Table of Contents
Definition / general | Essential features | Terminology | Embryogenesis | Physiology | Diagrams / tables | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Electron microscopy images | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sule N. Histology-blood vessels. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuevascnormal.html. Accessed March 29th, 2025.
Definition / general
- The circulatory system facilitates the continuous movement of the body fluid including the blood and the lymph
- 2 main elements:
- Blood vascular system
- Arterial system
- Microcirculation: capillaries
- Venous system
- Lymph vascular system
- Blood vascular system
- Vasa vasorum: small blood vessels responsible for the supply of the walls of the big blood vessels
- Normal vessels contain endothelial cells facing lumen and pericytes, smooth muscle cells and glomus cells towards outside of vessel
Essential features
- 2 main elements:
- Blood vascular system (active, closed circuit pumping system [heart])
- Arterial system
- Microcirculation: capillaries
- Venous system
- Lymph vascular system (passive, open one way system)
- Blood vascular system (active, closed circuit pumping system [heart])
- 2 types of new blood vessel formation:
- Vasculogenesis: vessels from precursor cells angioblasts
- Angiogenesis from pre-existing vessels via sprouting
- General structure of the arterial and venous system (thickness depends on size and type of vessel)
- Tunica adventitia (TA)
- Tunica media (TM)
- Tunica intima (TI)
- Capillaries and sinusoids: single endothelial layer with nuclei bulging into the capillary lumen
Terminology
- Sinusoid - large diameter capillary
Embryogenesis
