Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Thompson A, Zynger DL. Choriocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testischorio.html. Accessed November 29th, 2024.
Definition / general
- Choriocarcinoma is a malignant nonseminomatous germ cell tumor (GCT) composed of trophoblastic cells with associated hemorrhage
Essential features
- Tumor that arises from trophoblastic tissue and consists of syncytiotrophoblasts, cytotrophoblasts and intermediate trophoblasts with associated hemorrhage
- Increased serum beta hCG
- Early hematogenous metastasis
- Mixed germ cell tumor with choriocarcinoma component has better outcome than pure choriocarcinoma
Terminology
- Nonseminomatous germ cell tumor (NSGCT)
- Trophoblastic malignant teratoma, chorionepithelioma (not recommended)
ICD coding
- ICD-O:
- ICD-10:
- C62.90 - malignant neoplasm of unspecified testis, unspecified whether descended or undescended
- ICD-11:
Epidemiology
- Testicular GCT are the most common solid tumors in young men (Expert Rev Anticancer Ther 2020;20:75)
- 95% of testicular tumors are GCT
- Testicular GCT with choriocarcinoma affects men aged 20 - 39, with a median age of 29 (Am J Surg Pathol 2014;38:111)
- 7 - 8% of testicular GCT have choriocarcinoma as a component, usually admixed with other GCT types (J Urol 2014;192:934)
- 0.9% of testicular mixed GCT have choriocarcinoma as a main component (Am J Surg Pathol 2014;38:111)
- 0.2 - 0.6% of testicular GCT are pure choriocarcinoma (J Urol 2014;192:934, Am J Surg Pathol 2014;38:111)
