Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Obeidin F, Alexiev B. Epithelioid sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissueepithelioidsarcoma.html. Accessed March 31st, 2025.
Definition / general
- A malignant mesenchymal neoplasm that exhibits epithelioid cytomorphology and a predominantly epithelial phenotype
Essential features
- Malignant epithelioid tumor occurring in pediatric and adult populations
- Unpredictable clinical course; better prognosis in pediatric patients
- Two typical morphologies, including classic type with epithelioid to spindled cells with central pseudogranulomatous architecture; and proximal type with predominant epithelioid and rhabdoid cells
- IHC: Pancytokeratin+, INI1 lost
- Molecular: Mutations in INI1/SMARCB1
Terminology
- Classic or conventional type is also known as distal type
- Proximal type is also known as large cell type
- Defunct name: sarcoma aponeuroticum
ICD coding
Epidemiology
- Rare, < 1% of all adult soft tissue sarcomas, 4 - 8% of pediatric non rhabdomyoblastic sarcomas
- Classic type epithelioid sarcoma is more common than the proximal type epithelioid sarcoma
- Classic type: Most common in adolescents and young adults, between ages 10 and 40 years; M:F = 1.9:1 (Adv Anat Pathol 2016;23:41)
- Proximal type: Middle aged to older adults, > 80% presenting between ages of 20 and 65 years; M:F = 1.6:1
Sites
- Either type may arise anywhere
- Classic type: usually distal upper extremity, > 60% arising in the fingers and hand
- Proximal type: more common in deep soft tissue, truncal tissue (including pelvic peritoneal, genital and inguinal) and buttock / hip
Pathophysiology