- Development of the vascular system begins in the yolk sac of the embryo with the formation of hemangioblasts, which differentiate into hematopoietic cells and angioblasts, a mesoderm derived precursor of endothelial cells (Development 2011;138:4569, Int J Dev Biol 2011;55:419)
- Vasculogenesis describes the formation of new blood vessels from precursor cells angioblasts
- Angiogenesis describes the formation of new blood vessels from pre-existing vessels via sprouting, a coordinated expansion of a pre-existing network.
- Notch signaling pathway plays a central role in all the processes of vascular development
- Postnatal angiogenesis and ischemic vascularization / endothelial progenitor cells - endothelium transformation
- Artery formation by upregulating the expression of arterial markers (lack of Notch will result in venous endothelial cells allows the expression of venous markers) (Stem Cells Int 2012;2012:805602)
Physiology
- Principal functions are:
- Transportation of gases (O2 and CO2) and metabolites (nutrients and metabolic waste product) to and from tissue cells
- Temperature regulation
- Dispersion of hormones
- Immune system
- Blood clotting
- Blood vascular system:
- Active pumping system (heart)
- Closed circuit: arterial system - capillary network - venous system
- Lymph vascular system:
- Passive system
- Open one way system: drains the excess extravascular fluid (lymph) to the blood vascular system
Diagrams / tables
Gross description
- Arterial system
- Elastic artery: major distribution vessels
- Aorta, subclavian, iliac and pulmonary
- Muscular artery: main distributing branches
- Radial, femoral, renal cerebral arteries
- Arteriole: terminal branches supplying the capillaries
- Elastic artery: major distribution vessels
Microscopic (histologic) description
- Normal histology:
- Structural transition is gradual between the different types of vessels