Sites
- Testicular parenchyma
- Metastases to lung, brain, liver, retroperitoneum, gastrointestinal tract, lymph node, bone (Int J Health Sci (Qassim) 2017;11:81, World Neurosurg 2017;106:536, Cureus 2018;10:e3083, J Pak Med Assoc 2013;63:1544, Curr Oncol Rep 2015;17:2)
Pathophysiology
- Unknown
Etiology
- No specific known cause
- Precursor lesion: germ cell neoplasia in situ (GCNIS)
- Testicular GCT risk factors include cryptorchidism and a personal or family history of testicular cancer (Am Fam Physician 2018;97:261)
- Testicular GCT are likely the result of genetic and environmental factors during fetal development and subsequent changes in premalignant germ cells following puberty (Expert Rev Anticancer Ther 2020;20:75)
Clinical features
- Presentation with elevated serum beta hCG, scrotal mass with or without pain, possible hyperthyroidism and gynecomastia (Curr Oncol Rep 2015;17:2, Am Fam Physician 2018;97:261)
- Can present with hemoptysis, seizures, confusion (Radiol Case Rep 2021;16:923, Curr Oncol Rep 2015;17:2)
- Patients with pure or predominant choriocarcinoma have distant metastasis at presentation (100% in 1 study), usually to the lungs (67%), liver (60%) and less frequently brain (20%) (Am J Surg Pathol 2014;38:111)
- Cases with minimal choriocarcinoma component (≤ 5%) have regional lymph node metastases in 10% and distant metastases in 7% at presentation (Am J Surg Pathol 2018;42:1113)
