Table of Contents
Nevi-general | Junctional nevus | Compound nevus | Dermal nevus | Lentiginous nevusCite this page: Hale CS. Nevi-general. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumormelanocyticnevigeneral.html. Accessed December 26th, 2024.
Nevi-general
Definition / general
Terminology
Epidemiology
Patterns associated with benign behavior
Clinical features
Prognostic factors
Case reports
Treatment
Gross description
Microscopic (histologic) description
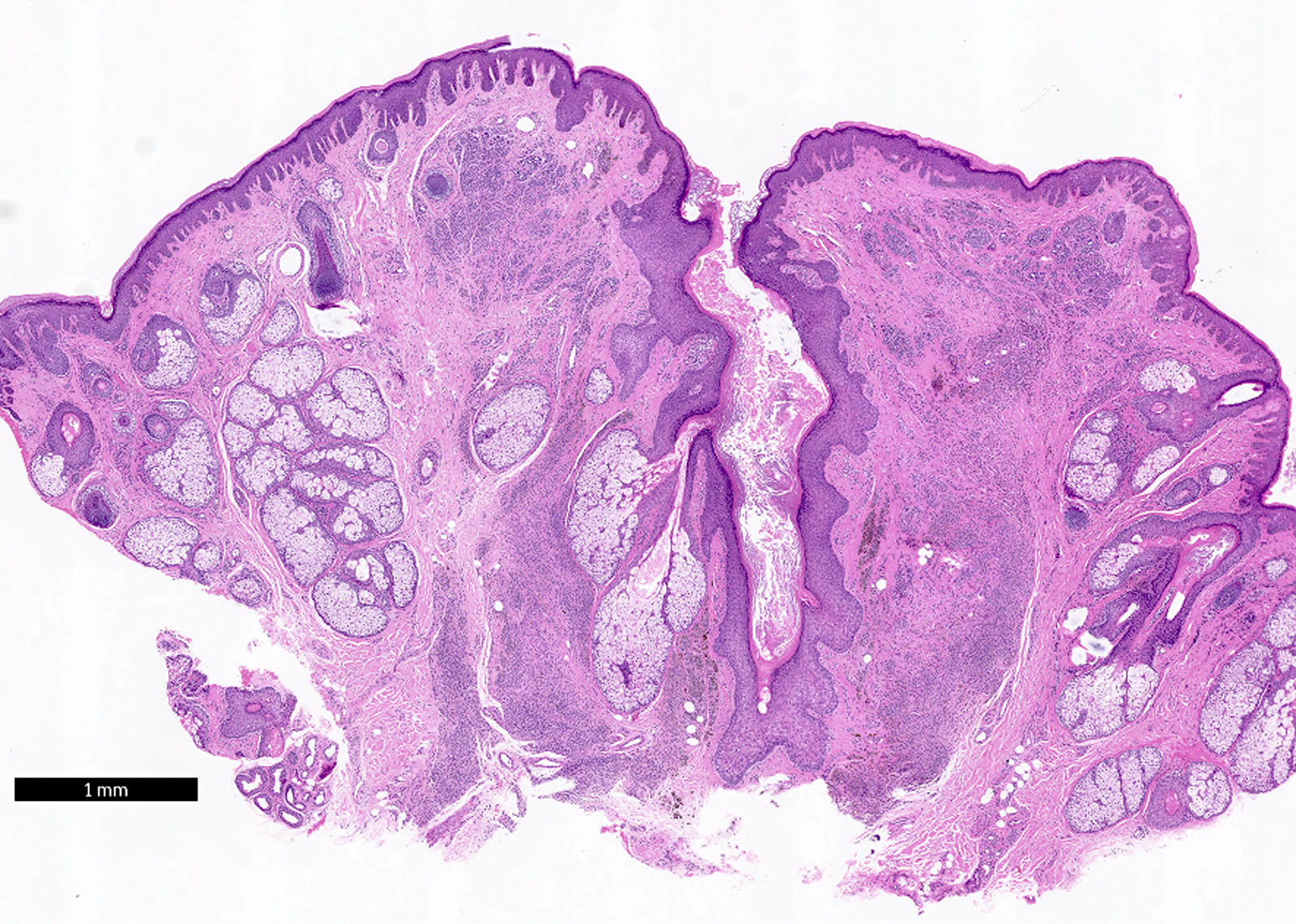
Microscopic (histologic) images
Contributed by Yuri Tachibana, M.D.