- Tumor of uncertain differentiation
- Structural and immunohistochemical studies suggest a multidirectional differentiation, including epithelial, histiocytic, fibroblastic, myofibroblastic, endothelial and perineural (Arch Pathol Lab Med 2009;133:814, Adv Anat Pathol 2006;13:114)
Etiology
- An association with prior trauma at the site of the tumor has been noted in up to 27% of occurrences (J Clin Aesthet Dermatol 2009;2:49)
Clinical features
- Solitary or multiple, slowly growing, usually painless, firm nodules (J Clin Aesthet Dermatol 2009;2:49)
- Lesion often results in non healing skin ulcers that have a tendency to clinically mimic other ulcerative dermal processes
Diagnosis
- Core needle biopsy for deep tumors and punch biopsy for dermal tumors
- Followed by wide resection
Radiology description
- No distinct MR imaging characteristic of this tumor that would enable early specific diagnosis
- Tumors may show variable amounts of fibrosis, granulomatous pattern, necrosis and cellularity, corresponding to variable T2-weighted signal; T1-weighted images usually isointense to muscle but may have variability due to hemorrhage or necrosis
- Suspicion should arise when presenting with multiple soft tissue nodules or persistent punched out ulcers involving the skin and subcutaneous tissues (Skeletal Radiol 2002;31:400)
Prognostic factors
- Course is often unpredictable; common to present with extensive disease, lymph node metastases or distant metastases (J Clin Aesthet Dermatol 2009;2:49)
- Adverse prognostic factors include proximal site, large size, male sex, older age, necrosis, vascular invasion, rhabdoid cytomorphology and inadequate excision (Adv Anat Pathol 2016;23:41, Adv Anat Pathol 2006;13:114)