- General structure of the arterial and venous system (thickness depends on size and type of vessel)
- Tunica adventitia (TA):
- Longitudinally arranged collagen
- Layer is larger in veins than arteries
- Tunica media (TM):
- Concentrically arranged smooth muscle
- Diameter is altered by autonomic control
- Smooth muscle may secrete collagen, elastic fibers, elastic lamellae and proteoglycans
- Larger diameter in arteries than veins of similar size
- Tunica intima (TI):
- Inner endothelium
- Variable outer subendothelial connective tissue (SCT) composed of scattered fibroblasts and myointimal cells producing collagen and elastin fibers
- With age myoepithelial cell can accumulate lipids causing tunica intima thickening
- Tunica adventitia (TA):
- Arterial system:
- Artery types:
- Elastic artery
- Muscular artery
- Arteriole (lumen < 0.3 mm)
- Artery types:
| Tunica intima | Tunica media | Tunica adventitia | |
| Elastic artery |
|
|
|
| Muscular artery |
|
|
|
| Arteriole (large; lumen < 0.3 mm) |
|
|
- Microcirculation:
- Direction of blood flow:
- Arterioles → capillaries → postcapillary venules → small muscular venules
- AV shunt: direct connection between the arterioles and venules
- Arteriole (small):
- Lumen < 0.1 mm)
- TI with almost no subendothelial connective tissue
- No internal elastic lamina
- < 2 layers of smooth muscle
- No external elastic lamina
- Capillaries and sinusoids:
- 3 - 40 micrometers
- Single endothelial layer with nuclei bulging into the capillary lumen
- No muscular layer or elastic lamina
- 3 types:
- Continuous capillaries: uninterrupted endothelial layer (brain, muscle, lung, connective tissue)
- Fenestrated capillaries: capillaries with multiple large pores (kidney, endocrine organ)
- Sinusoid with discontinuous endothelium: disrupted Interface between the tissue and capillary lumen (spleen sinusoid, liver sinusoids)
