Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zot P, Jimenez RE. Atrophy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testisatrophy.html. Accessed April 23rd, 2024.
Definition / general
- Testicular atrophy is a nonneoplastic process characterized by the disappearance of tubular or germinal epithelium and replacement with variable degrees of fibrosis
- Atrophy can present in the setting of testicular regression syndrome, postvasectomy, vascular accidents, testicular torsion, cryptorchidism, infectious process, external insults, iatrogenic and other settings
Essential features
- Etiology of testicular atrophy is varied; it can be seen in a variety of clinical pathologic settings
- Microscopic features include small tubules with few or no viable germ cells and a relative predominance of Leydig cells
- Potential risk for germ cell neoplasia in testicular regression syndrome with retained viable germ cells
Terminology
- Testicular atrophy
- Testicular regression syndrome
- Atrophy or disappearance of initially normal testis in fetal life
- Presence of spermatic cord is evidence of testis in early intrauterine life (J Clin Res Pediatr Endocrinol 2012;4:116)
- Bilateral anorchia (BMJ Case Rep 2018;2018:bcr2018225530)
- Vanishing testes (Front Pediatr 2022;10:834083)
- Postvasectomy atrophy
- End stage testis
Epidemiology
- Newborn / children for testicular regression syndrome
- Any age for other etiologies
Sites
- Testicle parenchyma
Pathophysiology
- In testicular regression syndrome, absence of a testis in an otherwise normal 46,XY male is usually unilateral and is assumed to be a consequence of intrauterine or perinatal torsion or infarction (J Clin Res Pediatr Endocrinol 2012;4:116)
- Hypothalamic - pituitary - gonadal axis dysregulation, leading to reduced steroidogenesis and spermatogenesis (Reprod Sci 2021;28:2735)