- In adults: 5 year overall survival of 50 - 85%
- In pediatric population: better prognosis; 5 year overall survival of 92.4%, more likely to have localized, classic type morphology, fewer nodal or distant metastases at presentation (Adv Anat Pathol 2016;23:41)
- Proximal epithelioid sarcoma is an aggressive tumor; 65% of patients die of disease (Mod Pathol 2001;14:655)
Case reports
- 12 year old girl with a slow growing, deep and asymptomatic mass on right buttock (Pediatr Dermatol 2004;21:117)
- 41 year old woman with rapidly growing mass in the right mons pubis (Ann Diagn Pathol 2012;16:411)
- 47 year old woman with an abnormal, lobulated and lumpy signal in the intrasellar region, suprasella and sphenoid sinus (Pathol Oncol Res 2019;25:201)
- 50 year old man with scrotal mass (Eur Urol 2006;49:406)
- 80 year old man with a painful swollen mass in his scalp (Int J Clin Exp Pathol 2019;12:3908)
Treatment
- Wide surgical excision remains the mainstay of treatment (Am J Surg 2008;196:407)
- Systemic chemotherapy provides satisfactory palliation but response is of short duration (Adv Anat Pathol 2016;23:41)
- Relapse rates remain high despite multimodal therapy (Adv Anat Pathol 2016;23:41)
Gross description
- Classic subtype usually presents as one or more indurated, ill defined, dermal or subcutaneous nodules (Cancer 1970;26:1029)
- Deep seated tumors are multinodular masses and involve tendons or fascia
- Cut surface is glistening with gray-white or gray-tan color and multiple areas of hemorrhage and necrosis (Arch Pathol Lab Med 2009;133:814)
