Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Manafi F, Anani O, Asadbeigi SN. Sebaceous hyperplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticsenilesebaceoushyperplasia.html. Accessed April 3rd, 2025.
Definition / general
- Most common sebaceous gland neoplasm; benign
- Usually affects elderly patients on the face (Diagnostics (Basel) 2023;13:1676, StatPearls: Sebaceous Hyperplasia [Accessed 21 November 2024], J Invest Dermatol 1978;70:207)
Essential features
- Increased number and size of normal appearing sebaceous lobules
- Typically associated with a central hair follicle, which may be dilated (Pathology 2017;49:688)
- Peripheral basaloid germinative cell layer is not expanded and does not exceed 1 - 2 cell layer(s) (Histopathology 2020;76:640)
Terminology
- Sebaceous hyperplasia
- Sebaceous gland hyperplasia
- Sebaceous glandular hyperplasia
ICD coding
Epidemiology
- Affects people of middle age and older (StatPearls: Sebaceous Hyperplasia [Accessed 21 November 2024], J Invest Dermatol 1978;70:207)
- Mostly affects men (StatPearls: Sebaceous Hyperplasia [Accessed 21 November 2024], J Am Acad Dermatol 1997;36:120)
- Common and transient in newborns due to maternal hormone withdrawal (Pediatr Dermatol 2006;23:61)
- Prevalence in general population is estimated to be ~1% (J Am Acad Dermatol 2006;55:878)
- Incidence among patients receiving systemic corticosteroid therapy is > 10% (Ginekol Pol 2023;94:509)
Sites
- Most often presents on nose, cheeks and forehead
- Occasionally appears on chest, areola, mouth, scrotum, foreskin, shaft of penis or vulva (Int J Dermatol 1991;30:306, BMJ Case Rep 2014;2014:bcr2014204025, Ann Dermatol 2011;23:S341, Ginekol Pol 2023;94:509)
Pathophysiology
- Sebaceous glands are highly sensitive to androgens: decreasing levels of androgens with aging → lowers sebocytes turnover → feedback stimulates proliferation → sweat gland hyperplasia
- Positive feedback from hormonal influences, such as hydrocortisone, thyroid stimulating hormone (TSH) and insulin, leads to sebaceous hyperplasia (Ginekol Pol 2023;94:509)
- Other factors that can promote sebaceous gland hyperplasia: ultraviolet exposure, hydrocortisone
- Some medications, such as immunotherapeutic medication and specifically cyclosporine, HIV antiretroviral treatment and steroids (J Drugs Dermatol 2018;17:118, Clin Exp Dermatol 2008;33:354)
