Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Rastegar S, Suster D. Myxoinflammatory fibroblastic sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuemyxoinflammatory.html. Accessed April 19th, 2024.
Definition / general
- Rare, low grade sarcoma of the distal extremities with prominent myxoid stroma, mixed inflammation, virocyte-like cells, pseudolipoblasts and emperipolesis (Am J Surg Pathol 2014;38:1)
- First described in 1998 simultaneously by Montgomery et al. and Meis-Kindblom and Kindblom (Mod Pathol 1998;11:384, Am J Surg Pathol 1998;22:911)
- High grade variant of myxoinflammatory fibroblastic sarcoma (MIFS) has been reported, although currently a matter of debate (Ann Diagn Pathol 2015;19:157)
Essential features
- Rare, low grade sarcoma of the distal extremities with prominent myxoid stroma, mixed inflammation, virocyte-like cells, pseudolipoblasts and emperipolesis (Am J Surg Pathol 2014;38:1)
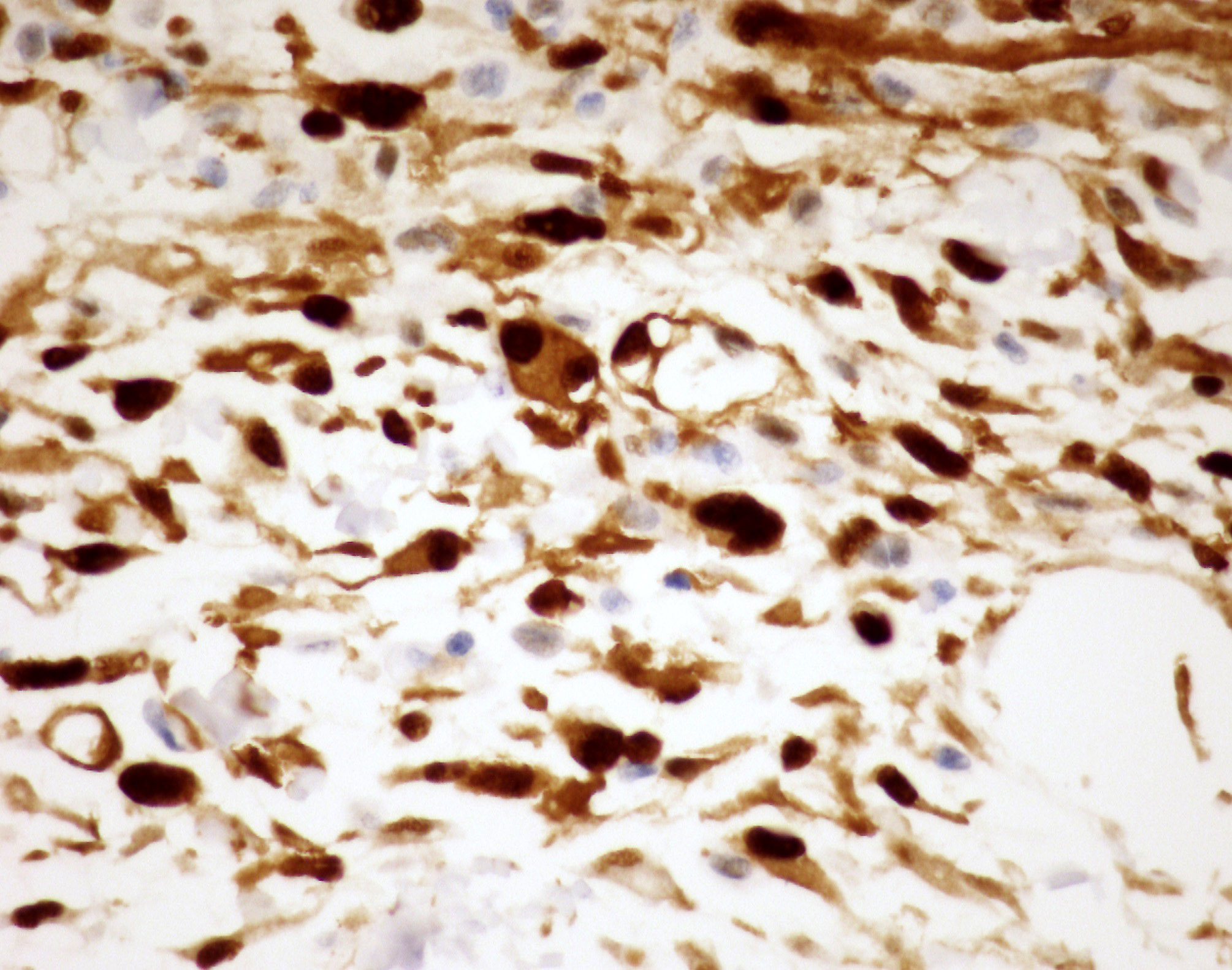
