Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Hart J. Chordoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonechordoma.html. Accessed March 31st, 2025.
Definition / general
- Malignant tumor with notochordal differentiation
- 3 types:
- Conventional chordoma: ~95% of cases; chondroid chordoma is a subtype of conventional chordoma (World Neurosurg 2017;104:346)
- Poorly differentiated chordoma (very rare): cohesive sheets of epithelioid cells with eosinophilic cytoplasm and loss of INI1 staining; positive for brachyury
- Dedifferentiated chordoma (< 1% of chordomas): a biphasic tumor composed of a conventional chordoma with high grade sarcomatous transformation (usually high grade undifferentiated pleomorphic sarcoma or osteosarcoma); poor prognosis
- Chordoma periphericum is a primary soft tissue chordoma and is very rare
Essential features
- Typically involves the clivus, sacrococcygeal bones or vertebrae
- Chords, sheets and individual cells, including cells with bubbly cytoplasm (physaliphorous cells), arranged in lobules set in a myxoid matrix
- Positive for cytokeratin, EMA, S100 protein and brachyury
- Poorly differentiated chordoma demonstrates loss of INI1
ICD coding
Epidemiology
- 1 - 5% of primary malignant bone tumors (Orthop Clin North Am 1989;20:417)
- Most commonly arises in the 40 - 60 year old age group (may occur at any age) (Cancer Causes Control 2001;12:1)
- Male predominance (~2:1) in sacrococcygeal and vertebral body cases; no sex difference in tumors involving the skull base
- Poorly differentiated chordoma usually affects children and young adults with a female (~2:1) predominance
Sites
- Intraosseous: > 95% of cases (usually axial skeleton) (Cancer Causes Control 2001;12:1)