- Pericytes:
- Present but difficult to identify on H&E
- Contractile cell that regulates microvascular blood flow (SMA+) (Histol Histopathol 1991;6:269, Microvasc Res 2009;77:235)
- Postcapillary venules - small muscular venules:
- Series of postcapillary draining vessels with increasing luminal diameter and wall thickness
- Direction of blood flow:
- Venous system:
- Low pressure draining system returning the blood to the heart
- Blood flow is maintained by:
- Negative pressure created in the chest cavity / right atrium during inspiration
- Compression of veins during contraction of skeletal muscle
- Venous valves
- Elastic and muscular components of the veins are less prominent
- Lymphovascular system:
- Low pressure draining system returning the lymph to the venous system
- Lymph flow is maintained by
- Negative pressure created in the chest cavity during inspiration
- Compression of vessels during contraction of skeletal muscle
- Lymphovascular valves
- Lymphoid capillary:
- Similar size to the regular capillary
- No pericytes
- No or minimal basement membrane
- Greater permeability compared to regular capillary
- No lymphatic vessels in CNS, cartilage, bone, teeth, thymus, placenta
- Lymph nodes:
- Site of antigen presentation, antibody secretion, activated lymphoid cells entry into lymph
- Glomus body:
- Encapsulated glomeriform arteriovenous anastomosis (glomus body) richly innervated by autonomic nervous system fibers
- Located in dermis
- High number in finger and toes
- Involved in the thermal regulation
- Glomus cells:
- Specialized modified smooth muscle cell with indistinct borders, pale cytoplasm, uniform nuclei; surround arterial segment of glomeriform arteriovenous anastomosis (glomus body)
