Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Li Y, Zhang L. Meckel diverticulum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallbowelMeckels.html. Accessed April 26th, 2024.
Definition / general
- Meckel diverticulum is a congenital disorder caused by incomplete obliteration of omphalomesenteric duct (also called vitelline duct), which results in a true diverticulum, typically located in the ileum within 2 feet from the ileocecal valve (Zhang: Surgical Pathology of Non-neoplastic Gastrointestinal Diseases, 1st Edition, 2019)
Essential features
- Most common congenital malformation of the GI tract, affecting 2 - 4% of the population
- Most common cause of GI tract bleeding in children, usually before age 2
- Usually occurs within 2 feet from the ileocecal valve at the antimesenteric border of the ileum
- True diverticulum that consists of all layers of intestinal wall
- 50% with ectopic tissue, most common is gastric mucosa and then followed by pancreatic tissue
- Rule of 2s:
- Occurring in about 2% of infants
- Usually 2 inches long
- Located in the ileum approximately 2 feet from the ileocecal valve
- M:F = 2:1
- 2 types of ectopic tissue (gastric or pancreatic)
ICD coding
- ICD-10: Q43.0 - Meckel diverticulum (displaced) (hypertrophic)
Epidemiology
- Most common congenital malformation of the gastrointestinal tract
- Difficult to determine the prevalence because many patients are asymptomatic
- Estimated to be in approximately 2 - 4% of the population
- 63% occur in men (Ann Surg 2005;241:529)
Sites
- Usually occurs within 2 feet from the ileocecal valve at the antimesenteric border of the ileum
- In children under 2 years old, the average distance is 34 cm from the ileocecal valve and for adults is 67 cm (J Antibiot (Tokyo) 1978;31:3)
Pathophysiology
- Remnant of the omphalomesenteric duct, which connects the yolk sac with the developing midgut in the fetal life
- Normally regresses by the seventh to eighth week of gestation
- Incomplete obliteration of the omphalomesenteric duct results in Meckel diverticulum
- Reference: Radiographics 2004;24:565
Etiology
- Congenital disorder, caused by the incomplete obliteration of the omphalomesenteric duct
- Diverticulum results from fibrous obliteration of the umbilical end of the omphalomesenteric duct and complete patency of the ileal end of the duct
