Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Regmi A, Speiser J. Poroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticeccrineporoma.html. Accessed December 20th, 2024.
Definition / general
- Benign glandular adnexal tumor that usually originates from cells of the outer layer of the acrosyringium and terminal eccrine duct
- Has both eccrine and apocrine origin (AMA Arch Derm 1956;74:511)
- Malignant counterpart is referred to as porocarcinoma
Essential features
- Single, slow growing, asymptomatic, well circumscribed, smooth, skin colored to red, slightly scaly papule or nodule
- Most commonly on palms and sole or sides of the foot
- Well circumscribed broad anastomosing bands of poroma cells with sharp demarcation from adjacent keratinocytes
- Excellent prognosis with simple excision
Terminology
- Eccrine poroma / hidroacanthoma simplex / dermal duct tumor, apocrine poroma
ICD coding
- ICD-10: D23.9 - other benign neoplasm of skin, unspecified
Epidemiology
- M = F (Arch Craniofac Surg 2017;18:44)
- Most commonly affects adults (Ann Dermatol 2011;23:250)
- Presentation in childhood and congenital onset are unusual (J Eur Acad Dermatol Venereol 2008;22:366)
- Eccrine porocarcinoma:
- Also known as malignant eccrine poroma
- Develops after several years from a pre-existing poroma
- Most commonly affects elderly, with F > M