Etiology
- Sporadic in advanced age
- Congenital disorder
- Genetic predisposition
- Immunosuppressive medication
- Muir-Torre syndrome (Br J Dermatol 2003;149:198)
Clinical features
- Soft, discrete, yellow-white or skin colored papules with central umbilication, usually incidentally discovered and described as asymptomatic; patients can present for cosmetic concerns
- Several variants exist: singularly, grouped, diffuse, extensive or juxtaclavicular beaded lines
- Juxtaclavicular beaded lines are characterized as papules arranged in parallel rows within the skin of the neck and overlying the clavicle (J Cutan Pathol 1991;18:464)
Diagnosis
- Presumptive diagnosis is made using clinical examination; confirmatory diagnosis can be made upon biopsy and subsequent histologic examination
Case reports
- 26 year old man presented with sebaceous hyperplasia of the face, neck and precordium (J Dermatol 2022;49:e226)
- Woman in her 30s presented with a sebaceous hyperplasia involving both nipples and areolae (BMJ Case Rep 2023;16:e258492)
- 38 year old man with a history of renal transplants presented with sebaceous hyperplasia (HCA Healthc J Med 2023;4:315)
- 52 year old man presented with gradually enlarging sebaceous hyperplasia on the lower eyelid (Heliyon 2024;10:e28511)
- 59 year old woman developed sebaceous hyperplasia after excimer phototherapy (Ann Dermatol 2023;35:S268)
Treatment
- Disease is benign and treatment is usually not indicated; typically treated for cosmetic reasons
- Traditional treatments of sebaceous hyperplasia include cryosurgery, electrodessication, curettage, shave excision and topical trichloroacetic acid (TCA)
- Isotretinoin has proven effective in treating sebaceous hyperplasia; however, it is associated with adverse effects and the lesions can reappear quickly once the medication is stopped
- Light and laser based treatments provide an alternative to traditional treatment modalities for treatment of sebaceous hyperplasia, demonstrating minimal side effects and no long term adverse effects (J Eur Acad Dermatol Venereol 2015;29:2080)
Clinical images
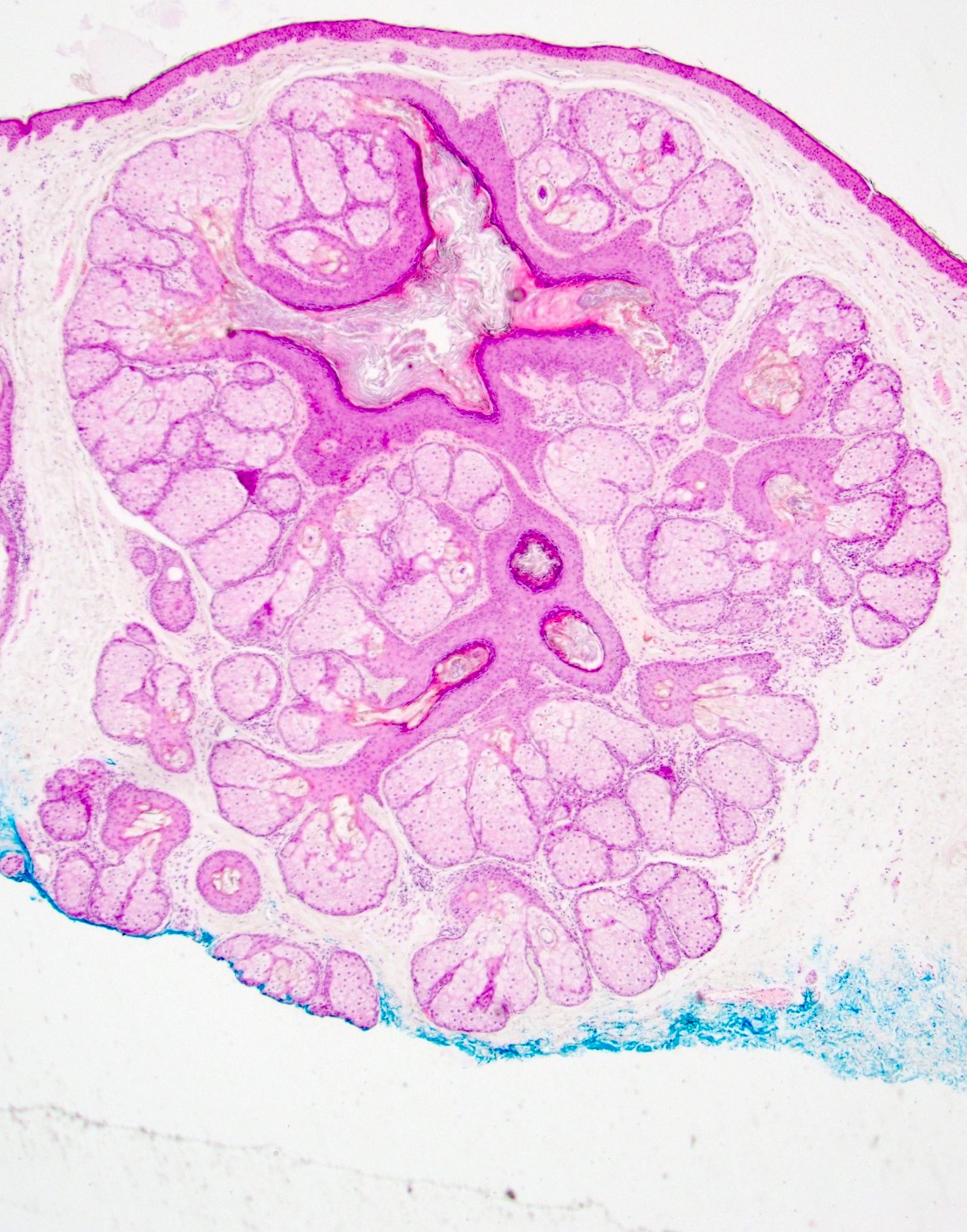
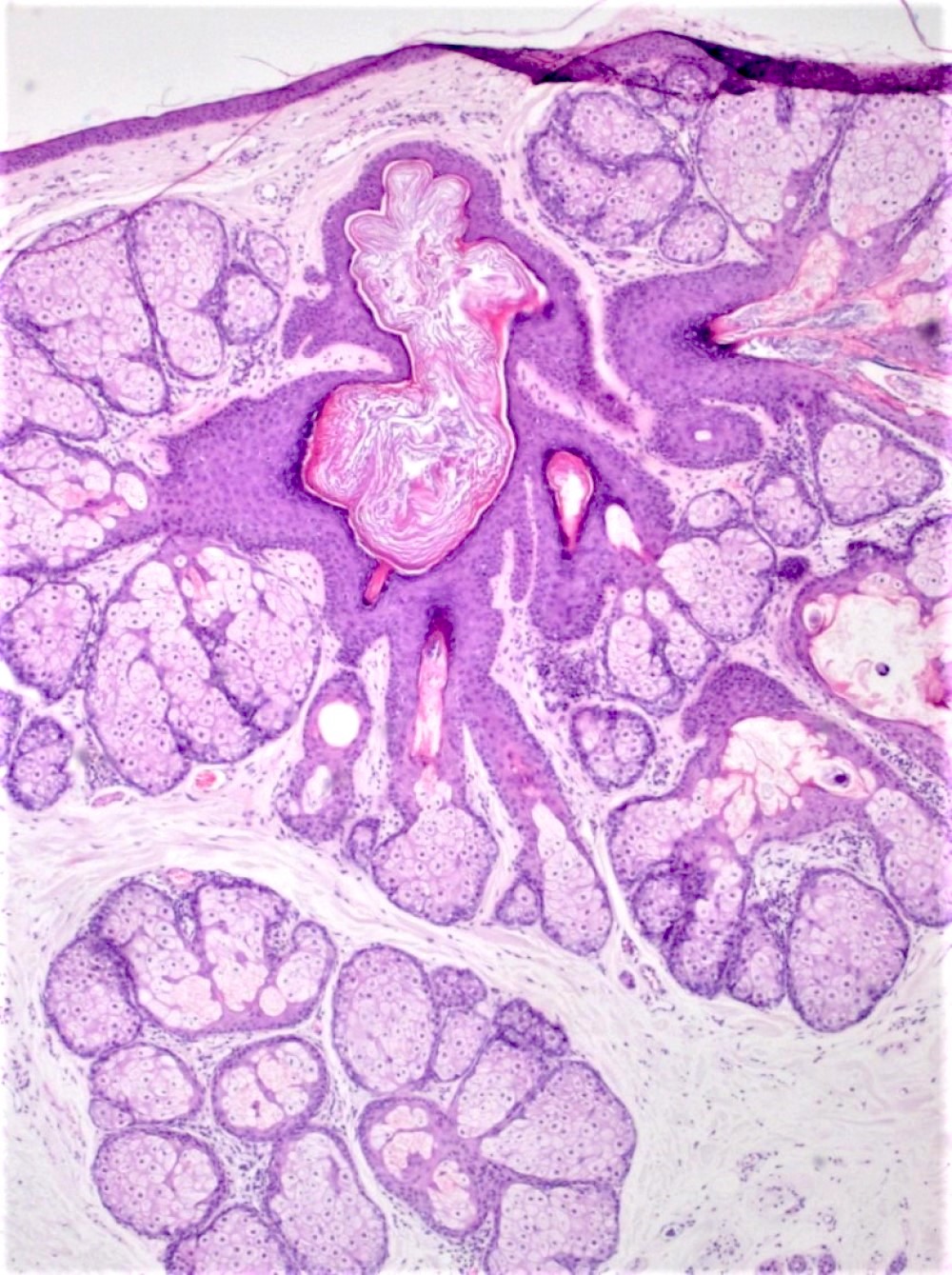
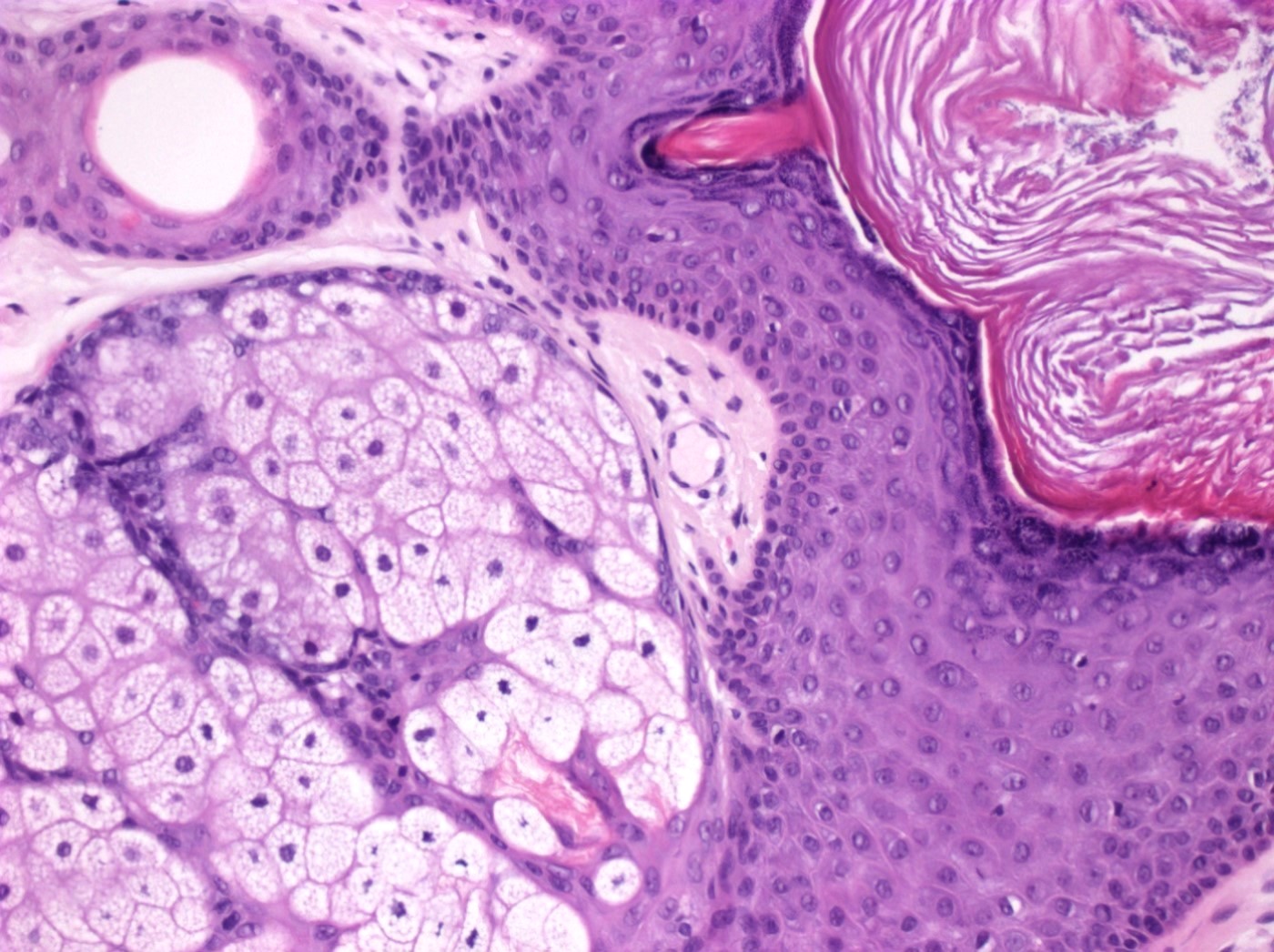
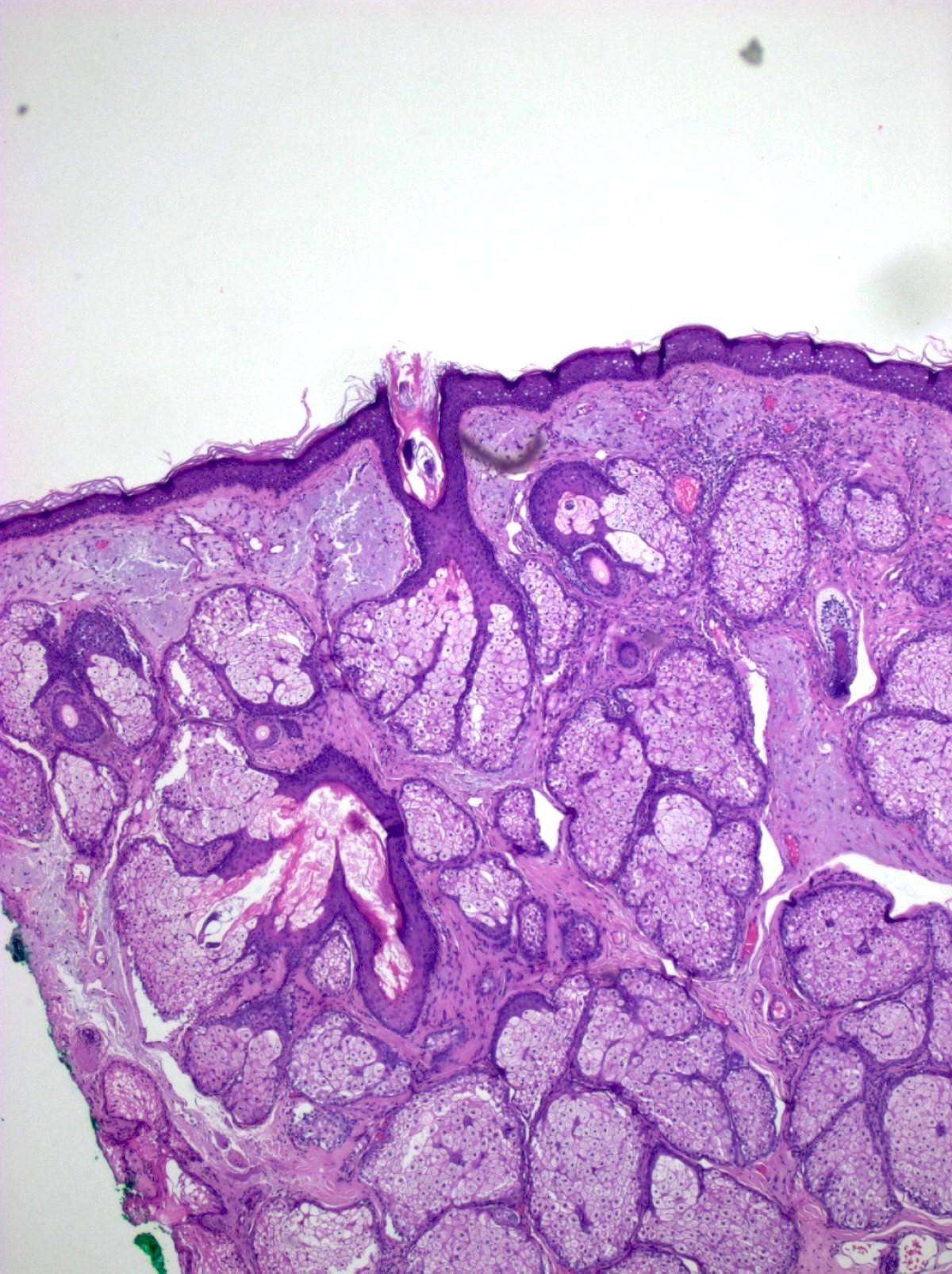
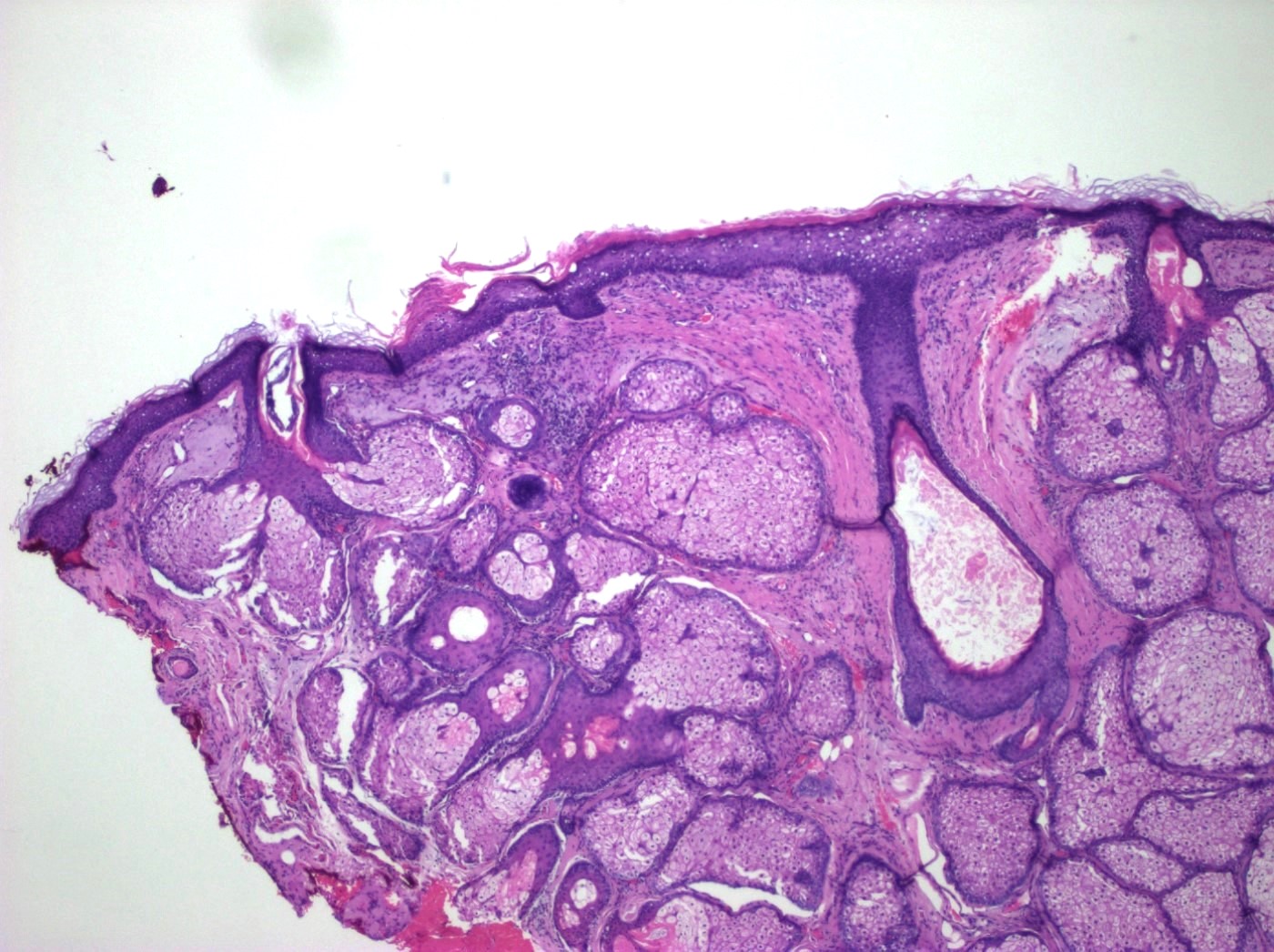
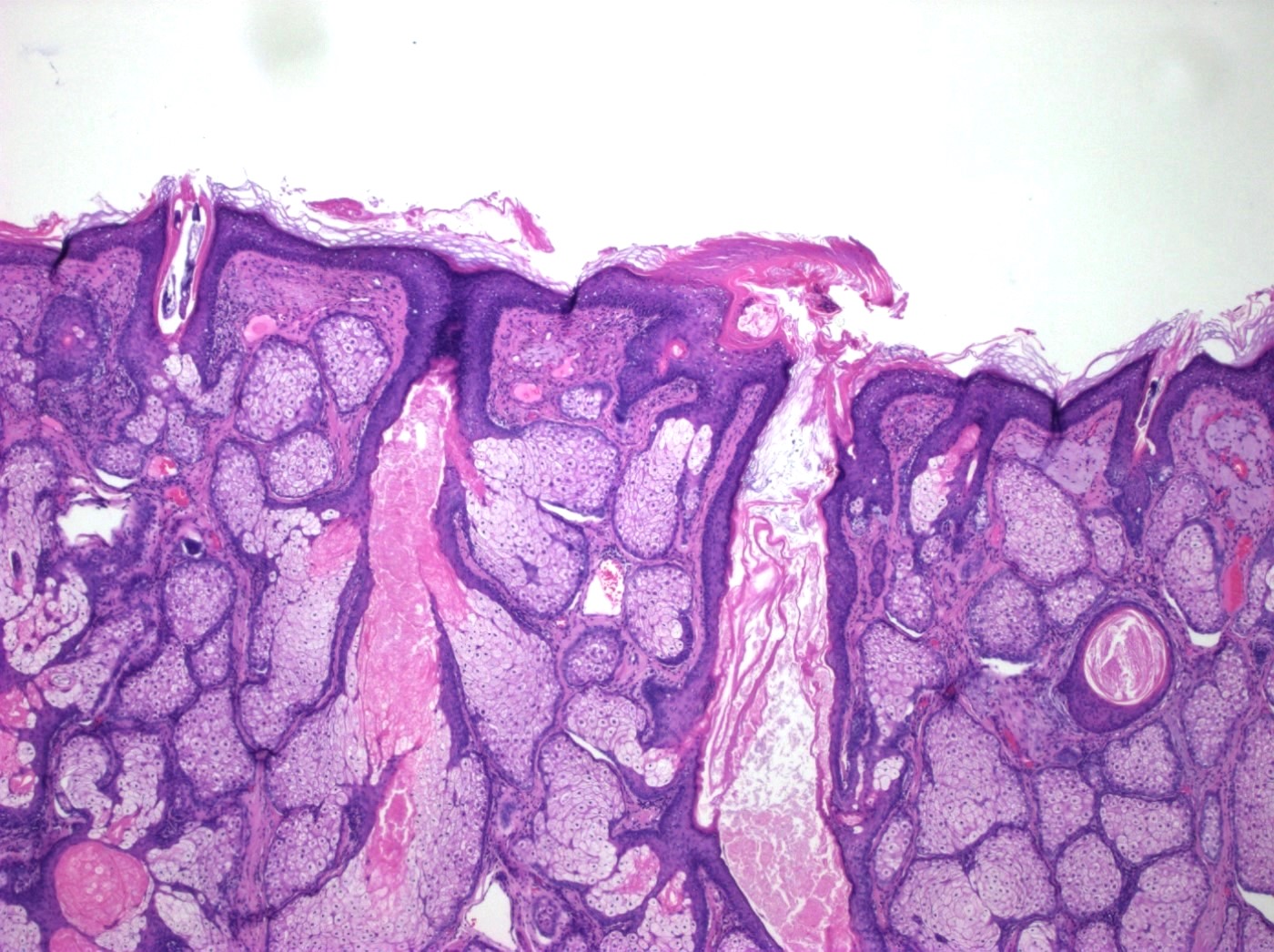
