Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Patton A, Parwani A. Spermatocele. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testisspermatocele.html. Accessed January 12th, 2025.
Definition / general
- Benign dilatation of efferent ductules in the rete testis or head of epididymis
- Size ranges from a few millimeters up to 2 cm
Essential features
- Benign dilatation of the efferent ductules in the rete testis or head of the epididymis
- Usually idiopathic but cystic dilation from outflow obstruction may play a role
- Diagnose by ultrasound demonstrating a well defined simple cyst
- Lined by cuboidal, columnar, ciliated or flattened epithelium
- Cystic contents often contain spermatozoa
Terminology
- Often indistinguishable from epididymal cyst
Epidemiology
- All ages affected but typically occurs in 20 - 50 year old men
Sites
- Testis, epididymis
Etiology
- Usually idiopathic but cystic dilation from outflow obstruction may play a role (Am J Hematol 1990;34:132)
- Higher incidence in cystic fibrosis and diethylstilbestrol exposure in utero (J Pediatr Surg 2013;48:2153)
Clinical features
- Painless bulging mass separate from testicle
Diagnosis
- Diagnosed by radiological imaging, including ultrasound and less commonly by MRI, followed by pathological evaluation of the resection specimen
Radiology description
- By ultrasound, simple cysts are generally well defined and anechoic; however, low level echos (falling snow sign) or sedimentation levels can be seen (Clin Radiol 2008;63:929, Abdom Radiol (NY) 2020;45:587)