- Tumors are often ulcerated and many bleed on trauma
Sites
- Most commonly on palms and sole or sides of the foot (AMA Arch Derm 1956;74:511)
- Occasionally on the head, neck, scalp, chest, abdomen, proximal extremities and the external auditory canal (J Am Acad Dermatol 2001;44:48, Otolaryngol Head Neck Surg 2003;128:439)
Pathophysiology
- Falls under the broad category of poroid neoplasms or acrospiromas
- Poroid neoplasms include the eccrine poroma, apocrine poroma, hidroacanthoma simplex and dermal duct tumor (Clin Exp Dermatol 2014;39:119)
- Eccrine poroma: derived from cells of the outer layer of the acrosyringium and the upper dermal eccrine duct, both epidermal and dermal (AMA Arch Derm 1956;74:511)
- Apocrine poroma: reflects the common embryological ancestry of the 3 units (the folliculosebaceous apocrine unit) (Pathologe 2014;35:456)
Etiology
- Exact etiology is unknown (World J Surg Oncol 2011;9:94)
- No family predilection has been identified for the development of poromas
- Rare cases are associated with radiation therapy or chronic scarring (J Eur Acad Dermatol Venereol 2007;21:1128, Am J Dermatopathol 2013;35:615)
Clinical features
- Asymptomatic, slow growing, solitary, sessile, skin colored to red, slightly scaly nodule, papule or plaque (Int J Dermatol 2014;53:1053)
- Less commonly pigmented or pedunculated (J Dermatol 1990;17:555)
