Table of Contents
Definition / general | Diagrams / tables | Clinical features | Clinical images | Gross description | Gross images | Microscopic (histologic) images | Videos | Additional referencesCite this page: Bychkov A. Anatomy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidanatomy.html. Accessed April 23rd, 2024.
Definition / general
- Thyroid gland is a bilobed organ in the lower half of anterior neck, which is composed of two bulky lateral lobes joined by a thin isthmus
- Location
- Anterior region of the neck, midway between thyroid cartilage and suprasternal notch (level of C5 - T1 vertebrae)
- Immediately anterior to larynx and trachea, being attached to anterior trachea by loose connective tissue
- Two lobes lie on both sides of larynx and trachea, reaching the lower halves of thyroid cartilage and covering II - IV tracheal rings
- Isthmus lies across the trachea anteriorly, below the level of cricoid cartilage (II - III tracheal rings)
- Shape of adult thyroid resembles a butterfly or a capital H, with each lobe having pointed upper and blunted lower poles
- Practical implications for pathologists
- Grossing of surgical thyroid specimens, which are submitted as a single lobe (lobectomy), lobe with isthmus (hemithyroidectomy) or the whole gland (total thyroidectomy); other procedures are subtotal thyroidectomy and neck dissection
- Evaluation of the organ on autopsy
- Thyroid FNA by interventional cytopathologist, often combined with ultrasound
- Historical aspects
- English name for thyroid gland is derived from the Greek thyreoeidos (Thyreos = shield, eidos = form); German word Schilddrüse means "shield gland"
- Leonardo Da Vinci (1452 - 1519) is credited as the first to draw thyroid gland as an anatomical organ, although "glands" in the neck corresponding to the thyroid (mainly pathologically enlarged) were known for thousands of years (Clin Anat 2011;24:1)
- The gland was named thyroid by Thomas Wharton (1614 - 1673) because of its proximity to the thyroid cartilage (Wharton, Adenographia: sive glandularum totius corporis descriptio)
Diagrams / tables
Clinical features
Anatomical relationships
Variations
Blood supply
Lymphatic drainage
Innervation
- Thyroid gland is enveloped by the middle layer of deep cervical fascia (false capsule), which forms a suspensory ligament (ligament of Berry) on the posterior surface; this ligament fixes the gland to the trachea and facilitates movement of thyroid during swallowing
- Anterior surface of thyroid lobes and isthmus is covered by sternothyroid muscle
- Medial surface is adjacent to superior trachea and larynx with thyroid cartilage
- Lateral surface of both lobes is covered by sternothyroid muscle
- Recurrent laryngeal nerves run in groove between trachea and esophagus behind the medial aspects of the lateral lobes
- Common carotid artery, internal jugular vein and vagus, encased within the carotid sheath, course along the posterolateral aspects of the lateral lobes
- Parathyroid glands are usually adjacent to posterior surface