- SMA+, MSA+, type IV collagen (outlines basement membrane), desmin variable / +, S100-, CK-
- Normal aging related changes:
- Normal vascular structure changes during life, resulting with progressive vascular stiffness
- Elastic arteries:
- Increase in diameter
- Fibrous intimal thickening
- Fragmentation of elastic laminae
- Thickening of vasa vasorum walls
- Muscular arteries:
- Dilatation and tortuosity
- Fibrous intimal thickening
- Fragmentation and calcification internal of elastic laminae
- Fibrosis and hyalinization of tunica media
- Arterioles:
- Fibrous intimal thickening
- Hyalinization of tunica media
- Capillaries:
- Basement membrane thickening
- Venules and veins:
- Fibrous intimal thickening
- Hypertrophy of the muscle bundles
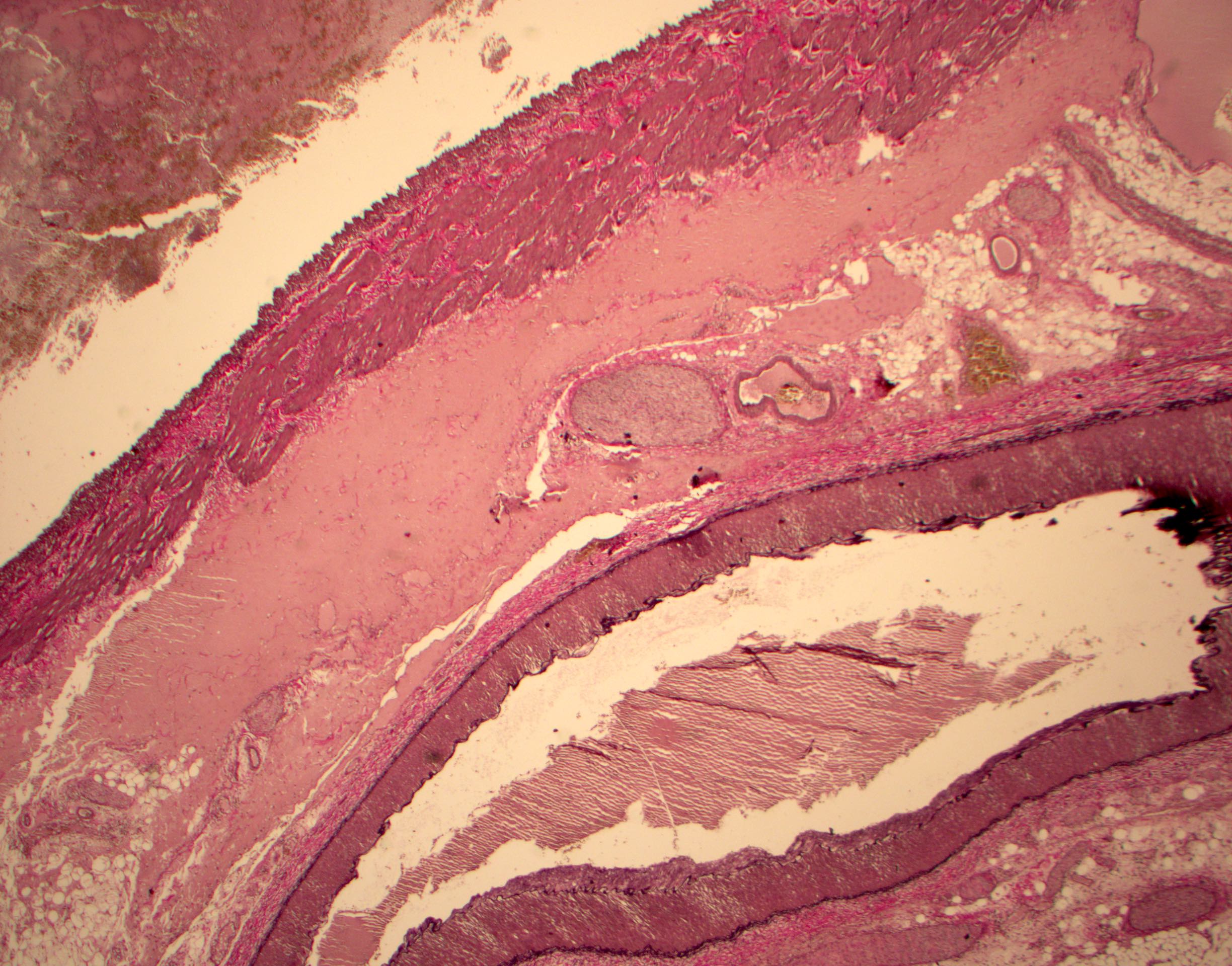
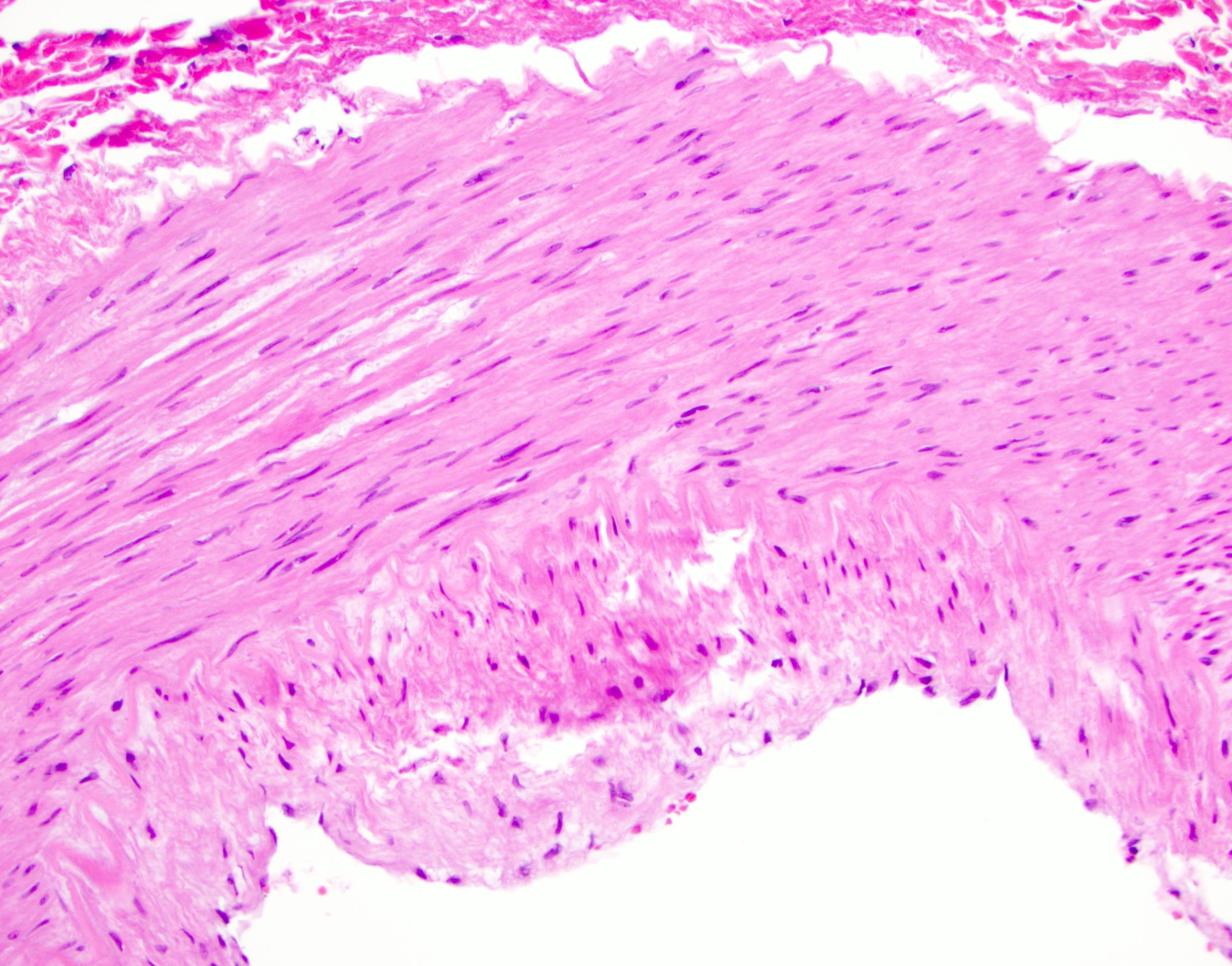
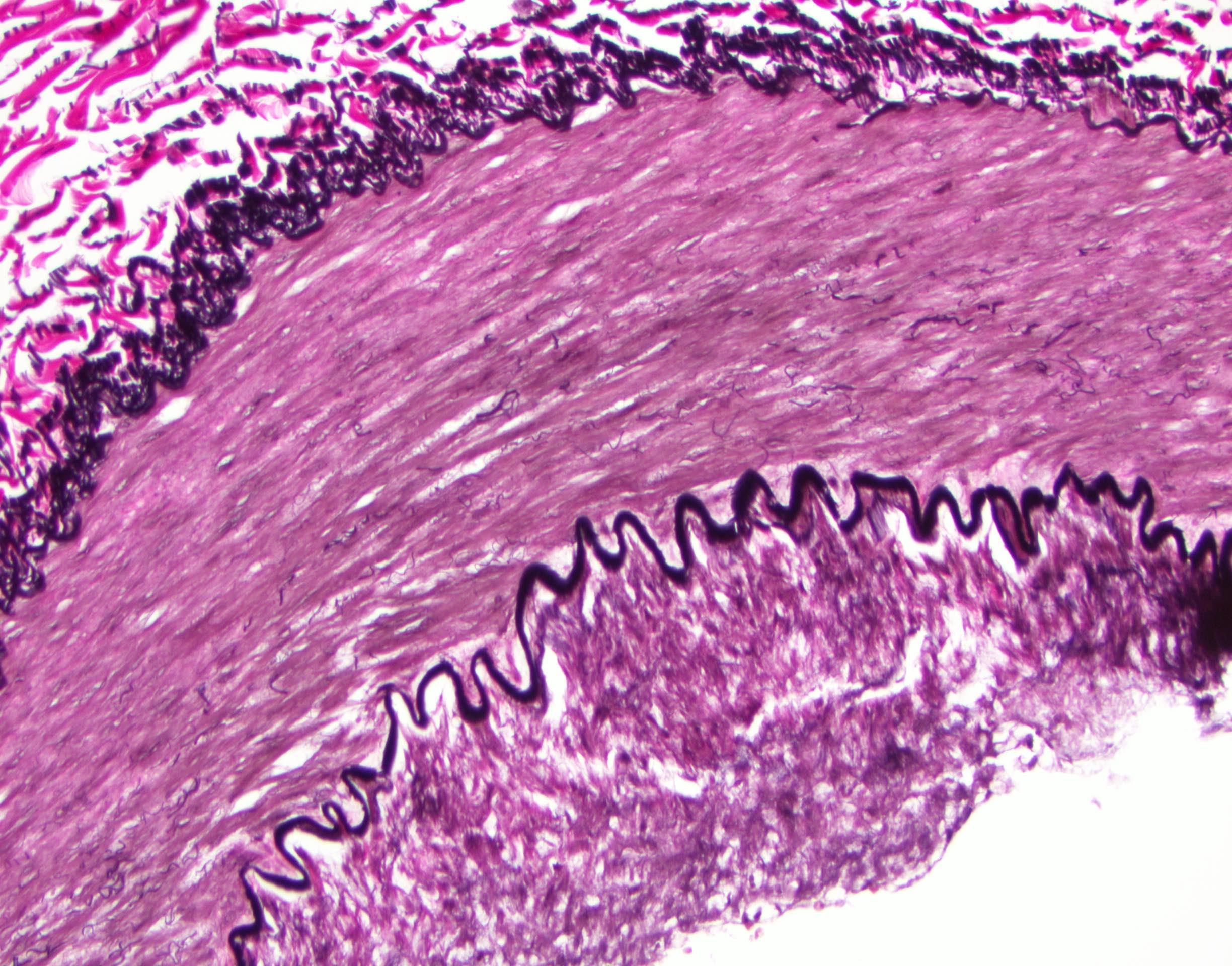
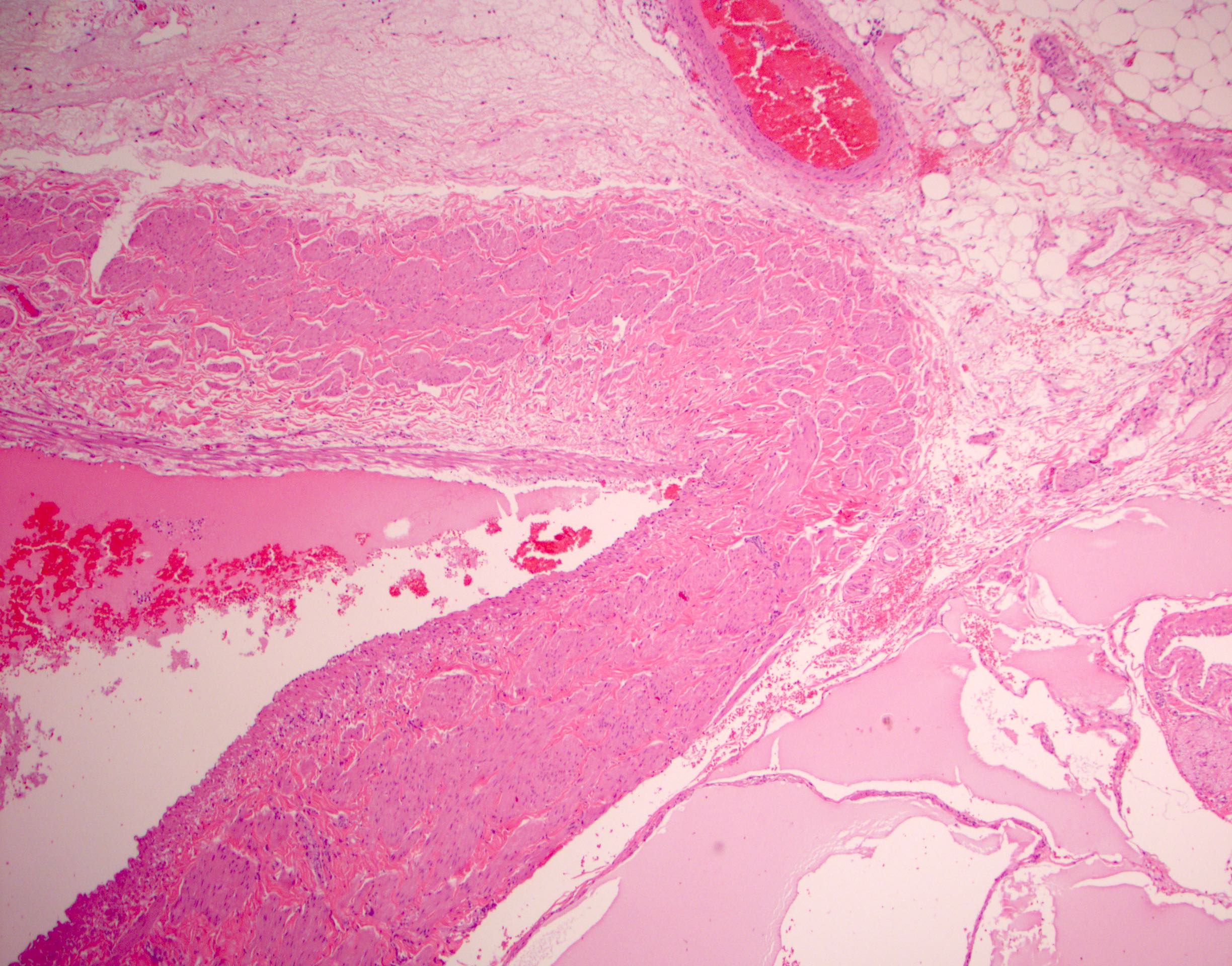
Microscopic (histologic) images
Positive stains
- Vascular endothelium: CD34, CD31, factor VIII related antigen, vimentin, Ulex europaeus I lectin (binds to alpha-L-fructose compounds), endothelin, von Willebrand factor; also FLI1 (nuclear stain) and ERG (Am J Surg Pathol 2001;25:1061, Am J Clin Pathol 2012;138:803)
- Lymphatic endothelium: similar staining as vascular endothelial cells but also D2-40+, LYVE1+ and only weakly factor VIII related antigen+
- Pericytes: alpha smooth muscle actin, myosin, vimentin; also CD31
- Smooth muscle cells of tunica media: actin, desmin
Electron microscopy description
- Endothelial cells: cells are joined by tight, adherens or gap junctions; numerous pinocytotic vesicles, cytoplasmic microfilaments, microvilli, continuous basal lamina and Weibel-Palade bodies (membrane bound organelle which contains von Willebrand factor)
- Capillary endothelium: surrounded by basement membrane, numerous supporting pericytes with its own basement membrane