- Occasionally reported with Bowen disease, pregnancy and hypohidrotic ectodermal dysplasia (Ann Dermatol 2018;30:222, Arch Dermatol 1977;113:472)
- Rarely reported as arising within nevus sebaceous (Case Rep Dermatol 2016;8:80)
- Rarely, multiple poromas known as poromatosis can occur following chemotherapy or radiotherapy (Ann Dermatol 2020;32:422)
- Dermoscopic findings: white interlacing areas around vessels, yellow structureless areas, milky red globules, poorly visualized vessels and branched vessels with rounded endings (J Eur Acad Dermatol Venereol 2018;32:1263, Clin Case Rep 2021;9:1601)
Diagnosis
- Clinical appearance confirmed by characteristic histologic findings
Prognostic factors
- Excellent; most cases do not show aggressive behavior
- Rarely progresses to porocarcinoma (World J Surg Oncol 2011;9:94)
- Poromatosis is of cosmetic concern for the patient (Skin Appendage Disord 2015;1:95)
Case reports
- 40 year old woman with an asymptomatic red to brown colored hemorrhagic crusted nodule on the left forearm (Ann Dermatol 2011;23:250)
- 58 year old man had painless, progressive mass below the left temporal eyebrow for 8 years (Indian J Ophthalmol 2020;68:2522)
- 64 year old man with papules near his left nipple and left ankle (Dermatol Online J 2008;14:3)
- 67 year old man initially presented with a nonpainful, exophytic and pigmented lesion on scalp (Am J Case Rep 2019;20:179)