- Surgically important anatomical relations of thyroid are recurrent laryngeal nerve, parathyroid glands and external branch of laryngeal nerve and accidental injury of these structures during thyroid surgery may result in lifelong clinical consequences (Clin Anat 2012;25:19)
Variations
- Mild thyroid developmental anomalies include pyramidal lobe, thyroglossal duct cysts and thyroid hemiagenesis (Pediatr Endocrinol Rev 2016;13:612)
- Pyramidal lobe (lobe of Lalouette) is a vestige of the inferior portion of thyroglossal duct
- Narrow conical shaped projection of thyroid tissue extending upward from isthmus to hyoid bone and lying on the surface of thyroid cartilage (Surg Radiol Anat 2007;29:21)
- Present in approximately half of all thyroid glands, reported range 30% - 75% (Surg Radiol Anat 2007;29:21)
- Mean length 24 mm, with half of pyramidal lobes exceeding 20 mm (Rom J Morphol Embryol 2013;54:285)
- More frequently attached to the left side of the isthmus and even to the left lobe itself
- Usually appears as fibrous tract, but in pathologic conditions becomes prominent or cystic
- Thyroid tissue in pyramidal lobe is usually not active, hence is not visible on scintigraphy (Rom J Morphol Embryol 2013;54:285)
- Pyramidal lobe can be a source of recurrent disease if it is left behind during thyroid surgery
- Rare structural abnormalities
- Small accessory thyroids derived from thyroglossal duct remnants can be found close to the normally located gland
- Absence of the isthmus with two independent lateral lobes has been reported in 5% - 30% (J Anat Physiol 1895;29:234, Singapore Med J 2008;49:831)
- Infrequent anatomic variants:
- Posterior part is split into two distinct globes of thyroid tissue (5% of population, Netter: Endocrine System and Selected Metabolic Diseases, Vol 4, 1965)
- Absence of a significant portion of a lateral lobe (< 1% of healthy individuals), frequently the lower half of the left lobe (De Groot: Endocrinology Adult and Pediatric: The Thyroid Gland, 6th edition, 2013)
- Inverted U shaped thyroid (Indian J Otolaryngol Head Neck Surg 2014;66:224)
- W shaped thyroid (J Clin Diagn Res 2014;8:AD03)
- Levator muscle of thyroid gland (levator glandulae thyroideae of Soemmerring)
- Fibrous or fibromuscular band that stretches from pyramidal lobe or upper border of isthmus, usually on the left side, to the body of hyoid bone
- Origin is related to thyroglossal duct (can be considered as caudal extension/part of pyramidal lobe), may contain thyroid follicles
- Tubercle of Zuckerkandl
- Posterior extension of the lateral edge of thyroid lobe that stems from the fusion of the lateral and median thyroid anlages (Clin Anat 2012;25:19)
- Appears as focal enlargement from a slight thickening to 1 cm or larger nodular structure
- Can be found on either side or bilaterally in 60% - 95% of thyroidectomies (World J Endoc Surg 2014;6:110)
- Helpful surgical landmark for identification of recurrent laryngeal nerve, which runs medially, sometimes in a cleft between the tubercle and lateral lobe
- Superior parathyroid gland is commonly found just cephalad to the tubercle