- Compromised vascular supply after a vascular accident or testicular torsion, leading to atrophy
Etiology
- Vascular accident, testicular torsion, thrombosis (Best Pract Res Clin Endocrinol Metab 2022;36:101619)
- Trauma
- Cryptorchidism
- Genetic abnormalities, such as microdeletion of Y chromosome, persistence of Müllerian duct structures (J Clin Res Pediatr Endocrinol 2012;4:116)
- Filariasis and other infectious etiologies (J Endourol Case Rep 2019;5:113)
- AIDS (Am J Clin Pathol 1990;93:196)
- Chemotherapy and radiation
- Vasectomy, outflow obstruction
- Hormonal imbalances (e.g., persistent FSH stimulation, elevated serum estrogen)
- Sequela of COVID-19 infection (Reprod Sci 2021;28:2735)
Clinical features
- Unilateral or bilateral nonpalpable testis
- Normal external genitalia
- Infertility
- Presence of micropenis in a subset of patients with testicular regression syndrome (J Clin Res Pediatr Endocrinol 2012;4:116)
- Variable degrees of sexual ambiguity in familial cases of testicular regression syndrome
Diagnosis
- Measurement of gonadotropin and testosterone levels, human chorionic gonadotropin stimulation test, measurement of anti-Müllerian hormone, inhibin B levels, INSL3 levels and karyotype analysis
- Scrotal and abdominal ultrasound
- Laparoscopic exploration to visualize blind ending spermatic vessels within the retroperitoneum, or visualization of spermatic vessels and vas deferens exiting a closed internal inguinal ring (J Clin Res Pediatr Endocrinol 2012;4:116)
Laboratory
- In bilateral testicular regression syndrome, testosterone, inhibin B and INSL3 are undetectable, gonadotropins are elevated and karyotype is 46,XY (Best Pract Res Clin Endocrinol Metab 2022;36:101619)
- Hypothalamic - pituitary - gonadal axis dysregulation causes impaired LH:FSH ratio and decreased testosterone
- Lower sperm concentration, lower total sperm count and motility
- Azoospermia
