Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Staging | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Yan S. Squamous cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticscc.html. Accessed April 26th, 2024.
Definition / general
- Cutaneous squamous cell carcinoma is a malignancy of epidermal keratinocytes that displays variable degrees of differentiation and cytological features
Essential features
- Most patients have a favorable outcome after surgical resection
- Only a subset of patients carry a higher risk of local recurrence, distant metastasis and mortality
- Identifying and reporting the high risk features is important
Terminology
- Cutaneous squamous cell carcinoma (cSCC)
- Squamous cell carcinoma (SCC)
- Squamous cell carcinoma in situ (SCCIS)
- Bowen disease (BD)
ICD coding
- ICD-O: 8070/3 - squamous cell carcinoma, NOS
Epidemiology
- M > F
- Incidence: 5 - 499 per 1,000 individuals depending on the latitude (Hematol Oncol Clin North Am 2019;33:1)
Sites
- Most often in sun exposed areas
- Scalp, ear, lip, nose, eyelid are high risk anatomic sites
Pathophysiology
- Cutaneous squamous cell carcinoma appears to develop through a multistep process
- UV radiation, mutations involving genes (such as TP53, CDKN2A, NOTCH1 and NOTCH2, EGFR and TERT) and molecular pathways (RAS / RAF / MEK / ERK and PI3K / AKT / mTOR) have been shown to play an important role in the pathogenesis (J Eur Acad Dermatol Venereol 2020;34:932)
Etiology
- Ultraviolet light radiation and other forms of radiation
- Chronic immunosuppressions
- Actinic keratosis (precursor lesion), albinism (lack of pigmentation in skin), arsenic
- Burn scars
- Chronic ulcers
- Chronic inflammation
- Sinus tract
- Human papillomavirus infection