Blood supply
- Thyroid is extremely vascular
- Arterial supply is derived from the right and left superior thyroid arteries and the right and left inferior thyroid arteries
- Inferior thyroid artery (originates from thyrocervical trunk of the subclavian artery) approaches base of the gland and divides into superior and inferior branches to supply inferior and posterior surfaces of thyroid gland
- Smaller superior thyroid artery (arises from the external carotid) enters upper pole of the gland and divides into anterior and posterior branches to supply anterior, lateral and medial surfaces
- Arteria thyroidea ima is inconsistent (3% - 10%) and variable in terms of origin (from brachiocephalic trunk or aortic arch), size and area of supply
- Branches of arteries anastomose frequently on surface and within the gland
- Venous drainage is through the superior, middle and inferior thyroid veins (form venous plexus in the thyroid capsule), which open into the internal jugular and brachiocephalic veins
Lymphatic drainage
- Thyroid lymphatics originate from interfollicular spaces and form rich intraglandular (lying in the interlobular connective tissue) and subcapsular networks
- Larger subcapsular collecting trunks leave the gland in close proximity to the veins and drain into the regional lymph nodes
- Pericapsular (perithyroidal) nodes
- Internal jugular chain nodes (e.g. subdigastric) draining superior portion of thyroid lobes and isthmus
- Pretracheal, paratracheal and prelaryngeal (including midline located Delphian node), draining inferior portion of the gland
- Recurrent laryngeal nerve chain nodes
- Retropharyngeal and retroesophageal lymph nodes
- Bypass routes
- Anterosuperior mediastinal lymph nodes are secondary to the recurrent laryngeal nerve chain and pretracheal groups, but thyroid isthmus portion can be also drained directly into them (Ann Surg 1957;145:317)
- Thyroid lymphatics may empty directly with no intervening node into thoracic duct
- Grouping of the thyroid draining lymph nodes according to the cervical lymph node levels (ordered by proximity)
- Level VI: pericapsular, paralaryngeal, paratracheal, prelaryngeal and recurrent laryngeal chain
- Levels III - IV: internal jugular (also known as deep cervical)
- Level VII: superior mediastinal
- Level I: submandibular and submental
- Anatomy of thyroid lymphatics explains patterns of spread of thyroid cancer
- Abundant network of intraglandular lymphatics freely anastomosing between lateral lobes through the isthmus is responsible for the intrathyroidal spread common in papillary carcinoma
- Plexus of pericapsular lymph nodes and vessels permits the transfer of cancer cells from the surface of one part of the gland to another (Cancer 1963;16:1425)
- First extraglandular metastasis of papillary carcinoma occurs in paratracheal nodes, regardless of the location of the primary tumor
- In the early cancer stages, metastases are more frequent in the lower part of the neck, and in later stages, when lymphatic obstruction has occurred, metastases appear in upper (up to submandibular) nodes (Cancer 1970;26:1053)
