Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Hamza M, Moshiri A. Sebaceous adenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticsebaceousadenoma.html. Accessed April 19th, 2024.
Definition / general
- Benign neoplasm composed of mature sebaceous lobules with the expansion of germinative basaloid cell layers at the periphery
- Associated with Muir-Torre syndrome, especially when it arises outside the head and neck region (Histopathology 2010;56:133)
- Unrelated to adenoma sebaceum (facial angiofibromas of tuberous sclerosis)
Essential features
- Well circumscribed, multilobulated tumor
- Increased number of basaloid germinative cells of more than 2 layers
- Shows distinct maturation, meaning that the basaloid germinative cells are usually at the periphery and the sebaceous cells are located centrally
- Associated with Muir-Torre syndrome, a variant of Lynch syndrome with mutations in the DNA mismatch repair (MMR) genes
ICD coding
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
Epidemiology
- Mostly in older people with a mean age of 60 years (Ann Dermatol 2019;31:14)
Sites
- Mostly in the head and neck, particularly on the face and scalp
Pathophysiology
- Subset of these lesions has inactivating mutations in LEF1 affecting the Wnt / β catenin pathway, which is important in sebaceous differentiation (Nat Med 2006;12:395)
Clinical features
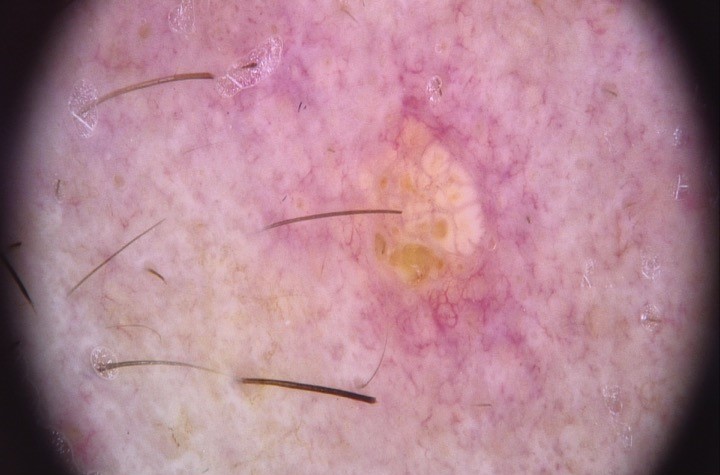
- Clinically presents as a yellow or pink-tan papule or nodule
- Clinically can be mistaken for basal cell carcinoma
- Muir-Torre syndrome (MTS) is a clinical variant of Lynch syndrome, which is defined as at least 1 sebaceous neoplasm (sebaceous adenoma, sebaceoma and sebaceous carcinoma) or keratoacanthoma and at least 1 Lynch syndrome related internal cancer
- MTS is caused by germline variants in the DNA mismatch repair (MMR) genes encoding for MSH2 and MLH1, accounting for most of the cases
- Isolated mutations in MSH6 and PMS2 account for a small minority of cases (J Cutan Pathol 2017;44:931)