- Tars / oils
- Xeroderma pigmentosa (J Am Acad Dermatol 2018;78:237)
Clinical features
- Thin squamous cell carcinoma: erythematous scaly thin papule or plaque
- Thicker tumors typically present as erythematous plaque, nodule, ulcer (Eur J Cancer 2015;51:1989)
Diagnosis
- Characteristic gross features are suggestive of the diagnosis
- Definitive diagnosis is made by shave, punch or excisional biopsies
Prognostic factors
- Diameter: > 2 cm doubles the risk of recurrence, triples the rate of metastasis (JAMA Dermatol 2016;152:419)
- Depth: > 2 mm, tenfold higher risk of local recurrence
- Beyond subcutaneous fat, elevenfold higher risk of metastasis (Lancet Oncol 2008;9:713, JAMA Dermatol 2016;152:419)
- Perineural invasion: involved nerves ≥ 0.1 mm associated with increased nodal metastases (Dermatol Surg 2009;35:1859)
- Differentiation: poor differentiation indicates poor prognosis (Lancet Oncol 2008;9:713)
- Lymphovascular invasion: risk factor for lymph node metastasis (Laryngoscope 2005;115:1561)
- Site: high risk anatomic sites (scalp, ear, lip, nose, eyelid) (J Am Acad Dermatol 1992;26:976, JAMA Dermatol 2018;154:701)
- Immunosuppression: increased recurrence (13%) and metastasis (5 - 8%) (Hematol Oncol Clin North Am 2019;33:1)
- Previously treated / recurrent: worse prognosis compared to primary tumors
- Arising in scar: arising from ulcer, burn scar, radiation dermatitis and other chronic wounds have increased rate of metastasis (J Am Acad Dermatol 1992;26:976)
Staging
- Based on lesion size, depth of invasion, differentiation and perineural invasion
- Helps to identify cutaneous squamous cell carcinomas with worse prognosis
- 3 major staging methods (J Am Acad Dermatol 2019;80:106, JAMA Dermatol 2018;154:428)
