Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Paulsen JD, Polydorides AD. Whipple disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallbowelwhipple.html. Accessed December 25th, 2024.
Definition / general
- Rare systemic infection caused by intracellular rod shaped actinobacterium Tropheryma whipplei
Essential features
- Whipple disease is a rare, multisystem infection due to Tropheryma whipplei that most commonly affects the small bowel but may involve any part of the gastrointestinal tract
- Histologically, small intestinal biopsies show infiltration of the lamina propria by foamy macrophages containing PAS positive, AFB negative bacteria
- Electron microscopy shows intact and degenerated rod shaped bacterial forms
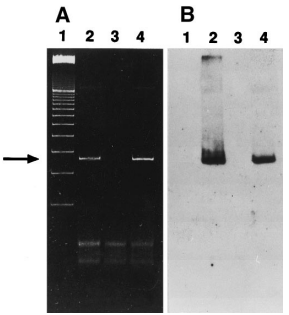
- PCR for 16S ribosomal genes of T. whipplei is often diagnostically useful and can be performed on fresh or paraffin embedded, formalin fixed tissue
- Treatment consists of long term antimicrobial therapy
Terminology
- Tropheryma whipplei is also known as the Whipple bacillus
- Formerly called Tropheryma whippelii
- Historical term: intestinal lipodystrophy (Clin Gastroenterol Hepatol 2004;2:849)
ICD coding
- ICD-10: K90.81 - Whipple disease
Epidemiology