Images hosted on other servers:
Positive stains
Molecular / cytogenetics description
- Congenital or acquired benign melanocytic proliferation
- Dermoscopy: nevus type varies by skin type in whites (Arch Dermatol 2007;143:351)
- Color: due to Tyndall effect (scattering of light as it hits melanin granules); melanin in stratum corneum appears black, melanin in reticular dermis appears slate-gray or blue (Wikipedia: Tyndall Effect [Accessed 2 December 2021])
- Nevi may regress due to lymphocytic infiltration (see halo nevus)
Terminology
- Nevus (singular) also spelled naevus
- Means birthmark in Latin
- Also called melanocytic, nevocellular or pigmented lesion
Epidemiology
- Most common melanocytic tumor
- Usually clinically evident between ages 2 - 6 years
- Most whites have 20 - 30 nevi; much less common in Asians and Afro-Caribbeans
- Can estimate total body count in 13 - 14 year olds by examining lateral arms (Am J Epidemiol 2007;166:472)
- 2 theories of nevogenesis: Abtrofung versus Hochsteigerung (Arch Dermatol 2007;143:284)
Patterns associated with benign behavior
- Small size, circumscription and symmetry
- Nested proliferation with nests regularly distributed at tips of the rete ridges
- Melanocyte nuclei smaller than in adjacent keratinocytes
- Uniform cellular density throughout same level of lesion
- Melanocytes decrease in size towards base of lesion (maturation)
- Coalescent eosinophilic globules (Kamino bodies) are associated with Spitz nevi