Radiology description
- Absence or decreased size of testicle in scrotum
Prognostic factors
- Potential risk for germ cell neoplasia in testicular regression syndrome with retained viable germ cells
Case reports
- Newborn boy with bilateral testicular torsion, resulting in testicular atrophy (Acta Medica (Hradec Kralove) 2017;60:120)
- 30 year old man with bilateral leiomyomas of the tunica albuginea, causing testicular atrophy (Int J Clin Exp Pathol 2015;8:9703)
- 40 year old man with filariasis (J Endourol Case Rep 2019;5:113)
- 42 year old man with bilateral anorchia (BMJ Case Rep 2018;2018:bcr2018225530)
Treatment
- Surgical removal of the testicular remnant may or may not be necessary (Front Pediatr 2022;10:834083)
- Procedure for removal of outflow obstruction, if fertility is desired
- Hormonal supplementation in cases of hypothalamic - pituitary - gonadal axis dysregulation
- Treatment of underlying infection
Gross description
- Spermatic cord with a small mass of firm, fibrotic tissue at one end as well as elements of the vas deferens, spermatic artery and venous plexuses (J Clin Res Pediatr Endocrinol 2012;4:116)
- Small, fibrotic testis
Gross images
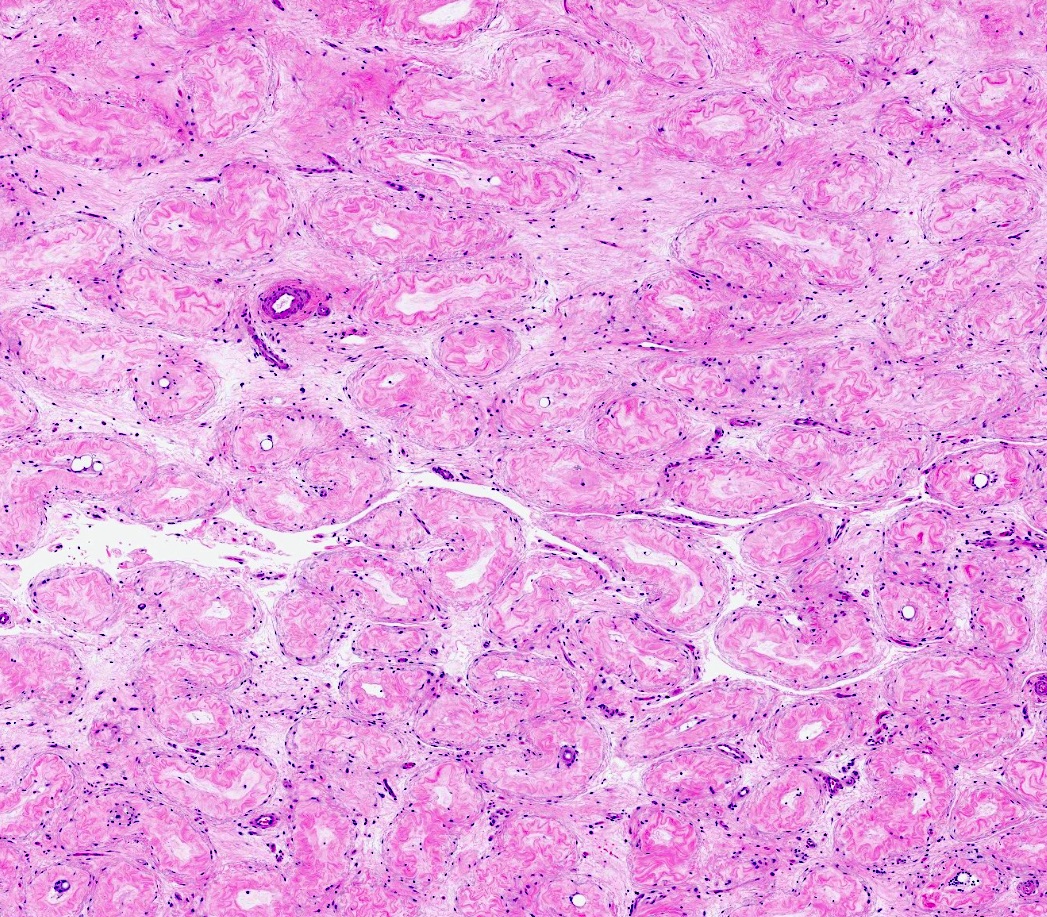
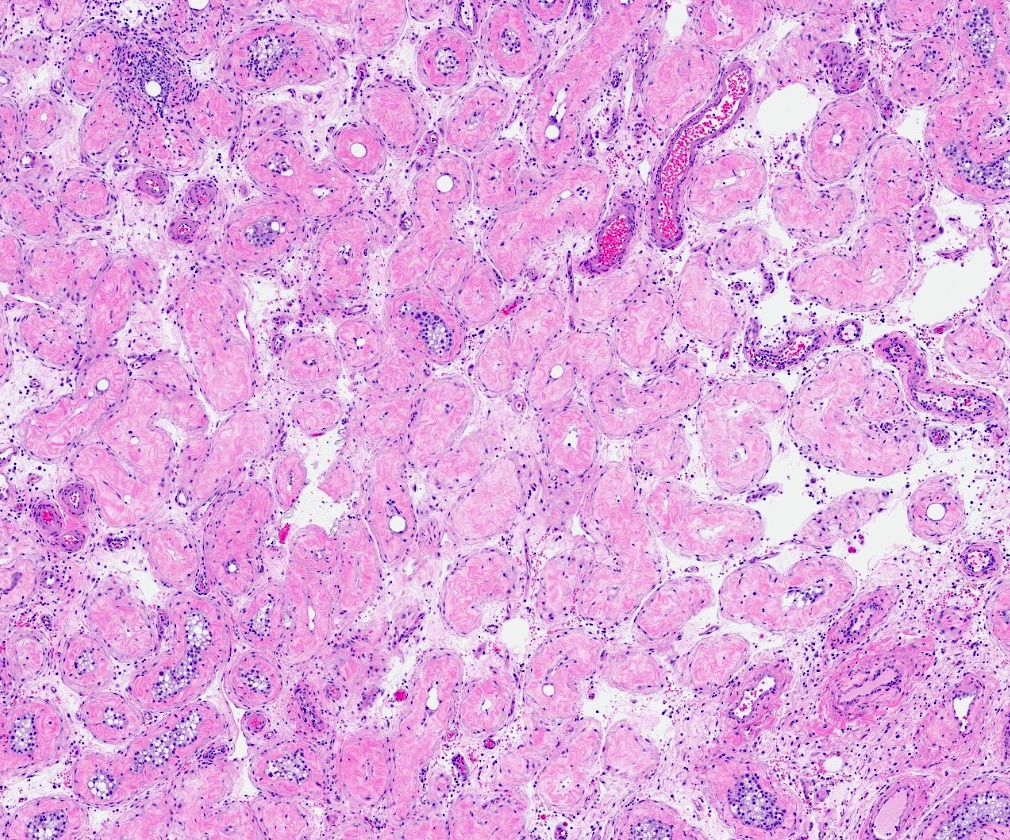
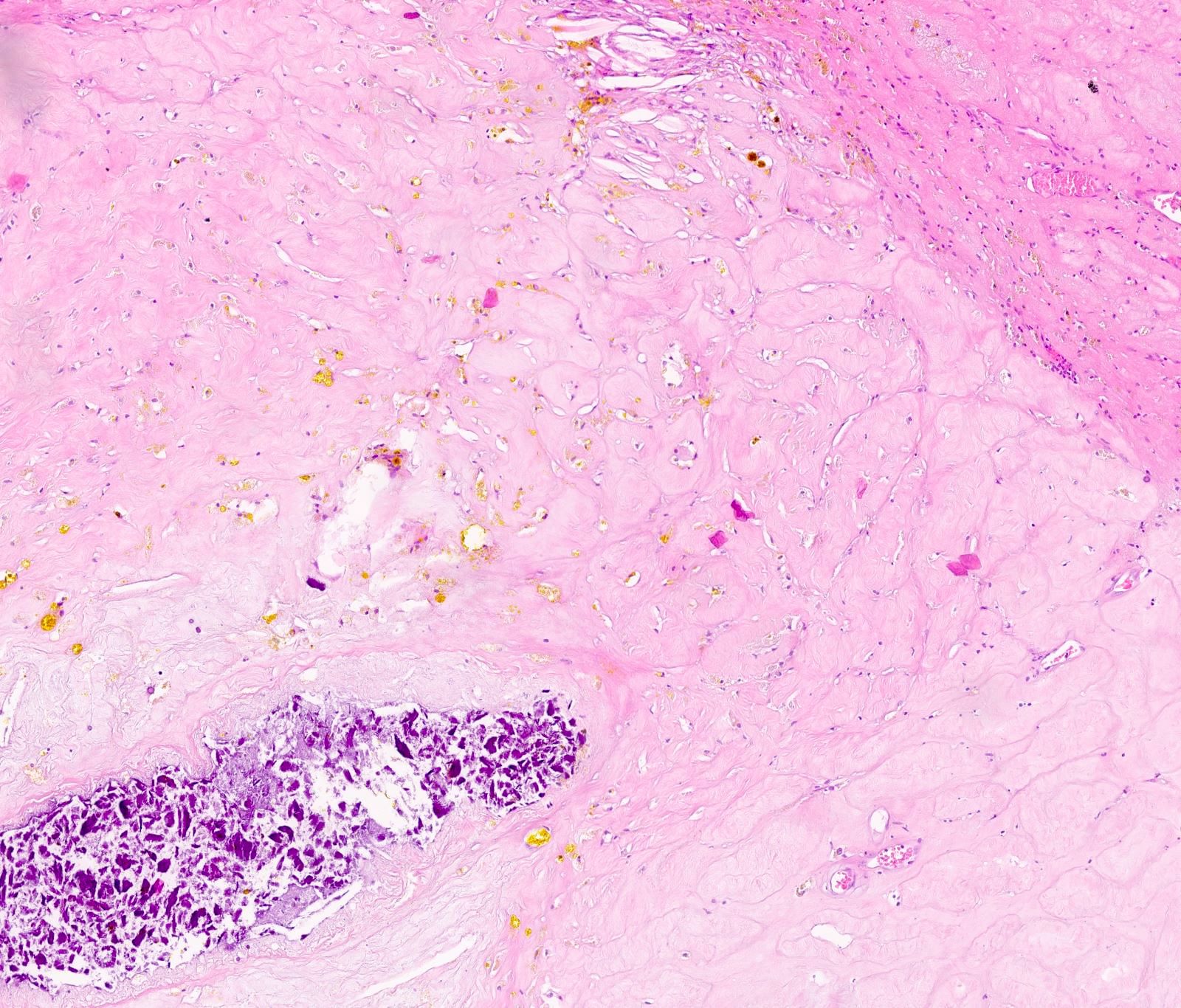
Microscopic (histologic) description
- Fibrovascular nodule with hemosiderin laden macrophages and dystrophic calcifications
- Rare presence of seminiferous tubules (6.3% of cases) and viable germ cells (2.1% of cases) in testicular remnants in testicular regression syndrome (Front Pediatr 2022;10:834083)
- Small tubules, thick basement membrane and few or no germ cells in postvasectomy specimens
- Sclerotic tubules
- Interstitial fibrosis
- Increased Leydig cells
Microscopic (histologic) images
Contributed by Patricija Zot, M.D., Rafael E. Jimenez, M.D., @ThatGlassTho on Twitter and @Andrew_Fltv on Twitter