- Diverticulum is on the antimesenteric side of the ileum and may connect to the umbilicus by a fibrous band if the fibrous portion of the duct fails to be completely obliterated and absorbed
Clinical features
- 16% of patients may be symptomatic; among symptomatic patients, M:F ≈ 3:1 (Ann Surg 2005;241:529)
- Most frequent complications are bleeding from ectopic gastric mucosa and bowel obstruction due to the intussusception, volvulus or adhesive band
- Other uncommon complications include ulceration, diverticulitis, perforation and tumors
- Can also be present in an external hernia, typically on the right side, known as a hernia of Littre
- May be associated with other congenital anomalies
Diagnosis
- Asymptomatic Meckel diverticulum is often incidentally diagnosed during laparoscopy or laparotomy
- However, preoperative diagnosis is still challenging
- Technetium 99m pertechnetate scan, also called Meckel scan, detecting gastric mucosa, has become the most common and accurate noninvasive test to diagnose Meckel diverticulum in children, with a 95% specificity and 85% sensitivity
- However, this test is only 9% specific and 62% sensitive in adults (Clin Anat 2011;24:416)
Radiology description
- Identified as a saccular, blind ending structure located on the antimesenteric border of the ileum
- Antimesenteric location can be confirmed from the position of the diverticulum, which faces away from the axis of the root of the small intestinal mesentery (Br J Surg 1980;67:417)
- Junction of the diverticulum with the ileum may show a mucosal triangular plateau or triradiate fold pattern, which represents the site of omphalomesenteric duct attachment to the ileum (AJR Am J Roentgenol 1980;134:925)
- Technetium 99m pertechnetate scan, also called Meckel scan, can detect gastric mucosa in Meckel diverticulum (Clin Anat 2011;24:416)
Radiology images
Case reports
- 6 year old boy with desmoplastic small round cell tumor arising in Meckel diverticulum (J Clin Oncol 2007;25:3372)
- 11 year old boy with a giant Meckel diverticulum in distal ileum (Radiol Case Rep 2020;16:400)
- 16 year old girl with Meckel diverticulum presenting with necrotic diverticulitis attached to the bladder dome (Medicina (Kaunas) 2021;57:495)