- Absence of mitotic activity (particularly at base of lesion), although rare mitoses may be seen in benign nevi (J Cutan Pathol 2007;34:713, Am J Dermatopathol 2010;32:643)
- Lack of necrosis and cytologic atypia
Clinical features
- Nevi common on head, neck and trunk in Caucasians, on acral sites in Asians and Afro-Caribbeans
- Mostly occur in skin but also mucosal membranes covered by squamous epithelium
- May be neoplastic since many are clonal
- Existence of freckles, lentigines (small, pigmented, flat or slightly raised spots with a clearly defined edge but no nests of melanocytes) and melanocytic nevi increases chance of having melasma (BMC Dermatol 2008;8:3)
- Often accompanied by keratinous cysts, abscess or folliculitis
- Incidental microscopic aggregates of nevus cells occur in 1% of skin excisions (Am J Dermatopathol 2008;30:45); also occur in clusters in lymph node capsules (intracapsular nevus), particularly in axilla (see lymph nodes chapter)
- Large numbers of nevi are risk factor for melanoma (Int J Cancer 2009;124:420)
- Increasing numbers of nevi are associated with neonatal phototherapy, sun exposure on hot holidays and number of nevi in parents, although this does not necessarily mean that these factors are risk factors for melanoma (Arch Dermatol 2006;142:1599, J Invest Dermatol 2005;124:56, Cancer 2003;97:628)
Prognostic factors
- May recur with incomplete excision (shave biopsy), usually within 3 months