- Cyst may displace the testis if it is large
- Distinct from hydrocele, which envelops the testis but does not displace it
Case reports
- 25 year old man with rare acute scrotal pain associated with a spermatocele (Urol J 2008;5:206)
- 53 year old man with spermatocytes observed in an FNA of a spermatocele (Diagn Cytopathol 2019;47:972)
- 55 year old man with a giant spermatocele mimicking a hydrocele (Kaohsiung J Med Sci 2007;23:366)
Treatment
- Surgical resection, spermatocelectomy
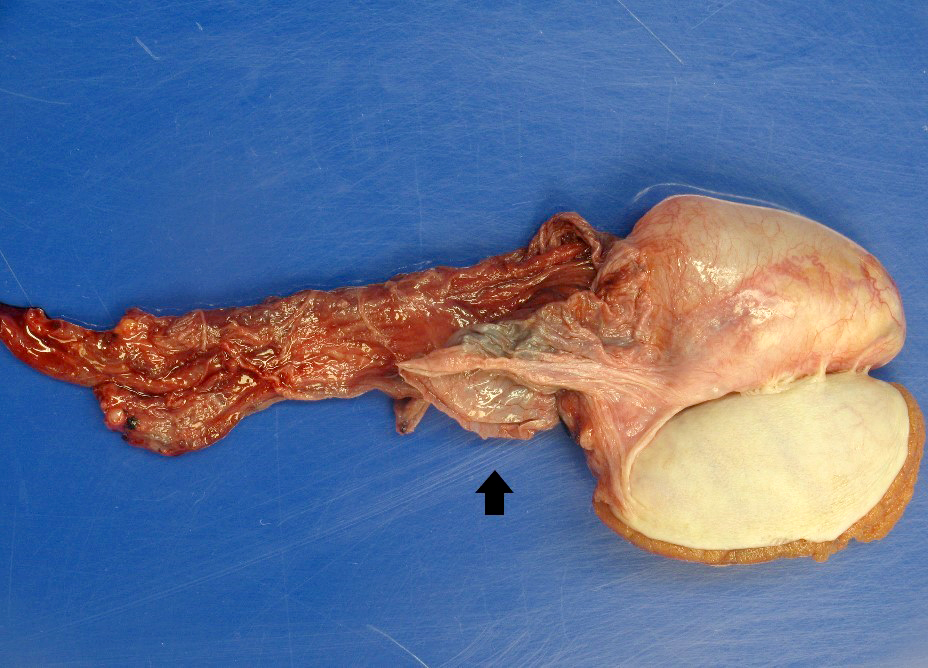
Gross description
- Arrives in laboratory as a collapsed, thin walled membrane (Urology 1984;24:372)
- Round or ovoid
- Cysts may be unilocular or multilocular and translucent (Urology 1984;24:372)
- Most commonly arises from the head of the epididymis
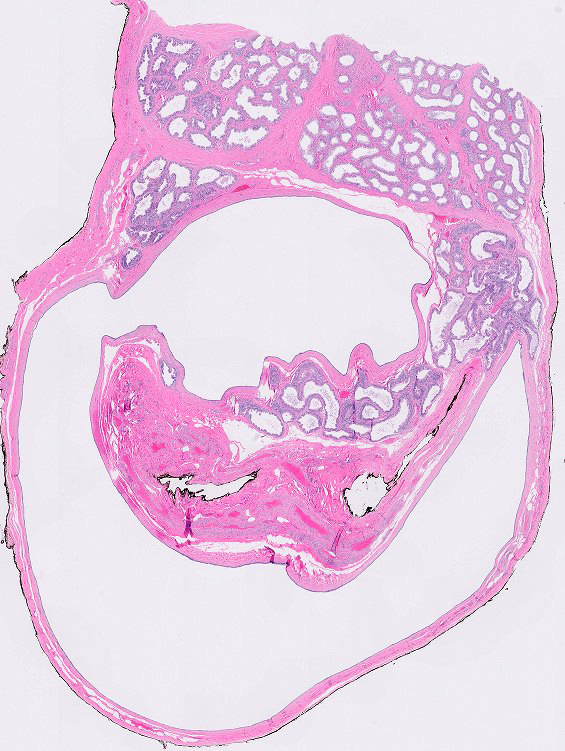
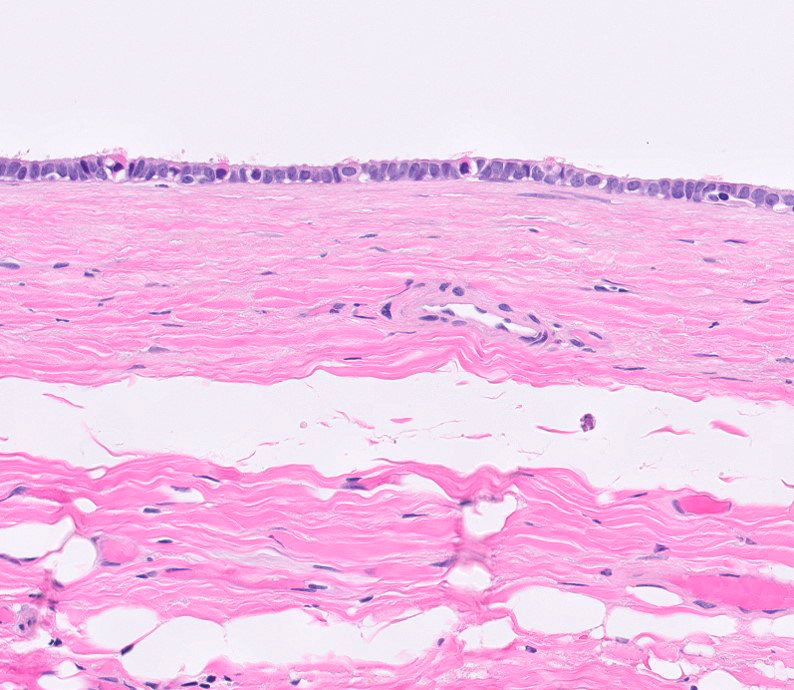
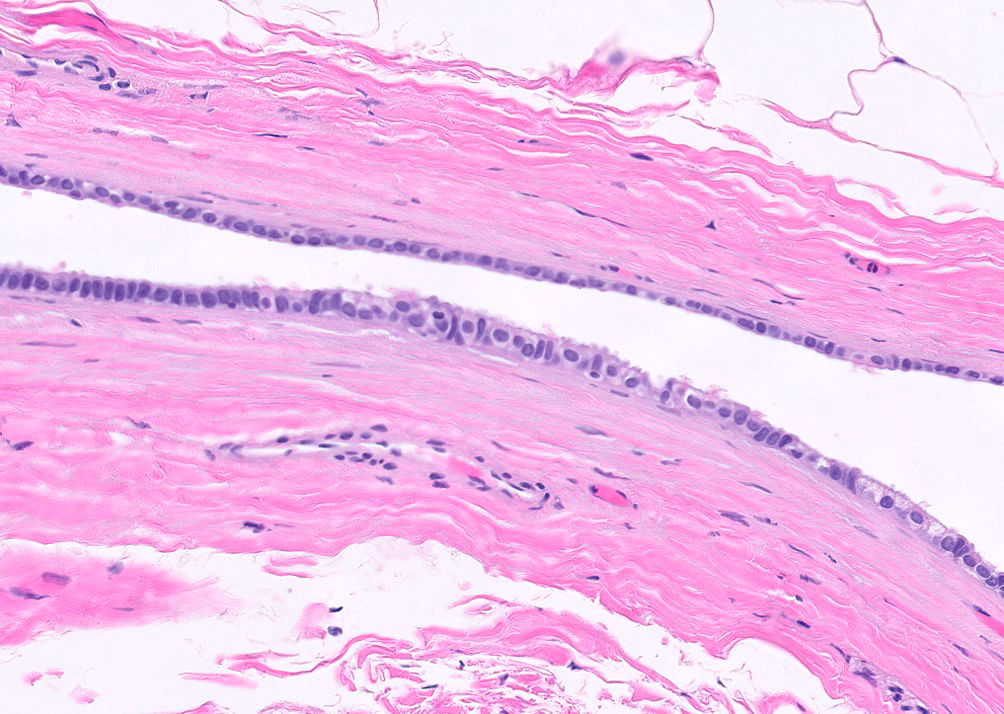
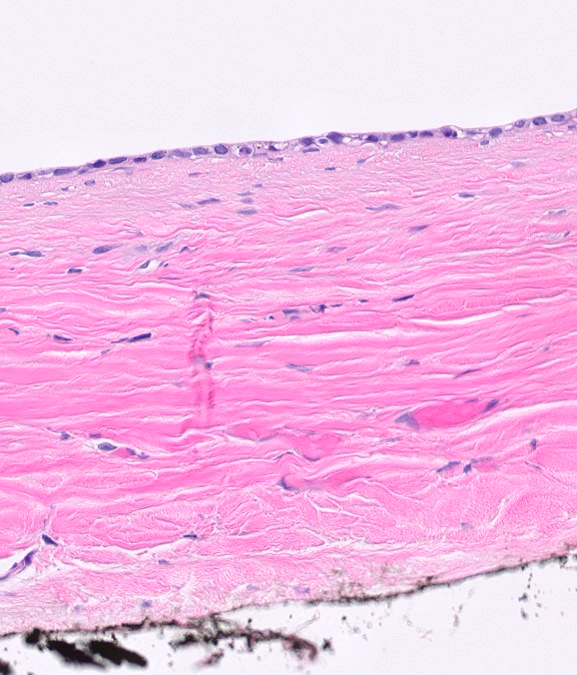
Microscopic (histologic) description
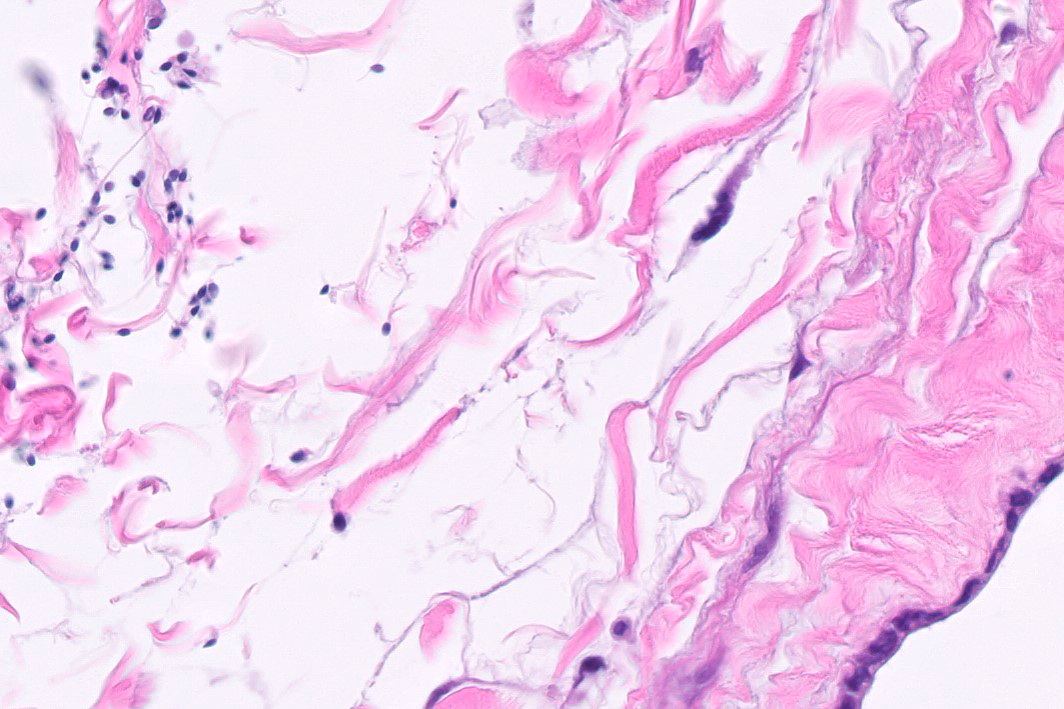
- Initially lined by single layer of cuboidal to ciliated columnar epithelium which becomes flattened as fluid accumulates (Urology 1984;24:372)
- Thin wall of fibromuscular soft tissue
- Lumen, cyst wall and adjacent soft tissue contains spermatozoa and proteinaceous fluid (Diagn Cytopathol 2010;38:816)
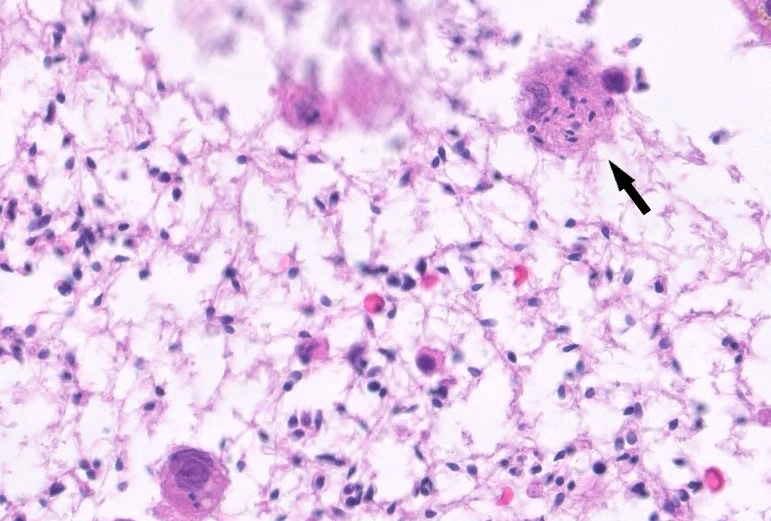
- Associated with foreign body giant cell reaction, cholesterol clefts (Diagn Cytopathol 2010;38:816)