- MUTYH associated polyposis (MAP) is an autosomal recessive disorder associated with colorectal polyps (adenomas) and adenocarcinomas that can also be associated with cutaneous sebaceous neoplasms, closely imitating MTS (Am J Dermatopathol 2016;38:915)
- Overall quality of evidence in support of MMR IHC reflex testing on MTS associated cutaneous neoplasms is weak to moderate
- Some pathologists do targeted testing specially if patient has multiple sebaceous neoplasms, outside the head and neck or history of colorectal, breast or urothelial cancer (J Cutan Pathol 2017;44:931)
Diagnosis
- Diagnosis is made using clinical examination and biopsy
Prognostic factors
- Solitary tumors are treated by complete surgical removal with a 100% cure rate
- Incomplete removal has occasionally resulted in local recurrence (Pathology 2017;49:688)
Case reports
- 57 year old man with a history of colon cancer diagnosed at age 32 and multiple sebaceous adenomas (Cureus 2021;13:e14582)
- 60 year old man, with a history of kidney transplantation 11 years prior, presented with new lesion on his left lower abdomen, which was sebaceous adenoma (JAAD Case Rep 2019;5:818)
- 68 year old man presented to the dermatology clinic with a solitary enlarging, bleeding lesion on his right central zygoma (Dermatol Arch 2019;3:77)
Treatment
- Because sebaceous adenomas are benign, treatment for most individuals is conservative management, although bothersome lesions can be removed for patient comfort
- Consider complete excision also if the lesion is partially biopsied or of clinical concern for carcinoma with sebaceous differentiation (Pathology 2017;49:688)
Clinical images
Gross description
- Well circumscribed superficial dermal nodule with sharp demarcation from the underlying tissue
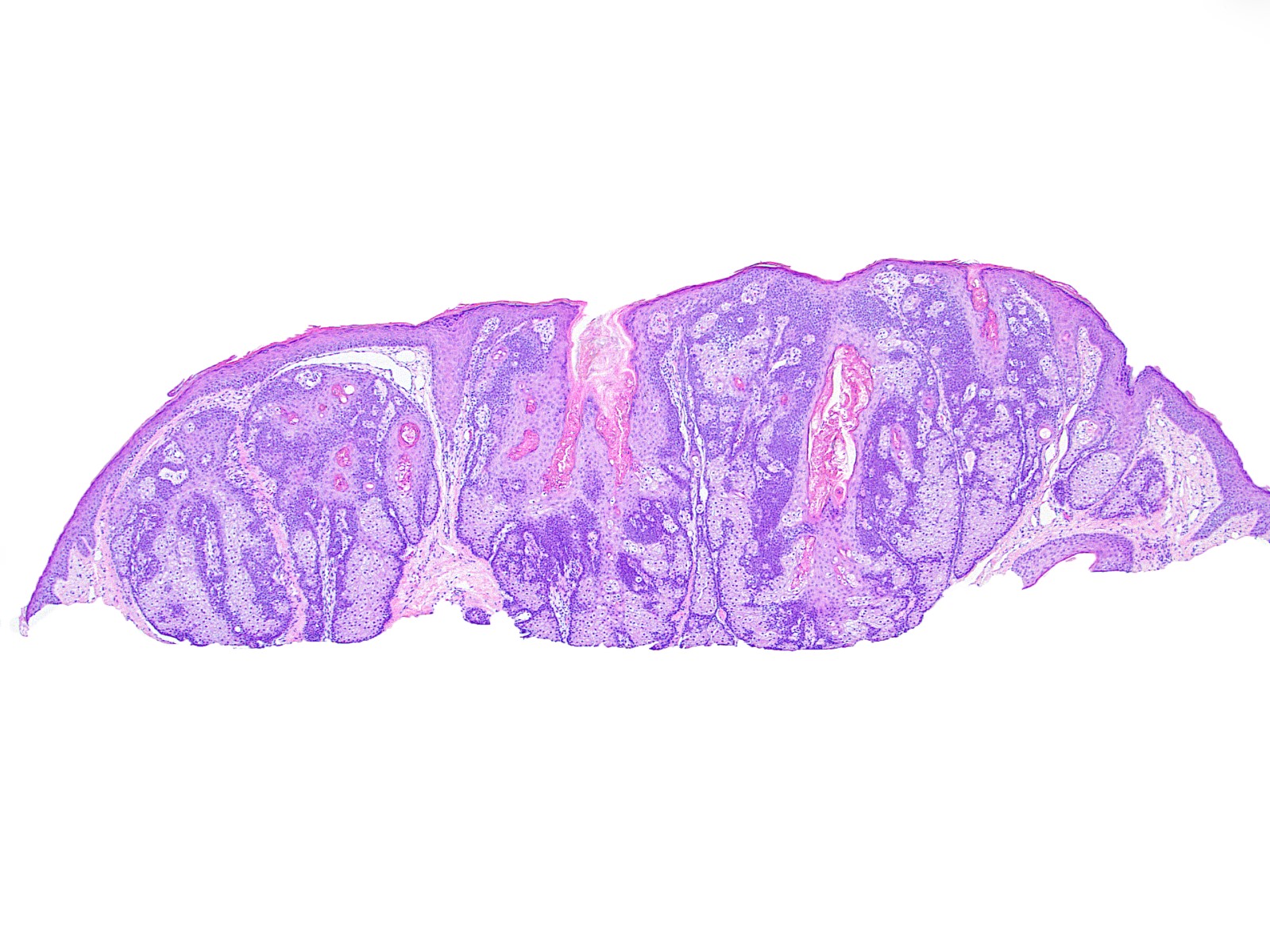
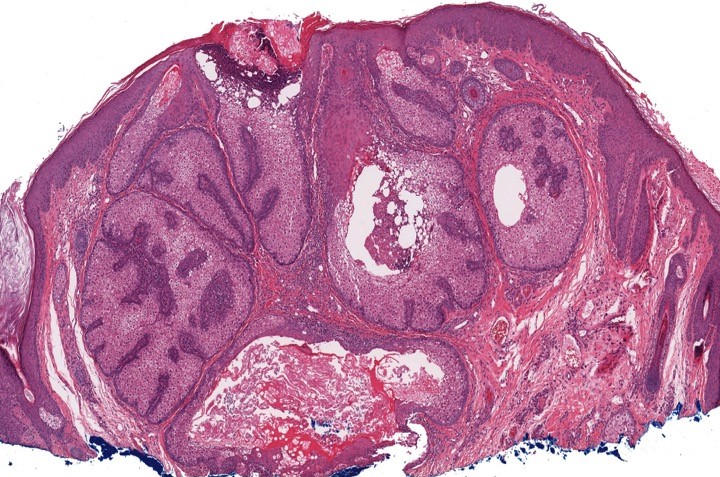
Microscopic (histologic) description
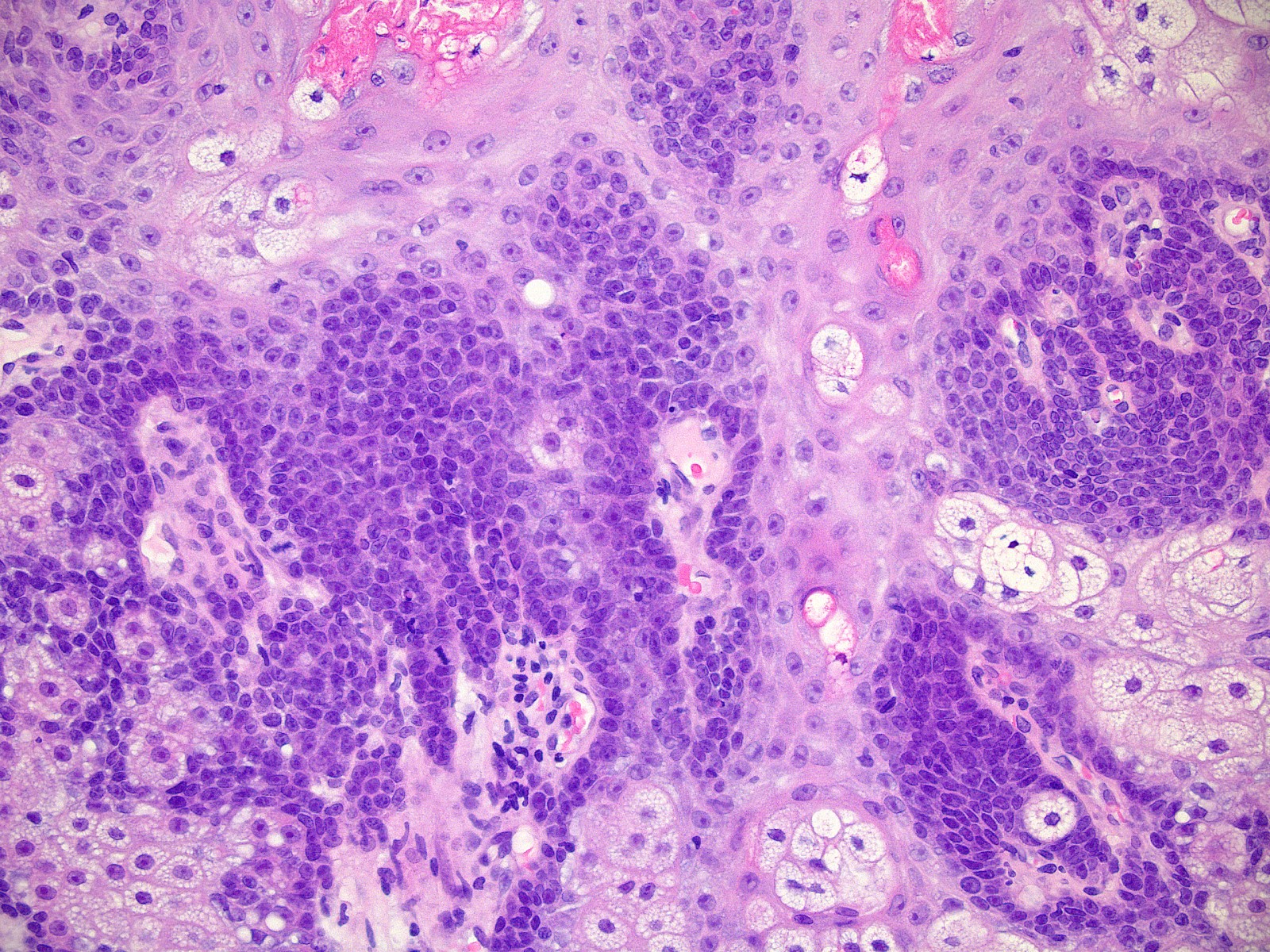