- Recurrent nevus (persistent nevus) may resemble melanoma (pseudomelanoma) due to irregular scarring, lentiginous melanocytic hyperplasia, basilar keratinocytic hyperpigmentation, nuclear enlargement and prominent nucleoli (J Cutan Pathol 2011;38:503)
Case reports
- 65 year old man with melanocytic intranuclear inclusions due to molluscum contagiosum (J Cutan Pathol 2008;35:782)
- Nodal nevus cells associated with dermatopathic lymphadenopathy (Diagn Cytopathol 2004;31:180)
Treatment
- Biopsy any clinically atypical melanocytic lesions in adults, such as nevi causing chronic mechanical irritation, itching, bleeding, ulceration or oozing of serum, nevi with rapid growth, deepening pigmentation, pigmentation beyond outline of lesion, flat areas of depigmentation or erythema
- Pathologically confirmed banal nevi and mildly atypical nevi do not require additional treatment
- Nevi with moderate and severe atypia usually are excised with negative margins
Gross description
- Papule or macule, tan-brown, uniformly pigmented and small (≤ 0.6 cm)
- Often erosion or ulceration if adjacent to a hair follicle, with a granulomatous response or scale crust
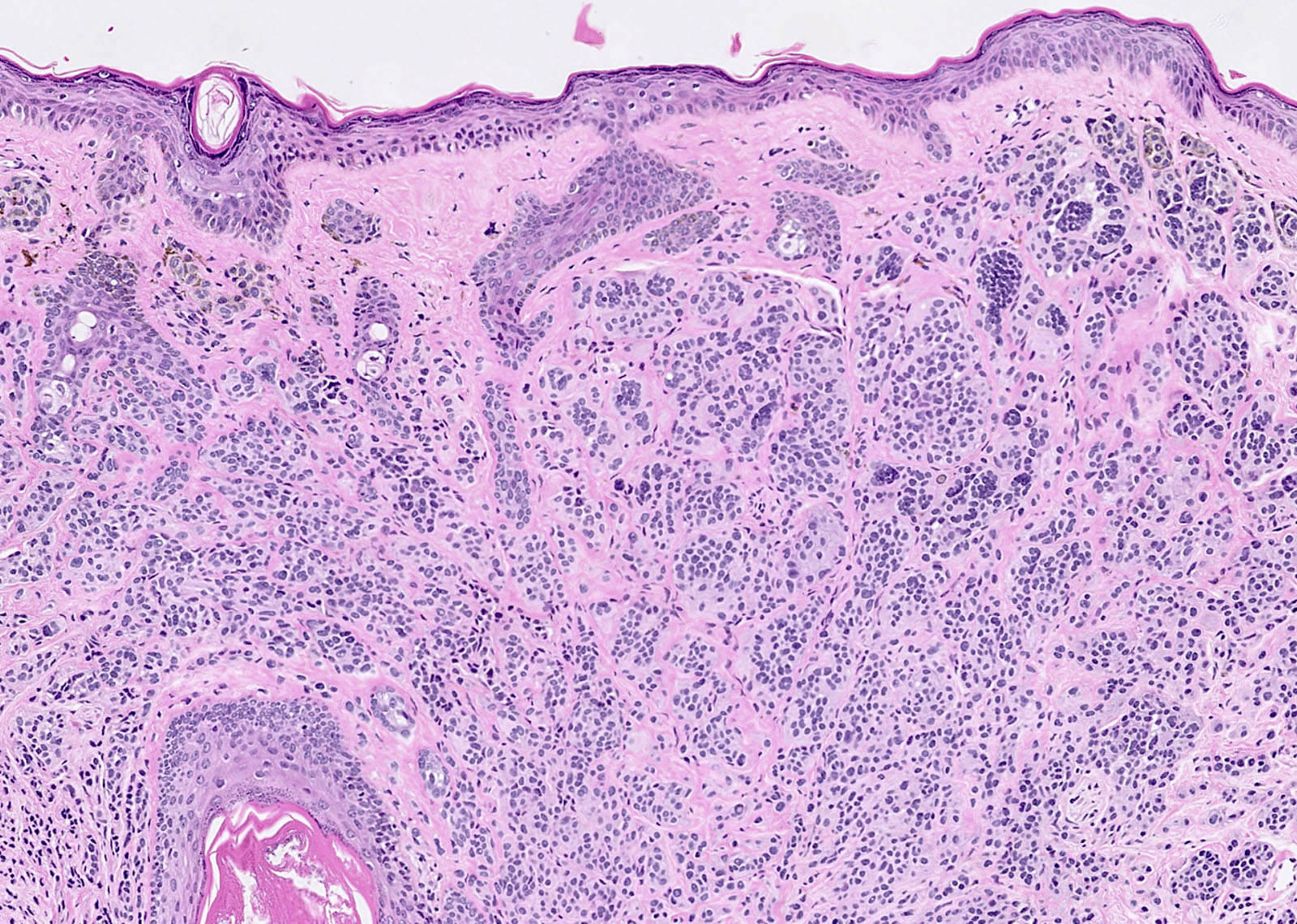
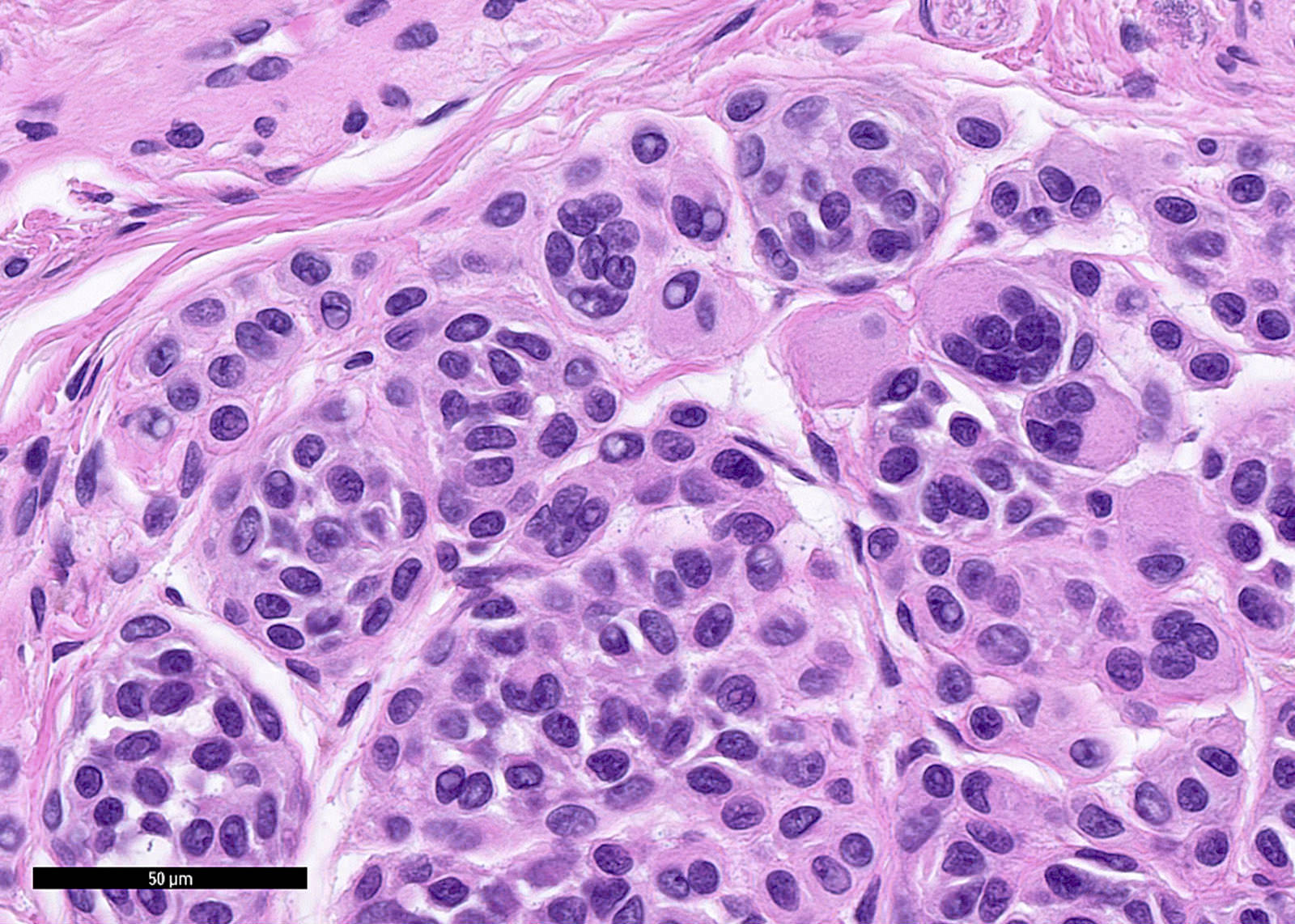
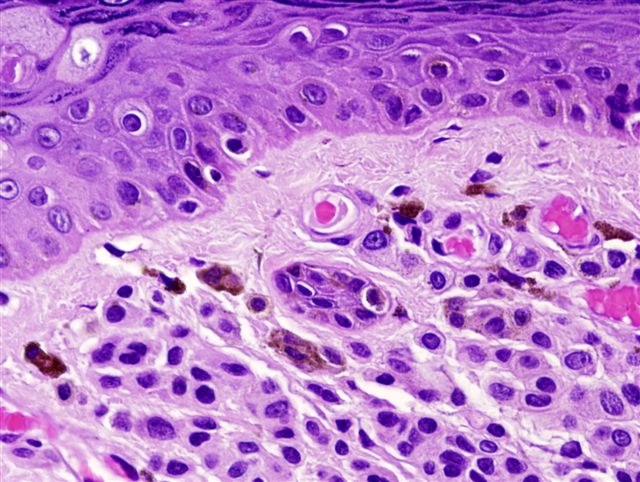
Microscopic (histologic) description
- Intraepidermal component: junctional nests of melanocytes uniform in size, distributed at the tips of the rete ridges
- Dermal component:
- Type A morphology:
- In superficial dermis