- AJCC, seventh edition of the American Joint Committee on Cancer (this staging system is not included in the eighth edition)
- pT1: Tumor diameter < 2 cm, with < 2 high risk factors
- pT2: Tumor diameter ≥ 2 cm or with ≥ 2 high risk factorsa
- pT3: Tumor with invasion of maxilla, mandibular, orbit or temporal bone
- pT4: Tumor with invasion of skeleton (axial or appendicular) or perineural invasion of skull base
- aHigh risk factors: tumor thickness > 2 mm, Clark level IV / V, poor or undifferentiated, perineural invasion (PNI), location at ear or lip
- AJCC, eighth edition of the American Joint Committee on Cancer for cutaneous squamous cell carcinoma of the head and neck
- pT1: Tumor diameter ≤ 2 cm
- pT2: Tumor diameter ≥ 2 cm and < 4 cm
- pT3: Tumor with diameter ≥ 4 cm or with one of the high risk featuresb
- pT4a: Tumor with gross cortical bone / marrow invasion of maxilla, mandibular orbit or temporal bone
- pT4b: Tumor with skull base invasion or skull base foramen involvement
- bHigh risk features: perineural invasion (of a nerve lying beneath the dermis or ≥ 0.1 mm in caliber or presenting with clinical or radiographic involvement of named nerves without skull base invasion or transgression), deep invasion (involvement beyond the subcutaneous fat or > 6 mm) and minor bone erosion
- Brigham and Women's Hospital (BWH) classification
- pT1: 0 high risk factorsc
- pT2a: 1 high risk factor
- pT2b: 2 - 3 high risk factors
- pT3: ≥ 4 high risk factors or bone invasion
- cHigh risk factors: tumor diameter ≥ 2 cm, poorly differentiated, perineural invasion ≥ 0.1 mm or tumor invasion beyond fat
- AJCC, seventh edition of the American Joint Committee on Cancer (this staging system is not included in the eighth edition)