- Well circumscribed, nodular growth of lobules consist of admixture of basaloid cells and mature sebocytes
- Some lobules may communicate directly with the surface epithelium
- Basaloid cells are usually located at the periphery of lobules and sebaceous cells with intracytoplasmic lipid vacuoles, which are usually located at the center of lobules
- Basaloid cells are composed of expanded germinative layer, with more than the normal 2 cell layers seen in mature sebaceous glands or sebaceous hyperplasia but still less than 50% of the tumor volume (> 50% is seen in sebaceoma / sebaceous epithelioma)
- Increased mitotic activity is sometimes seen in the basaloid cell component (Surg Pathol Clin 2017;10:367)
Microscopic (histologic) images
Positive stains
- Diagnosis is usually made by standard histology; the following immunostains can be used to confirm sebaceous origin:
- Adipophilin: membranous vesicular pattern of staining is suggestive of intracellular lipids (Mod Pathol 2010;23:567)
- Androgen receptor (AR)
- Preferentially expressed antigen in melanoma (PRAME) may show a cytoplasmic and perinuclear (but not nuclear) pattern (J Cutan Pathol 2021;48:1252)
- CK7
- D2-40 (Podoplanin)
- Epithelial membrane anttigen (EMA)
Negative stains
Videos
Sebaceous adenoma: 5 minute pathology pearls by Dr. Jerad Gardner
Sample pathology report
- Skin, right cheek, shave biopsy:
- Sebaceous adenoma
Differential diagnosis
- Sebaceous hyperplasia:
- Hyperplastic sebaceous lobules
- Located slightly higher in the dermis than normal
- Individual lobules are increased in number but are not significantly different in size compared to normal
- Basaloid layer is not expanded
- Sebaceoma / sebaceous epithelioma:
- Tumor consists of a random admixture of basaloid cells and mature sebocytes with loss of regular maturation that is seen in sebaceous adenoma
- No nuclear pleomorphism and mitotic activity is generally sparse; however, it can sometimes be prominent