- Pigmented epithelioid cells with well defined cell boundaries
- Abundant eosinophilic to amphophilic cytoplasm containing coarse melanin granules
- Uniform round / oval nuclei slightly smaller than that of adjacent keratinocytes
- Finely dispersed chromatin
- Delicate nuclear membrane
- No / small distinct eosinophilic nucleoli
- Type B morphology:
- In intermediate dermis
- Cells more lymphoid than epithelioid
- Decreased cytoplasm with no melanin
- Smaller and slightly hyperchromatic nuclei with dispersed chromatin and no nucleoli
- Type C morphology:
- In deep dermis
- Spindled, fibroblast-like or schwannian cells with oval nuclei and bland chromatin
- Single cell infiltration of superficial reticular collagen
- Maturation:
- Deeper portion of lesion has smaller cells with less pigment and less atypia
- Deep cells grow in smaller sized nests or single cells
- May resemble neural tissue
- Terminal differentiation recapitulates some aspects of Schwann cell development (Am J Pathol 1999;155:549)
- Traumatized nevi:
- Features include parakeratosis (92%), dermal telangiectasias (61%), ulceration (51%), dermal inflammation (49%), melanin within stratum corneum (24%), dermal fibrosis (25%), pagetoid spread of melanocytes limited to the site of trauma (20%) or away from areas of trauma (8%) (Am J Dermatopathol 2007;29:134)
- Type A morphology:
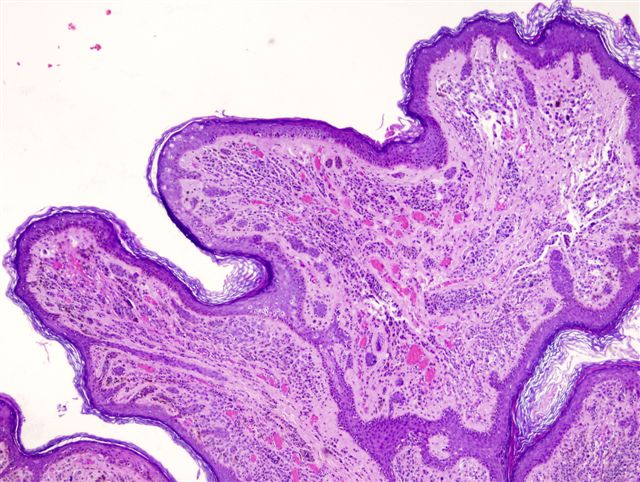
Microscopic (histologic) images
Contributed by Yuri Tachibana, M.D.