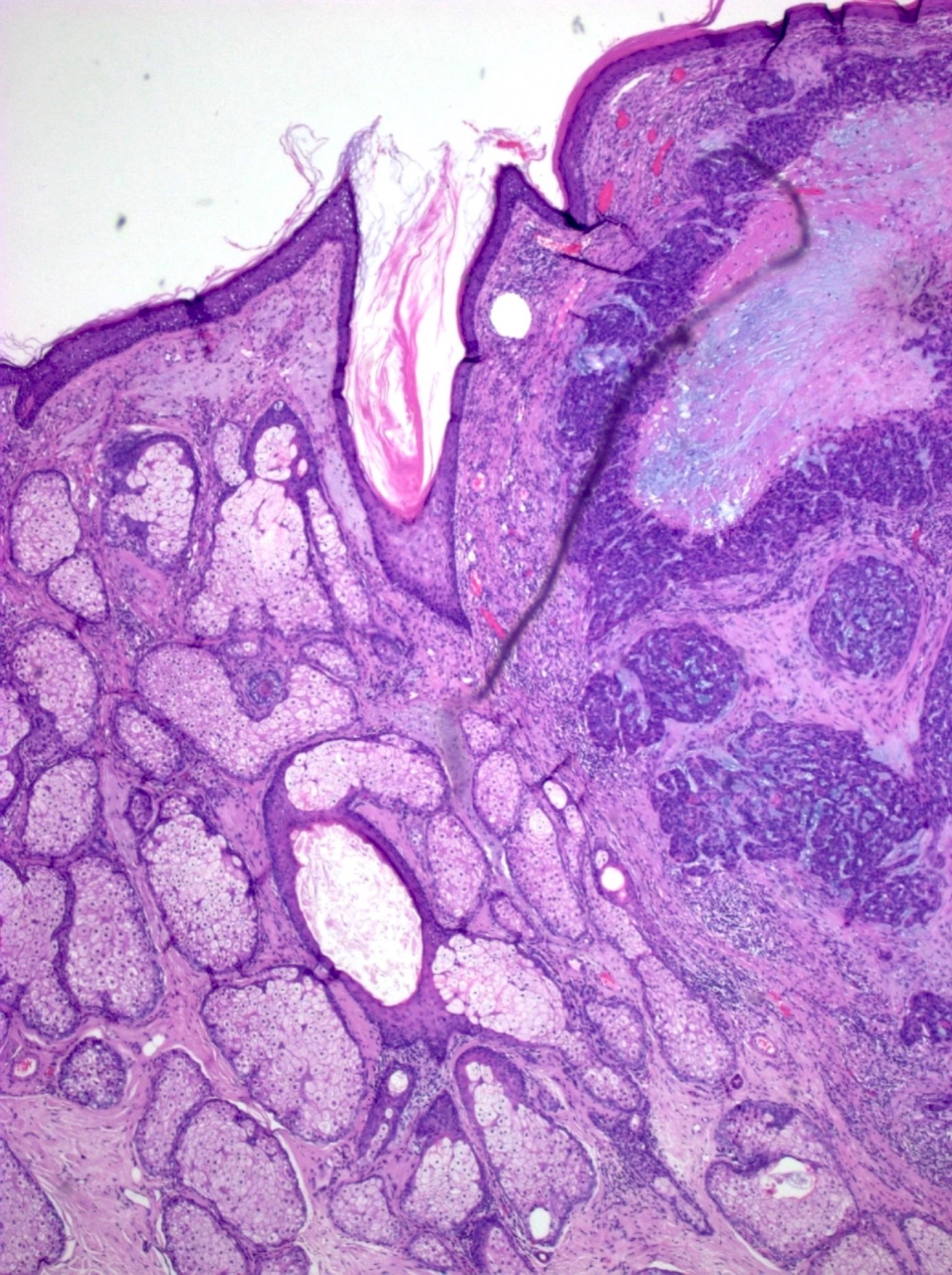
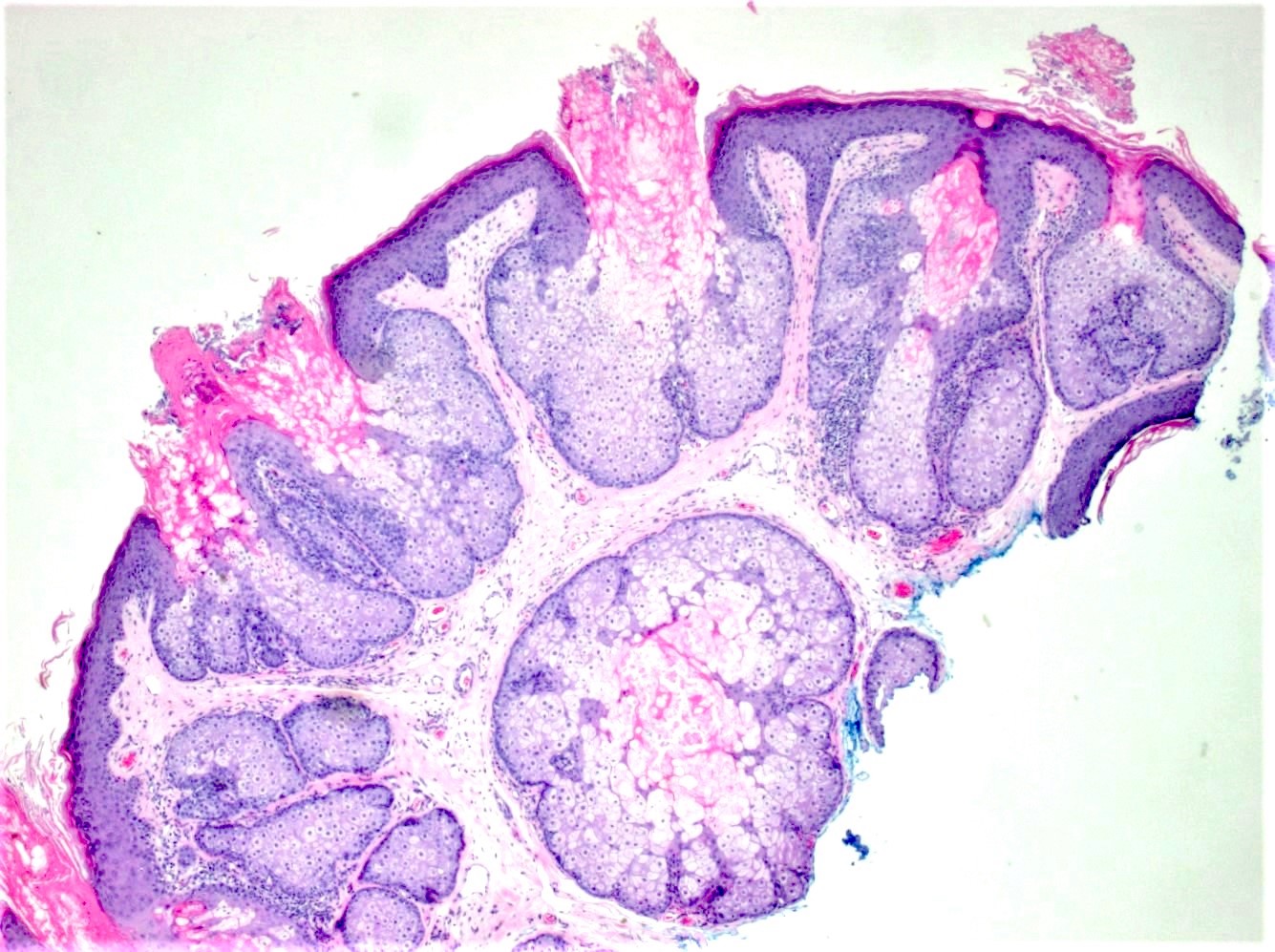
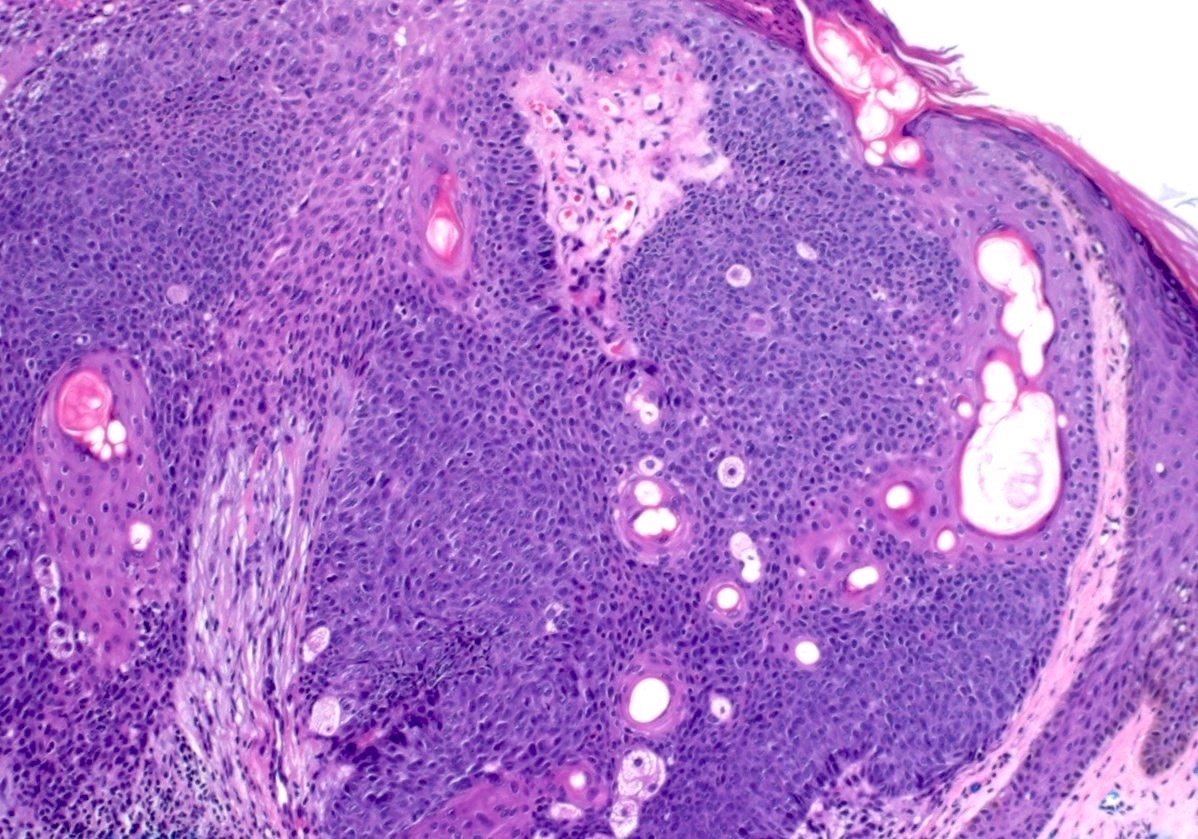
Microscopic (histologic) description
- Increase in size and number of sebaceous glands but the structure remains normal
- Multiple, normal appearing sebaceous lobules draining into a common central duct that is commonly dilated
- Often in association with a hair follicle
- Unlike sebaceous adenoma, peripheral basaloid germinative cell layer is not expanded and does not exceed 1 - 2 cell layer(s) (Histopathology 2020;76:640)
- Presence of overlying epithelial proliferation can help with the diagnosis in superficial biopsies
Microscopic (histologic) images
Positive stains
- Androgen receptor: uniform immunoreactivity for androgen receptor in the sebocytes and seboblasts and gradually diminishing immunoreactivity with increasing central location of sebocytes (Am J Dermatopathol 1999;21:426)
- EMA
- Adipophilin
- p63 and pancytokeratin
- GLUT1: highlights the basal layer of each gland (Dermatopathology (Basel) 2021;8:258)
- Aquaporin 3
- MLH1: retained expression
- MSH2: retained expression
- MSH6: retained expression