- Base of skull / clivus of occipital bone
- Vertebral bodies
- Sacrococcygeal bones
- Extra-axial skeleton (rare)
- Soft tissue (chordoma periphericum): rare (Skeletal Radiol 2013;42:1451)
- Children and young adults: usually cranial chordoma
- Poorly differentiated chordoma: clivus or cervical spine (most cases); rare sacrococcygeal cases reported
Pathophysiology
- Most cases are sporadic but rare cases may be associated with benign notochordal tumor (Br J Radiol 2010;83:e49)
- T gene (brachyury) duplication (6q27)
- T box transcription factor involved in mesodermal differentiation during gastrulation (formation of 3 germ layers), including notochordal development (Development 2014;141:3819)
- 7% of sporadic chordomas
- Familial associated tumors (autosomal dominant) are rare; they are associated with T gene duplication
- Rare cases associated with tuberous sclerosis; biallelic inactivation of TSC1 or TSC2 identified in the cases analyzed (Neurosurg Clin N Am 2015;26:437, Nat Rev Mol Cell Biol 2009;10:307)
Diagnosis
- Diagnosis is based on morphology, immunohistochemical findings and anatomic location of the tumor
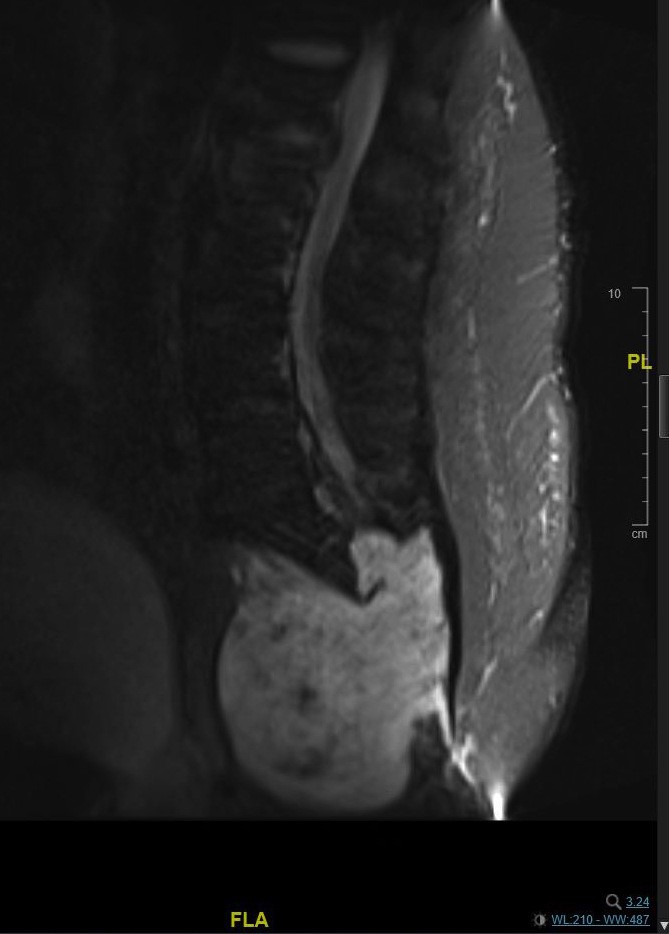
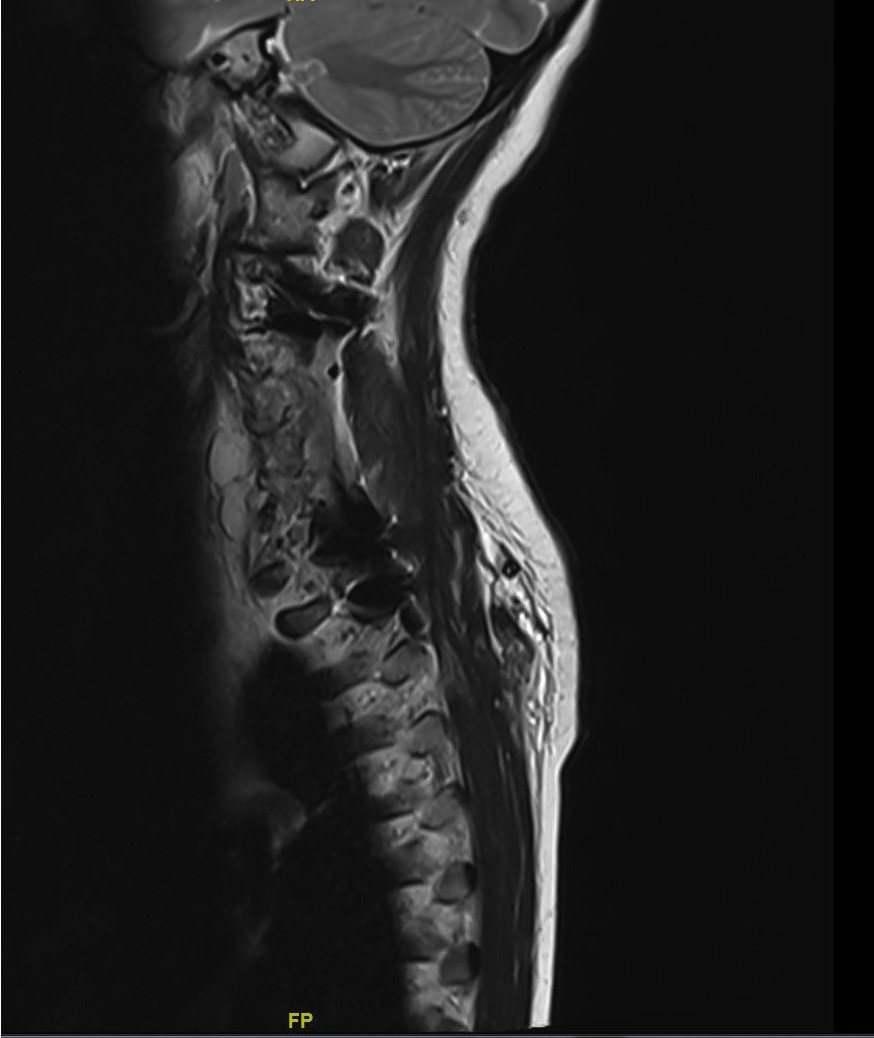
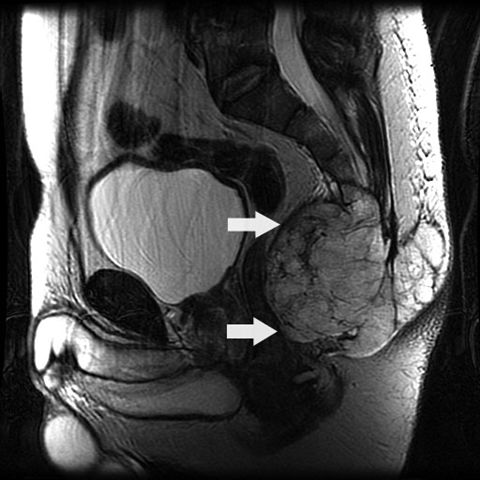
Radiology description
- Lytic bone tumor with osseous destruction and soft tissue invasion
- T2 weighted MRI demonstrates high signal intensity (AJR Am J Roentgenol 2011;196:644)
Radiology images
Prognostic factors
- Median survival is 7 years
- 5 year overall and disease free survival are 61% and 71%; 10 year overall and disease free survival are 41% and 57% (World Neurosurg 2017;104:346)
- Worse prognosis in cranial cases