- 70 year old nondiabetic man presented with mass over the medial aspect of his right upper eyelid (Indian J Ophthalmol 2019;67:131)
- 74 year old man with a 4 year history of nodules on the chest and back (An Bras Dermatol 2017;92:550)
Treatment
- No treatment is necessary
- Simple excision with shave or electrosurgical destruction is curative
- Reference: StatPearls: Poroma [Accessed 30 September 2021]
Clinical images
Gross description
- Solitary, well circumscribed, smooth, pink to red papule, nodule or plaque (Int J Dermatol 2014;53:1053)
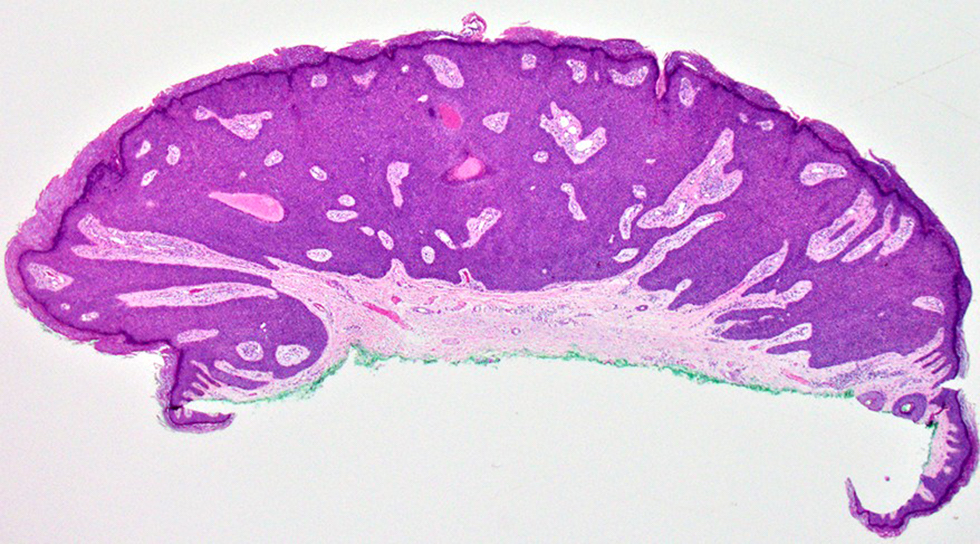
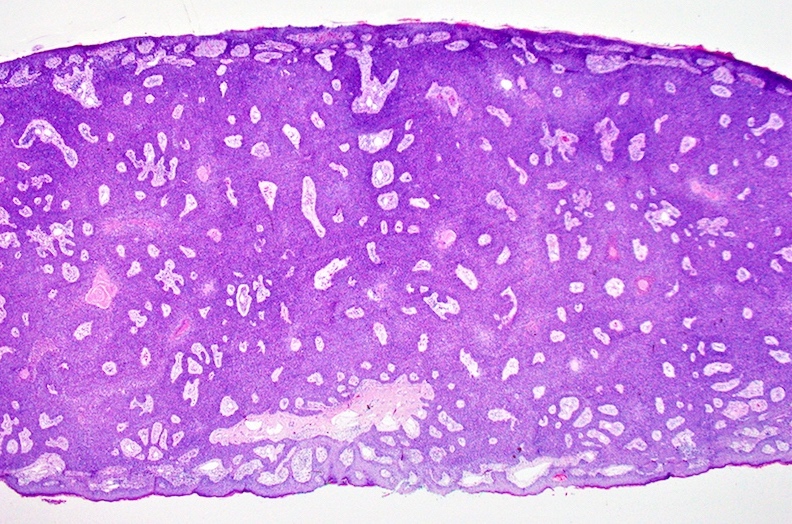
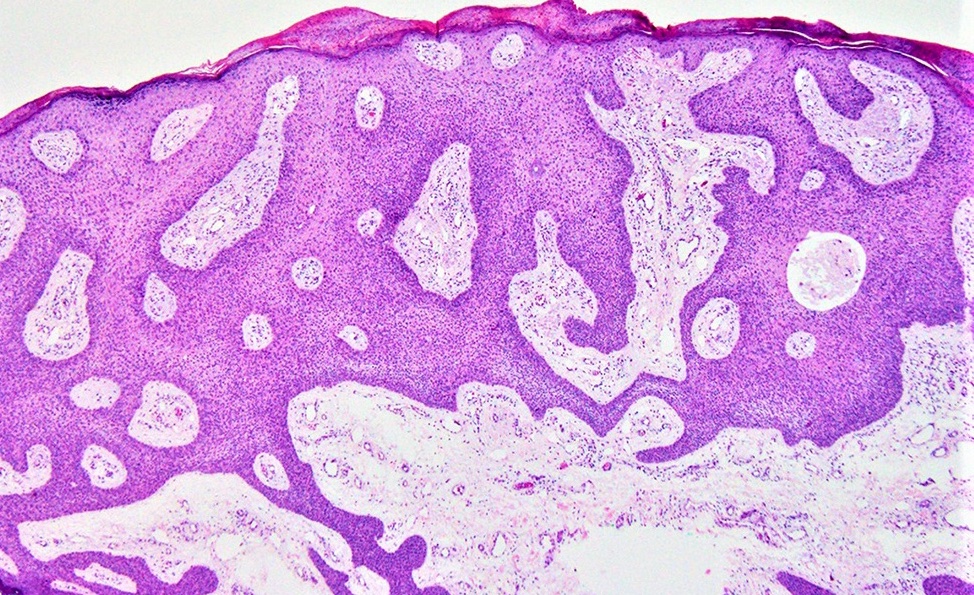
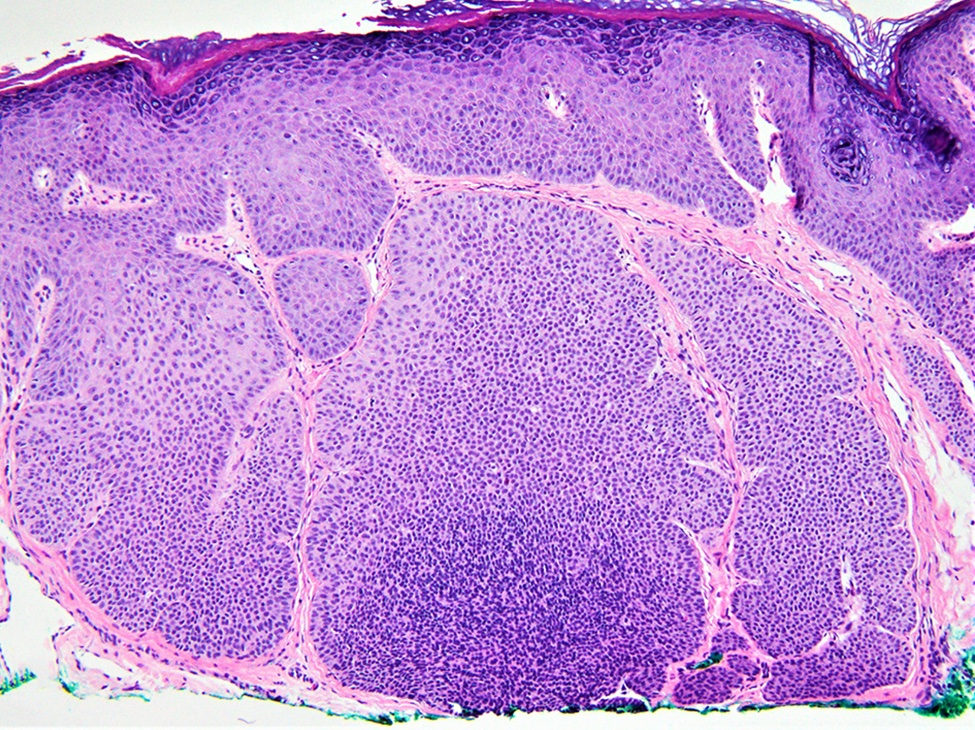
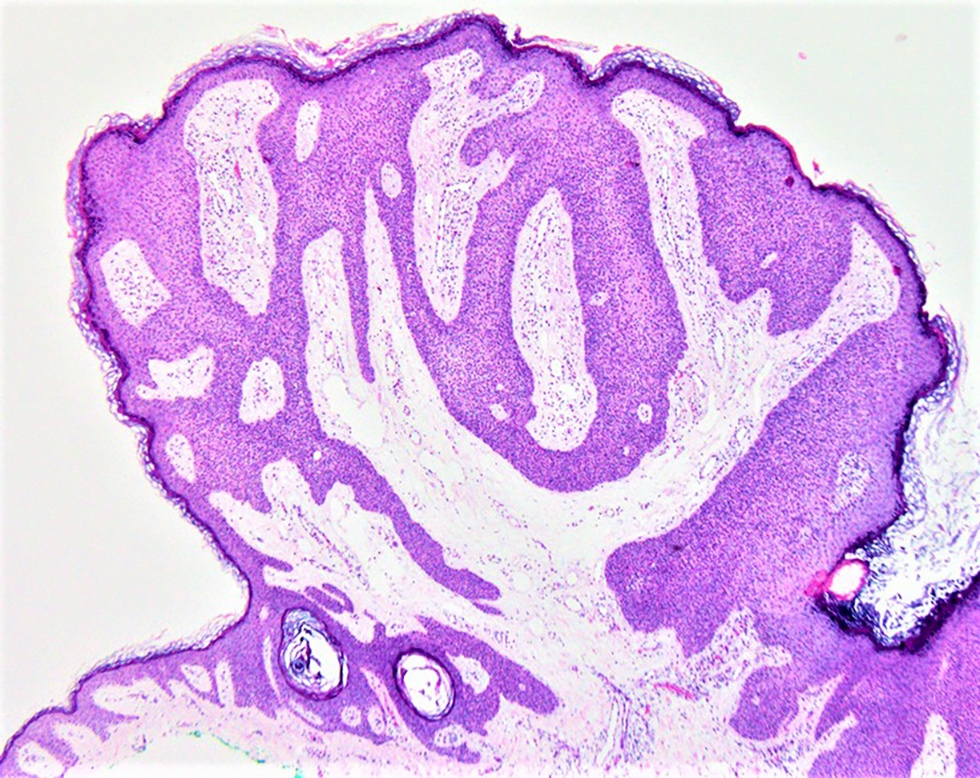
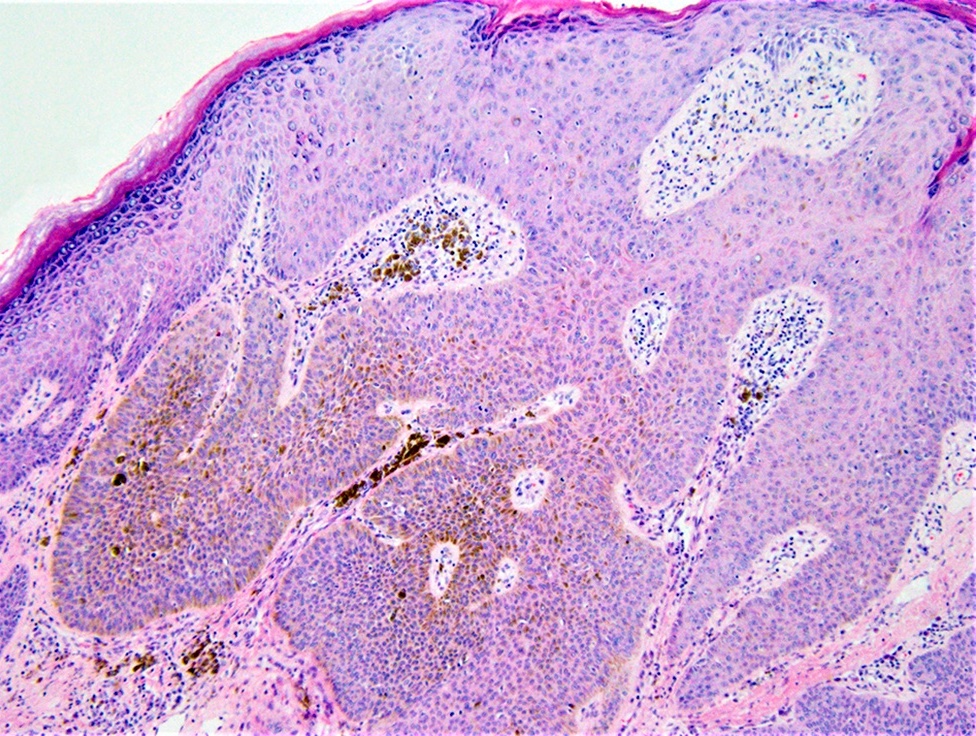
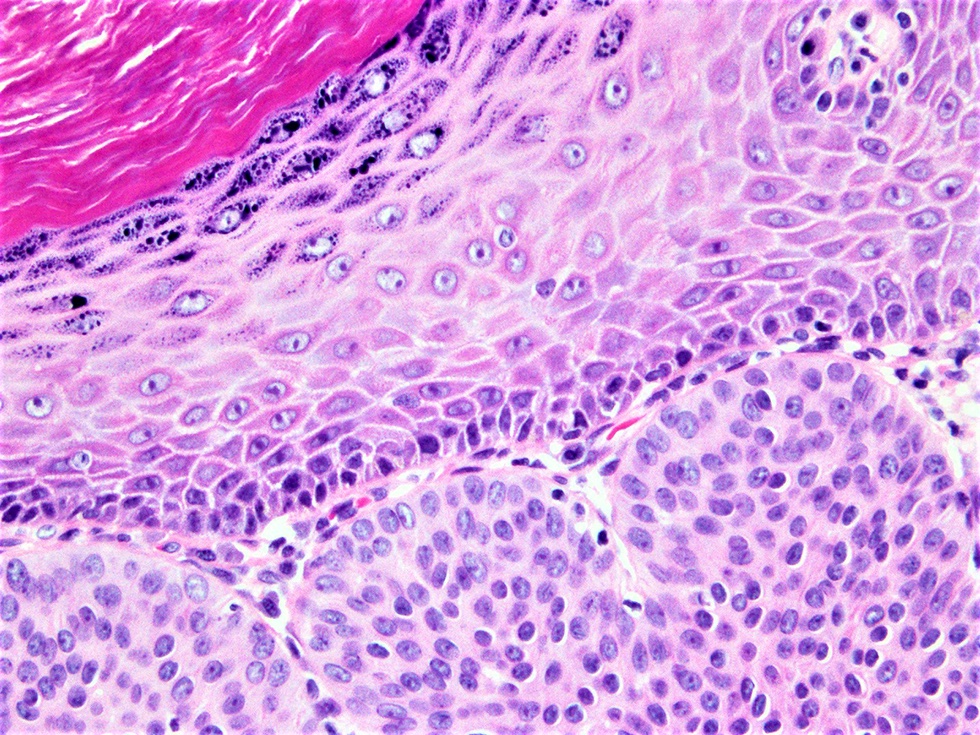
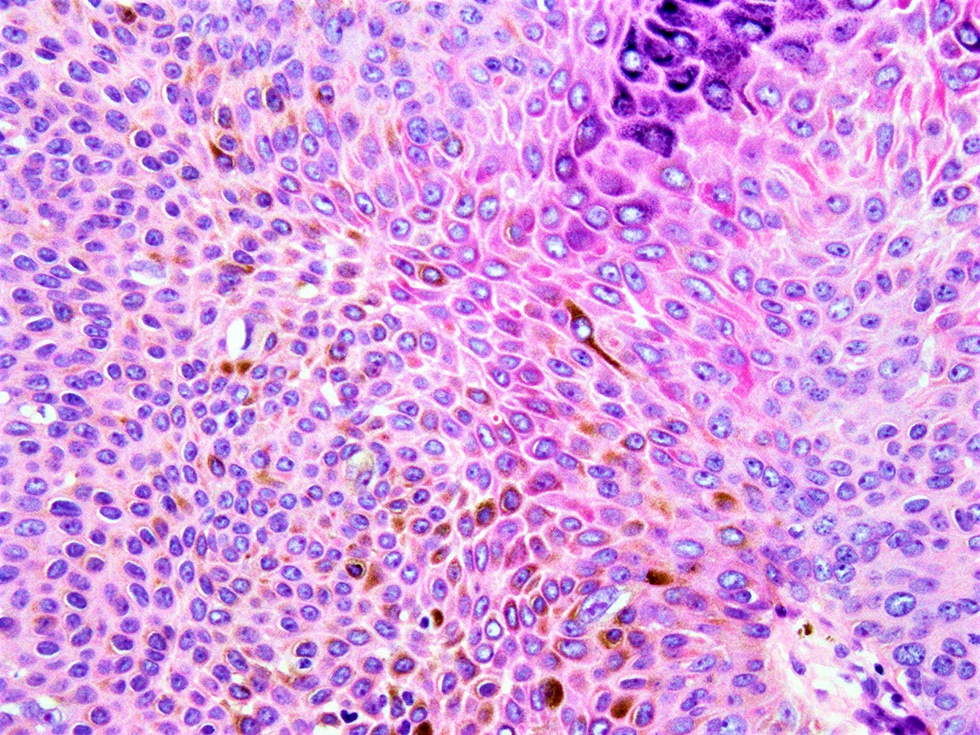
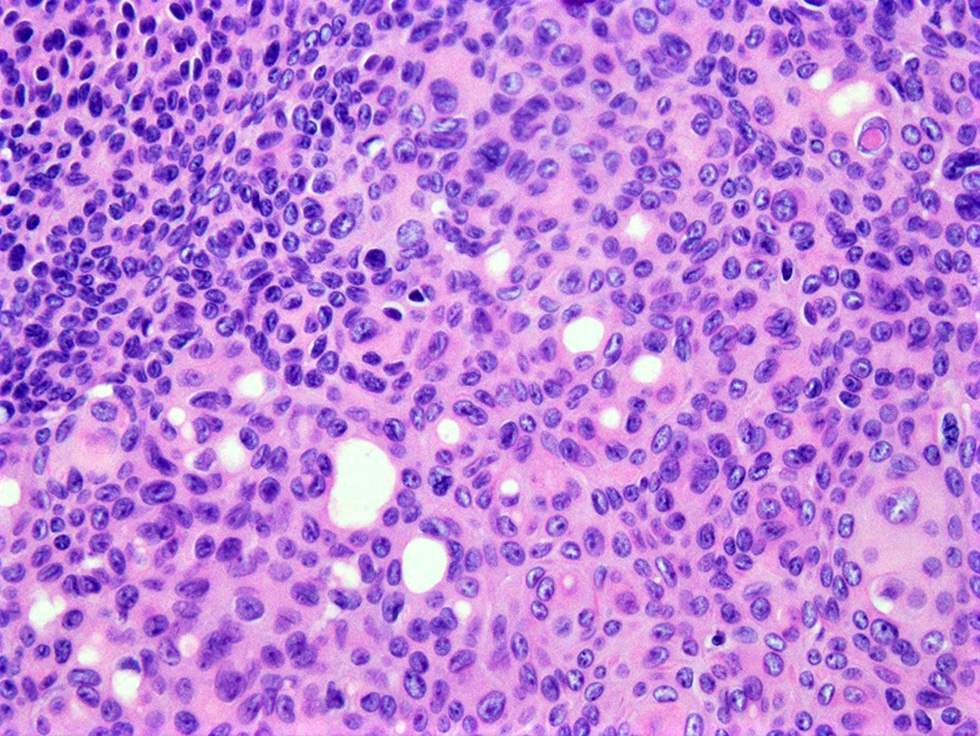
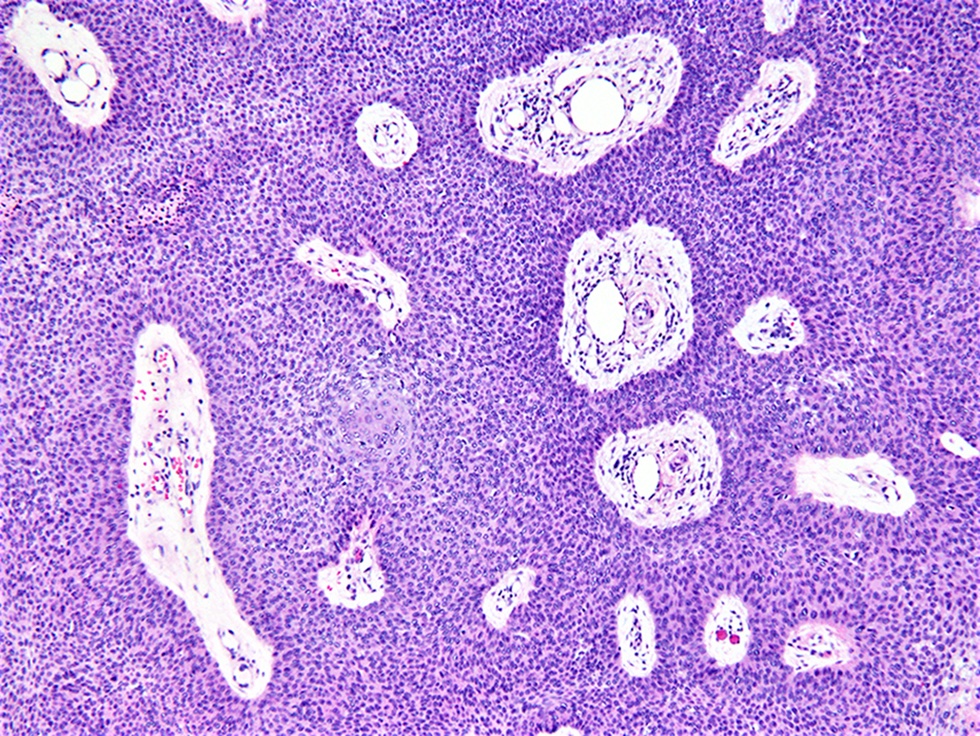
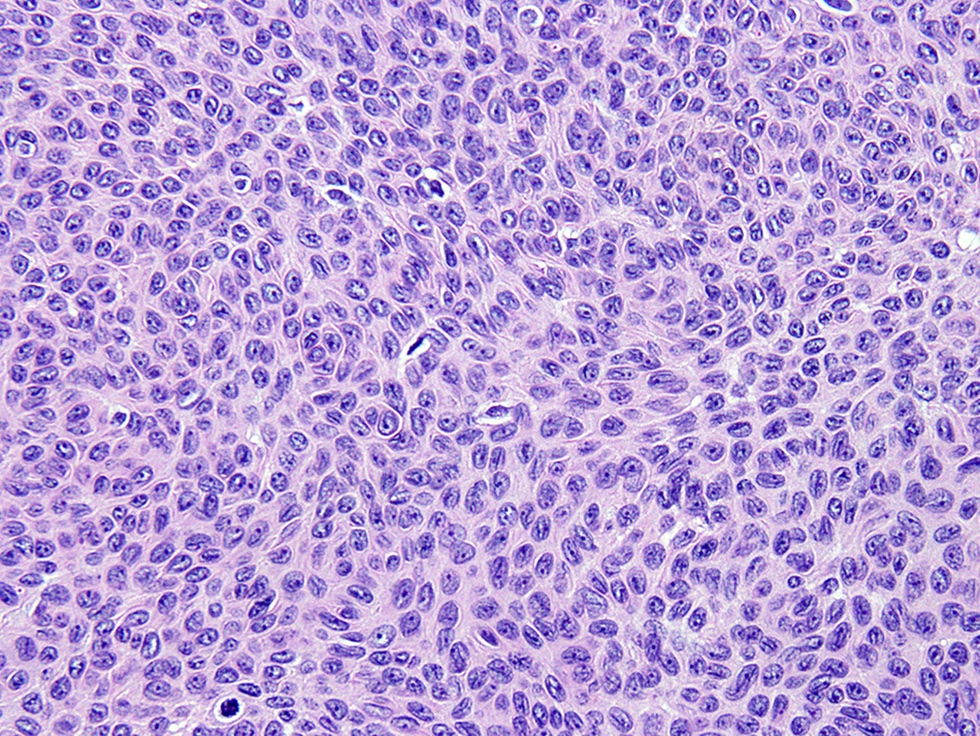
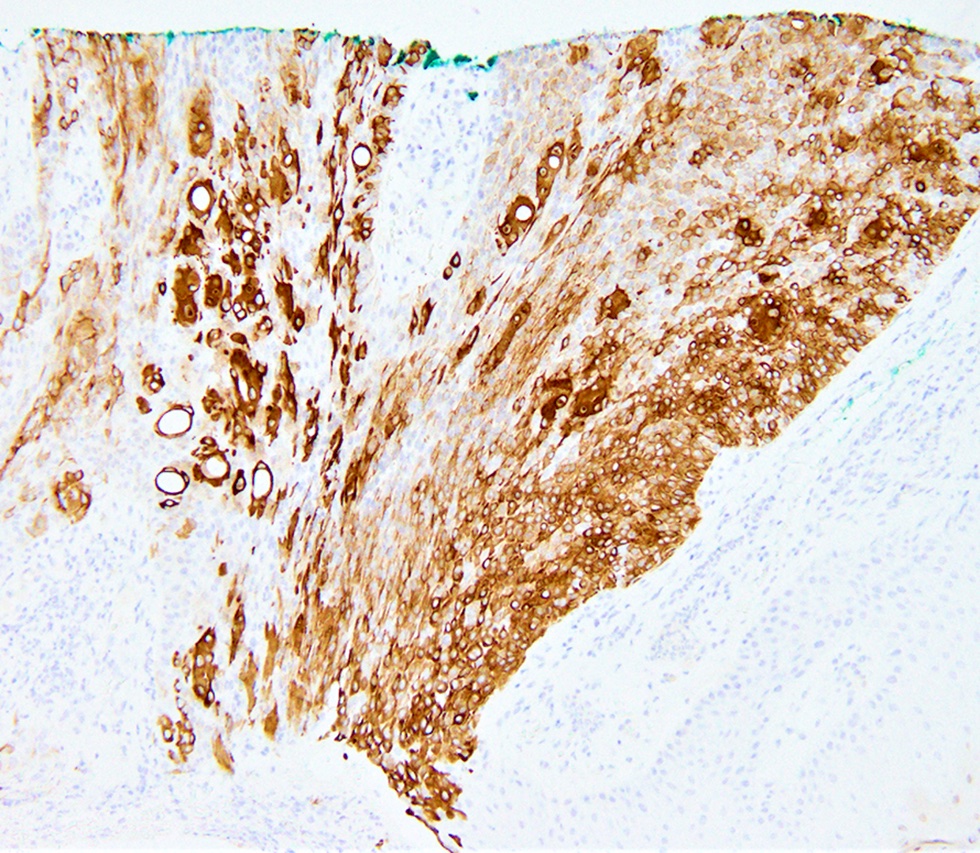
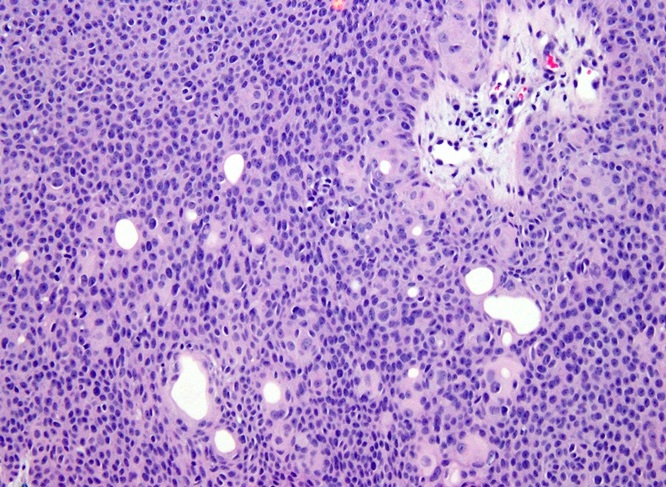
Microscopic (histologic) description
- Eccrine poroma:
- Well circumscribed
- Replaces the epidermis and extends into the dermis in broad anastomosing bands
- Poroma cells are monomorphic, small, cuboidal with basophilic round nuclei, inconspicuous nucleoli and compact eosinophilic cytoplasm
