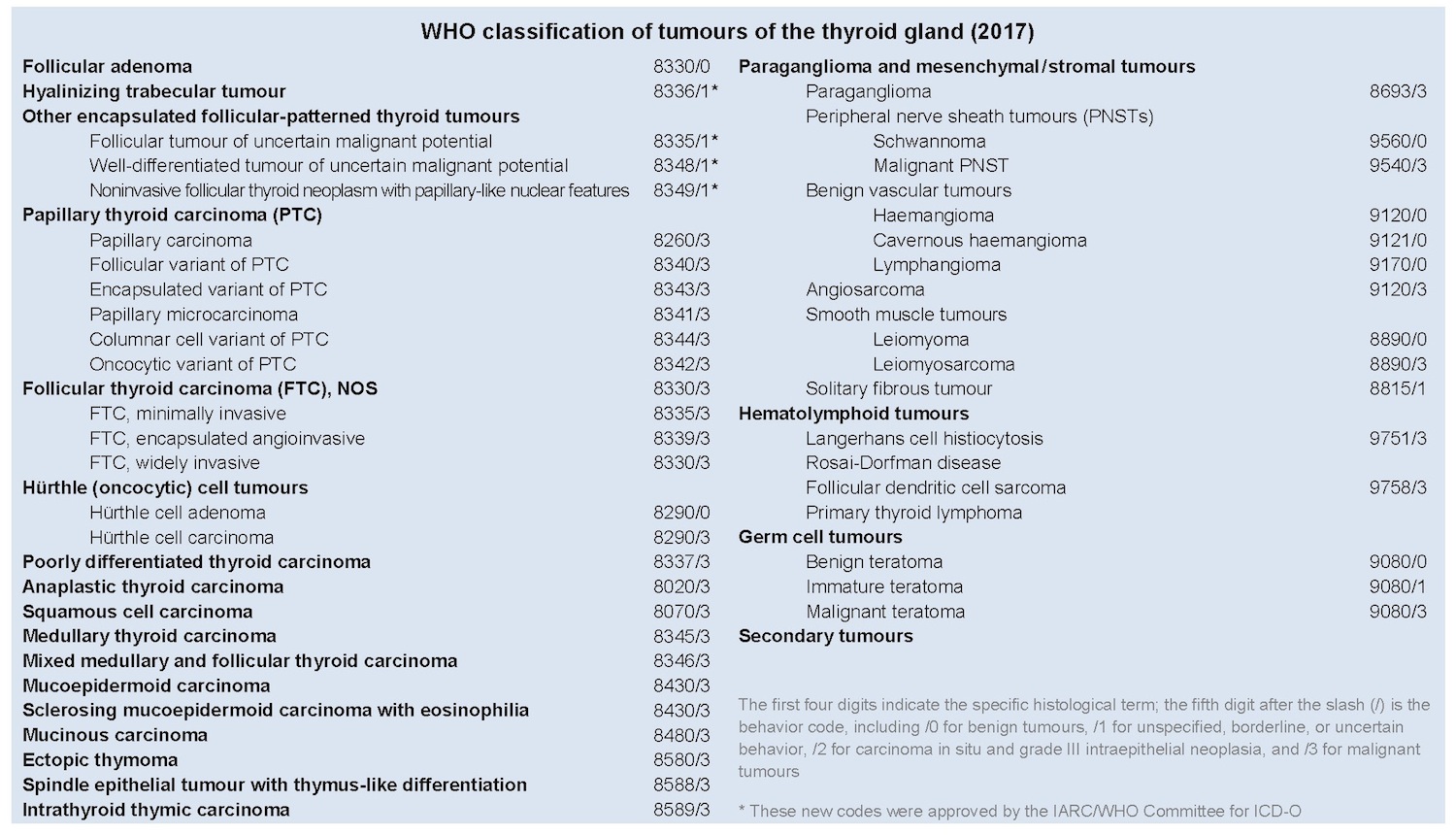
- Histologic type (see topic: Thyroid gland - WHO classification - Major Updates)
- Papillary carcinoma, specify variant
- Follicular carcinoma, specify type
- Poorly differentiated carcinoma
- Anaplastic carcinoma, including just focal component
- Medullary carcinoma
- Comment:
- Papillary microcarcinomas (≤ 1 cm), whether incidental / occult or nonincidental, are reported
- Hürthle cell (oncocytic) tumors have been reintroduced as a separate entity in the new WHO classification
- Poorly differentiated and anaplastic carcinomas are often seen with pre-existent well differentiated carcinoma
- Minor component with high grade (insular, anaplastic) and "aggressive" histology (tall cell, solid, hobnail) can be of significance and is worth reporting as an additional feature
- Papillary carcinoma is the most common type (up to 85 - 90% of all thyroid cancers) in daily practice, mainly represented by classic variant, follicular variant and microcarcinomas (Annu Rev Pathol 2017 Oct 30 [Epub ahead of print])
- Margins
- Positive
- Negative
- Cannot be assessed
- CAP note: site of invasion and distance, from the closest margin in millimeters, are optional