- Choriocarcinoma syndrome is a rare, life threatening complication in patients with substantially increased serum beta hCG (usually > 50,000 IU/L) due to high choriocarcinoma tumor burden at metastatic sites, often following chemotherapy induction, yielding fatal bleeding and pulmonary hemorrhage leading to acute respiratory failure (Cureus 2021;13:e14286)
Diagnosis
- Initial scrotal ultrasonography followed by orchiectomy histopathology (Am Fam Physician 2018;97:261)
- CT, MRI, Xray for staging
Laboratory
- Higher levels of serum beta hCG indicate heavier choriocarcinoma burden at presentation (Case Rep Oncol Med 2019;2019:4092941):
- Pure choriocarcinoma: 65,000 - 899,000 IU/L (Am J Surg Pathol 2014;38:111)
- Predominant choriocarcinoma: 55,000 - 666,000 IU/L (Am J Surg Pathol 2014;38:111)
- Pure or predominant choriocarcinoma: median 199,000 IU/L (Am J Surg Pathol 2014;38:111)
- Minimal choriocarcinoma component (≤ 5%): 0.1 - 60,715 IU/L (median 485 IU/L) (Am J Surg Pathol 2018;42:1113)
- Serum beta hCG in circulation reflects residual tumor (Curr Oncol Rep 2015;17:2)
Radiology description
- Ultrasonography of testicle can reach 100% sensitivity in combination with physical exam for testicular tumors (AJR Am J Roentgenol 2013;200:1215)
- Choriocarcinoma appears as hypoechoic lesion on ultrasound (Radiol Case Rep 2021;16:923)
- CT, MRI, Xray to identify metastasis and for staging
- Metastatic choriocarcinoma forms hemorrhagic masses and in lungs has cannonball appearance on Xray and CT (Radiol Case Rep 2021;16:923)