- Sharp demarcation present between the normal keratinocytes and poroma cells
- Devoid of peripheral palisading
- Ductal lumina with single row of luminal cells covered by eosinophilic lining or cystic spaces devoid of any formal lining
- Cells are united by conspicuous intercellular bridges and supported by a delicate fibrovascular stroma (J Dermatol 1980;7:263)
- Poroma cells usually contain glycogen (Int J Dermatol 2014;53:1053)
- Occasionally, pigmented variants with associated dendritic melanocytes and tumor cell melanin deposition (J Dermatol 2010;37:542, J Eur Acad Dermatol Venereol 2008;22:303)
- Dystrophic calcification and transepidermal elimination of tumor nests are exceptional findings (J Dermatol Case Rep 2009;3:38, J Dermatol 1997;24:539)
- Apocrine poroma:
- Shows sebaceous differentiation with the occasional presence of follicular differentiation and foci of apocrine-like features (J Cutan Pathol 2001;28:101)
- Anastomosing trabeculae, displaying multiple points of origin from the epidermis and located largely in the papillary and upper reticular dermis
- Cells are small and uniform with scanty cytoplasm and round to oval nuclei united by inconspicuous intercellular bridges
- Foci of ductal differentiation with a well developed eosinophilic cuticle
- Follicular differentiation in the form of epithelial lobules (Am J Dermatopathol 1999;21:31)