- PMS2: retained expression
- Factor XIIIa (J Cutan Pathol 2018;45:1)
- GATA3 (Am J Dermatopathol 2015;37:885)
- PRAME: cytoplasmic pattern
Videos
Sebaceous hyperplasia
Sample pathology report
- Skin, forehead, shave:
- Sebaceous gland hyperplasia (see comment)
- Comment: The sections show an increased number of enlarged sebaceous lobules arranged around a central dilated sebaceous duct. The lobules are composed of mature sebocytes. Atypia is not identified.
Differential diagnosis
- Sebaceous adenoma:
- Well circumscribed, nodular growth of lobules consisting of an admixture of basaloid cells and mature sebocytes
- Basaloid layer is expanded
- Direct connection to the epidermis can be present (Surg Pathol Clin 2017;10:367)
- Acrochordon:
- Adnexa are not typically present
- Epidermal hyperplasia and papillomatosis are present, which is not common in sebaceous gland hyperplasia (J Low Genit Tract Dis 2006;10:55, Am J Dermatopathol 2006;28:478)
- Nevus sebaceus:
- Hamartomatous growth of the epidermis and related structures, typically appearing at birth as a single yellow patch of hair loss on the scalp
- Proliferation and alteration of epidermis and adnexal structures, abnormal distribution and configuration of sebaceous glands