Images hosted on other servers:
Positive stains
- MelanA in type A and B but not type C cells
- S100, HMB45 in the intraepidermal and superficial dermal component
Molecular / cytogenetics description
- BRAF mutations in 75% of congenital and acquired nevi, have clonal genetic changes (Hum Pathol 2002;33:191, Am J Dermatopathol 2007;29:534)
Junctional nevus
Definition / general
Terminology
Epidemiology
Sites
Clinical features
Case reports
Treatment
Dermoscopy
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Mark R. Wick, M.D.
Differential diagnosis
- Melanocytic proliferation restricted to basal epidermis (junctional area)
- Earliest stage of intraepidermal melanocytic proliferation
Terminology
- Lentigo simplex:
- Also called lentigo, lentigines
- Often in acral sites
- Precursor lesion to nevi, with proliferation of melanocytes (but no nests) in epidermal basal layer along rete ridges (DermNet NZ: Lentigo Simplex [Accessed 2 December 2021])
- Multiple lentigines:
- Associated with Peutz-Jeghers syndrome, centrofacial lentiginosis, Moynahan’s syndrome, LEOPARD syndrome, Carney’s syndrome and xeroderma pigmentosum
Epidemiology
- Traditionally considered more common in children (possible sampling bias), may actually occur in all ages (J Am Acad Dermatol 2007;56:825)
- Melanomas may arise from junctional nevi
Sites
- Usually non sun exposed areas, such as palms and soles (J Am Acad Dermatol 2007;56:825)
Clinical features
- Small, flat or slightly elevated; non hairy, deeply pigmented
Case reports
- 57 year old woman with coexisting mastocytoma (Am J Dermatopathol 2004;26:478)
Treatment
- None needed; excision for cosmetic reasons, laser for flat lesions (Br J Dermatol 2003;148:80)
Dermoscopy
- Regular pigmented network of brown and uniform color, more prominent in center with gradual fading to borders (reticular pattern)
- May have black or brown globules and dots regularly distributed inside lesion (usually in central region)
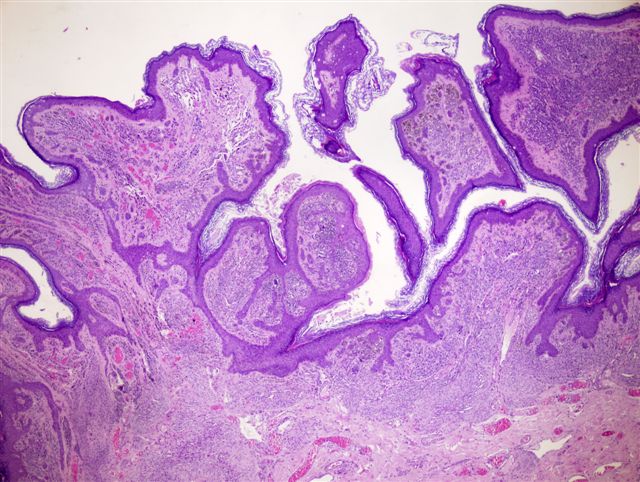
Microscopic (histologic) description
- Rounded nests of melanocytes / nevus cells on epidermal side of dermoepidermal junction, originating from tips of rete ridges
- Variable lentiginous melanocytic hyperplasia
Microscopic (histologic) images
Contributed by Mark R. Wick, M.D.