- Fenestrated capillary endothelium: fenestration (thin electron dense line), surrounded by basement membrane, rare supporting pericytes
- Lymphatic endothelium: minimal or no little basement membrane, no pericytes
Electron microscopy images
Additional references
Board review style question #1
Which of the following is part of the arteriolar wall structure?
- External elastic lamina (EEL)
- Fenestrated elastic sheets
- Internal elastic lamina (IEL)
- Muscularis propria
Board review style answer #1
C. Internal elastic lamina (IEL).
The arteriolar wall is composed of thin tunica intima with endothelial layers and subendothelial connective tissue, tunica media with thin internal elastic lamina (answer C) and smooth muscle and tunica adventitia. External elastic lamina is present only in muscular type arteries and the fenestrated elastic sheets are present in the elastic type arteries. Muscular wall of a luminal visceral organ is called muscularis propria. The muscular wall of a blood vessel is called tunica media.
Comment Here
Reference: Histology-blood vessels
Comment Here
Reference: Histology-blood vessels
Board review style question #2
Board review style answer #2
D. Muscular type artery.
The depicted portion of this blood vessel shows 2 (internal and external) elastic lamina. Arterioles and large muscular vein have only internal elastic lamina. Elastic type artery has multiple layers of elastic membranes in the tunica media. Muscularis type artery as shown has 2 distinct internal and external elastic laminae. Sinusoid is a type of capillary and has only a single layer of endothelium without tunica media / adventitia or elastic lamina.
Comment Here
Reference: Histology-blood vessels
Comment Here
Reference: Histology-blood vessels