Radiology images
Prognostic factors
- Patients with beta hCG > 50,000 IU/L have a 5 year survival of 48% (Int J Health Sci (Qassim) 2017;11:81)
- Pure or predominant choriocarcinoma has a median survival of 13 months (Lancet 2006;367:754)
- 79% of patients with pure or predominant choriocarcinoma (> 50%) treated with orchiectomy and chemotherapy died within 3 years (Am J Surg Pathol 1993;17:1075)
- Minimal choriocarcinoma component (≤ 5%) does not seem to negatively impact prognosis (Am J Surg Pathol 2014;38:111)
Case reports
- 17 year old boy with thyroid storm (Eur J Case Rep Intern Med 2020;7:001754)
- 18 year old man with metastases to skin, lungs, retroperitoneum (Medicine (Baltimore) 2018;97:e10736)
- 28 year old man with choriocarcinoma syndrome (Cureus 2021;13:e18681)
- 30 year old man with upper gastrointestinal bleed (Cureus 2019;11:e5243)
- 37 year old man with metastases to skin, brain, gastrointestinal tract (Cureus 2018;10:e3083)
Treatment
- Unlike other testicular GCT, chemotherapy may be indicated prior to a tissue diagnosis in patients with radiologic findings and a serum hCG > 50,000 mIU/mL (Curr Oncol Rep 2015;17:2)
- Orchiectomy is primary treatment for nonmetastatic tumors
- Retroperitoneal lymph node dissection or chemotherapy for pT2 or higher
- Chemotherapy for pN2 - 3
- Treatment regimens:
- Bleomycin, etoposide, cisplatin (BEP) (Curr Oncol Rep 2015;17:2, World Neurosurg 2017;106:536)