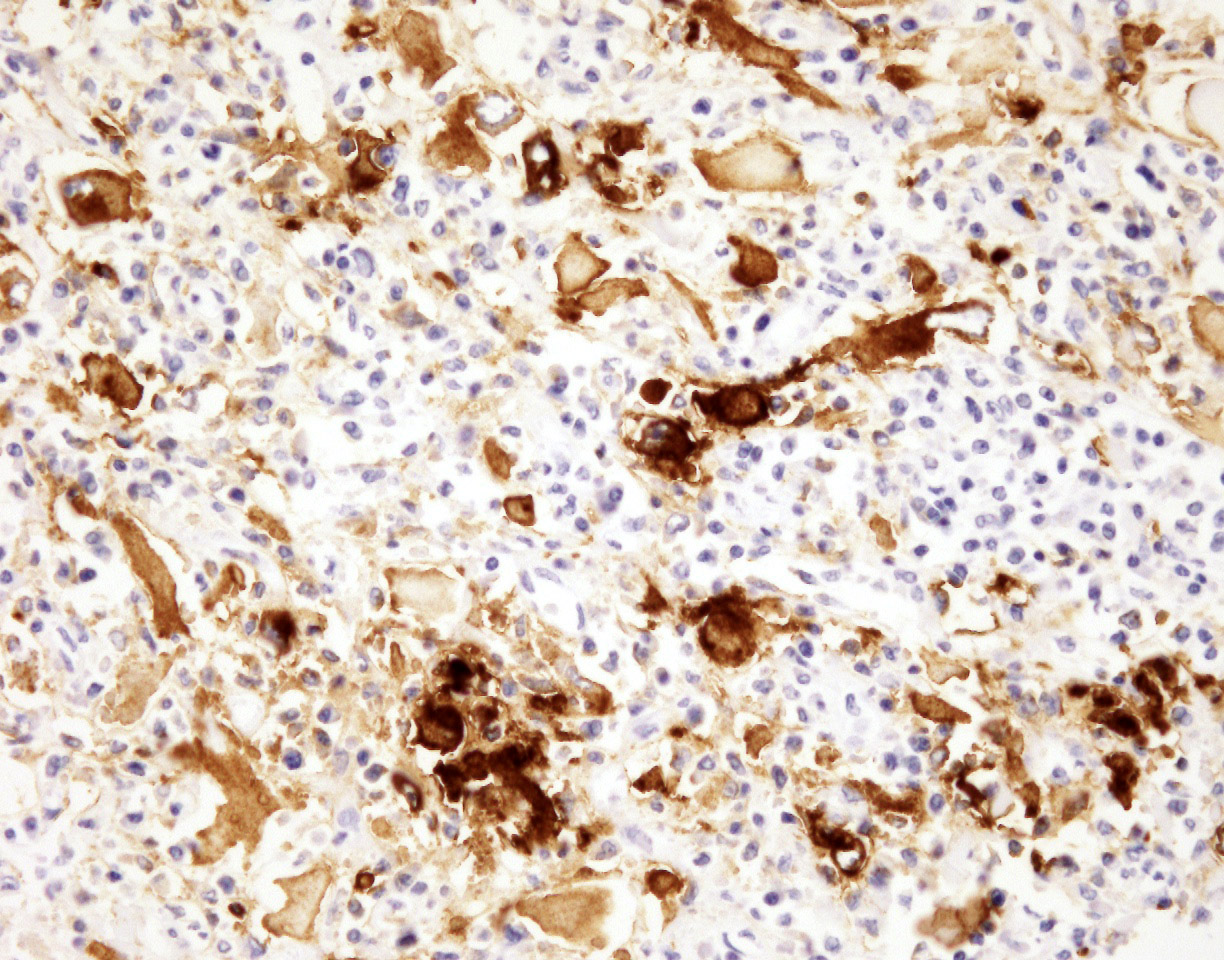
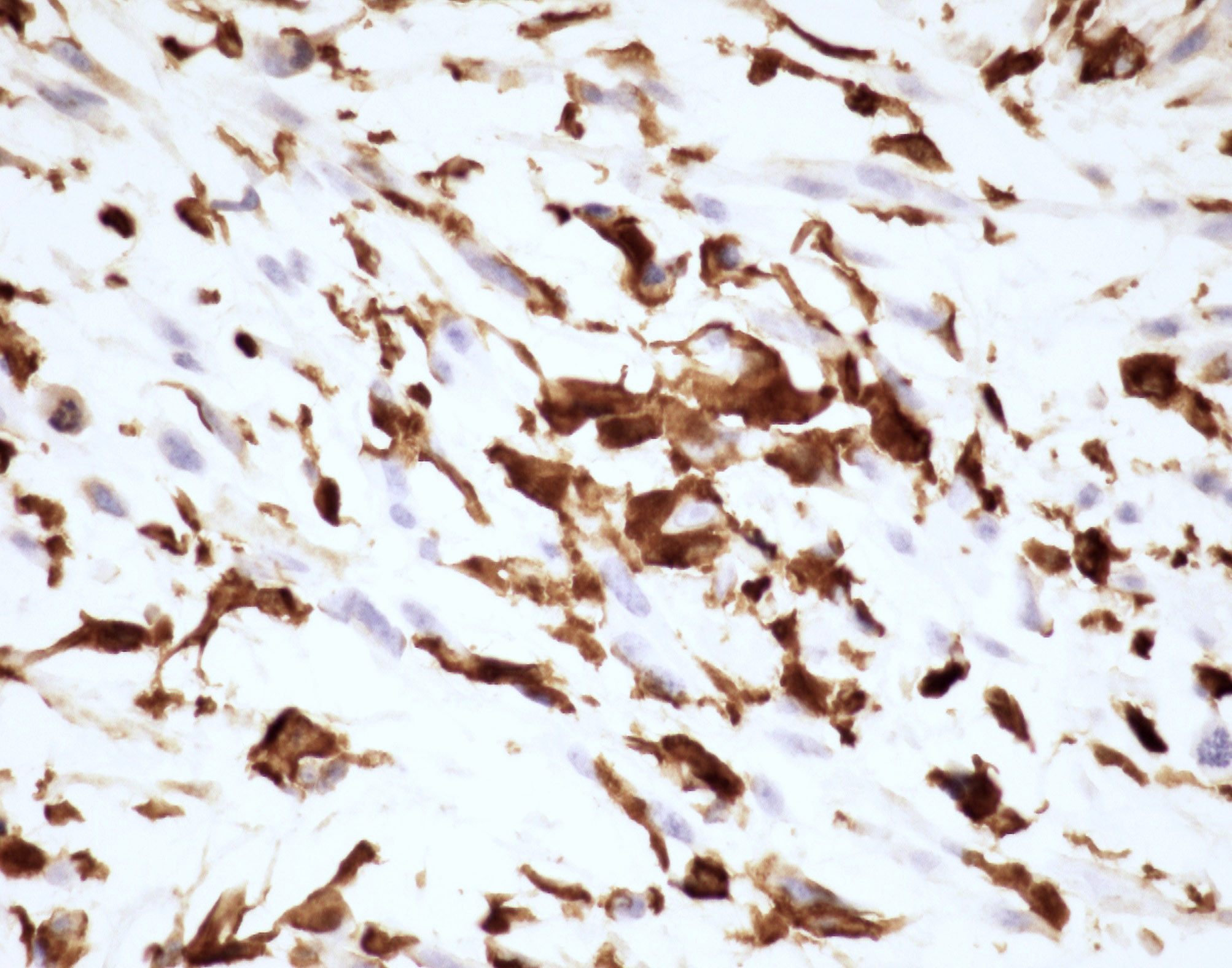
- Immunohistochemistry is relatively nonspecific, although an immunoprofile showing positivity for BCL1, CD10 and factor XIIIa may help strengthen the diagnosis
- Most common molecular alteration is VGLL3 amplification; a small number of cases demonstrate a t(1;10) translocation or BRAF rearrangements
- Diagnosis is primarily based on microscopic appearance and clinical characteristics
Terminology
- Not recommended: inflammatory myxohyaline tumor of the distal extremities with virocyte or Reed-Sternberg-like cells, acral myxoinflammatory fibroblastic sarcoma, inflammatory myxoid tumor of the soft parts with bizarre giant cells
ICD coding
- ICD-0: 8811/1 - myxoinflammatory fibroblastic sarcoma (MIFS)
- ICD-10: C49.9 - malignant neoplasm of connective and soft tissue, unspecified
- ICD-11: 2B5F.2 & XH2D15 - sarcoma, not elsewhere classified of other specified sites and myxoinflammatory fibroblastic sarcoma