- Direct opening of the sebaceous glands into epidermis
- Ectopic apocrine glands (Int J Dermatol 2016;55:193)
- Sebaceous carcinoma:
- Lobular or sheet-like growth of sebocytes with pleomorphism and atypia
- Infiltrative growth with an increase in mitotic activity (Dermatol Surg 2015;41:1)
Board review style question #1
A 36 year old woman presents to the clinic with several 2 - 6 mm, whitish yellow papular lesions on her face that were first noticed 3 months prior to her visit. Biopsy reveals an expansion of normal lobular sebaceous gland architecture without atypia. Which of the following is the most likely diagnosis?
- Sebaceoma
- Sebaceous adenoma
- Sebaceous carcinoma
- Sebaceous hyperplasia
Board review style answer #1
D. Sebaceous hyperplasia. The clinical presentation and microscopic description are typical for sebaceous gland hyperplasia, a benign entity in which there is an expansion of sebaceous glands without mitosis, necrosis or atypia. Answer A is incorrect because in sebaceoma, there is a basaloid growth pattern into the dermis. Answer B is incorrect because epidermal thickening and hyperplasia can be noted under microscopic examination. Answer C is incorrect because in sebaceous carcinoma, there is usually a lobular or sheet-like growth pattern with multivacuolated cells.
Comment Here
Reference: Sebaceous hyperplasia
Comment Here
Reference: Sebaceous hyperplasia
Board review style question #2
A 38 year old woman has been recently diagnosed with sebaceous gland hyperplasia. Which of the following most likely contributed to her condition?
- Androgen withdrawal
- Chronic sun exposure
- Inactivating mutation in LEF1 gene
- Insulin insensitivity
Board review style answer #2
A. Androgen withdrawal. Androgen withdrawal is believed to be the etiology of sebaceous gland hyperplasia. Answer C is incorrect because inactivating mutations in LEF1 gene can contribute to subsets of sebaceous adenoma. Answer D is incorrect because insulin insensitivity is associated with other dermatologic conditions, such as acrochordon and acanthosis nigricans. Answer B is incorrect because chronic sun exposure would be a risk factor for some skin malignancies, such as basal cell carcinoma.
Comment Here
Reference: Sebaceous hyperplasia
Comment Here
Reference: Sebaceous hyperplasia