- Bleomycin might be held until after induction therapy to avoid pulmonary fibrosis (Front Endocrinol (Lausanne) 2019;10:218)
- 4 cycles with hCG monitoring is often needed (Curr Oncol Rep 2015;17:2)
- Delay can be fatal (Curr Oncol Rep 2015;17:2)
- Goal of treatment is tumor marker normalization
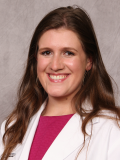
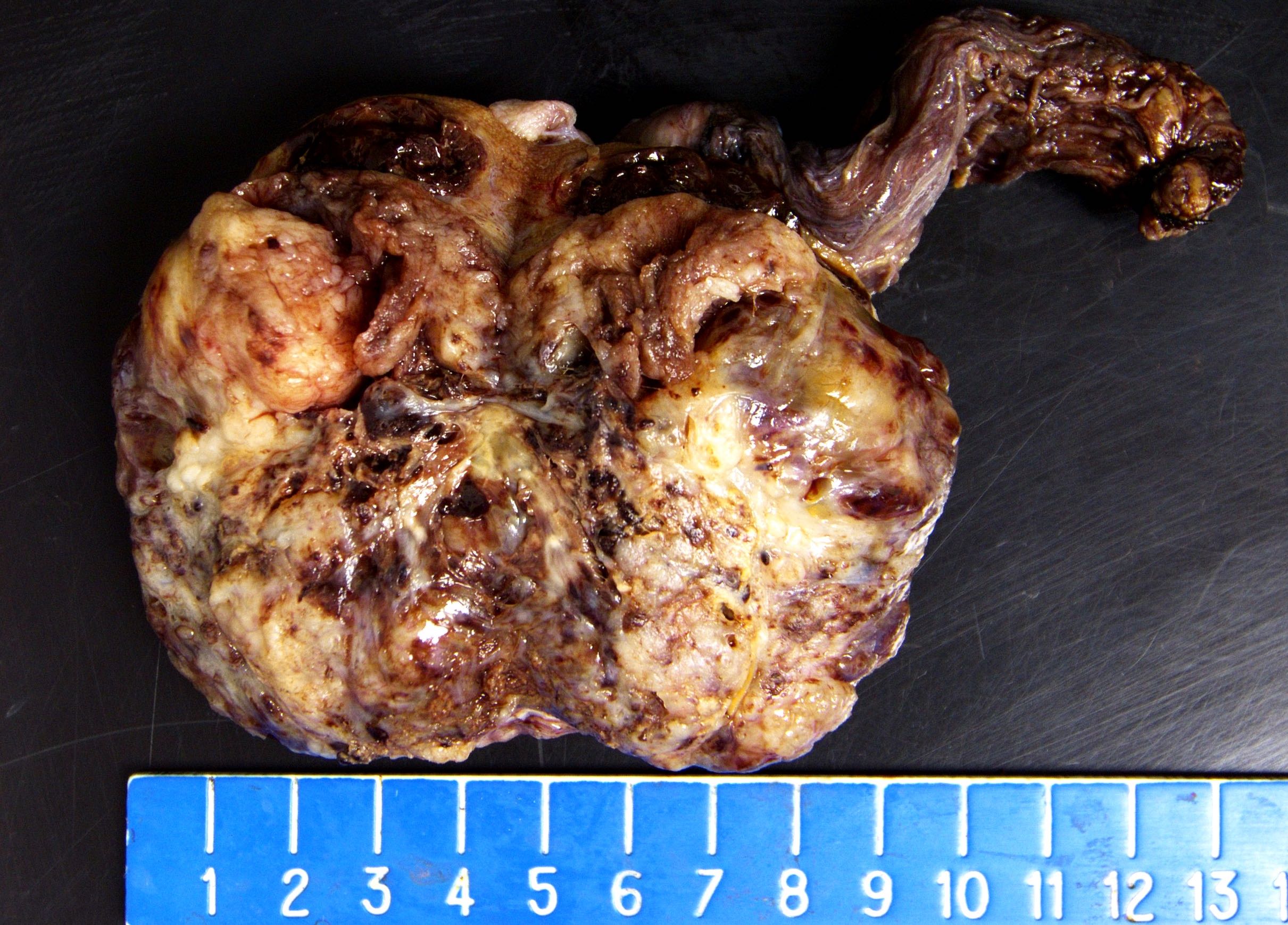
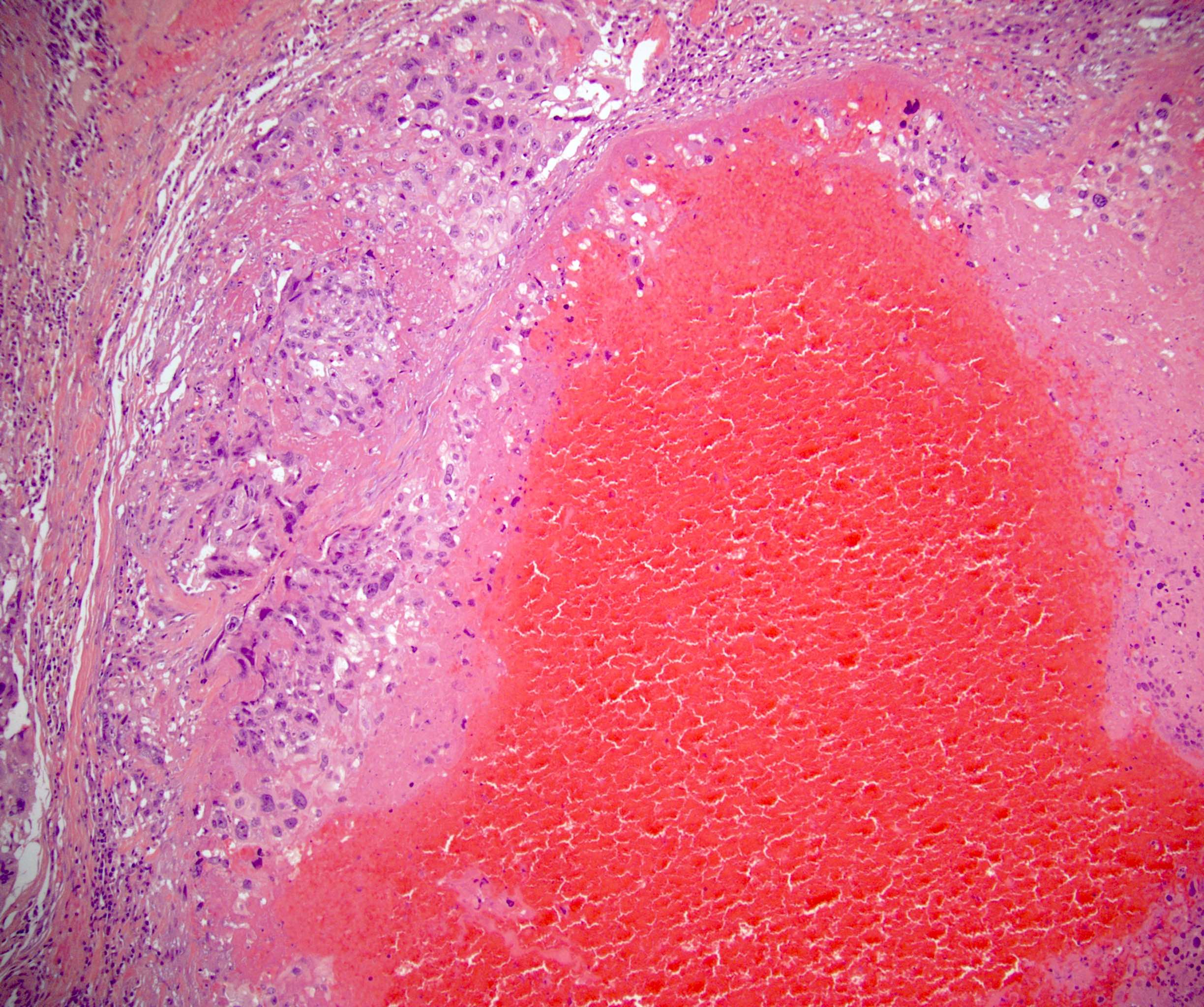
Gross description
- Central hemorrhage and necrosis, surrounded by viable tumor
- Tumor size has a wide range:
- Pure or predominant choriocarcinoma: 1.5 - 10 cm, median 7 cm (Am J Surg Pathol 2014;38:111)
- Minimal choriocarcinoma component (≤ 5%): 1.1 - 8.0 cm, median 4.5 cm (Am J Surg Pathol 2018;42:1113)
Gross images
Frozen section description
- Intraoperative definitive diagnosis of the type of testicular GCT is not needed because it does not impact intraoperative management
- Determination of benign versus malignant testicular tumor for small masses via frozen section is highly accurate (Eur Urol 2003;44:458)
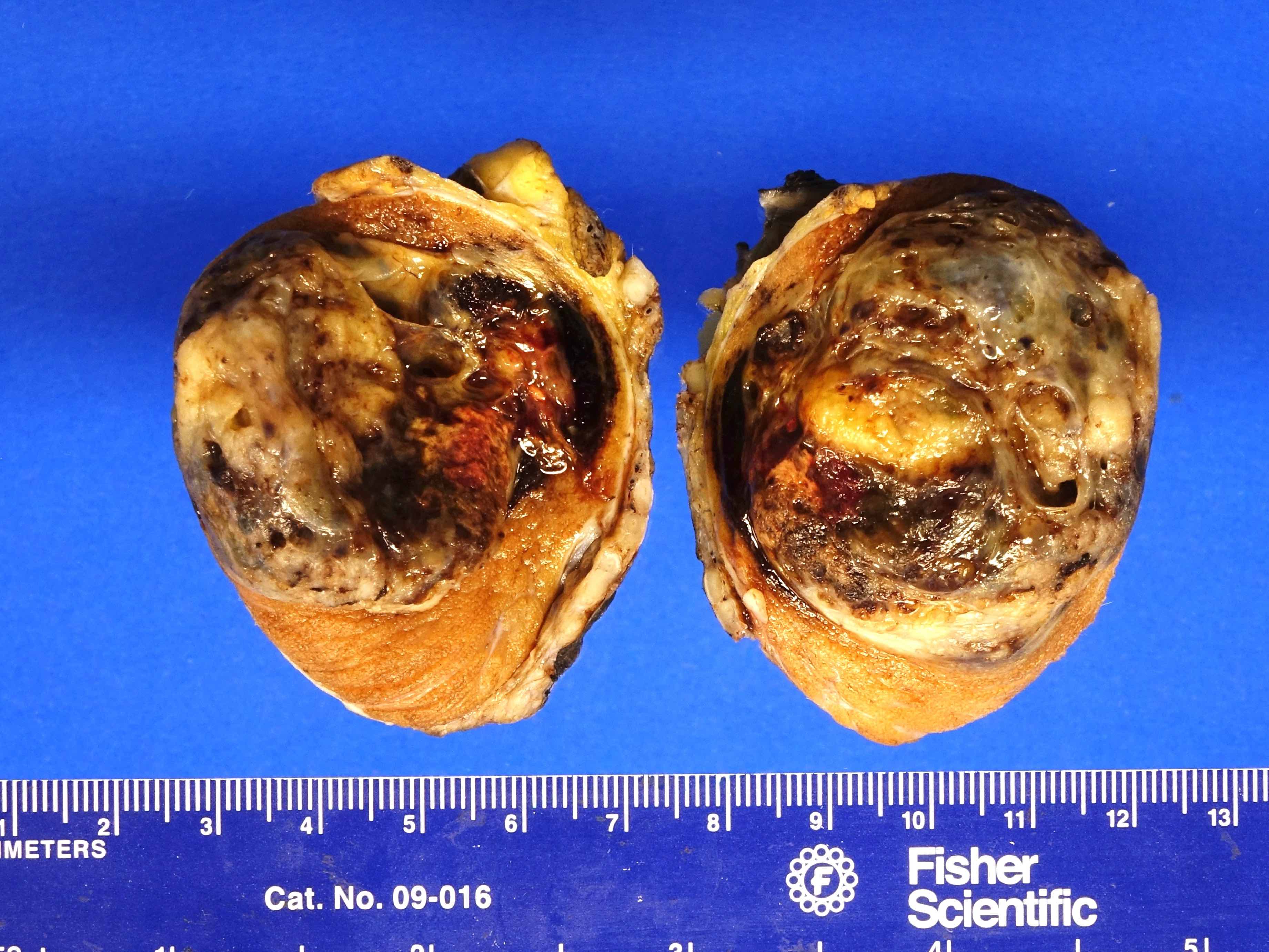
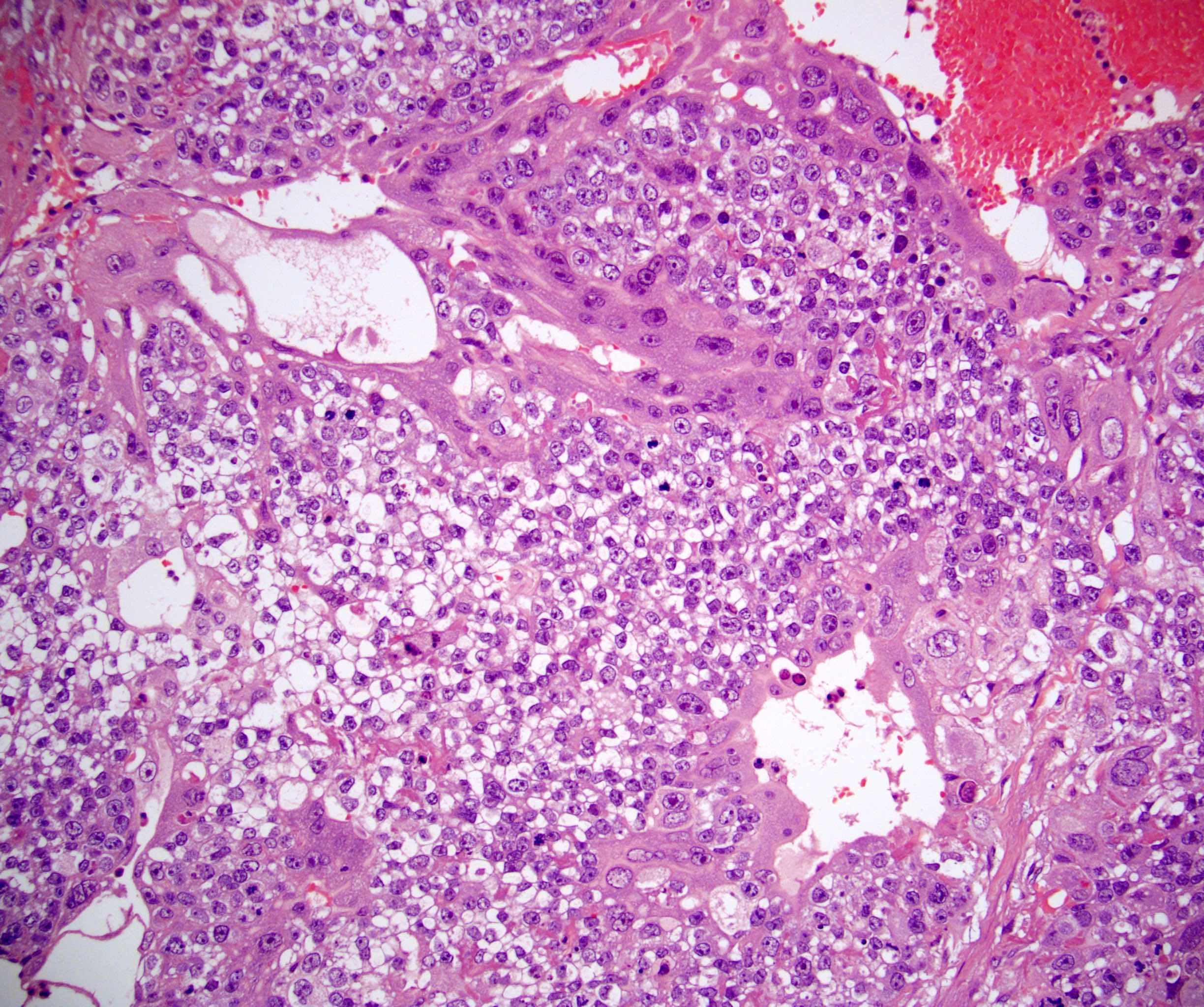
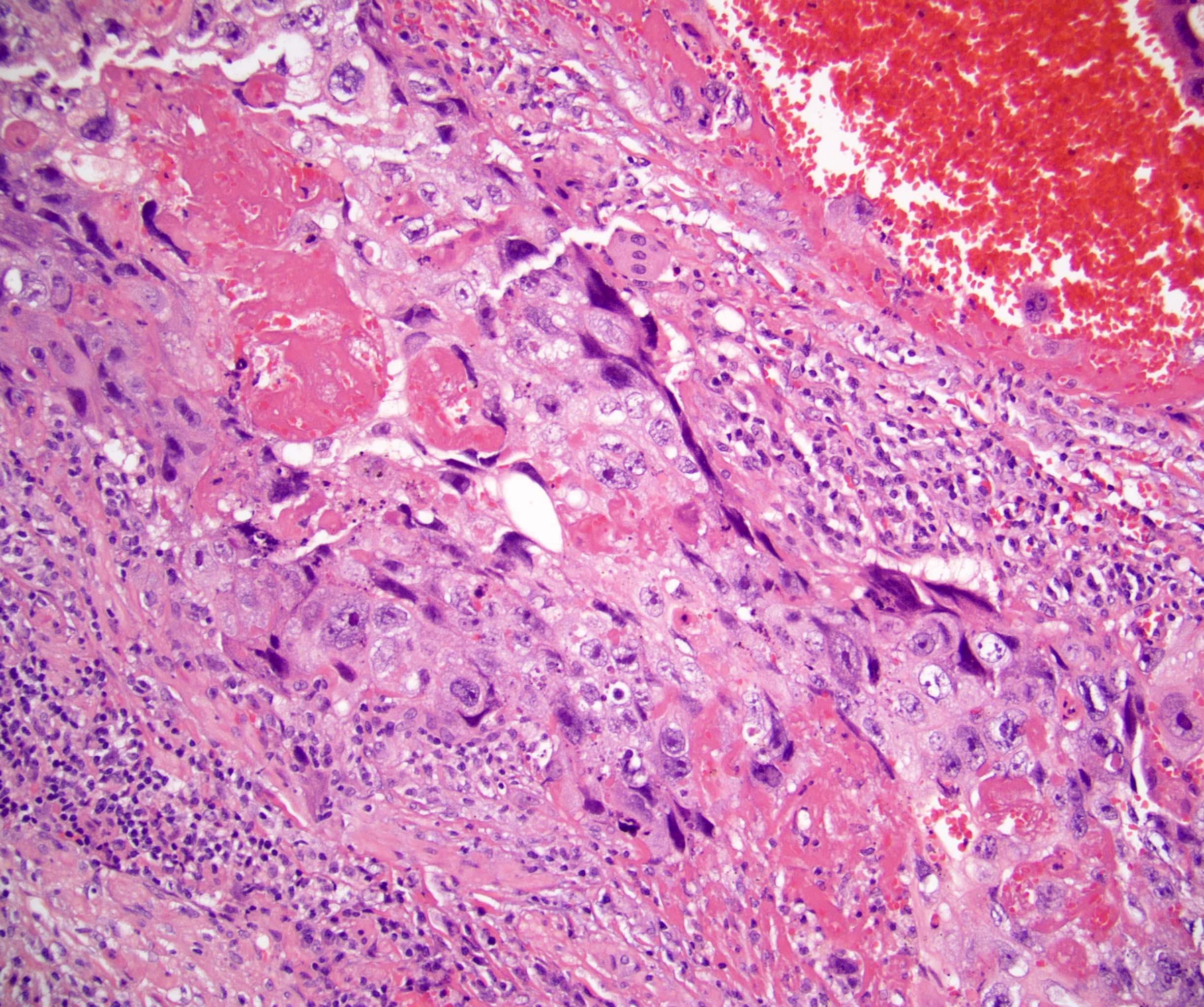
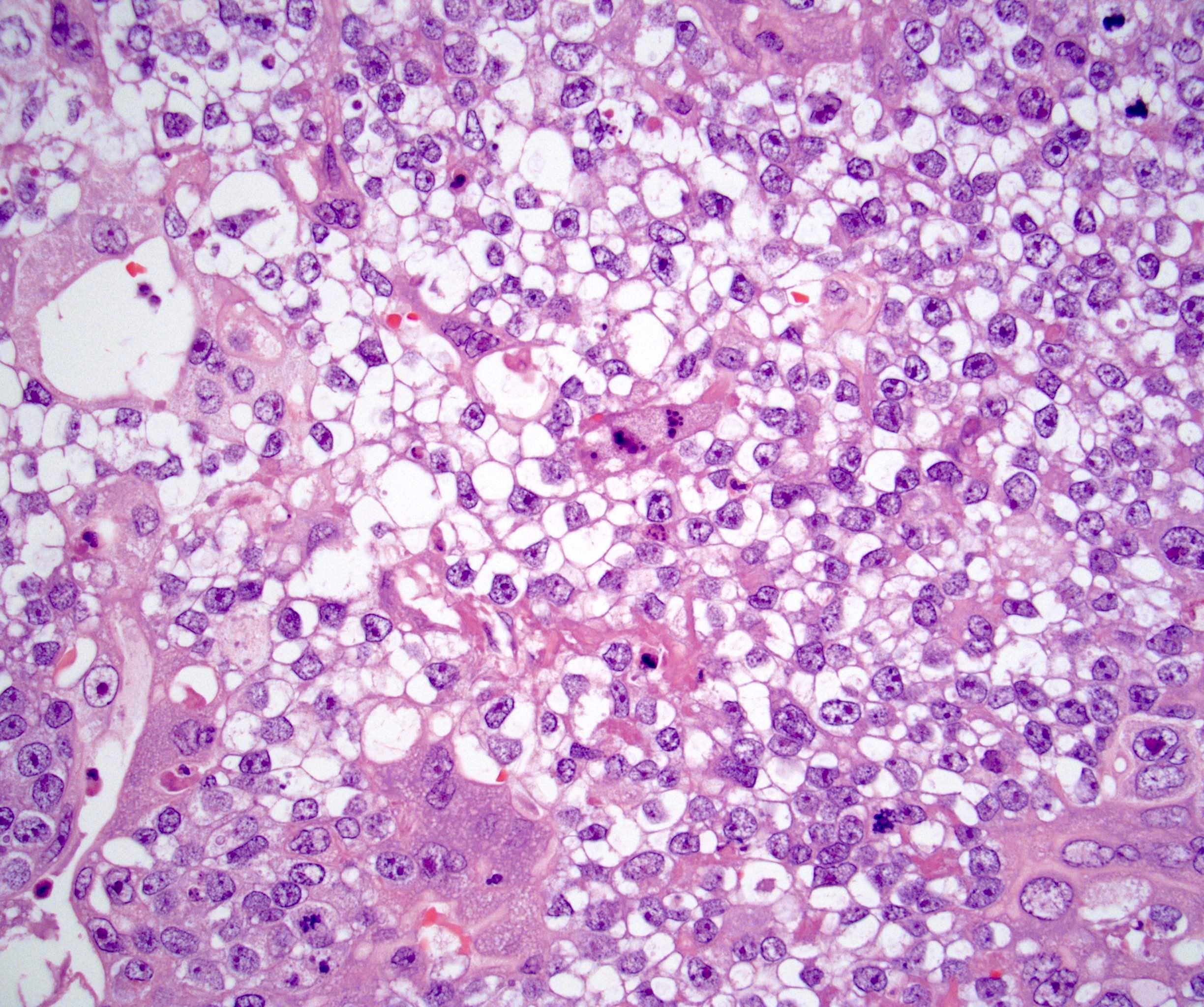
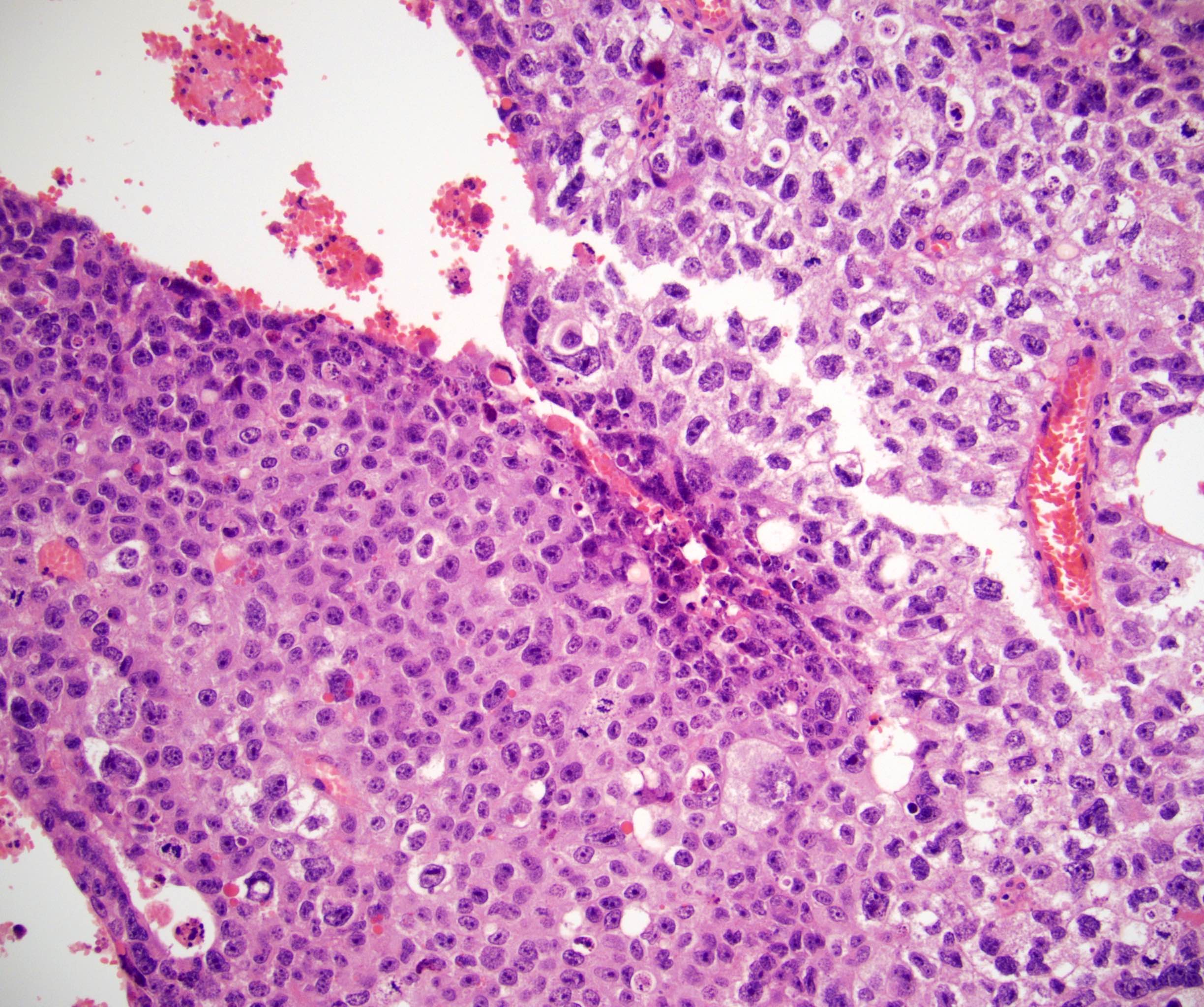
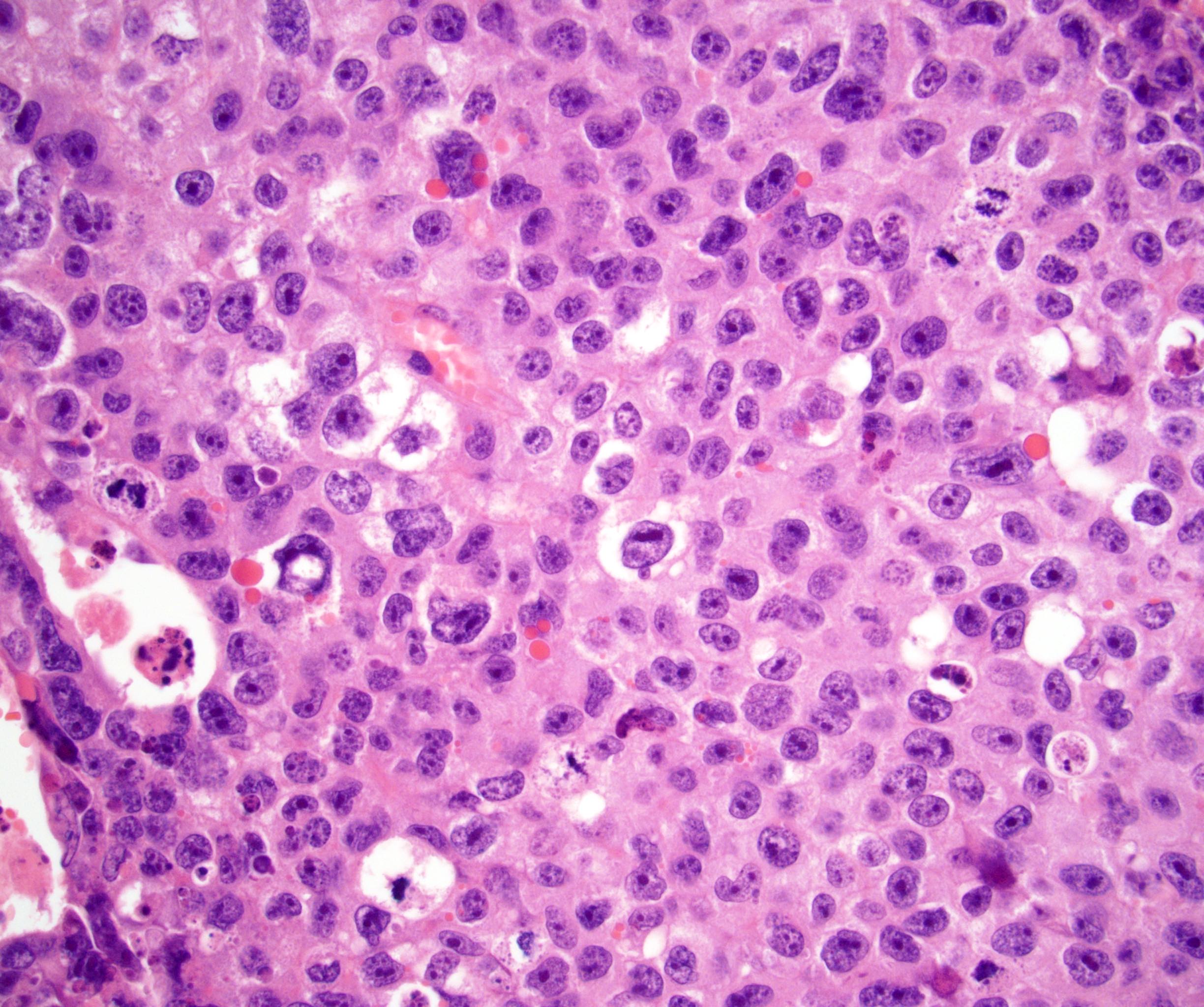
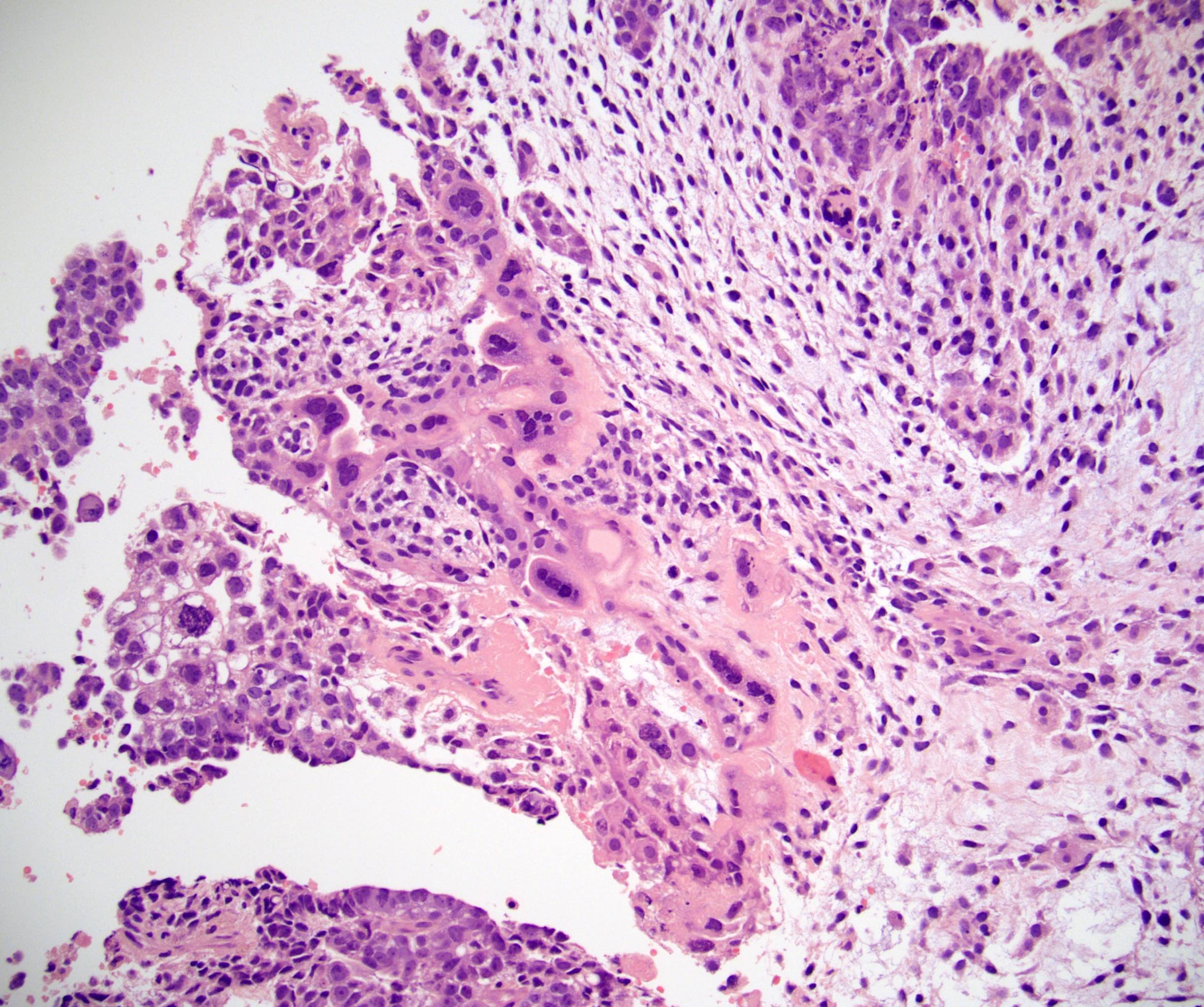
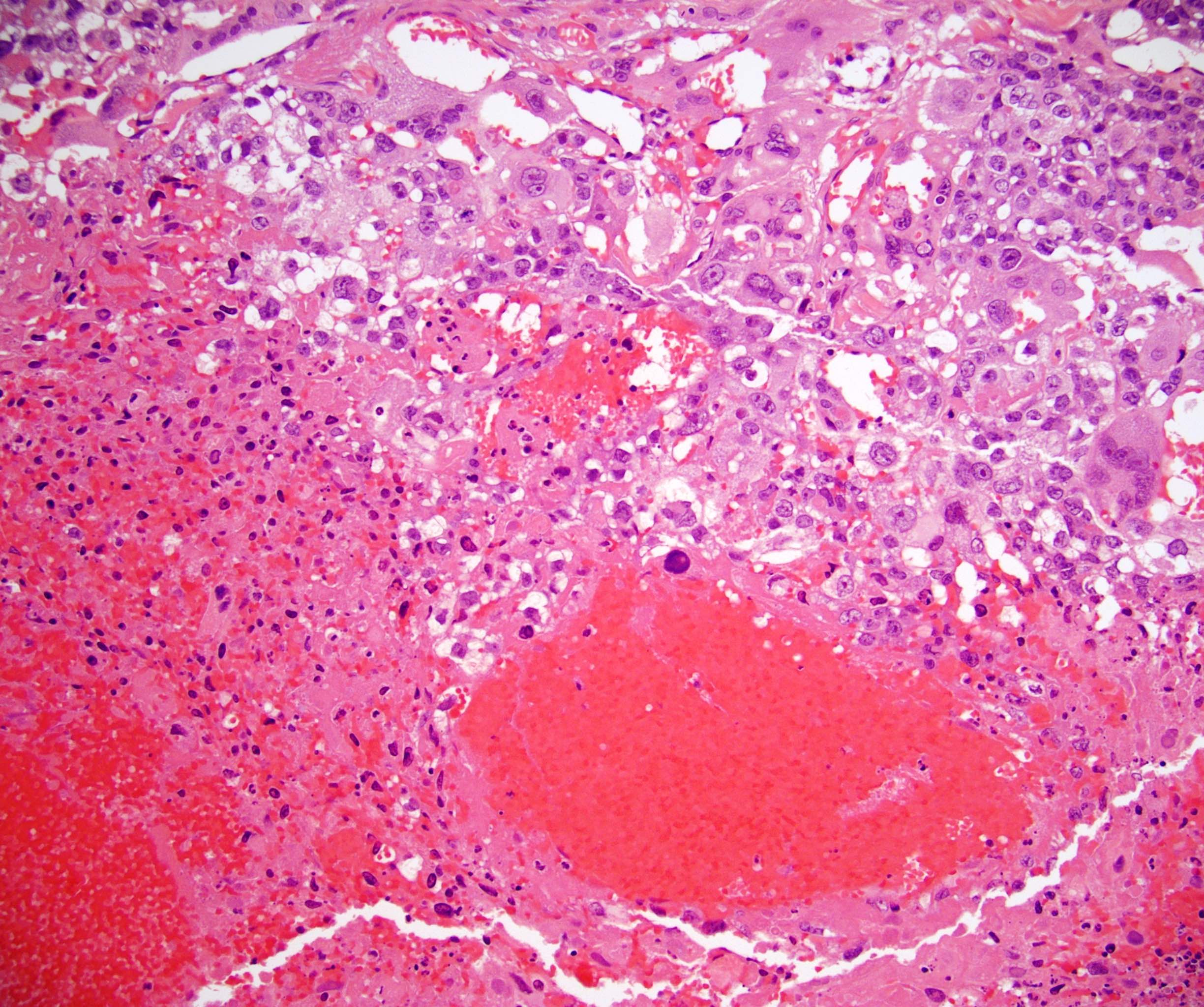
Microscopic (histologic) description
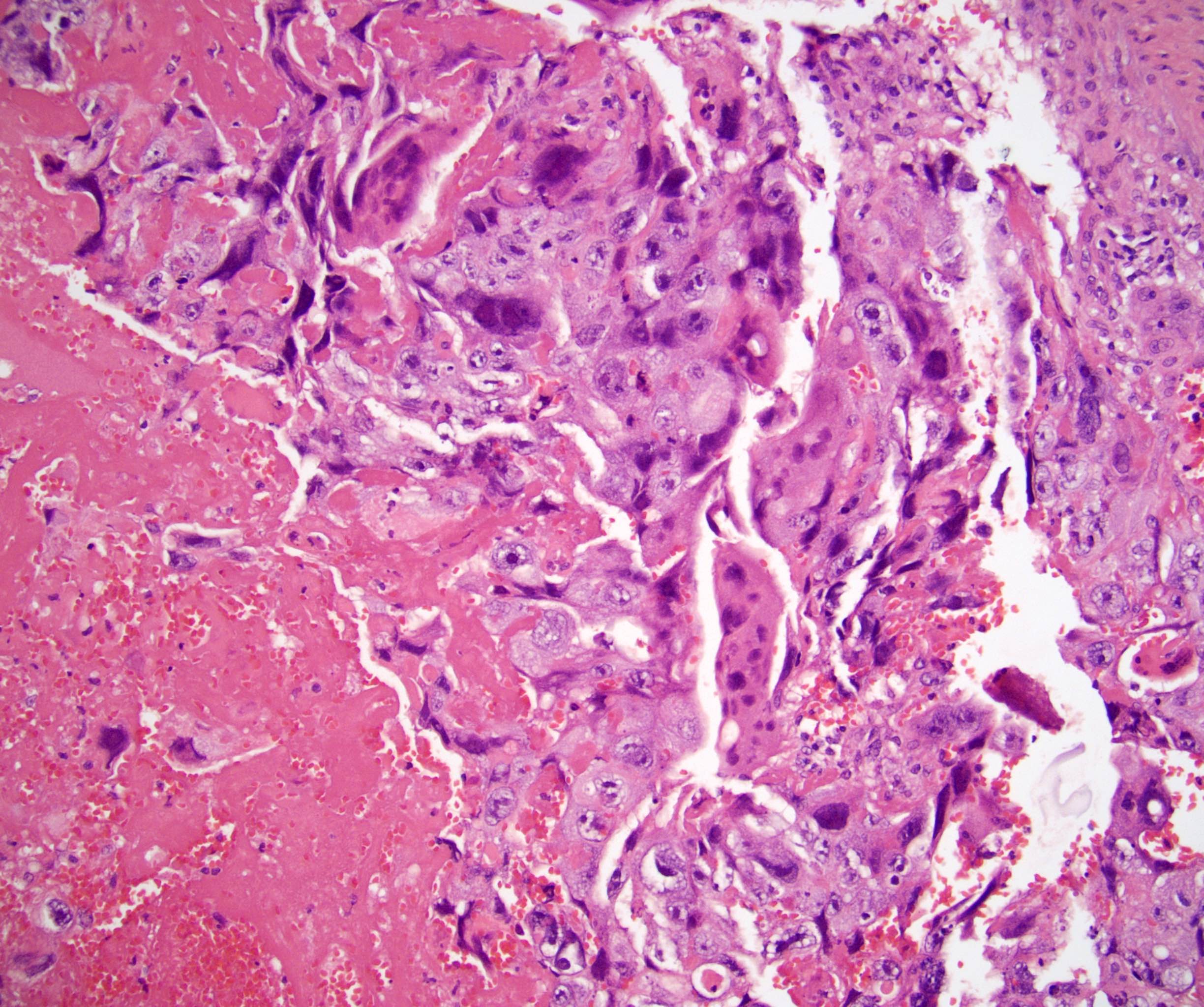
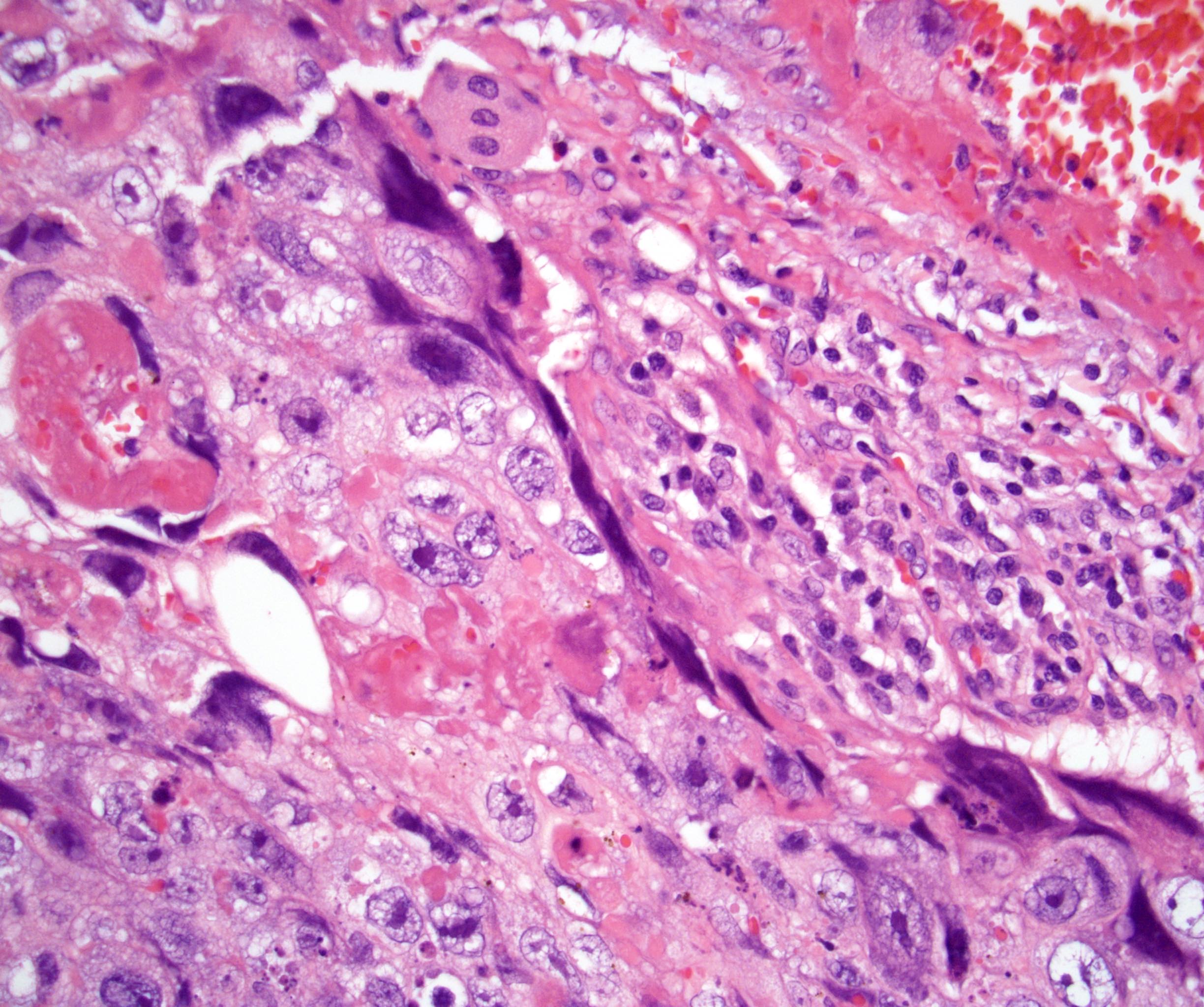