- M:F = 8:1
- More common in middle aged white males
- Extremely rare, annual incidence of approximately 1 - 6 new cases per 10,000,000 persons per year worldwide (Scand J Gastroenterol 1997;32:52)
Sites
- Multisystem infection
- Most often involves gastrointestinal tract
- Small intestine > esophagus / stomach / appendix / colorectum
- May involve mesenteric lymph nodes, joints, heart, lungs, eyes and central nervous system
- Most often involves gastrointestinal tract
Pathophysiology
- Many individuals carry antibodies against Tropheryma whipplei, despite the extremely low incidence of Whipple disease
- Disease presumably develops in individuals with predisposing immune factors
- Patients with Whipple disease often have immunomodulatory conditions, such as alcohol abuse, sarcoidosis, ankylosing spondylitis, Crohn's disease and rheumatoid arthritis (Am J Surg Pathol 2012;36:1066)
- Association with HLA-B27 (Eur J Clin Invest 1979;9:385)
- Organism laden macrophages mechanically compress lymphatics in small bowel, leading to malabsorption
Etiology
- Causative agent is Tropheryma whipplei
- Actinomycete, related to mycobacteria
Clinical features
- Clinical presentation is highly variable
- Most common symptoms are malabsorption, weight loss, diarrhea, arthralgias and abdominal pain
- Generalized lymphadenopathy may be present (particularly in the abdomen)
- Often referred to as protean and the great mimicker, like syphilis, because of nonspecific clinical presentation (Am J Surg Pathol 2012;36:1066)
- Approximately 15% of patients do not have typical symptoms
- Neurological symptoms (such as cognitive changes, ophthalmoplegia, nystagmus and myoclonia) present in ~24% of patients (Medicine (Baltimore) 2015;94:e714)
- Tropheryma whipplei accounts for ~6.3% of culture negative endocarditis (J Clin Microbiol 2012;50:216)
- Rarely, can present in retroperitoneum, mimicking a neoplasm (Braz J Infect Dis 2014;18:346)
- Esophagogastroduodenoscopy findings:
- Unremarkable (majority of cases) (Medicine (Baltimore) 2015;94:e714)
- Pale yellow, shaggy mucosa
- Thickened mucosal folds
- Yellow-white plaques
- Erosions, erythema, friability
Diagnosis
- Upper endoscopy with biopsies of small intestine
- H&E histology
- Periodic acid-Schiff (PAS) staining
- PCR on paraffin embedded, formalin fixed tissue for 16S ribosomal genes of Tropheryma whipplei
- PCR testing can also be performed on fresh tissue, vitreous fluid and cardiac valves (N Engl J Med 1992;327:293, N Engl J Med 1995;332:363, J Infect Dis 2004;190:935)