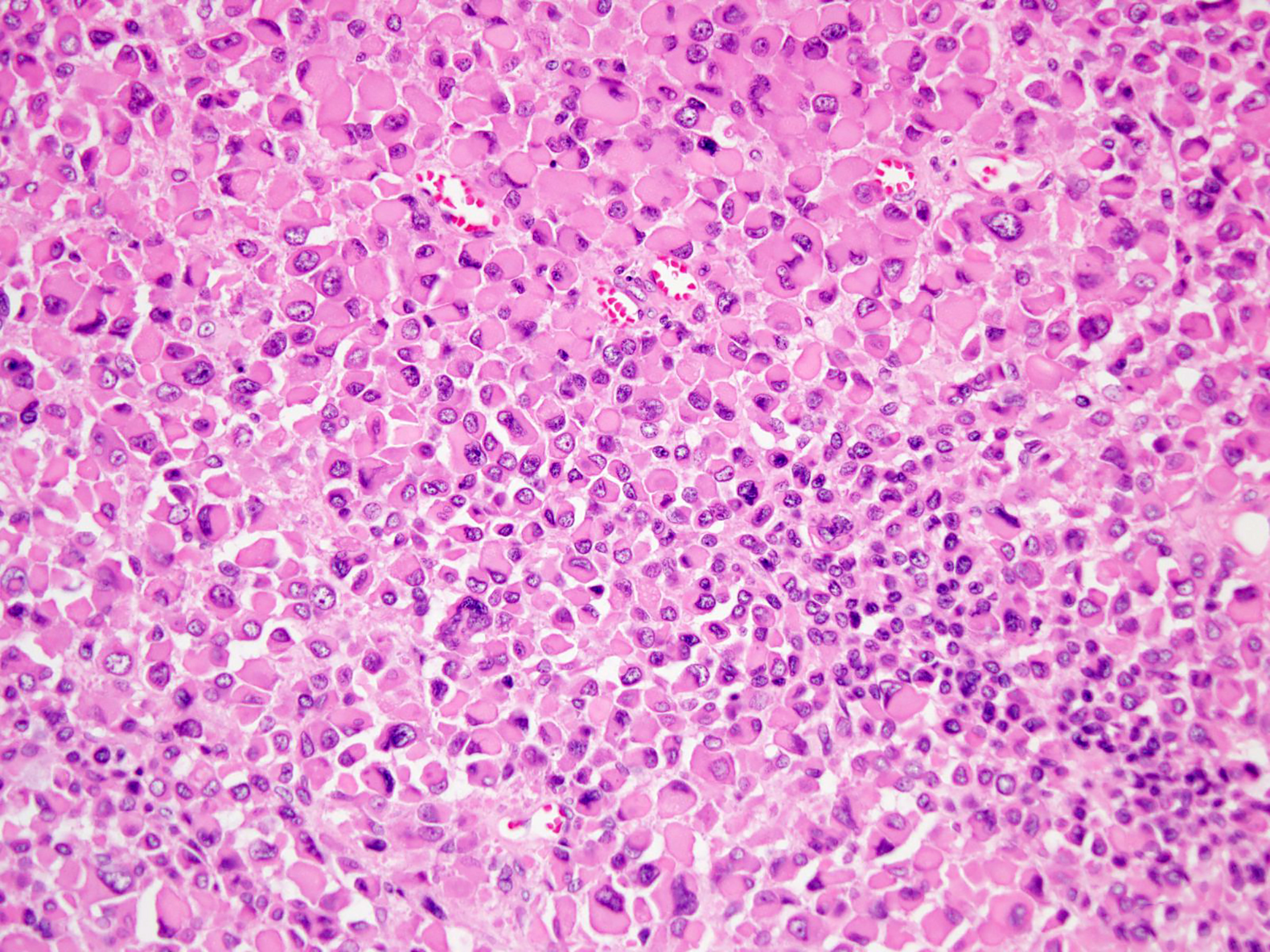
Microscopic (histologic) description
- Classic and proximal epithelioid sarcoma can each occur in either proximal or distal sites and may show features of both types (Histopathology 2001;39:641)
- Classic or conventional, distal type (Adv Anat Pathol 2006;13:114)
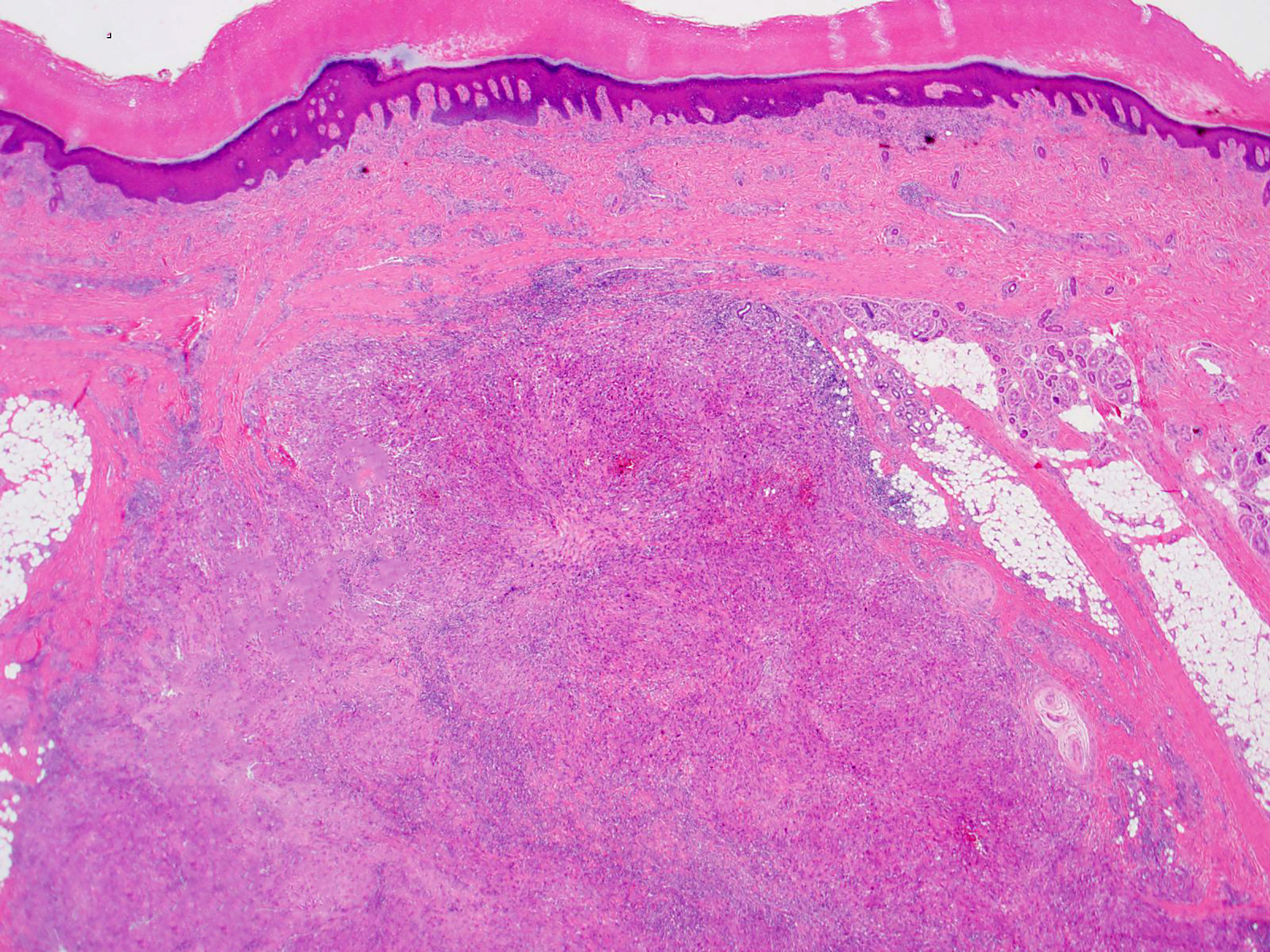
- Dermal / subcutaneous nodule(s)
- Can simulate granulomatous process, with or without necrosis (pseudogranulomatous morphology)
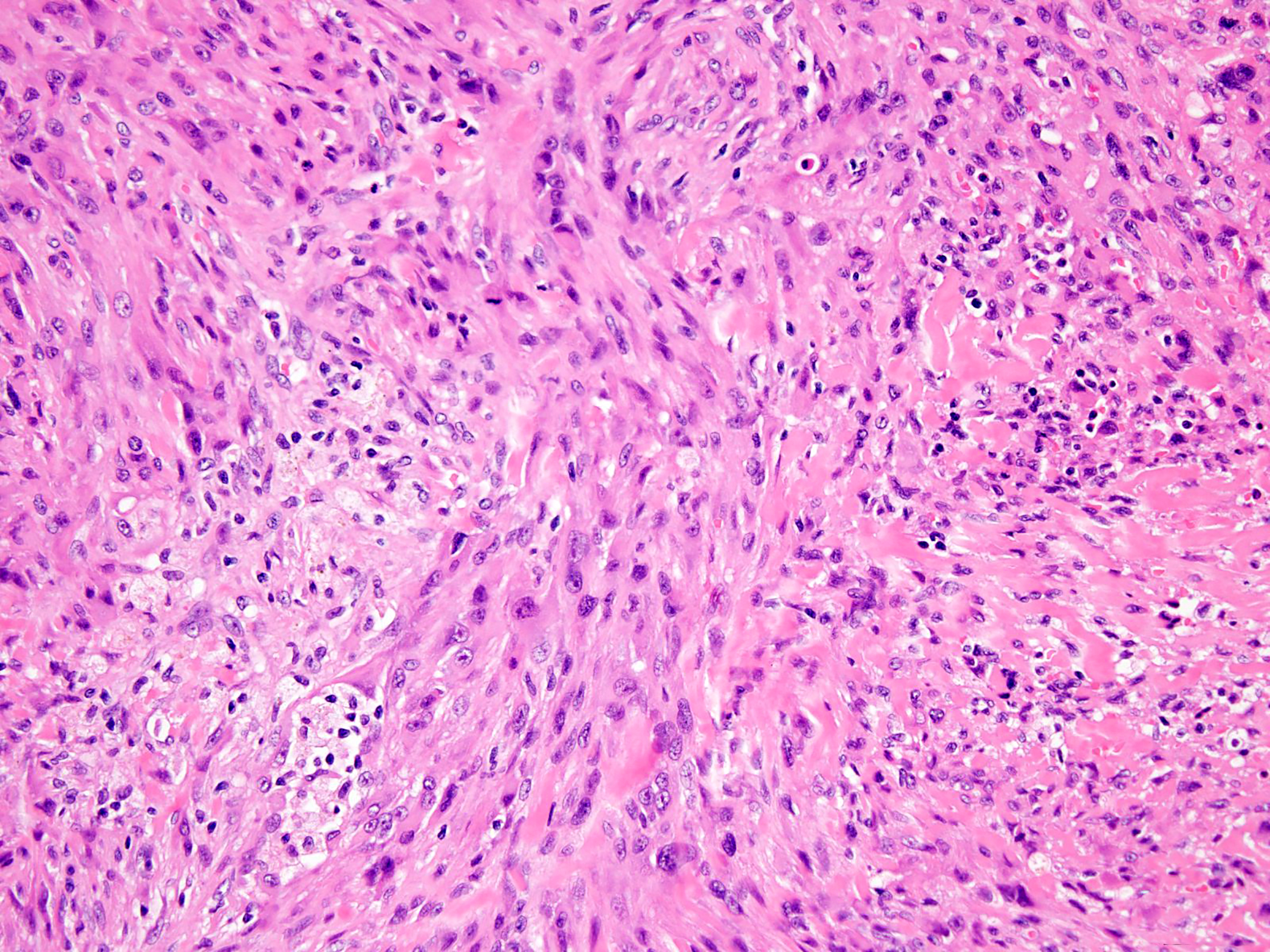
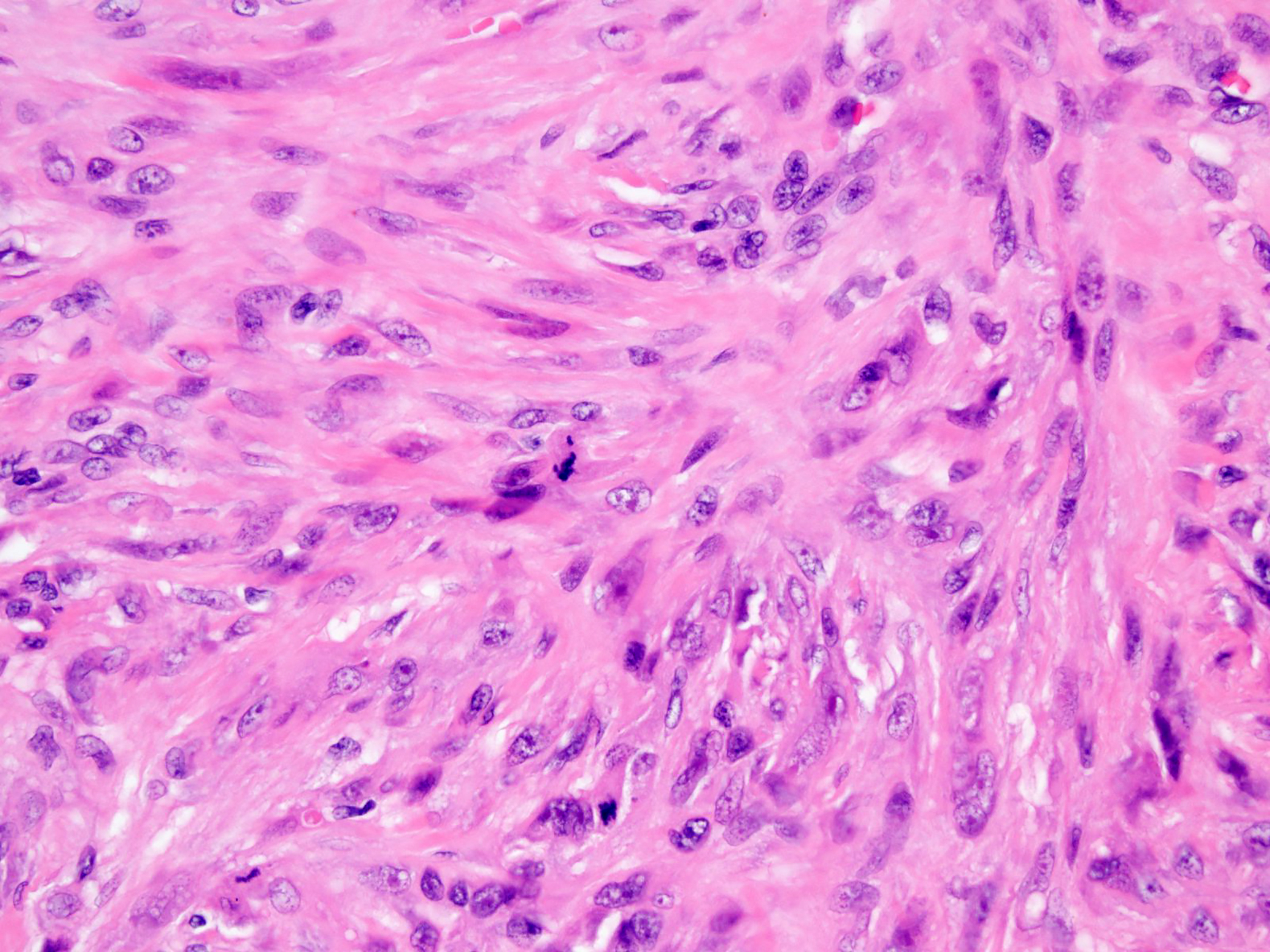
- Fairly uniform plump small to medium sized cells with eosinophilic cytoplasm (Adv Anat Pathol 2016;23:41)
- Spindle cells can also be identified and often appear more conspicuous at the periphery of a nodule
- Mildly atypical nuclei with vesicular chromatin and small nucleoli
- Variable mitotic activity
- Mixed chronic inflammatory infiltrate common
- Dystrophic calcification and metaplastic bone formation
- Other variant morphologies (Adv Anat Pathol 2016;23:41)
- Angiomatoid variant
- Myxoid variant
- Other features include intracytoplasmic vacuoles, multinucleated giant cells and storiform pattern
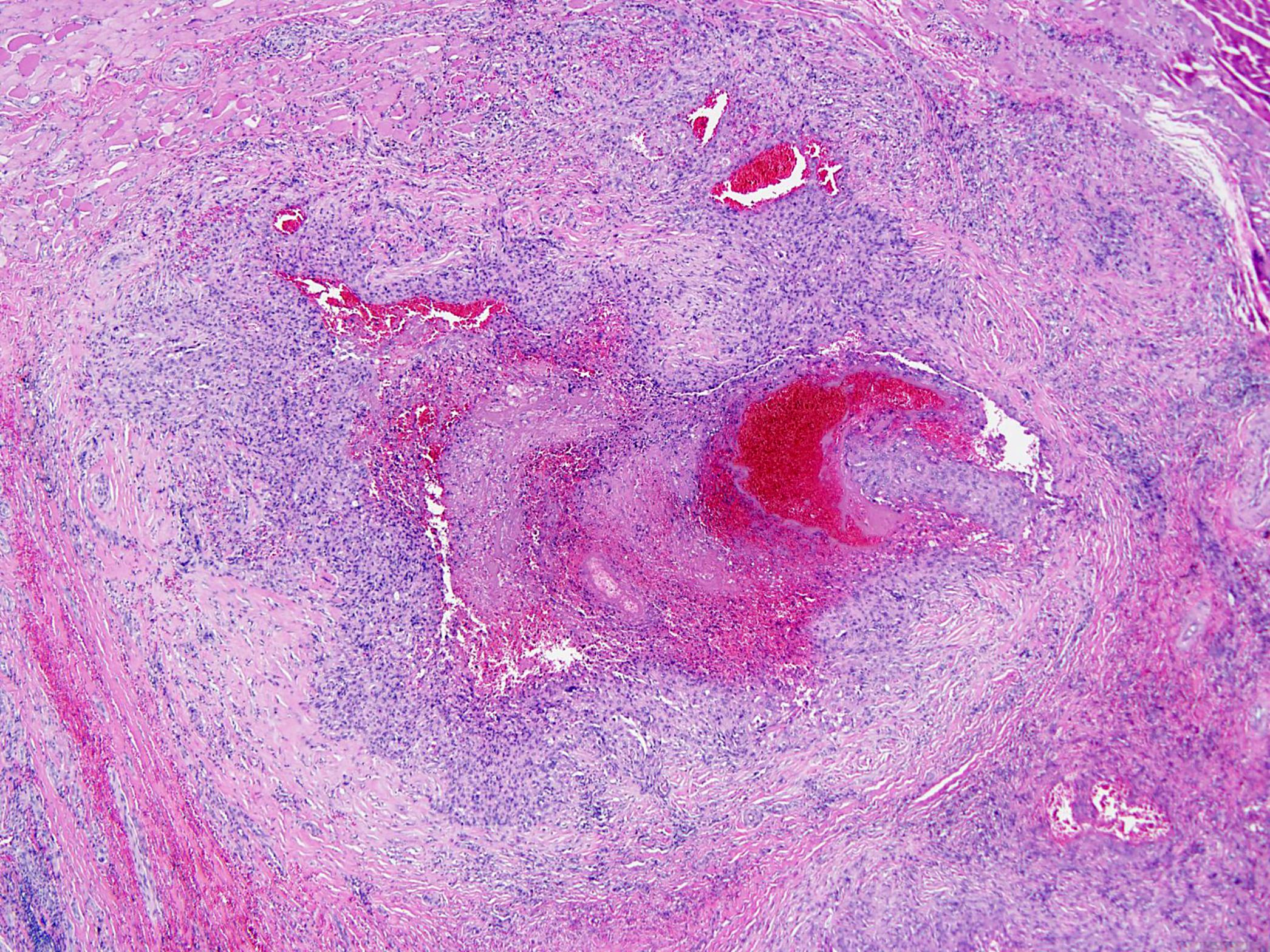
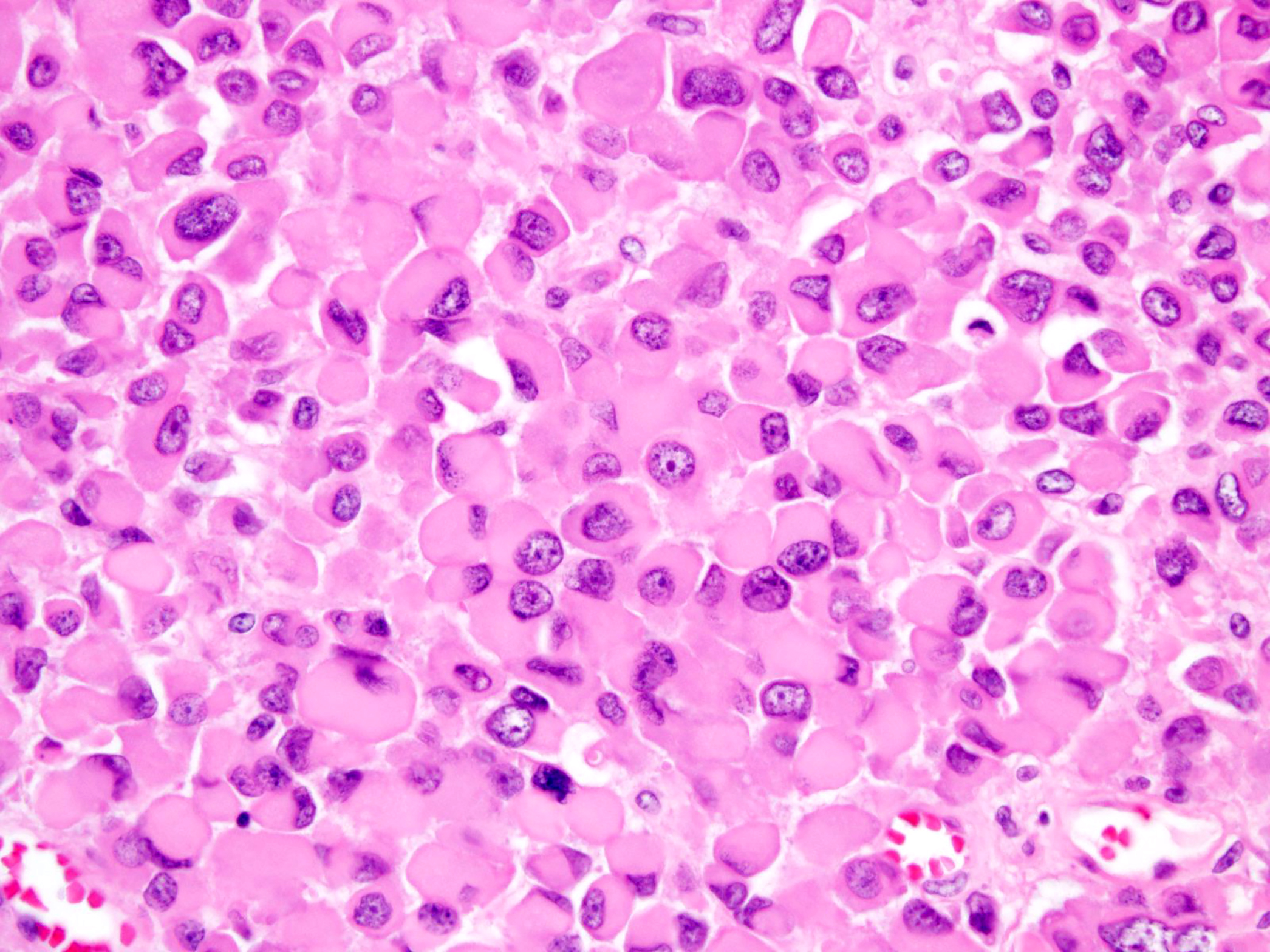
- Proximal, large cell type (Am J Surg Pathol 1997;21:130, Adv Anat Pathol 2016;23:41)
- Infiltrative growth pattern with less defined peripheral borders
- Multiple large nodules
- Large polygonal cells with abundant eosinophilic cytoplasm
- Rhabdoid morphology common
- Vesicular nuclei with prominent macronucleoli
- Mitoses, necrosis and hemorrhage common
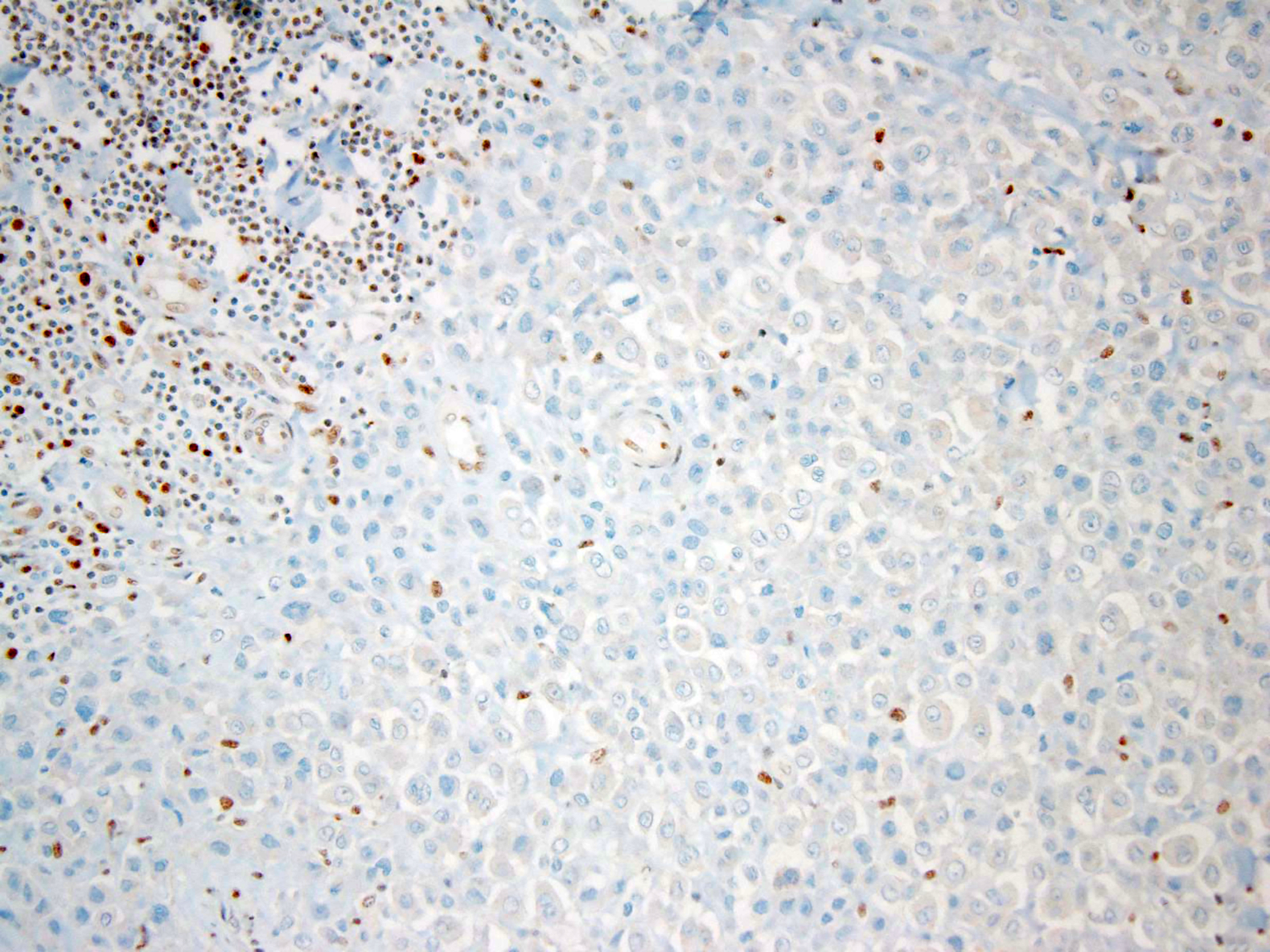
Microscopic (histologic) images