- Solid nests and sheets of syncytial cells (syncytiotrophoblasts) and mononucleated trophoblasts (cytotrophoblasts and intermediate trophoblasts)
- Syncytiotrophoblasts:
- Large cells
- Abundant, dense, eosinophilic cytoplasm
- Indistinct cell border
- Multinucleated
- Pleomorphic, hyperchromatic nuclei which can have a degenerated, smudged appearance
- Grow over mononucleated cells and can form a thin compressed rim or a thicker cap
- Mononucleated trophoblasts (cytotrophoblasts and intermediate trophoblasts):
- Medium sized cells
- Pale, eosinophilic cytoplasm
- Distinct cell border
- Mitotically active
- Hemorrhage, cyst formation and necrosis are common (Am J Surg Pathol 2014;38:111)
- Lymphovascular invasion is often present in tumors with pure or predominant choriocarcinoma (Am J Surg Pathol 2014;38:111)
- Germ cell neoplasia in situ may be present
- Remaining nonneoplastic testicular parenchyma may show findings seen in other germ cell tumors, including atrophy, maturation arrest, Leydig cell hyperplasia, microlithiasis, angiopathy, Sertoli cell only tubules and Sertoli cell nodules (Am J Surg Pathol 2006;30:1260)
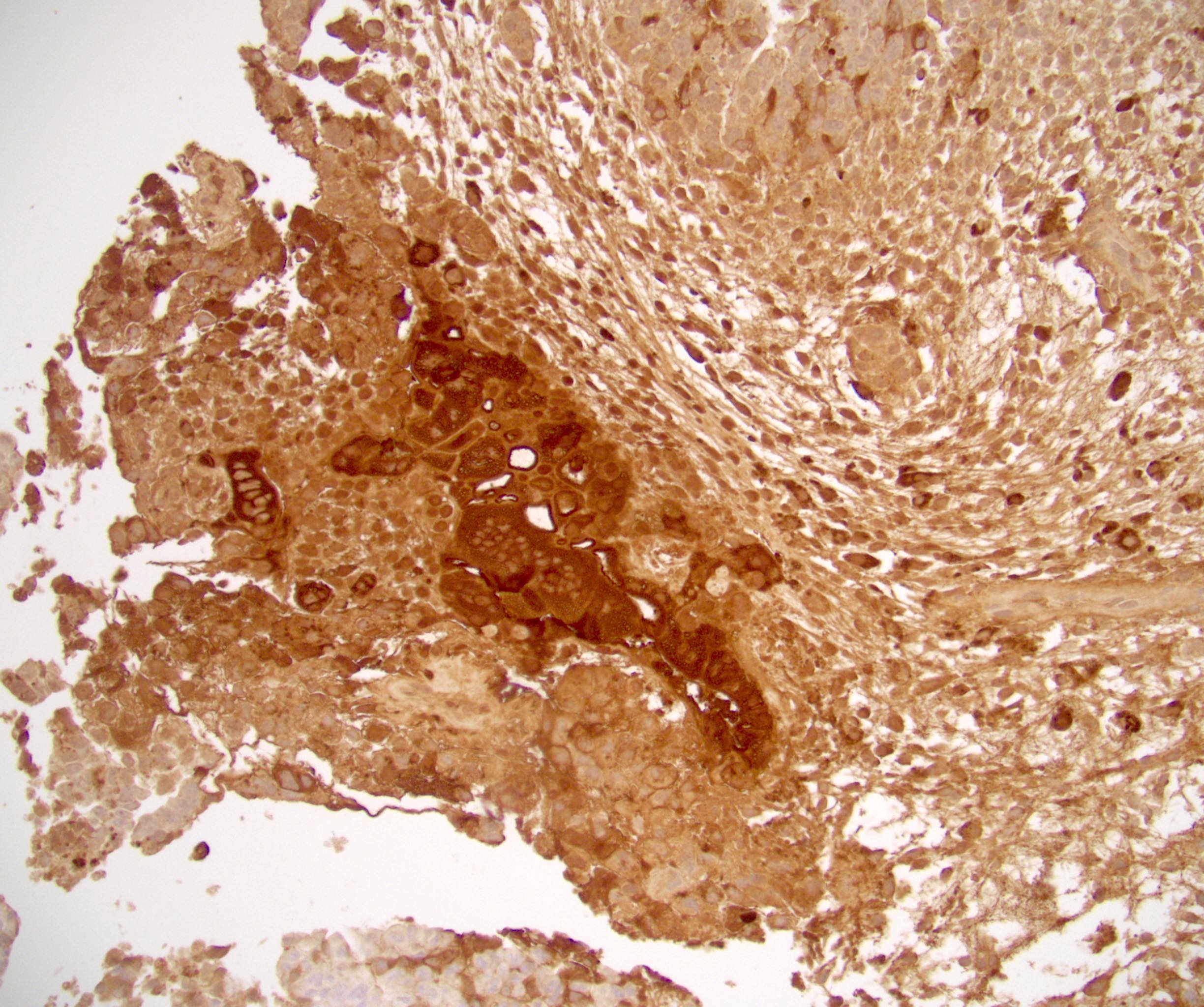
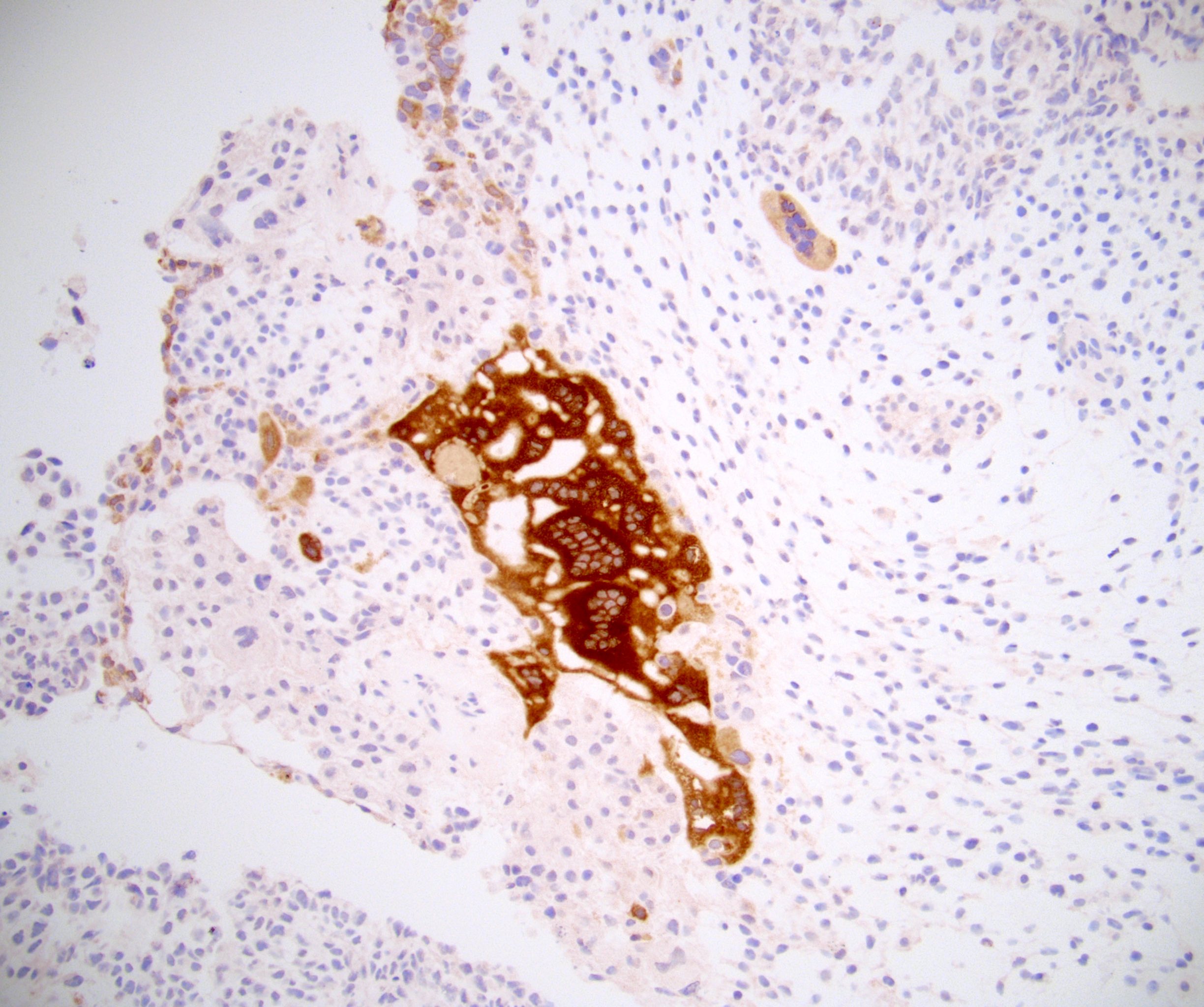
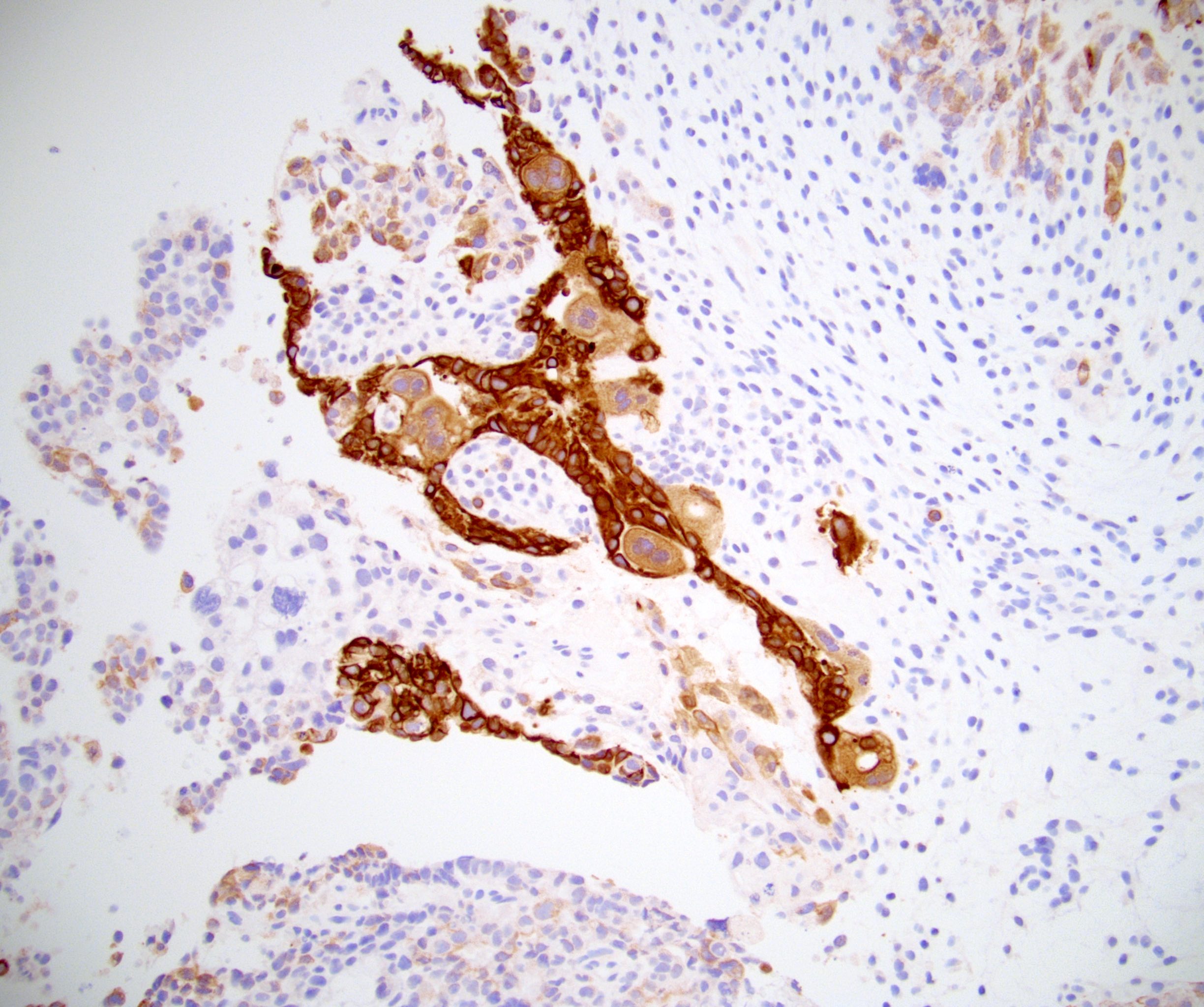
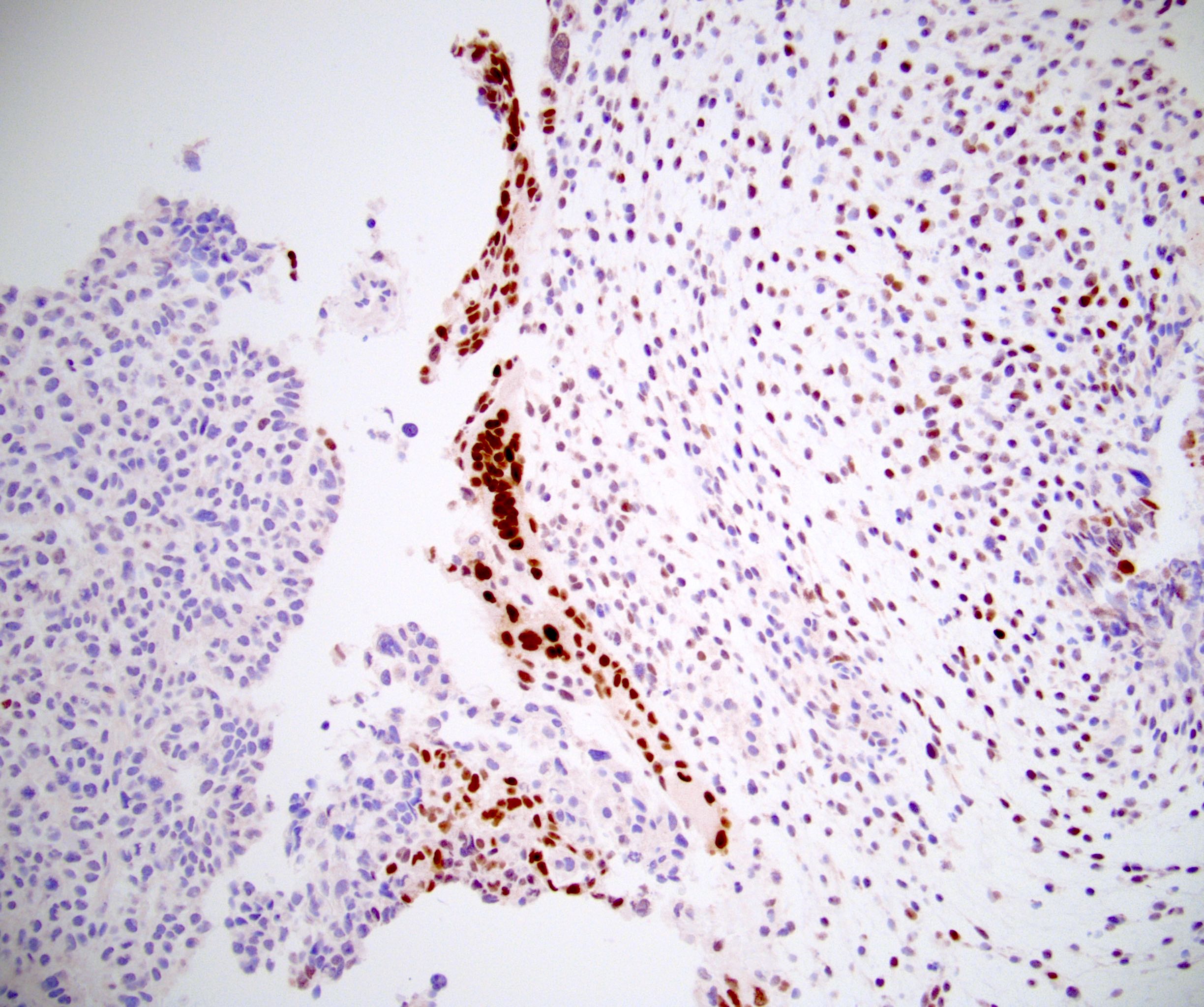
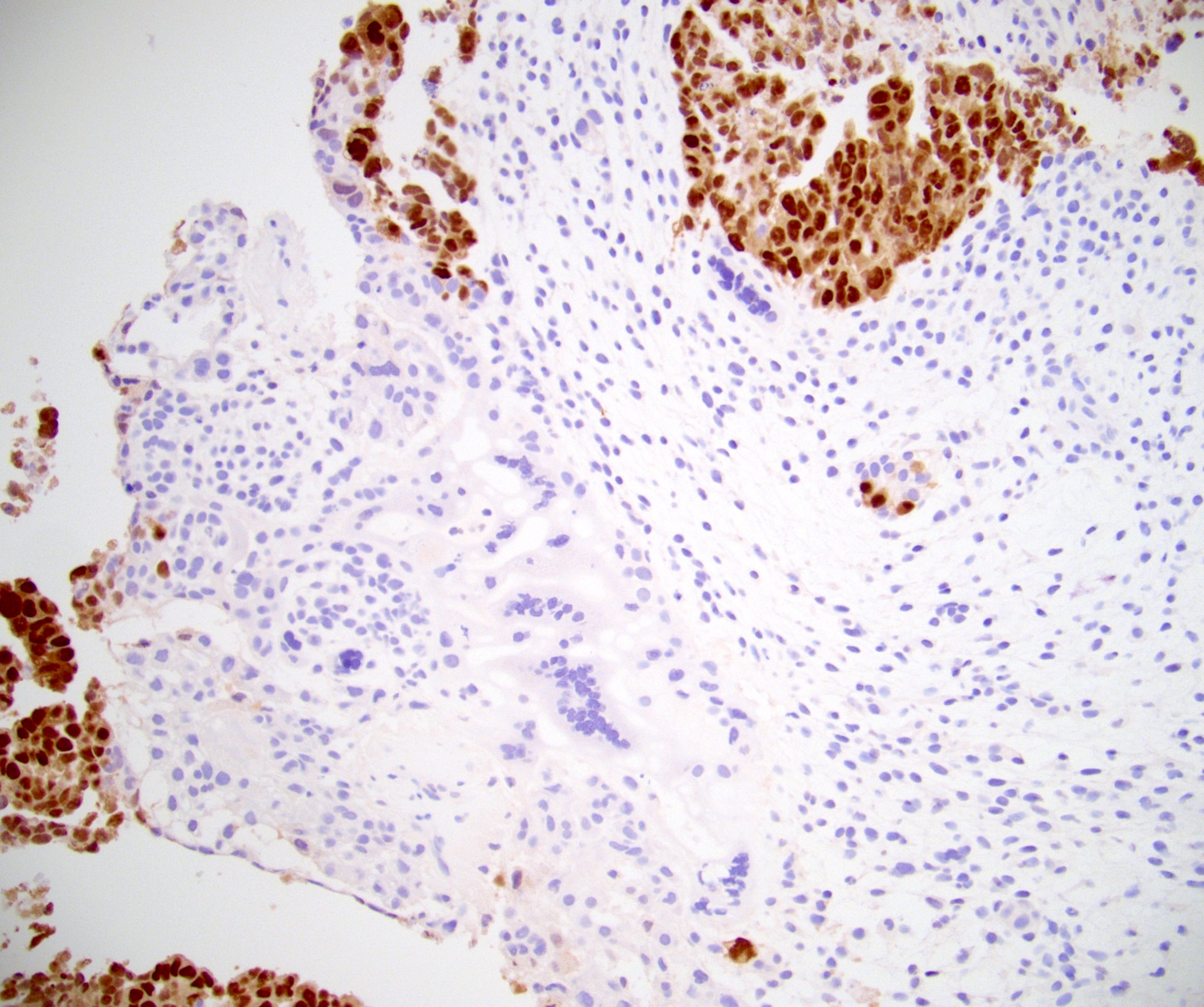
Microscopic (histologic) images
Cytology description
- Dual cell population composed of mononucleated trophoblasts and syncytiotrophoblasts (Ann Saudi Med 1997;17:432)
- Mononucleated trophoblasts:
- Intermediate size, round
