Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Rodríguez-Jiménez P, Muñoz-Hernández P. Urticaria (hives). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorurticaria.html. Accessed March 31st, 2025.
Definition / general
- Cutaneous reaction pattern characterized clinically by transient, often pruritic, edematous, erythematous papules or wheals due to localized mast cell degranulation and dermal microvascular hyperpermeability
- Individual lesions fade within 24 hours, although episodes may last days to months (Allergy 2018;73:1393, J Eur Acad Dermatol Venereol 2018;32:282)
- Chronic urticaria is defined as recurrent whealing that lasts for more than 6 weeks
Essential features
- Urticaria is characterized by transient skin or mucosal swellings due to plasma leakage
- Superficial dermal swellings are termed wheals and deep swellings of the skin or mucosa are termed angioedema
- Wheals are characteristically pruritic and pink or pale in the center, whereas angioedema is often painful, less well defined and shows no color change
Terminology
- Urticaria / hives
- Superficial dermal swellings are termed wheals: characteristically pruritic and pink or pale in the center
- Deep swellings of the skin or mucosa are termed angioedema: often painful, less well defined and showing no color change
ICD coding
- ICD-10: L50.9 - urticaria, unspecified
Epidemiology
- 15% of population on at least 1 occasion in their lifetime (Allergy 2011;66:317)
- F:M = 2:1
- Children and young adults more likely to have acute urticaria