Cytology description
- Smears in most cases were moderate to hypercellular, composed of polygonal cells and spindle cells
- Cells are arranged in loosely cohesive groups, non overlapping clusters and scattered singly, containing moderate to abundant cytoplasm, defined cell borders, vesicular nuclei and discernible nucleoli
- Variable cytopathologic features include rhabdoid-like intracytoplasmic inclusions, giant cells, marked nuclear atypia and interspersed scanty, metachromatic stroma (Diagn Cytopathol 2016;44:636)
- Necrotic and inflammatory background (Cancer Cytopathol 2018;126:934)
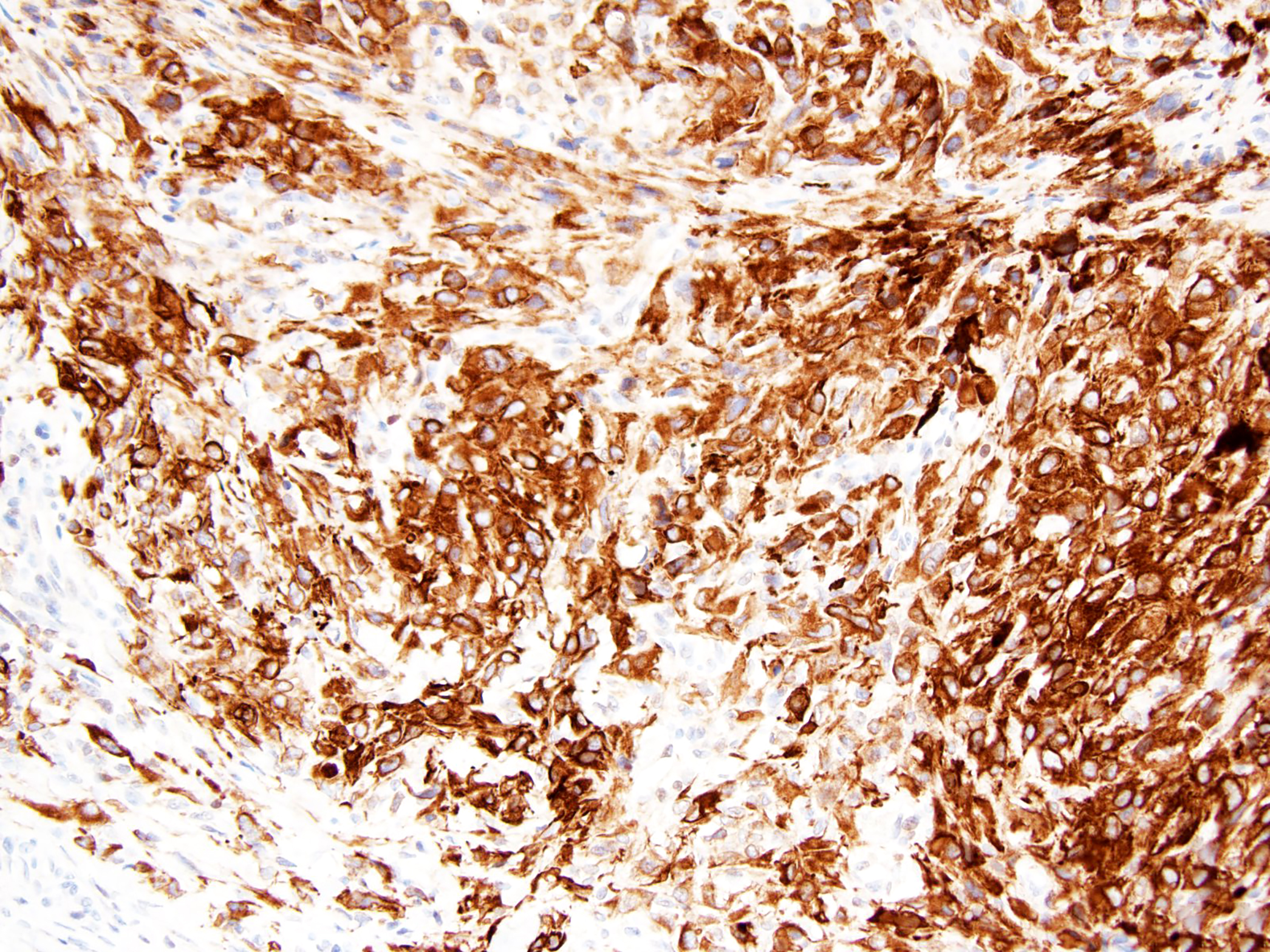
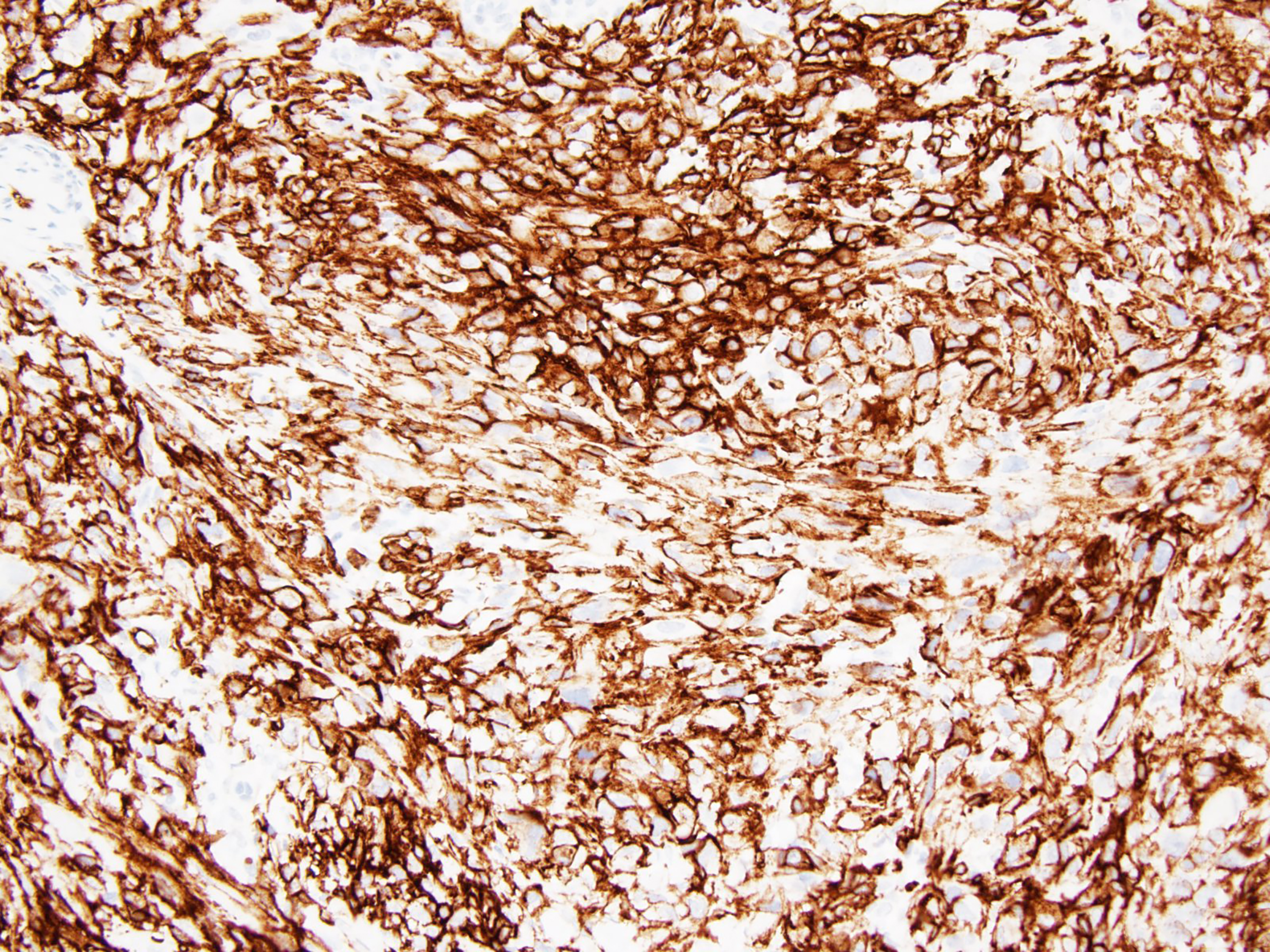
Positive stains
- Pancytokeratin, CAM 5.2, EMA (nearly all cases)
- Percentage expression of cytokeratins: CK8 (94%), CK19 (72%), CK14 (48%), CK7 (22%), CK20 (15%), CK5/6 (30%) (Arch Pathol Lab Med 2009;133:814)
- Vimentin
- CD34 (50%) (Adv Anat Pathol 2006;13:114)
- ERG (40%) (Hum Pathol 2015;46:225)
- CA-125 (91%; nonspecific but may be useful for monitoring) (Arch Pathol Lab Med 2009;133:814)
Negative stains
- INI1 / SMARCB1 (> 90%) (Am J Surg Pathol 2009;33:542, Diagn Cytopathol 2016;44:636)
- CD31
- CD68
- S100 protein, desmin, FLI1 are usually negative (Adv Anat Pathol 2006;13:114)
- A wide range of other antigens can be expressed including SALL4 in 3% of cases (Adv Anat Pathol 2006;13:114, Hum Pathol 2015;46:225, Histopathology 2015;66:252)
Electron microscopy description
- Shows a spectrum of cellular differentiation, from undifferentiated cells or primitive fibrohistiocytic cells to epithelial type cells with junctions, tonofilaments and microvilli (Hum Pathol 1988;19:265)