Epidemiology
- Rare lesion; men and women with a wide age range (mean age 40 - 49 years) presenting with a slow growing mass (Am J Surg Pathol 2014;38:1)
Sites
- Approximately 75% of tumors arise in the distal upper and lower extremities, including forearm, elbow, wrist, hand and fingers or ankle, feet and toes (J Cutan Pathol 2008;35:192)
- May also arise in proximal extremities (Am J Surg Pathol 2014;38:1)
Pathophysiology
- Some studies have shown morphologic overlap with hemosiderotic fibrolipomatous tumor and pleomorphic hyalinizing angiectatic tumor but the precise classification of these tumors and their relationship is debated
- Complex karyotypes with multiple reported recurrent genetic alterations
- Reference: Mod Pathol 2020;33:2520
Etiology
- Currently classified under tumors of unknown etiology
Clinical features
- Solitary painless pseudonodular mass (typically of the distal extremities)
- Wide size range
- Common local recurrence, rare metastases (J Cutan Pathol 2008;35:186, Virchows Arch 2003;442:25)
Diagnosis
- Clinicopathologic diagnosis: a combination of the appropriate clinical setting along with the characteristic histopathologic findings
- Immunohistochemistry pattern is not specific, although positivity for factor XIIIa, BCL1 and CD10 may support the diagnosis
- Demonstration of the VGLL3 amplification in the appropriate clinical setting supports the diagnosis (Am J Surg Pathol 2014;38:1)
Laboratory
- Unknown at this time
Radiology description
- Generally nonspecific radiological findings that may mimic benign or malignant processes (J Comput Assist Tomogr 2017;41:104)
Prognostic factors
- Completeness of initial surgical excision correlates with a lower incidence of recurrence (Am J Surg Pathol 2014;38:1)
Case reports
- 38 year old man with extensive local spread and multiple synchronous metastases (BMJ Case Rep 2018;2018:bcr2018224259)