- Approximately 40% of noncranial tumors metastasize (lung, bone, lymph nodes, subcutaneous tissue)
- Poorly differentiated chordoma has a worse prognosis than conventional chordoma and dedifferentiated chordoma has a worse prognosis than conventional and poorly differentiated chordoma
Case reports
- 36 year old man with chordoma of distal ulna (chordoma periphericum) (Am J Surg Pathol 2001;25:263)
- 47 year old Caucasian man with persistent pain in the low back area (Case #110)
- 58 year old man with clival dedifferentiated chordoma (Anal Quant Cytopathol Histpathol 2014;36:330)
- 67 year old woman with a poorly differentiated chordoma of the distal femur (Histopathology 2020;76:924)
- 71 year old man with lumbosacral tumor with high grade malignant cartilaginous and spindle cell components (Am J Surg Pathol 1990;14:384)
- 72 year old man with giant lumbar chordoma (Medicine (Baltimore) 2018;97:e11128)
- 77 year old woman with clival chordoma (Pol J Radiol 2017;82:670)
- Patient with spheno-occipital tumor evolving to an acute pontocerebellar hemorrhage (Arch Pathol Lab Med 1989;113:1075)
- 2 cases of poorly differentiated chordoma in the clivus of pediatric patients (Neuropathology 2018;38:47)
Treatment
- Usually surgery followed by radiation or radiation alone in poor surgical candidates (J Orthop 2018;15:679, Int J Radiat Oncol Biol Phys 2006;65:1514)
- Poor response to chemotherapy
- Tyrosine kinase inhibitors have been used in advanced cases (Eur J Cancer 2017;79:119)
- Ongoing clinical trials include CDK4/6 inhibitors, inhibitors of chromatin remodeling enzymes (in INI1 deficient tumors), PD1 / LAG3 inhibitors and brachyury therapeutic vaccines in combination with radiotherapy