- Middle aged adults for chronic urticaria
Sites
- Acute: disseminated
- Chronic:
- Spontaneous: disseminated
- Inducible: areas of exposure (sun exposed sites, colder areas, physical pressure, etc.)
Pathophysiology
- Stimuli → mast cell degranulation → histamine and other proinflammatory mediators release → vasodilation and increased permeability of postcapillary venules to large plasma proteins, including albumin and immunoglobulins → transient skin or mucosal swellings due to plasma leakage
Etiology
- Approximately 75% of cases are idiopathic
- Infections (typically viral, including SARS-CoV2)
- Collagen vascular disorders (SLE, autoinflammatory disorders, etc.)
- Malignancy (most common: Hodgkin lymphoma)
- IgE mediated allergies or IgE independent allergies (contrast dye, opiates, aspirin, ACE inhibitors - suppresses prostaglandins)
- Hereditary angioedema (deficiency of C1 esterase inhibitor causes uncontrolled complement component activation)
- Physical stimuli (heat, cold, pressure, vibration, etc.)
- Reference: Allergy 2018;73:1393
Diagrams / tables
Clinical features
- Acute spontaneous urticaria can have an allergic basis but chronic spontaneous urticaria usually does not
- While urticaria often develops in the setting of anaphylaxis, the vast majority of patients who present with wheals rarely progress to anaphylaxis
Laboratory
- Chronic spontaneous urticaria (positivity variable):
- Acute phase reactants elevation (ESR, CRP, D-dimer)
- TSH and antithyroid antibodies
- IgE level elevation
- Tryptase if suspicion of systemic mastocytosis