Case reports
- 40 year old man with pseudovascular adenoid squamous cell carcinoma of oral cavity (J Oral Maxillofac Pathol 2012;16:288)
- 43 and 82 year old Japanese women immunosuppressed with chronic human papillomavirus infection (Case Rep Dermatol 2015;7:178)
- 54 year old man with tumor in burn wound that recurred with direct invasion of the pleural (Cureus 2019;11:e5115)
- 57 year old woman with adenoid squamous carcinoma of vulva (Int J Gynecol Pathol 2008;27:288)
- 64 year old man with a rapidly growing tumor in left buttock and intergluteal cleft area (SAGE Open Med Case Rep 2019;7:2050313X19847359)
- 73 year old woman with adenoid squamous cell carcinoma of oral cavity (Int J Clin Exp Pathol 2012;5:442)
- 87 year old woman with cutaneous spindle cell carcinoma following basal cell carcinoma (Am J Dermatopathol 2005;27:17)
- 87 year old woman with sarcomatoid carcinoma of hand (Clin Exp Dermatol 2012;37:505)
- 88 year old woman with a recurrence on left lower leg (JAAD Case Rep 2019;5:491)
- Rare case of poorly differentiated squamous cell carcinoma with osteoclastic giant cell-like proliferation (J Cutan Pathol 2007;34:930)
Treatment
- Mohs, surgical excision with adequate margins, especially for high risk squamous cell carcinoma
- Also curettage, electrodessication, cryotherapy, radiation therapy (J Cutan Pathol 2016;43:994)
- Immunotherapy if inoperable (JAAD Case Rep 2019;5:491)
Clinical images
Gross description
- Often hyperkeratotic scaly plaque
- May have induration, ulceration, hemorrhage (Eur J Cancer 2015;51:1989)
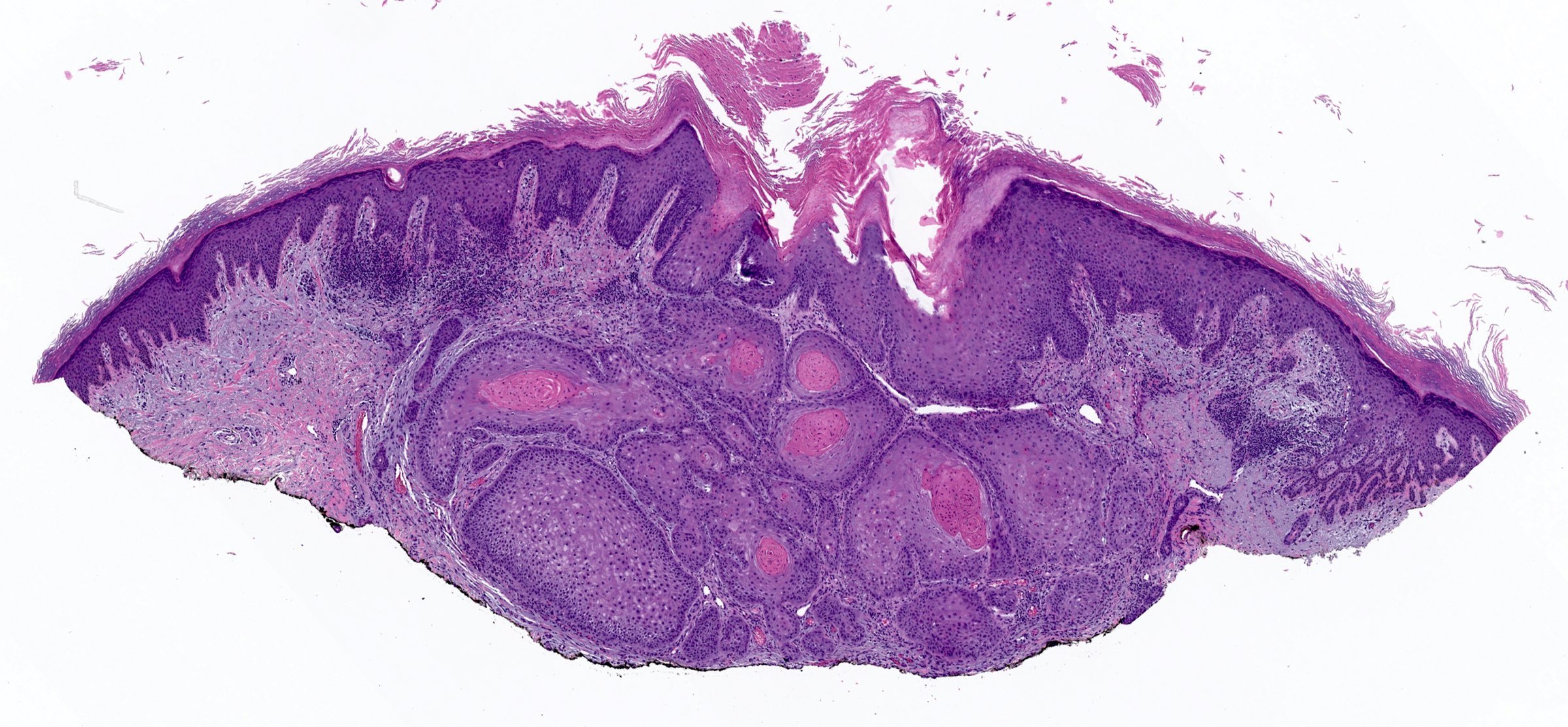
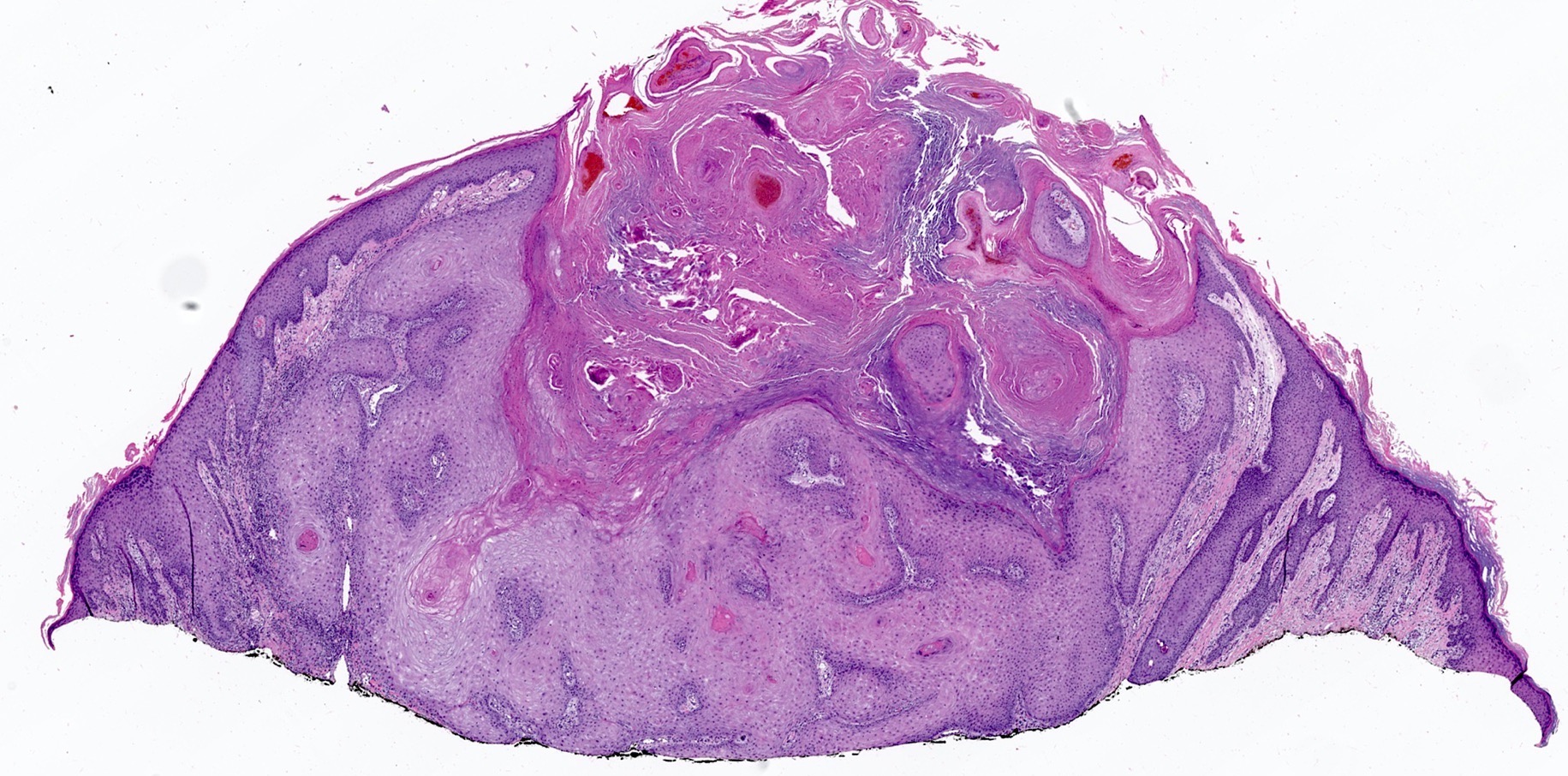
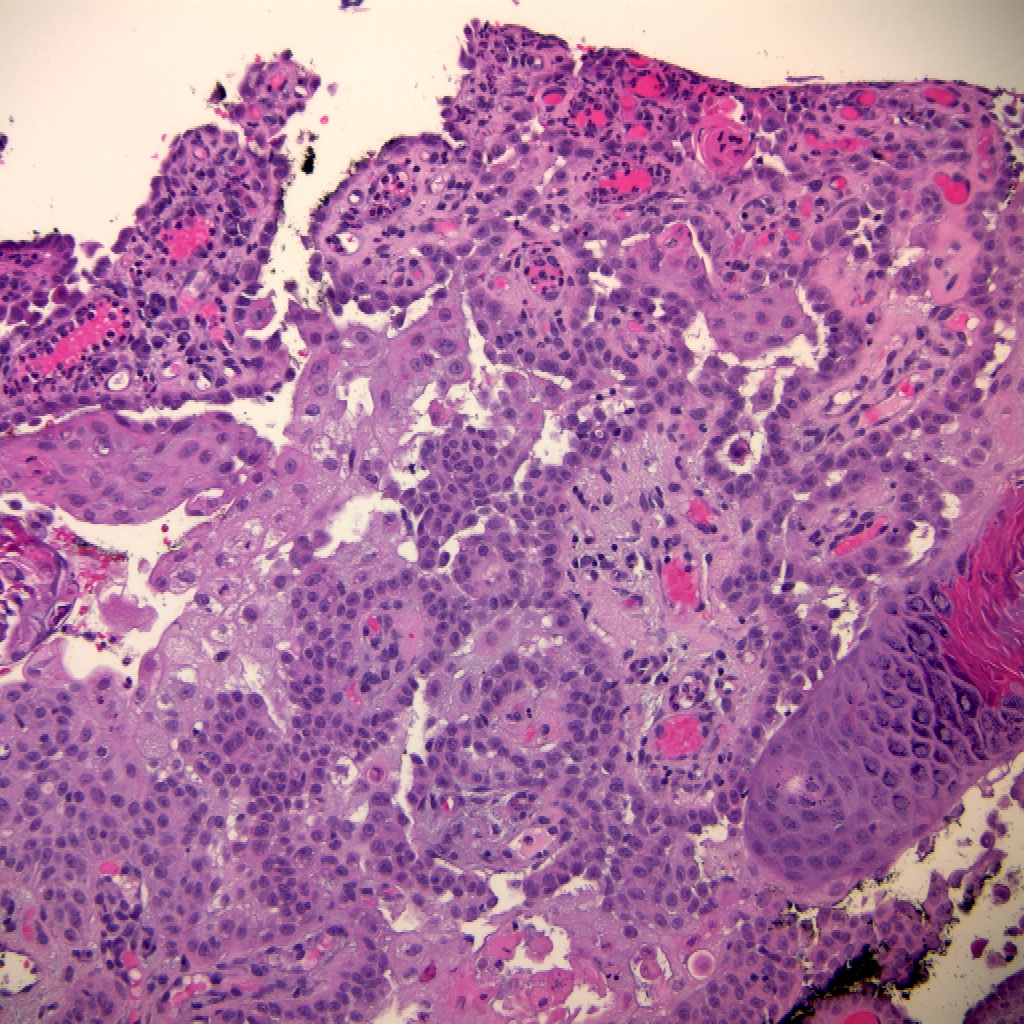
Microscopic (histologic) description