Differential diagnosis
- Lentigo
- Melanoma
Compound nevus
Definition / general
Terminology
Epidemiology
Clinical features
Clinical images
Images hosted on other servers:
Case reports
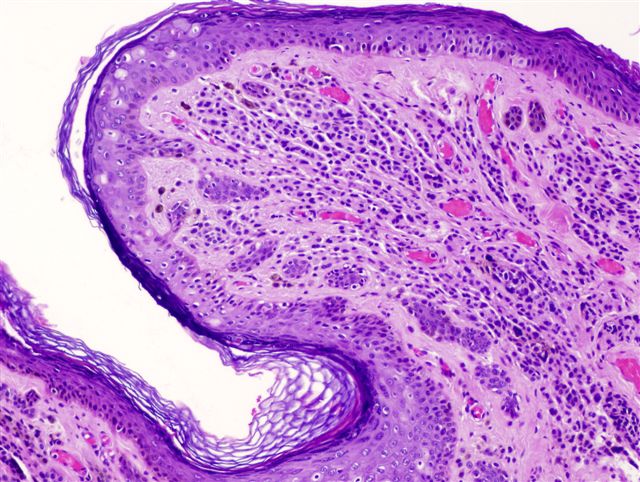
Microscopic (histologic) description
Videos
Differential diagnosis
- Features of both junctional and intradermal nevi (i.e. epidermal and dermal components)
Terminology
- Compound = junctional and intradermal components
- Do not confuse with combined nevus
Epidemiology
- Highest incidence in second decade, then decreases (Arch Dermatol 1962;86:310)
Clinical features
- Elevated or dome shaped
- Less pigmented than junctional nevi
- Only rarely undergoes malignant transformation
- Nevogenesis may be due to ultraviolet light (Am J Dermatopathol 2005;27:456)
Clinical images
Images hosted on other servers:
Case reports
- 17 year old girl with pigmented lesion on mons pubis (Arch Pathol Lab Med 2003;127:e391)
- 17 year old girl with compound nevus and spindle cell Spitz nevus (J Dermatol 2000;27:233)
Microscopic (histologic) description
- Features of both junctional and intradermal nevi (i.e. epidermal and dermal components)
- Junctional component is similar to junctional nevus, with nests regularly distributed at bases of rete ridges, occasional lentiginous pattern, no pagetoid spread, no atypia, symmetry diminishes with patient age
- Dermal component consists of nests (may be very large) or linear pattern of melanocytes, cells are small with scant cytoplasm and regular nuclei and mature with depth by becoming more slender / spindled with less pigment
- Dermal melanocytes or nests are separated by collagenous stroma
- Often clusters of chronic inflammatory cells at base of nevus
- Mucin in < 1% (Am J Dermatopathol 2008;30:236)
- May have occasional mitoses (Am J Dermatopathol 2013;35:30)
Videos
Compound nevus with halo reaction
Differential diagnosis
- Other melanocytic proliferations
Dermal nevus
Definition / general
Terminology
Epidemiology
Clinical features
Dermoscopy description
Case reports
Clinical images
Contributed by Mark R. Wick, M.D.
Images hosted on other servers:
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Yuri Tachibana, M.D. and Angel Fernandez-Flores, M.D., Ph.D.
Images hosted on other servers:
- Nevus with all melanocytes within the dermis
Terminology
- Also called intradermal nevus
Epidemiology
- Most common adult nevus
- Represents final stage in progression from junctional to compound to dermal nevus
- Seen mainly after adolescence
Clinical features
- Flat, pedunculated or papillary, often hairy
- Flesh colored or lightly pigmented (usually becomes lighter over time)
- Pigmentation may be in flecks up to 1 cm
- Melanomas only rarely arise from intradermal nevi (Dermatology 1998;196:425)
- Rarely has cerebriform appearance; these nevi may be congenital (Cutis 2004;73:254)
Dermoscopy description
- Nonpigmented lesions: brown pigment (78%), white areas (53%), comma shaped vessels (50%), hair (47%), hairpin vessels (22%), comedolike openings (22%) and dotted vessels (19%) (Dermatol Surg 2007;33:1120)
Case reports
- 46 year old woman with osseous metaplasia / osteonevus of Nanta in intradermal melanocytic nevus (Dermatol Online J 2007;13:16)
- Intradermal melanocytic nevus with prominent Verocay-like bodies (Am J Dermatopathol 2002;24:39)
Clinical images
Contributed by Mark R. Wick, M.D.