- Epithelial lining may form papillary structures with fibromuscular cores lined by a single layer of columnar to cuboid epithelium with vacuolated cytoplasm
Microscopic (histologic) images
Cytology description
- Cysts can contain spermiophages, macrophages with abundant distended cytoplasm containing intact spermatozoa (Diagn Cytopathol 2010;38:816)
Positive stains
Negative stains
Sample pathology report
- Cyst, spermatocelectomy:
- Spermatocele (see comment)
- Comment: A cyst with bland cuboidal lining is present, compatible with spermatocele.
Differential diagnosis
- Hydrocele:
- Originates between the parietal and visceral layers of tunica vaginalis
- Lining is mesothelial; lumen does not contain spermatozoa
- Mesothelial cyst:
- Usually originates from tunica vaginalis or tunica albuginea
- Cystic dysplasia of rete testis:
- Congenital lesion of newborns that is associated with ipsilateral renal agenesis
- Sertoliform cystadenoma of rete testis:
- Contains tubules with or without lumen (Am J Surg Pathol 2018;42:141)
- Simple cyst of rete testis:
- Bulges into the testis proper
- Common in men undergoing renal dialysis
- Columnar epithelium, calcium oxalate crystals, fibrosis and giant cells
- Tubular ectasia of rete testis:
- Has numerous dilated canaliculi
- Can coexist with a spermatocele (Arch Ital Urol Androl 2015;87:5)
- Dermoid cyst:
- Rarely presents within the spermatic cord or as a paratesticular mass
Additional references
Board review style question #1