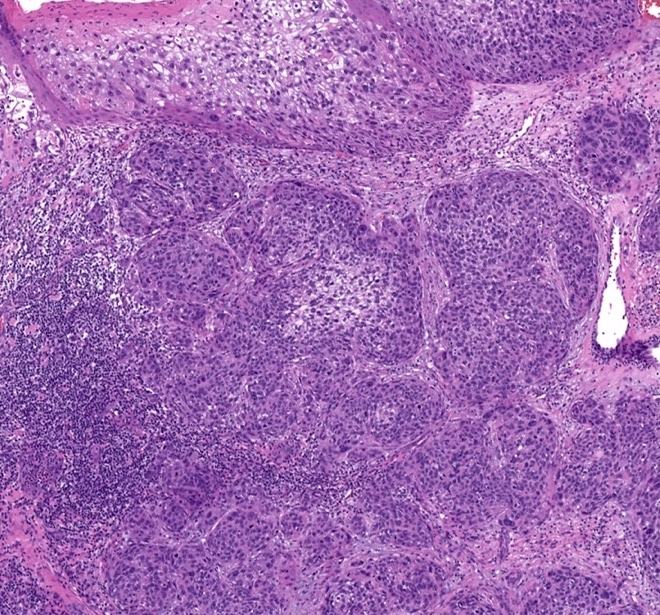
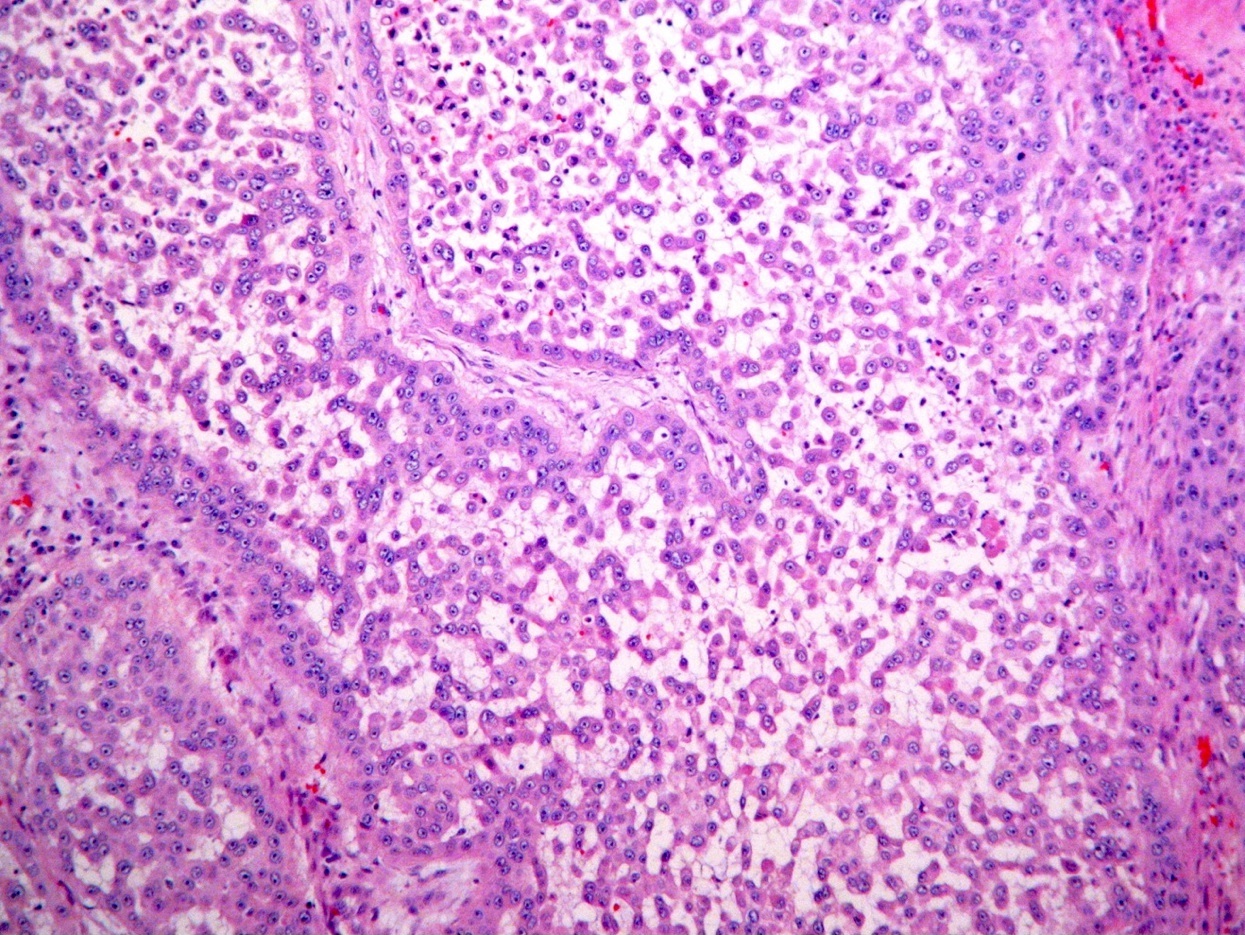
- Carcinoma of keratinocytes that infiltrates the dermis
- An associated precursor lesion (actinic keratosis / keratinocytic dysplasia / squamous cell carcinoma in situ) is often present
- Spectrum of histologic features; all share downward growth below level of adjacent or overlying epidermis
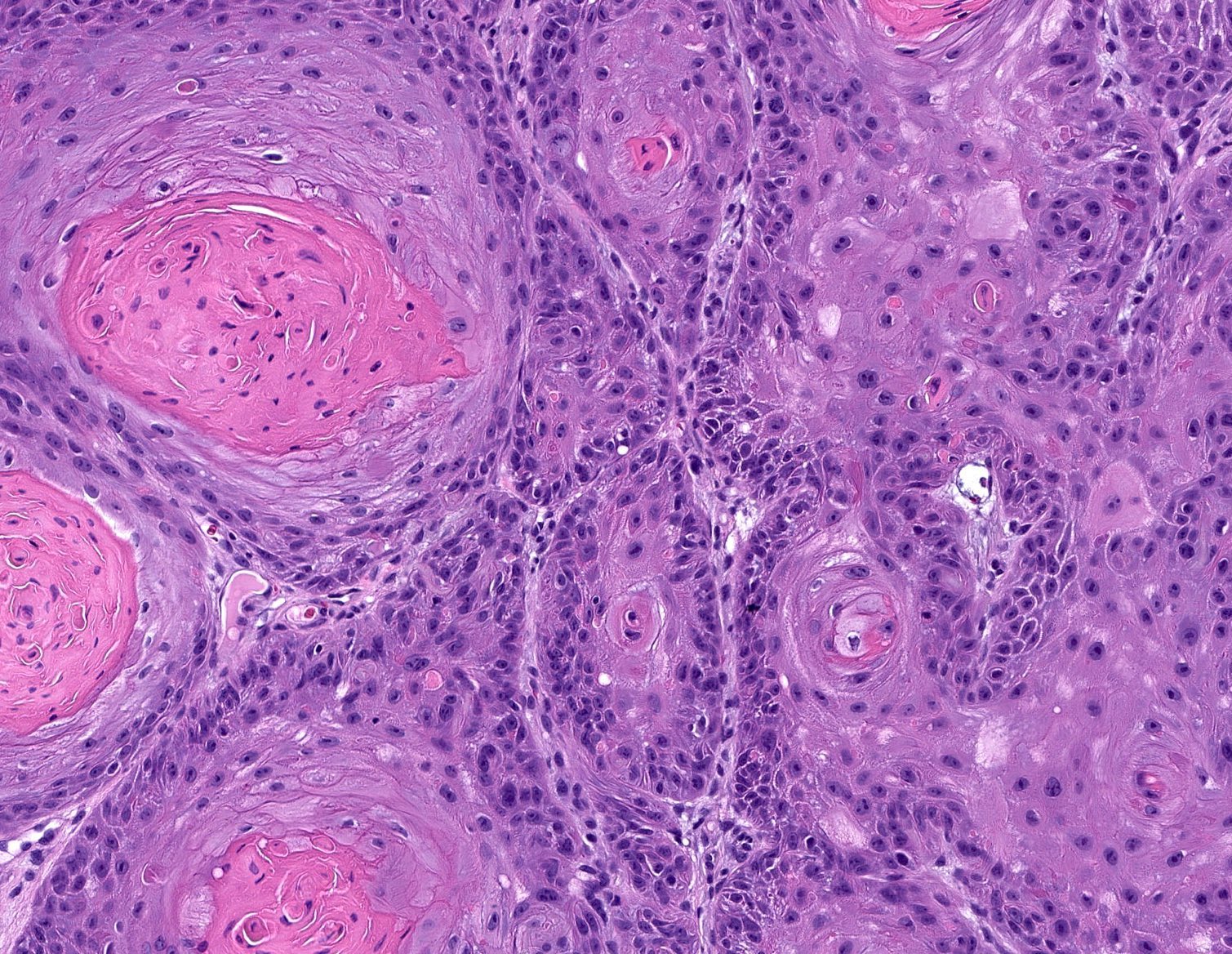
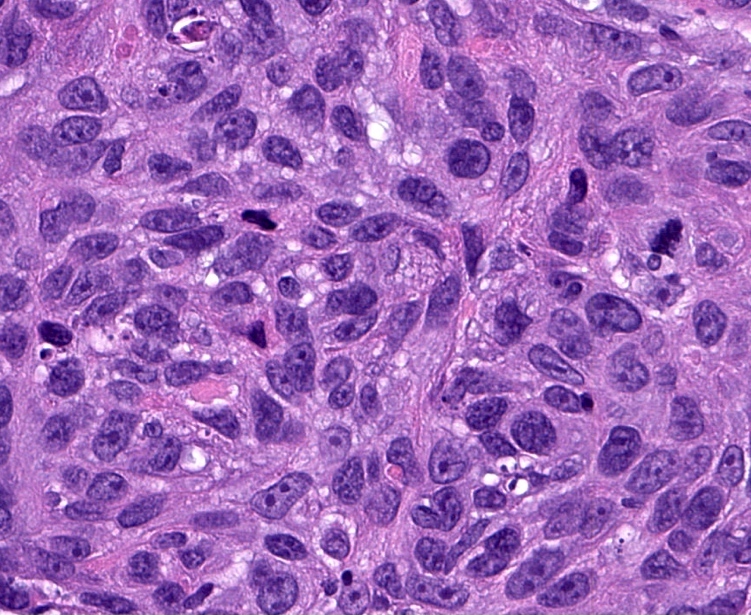
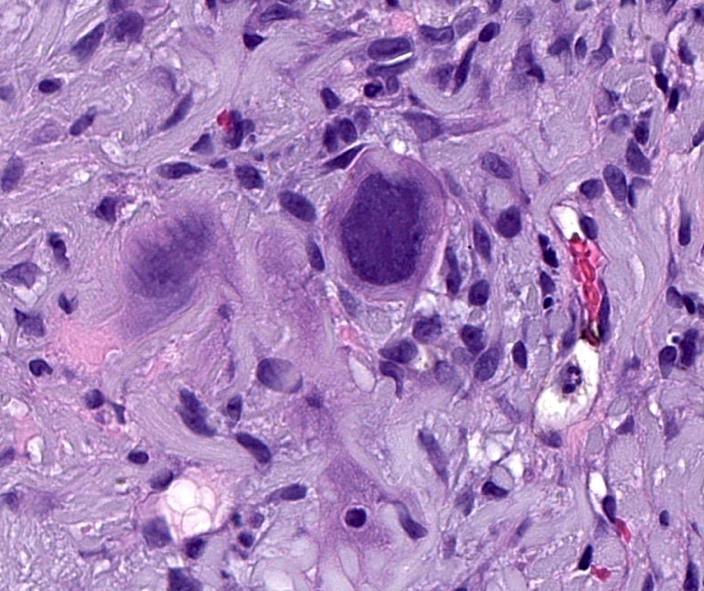
- Grading based on degree of differentiation and keratinization (J Am Acad Dermatol 2018;78:237)
- Well differentiated: easily recognizable squamous epithelium, abundant keratinization, intercellular bridges apparent, minimal pleomorphism, mitotic figures basally located
- Moderately differentiated: focal keratinization; features between well and poorly differentiated
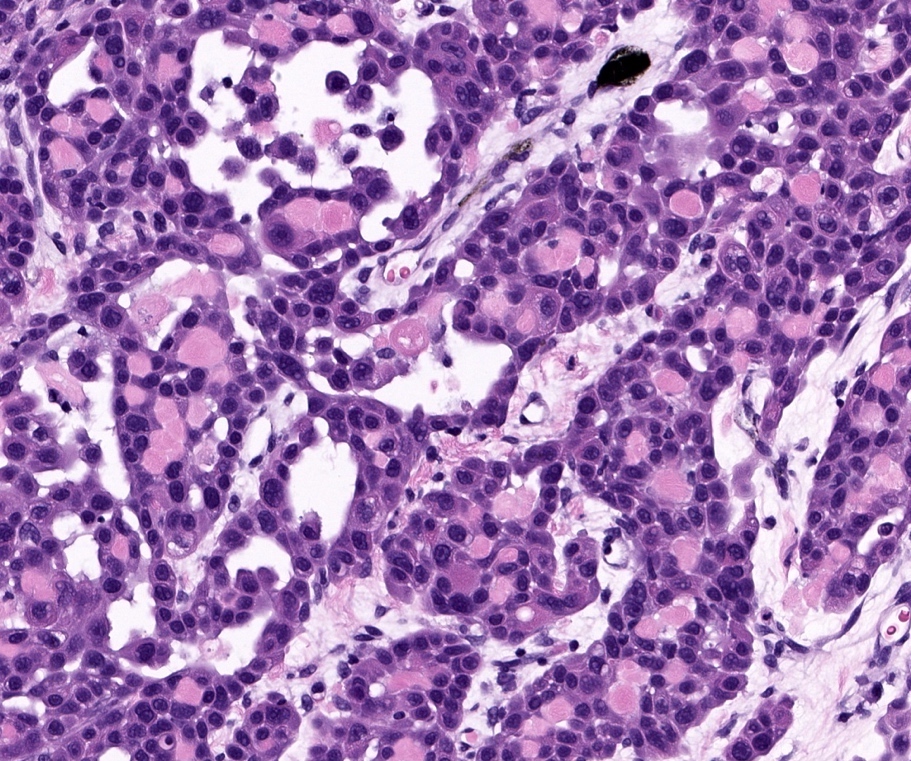
- Poorly differentiated: no / minimal keratinization, marked nuclear atypia, may be difficult to establish squamous differentiation
- Undifferentiated: no keratinization, immunohistochemistry is usually necessary to confirm the diagnosis and to exclude melanoma or sarcoma
- Histologic patterns (Hematol Oncol Clin North Am 2019;33:1)
- Low risk histologic variants
- Keratoacanthoma: well differentiated, crateriform appearance
- Verrucous carcinoma: verruciform surface, blunt endophytic growth, minimal atypia
- Clear cell squamous cell carcinoma: > 25% cells with cytoplasmic clearing (glycogen accumulation or hydropic degeneration)
- High risk histologic variants
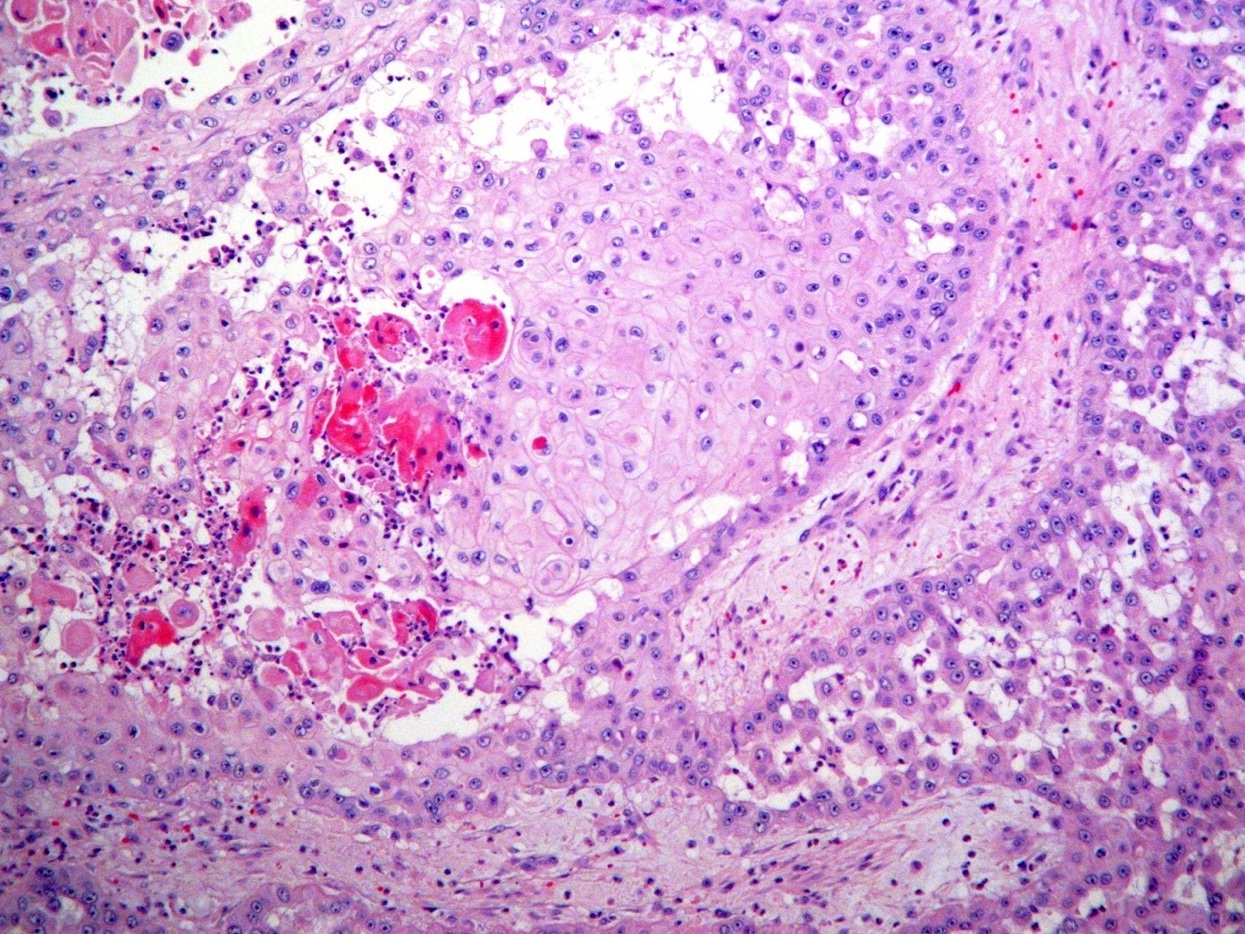
- Acantholytic: squamous cell carcinoma with acantholysis, pseudoglandular (CEA negative) (J Cutan Pathol 2022;49:133, J Clin Pathol 2006;59:1206, Dermatol Surg 2011;37:353)