- PCR can be negative after antibiotic treatment (Ann Intern Med 1997;126:520)
- Immunohistochemical stain: polyclonal rabbit antibody against T. whipplei, available from reference center, such as Centers for Disease Control and Prevention (Am J Clin Pathol 2002;118:742)
- Electron microscopy
- Cerebrospinal fluid and synovial fluid
- Cytology
- PAS staining
- PCR
Laboratory
- Laboratory abnormalities seen in chronic inflammatory conditions are common (Medicine (Baltimore) 2015;94:e714):
- Anemia (81% of patients)
- Leukocytosis (48% of patients)
- Thromobocytosis (56% of patients)
- Elevated C reactive protein (69% of patients)
Radiology description
- Radiological findings are nonspecific (Clin Gastroenterol Hepatol 2004;2:849)
- Abdominal computed tomography and magnetic resonance imaging:
- Thickened small bowel mucosal folds
- Mesenteric lymphadenopathy
- Small bowel contrast radiology may also show thickened mucosal folds
Prognostic factors
- Response to antimicrobial treatment is unpredictable
- Relapse is common after treatment
Case reports
- 4 year old girl with chronic bloody diarrhea and growth retardation (Intest Res 2021;19:119)
- 49 year old man with weakness, loss of appetite, weight loss and joint pain (Med Princ Pract 2020;29:90)
- 52 year old man with diarrhea, marked weight loss and vision changes (GE Port J Gastroenterol 2020;27:283)
Treatment
- Antimicrobial treatment (Clin Microbiol Rev 2017;30:529)
- Optimal treatment regimen is uncertain and without consensus but most regimens involve an initial phase followed by a maintenance phase
- Initial phase (2 - 4 weeks): ceftriaxone or penicillin G
- Maintenance phase (one year): trimethoprim sulfamethoxazole
- Doses and durations of therapy depends on presence or absence of central nervous system disease or endocarditis
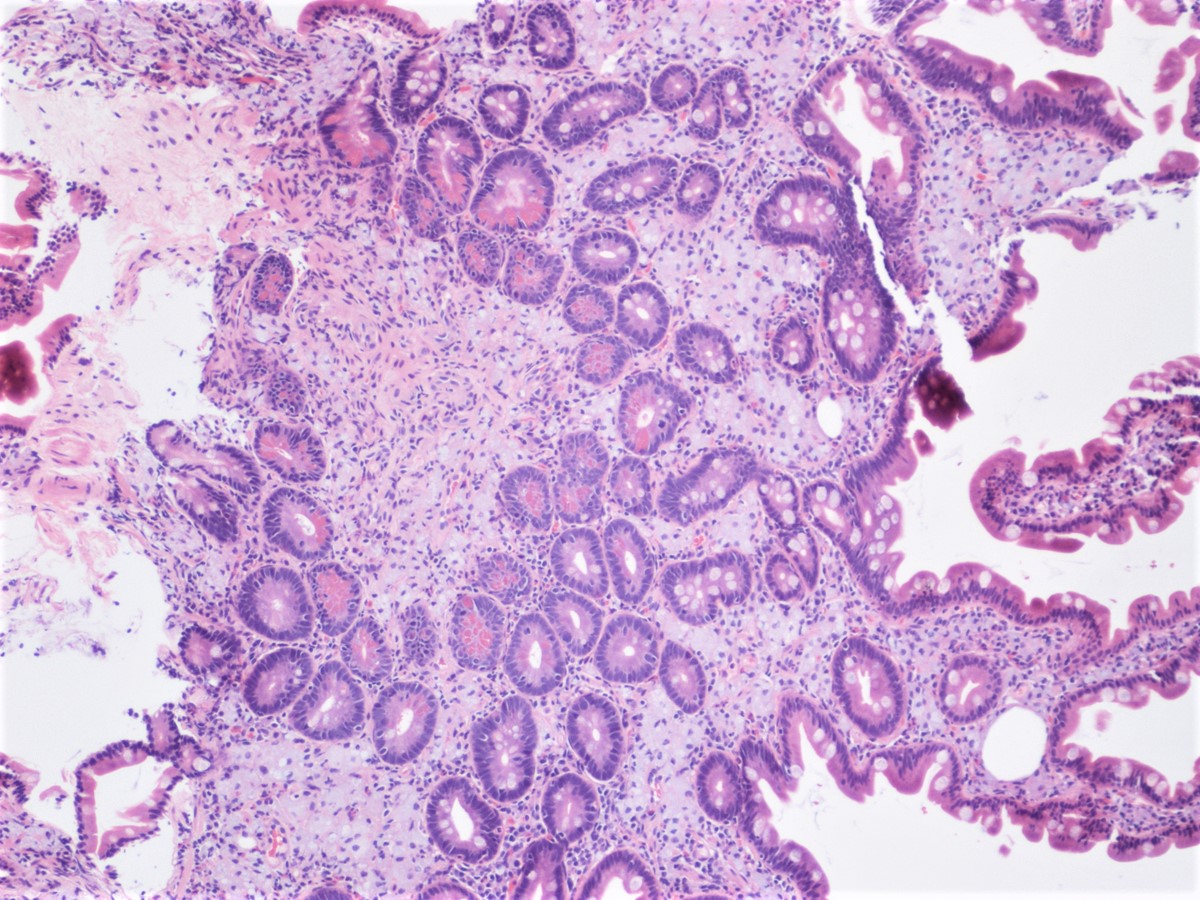
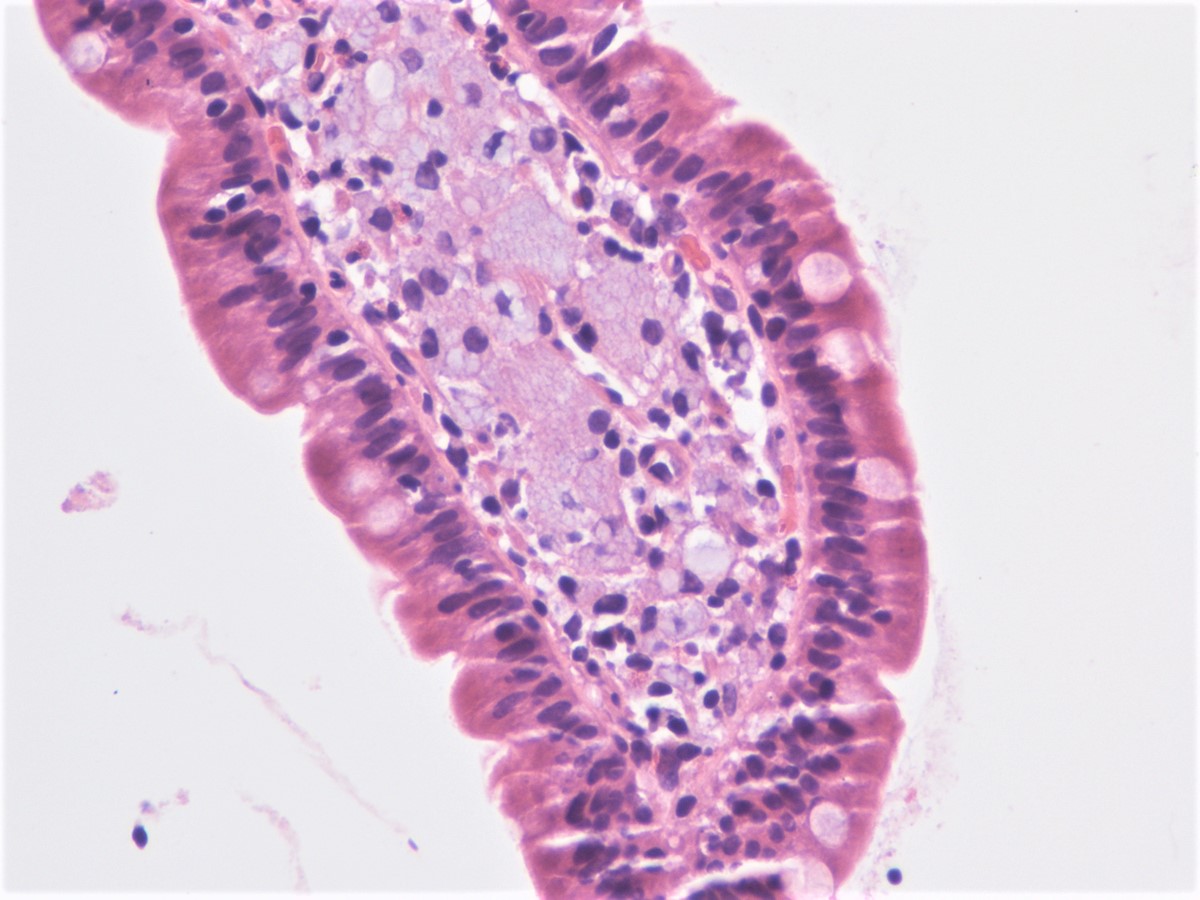
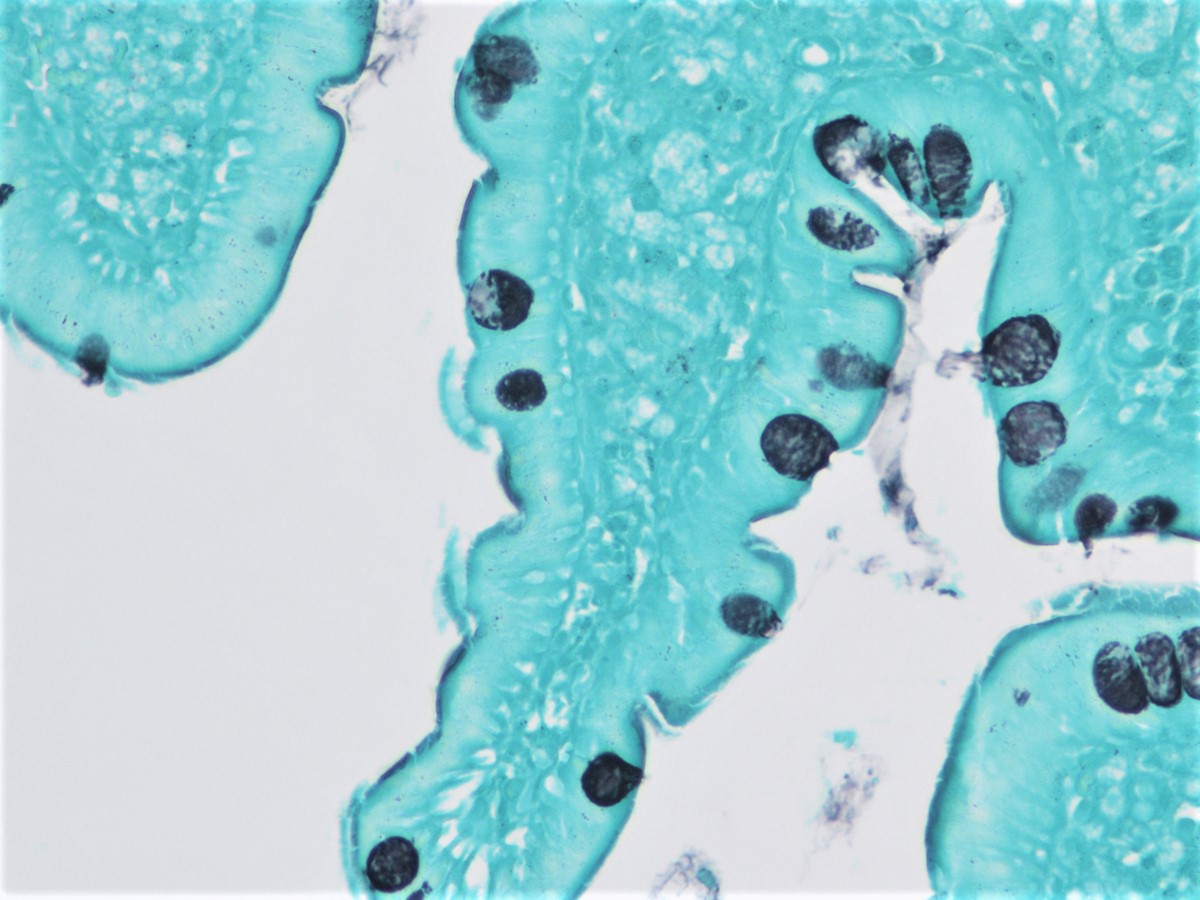
Microscopic (histologic) description
- Lamina propria expanded by foamy macrophage infiltrate (Am J Surg Pathol 2012;36:1066)
- Infiltrate may be diffuse or patchy
- Blunt or distended villi (Dig Dis Sci 2019;64:213)
- Scattered dilated lacteals (Am J Surg Pathol 2012;36:1066)
- Fat vacuoles within lamina propria (Dig Dis Sci 2019;64:213)
- Overlying enterocyte vacuolization due to intracytoplasmic lipid accumulation
- Acute inflammation (variable)