- Sebaceous cells, singly and in clusters with bubbly cytoplasm and crenated nuclei is an infrequent feature (Am J Dermatopathol 1996;18:1)
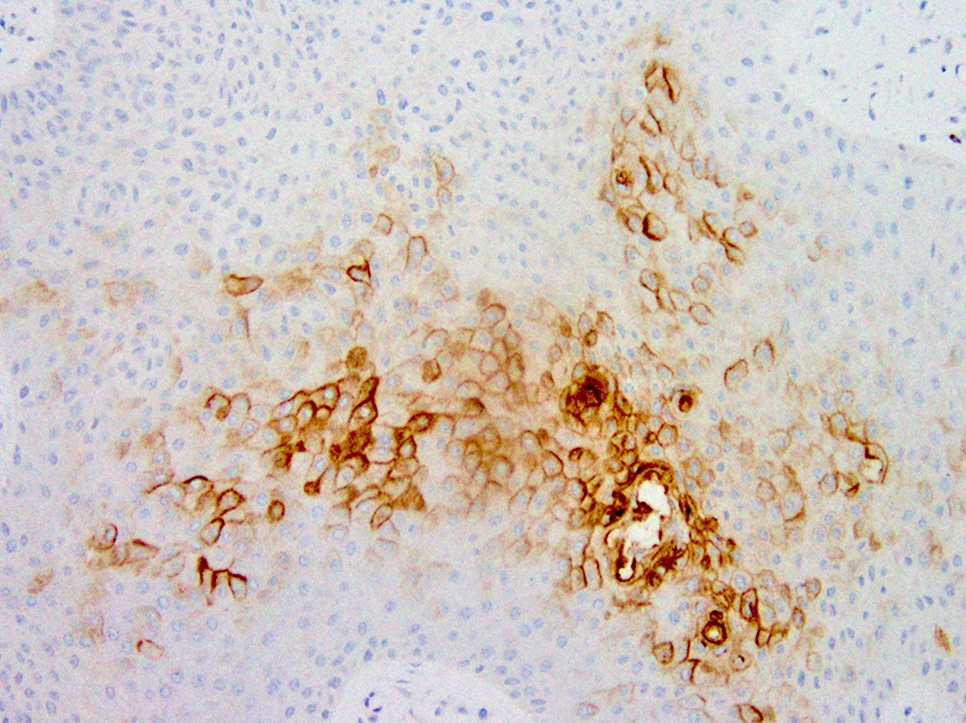
- Eccrine porocarcinoma:
- May remain completely intraepidermal (in situ porocarcinoma) but is more often associated with an invasive dermal component
- Poroma cells, with typical ductal lumina, associated with cytological features of malignancy, including nuclear and cytoplasmic pleomorphism, nuclear hyperchromatism and mitotic activity (Am J Surg Pathol 2001;25:710)
- Prone to have local recurrence (17%) and is occasionally associated with nodal metastases (19%); however, systemic spread is rare (11%) (Am J Surg Pathol 2001;25:710)
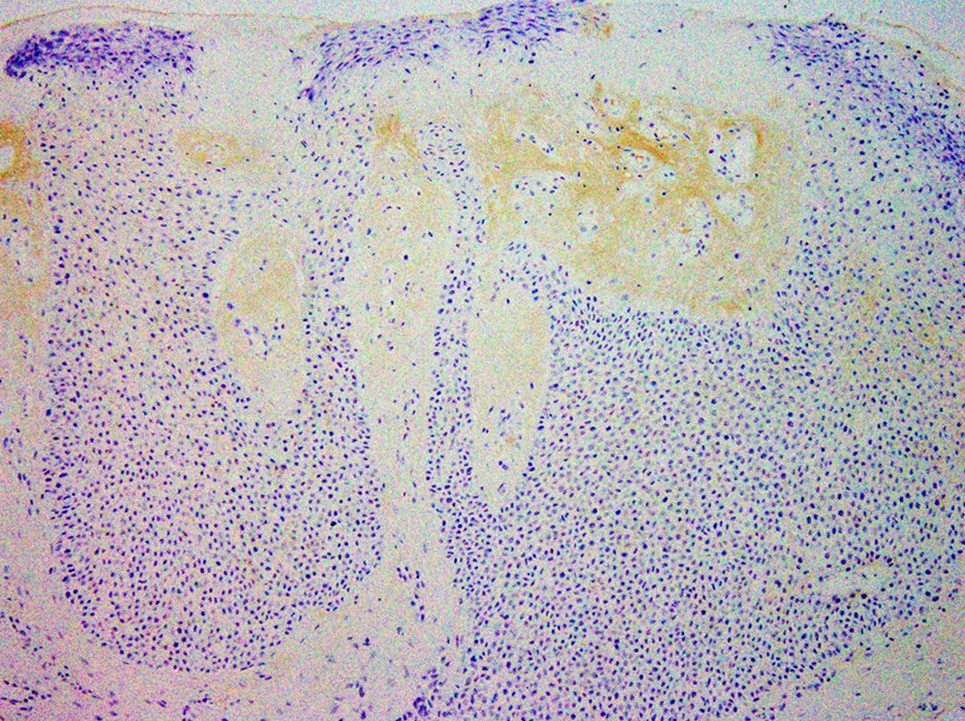
Microscopic (histologic) images
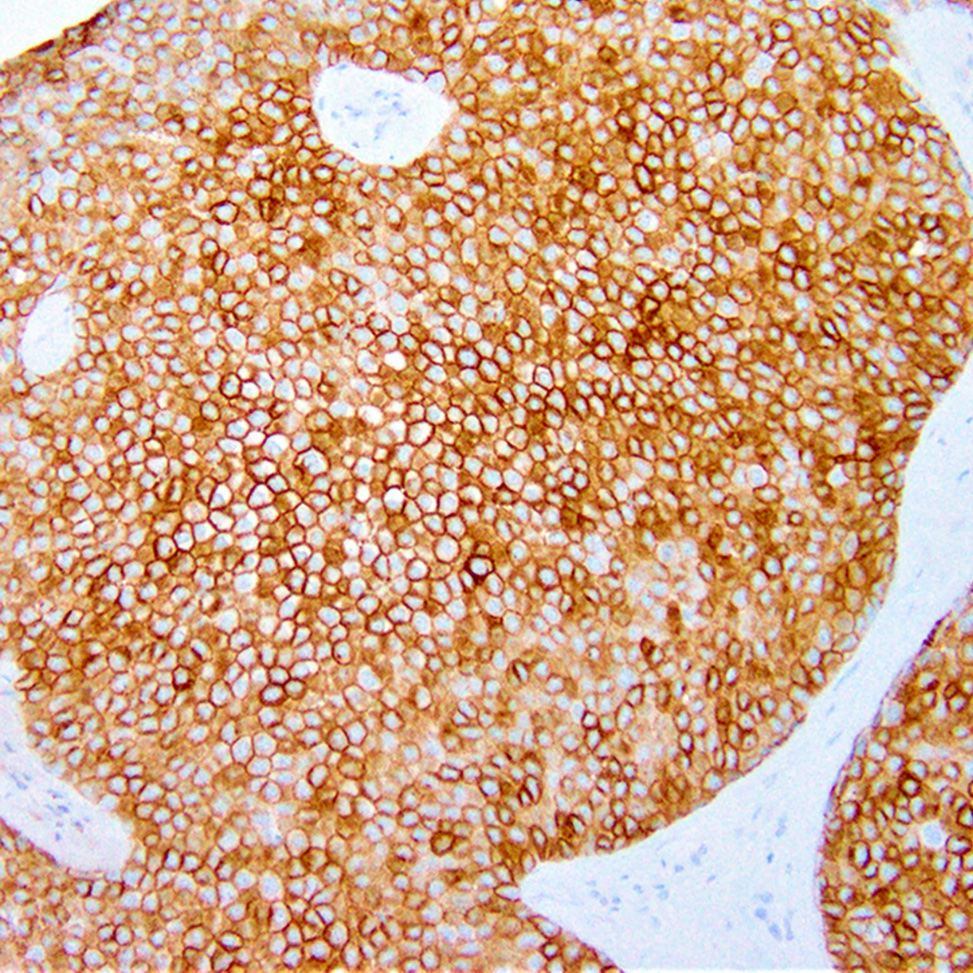
Positive stains
- CK5/6, CK7, EMA, CEA, CAM5.2, CD117, diastase PAS (J Cutan Pathol 1999;26:232)
- S100 protein in the diagnoses of recurrent and metastatic dedifferentiated eccrine porocarcinoma (Ann Dermatol 2013;25:348)
Negative stains
- BerEP4, S100 (benign poroma) (Recent Results Cancer Res 1995;139:303)
Electron microscopy description
- Cells have numerous connecting desmosomes, cytoplasmic tonofilaments, glycogen granules and intracytoplasmic lumina (J Dermatol 1980;7:263)
Molecular / cytogenetics description
