Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Electron microscopy description | Additional referencesCite this page: Chi A, Guilmette J. Amiodarone induced hyperthyroidism. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidamiodarone.html. Accessed April 19th, 2024.
Definition / general
- Amiodarone is an antiarrhythmic medication for atrial and ventricular tachyarrhythmias, and less commonly for ischemic heart disease and congestive heart failure; also used for fetal tachycardia (Arch Cardiovasc Dis 2008;101:619, eMedicine)
- Contains 37% iodine by weight, and structurally resembles thyroxine, which interferes with thyroid hormone metabolic pathways, causing hypo- or hyperthyroidism
- The relative frequency of amiodarone induced hypothyroidism (AIH) and amiodarone induced thyrotoxicosis (AIT) depends on the iodine status of the population
- In populations with iodine deficiency, amiodarone induced thyrotoxicosis is more common
- Conversely, in the United States, amiodarone induced hypothyroidism is more common (Proc (Bayl Univ Med Cent) 2008;21:382)
- AIT is classified in two subtypes, type 1 AIT and type 2 AIT
- Distinguishing between the two subtypes is important as both arise in different settings and have different treatments (Case Rep Med 2014;2014:231651)
Essential features
- Amiodarone induced thyrotoxicosis (AIT) is classified in two subtypes (Case Rep Med 2014;2014:231651)
- Type 1 AIT arises in thyroid glands with preexisting disease (Jod-Basedow phenomenon)
- Type 2 AIT develops in a previously normal thyroid gland due to a destructive amiodarone induced inflammatory process
- Presents with worsening cardiac arrhythmia, recurrent atrial fibrillation and palpitations (NCBI - Amiodarone Induced Thyrotoxicosis)
- Diagnosis requires correlation of clinical, imaging and laboratory findings
- Histologically, type 1 AIT has features of preexisting disease; type 2 AIT shows involuted follicles filled with desquamated vacuolated epithelial cells, scattered inflammatory infiltrate composed of foamy macrophages and lymphocytes, and fibrosis (Proc (Bayl Univ Med Cent) 2008;21:382, Pathol Int 2008;58:55)
Epidemiology
- More frequent in males than in females (3:1)
- Occurs in 3% of patients treated with amiodarone in North America, increasing to 10% in countries with low iodine dietary intake (NCBI - Amiodarone Induced Thyrotoxicosis)
Sites
- In addition to the thyroid gland, amiodarone can affect the lungs, liver, cornea and skin (Pathol Int 2008;58:55, Cutan Ocul Toxicol 2017;36:98 )
Pathophysiology
- Thyrotoxicosis is due to amiodarone's iodine content and structural resemblance to thyroxine
- Amiodarone has pharmacological properties enabling its toxicity (Can J Cardiol 2009;25:421), including:
- Lipophilia, promoting accumulation in adipose tissue, cardiac and skeletal muscle, and thyroid
- Inhibition of thyroidal T4 and T3 production and release within the first two weeks of treatment (Wolff-Chaikoff effect)
- Direct toxicity to cultured thyroid cells exposed to media with concentrations above those normally found in patients
Clinical features
- Associated with worsening cardiac arrhythmia with recurrence of atrial fibrillation and palpitations (NCBI - Amiodarone Induced Thyrotoxicosis)
- May occur suddenly in patients treated with amiodarone for several years, likely due to its long half life, lipid solubility and accumulation in almost all tissue
- Type 1 amiodarone induced thyrotoxicosis:
- Occurs with preexisting thyroid disease, due to iodine induced excess thyroid hormone synthesis
- Microscopic changes are due primarily to preexisting disease
- Type 2 amiodarone induced thyrotoxicosis:
- Develops as an inflammatory process in a normal thyroid (NCBI - Amiodarone Induced Thyrotoxicosis)
- Due to destructive thyroiditis (Endocr Rev 2001;22:240)