- Single round nuclei, coarse chromatin and visible single nucleoli
- Clear to slightly basophilic cytoplasm with few small vacuoles (Ann Saudi Med 1997;17:432)
- Syncytiotrophoblasts:
- Large cells
- Multiple, pleomorphic nuclei
- Abundant cytoplasm with variable numbers of small vacuoles (Ann Saudi Med 1997;17:432)
- Background of necrosis and hemorrhage which may limit cellularity of specimen (Ann Saudi Med 1997;17:432)
Positive stains
- AE1 / AE3
- hCG: 96% (caveat that tumors containing choriocarcinoma can have expression that diffuses into all GCT types, requiring careful interpretation and use of more specific markers) (Hum Pathol 2019;84:254)
- GATA3: 100% (syncytiotrophoblasts, mononucleated trophoblasts) (Hum Pathol 2016;48:18)
- Glypican 3: 30 - 100% (strong in syncytiotrophoblasts, mononucleated trophoblasts) (Am J Surg Pathol 2020;44:e66, Am J Surg Pathol 2006;30:1570, Mod Pathol 2020;33:2354, Urol Ann 2022;14:21)
- Syncytiotrophoblasts:
- CK7: 100% (Hum Pathol 2019;84:254)
- Inhibin: 89% (Hum Pathol 2019;84:254)
- HPL: 100% (Am J Surg Pathol 2014;38:111)
- Mononucleated trophoblasts:
- SALL4: 100%, but variable percentage of cells (Am J Surg Pathol 2009;33:1065)
- p63 (cytotrophoblasts): 85 - 100% (Hum Pathol 2019;84:254, Am J Surg Pathol 2014;38:111)
Negative stains
- OCT 3/4: 0% (Am J Surg Pathol 2020;44:e66, Urol Ann 2022;14:21)
- CD30: 0% (Urol Ann 2022;14:21)
- CD117 / KIT: 0% (Urol Ann 2022;14:21)
- HNF-1B: 13% (Mod Pathol 2020;33:2354)