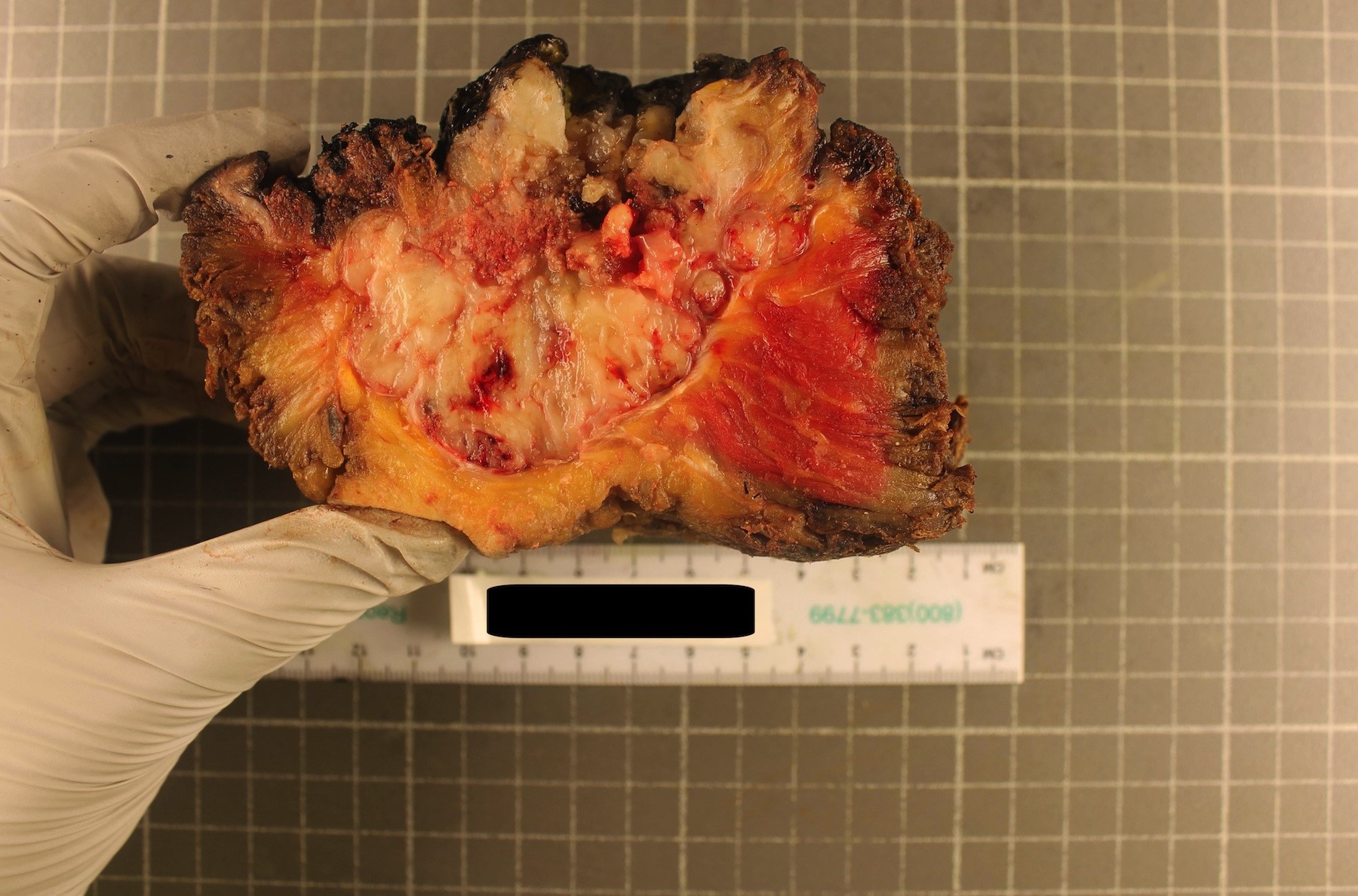
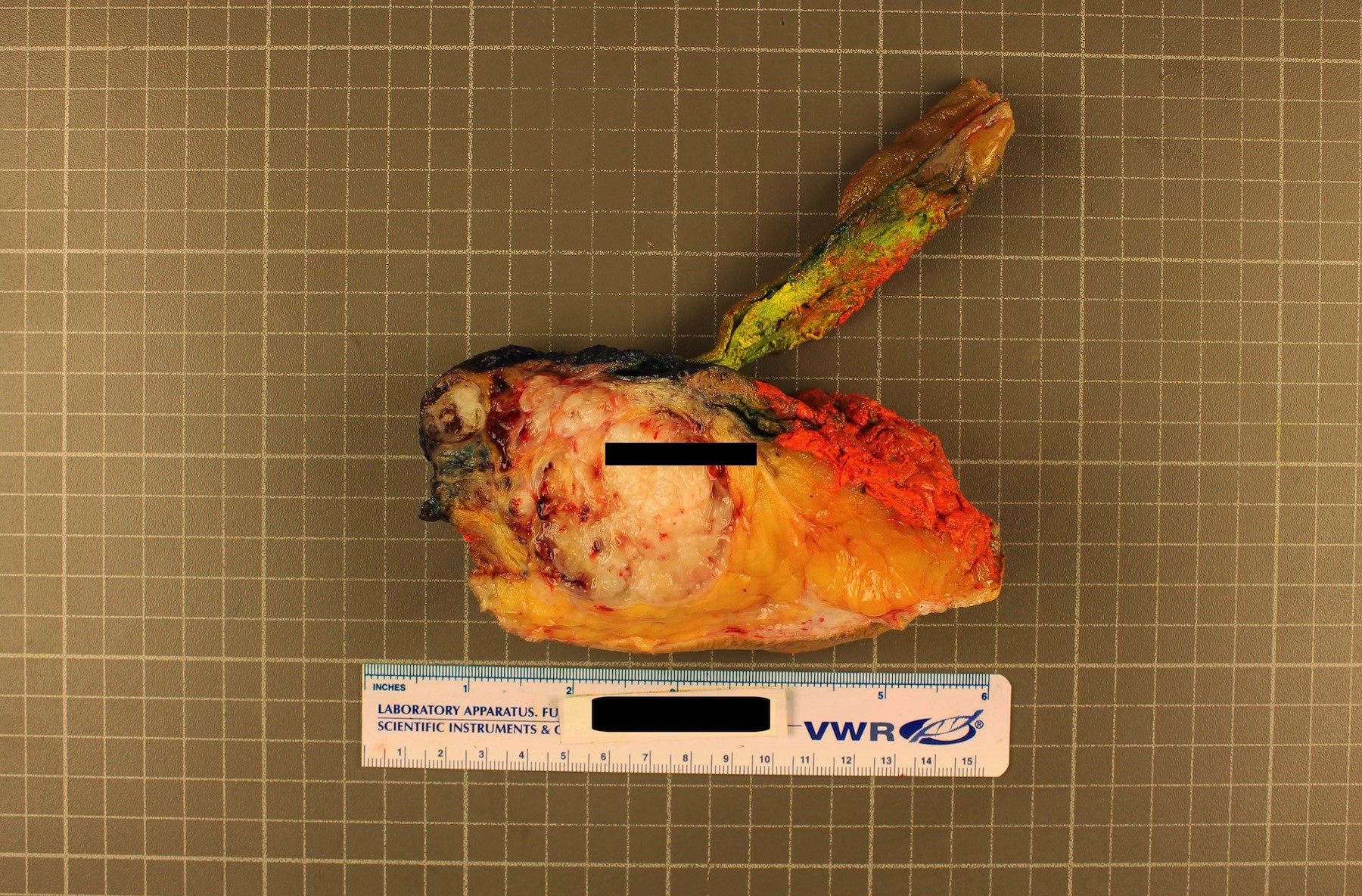
Gross description
- Expansile lobulated intraosseous mass that usually permeates the cortex and invades adjacent soft tissue
- 2 - 22 cm in greatest dimension
- Cut surface is gelatinous to chondroid
- Reference: Arch Pathol Lab Med 2021 Jul 28 [Epub ahead of print]
Gross images
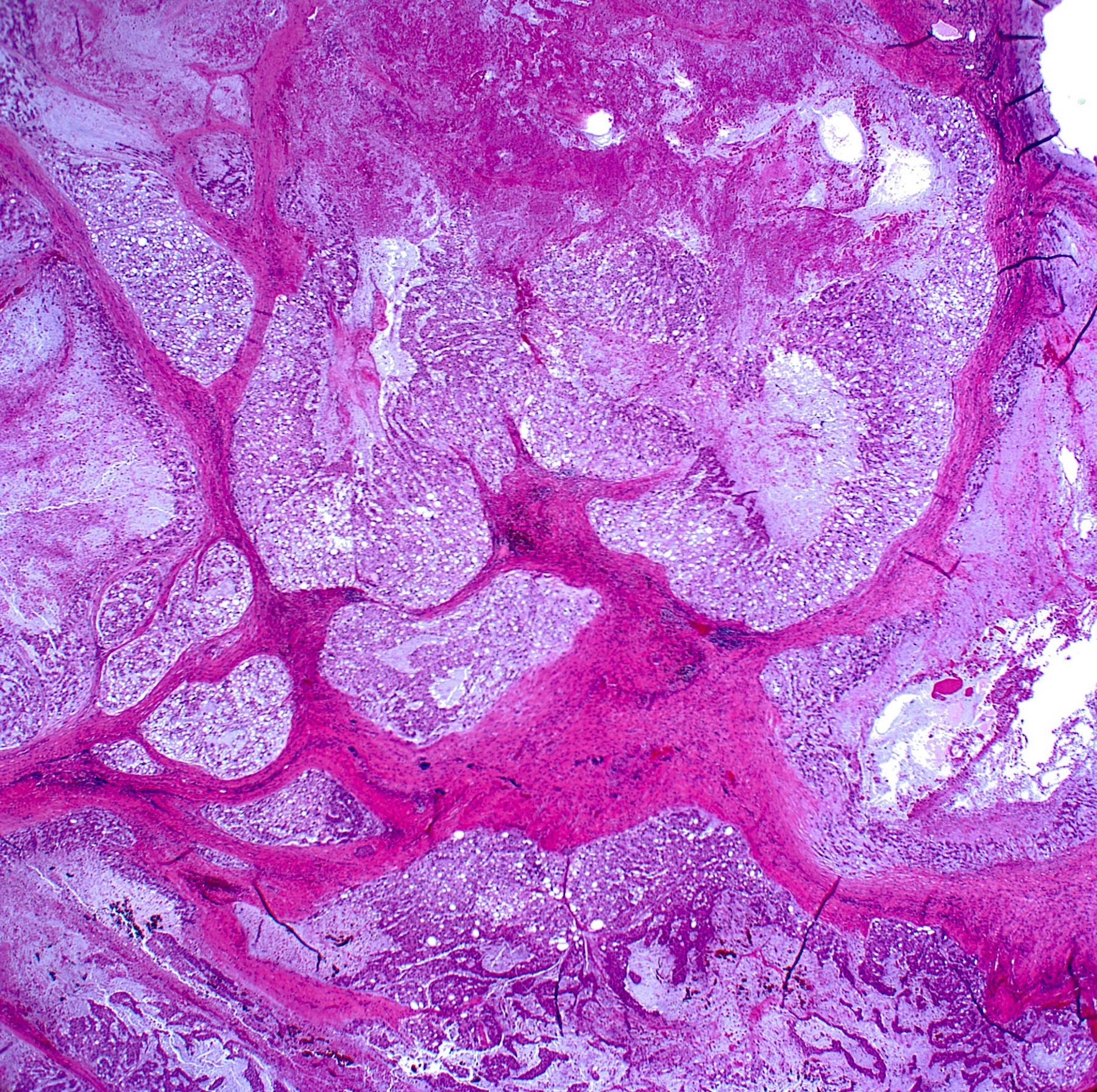
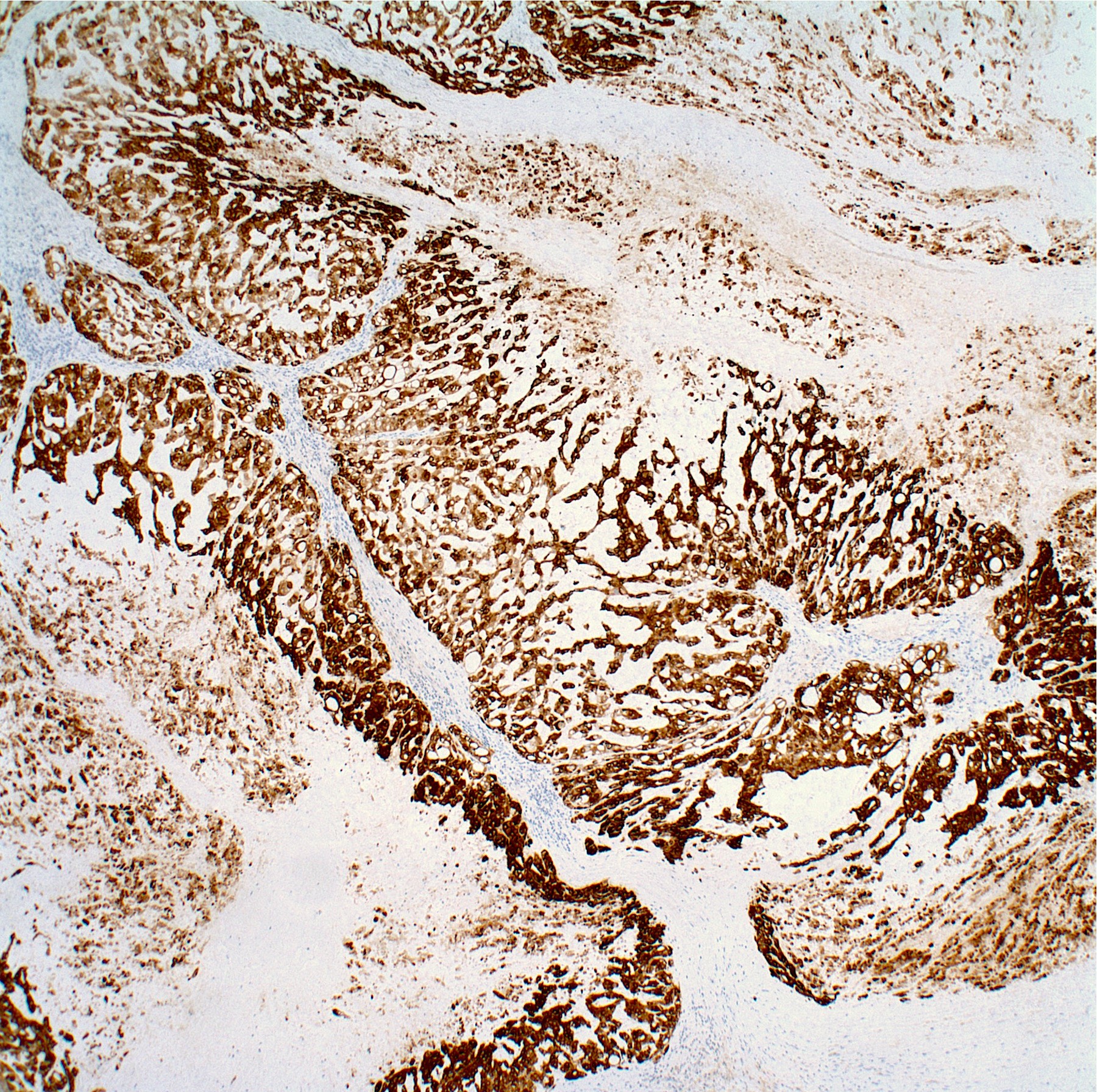
Microscopic (histologic) description
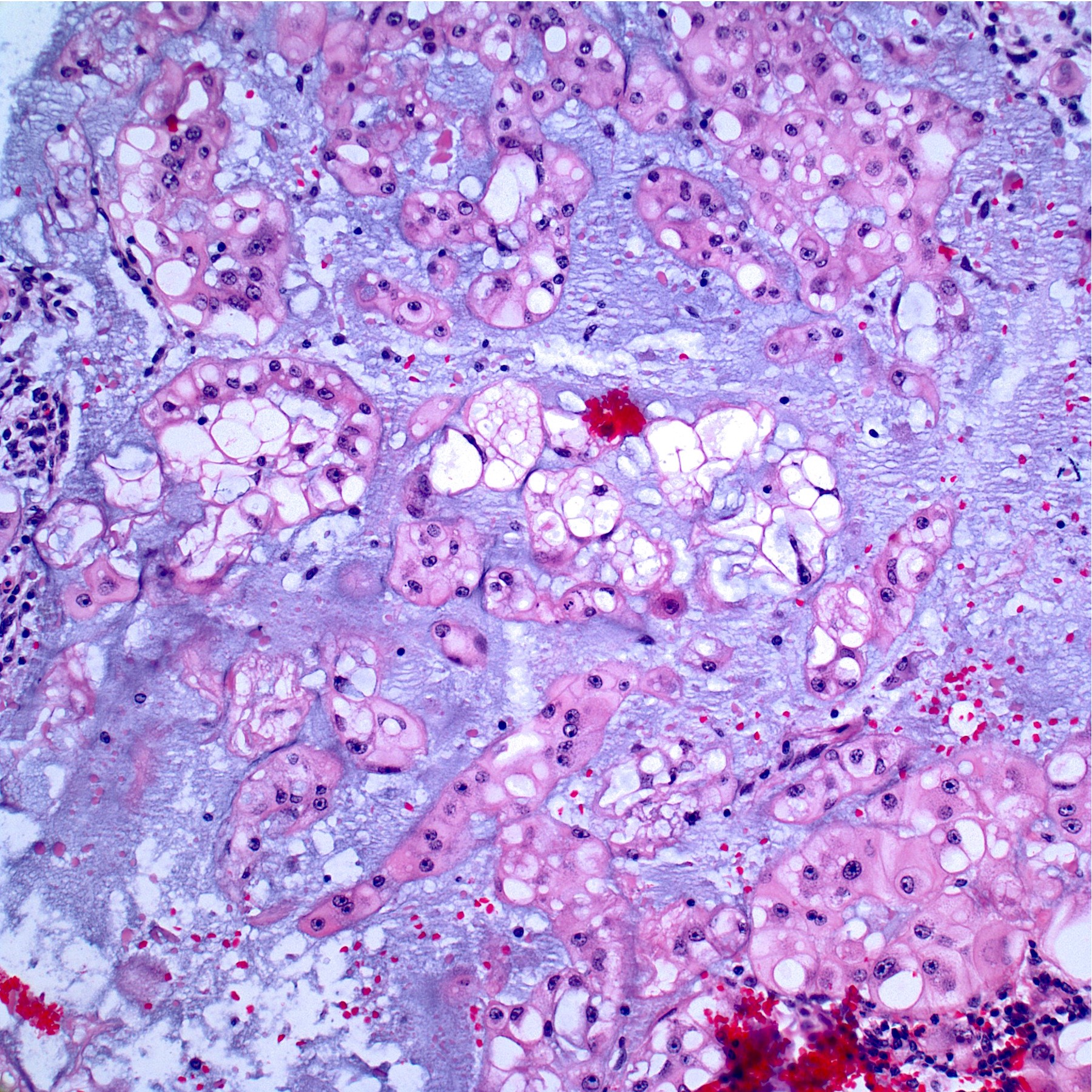
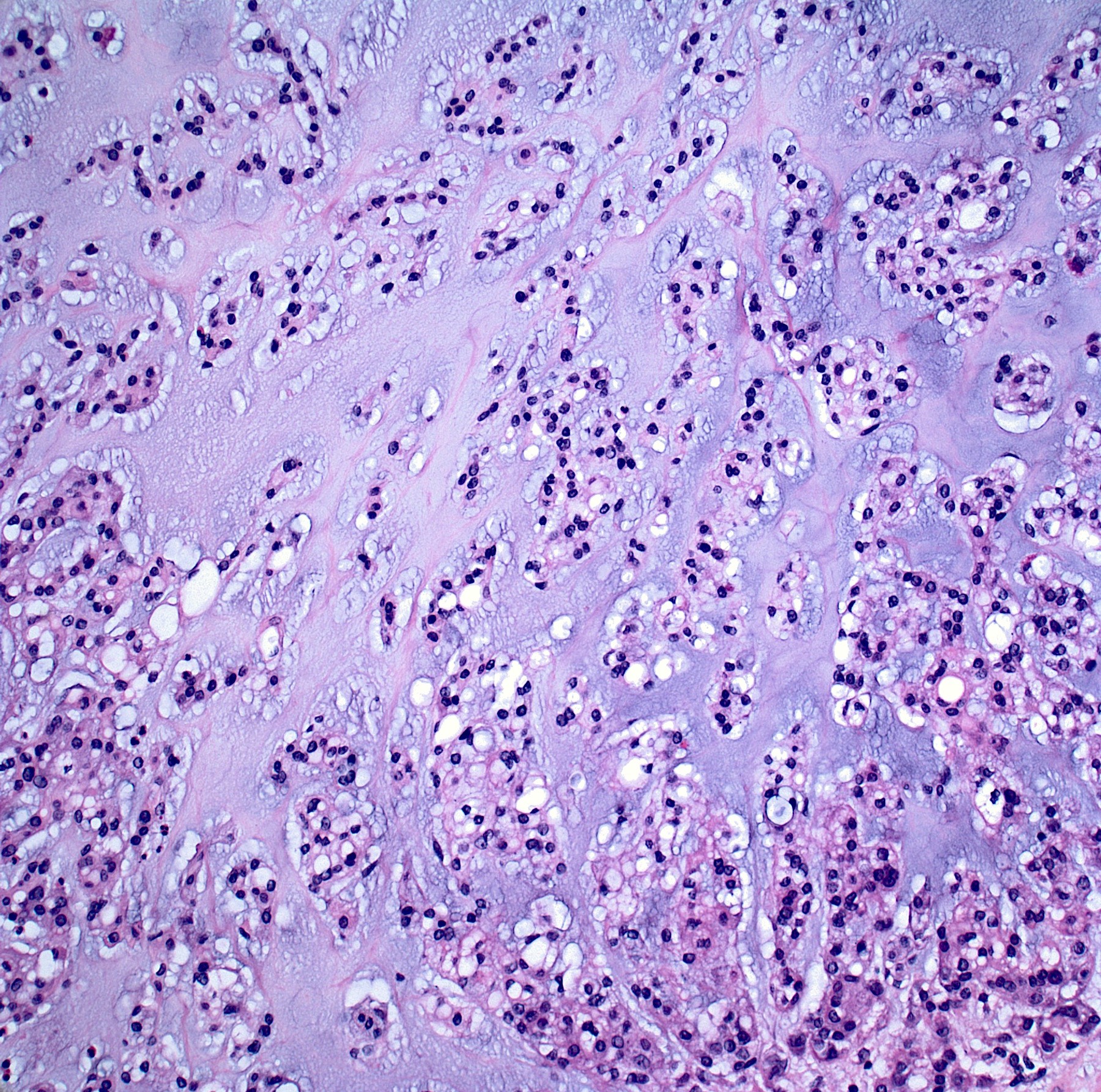
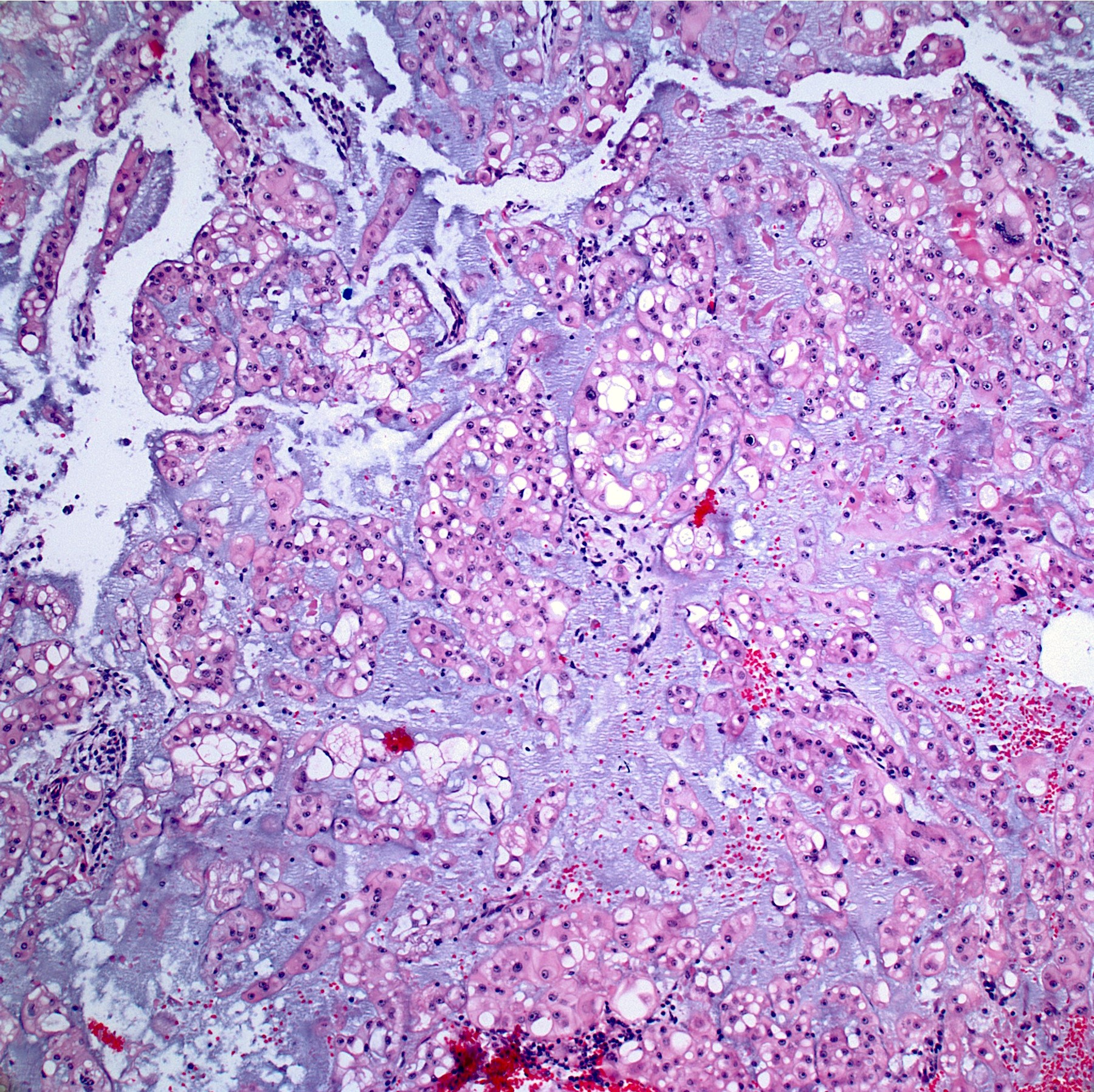
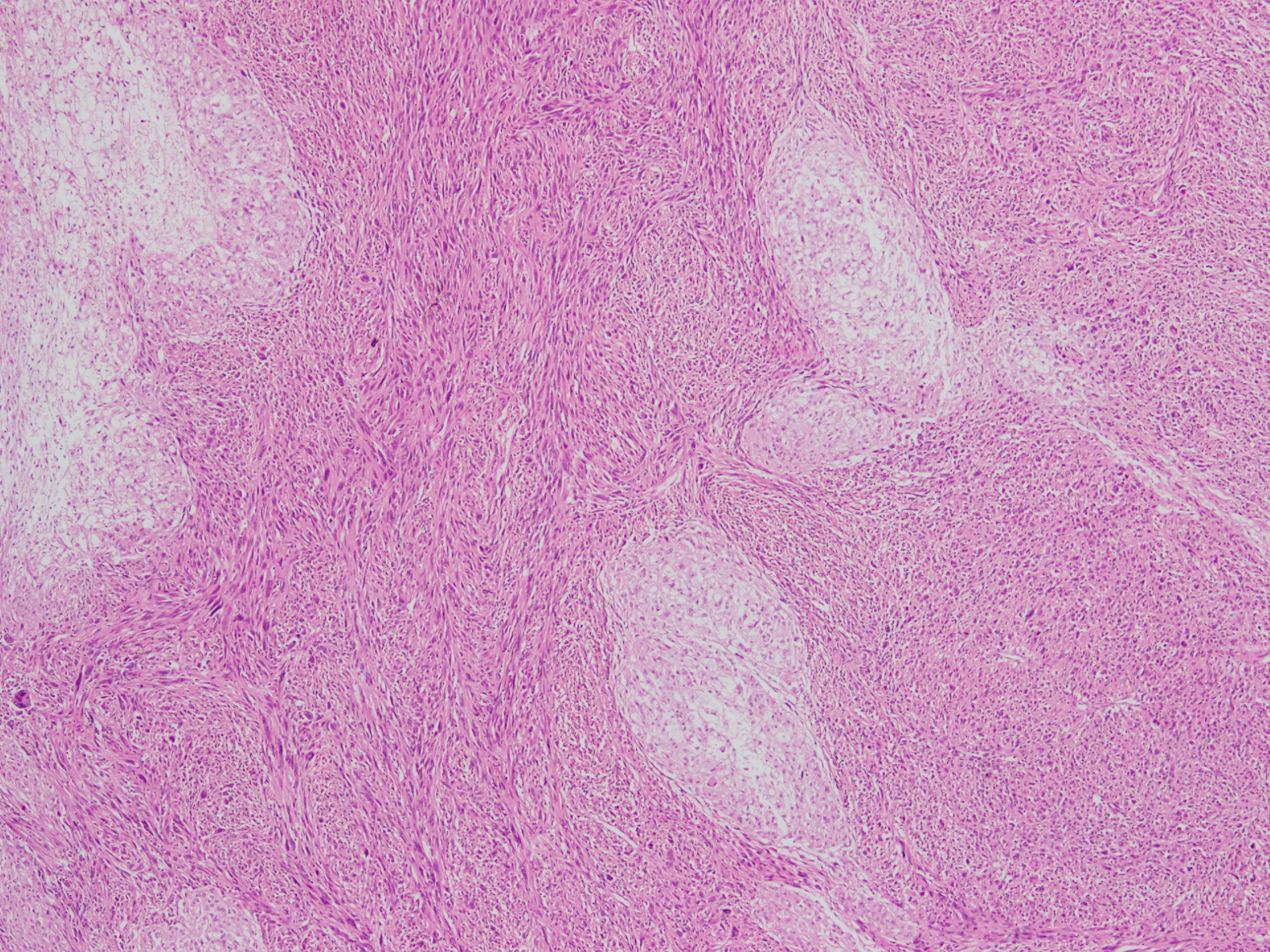
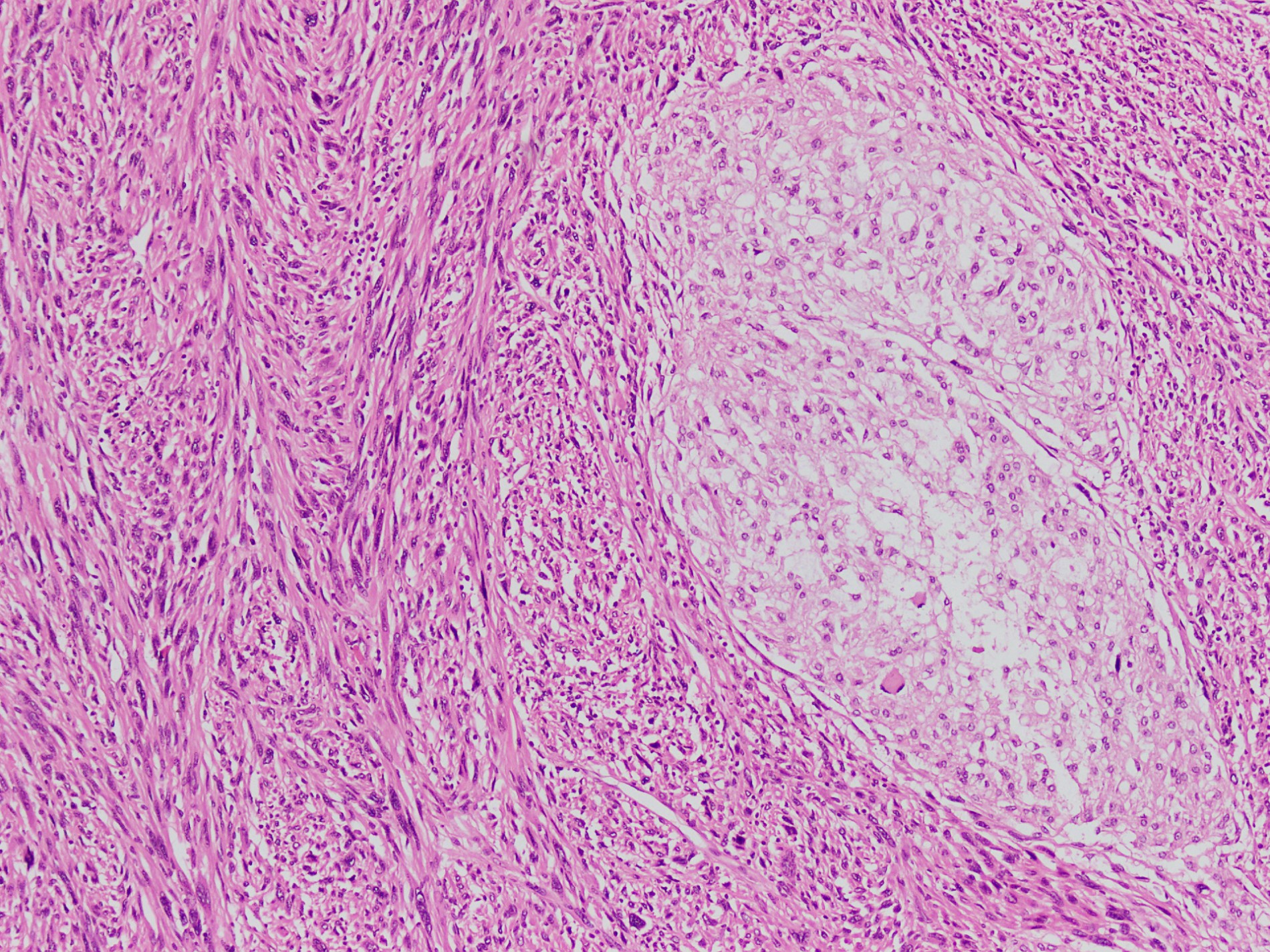
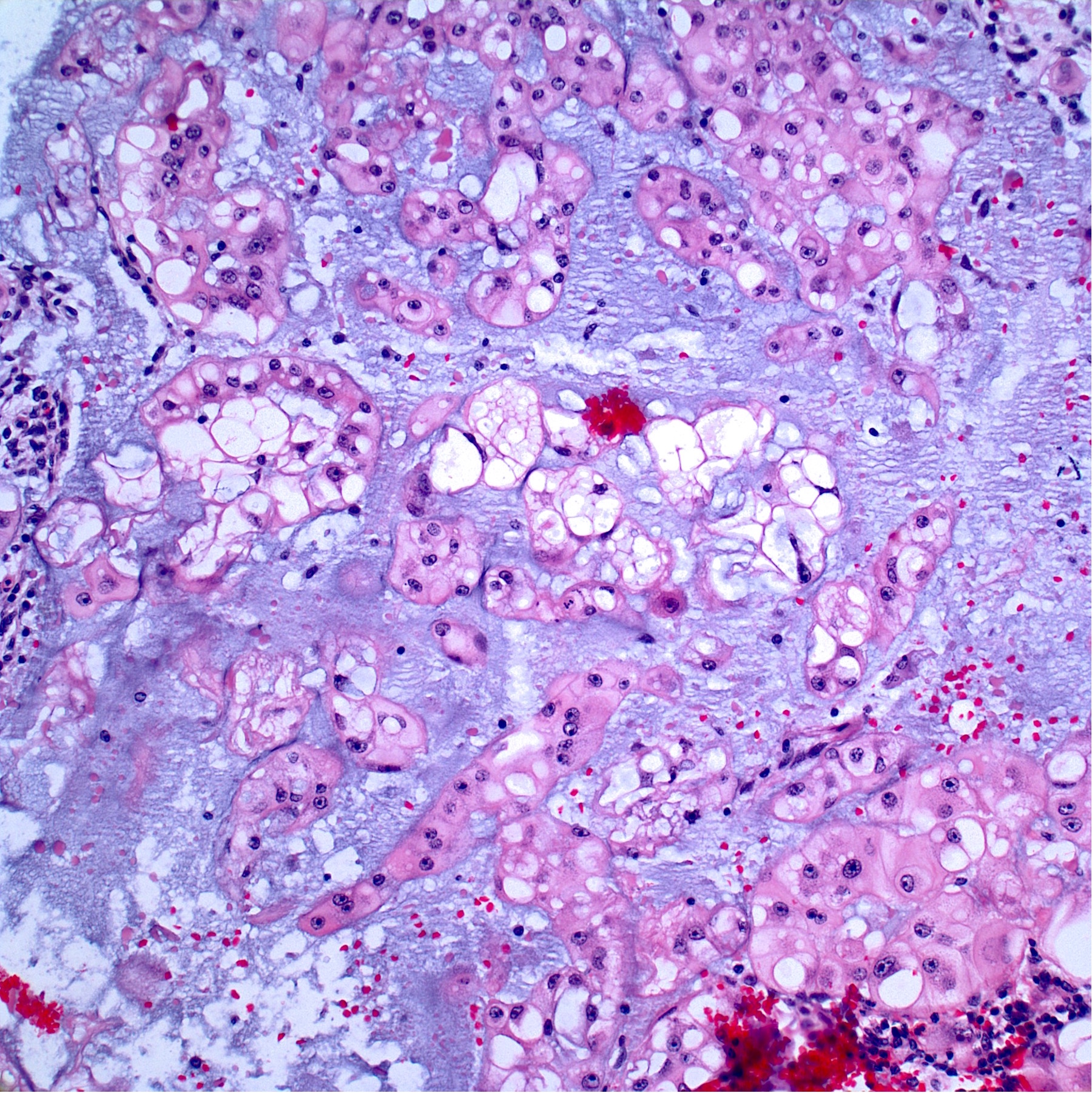
- Conventional chordoma:
- Infiltrative border
- Low power architecture is lobular, with fibrous bands separating lobules
- Cytoarchitecture (within the lobules) consists of cells forming short chords, dense epithelioid sheets / nests and single cells within the matrix
- Extracellular myxoid matrix
- Cells are epithelioid with abundant clear (glycogen) to eosinophilic cytoplasm that may be have a bubbly / vacuolated appearance (physaliphorous cells)
- Nuclear pleomorphism is heterogenous throughout the neoplasm, with low grade and higher grade areas; vesicular nucleus is common; nuclear pseudoinclusions may be seen
- Mitoses usually identifiable (high grade areas)
- Necrosis may be present
- Occasionally, mitotically active spindle cells
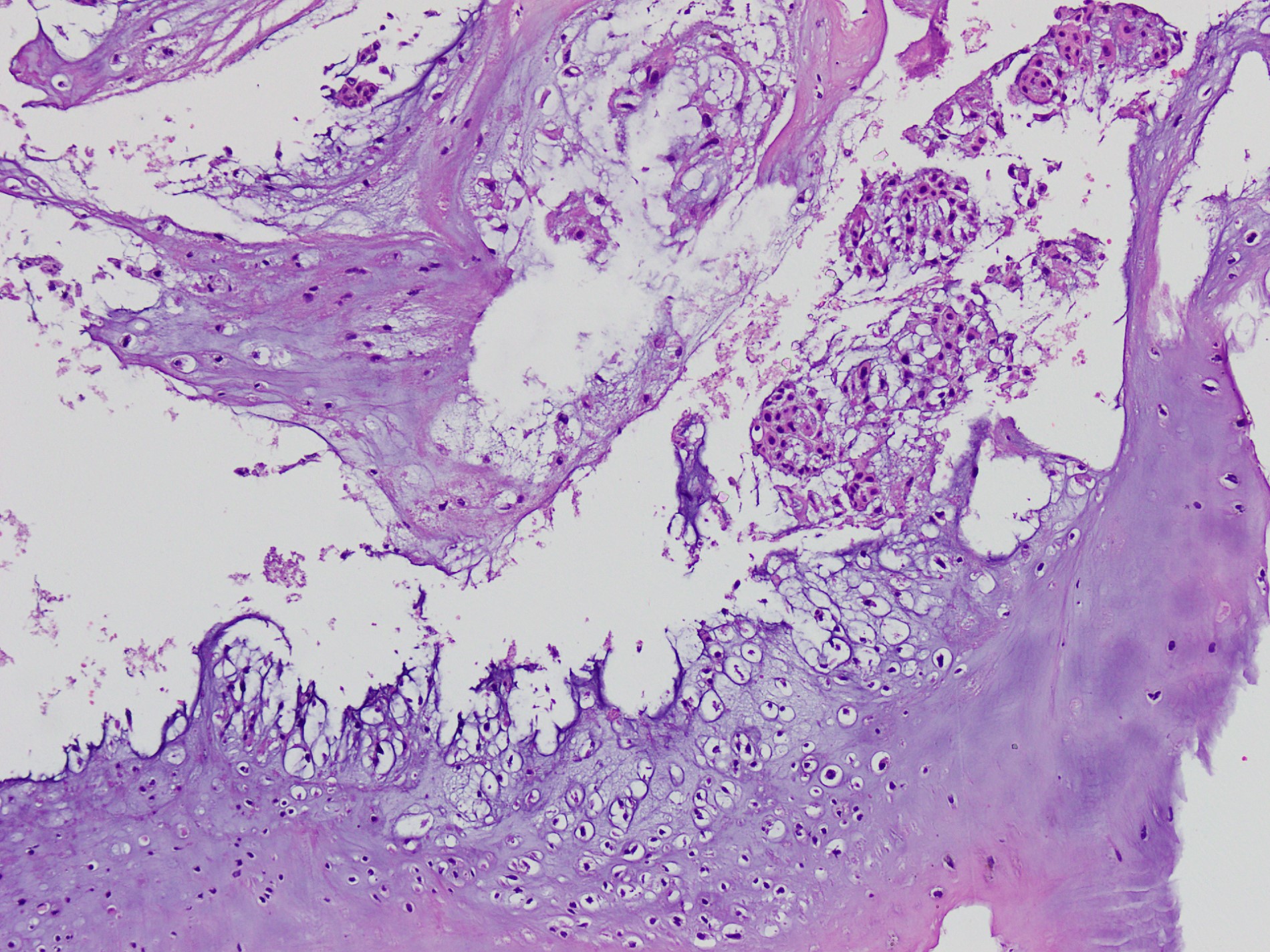
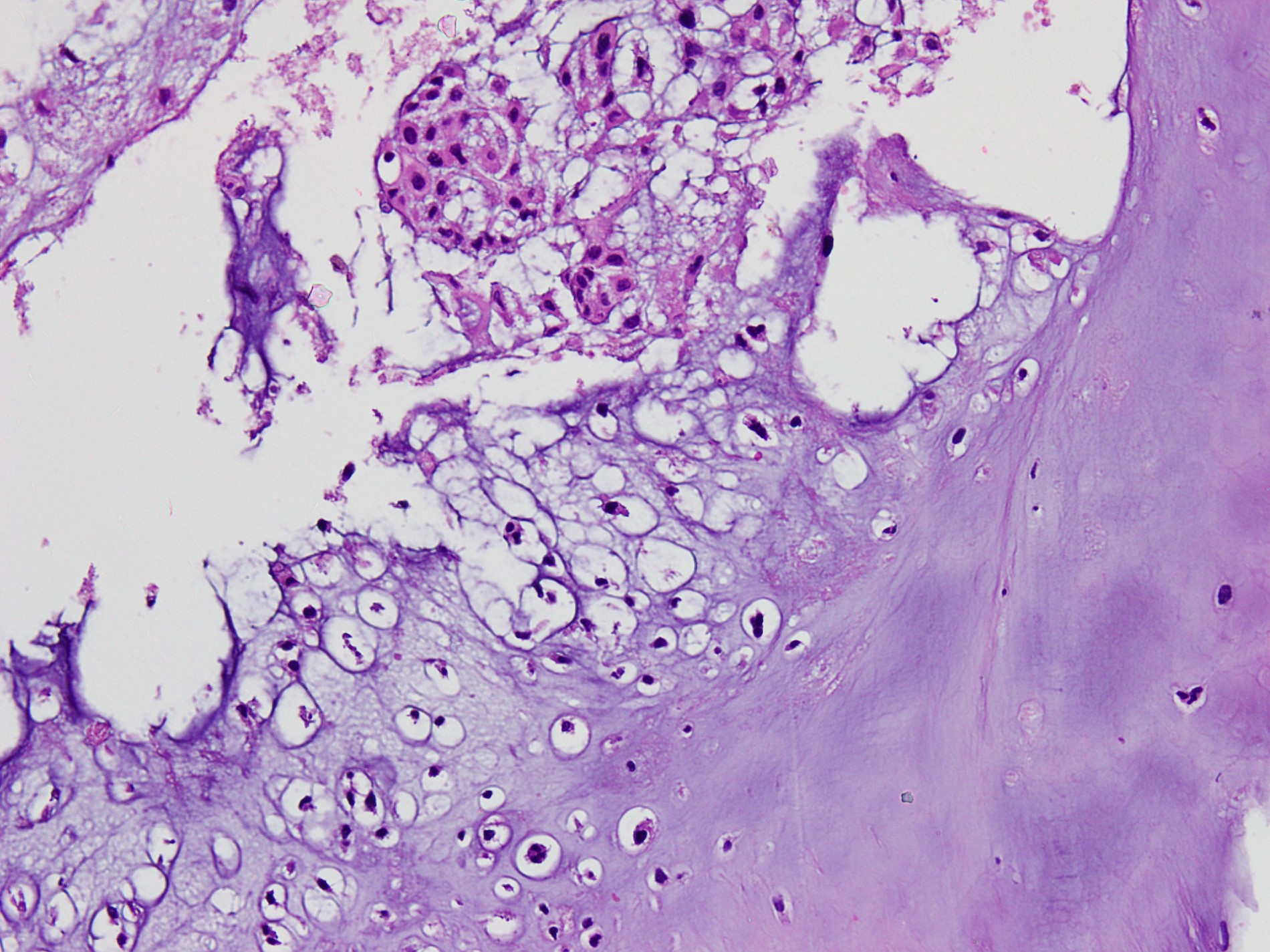
- Chondroid chordoma (a subtype of conventional chordoma):
- Matrix mimics hyaline cartilage (may be focal or extensive)