- 64 year old man with Meckel diverticulum presenting with acute appendicitis (Int J Surg Case Rep 2021;83:105994)
- 70 year old man with Meckel diverticulum initially presented with left strangulated inguinal hernia (Int J Surg Case Rep 2021;79:271)
Treatment
- Treatment for symptomatic Meckel diverticulum is surgical resection
- Prophylactic diverticulectomy is recommended for incidental asymptomatic Meckel diverticulum (Ann Surg 2005;241:529)
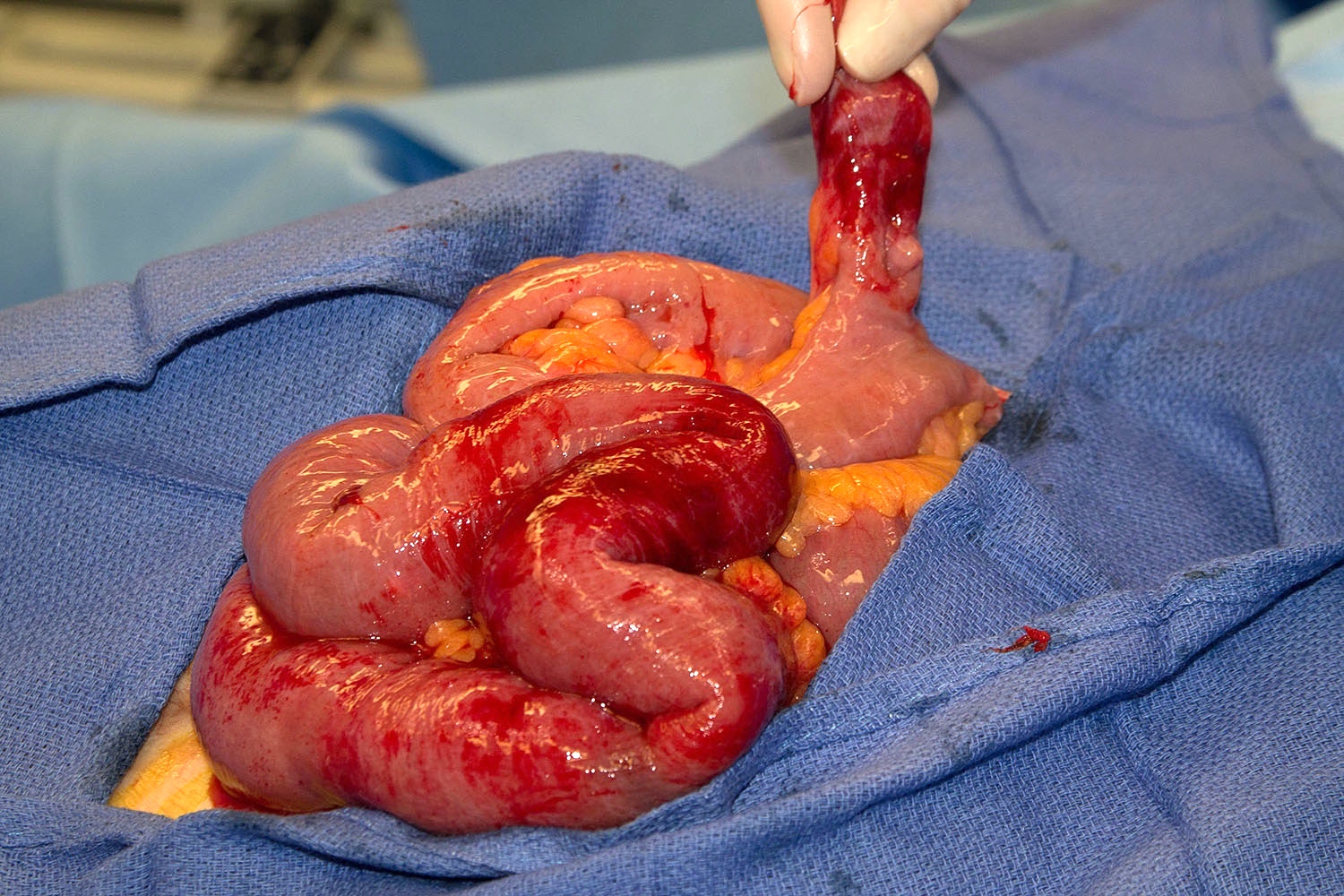
Gross description
- Small bowel with blind pouch or diverticulum on antimesenteric aspect
- Average length is 3 cm but can be longer than 10 cm; giant Meckel diverticulum refers to those longer than 5 cm (Radiographics 2004;24:565)
- Diameters are usually smaller than ileum
- Other lesions may also be identified, such as umbilical bands or omphalomesenteric duct cyst
- Grossly specimen should be examined for evidence of perforation or presence of tumor (J Med Case Rep 2010;4:264)
Gross images
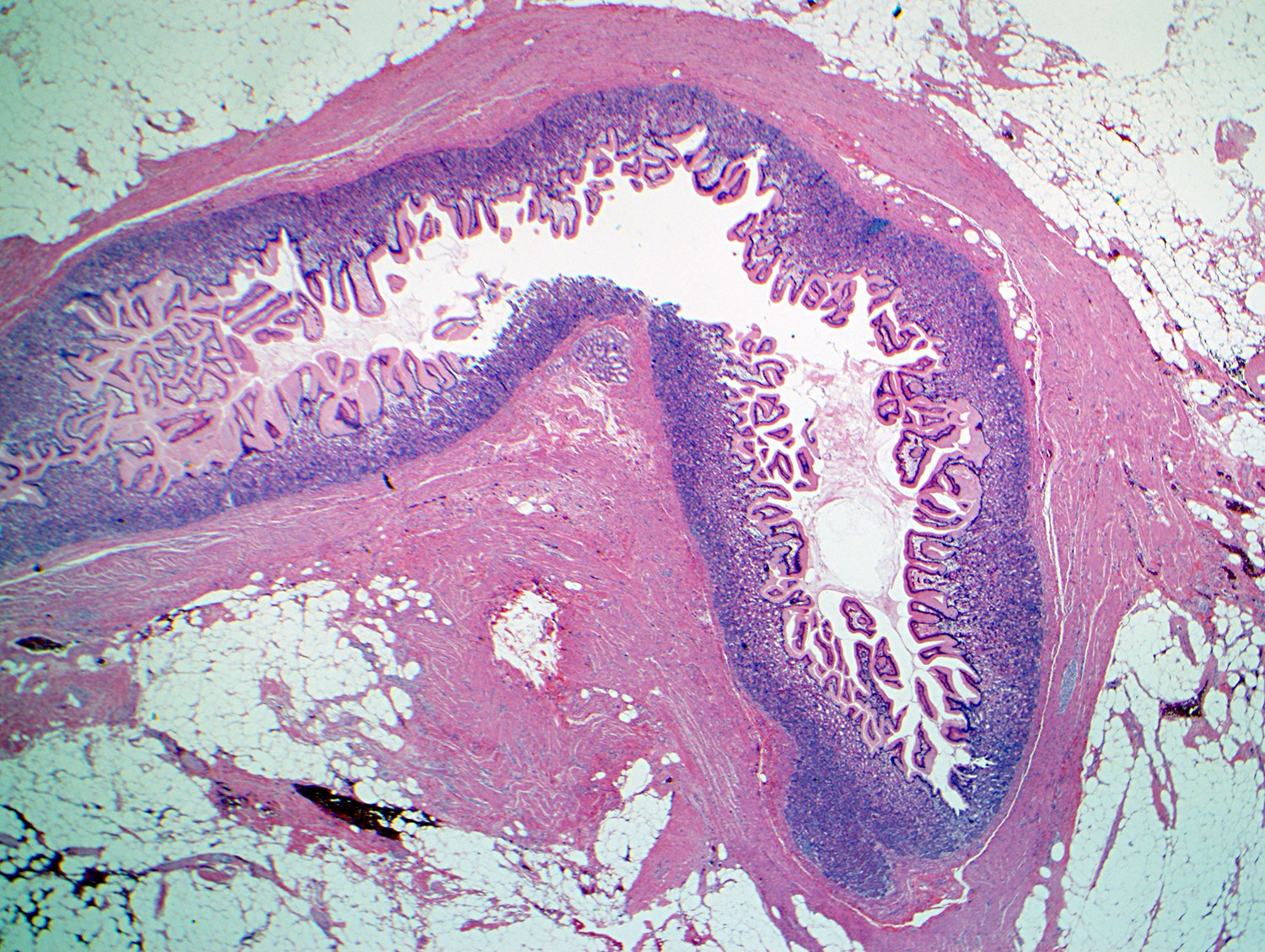
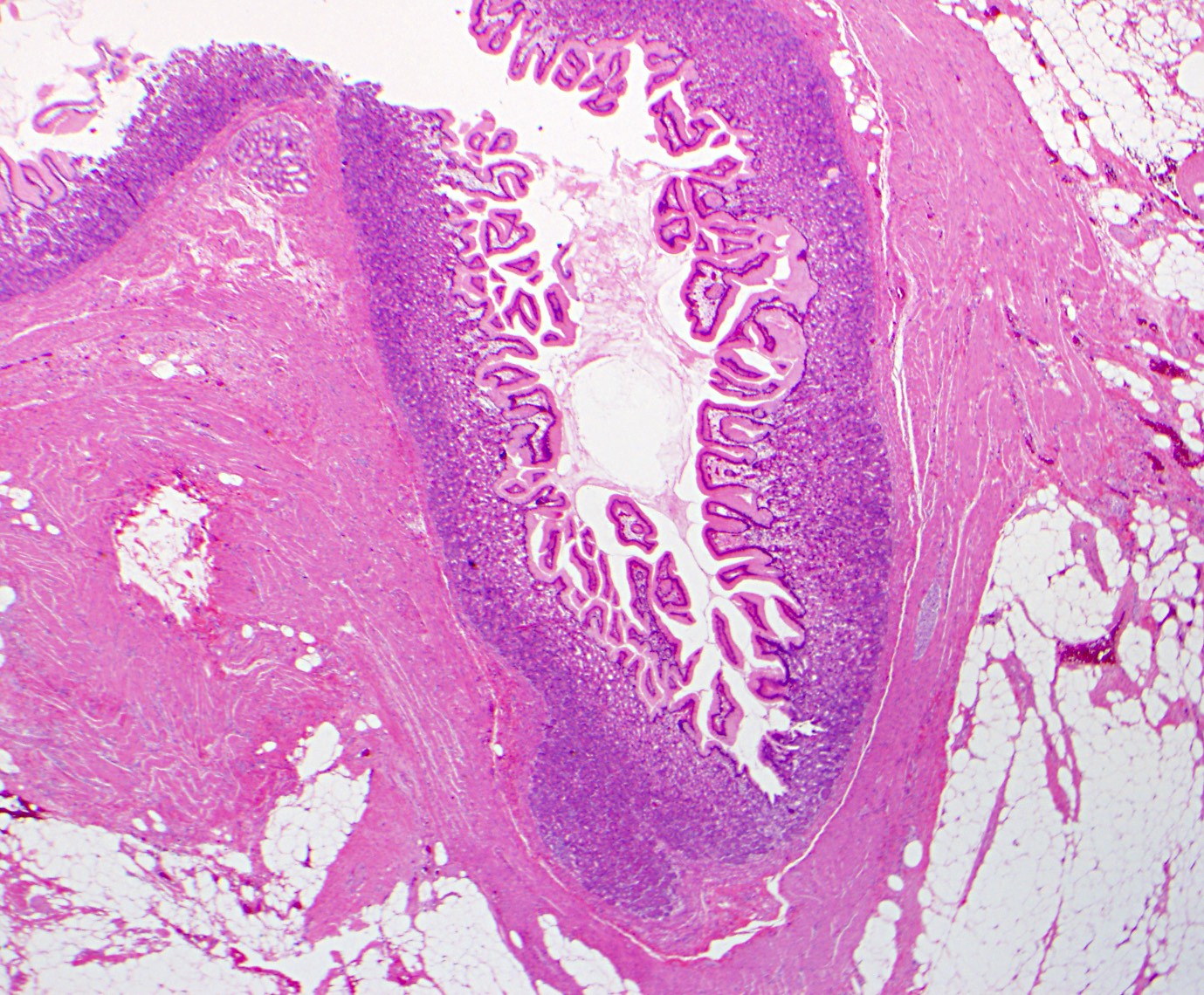
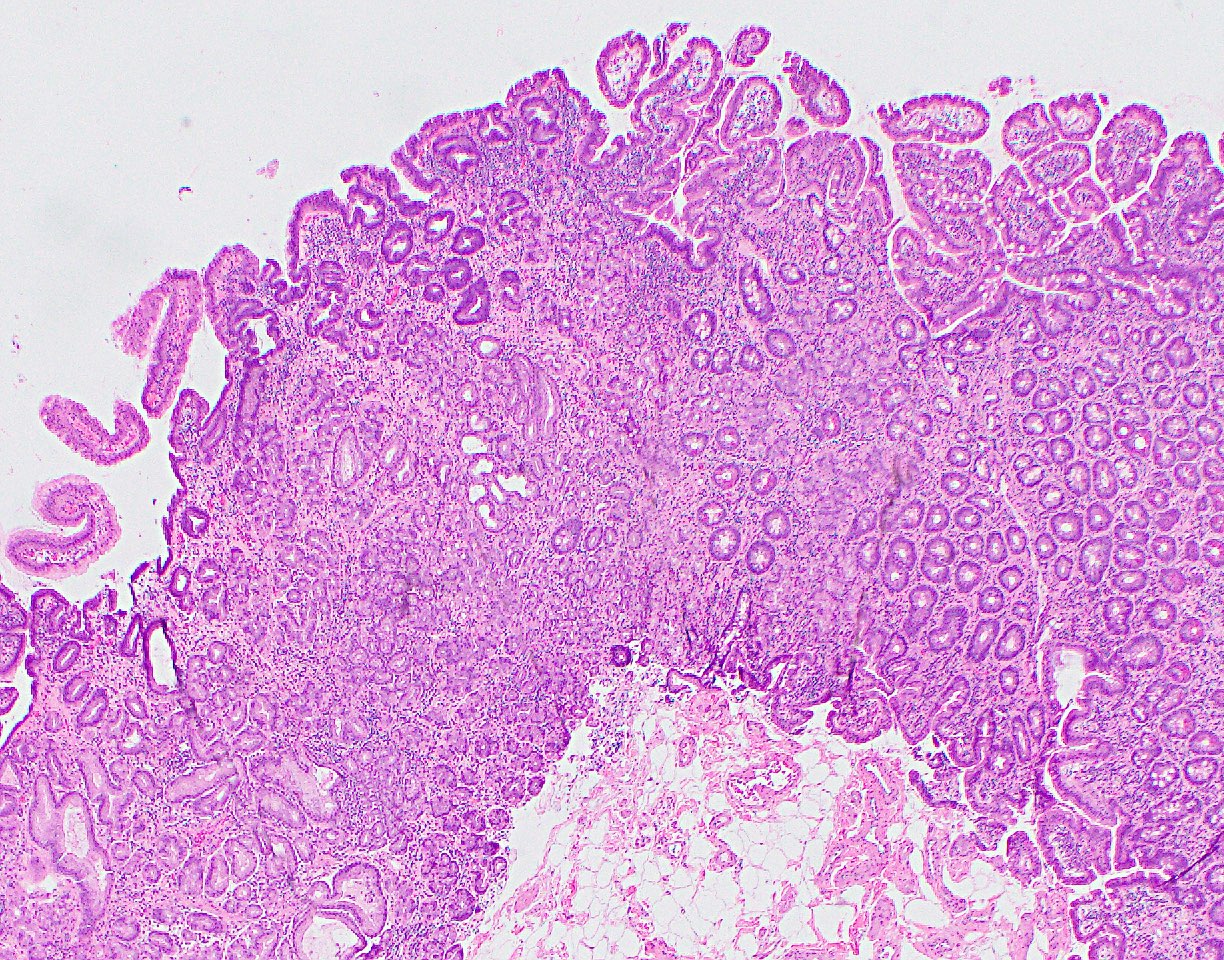
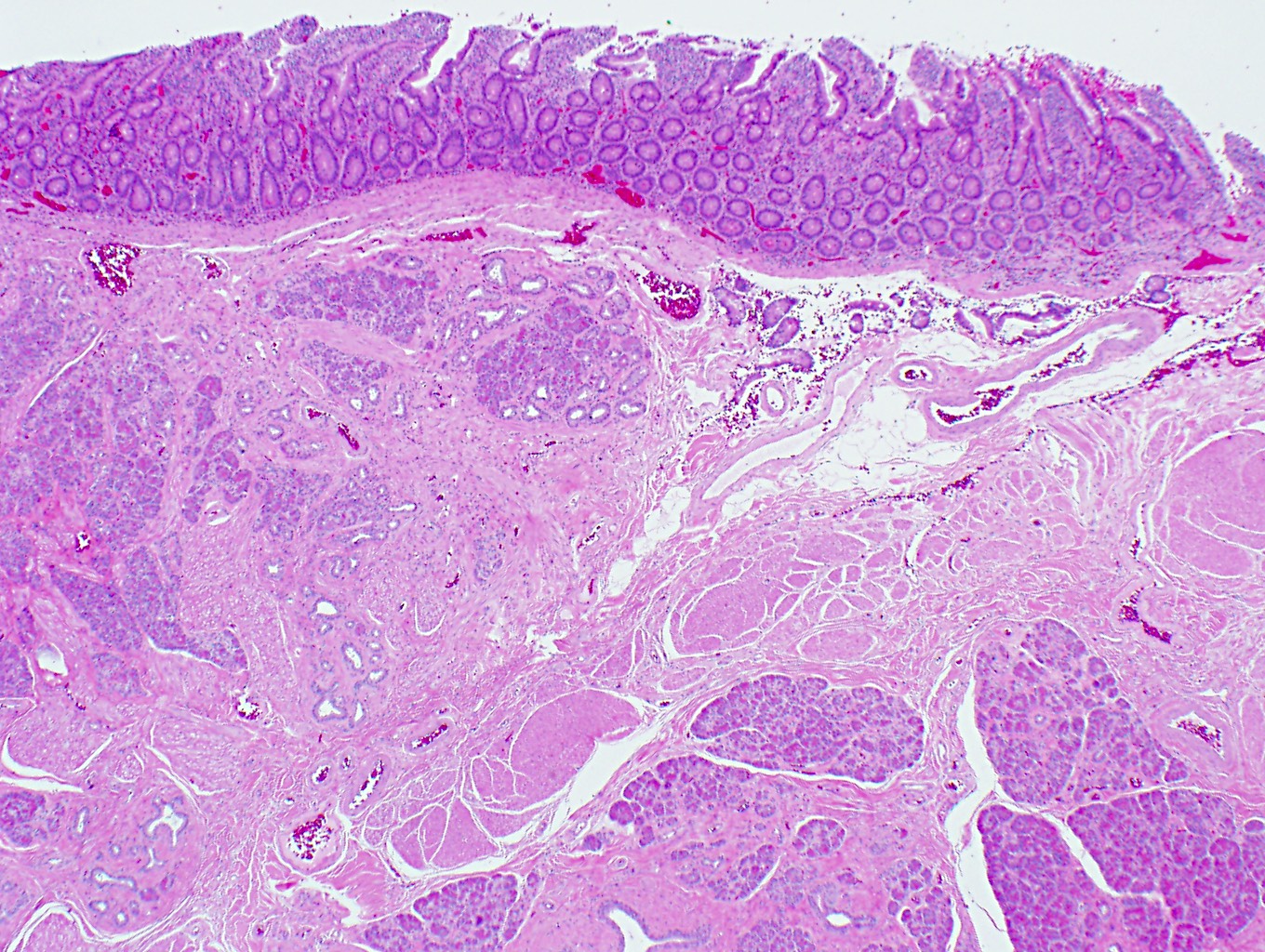
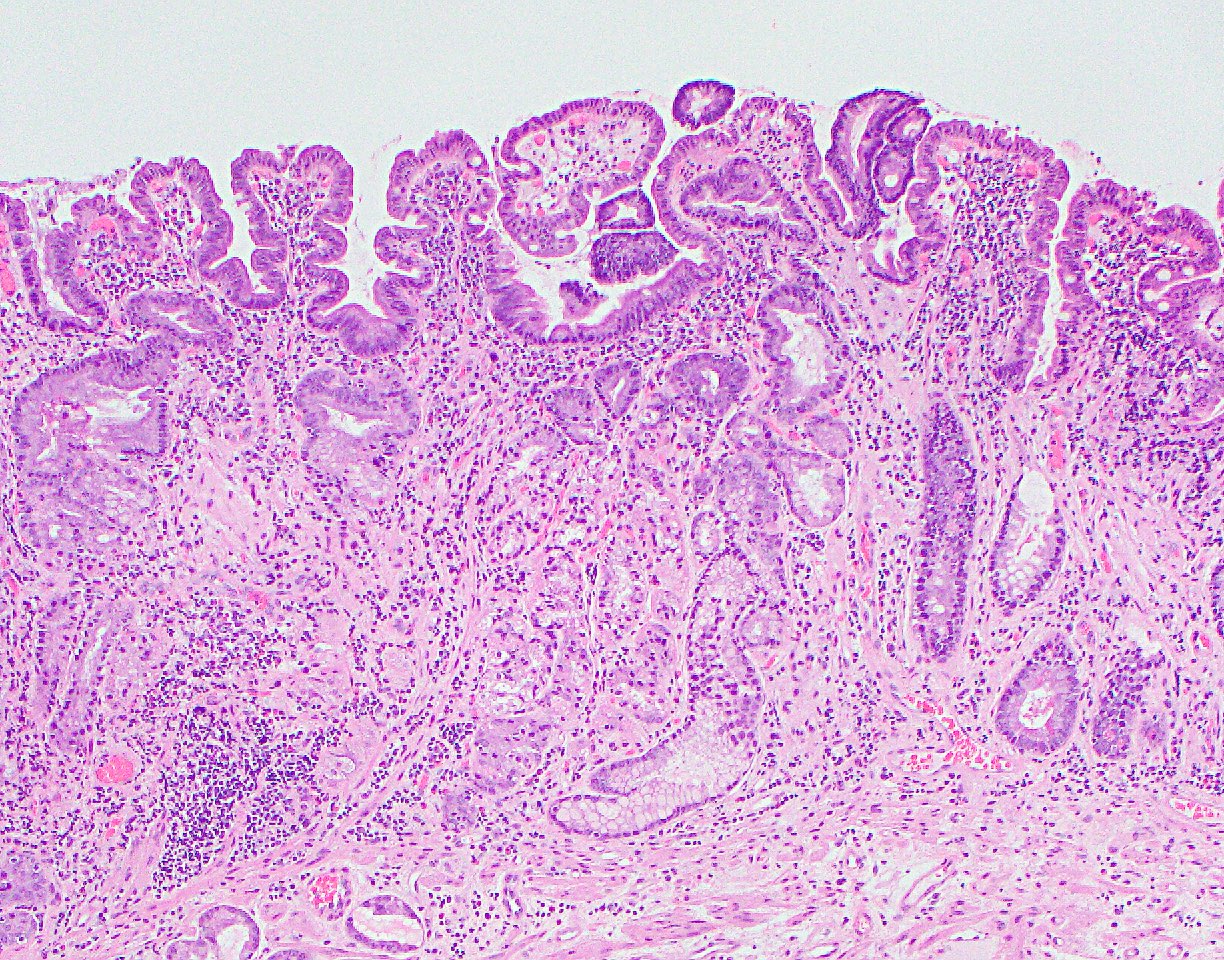