- CDX2: 25% (Hum Pathol 2016;48:18)
- AFP: 25% (Mod Pathol 2020;33:2354)
Molecular / cytogenetics description
- 12p abnormalities are found in testicular GCT (Am J Surg Pathol 2020;44:e66, Genes Chromosomes Cancer 1990;1:289)
Sample pathology report
- Right testis, radical orchiectomy:
- Mixed germ cell tumor, teratoma (35%), seminoma (20%), embryonal carcinoma (20%), yolk sac tumor (20%) and choriocarcinoma (5%) types (see synoptic report)
Differential diagnosis
- Embryonal carcinoma:
- Seminoma:
- Patients tend to be 10 years older at diagnosis (Andrology 2015;3:4)
- Expansile nodules separated by fibrous bands containing lymphocytes
- Monotonous, smaller cells with distinct cell borders throughout
- Can have scattered, occasional clusters of syncytiotrophoblasts
- Usually lacks hemorrhage and necrosis (Am J Surg Pathol 2014;38:111)
- Positive OCT 3/4, CD117 / KIT, D2-40 / podoplanin; negative CK7, inhibin, beta hCG
- Squamous cell carcinoma somatic malignancy arising from teratoma:
- Nonchoriocarcinomatous trophoblastic tumors (cystic trophoblastic tumor, epithelioid trophoblastic tumor, placental site trophoblastic tumor):
- Very rare
- Usually seen posttreatment, particularly in metastatic sites
- Only mild serum beta hCG elevation (unless choriocarcinoma elsewhere)
- Lacks 2 different cell types
- Carcinoma of nongerm cell origin, especially squamous cell carcinoma:
Board review style question #1
Board review style answer #1
Board review style question #2
Board review style answer #2