- Comment:
- According to Amin: AJCC Cancer Staging Manual, 8th ed, 2017, there is no difference in outcome between tumors with microscopically negative margins (R0) versus those with microscopically positive margins (R1); only grossly positive margins (R2) carry higher risks of recurrence and disease specific mortality (CA Cancer J Clin 2017 Nov 1 [Epub ahead of print])
- Reported frequency of microscopically positive margin is 6 - 14% (Histopathology 2018;72:32)
- Microscopic positive posterior but not anterior margin is a predictor for recurrence (J Surg Oncol 2016;113:635)
- Angioinvasion (vascular invasion)
- Present
- Absent
- Cannot be determined
- CAP note: extent of invasion can be optionally reported as focal (< 4 vessels) or extensive (≥ 4 foci)
- Comment:
- Only extensive vascular invasion predicts adverse outcome (recurrence, distant metastasis and cancer related death) (Histopathology 2018;72:32)
- Angioinvasion is mainly seen in encapsulated (follicular carcinoma, follicular variant of papillary carcinoma) or ex-encapsulated (poorly differentiated carcinoma) thyroid cancers
- In nonencapsulated cancers, e.g. papillary carcinomas, it sometimes can be seen in the extraglandular component of the tumor associated with extrathyroidal extension
- Vascular invasion is applicable to vessels of the tumor capsule or vessels beyond tumor interface
- Areas of angioinvasion that are closely adjacent to one another are counted as separate foci (Hum Pathol 2015;46:1789)
- Clinical significance - association with distant metastasis (bones / spine, lungs)
- Extensive angioinvasion is a rare event, found in less than 10% of encapsulated well differentiated cancers (Hum Pathol 2015;46:1789)
- Lymphatic invasion
- Present
- Absent
- Cannot be determined
- Comment:
- Extremely common in papillary cancers, can be identified by peritumoral foci / seeds, psammoma bodies or (indirectly) by presence of nodal metastasis
- Clinical significance - association with lymph node metastasis and multifocality
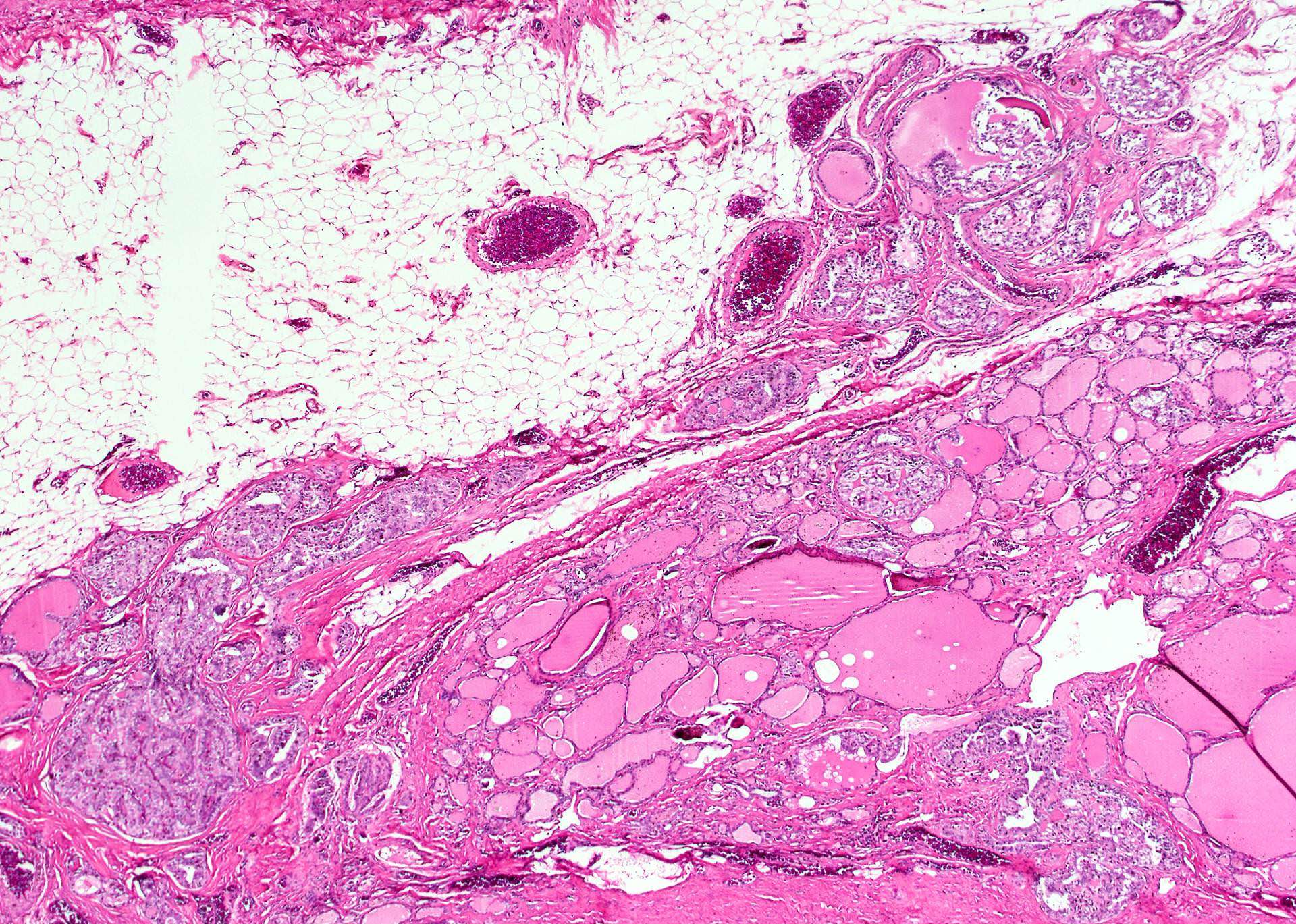
- Extrathyroidal extension (ETE)
- Present
- Absent
- Cannot be determined
- Comment:
- If present, specify extent as gross ETE (usually involving larynx / trachea, large vessels / nerves) or only microscopic / minimal ETE (perithyroid fat, strap muscles)