- Acantholysis is the loss of cell to cell connections between keratinocytes, resulting in loss of intercellular cohesion
- Acantholytic cutaneous squamous cell carcinomas have been classically considered as a high risk variant of CSCC; however, some recent studies show that acantholytic squamous cell carcinomas does not confer more aggressiveness
- Invasive Bowen disease: invasive islands of squamous and basaloid cells with overlying classic Bowen disease
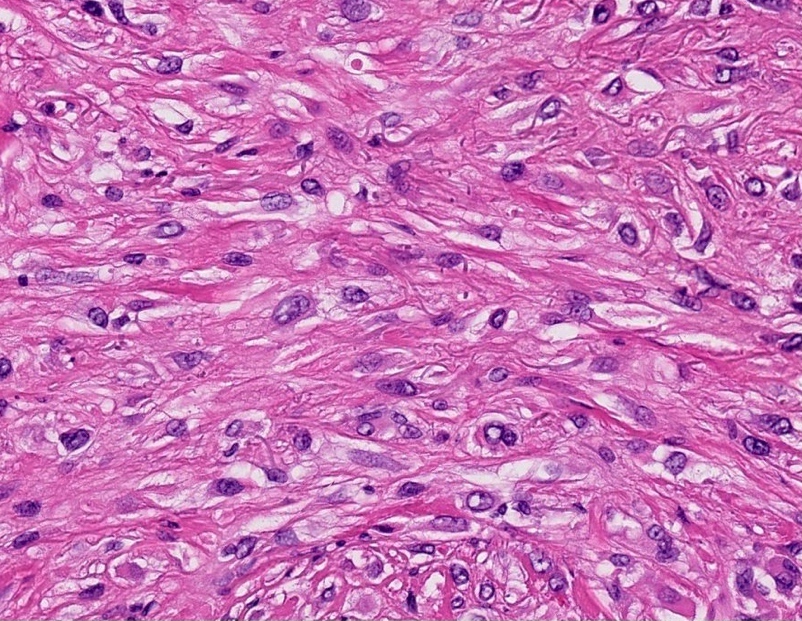
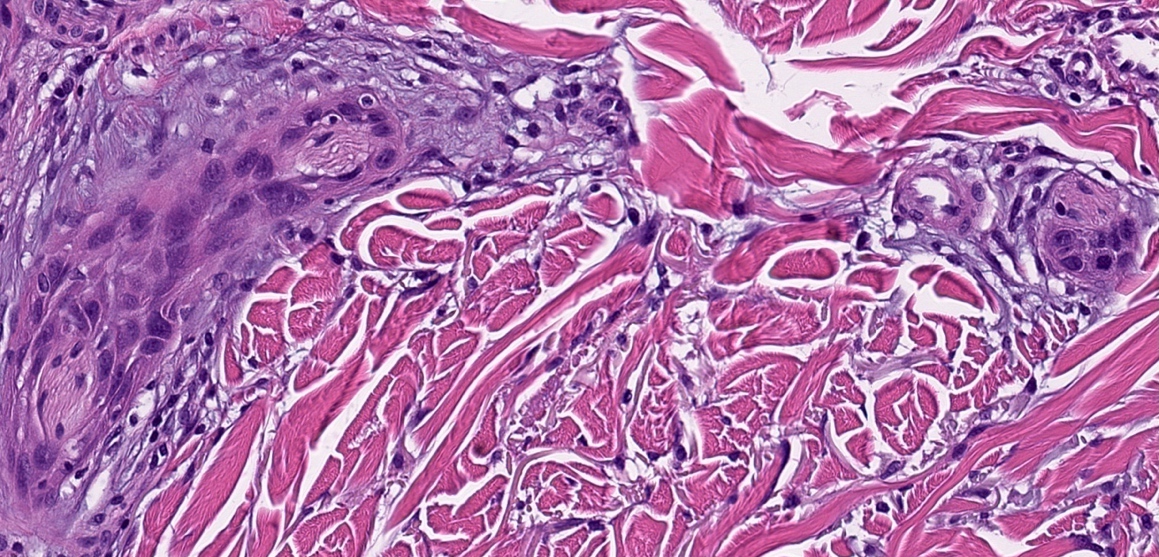
- Spindle cell squamous cell carcinoma:
- Uncommon variant in which keratinocytes infiltrate dermis as single cells with elongated nuclei, not as cohesive nests or islands and there are no / minimal signs of keratinization of conventional squamous cell carcinoma (Am J Dermatopathol 2008;30:228, J Skin Cancer 2011;2011:210813)
- Commonly associated with a good prognosis, less often associated with a poor prognosis following exposure to ionizing radiation, trauma or burn
- Desmoplastic squamous cell carcinoma: poorly differentiated, pleomorphic spindle cells with a dense stromal response
- Adenosquamous carcinoma: mixed squamous and glandular differentiation (CEA positive)
- Acantholytic: squamous cell carcinoma with acantholysis, pseudoglandular (CEA negative) (J Cutan Pathol 2022;49:133, J Clin Pathol 2006;59:1206, Dermatol Surg 2011;37:353)
- Uncommon variants
- Lymphoepitheliomatous
- Pseudovascular squamous cell carcinoma
- Squamous cell carcinoma with sarcomatoid differentiation
- Squamous cell carcinoma with osteoclast-like cells
- Low risk histologic variants
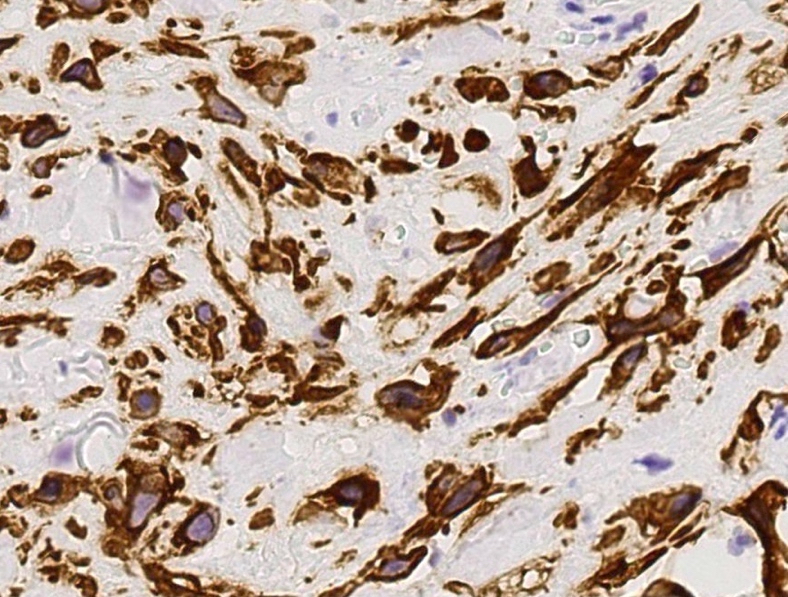
Microscopic (histologic) images