- Nearly all cases arise in the base of the skull
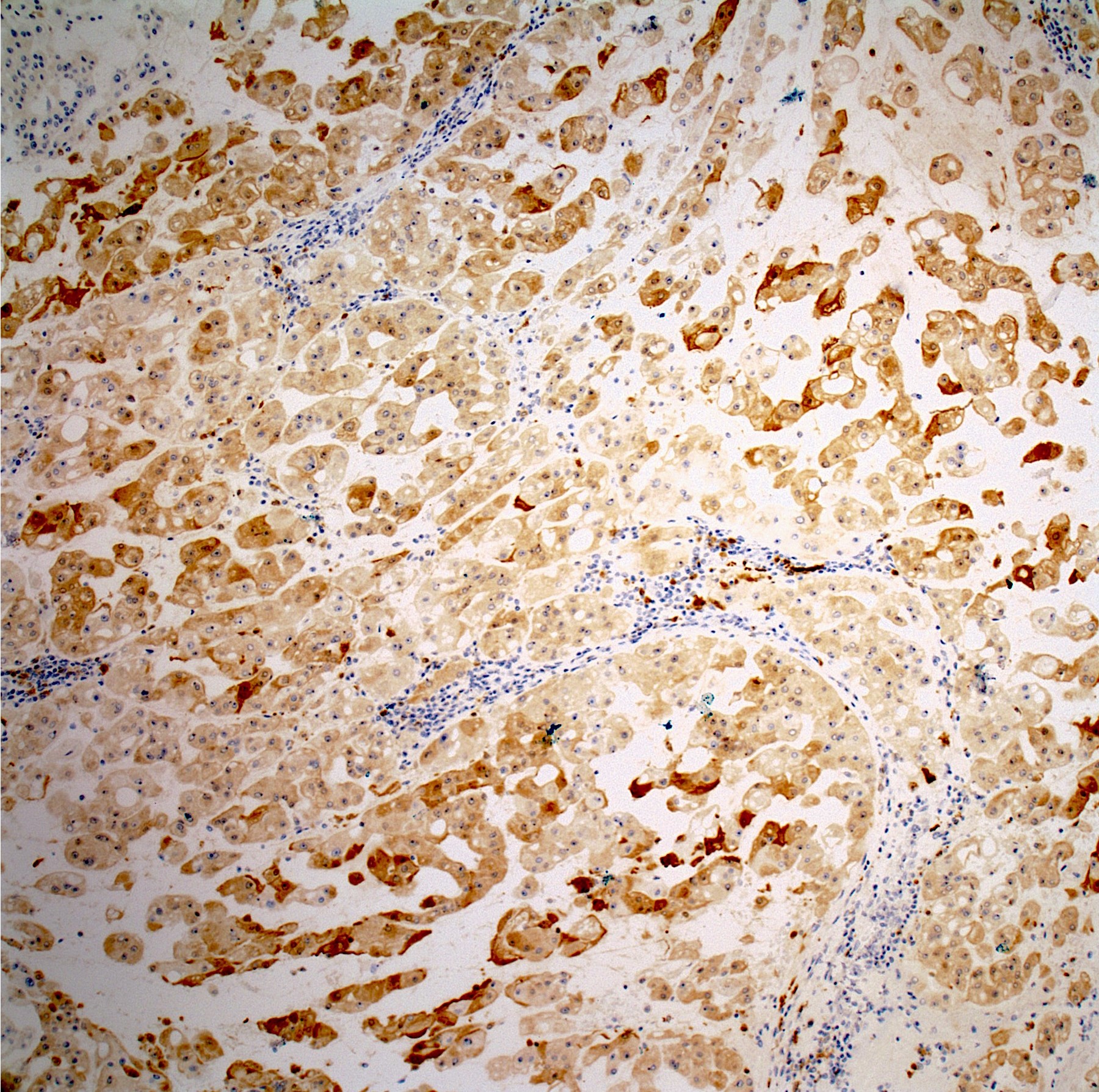
- Dedifferentiated chordoma:
- Biphasic tumor with 2 juxtaposed components (de novo):
- Conventional chordoma component
- High grade sarcomatous component (high grade undifferentiated pleomorphic sarcoma or osteosarcoma)
- May only have sarcomatous component posttreatment at a site of previously treated chordoma
- Biphasic tumor with 2 juxtaposed components (de novo):
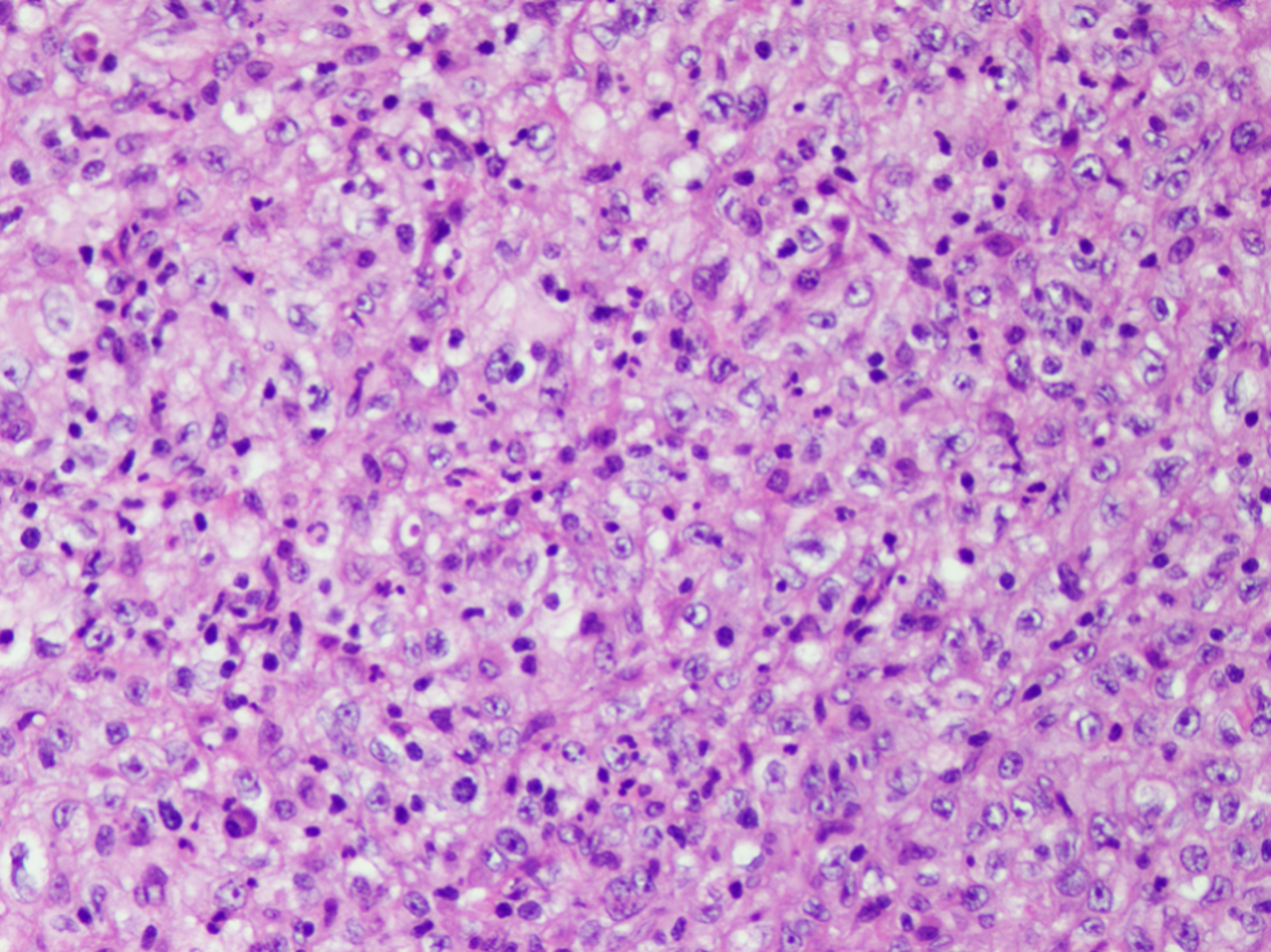
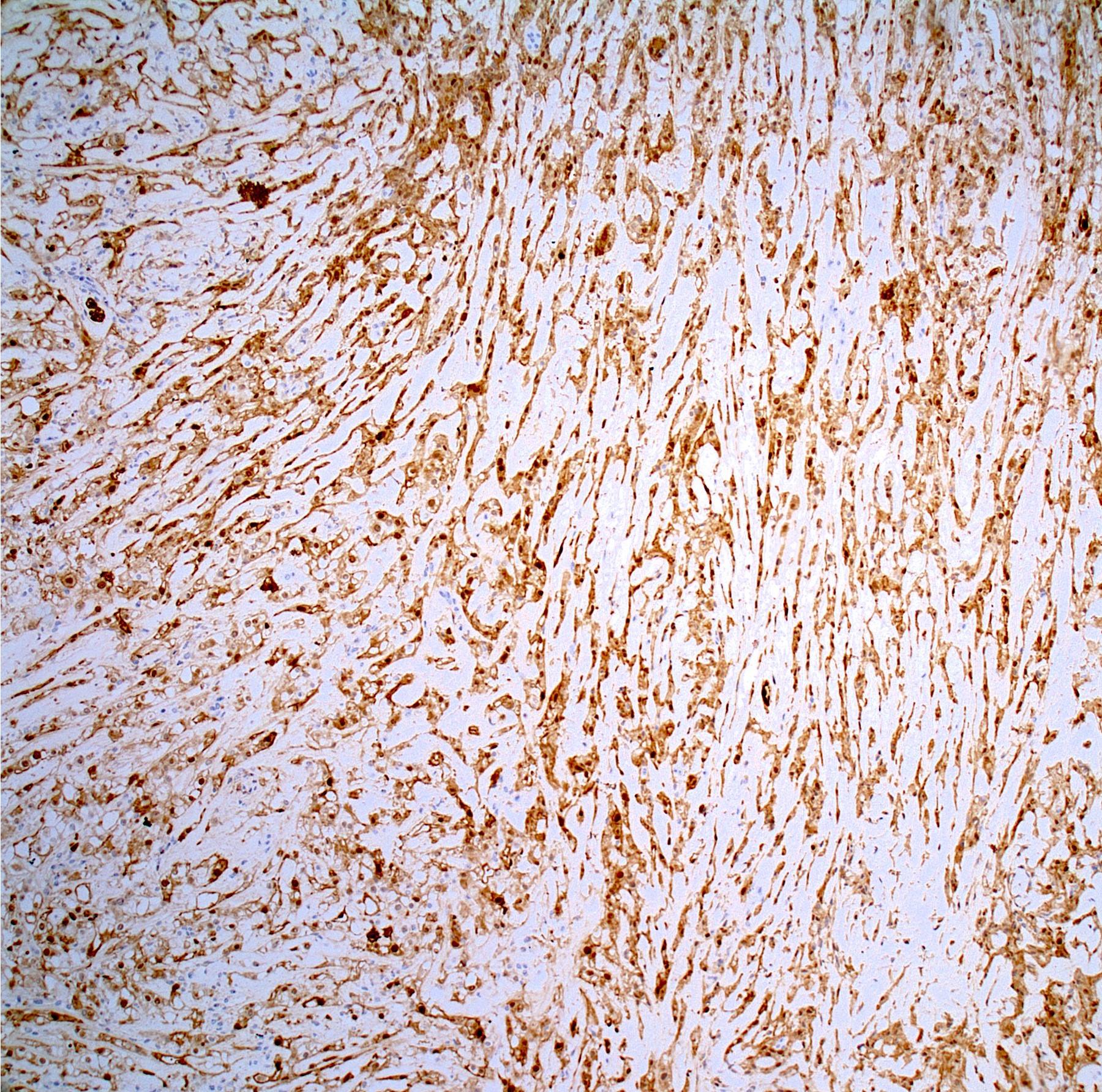
- Poorly differentiated chordoma:
- Sheets of nests of epithelioid cells with eosinophilic cytoplasm and scattered intracytoplasmic vacuoles (signet ring-like)
- Focal rhabdoid morphology is often seen
- Numerous mitotic figures
- Necrosis is common
- No physaliphorous cells and myxoid stroma is usually absent (occasional cases have focal myxoid stroma)
- Reference: Arch Pathol Lab Med 2021 Jul 28 [Epub ahead of print]
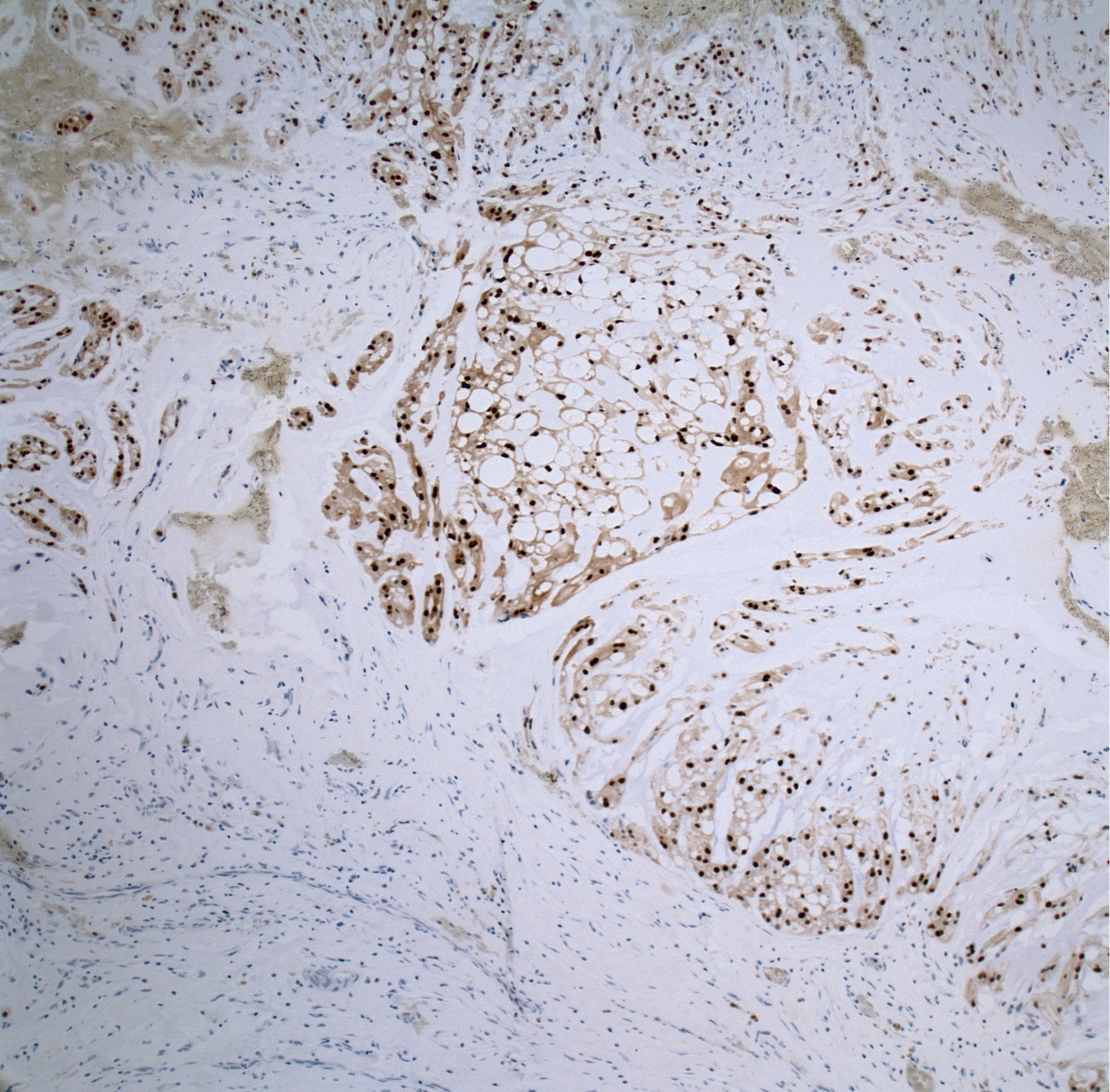
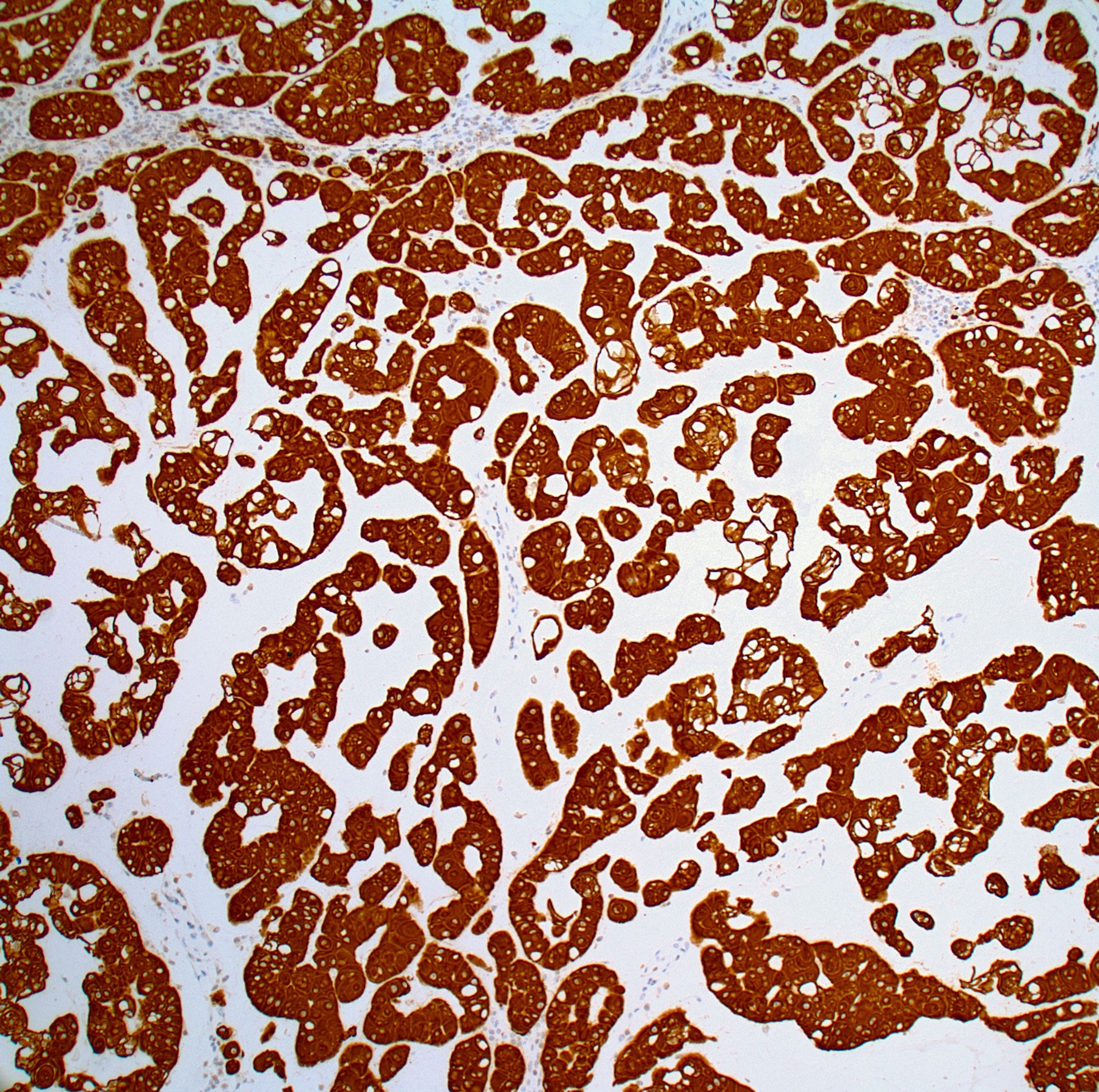
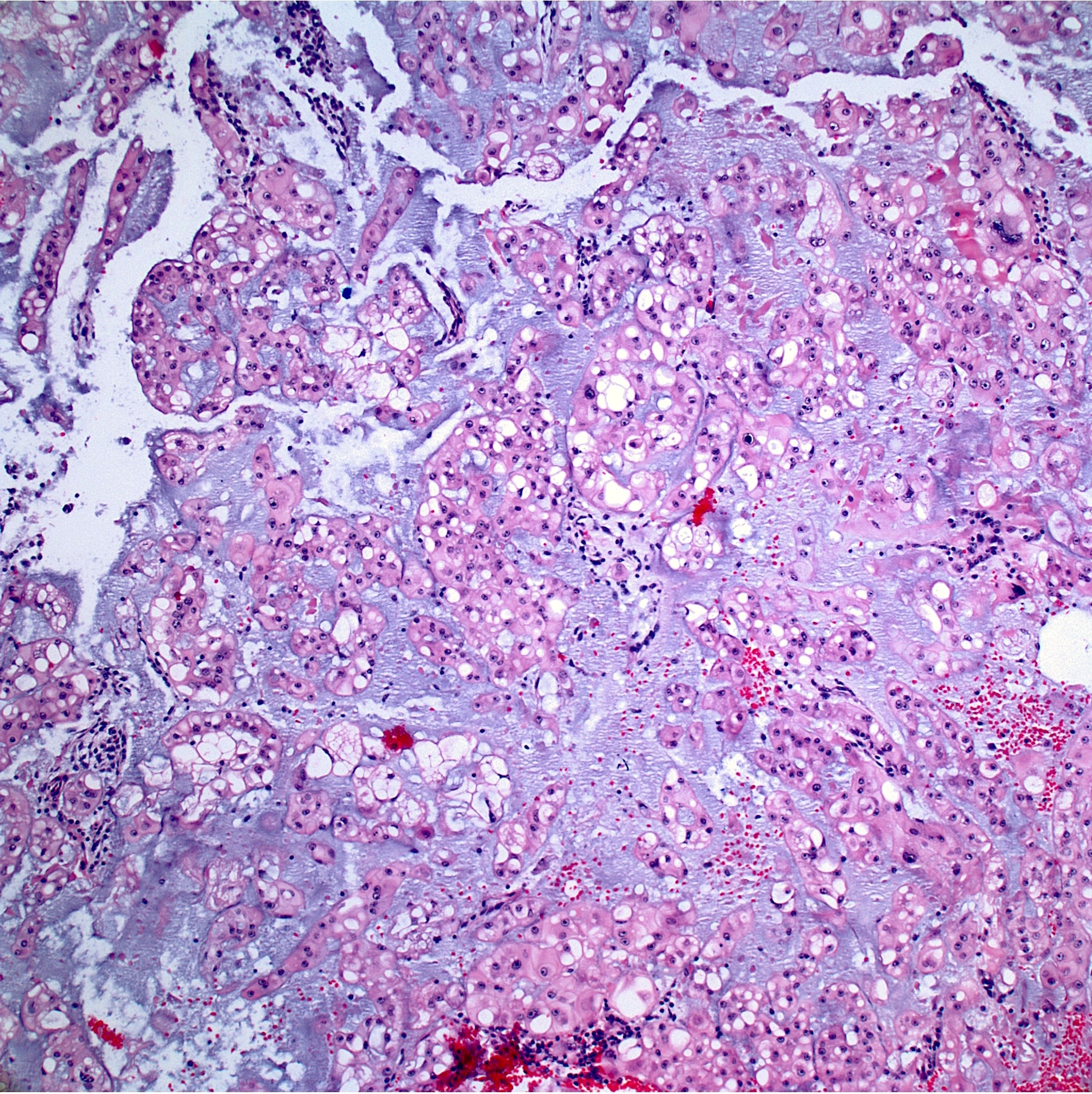
Microscopic (histologic) images
Contributed by Jesse Hart, D.O. and Nasir Ud Din, M.B.B.S.
Positive stains
- Cytokeratin cocktail (CK8, CK18, CK19), EMA, S100 protein (expressed in conventional chordoma; usually negative in poorly differentiated chordoma), brachyury (a nuclear stain, highly specific, positive in poorly differentiated chordoma)
- Decalcification may result in a loss / decrease in brachyury immunoreactivity
- Dedifferentiated component may lose brachyury, EMA or S100 protein immunoreactivity
- Reference: Arch Pathol Lab Med 2021 Jul 28 [Epub ahead of print]
Negative stains
- PTEN loss is common
- CK7, CK20