Innervation
- Thyroid gland receives only a few nerve fibers compared to other visceral organs
- Innervated from superior, middle and inferior cervical sympathetic ganglia
- Adrenergic nerve fibers may influence thyroid secretion indirectly via vasomotor effects (J Endocrinol Invest 1978;1:175)
- Presence of adrenergic receptors in follicular cells and a network of adrenergic nerve terminals near follicular basement membrane suggest direct sympathetic regulation of thyroid secretion (Endocrinology 1975;97:1123)
- Cholinergic nerve fibers derived from vagus are also found, suggesting a role of parasympathetic nervous system in the regulation of thyroid activity (e.g. C cells in chicken are surrounded by rich cholinergic network, Am J Anat 1988;182:353)
- Overall impact of nervous system on thyroid secretion is negligible compared to hypothalamic-pituitary axis (via TSH)
- Small paraganglia are normally present close to thyroid and occasionally found beneath thyroid capsule, which explains origin of peri- and intrathyroidal paragangliomas
Clinical images
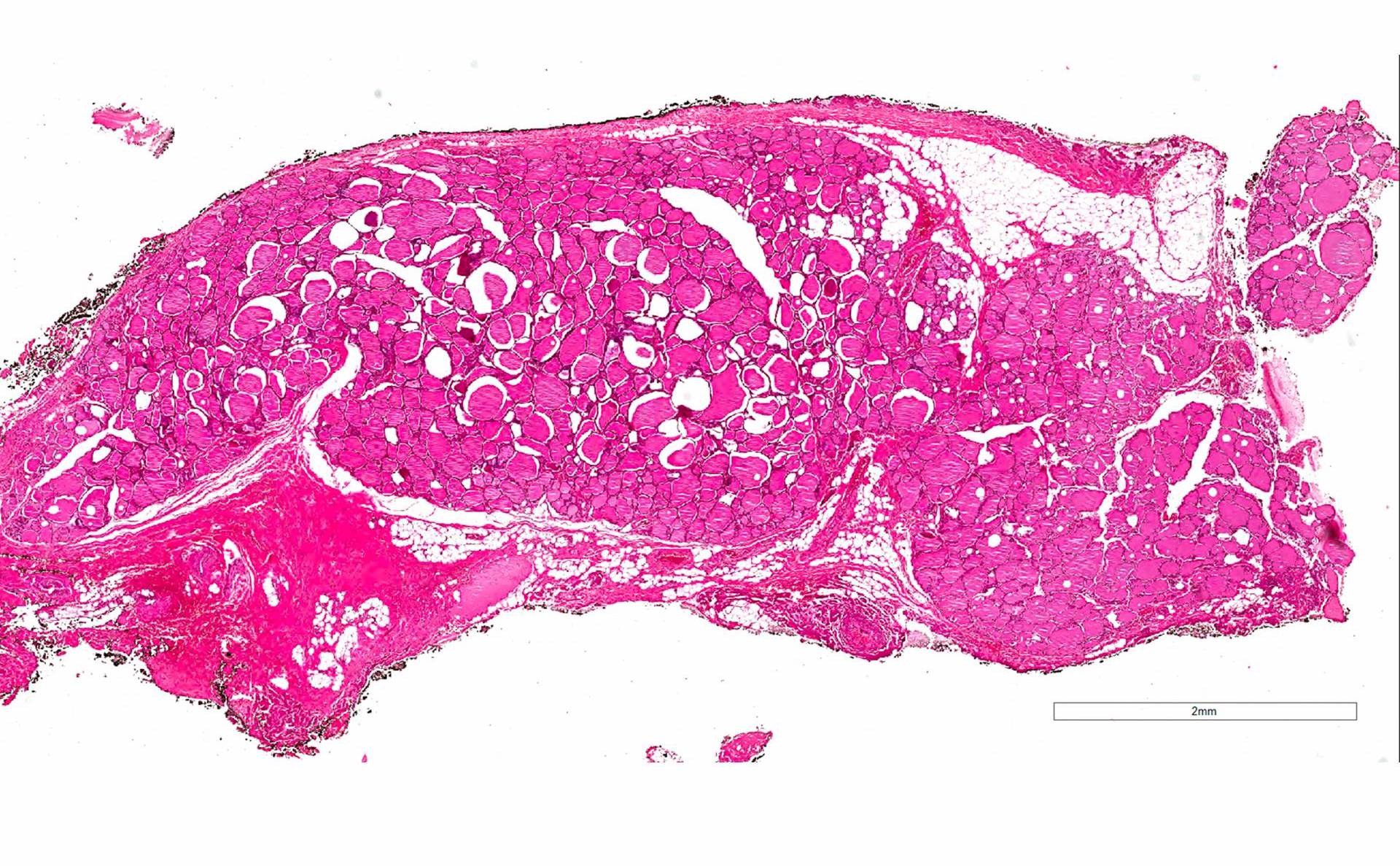
Gross description
- Weight
- Normal adult weight in non-endemic area is 15 - 20 g (M > F), increase over 50 g is likely abnormal (Health Phys 1985;49:1097, Ann ICRP 2002;32:5)
- Depends on gender (heavier in women during secretory phase of menstrual cycle), body weight and iodine intake (iodine deficiency is a main cause of goiter)
- Increases in childhood and adolescence (weight doubles from 5 to 10 years and from 10 to 20 years), also during pregnancy; shrinks in elderly (Health Phys 1963;9:1299, Ann ICRP 2002;32:5)
- Children
- Normal weight in newborn is 1 - 3 g, 5 g is borderline for goiter (Acta Obstet Gynecol Scand 1948;28:1, Virchows Arch Pathol Anat Physiol Klin Med 1964;338:30)
- Tables with a weight of fetal thyroid in relation to gestational age and body weight are available (Anat Rec 1964;148:123, Anat Rec 1971;171:227, Pediatr Dev Pathol 2002;5:559)
- Size
- Each lateral lobe is 4 - 6 cm long, 2 - 3 cm wide and 1.5 - 2 cm deep (anteroposterior)
- Isthmus is about 1.25 cm in greatest transverse and vertical dimensions and 0.5 cm thick
- Right lobe is usually larger than the left one (up to twice), isthmus may be exceptionally wide (De Groot: Endocrinology Adult and Pediatric: The Thyroid Gland, 6th Edition, 2013)
- Easily estimated by sonography along with thyroid volume (10 - 15 ml)
- Most thyroid diseases have significant alterations in these measurements
- Thyroid parenchyma is reddish brown in color
- Coal black stain due to pigment accumulation can be noted in elderly individuals (Mills: Histology for Pathologists, 4th Edition, 2012)
- Homogenous firm consistency
- 10% of endocrinologically normal adults have asymptomatic grossly identified thyroid nodules (J Clin Pathol 1986;39:475)
- Thin fibrous capsule is firmly attached to the surface and produces septa, which incompletely divide parenchyma into lobules (thyromeres)
Videos
Thyroid anatomy