Contributed by Shaofeng Yan, M.D., Ph.D. and Semir Vranić, M.D., Ph.D.
Sample pathology report
- Skin, left temple, shave biopsy:
- Invasive squamous cell carcinoma, well differentiated, present at the peripheral and deep specimen edges
- Skin, left temple, excision:
- Invasive squamous cell carcinoma, poorly differentiated, present at the peripheral specimen margin (see synoptic report)
Differential diagnosis
- Inflammatory dermatoses:
- Hypertrophic lupus erythematosus, lichen planus:
- Both can mimic due to marked squamous hyperplasia particularly if clinical information is not available
- Absence of infiltrating squamous epithelium, presence of multiple lesions and features of lupus erythematosus (such as vacuolar interface lymphocytic infiltrate, necrotic keratinocytes, increase of dermal mucin, superficial and deep perivascular and periadnexal lymphocytic infiltrate) or lichen planus (such as wedge shaped hypergranulosis, band-like lymphocytic infiltrate with colloid bodies) are key differentiators
- Hypertrophic lupus erythematosus, lichen planus:
- Miscellaneous keratoses:
- Proliferative actinic keratosis:
- Epithelial dysplasia variable from mild basal layer changes to carcinoma in situ and often associated with solar elastosis and parakeratosis
- Budding of atypical epithelium into the papillary dermis
- Distinction from early invasive squamous cell carcinoma is somewhat artificial, the presence of single or groups of atypical keratinocytes detached from the main lesion or associated with a stromal reaction supports invasive squamous cell carcinoma
- Inverted follicular keratosis, clonal seborrheic keratosis:
- Intradermal or inverted type of seborrheic keratosis is known as inverted follicular keratosis and is characterized by intradermal whorls of maturing squamous epithelium, so called squamous eddies