- Other findings have included desmosomes, surface microprocesses and interdigitating cell membranes, indicating epithelial (sometimes interpreted as synovial sarcoma-like) differentiation (Adv Anat Pathol 2006;13:114)
- Proximal epithelioid sarcoma often shows prominent intracytoplasmic intermediate filament aggregates that often take the shape of paranuclear whorls in keeping with the rhabdoid phenotype (Adv Anat Pathol 2016;23:41)
Molecular / cytogenetics description
- High frequency of SMARCB1 (INI1) deletion (22q11) (Hum Pathol 2009;40:349, Mod Pathol 2013;26:385)
Sample pathology report
- Right hand mass, excision:
- Epithelioid sarcoma, classic type (see comment)
- Comment: There is a dermal and subcutaneous multinodular lesion composed of small to medium sized oval or polygonal epithelioid cells and plump spindle shaped cells with eosinophilic cytoplasm and mildly atypical nuclei with vesicular chromatic and small nucleoli. The nodules contain centralized necrosis and hemorrhage imparting a granulomatous appearance to the process on low power magnification. The epithelioid cells are concentrated towards the center of the nodules with peripheral spindling. Aggregates of chronic inflammatory cells are present at the periphery of the nodules. The mitotic activity is low: 4 mitoses / 10 high power fields. The lesion involves the underlying facia. Immunohistochemically the epithelioid and spindled cells show strong expression of CAM5.2, EMA and CD34 and are negative for CD31 and CD68. There is loss of INI1 expression in lesional cells. This constellation of morphological and immunohistochemical features strongly supports the diagnosis of epithelioid sarcoma, classic type. The course of epithelioid sarcoma is often unpredictable and it is common for patients to present with extensive disease, lymph node metastases, or distant metastases.