Images hosted on other servers:
Microscopic (histologic) description
- Small nests of melanocytes in upper dermis, often around pilosebaceous units, with variable pigmentation and cellularity
- May have multinucleated melanocytes; deeper portion is usually less pigmented and less cellular and may have Wagner-Meissner corpuscles (representing neural portion of nevus)
- Mucin in 3% of stroma and within nests of nevus cells (Am J Dermatopathol 2008;30:236)
- Rarely nevus giant cells, balloon cells, infiltration by fat cells or osseous metaplasia
- No junctional component
- Can also be classified as Unna’s pattern (purely adventitial lesion confined to expanded papillary dermis and often to perifollicular dermis, usually neck, trunk or limbs) or Miescher’s pattern (melanocytes diffusely infiltrate adventitial and reticular dermis in wedge shaped pattern, usually on face) (Am J Dermatopathol 2007;29:141)
- Slit-like pseudovascular spaces may be seen through artifact of processing and biopsy procedure (Ultrastruct Pathol 1980;1:361, Am J Dermatopathol 1984;6 Suppl:25)
Microscopic (histologic) images
Contributed by Yuri Tachibana, M.D. and Angel Fernandez-Flores, M.D., Ph.D.
Images hosted on other servers:
Lentiginous nevus
Definition / general
Terminology
Epidemiology
Clinical features
Case reports
Treatment
Clinical images
Images hosted on other servers:
Microscopic (histologic) description
Microscopic (histologic) images
Images hosted on other servers:
Differential diagnosis
- Common type of agminate (clustered) nevus with multiple pigmented macules or papules within a pigmented patch (Cutis 2007;80:465, eMedicine: Speckled Lentiginous Nevus)
- May be congenital or acquired (Arch Dermatol 2001;137:172)
Terminology
- Also called speckled lentiginous nevus or nevus spilus
- Not related to acral lentiginous nevus (see acral nevi)
Epidemiology
- Speckled lentiginous nevus syndrome: hyperhidrosis, muscular weakness, dysesthesia or other neurological abnormalities
Clinical features
- Often benign mole with increase in size, formation of irregular borders or peripheral change in color
- May be due to reactivation of radial proliferation
- Usually ≤ 5 mm
- Note: atypia often present in childhood acral lesions (Pediatr Dev Pathol 1998;1:388)
Case reports
- 42 year old man with speckled lentiginous nevus on trunk (Dermatology 2004;209:228)
- 45 year old man with melanoma (Int J Dermatol 2006;45:1362)
Treatment
- Excision of speckles or entire lesion
Clinical images
Images hosted on other servers:
Microscopic (histologic) description
- Shoulder area of lentiginous junctional melanocytic proliferation beyond lateral border of underlying dermal nevus
- Elongation of rete ridges with small nests of melanocytes at tips of rete
- Individual unit melanocytes extending along sides of rete, often mild lymphohistiocytic infiltrate with pigment incontinence
- No atypia, no pagetoid spread and no dermal fibrosis
- Acral lesions: resemble dysplastic nevus due to elongation of rete ridges, continuous proliferation of melanocytes at dermoepidermal junction, single scattered melanocytes or less commonly small clusters within the upper epidermis; poor or absent lateral circumscription, melanocytes with abundant pale cytoplasm and round / oval, sometimes hyperchromatic nuclei and prominent nucleoli present at the dermoepidermal junction; however, unlike dysplastic nevi, they lack anastomosing rete ridges, cytological atypia and well formed lamellar fibroplasia (Histopathology 1995;27:549)
- Variants:
- Macular variant: jentigo pattern (lentiginous pattern plus nests of melanocytes at dermal epidermal junction) in the darker speckles and by some nests of melanocytes at the dermoepidermal junction at the tips of the papillae but background pigmentation has microscopic features of lentigo; tan-brown background with dark flat speckles in relatively even distribution resembling polka dots; associated with phacomatosis pigmentovascularis
- Papular variant: dermal or compound melanocytic nevi; light-brown macule superimposed by multiple melanocytic nevi in the form of papules or nodules that show a more uneven distribution reminiscent of a star map; small dark macules may be present; associated with phacomatosis pigmentokeratotica or speckled lentiginous nevi syndrome (Dermatology 2006;212:53)
Microscopic (histologic) images
Images hosted on other servers:
Differential diagnosis
- Dysplastic nevus
- Lentigines:
- No nests, may be nevi if examine serial sections (Am J Dermatopathol 1985;7 Suppl:5)
- Superficial spreading or lentiginous melanoma
- Pagetoid lateral spread, mitotic activity in deep dermis and no maturation (Mod Pathol 2005;18:1397)