Cite this page: Al-Hussain T. Infertility. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testisinfertility.html. Accessed December 3rd, 2024.
Hypospermatogenesis
Definition / general
Additional references
- All stages of spermatogenesis present but reduced to a varying degree
- Includes the mixed pattern with some tubules showing Sertoli cells only or hyaline sclerosis with others tubules containing complete spermatogenesis
- Mild if changes in occasional tubules; severe if significant reductions in all tubules, moderate in between
- Often is thickening of tunica propria, interstitial fibrosis, tubular sclerosis, germ cell disorganization and sloughing into lumina
- Many causes of infertility induce hypospermatogenesis, such as diabetes mellitus, toxins, excess heat, varicocele, hypothyroidism, irradiation and others
Additional references
Infertility
Definition / general
Additional references
- Causes: pretesticular, testicular, posttesticular
- Pretesticular: extragonadal endocrine disorders (hypothalamic, pituitary, adrenal); includes elevated prolactin levels (Arch Pathol Lab Med 1984;108:35)
- Testicular: little treatment currently available
- Posttesticular: duct obstruction (congenital, inflammatory, postsurgical); surgical treatment often successful since spermatogenesis is normal
- Impaired sperm motility due to epididymal or immunologic factors is considered posttesticular
- Evaluation: history and physical examination, semen analysis, white blood cell count in semen, detection of antisperm antibodies, sperm function tests (cervical mucus interaction, ova penetration, hemizonal assay)
- Testicular biopsy is helpful for azoospermia without endocrine abnormalities
- RNA binding motif: nuclear immunostain identifies spermatogenesis in biopsies that appear to be Sertoli cell only (Hum Pathol 2001;32:36)
Additional references
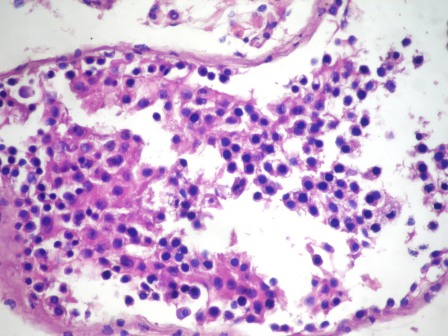
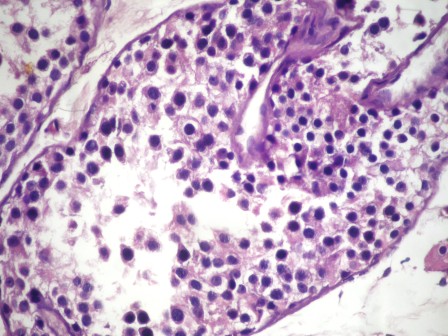
Maturation arrest
Definition / general
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Asmaa Gaber Abdou, M.D.
- Complete maturation arrest: germ cell maturity ceases at a specific point frequently at primary spermatocyte level; sperm counts usually zero
- Incomplete maturation arrest: similar to complete but a few late spermatids are present in a few seminiferous tubules, some prefer the term hypospermatogenesis instead of incomplete maturation arrest; patients are usually oligospermic (Arch Pathol Lab Med 2010;134:1197)
- Same etiologies as hypospermatogenesis (diabetes mellitus, toxins, excess heat, varicocele, hypothyroidism, irradiation); also postpubertal gonadotropin deficiency, alkylating agents
- Nonzero sperm counts indicate late spermatids are present somewhere in testis, although perhaps not in area biopsied
- Patients with early maturation arrest have a greater incidence of genetic anomalies and are more likely to have worse reproductive outcomes than are patients with late maturation arrest (Urology 2012;80:826)
Microscopic (histologic) description
- Numerous spermatogonia, few spermatocytes, no mature spermatozoa
- Sertoli cells prominent since reduced germ cells
- Tubules often contain degenerated cells with irregular dense nuclei
Microscopic (histologic) images
Contributed by Asmaa Gaber Abdou, M.D.