- Gross ETE is identified by clinician on imaging and during surgery or by pathologist on grossing
- Minimal ETE requires a tumor to extend beyond the contour of the gland with a desmoplastic response, invasion of strap muscles (reliable ETE) or at least perithyroidal fat (Thyroid 2016;26:512)
- Clinical significance - association with recurrence
- According to Amin: AJCC Cancer Staging Manual, 8th ed, 2017, minor extrathyroidal extension identified only on histologic examination is no longer a variable in determining the T category - only gross extrathyroidal extension (invasion of strap muscle, at least) has prognostic significance (CA Cancer J Clin 2017 Nov 1 [Epub ahead of print])
- ETE is detected in 1/4 of thyroid cancers (Thyroid 2017;27:1490)
- Additional histologic features of the tumor are optional
- Mitotic rate in 10 consecutive HPFs at 400x in the hot spots
- Comment: check carefully in the solid and trabecular patterned areas
- Perineural invasion
- Comment: search in tumors with extensive ETE
- Grading system is not established for thyroid cancer
- Mitotic rate in 10 consecutive HPFs at 400x in the hot spots
- Additional pathologic findings in nonneoplastic part are optional
- Nodular lesions: follicular adenoma, hyperplastic nodule(s)
- Diffuse disease: thyroiditis, Graves
- Presence of parathyroid gland
- Results of ancillary studies are optional
- Immunohistochemistry:
- Tumor type specific markers, e.g. calcitonin for medullary carcinoma or beta catenin for cribriform morular papillary carcinoma
- Markers to differentiate benign vs. malignant follicular-derived tumors (CK19, Galectin-3, HBME1)
- Markers of high grade progression (Tg loss, Ki67 >10%, p53)
- Mutation specific antibodies: VE1, SP174
- Molecular testing: not common on surgical samples
- Immunohistochemistry:
-
Key features to report for lymph nodes
- Number of lymph nodes examined and involved
- Nodal levels should be specified, e.g. levels VI-VII (central compartment) or II-V (lateral)
- Number of nodes depends on type of neck dissection (selective, modified radical or radical)
- CAP note:
- Adverse prognostic influence of lymph node metastasis in patients with differentiated carcinomas is observed only in the older age group
- Less prognostic significance in papillary than in medullary cancer
- Comment:
- Extremely common in papillary cancers (up to 50 - 80%, depending on the extent of neck dissection and sampling)
- According to Amin: AJCC Cancer Staging Manual, 8th ed, 2017, identification of a psammoma body in a cervical lymph node, even in the absence of associated malignant cells, meets the definition of pathologic N1 disease (CA Cancer J Clin 2017 Nov 1 [Epub ahead of print])
- To rule out occult nodal disease with 90% confidence, 6, 9 and 18 nodes would need to be examined for patients with T1b, T2 and T3 disease, respectively (J Clin Oncol 2016;34:3434)
- Size of the largest metastatic deposit, in centimeters
- Comment: micrometastases (< 2 mm and less than 5 involved nodes) likely do not increase risk of locoregional recurrence
- Extranodal extension
- Comment:
- Involvement of perinodal adipose tissue is the most consistent diagnostic criteria (Thyroid 2016;26:816)
- Reported in up to 12% of papillary thyroid carcinoma / PTC overall and 33% of nodal metastatic PTC
- Comment:
-
Pathologic stage classification (pTNM), see
(Thyroid gland - AJCC / TNM staging)
- The protocol described in this topic is not applicable to these thyroid tumors:
- Noninvasive follicular thyroid neoplasm with papillary like nuclear features (NIFTP): reporting of NIFTP is optional and only size, laterality and margin status are reported
- Thyroid carcinoma arising from struma ovarii
- Thyroid carcinoma arising in thyroglossal duct cysts
- Lymphoma: consider the Hodgkin (CAP Cancer Protocal Templates: Protocol for the Examination of Specimens From Patients With Hodgkin Lymphoma* [Accessed 31 October 2018]) or non-Hodgkin lymphoma protocols (CAP Cancer Protocal Templates: Protocol for the Examination of Specimens From Patients With Non-Hodgkin Lymphoma/Lymphoid Neoplasms [Accessed 31 October 2018])
- Sarcoma: consider the soft tissue protocol (CAP Cancer Protocal Templates: Protocol for the Examination of Specimens From Patients With Soft Tissue Tumors [Accessed 31 October 2018])
Diagrams / tables
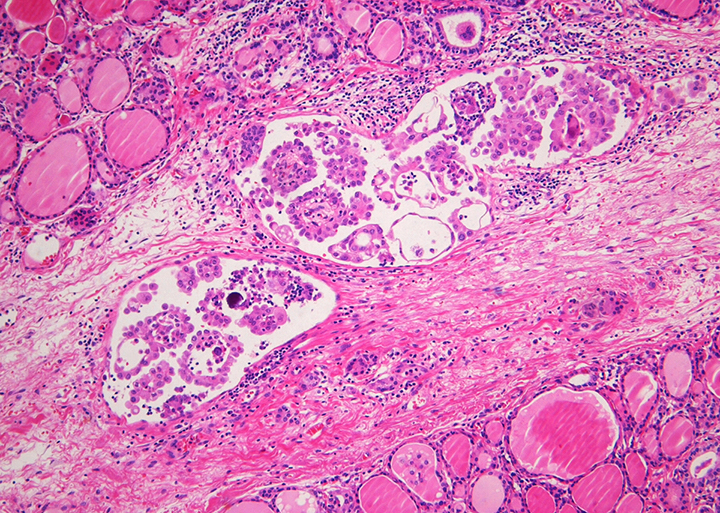
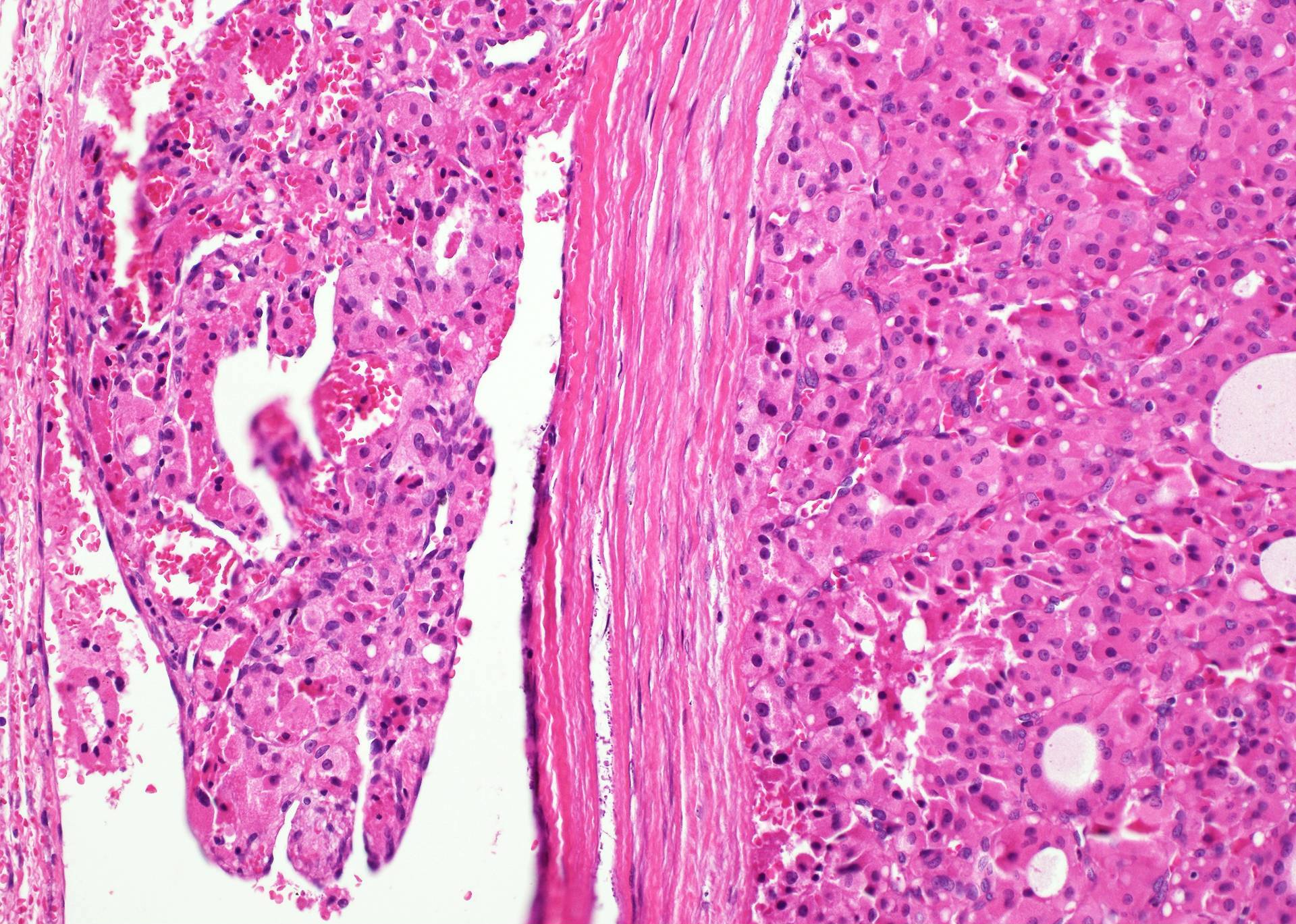
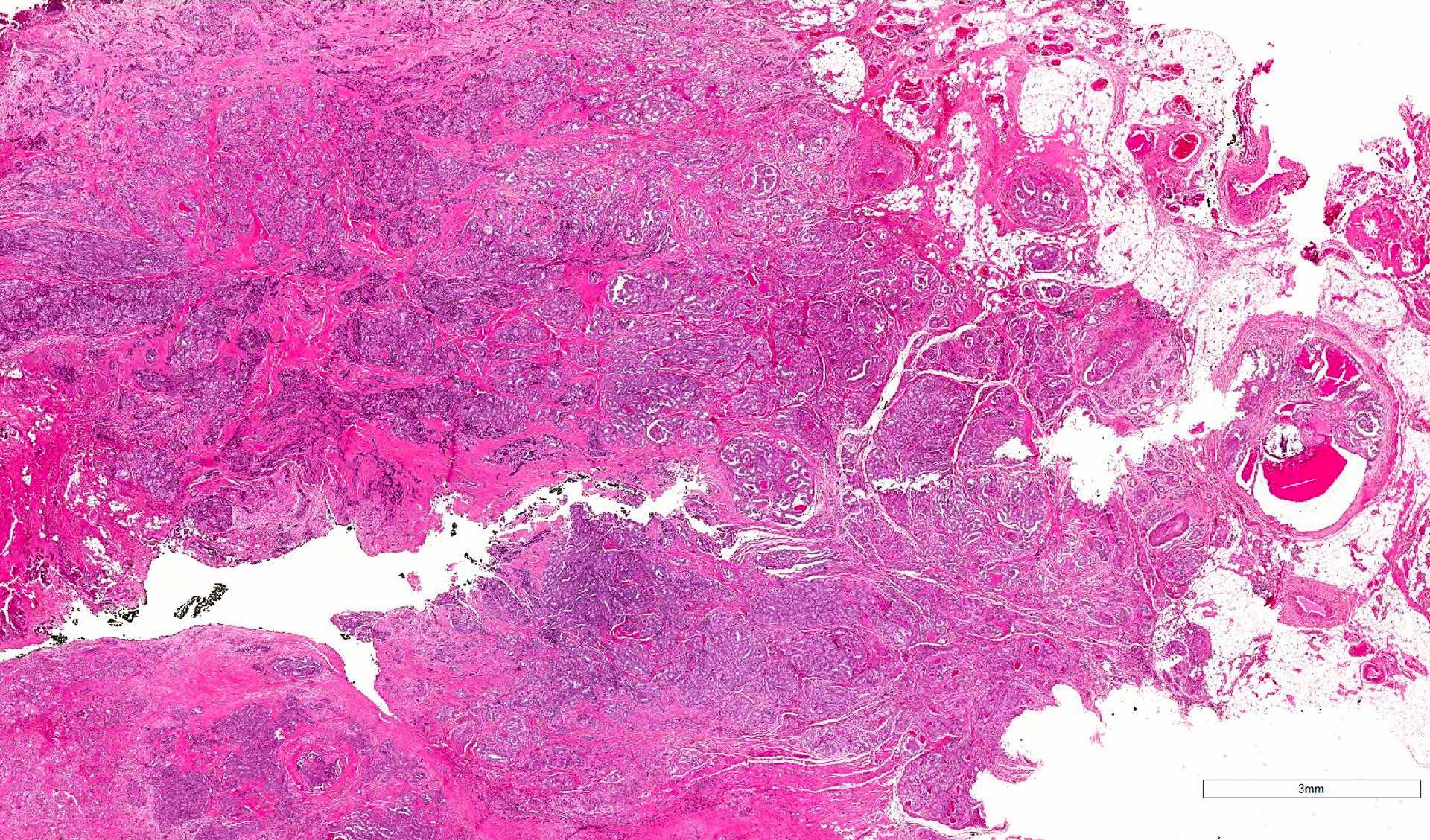
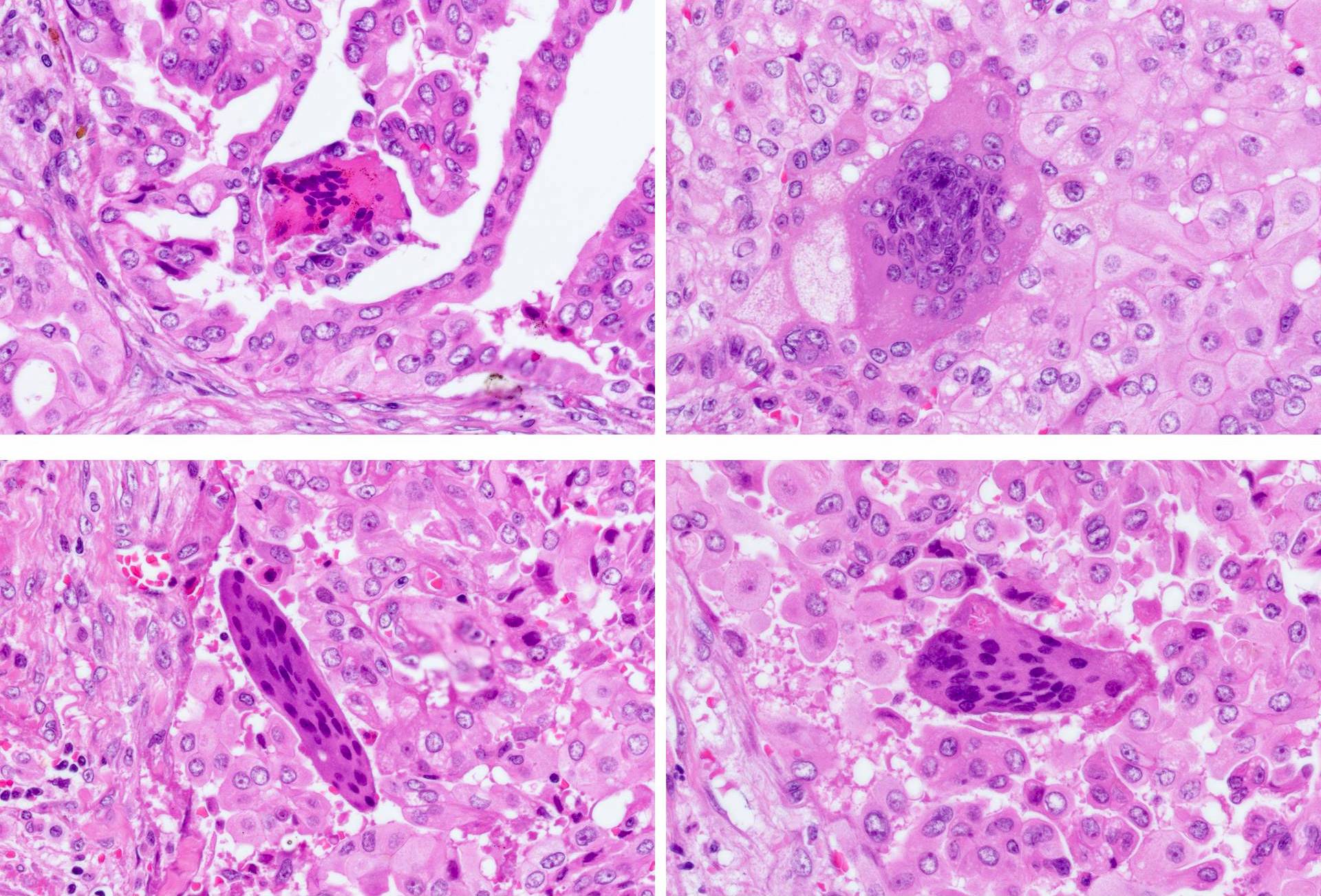
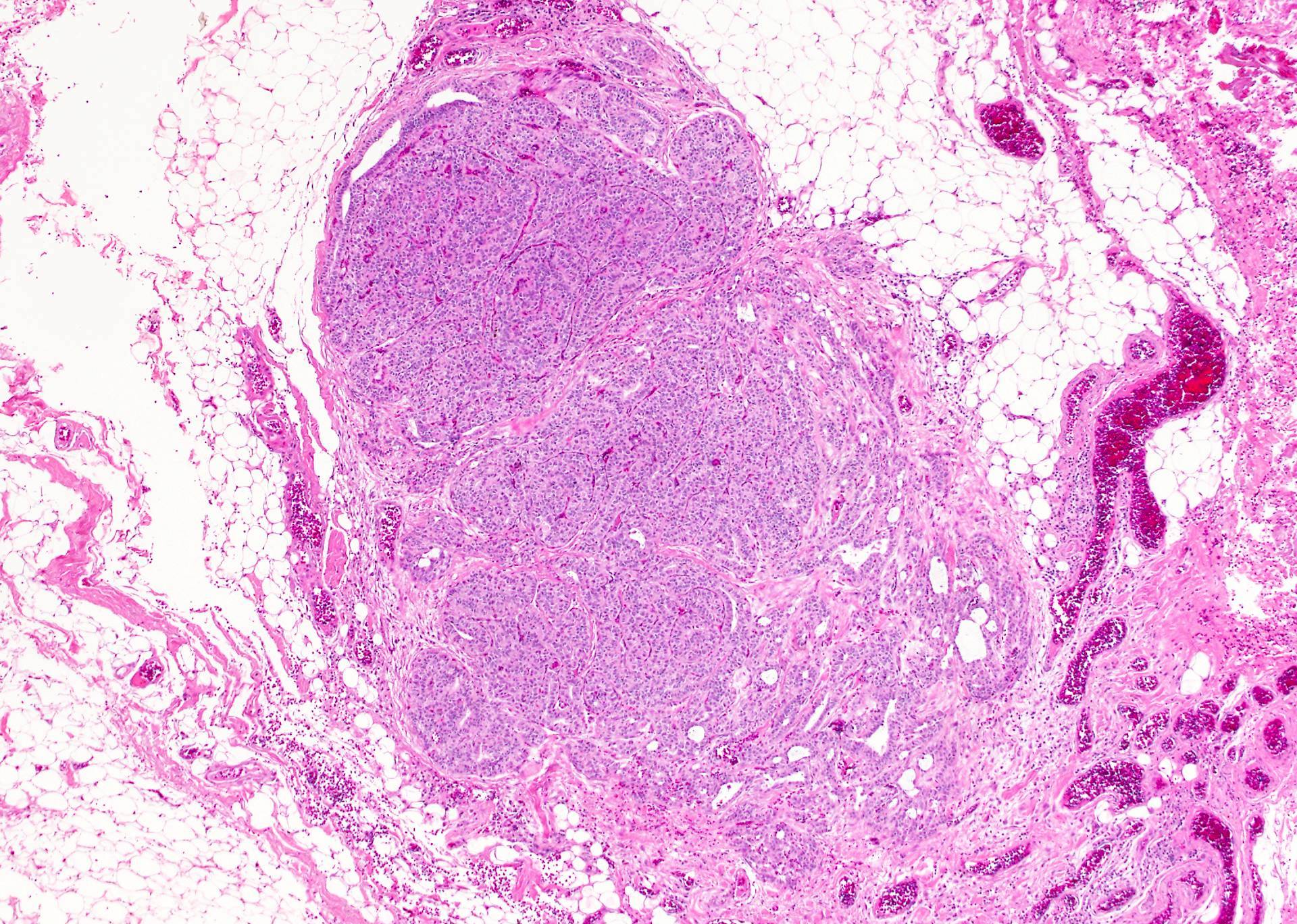
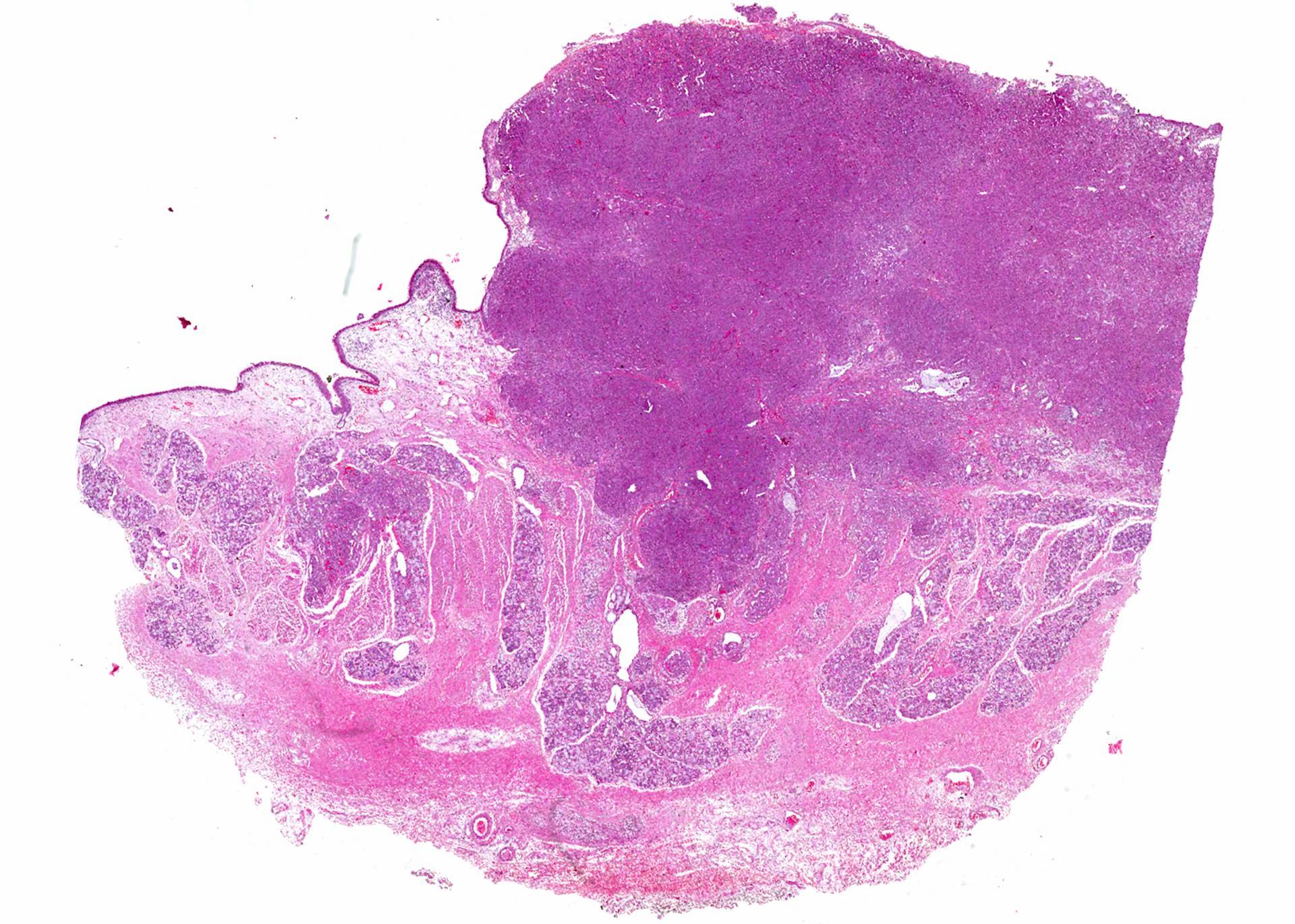
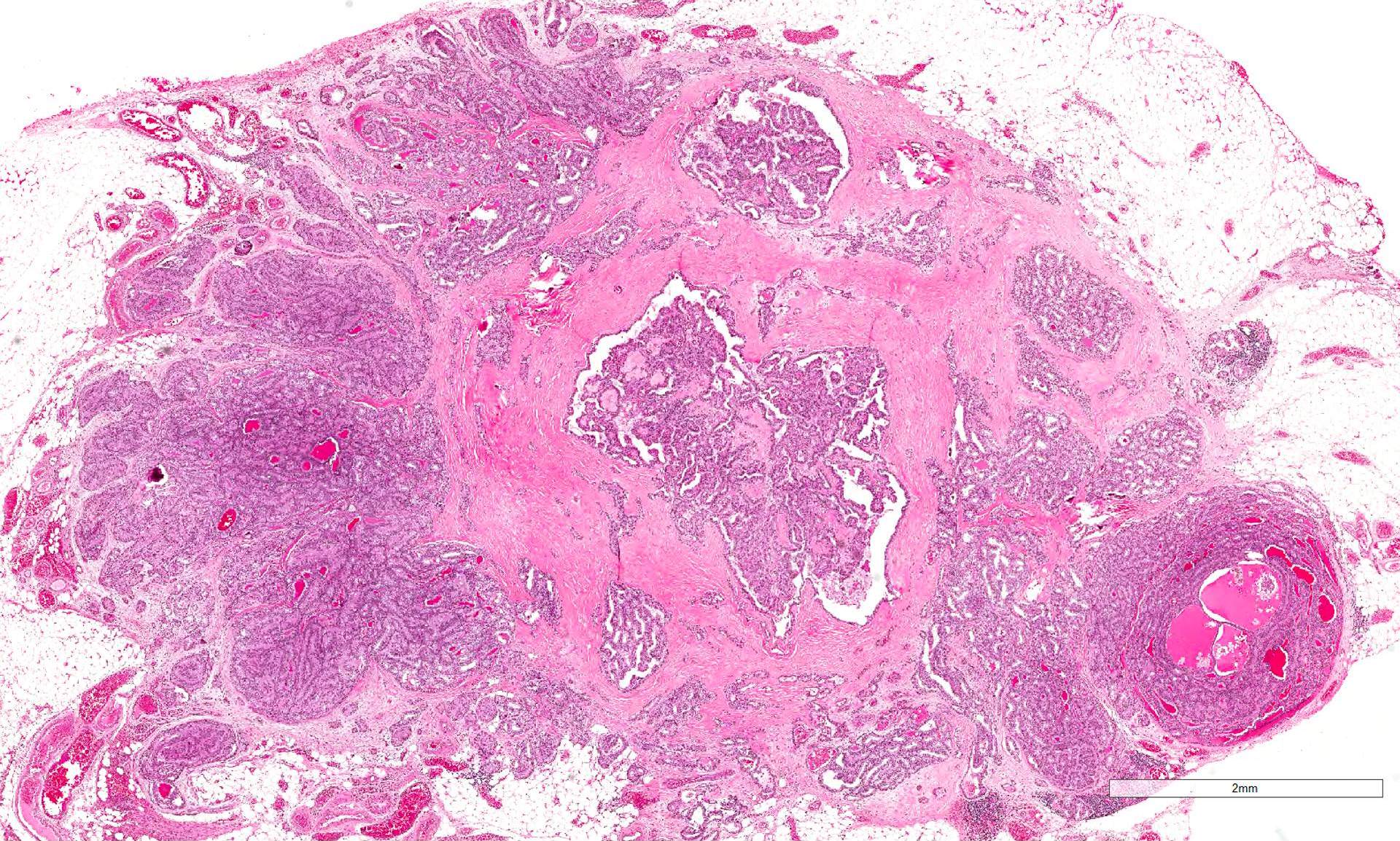
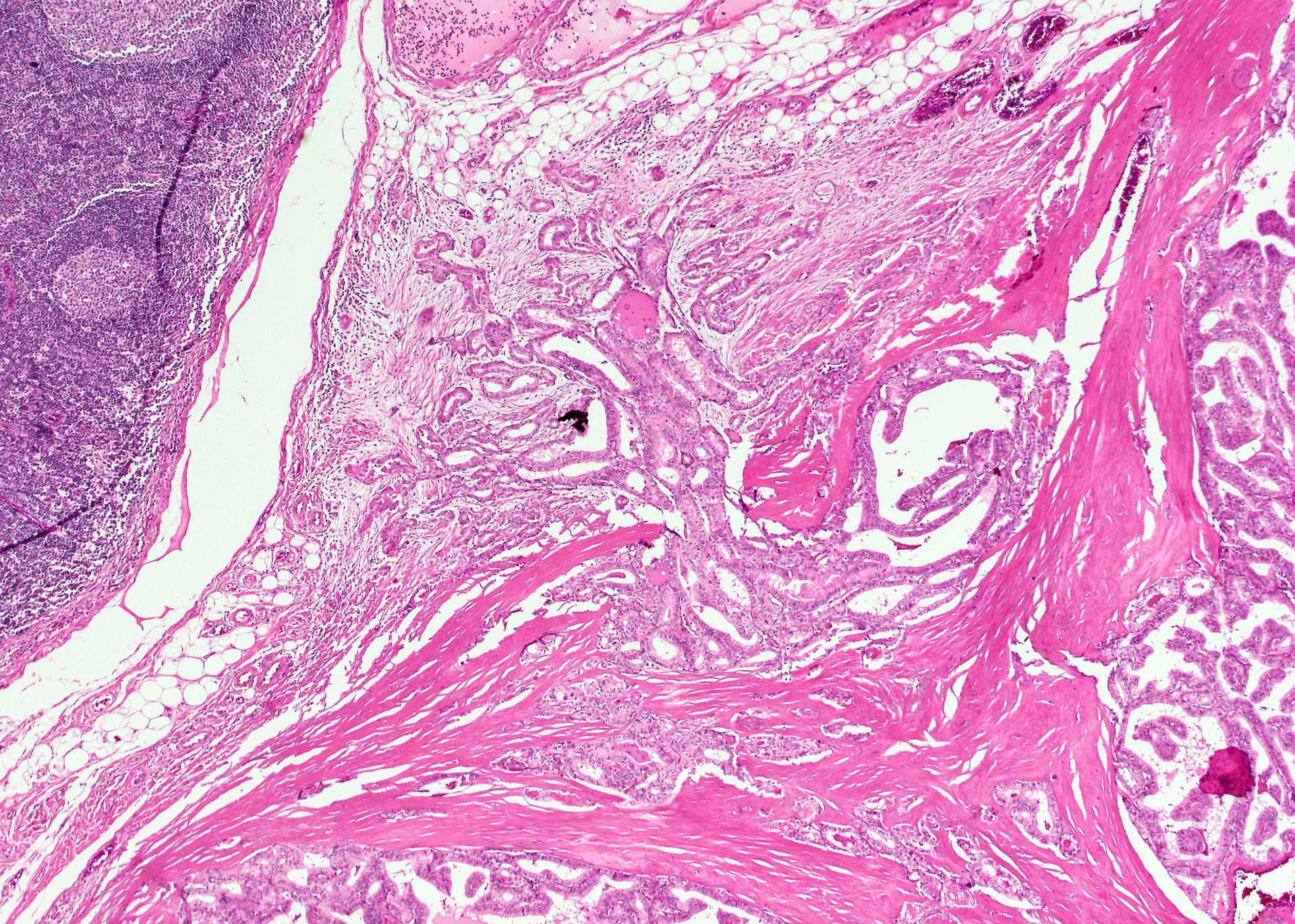
Microscopic (histologic) images
Contributed by Chan Kwon Jung, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D.
Videos
Extrathyroidal extension by J. Hernandez-Prera (2020)
Sample of case summary
-
Thyroid, total thyroidectomy:
- Papillary thyroid carcinoma of the right lobe, tall cell variant (4.7 x 2.5 x 2.5 cm)
- Lymphatic invasion positive
- No angioinvasion
- Minimal extrathyroidal extension (perithyroidal fat)
- Microscopically involved superior resection margin, all other margins negative
- Lymph node metastasis, 2/2 nodes (perithyroid), 0.5 cm in largest diameter, no extranodal extension
- Hashimoto thyroiditis of nonneoplastic thyroid
- pT3a (size > 4 cm), pN1a (positive perithyroidal nodes)
Additional references
- Expert guides
- Local experience
- Clinical guidelines
Board review style question #1
- Which histopathologic feature is not mandatory to report according to the CAP thyroid protocol?
- Extranodal extension
- Histologic type
- Lymphatic invasion
- Perineural invasion
- Tumor focality
Board review style answer #1
D. Perineural invasion is an optional feature to report, because its clinical significance is not well defined.
Comment Here
Reference: Features to report
Comment Here
Reference: Features to report