- 51 year old man with a lesion on the dorsum of the nose (Ear Nose Throat J 2016;95:E32)
- 54 year old man with an extremely large cervicothoracic mass (Oncol Lett 2016;12:1717)
- 77 year old woman with myxoinflammatory fibroblastic sarcoma with hybrid features of hemosiderotic fibrolipomatous tumor (Rare Tumors 2018;10:2036361318782626)
Treatment
- Wide local excision with or without radiation therapy (Cancer 2010;116:5733)
Gross description
- Multinodular tan-white lesion with gelatinous areas corresponding to fibrotic and myxoid areas
- Usually small tumors (~ 3 cm) but may attain larger sizes
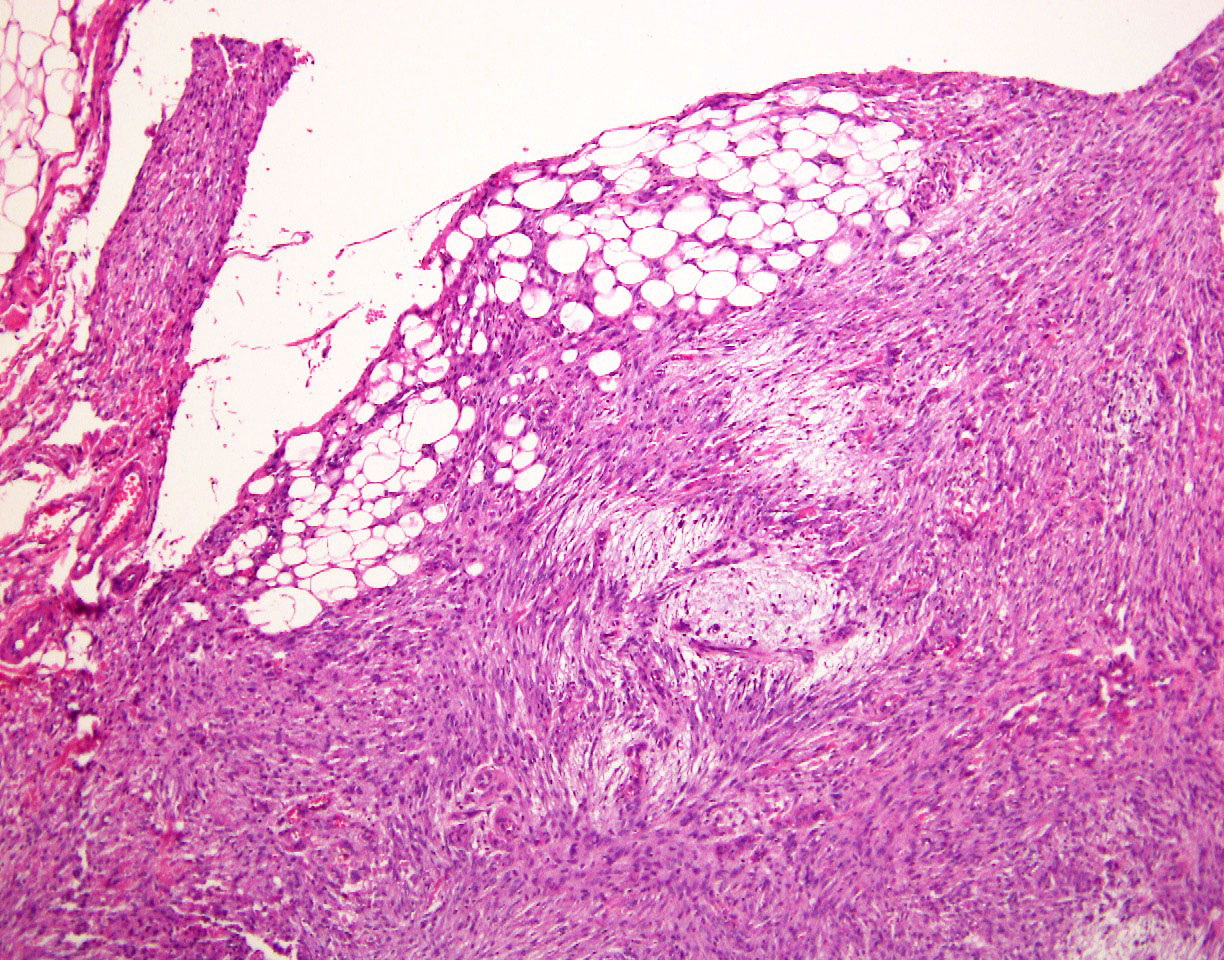
- Located in subcutaneous tissue of dermis; may be deeply infiltrative or involve joints and tendons
- Reference: Am J Surg Pathol 2014;38:1
Frozen section description
- Reported discrepancies in the histological grade between the frozen section and final diagnoses (Int J Clin Oncol 2020;25:2158)
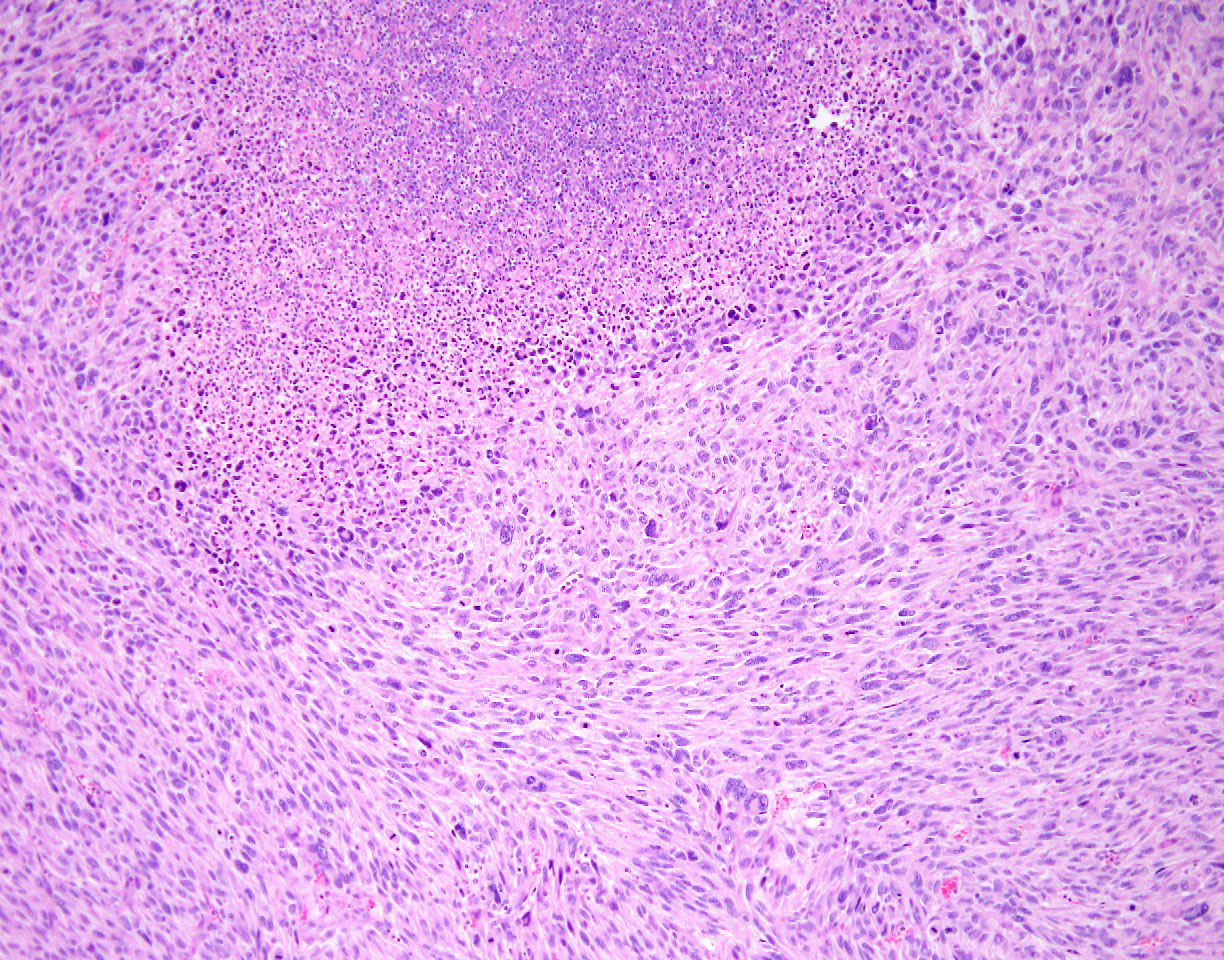
Microscopic (histologic) description