- Mononuclear inflammation usually absent
- Epithelioid granulomas (minority of cases) (Virchows Arch A Pathol Anat Histol 1979;382:227)
Microscopic (histologic) images
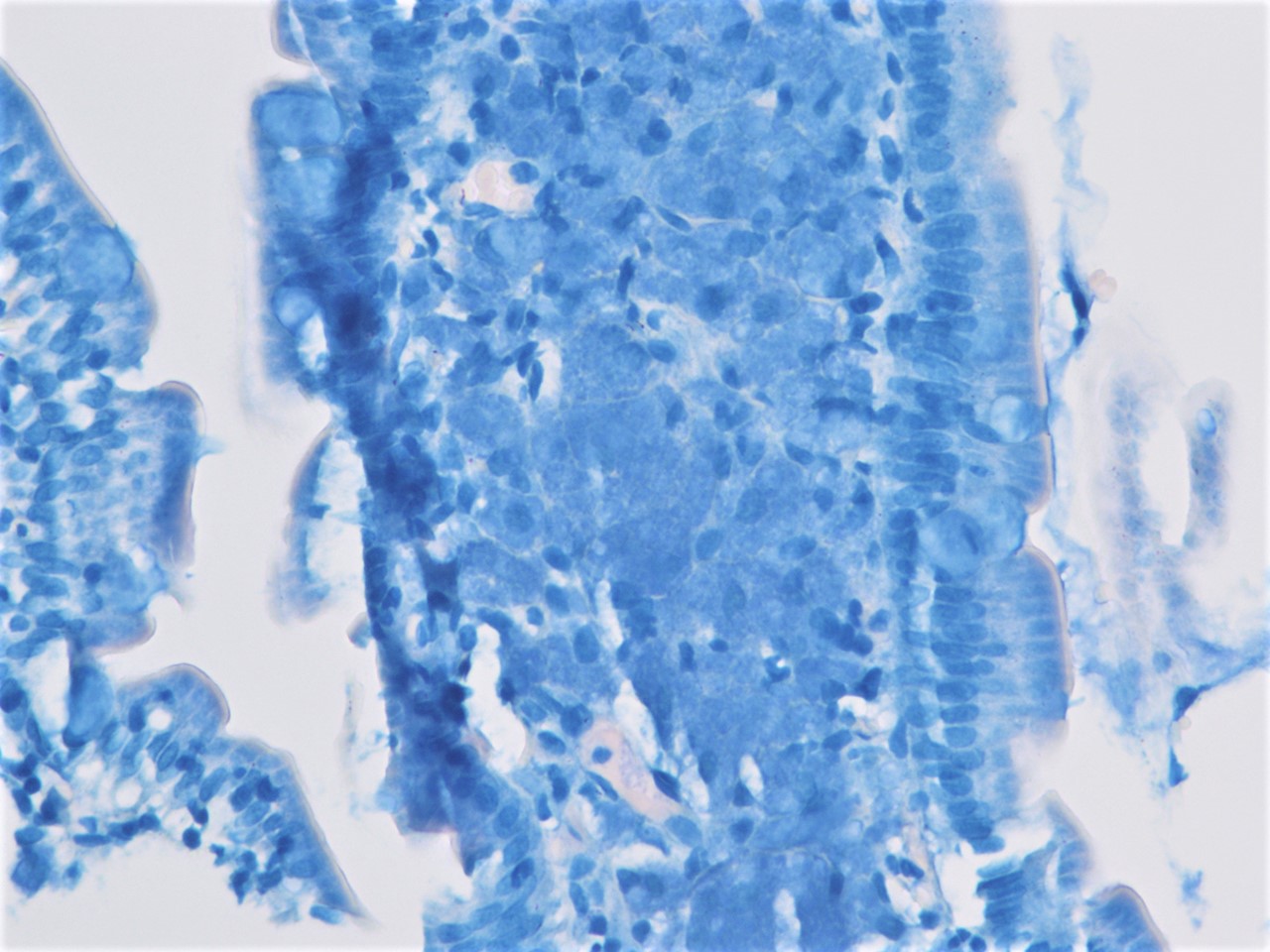
Cytology description
- Limited clinical utility
- Cytospin stained with PAS reagent may be used for fluid samples (i.e. cerebrospinal fluid [CSF], synovial fluid)
- Histiocytes with numerous intracellular PAS positive, granular particles
- Intracellular particles may appear sickle shaped, resulting in sickleform particle containing (SPC) cells (Gastroenterology 1997;113:434)
- CSF cytology may be positive in patients without neurological symptoms (Gastroenterology 1997;113:434)
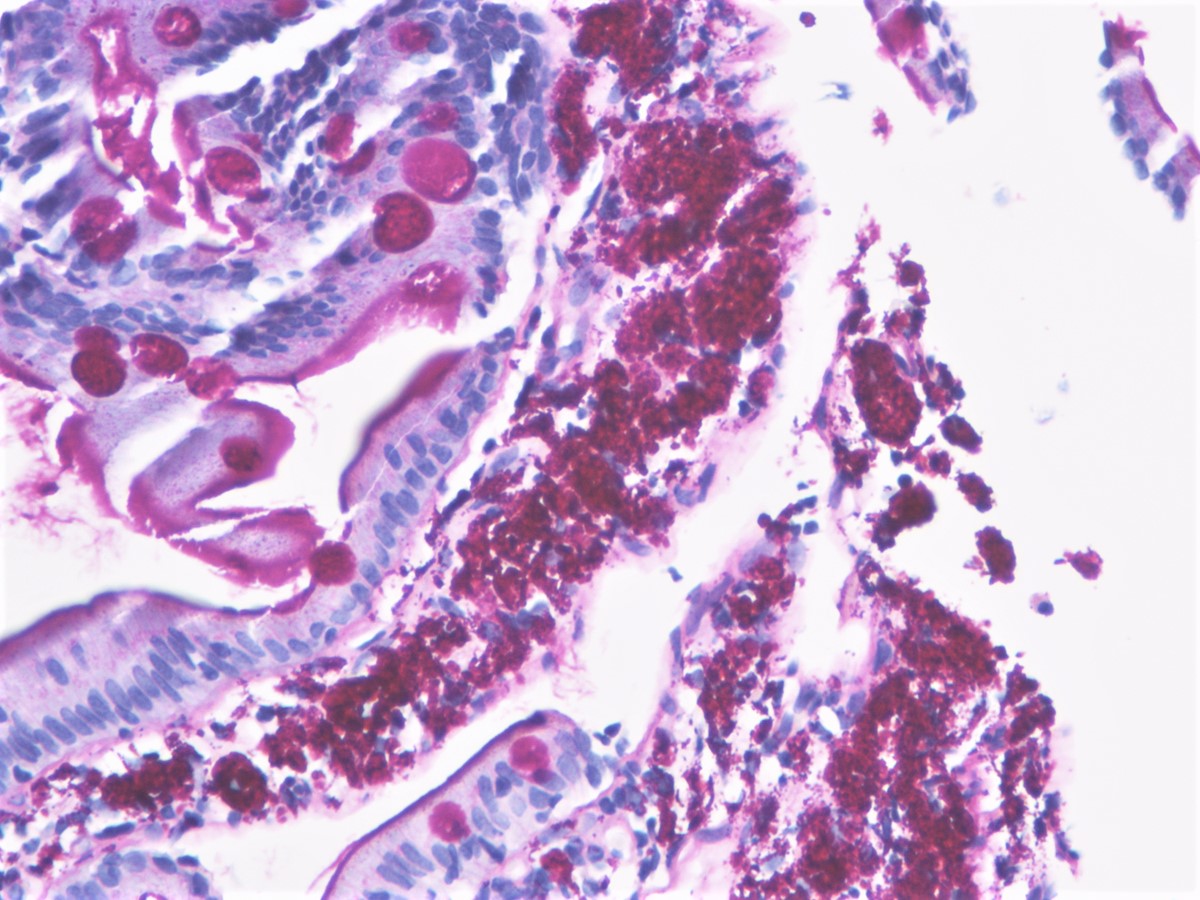
Positive stains
- PAS and PASD (granular staining)
- Stains the glycoprotein wall of the bacteria
- Can stain both viable and nonviable organisms
- Tropheryma whipplei immunostain (granular staining) (Am J Clin Pathol 2002;118:742)
- Can stain both viable and nonviable organisms
Electron microscopy description
- Rod shaped bacterium (bacillary bodies) within macrophages and lamina propria
- Intracellular forms may be associated with phagocytic vacuoles (Am J Surg Pathol 1981;5:507)
- After treatment, bacterial breakdown products and degenerating organisms may be seen
Electron microscopy images
Molecular / cytogenetics description
- PCR for 16S ribosomal genes of T. whipplei is an important diagnostic tool for diagnosing Whipple disease
- In patients with histologically confirmed disease: sensitivity 96.6% and specificity 100% (Ann Intern Med 1997;126:520)
- Conversion from positive to negative PCR results can occur before histologic resolution of disease because bacterial remnants and cell wall structures often persist in macrophages after treatment (Gastroenterology 1996;110:1735)
- Positive PCR can be seen in asymptomatic colonization of patients without disease
Sample pathology report
- Duodenum, endoscopic biopsy:
- Duodenal mucosa with abundant foamy macrophages in lamina propria (see comment)
- Special stains for PAS and PAS with diastase (PASD) show strong, granular positivity within macrophages
- AFB stain (Ziel-Neelsen method) is negative
- Comment: In the appropriate clinical setting, the findings are concerning for Whipple disease. Immunohistochemical stain for Tropheryma whipplei as well as PCR on the paraffin embedded block have been requested, results of which will be reported in a follow up addendum.