- p53 expression is a feature of both poroma and porocarcinoma (Am J Dermatopathol 2001;23:402)
- p16 overexpression is only seen in porocarcinoma (J Cutan Pathol 2019;46:659)
Sample pathology report
- Skin, left palm, excision:
- Eccrine poroma, extending to the deep margin
Differential diagnosis
- Hidroacanthoma simplex:
- Entirely intraepidermal
- Discrete circumscribed populations of poroma cells within an irregularly acanthotic epidermis
- Dermal duct tumor:
- Entirely intradermal, the epidermis is unaffected
- Large lobules of uniform poroma cells in the mid and lower dermis
- Basal cell carcinoma:
- Squamous cell carcinoma (SCC):
- Lacks evidence of ductal differentiation
- Squamous differentiation abundant, eosinophilic cytoplasm with keratin pearls, intercellular bridges and keratinization
- Greater cytologic atypia, dyskeratotic cells
- Irritated / clonal seborrheic keratosis (SK):
- Shows follicular differentiation with keratinizing pseudohorn cysts, no ductal differentiation
- Cells are typically larger than in poroma
- Hidradenoma:
- Nests and nodules of epithelial cells lacking epidermal connection
- Shows both solid and cystic components
- More commonly shows clear cell features
- Eccrine syringofibroadenoma:
- Benign eccrine proliferation
- Thin anastomosing reticulated cords and strands of basaloid monomorphous cuboidal cells extending from the basal layer of epidermis into dermis