- INI1 is lost in poorly differentiated chordoma
- Reference: Arch Pathol Lab Med 2021 Jul 28 [Epub ahead of print]
Molecular / cytogenetics description
- T gene (brachyury) duplication (6q27) occurs in ~27% of sporadic chordomas; however, nearly all notochordal tumors over express brachyury (epigenetic mechanisms) (Nat Commun 2017;8:890)
- Homozygous or heterozygous loss of CDKN2A (p16, p14ARF) or CDKN2B (p15) at 9p21 seen in ~70% of cases
- EGFR amplification is common (7p12)
- Commonly activated pathways:
- EGFR
- PDGFβ
- IGFR1
- IGF1
- mTOR
- MET
- PI3K
- Chromatin remodeling genes: ARID1A, PBRM1, SETD2
- Somatic mutation in the following genes is not present:
- Brachyury
- IDH1 or IDH2
- EGFR
- KRAS
- NRAS
- HRAS
- BRAF
- FGFR1-4
- Chromothripsis is seen in a subset of sporadic chordomas, which is a genetic mechanism in which hundreds of simultaneous gene rearrangements occur, secondary to a seminal event occurring when chromosomes are condensed in mitosis (ionizing radiation, aborted apoptosis in which chromosomes have already begun to fragment, telomere dysfunction), resulting in localized chromosomal fragmentation (involving 1 or a few chromosomes) and rejoining with incorrect orientations
- Poorly differentiated chordoma: molecularly different from conventional chordoma and characterized for SMARCB1 deletion and subsequent loss of INI1 expression (Genes Chromosomes Cancer 2019;58:804)
- Poorly differentiated chordoma: heterozygous or homozygous deletions involving SMARCB1
Sample pathology report
- Cervicothoracic chordoma, en block resection including C7 - T3 laminectomies, ribs 1 - 3 and a wedge resection of the upper lobe of the left lung:
- Conventional chordoma