Which of the following is a feature of spermatocele?
- Has a lining of mesothelial cells
- Is cytokeratin negative
- May have papillary infoldings with fibrovascular cores lined by vacuolated cuboidal or columnar cells
- Originates from the same membrane as hydrocele
Board review style answer #1
C. May have papillary infoldings with fibrovascular cores lined by vacuolated cuboidal or columnar cells. A benign papilloma consisting of papillary infoldings with fibrovascular cores lined by vacuolated or columnar cells may arise from the epithelial lining of the spermatocele. The lining can be cuboidal, columnar, ciliated or flattened epithelium, not mesothelium (answer A). Spermatocele is cytokeratin positive and can be distinguished from the mesothelial lining of a hydrocele by negative staining for D2-40 or calretinin (answer B). The origin of spermatocele is from rete testis / head of epididymis epithelium, whereas hydrocele originates from the mesothelium of the tunica vaginalis (answer D).
Comment Here
Reference: Spermatocele
Comment Here
Reference: Spermatocele
Board review style question #2
Board review style answer #2
A. Spermatoceles often originate from the epithelial lining of the epididymis. Varicoceles commonly originate from the pampiniform venous plexus (answer B). Dermoid cysts commonly originate from totipotential germ cells (answer C). Hydroceles commonly originate from the tunica vaginalis (answer D).
Comment Here
Reference: Spermatocele
Comment Here
Reference: Spermatocele