- Sometimes, intraepithelial nesting gives rise to the intraepidermal epitheliomatous (Borst-Jadassohn) nodular appearance, surrounded by normal basaloid cells; this is also called clonal seborrheic keratosis
- Proliferative actinic keratosis:
- Other malignant tumors:
- Basal cell carcinoma:
- Frequently originates from the overlying and consists of small basaloid cells with peripheral palisading, darkly staining nuclei and minimal cytoplasm
- Intercellular bridges are not as evident
- Mitoses and apoptosis are commonly present
- Adnexal carcinoma:
- Malignant melanoma, sarcoma, lymphoma:
- Adequate sampling to detect an epithelial origin or a junctional component is important
- Cytokeratin, SOX10, CD45 or desmin will usually enable distinction from melanoma, lymphoma, sarcoma (or leiomyosarcoma)
- p63 or p40 are usually negative in atypical fibroxanthoma or undifferentiated pleomorphic sarcoma
- Basal cell carcinoma:
- Pseudoepitheliomatous hyperplasia:
- After trauma, surgery, infection; may be associated with granular cell tumor
- Can be seen in association with chronic healing wounds, chronic irritation and infection
- Benign and reactive epidermal acanthosis showing irregular and often endophytic growth pattern
- Prominent acanthotic downgrowths and keratinocytes with bland nuclear features containing abundant cytoplasm
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is a good prognostic factor for cutaneous squamous cell carcinoma?
- Desmoplastic type squamous cell carcinoma
- Keratoacanthoma type squamous cell carcinoma
- Tumor invades beyond subcutaneous fat
- Tumor size > 2 cm
Board review style answer #2