- Tumor size: 8.5 x 6.2 x 5.4 cm
- Extent of disease: Tumor involves the T1 and T2 vertebrae, the intervertebral disk, the adjacent soft tissue and the parietal pleura of the resected lung; neither visceral pleural nor lung parenchymal invasion are seen.
- Lymphovascular invasion: Not identified
- Dedifferentiation: Not present
- Surgical margins:
- Soft tissue margins: < 1 mm from tumor (inferior)
- Lung staple line: 5 mm from tumor
- Vertebral bone margins: Negative for tumor
- Rib margins: Negative for tumor
- Stage (AJCC, 8th edition): pT1
- Conventional chordoma
Differential diagnosis
- Chondrosarcoma:
- May be confused with chondroid chordoma but will be negative for epithelial markers (cytokeratin / EMA) and brachyury
- Unlike chordoma, chondrosarcoma may demonstrate IDH1 or IDH2 mutations
- Metastatic carcinoma:
- Usually negative for S100 protein and brachyury
- Not usually lobulated with myxoid stroma
- Usually positive for origin specific markers (PAX8 in renal cell carcinoma, TTF1 in metastatic pulmonary adenocarcinoma, etc.)
- Correlate with chest, abdomen and pelvic imaging
- Myoepithelial tumors:
- May occur in soft tissue (the differential would be with chordoma periphericum) or bone, coexpresses epithelial markers (cytokeratin / EMA) and S100 protein, may have epithelioid cells in a myxoid stroma
- Will be negative for brachyury
- May have an EWSR1 gene rearrangement (~50% of cases) (Genes Chromosomes Cancer 2010;49:1114)
- Myxopapillary ependymoma:
- Involves the sacral region but negative for epithelial markers
- Ecchordosis physaliphora:
- Hamartomatous extraskeletal lesion derived from notochordal remnants
- Extraosseous