Differential diagnosis
- Mycobacterium avium intracellulare complex:
- Histoplasmosis:
- Malakoplakia:
- Lamina propria macrophage infiltrate showing targetoid Michaelis-Gutmann bodies (PAS positive, von Kossa positive)
- False positivity with Tropheryma whipplei immunostain has been documented (Am J Surg Pathol 2020;44:1251)
- Rhodococcus:
- Lamina propria macrophage infiltrate containing intracellular coccobacillary organisms
- Gram positive on tissue Gram stain
- PAS positive (typically more granular than T. whipplei)
- T. whipplei immunostain negative
- Gaucher disease:
- Lamina propria macrophage infiltrate with fibrillary cytoplasm (tissue paper-like)
- PAS positive
- Electron microscopy shows elongated lysosomes with tubular inclusions
- Crushed Brunner glands:
- Interpret in context of adjacent more intact Brunner glands
- PAS positive
Board review style question #1
A 54 year old man presents to his primary care physician with a 5 month history of diarrhea and abdominal pain. He is referred for esophagogastroduodenoscopy, which demonstrates diffuse yellow-white plaques of the duodenal mucosa. Multiple biopsies are performed. Representative H&E of the duodenal biopsy is shown above. Which of the following pairs of ancillary stains would be most helpful in establishing a diagnosis?
- AFB and CD68 immunostain
- GMS and AFB
- PAS and AFB
- PAS and CD68 immunostain
- PAS and GMS
Board review style answer #1
C. PAS and AFB. The photograph shows a single small intestinal villous containing numerous foamy macrophages in the lamina propria. The primary histologic differential diagnosis includes Mycobacterium avium intracellulare complex and Whipple disease. The most useful pair of stains for distinguishing these 2 entities is PAS and AFB given that Mycobacterium avium intracellulare complex is PAS positive and AFB positive, whereas Whipple disease is PAS positive and AFB negative. GMS does not help distinguish Mycobacterium avium intracellulare complex and Whipple disease. GMS highlights histoplasmosis; however, no intracellular yeast forms are seen on H&E stain in this case. CD68 immunostain highlights foamy lamina propria macrophages; however, it would not help distinguish the 2 entities.
Comment Here
Reference: Whipple disease
Comment Here
Reference: Whipple disease
Board review style question #2
A 45 year old man presents to the emergency department with a 6 month history of weight loss, diarrhea and joint pain in both his left knee and right elbow. He is admitted for further work up, including esophagogastroduodenoscopy (EGD), which reveals a pale shaggy mucosa in the duodenum. A diagnosis of Whipple disease is confirmed on biopsy. Which of the following is true regarding the patient's diagnosis?
- In a majority of patients with confirmed Whipple disease, EGD is unremarkable
- On H&E stain, infiltration of the duodenal lamina propria by macrophages is pathognomonic of Whipple disease
- PASD stain is usually negative due to the glycogen containing cell wall of the causative organism
- PCR for 16S ribosomal genes of Tropheryma whipplei cannot be performed on paraffin embedded formalin fixed tissue
- Stomach biopsies are superior to duodenal biopsies for establishing a tissue diagnosis
Board review style answer #2
A. In a majority of patients with confirmed Whipple disease, EGD is unremarkable. In the duodenum, a lamina propria infiltrate of macrophages can be seen in a variety of settings, including Whipple disease, Mycobacterium avium intracellulare complex infection, histoplasmosis, Rhodococcus infection, malakoplakia and Gaucher disease. Therefore, ancillary studies (such as PAS stain, PASD stain, AFB stain[s], PCR or electron microscopy) must be performed to confirm a diagnosis of Whipple disease on biopsy. Both PASD and PAS stains are positive on biopsies involved by Whipple disease due to the glycoprotein (not glycogen) present in the cell wall of T. whipplei. The glycoprotein does not get digested away by diastase and the organisms are therefore PASD positive. PCR for 16S ribosomal genes of T. whipplei can be performed on paraffin embedded formalin fixed tissue as well as fresh tissue, cerebrospinal fluid, synovial fluid, vitreous fluid and cardiac valves. Whipple disease most commonly involves the small bowel; therefore, biopsies of the small bowel, including duodenum, provide the best diagnostic yield.
Comment Here
Reference: Whipple disease
Comment Here
Reference: Whipple disease