Microscopic (histologic) description
- True diverticulum that consists of all layers of intestinal wall
- Common abnormalities in symptomatic Meckel diverticulum are ectopic tissue, diverticulitis, enterolith and tumors
- Most common ectopic tissue seen in Meckel diverticulum is gastric mucosa, which may consist of gastric foveolar or oxyntic glands
- Helicobacter pylori has also been seen in the ectopic gastric mucosa (Pathology 1998;30:7)
- Second most common ectopic tissue is pancreatic tissue
- Other rare ectopic tissue includes jejunal, duodenal mucosa or Brunner tissue, colonic mucosa, endometriosis or hepatobiliary tissue
- Tumors can occur in the ectopic tissue: the most common tumor is neuroendocrine tumor (Ann Med Surg (Lond) 2019;43:75)
- Other rare tumors include adenocarcinoma, gastrointestinal stromal tumor, intraductal papillary mucinous neoplasm or pancreatic intraepithelial neoplasm (within pancreatic heterotopia), leiomyosarcoma, peripheral nerve sheath tumor and desmoplastic small round cell tumor (Ann Med Surg (Lond) 2019;43:75)
Microscopic (histologic) images
Sample pathology report
- Small bowel, ileum, segmental resection:
- Meckel diverticulum identified measuring 3 x 1 cm
- Located 50 cm from the ileocecal valve
- Ectopic pancreatic tissue identified within the diverticulum, otherwise unremarkable
Differential diagnosis
- Intestinal duplication or duplication cyst:
- Tubular or cystic
- Located at the mesenteric side
- Small bowel bleeding or perforation:
- No outpouching structures at the site of bleeding or perforation
- No ectopic tissue
Board review style question #1
A 2 year old boy presented with abdominal pain and bloody stool. He has otherwise been healthy and growing normally. On physical exam, the patient is irritable, with guarding of the right lower quadrant of the abdomen. Based on clinical suspicion, a technetium 99m pertechnetate scan demonstrates increased uptake in the right lower abdomen. Which of the following embryologic structures is associated with this patient’s condition?
- Allantois
- Ductus arteriosus
- Metanephric mesenchyme
- Omphalomesenteric duct
- Paramesonephric duct
Board review style answer #1
D. Omphalomesenteric duct. Meckel diverticulum is a remnant of the omphalomesenteric duct, which connects the yolk sac with the developing midgut in the fetal life. It normally regresses by the seventh to eighth week of gestation. The incomplete obliteration of the omphalomesenteric duct results in Meckel diverticulum.
Comment Here
Reference: Meckel diverticulum
Comment Here
Reference: Meckel diverticulum
Board review style question #2
Regarding the histologic finding in the section from a Meckel diverticulum, which of the following statements is true?
- Atypical glands suspicious for a malignancy
- Clinically not significant
- Commonly seen in Meckel diverticulum
- Metaplastic change
- Small bowel mucosa with no significant pathological changes
Board review style answer #2
C. Commonly seen in Meckel diverticulum. The picture shows ectopic gastric mucosa, which is the most common ectopic tissue in Meckel diverticulum, followed by pancreatic tissue. The most frequent complication of Meckel diverticulum is bleeding from ectopic gastric mucosa. Benign and malignant tumors can rarely occur in the ectopic tissue but the pyloric glands and rare oxyntic glands in this case are totally benign.
Comment Here
Reference: Meckel diverticulum
Comment Here
Reference: Meckel diverticulum