Positive stains
Molecular / cytogenetics description
- DHX37 pathogenic variants are a new cause of an autosomal dominant form of 46,XY disorders of sex development, including gonadal dysgenesis and testicular regression syndrome (Genet Med 2020;22:150)
- Heterozygous partial loss of function mutations in SF1 may be associated with bilateral anorchia (vanishing testis syndrome) and micropenis in humans (Hum Reprod 2007;22:3255)
Sample pathology report
- Left testicle, orchiectomy:
- Testicular parenchyma with seminiferous tubule fibrosis
Differential diagnosis
- Regressed germ cell tumor:
- Leydig cell tumor:
- Unifocal
- Well circumscribed mass
- May have infiltrative borders in malignant variant
- Reinke crystals may be present
Board review style question #1
A 35 year old man presents for evaluation of infertility. After several laboratory and radiologic tests, a biopsy of a testicle was performed. The biopsy is shown in the image above. Presence or absence of which of the following would support a diagnosis of testicular atrophy?
- Absence of germ cell neoplasia in situ
- A nodule composed of cells containing Reinke crystals
- Presence of isochromosome 12p
- Presence of necrosis
Board review style answer #1
Board review style question #2
Parents of a 6 month old baby boy bring the child in for evaluation due to a concern for a nonpalpable testicle. On physical exam, there is only one testicle that has descended and is palpable in the scrotum. Imaging studies show no evidence of the second testicle in the abdomen or any other location; however, spermatic cord with a small nodule is present. The nodule is biopsied and shows benign fibrovascular tissue with no evidence of germ cells. What is the most likely diagnosis?
- Cryptorchidism
- Regressed mixed germ cell tumor
- Teratoma
- Testicular regression syndrome
Board review style answer #2