Differential diagnosis
- Granulomatous process (Histopathology 2001;39:641)
- Necrobiosis lipoidica, granuloma annulare, rheumatoid nodules or even infectious granulomas mimic conventional epithelioid sarcoma
- EMA-, cytokeratins-, CD34-
- CD68+
- Carcinoma (Adv Anat Pathol 2016;23:41)
- Malignant melanoma
- Almost always cytokeratin- and EMA-
- Retained nuclear INI1 (Adv Anat Pathol 2016;23:41)
- SOX10+, S100+, HMB45+, MelanA+ (Appl Immunohistochem Mol Morphol 2015;23:109)
- Extrarenal rhabdoid tumor
- Median age 8 - 9 years
- SALL4+ in 67% of cases (Histopathology 2015;66:252)
- Does not typically express CD34 (Adv Anat Pathol 2016;23:41)
- Epithelioid malignant peripheral nerve sheath tumor
- Can be associated with a nerve or a preexisting benign nerve sheath neoplasm
- S100+, diffuse and strong (Adv Anat Pathol 2016;23:41, Am J Surg Pathol 2015;39:673)
- Myoepithelial tumors of soft tissue (myoepithelial carcinoma)
- Also express cytokeratins and often EMA but in contrast typically coexpress S100 protein (Adv Anat Pathol 2016;23:41)
- Variably immunoreactive for SMA, calponin, CD10 and glial fibrillary acidic protein (Am J Surg Pathol 2007;31:1813)
- EWSR1 rearrangements in ~50% (Head Neck Pathol 2015;9:273)
- Epithelioid angiosarcoma
- Areas of vasoformation usually present
- Express other vascular markers, such as CD31 and FLI1, which are generally absent in most epithelioid sarcoma (Adv Anat Pathol 2016;23:41, Int J Clin Exp Pathol 2019;12:3944)