- Loose fibrovascular stroma
Board review style question #1
Which of the following vascular patterns is observed in the dermatoscopic evaluation of eccrine poroma?
- Glomerular
- Hairpin
- Mosaic
- Hairpin and glomerular
- Hairpin and mosaic
Board review style answer #1
D. Hairpin and glomerular. The vascular patterns commonly seen in eccrine poroma are the polymorphic, glomerular, linear irregular, leaf and flower-like and looped or hairpin variants. The leaf and flower-like pattern appears to be relatively unique to the poroma. Mosaic pattern is not observed in eccrine poroma (Clin Case Rep 2021;9:1601).
Comment Here
Reference: Poroma
Comment Here
Reference: Poroma
Board review style question #2
Which of the following is true about eccrine poroma?
- Most commonly occurs on central part of the body: frontal scalp, anterior chest and around umbilicus
- No distinct demarcation between the poroma cells and adjacent keratinocytes
- Presence of monomorphic, basaloid cells with peripheral palisading
- Presence of sheets and trabeculae of monomorphic, round basophilic cells containing scattered duct-like structures
Board review style answer #2
D. Presence of sheets and trabeculae of monomorphic, round basophilic cells containing scattered duct-like structures
Comment Here
Reference: Poroma
Comment Here
Reference: Poroma