- Polypoid mass arising on the clivus (ecchordosis physaliphora spheno-occipitalis) but may be found anywhere from the skull base to sacrum
- No lobular architecture, necrosis, conspicuous mitoses or high grade nuclei
- IHC identical to chordoma
- Benign notochordal cell tumor:
- Benign intraosseous neoplasm with notochordal differentiation
- Confined to bone (no cortical permeation)
- No lobular architecture, necrosis, conspicuous mitoses, high grade nuclei or myxoid matrix
- IHC identical to chordoma
Additional references
Board review style question #1
- A 56 year old man had a 6.2 cm sacral mass. The microscopic image is from the resection specimen. Which of the following is true about this entity?
- The tumor has a very low metastatic rate
- The tumor has the capacity to dedifferentiate
- The tumor is probably negative for EMA
- These tumors are very responsive to chemotherapy
- These tumors usually occur in the extremities
Board review style answer #1
B. This is a chordoma. The tumor has the capacity to dedifferentiate.
Comment Here
Reference: Chordoma
Comment Here
Reference: Chordoma
Board review style question #2
- A 65 year old man has a large vertebral tumor which was resected and found to express both EMA and S100 protein (image shown). His family history is negative for tumors of any type. The patient underwent adjuvant radiation therapy and is now disease free 1 year after surgery. Which of the following is most likely true?
- The patient is very unlikely to die of disease in the next 9 years
- The patient probably has hepatitis C
- The tumor has a duplication in the brachyury gene
- The tumor is positive for brachyury
- These tumors are benign and adjuvant radiation therapy was unnecessary
Board review style answer #2