- Amiodarone is probably the cause of thyroid cell damage in some patients, and follicular disruption (with consequent release of iodothyronines into the circulation) is likely to be an important contributor to associated thyrotoxicosis (Am J Surg Pathol 1987;11:197)
Diagnosis
- Based on clinical, laboratory and imaging correlations
Laboratory
- To confirm the diagnosis of amiodarone induced thyrotoxicosis, it is necessary to demonstrate a suppressed serum TSH associated with an increase in serum free T3 and free T4 levels in a patient treated with amiodarone (NCBI - Amiodarone Induced Thyrotoxicosis)
- In type 1: increased T4 / T3 due to destructive thyroiditis, in addition to increased levels of antibodies to thyroglobulin and TPO
- In type 2: elevated levels of IL6; 8% also have increased levels of antibodies to thyroglobulin and TPO
Radiology description
- Color flow Doppler ultrasonography is useful to differentiate between type 1 and type 2 (NCBI - Amiodarone Induced Thyrotoxicosis, World J Surg 2006;30:1957)
- Type 1:
- Increased intrathyroidal vascular flow
- Normal or raised radioactive iodine update
- Tc sestamibi thyroid scan shows a diffusely increased uptake and retention in an enlarged thyroid gland (Clin Nucl Med 2016;41:566)
- Type 2:
- Reduced or absent vascular flow
- Low or absent radioactive iodine update
Case reports
- 59 year old man with type 2 disease and papillary thyroid carcinoma (Arch Pathol Lab Med 2004;128:807)
- 64 year old woman with nodular goiter (Ann Pharmacother 2009;43:134)
- 65 year old man with fatal amiodarone induced thyrotoxicosis (J Med Case Rep 2007;1:134)
- 66 year old man with thyrotoxicosis (Arch Pathol Lab Med 2003;127:e275)
- 66 year old man with medically refractory amiodarone induced thyrotoxicosis requiring thyroidectomy (Proc (Bayl Univ Med Cent) 2008;21:382)
Treatment
- Differs for type 1 and 2 amiodarone induced thyrotoxicosis (Minerva Endocrinol 2008;33:213)
- Up to 20% of mild cases spontaneously resolve (NCBI - Amiodarone Induced Thyrotoxicosis)
- Type 1: treat with high doses of thioamides to block synthesis of thyroid hormones
- Potassium perchlorate can also be combined to increased sensitivity to thioamides
- Once the thyroid function is normalized, hyperthyroidism can be treated by either radioactive iodine or thyroidectomy depending on its severity
- Type 2: treat with prednisone; thionamides are generally not useful
- Clinically, "mixed" AIT is common, in which patients seems to be respond only to therapy with both thioamides and glucocorticoids (Proc (Bayl Univ Med Cent) 2008;21:382)
- Dronedarone is an alternative but less effective antiarrhythmic agent without the adverse thyroid effects (Clin Endocrinol (Oxf) 2009;70:2)
Gross description
Type 2 amiodarone induced thyrotoxicosis:
- Firm in consistency, normal shape (Case Reports in Endocrinology 2015; Article ID 416145)
- Homogeneous "beefy red" parenchyma (Arch Pathol Lab Med 2004;128:807)
Microscopic (histologic) description
- Associated with type 1 amiodarone induced thyrotoxicosis: changes are those of preexisting disease, usually multinodular goiter
- Associated with type 2 amiodarone induced thyrotoxicosis: often with no history of thyroid disorder
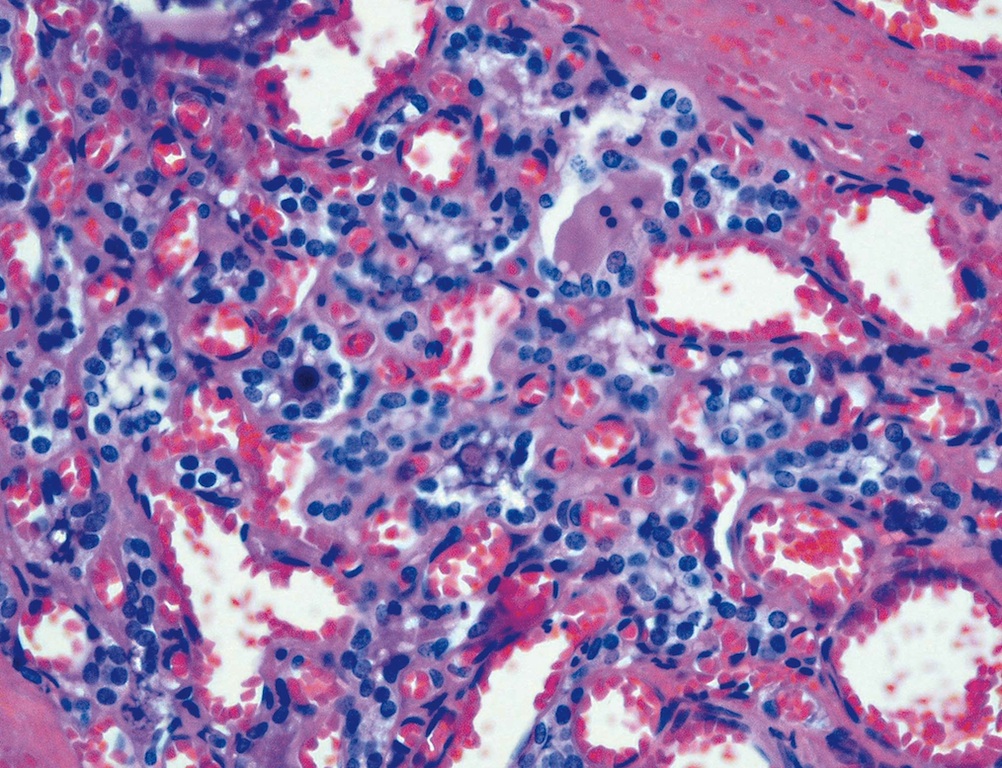
- Randomly distributed disrupted follicles filled with desquamated vacuolated epithelial cells, foamy macrophages and scattered lymphocytes, involutional changes, fibrosis
- Associated with hypothyroidism: involuted follicles with flattened follicular cells, dilated lumina with dense colloid; also small numbers of damaged follicles infiltrated by macrophages (Pathol Int 2008;58:55)
Microscopic (histologic) images
Electron microscopy description
- Prominent cytoplasmic vacuoles with lipid
- Also prominent lysosomes with lamellar configuration (Lloyd: Endocrine Diseases, 1st Edition, 2002)
- It is speculated that this may result from impairment of lysosome function
Additional references