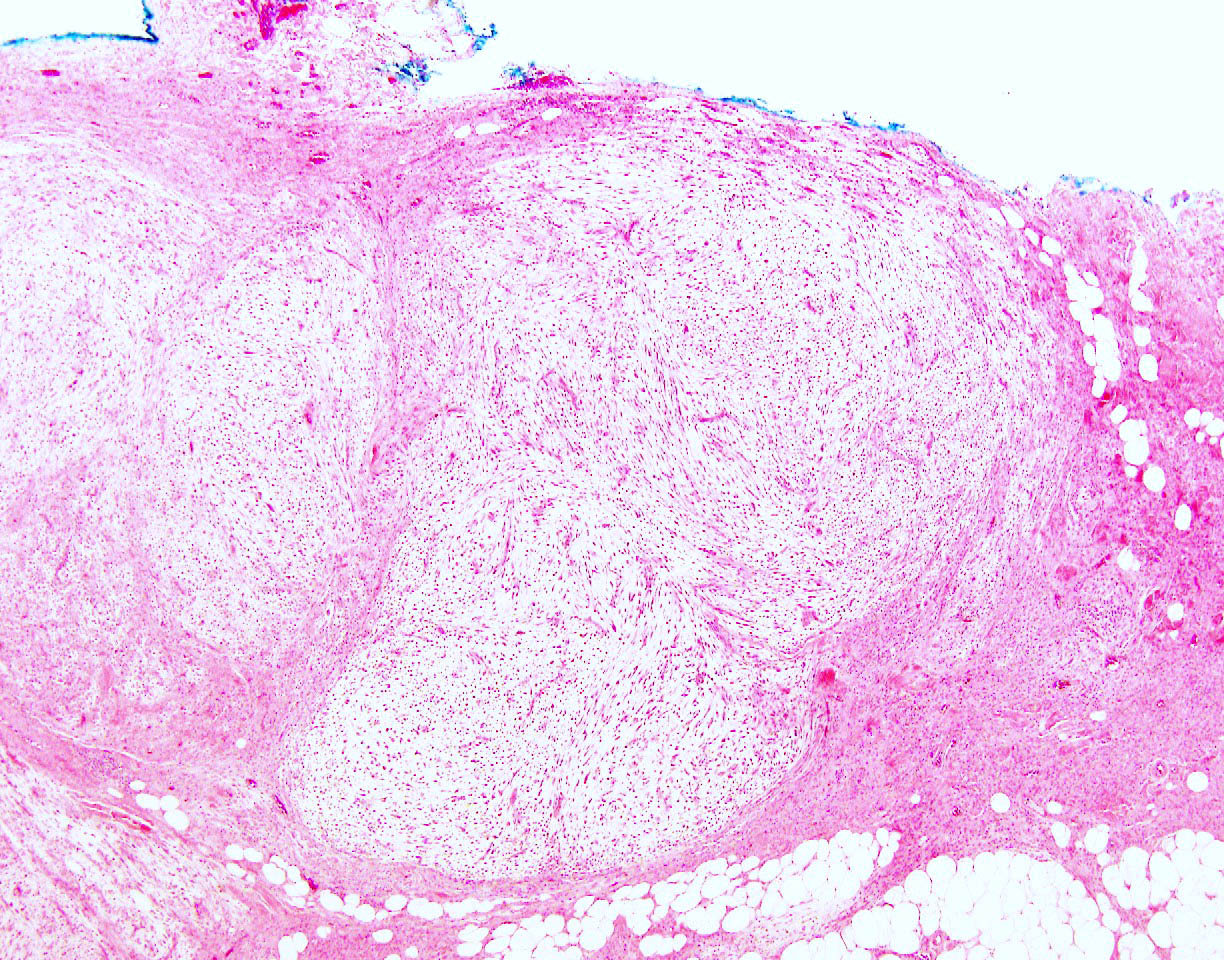
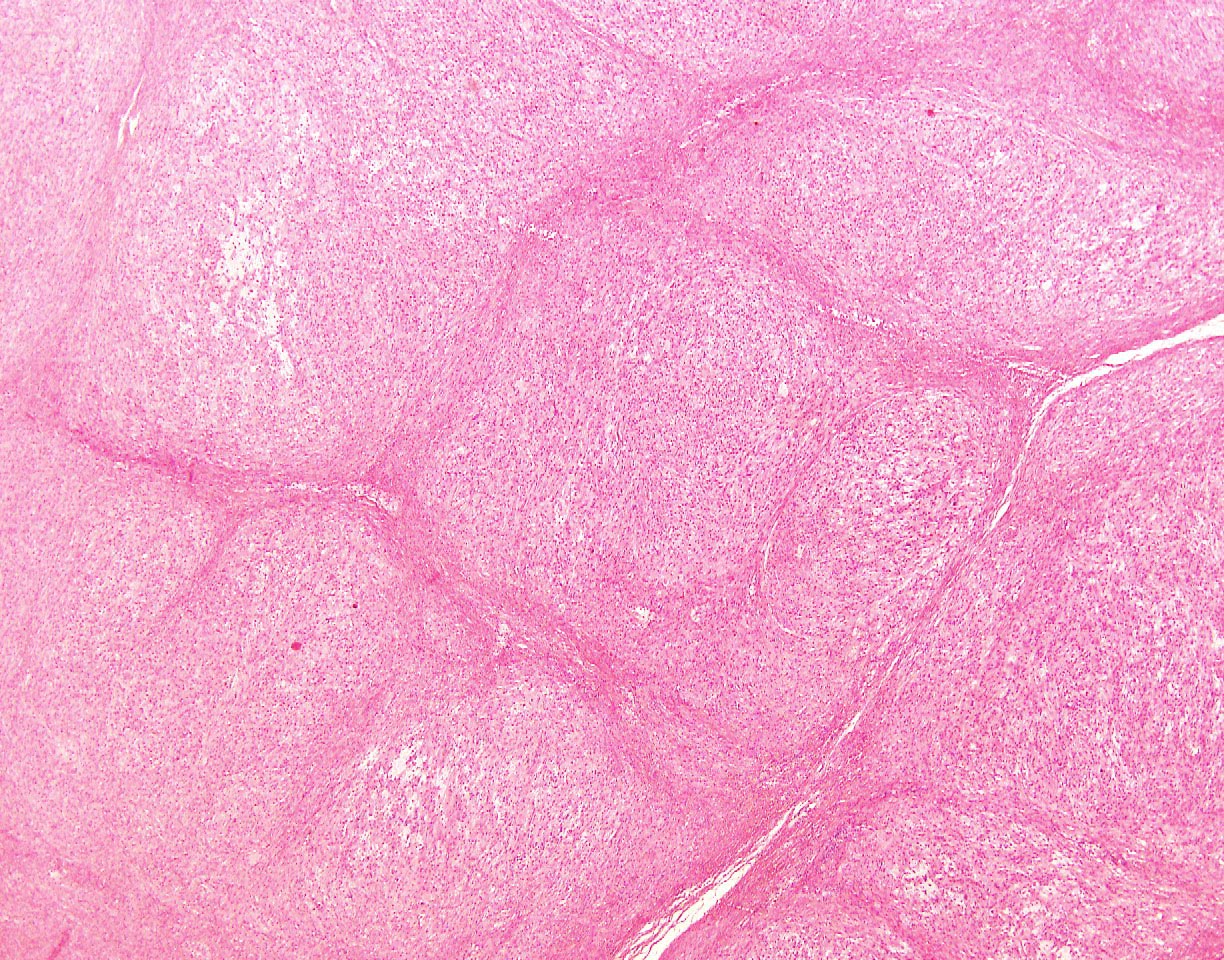
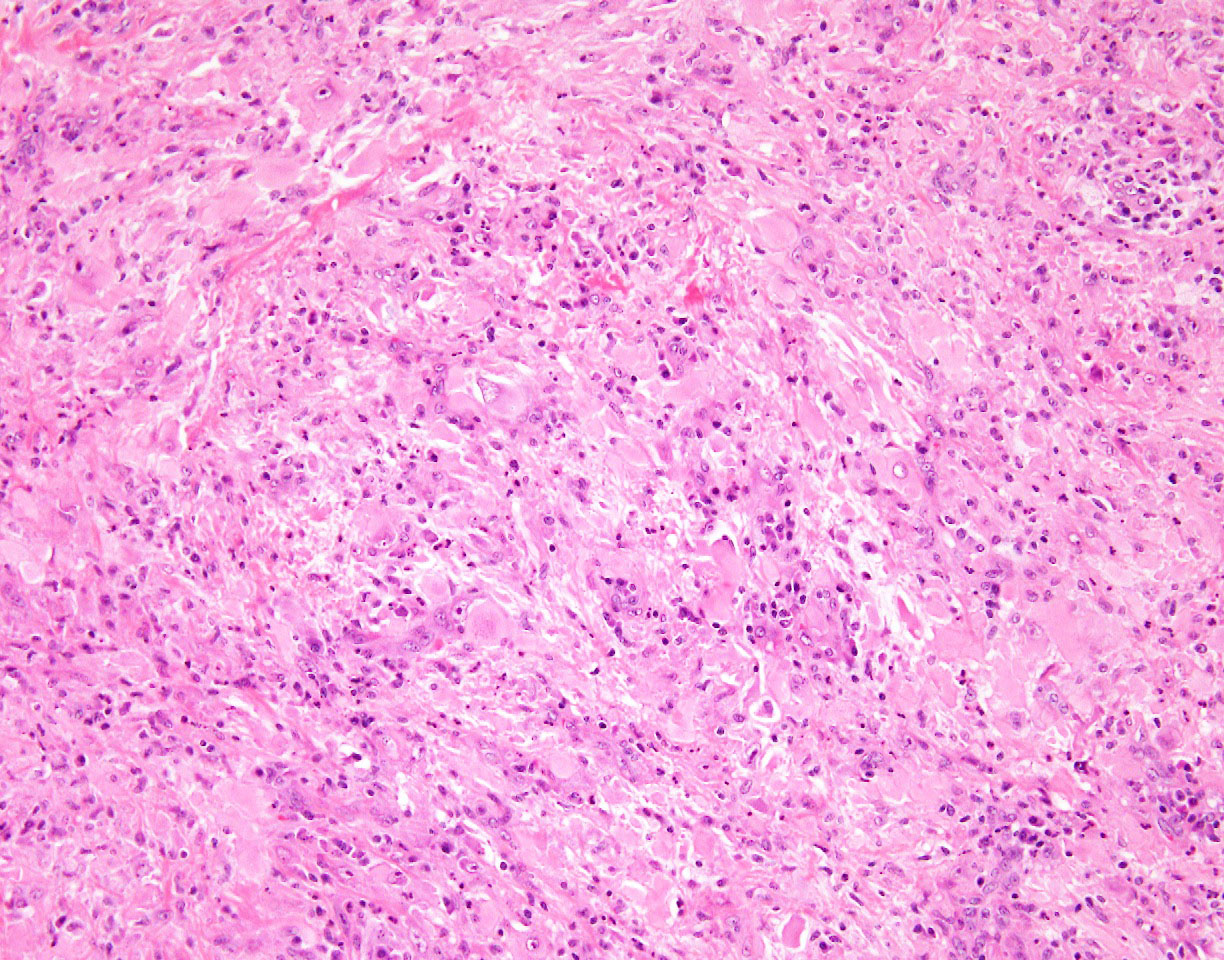
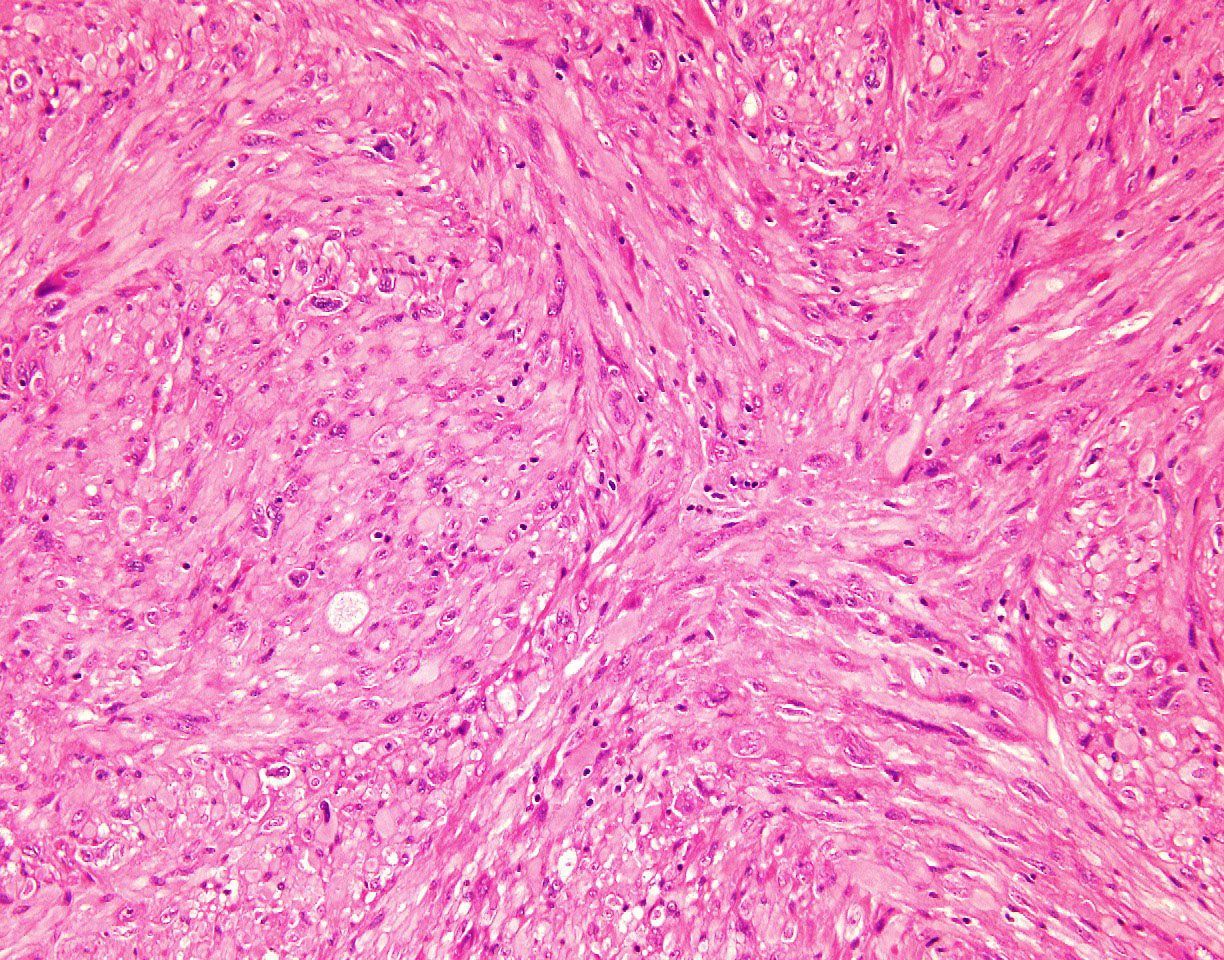
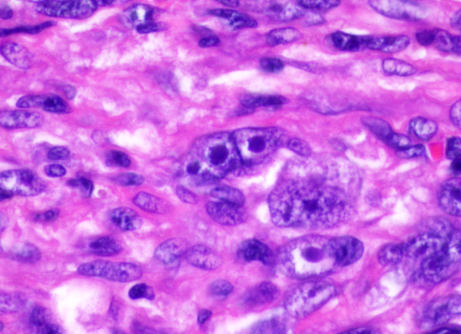
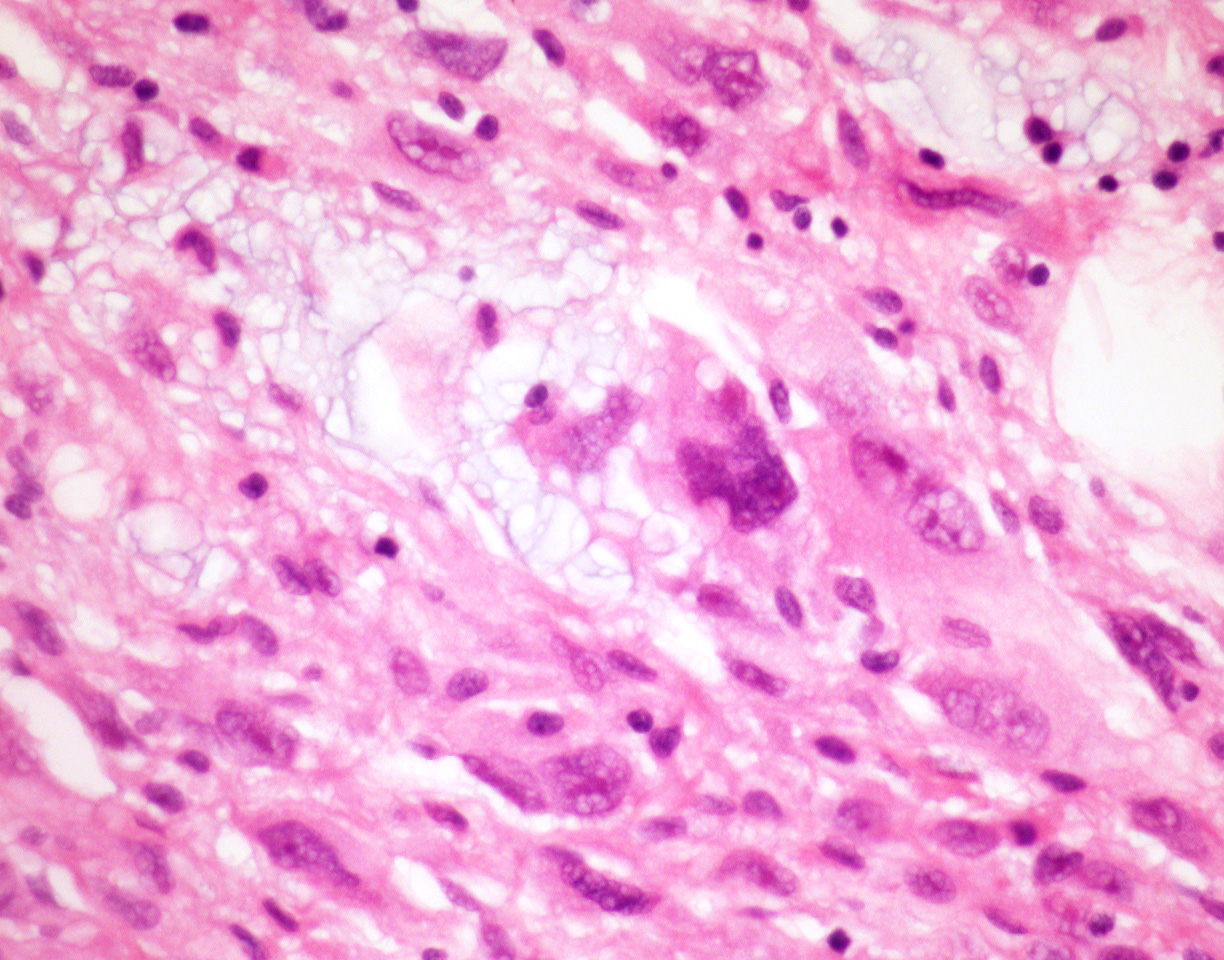
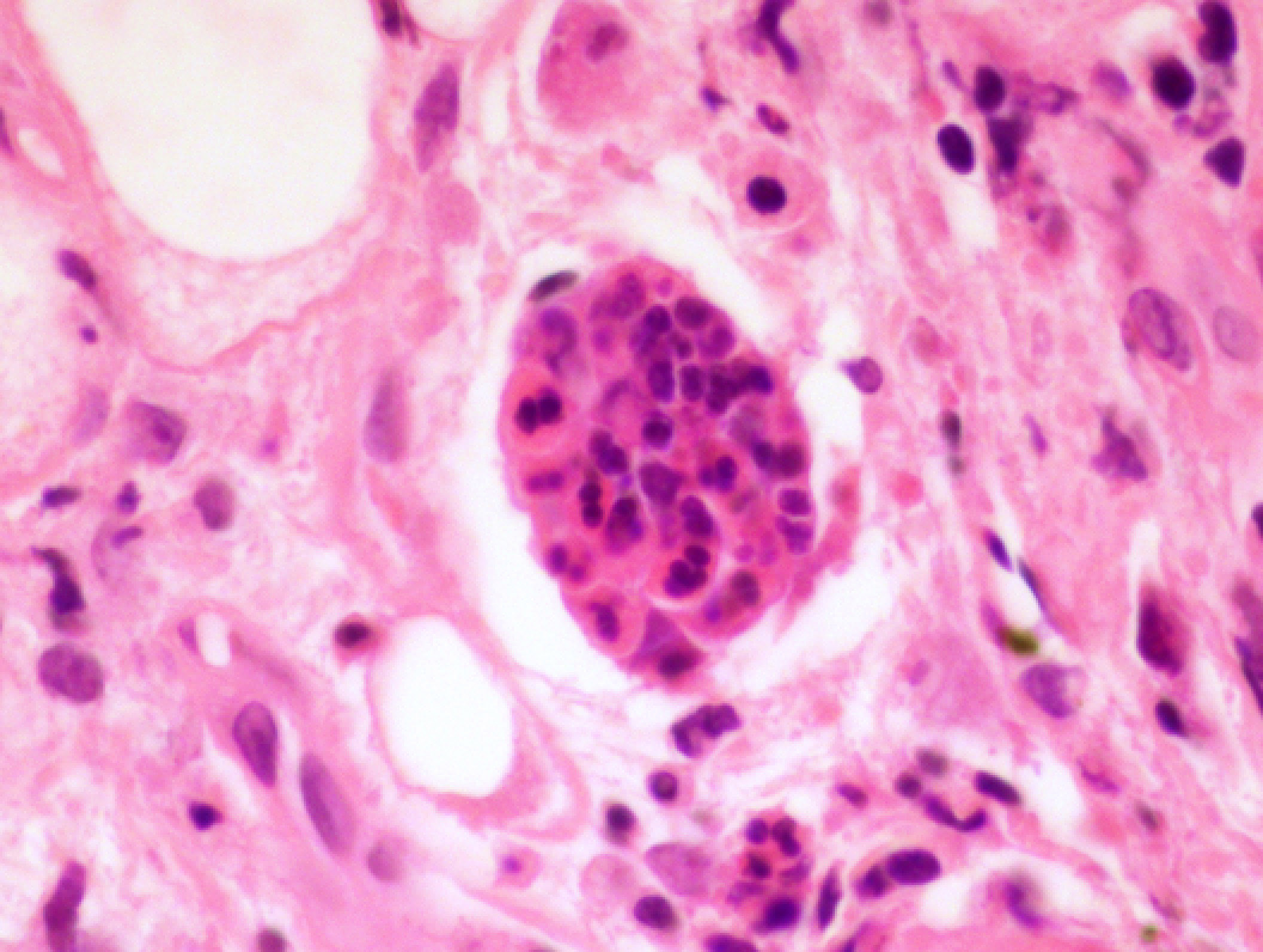
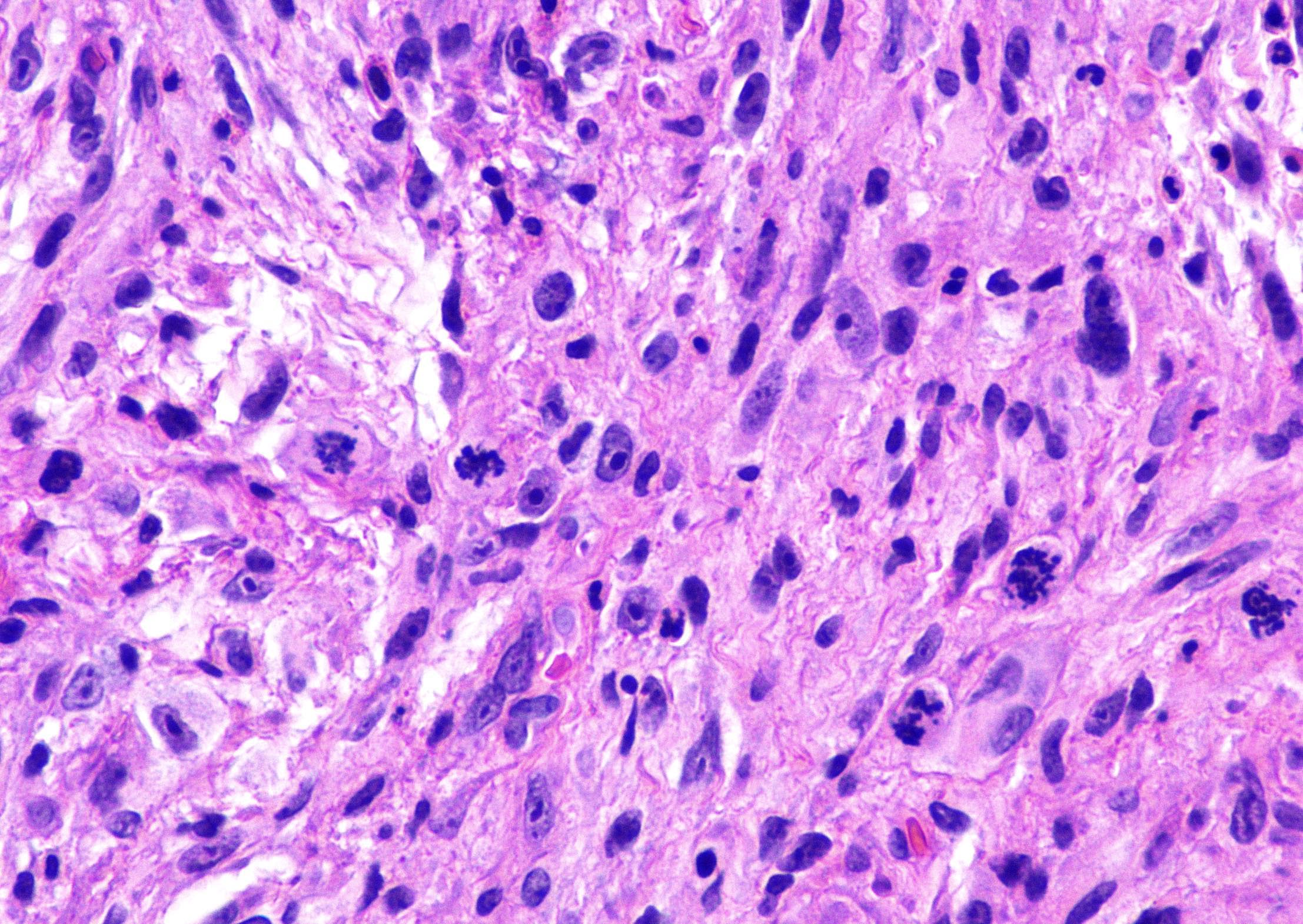
- Multinodular lesion composed of variable myxoid and fibrous / hyalinized areas with a dense associated inflammatory infiltrate
- Infiltrative growth pattern usually confined to subcutaneous tissue; may sometimes show involvement of deeper structures, including skeletal muscle
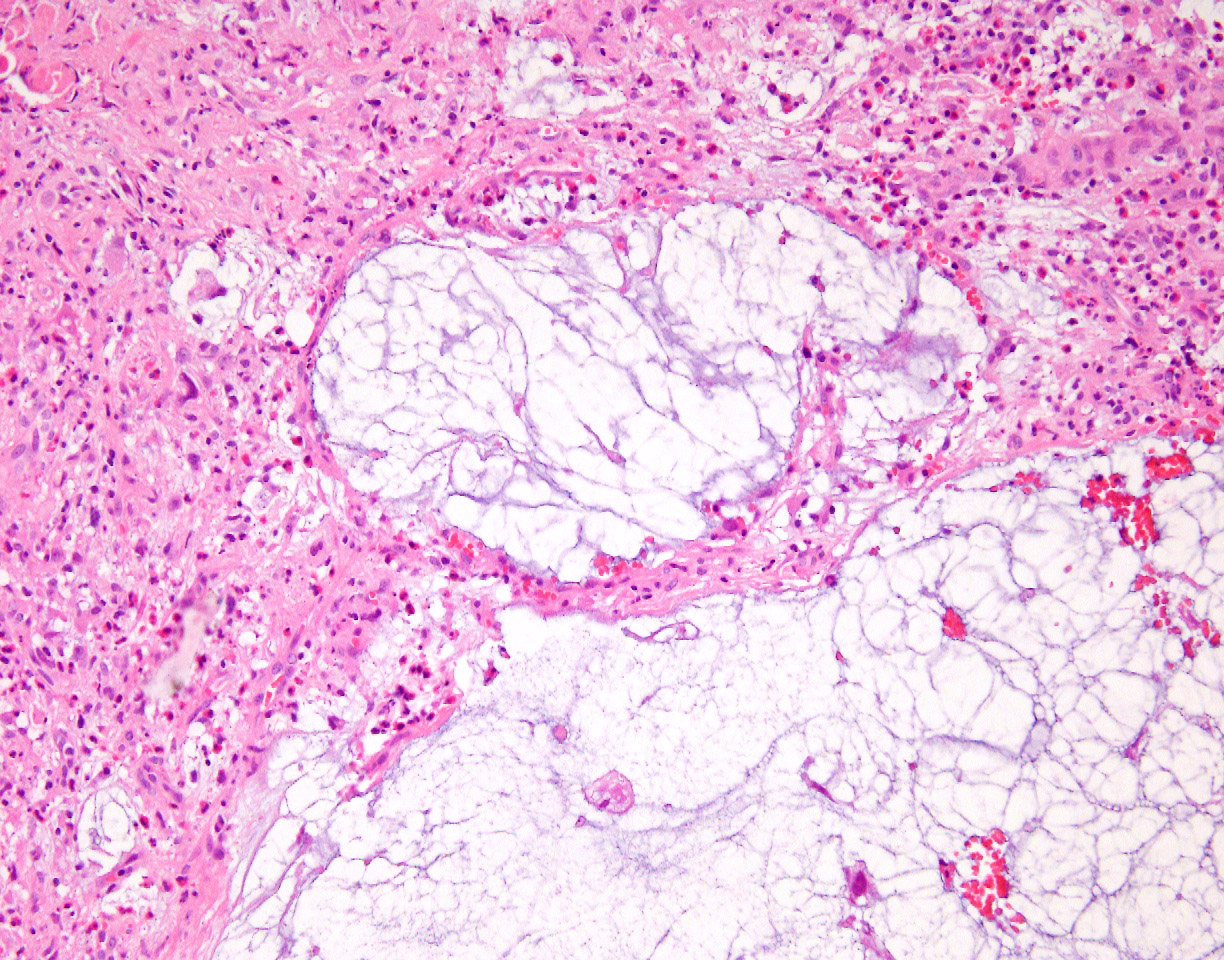
- Acute or chronic inflammatory cells, including neutrophils, lymphocytes, plasma cells, histiocytes and eosinophils, that blend through myxoid and fibrous areas
- Tumor cell population composed of epithelioid to spindled tumor cells
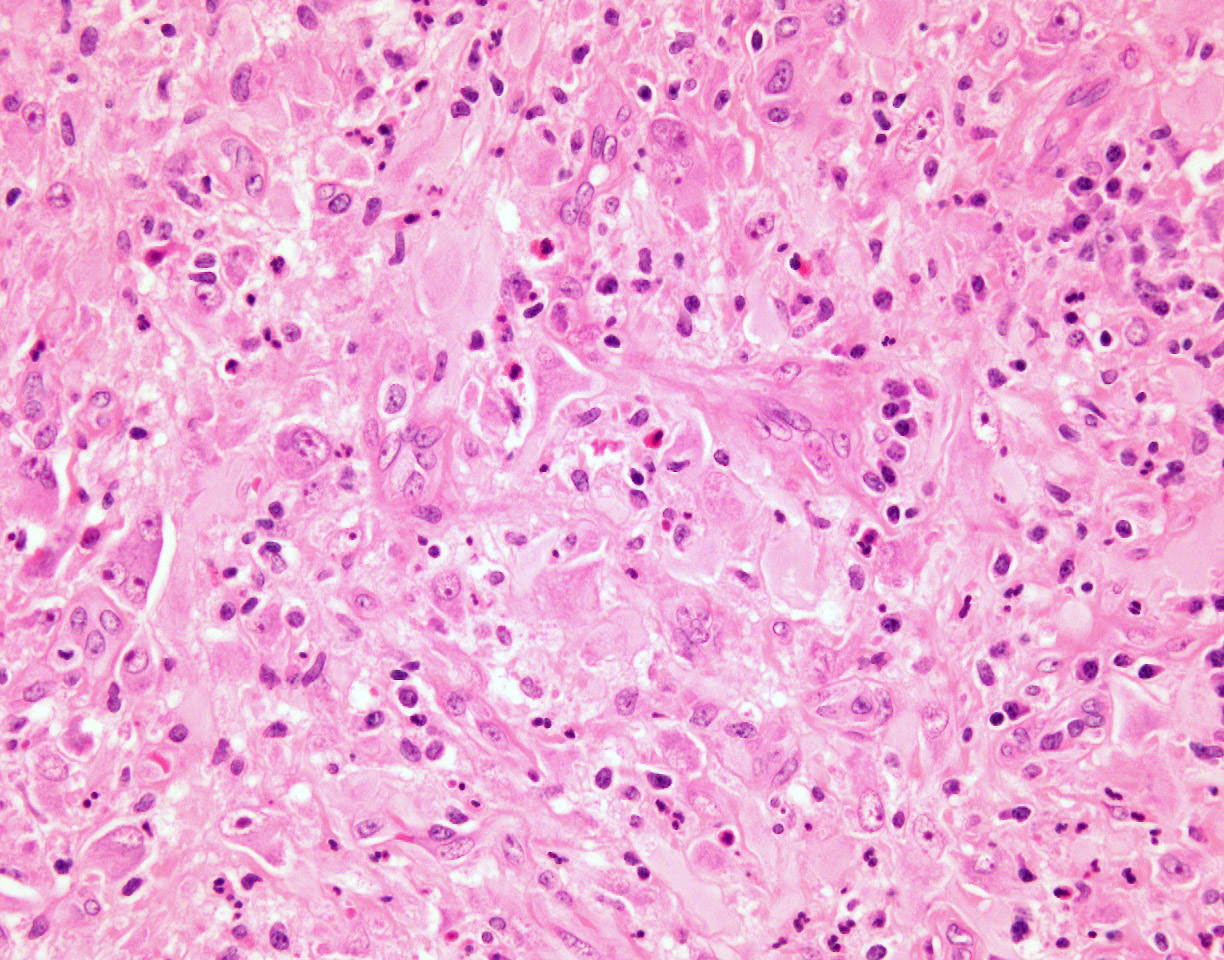
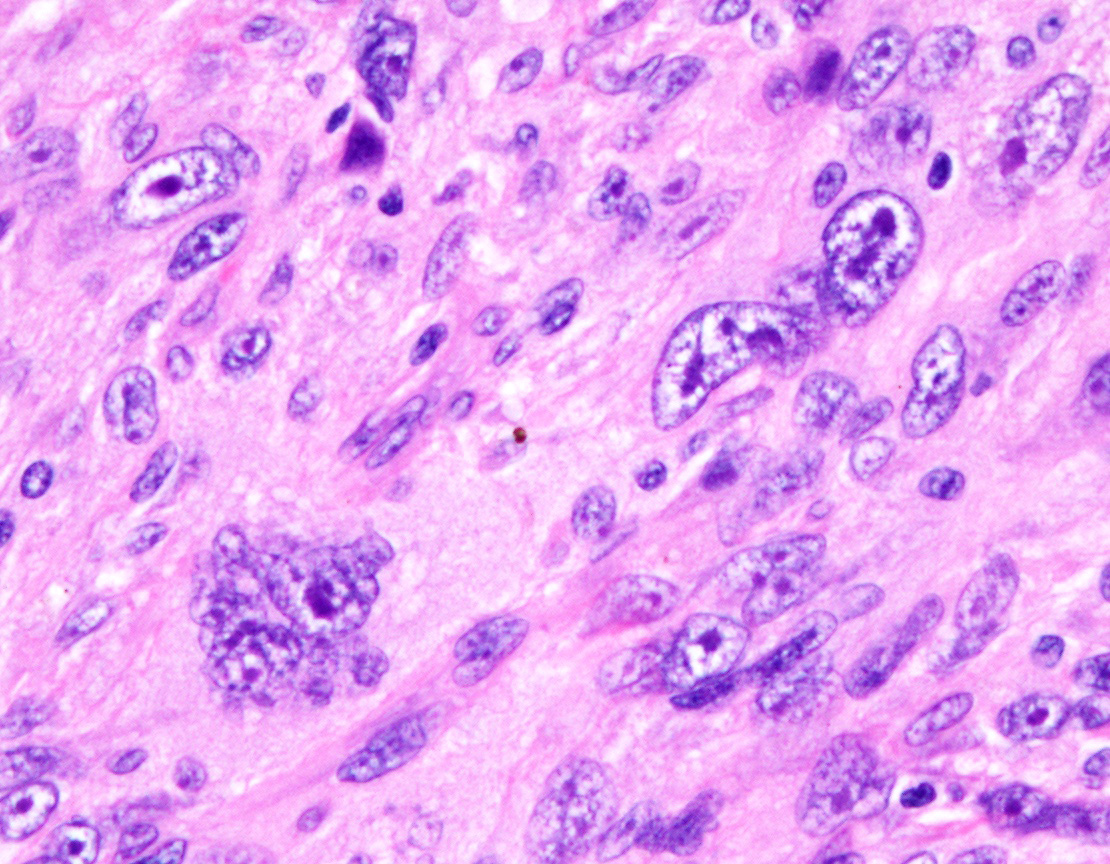
- Scattered large cells with bizarre nuclei and prominent nucleoli resembling viral inclusions (virocyte-like cells) or Reed-Sternberg cells
- Multivacuolated cells resembling pleomorphic lipoblasts (pseudolipoblasts - tumor cells with cytoplasmic vacuoles containing myxoid material)
- Giant tumor cells, predominantly within the myxoid areas, display prominent emperipolesis
- Low mitotic rate despite increased atypia; may display some areas of necrosis
- Can show focal areas that resemble hemosiderotic fibrolipomatous tumor (hemosidern laden histiocytic cells) or pleomorphic hyalinizing angiectatic tumor (pleomorphic cells and dilated hyalinized vessels)
- High grade variant: increased cellularity, increased mitotic activity and necrosis, retains characteristic virocyte / Reed-Sternberg-like cells, pseudolipoblastic cells (Am J Surg Pathol 2013;37:1627)
- Reference: Mod Pathol 2020;33:2520
Microscopic (histologic) images
Contributed by David Suster, M.D.