- No peripheral palisading or cleft formation
- Sebaceous carcinoma:
- Significant nuclear pleomorphism, nucleolar prominence and conspicuous mitotic activity
- Although in well differentiated variants, the tumor may have a smooth regular margin
- Less well differentiated examples typically show an infiltrating border
- Basal cell carcinoma with sebaceous differentiation:
- Features of basal cell carcinoma with proliferation of palisading basaloid cells, retraction artifact and loose mucinous stroma
- Within these nodules are foci of variable numbers of mature sebocytes
- EMA- and BerEP4+ (Can J Ophthalmol 2014;49:326)
- Trichoblastoma with sebaceous differentiation:
- Papillary mesenchymal bodies are often present
- Peripheral nuclear palisading and stromal induction are also generally present
- Balloon cell melanoma:
- Other lesions with clear cell differentiation (e.g., metastatic renal clear cell carcinoma)
Additional references
Board review style question #1
Board review style answer #1
E. Muir-Torre syndrome (MTS) is a clinical variant of Lynch syndrome, which is defined as at least 1 sebaceous neoplasm (sebaceous adenoma, sebaceoma and sebaceous carcinoma) or keratoacanthoma and at least 1 Lynch syndrome related internal cancer. Additionally, among the spectrum sebaceous neoplasms, sebaceous adenoma is the one most associated with Muir-Torre syndrome.
Comment Here
Reference: Sebaceous adenoma
Comment Here
Reference: Sebaceous adenoma
Board review style question #2
Mutations in which of the following genes are associated with Muir-Torre syndrome?
- CYLD
- Folliculin
- MLH1
- PTCH
- PTEN
Board review style answer #2
C. MLH1. Muir-Torre syndrome (MTS) is caused by germline variants in the DNA mismatch repair (MMR) genes encoding for MSH2 and MLH1, which account for most of the cases. Isolated mutations in MSH6 and PMS2 account for a small minority of cases (J Cutan Pathol 2017;44:931).
Comment Here
Reference: Sebaceous adenoma
Comment Here
Reference: Sebaceous adenoma