- Pseudomyogenic hemangioendothelioma
- CD34-
- Retained nuclear INI1
- FOSB+ (Am J Surg Pathol 2017;41:596)
- Some are associated with t(7;19)(q22;q13) translocations that result in fusion of the SERPINE1 and FOSB gene (J Pathol 2014;232:534)
Additional references
Board review style question #1
- Which of the following is true about epithelioid sarcoma?
- ~30% of cases metastasize
- Diagnosis always requires clinicopathological and radiological correlation
- Epithelioid sarcoma is positive for MDM2 amplification by FISH
- Pediatric patients appear to have a better prognosis
- Tumor is characterized by marked nuclear pleomorphism in most cases
Board review style answer #1
Board review style question #2
- A 53 year old man presents with a left hip mass. Hematoxylin-eosin stains demonstrate multinodular and sheet-like growth of large epithelioid cells with enlarged vesicular nuclei and prominent nucleoli. Aggregates of rhabdoid cells with glassy intracytoplasmic hyaline inclusions and foci of tumor necrosis are frequently encountered. Mitotic figures are uncommon (5 mitoses / 10 high power fields). The lesion involves deep soft tissue and underlying bone. Immunohistochemical stains for EMA, CAM5.2 and CD34 are positive in epithelioid cells and there is loss of INI1 expression. Stains for SMA, myogenin, MyoD1, CD31, FLI1 and SALL4 are negative. Which of the following is most likely the correct diagnosis?
- Epithelioid angiosarcoma
- Epithelioid hemangioendothelioma
- Epithelioid sarcoma, proximal type
- Extrarenal rhabdoid tumor
- Pleomorphic rhabdomyosarcoma
Board review style answer #2