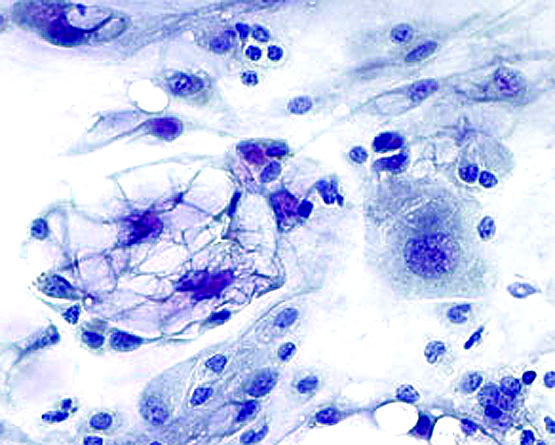
Cytology description
- Spindle, epithelioid, lipoblast-like and ganglion-like cells in myxoid background with prominent inflammatory infiltrate; cases may not display all features
- Must be cautious in diagnosis of soft tissue lesions by cytology alone (Acta Cytol 2007;51:231, Cytopathology 2003;14:73, Diagn Cytopathol 2012;40:E144)
Cytology images
Positive stains
Negative stains
- S100, SOX10, MITF, PGP9.5, GLUT1, calretinin, beta catenin, E-cadherin, calponin, androgen receptor, FLI1, WT1, TLE1, CD15, CD21, CD30, CD31, CD63, CD99, CD117, HBME1, MDM2, p53, PAX5, PAX8, MUC4 (some stains may show patchy, nonspecific staining) (Am J Surg Pathol 2014;38:1)
- INI1 shows retained expression
Electron microscopy description
- Fibroblastic features of abundant rough endoplasmic reticulum and mitochondria, intermediate filaments
- Lipoblast-like cells have cytoplasmic pseudoinclusions with extracellular mucin
- Reference: Am J Surg Pathol 1998;22:911
Molecular / cytogenetics description
- Complex and heterogeneous karyotypes described with multiple genetic aberrations, including aneuploidy, ring chromosomes and a t(2;6) (Virchows Arch 2007;451:923, Cancer Genet Cytogenet 2004;152:61, Cancer Genet Cytogenet 2007;177:139)
- Recurrent t(1;10)(p22;q24), resulting in gene rearrangements of TGFBR3 and MGEA5 has been described; initially thought to occur more commonly, subsequent studies have shown this rearrangement to be incredibly rare (~ 5%) in conventional myxoinflammatory fibroblastic sarcoma (Am J Surg Pathol 2010;34:1723)
- BRAF rearrangements have been described in a subset of myxoinflammatory fibroblastic sarcoma, although the largest molecular study examining BRAF rearrangement was able to identify BRAF in only ~ 5% of cases studied (Am J Surg Pathol 2014;38:1)
- Most common recurrent molecular alteration is amplification of VGLL3 on chromosome 3, which occurs in approximately 40% of cases (Am J Surg Pathol 2014;38:1)
Molecular / cytogenetics images
Videos
Whole slide review
Sample pathology report
- Foot, right, resection:
- Myxoinflammatory fibroblastic sarcoma (see comment)
- Comment: Sections show a multilobulated, infiltrative tumor within the subcutaneous soft tissues. There is a prominent mixed inflammatory cell population scattered throughout the tumor. Fibroblastic and myxoid areas are identified with a spindled to epithelioid neoplastic cell population with scattered prominent atypical cells (Reed-Sternberg-like cells), pseudolipoblastic cells and giant cells displaying emperipolesis. Mitotic activity is low. The tumor cells are positive for CD10, factor XIIIa and BCL1 and negative for SMA, desmin, cytokeratin AE1 / AE3, FLI1, CD45, MDM2, S100 and SOX10. Although nonspecific, the immunohistochemical profile is compatible with the above diagnosis.
Differential diagnosis
- Hemosiderotic fibrolipomatous tumor:
- Can show a spectrum of changes that resemble myxoinflammatory fibroblastic sarcoma
- Can also harbor the t(1;10) translocation, although debated
- Some authors believe these tumors may be related
- Pleomorphic hyalinizing angiectatic tumor:
- Spindled and epithelioid atypical cell population that may resemble myoxinflammatory fibroblastic sarcoma
- Prominent dilated vessels with peripheral hyalinization
- Epithelioid sarcoma:
- Most cells are round with dense eosinophilic cytoplasm, strongly keratin+, loss of INI1 / SMARCB1
- Hodgkin lymphoma:
- Myxofibrosarcoma:
- Rare in soft tissues of hands and feet
- More frequent mitotic figures with atypical forms
- No inflammatory infiltrate
- Dedifferentiated liposarcoma:
- Generally occurs in older patients
- Can occur in the proximal extremities, particularly proximal lower extremities
- Can show variable features, including atypical cells, myxoid areas, solid areas and some lipoblastic cells that may resemble myxoinflammatory fibroblastic sarcoma
- Can be separated by identifying MDM2 amplification or residual areas of well differentiated liposarcoma
- Rosai-Dorfman disease:
- Emperipolesis but no intranuclear viral-like inclusions
- S100+
- Usually not myxoid
- Inflammatory myofibroblastic tumor:
- Can show spindled to epithelioid neoplastic cells with prominent admixed inflammatory infiltrates, particularly plasma cells
- Characterized by ALK rearrangements
Board review style question #1
A 43 year old woman presents with a 4.5 centimeter, slowly enlarging, dorsally located foot mass. Resection of the specimen shows a multilobulated lesion located in the subcutaneous soft tissue with prominent myxoid areas (as shown in the picture above). Microscopic examination shows a dense inflammatory infiltrate with scattered atypical tumor cells with prominent nucleoli that resemble Reed-Sternberg cells. Which of the following is the most likely diagnosis?
- High grade osteosarcoma
- Hodgkin lymphoma
- Inflammatory myofibroblastic tumor
- Myxoinflammatory fibroblastic sarcoma
- Undifferentiated pleomorphic sarcoma
Board review style answer #1
D. Myxoinflammatory fibroblastic sarcoma. Of the other entities listed, only Hodgkin lymphoma has Reed-Sternberg cells; however, it would not present as a subcutaneous foot mass.
Comment Here
Reference: Myxoinflammatory fibroblastic sarcoma
Comment Here
Reference: Myxoinflammatory fibroblastic sarcoma
Board review style question #2
Which of the following is the most common genetic alteration identified in myxoinflammatory fibroblastic sarcoma?
- BRAF rearrangements
- MDM2 amplification
- t(1;10)(p22;q24)
- t(2;6)
- VGLL3 amplification
Board review style answer #2
E. VGLL3 amplification. VGLL3 is the most common genetic alteration identified; approximately 40% of cases.
Comment Here
Reference: Myxoinflammatory fibroblastic sarcoma
Comment Here
Reference: Myxoinflammatory fibroblastic sarcoma