- References: Allergy 2018;73:1393, J Eur Acad Dermatol Venereol 2018;32:282
Prognostic factors
- None reliable to date
Case reports
- 34 year old man presented with an eruption on his hands and forearms (J Clin Aesthet Dermatol 2020;13:20)
- 51 year old woman presented with a 3 day history of dry cough and arthralgias and simultaneous widespread pruritic evanescent skin lesions lasting < 24 hours (Int J Dermatol 2020;59:867)
Treatment
- Acute:
- Second generation antihistamines
- Oral corticoisteroids (only if angioedema or highly symptomatic)
- Chronic:
- Second generation antihistamines
- Oral corticoisteroids (only if angioedema or highly symptomatic)
- Omalizumab (anti IgE antibody)
- Reference: Allergy 2018;73:1393
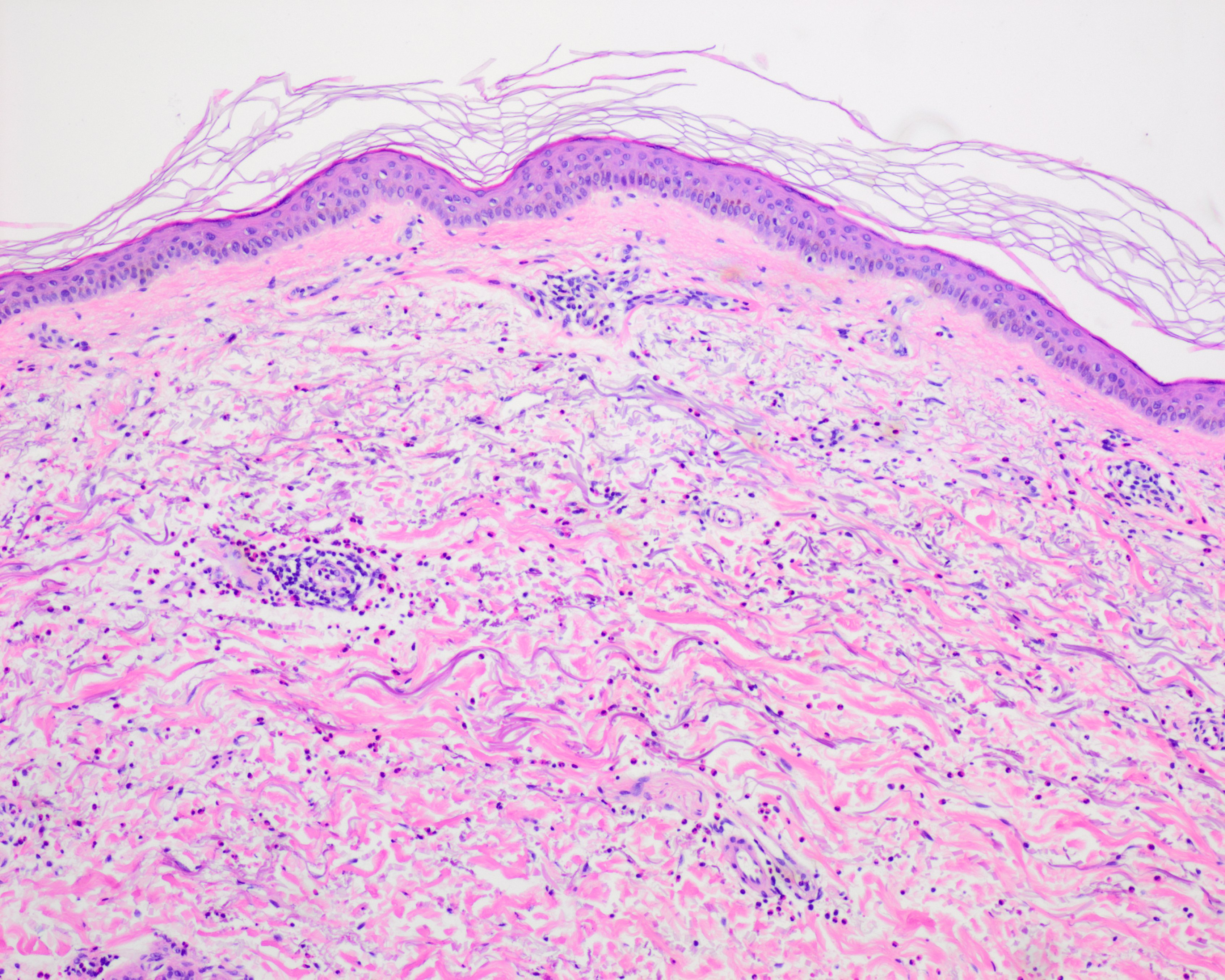
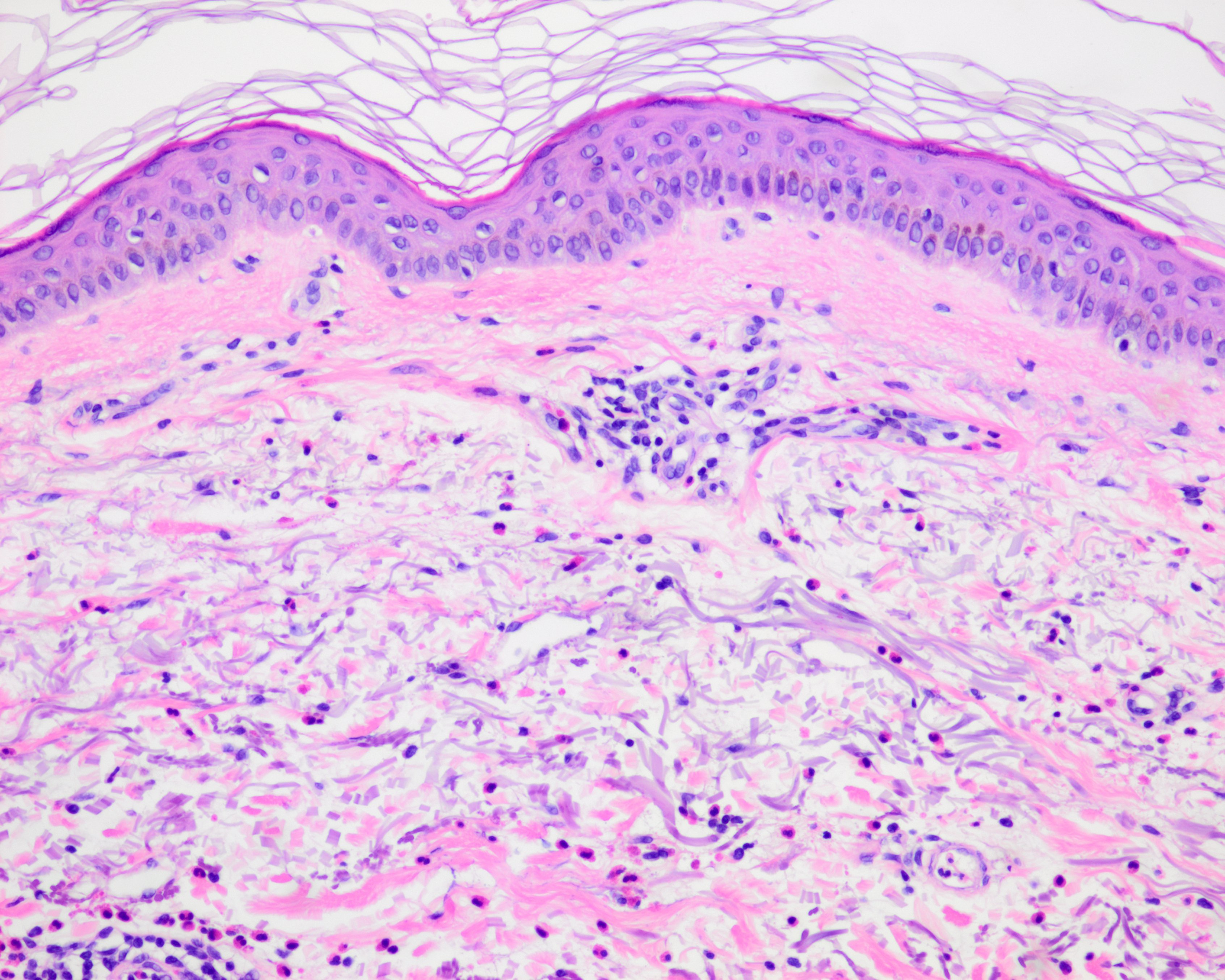
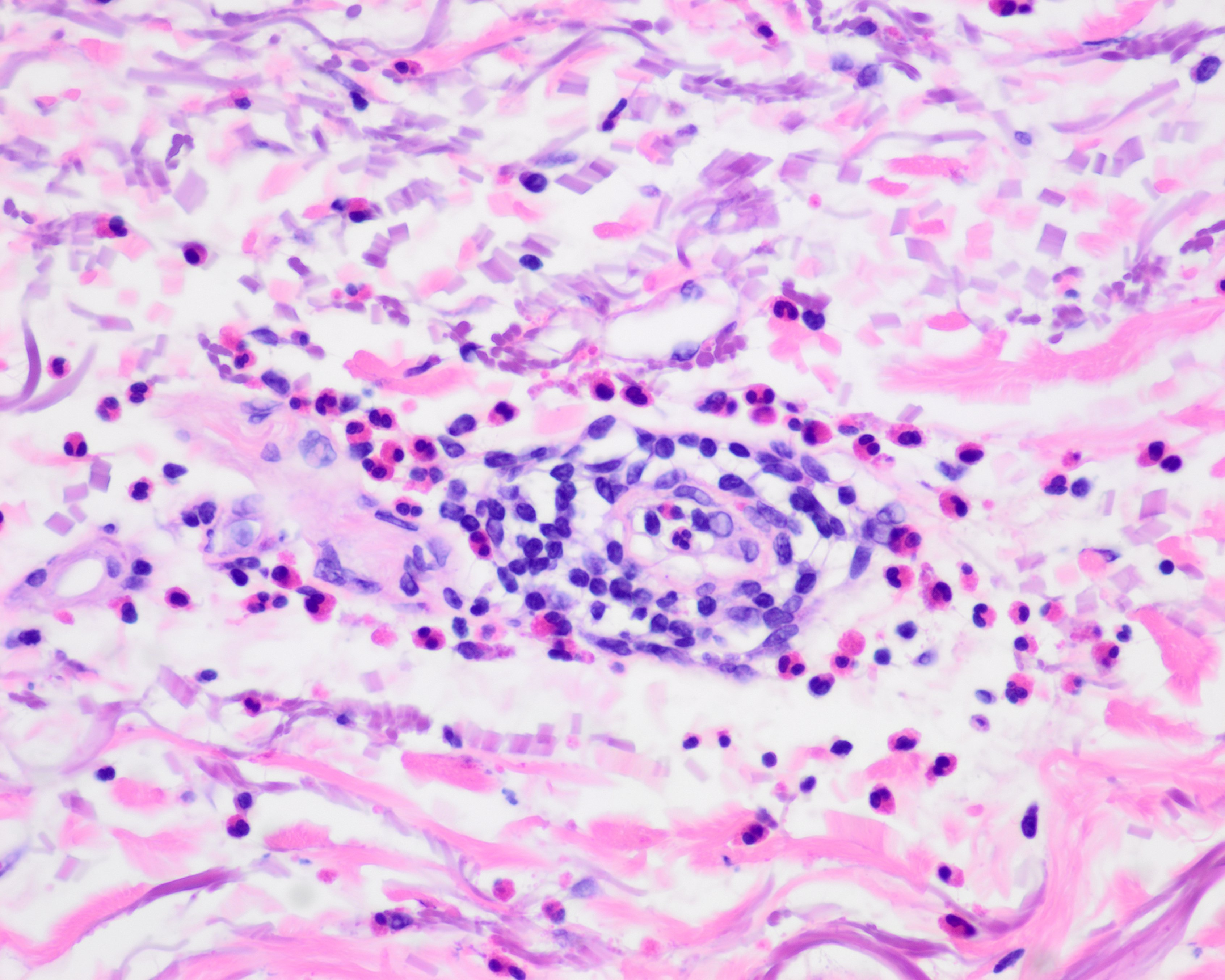
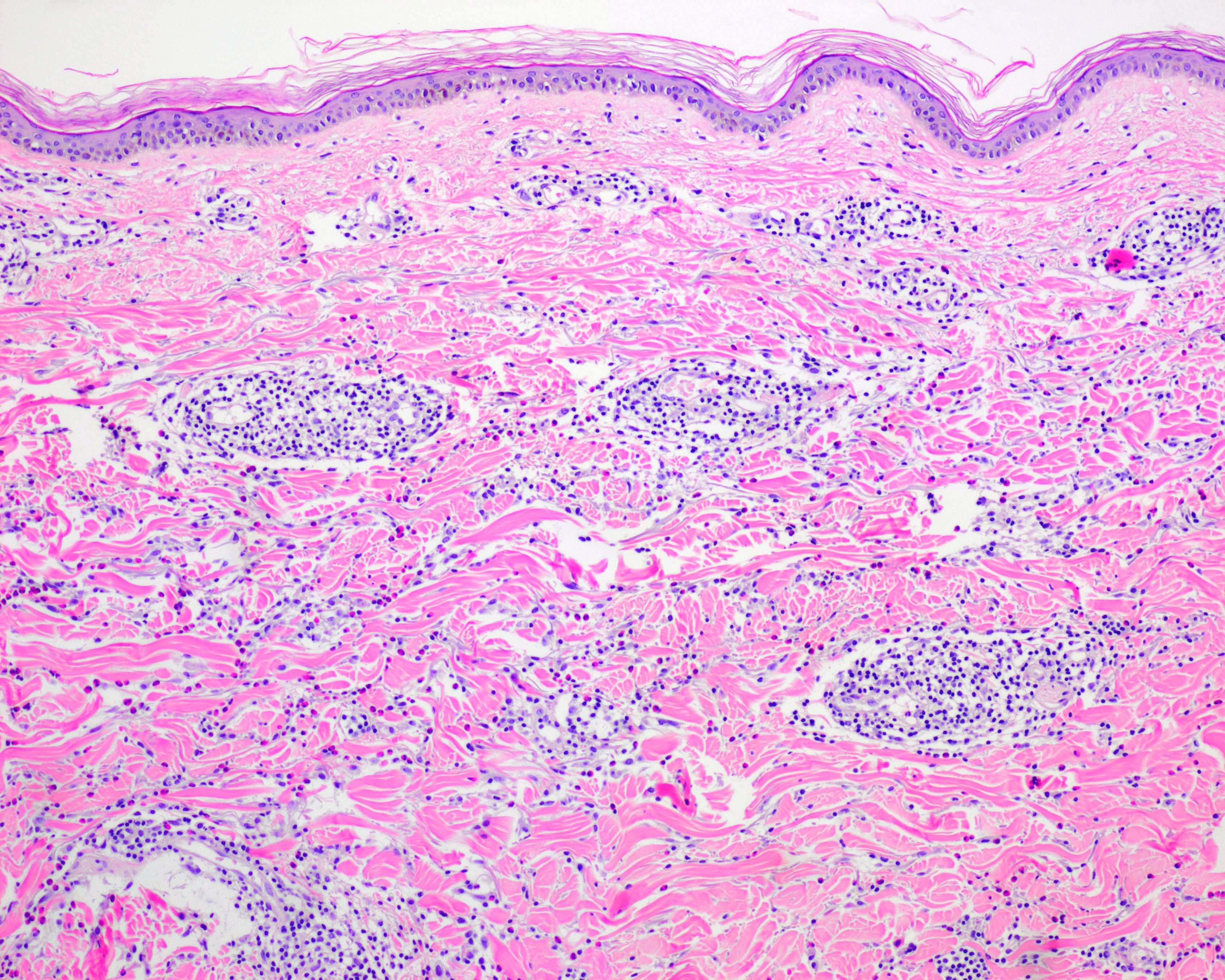
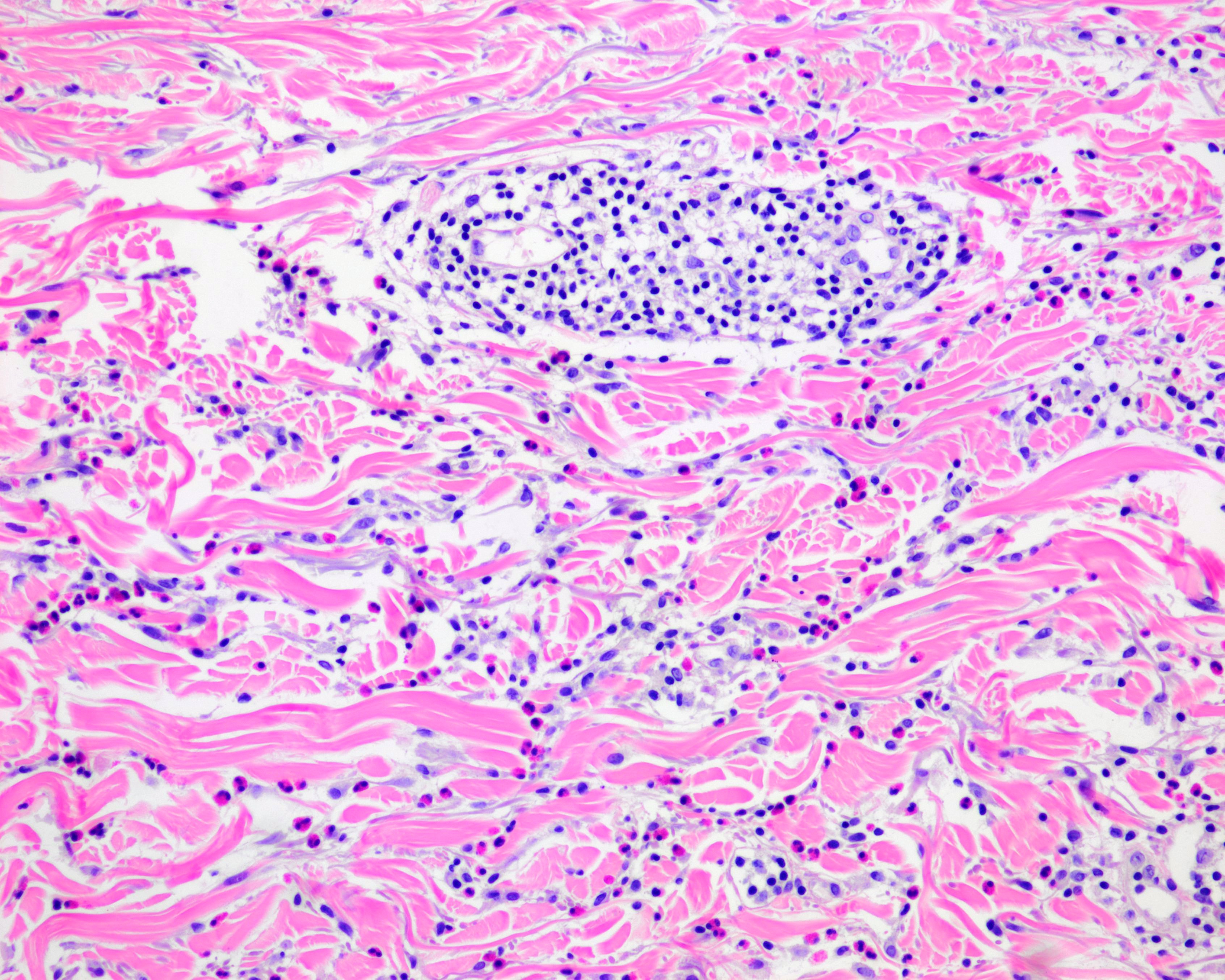
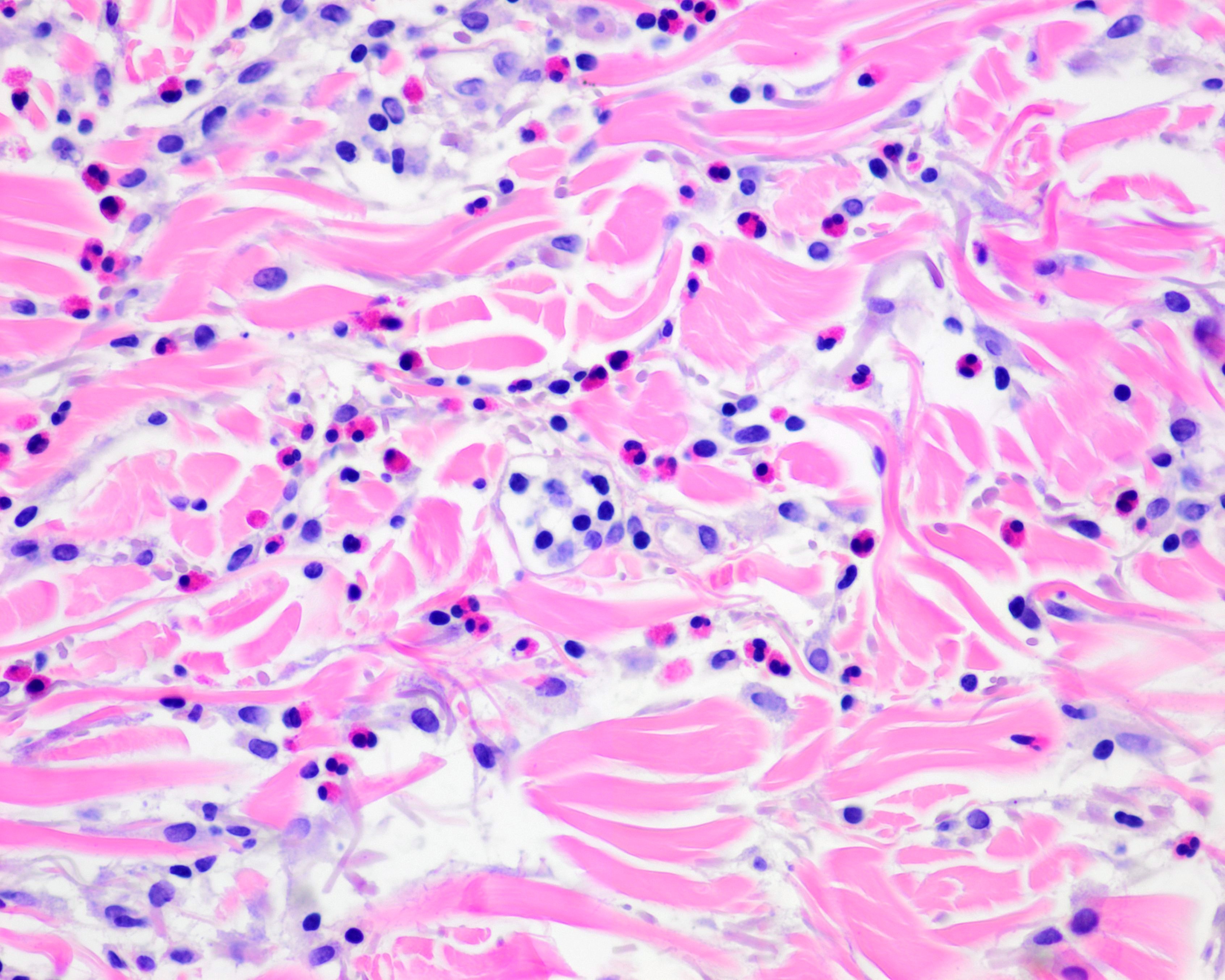
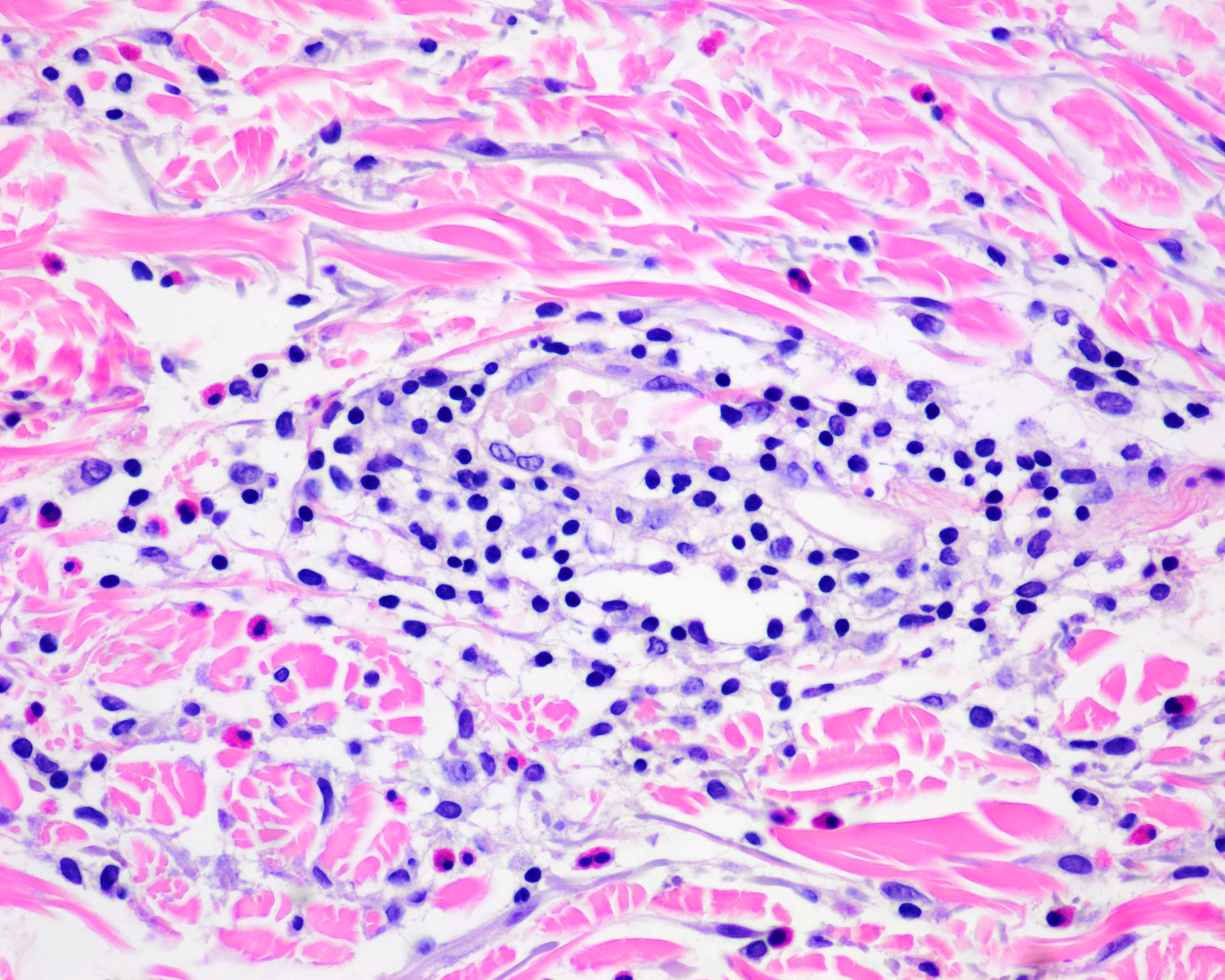
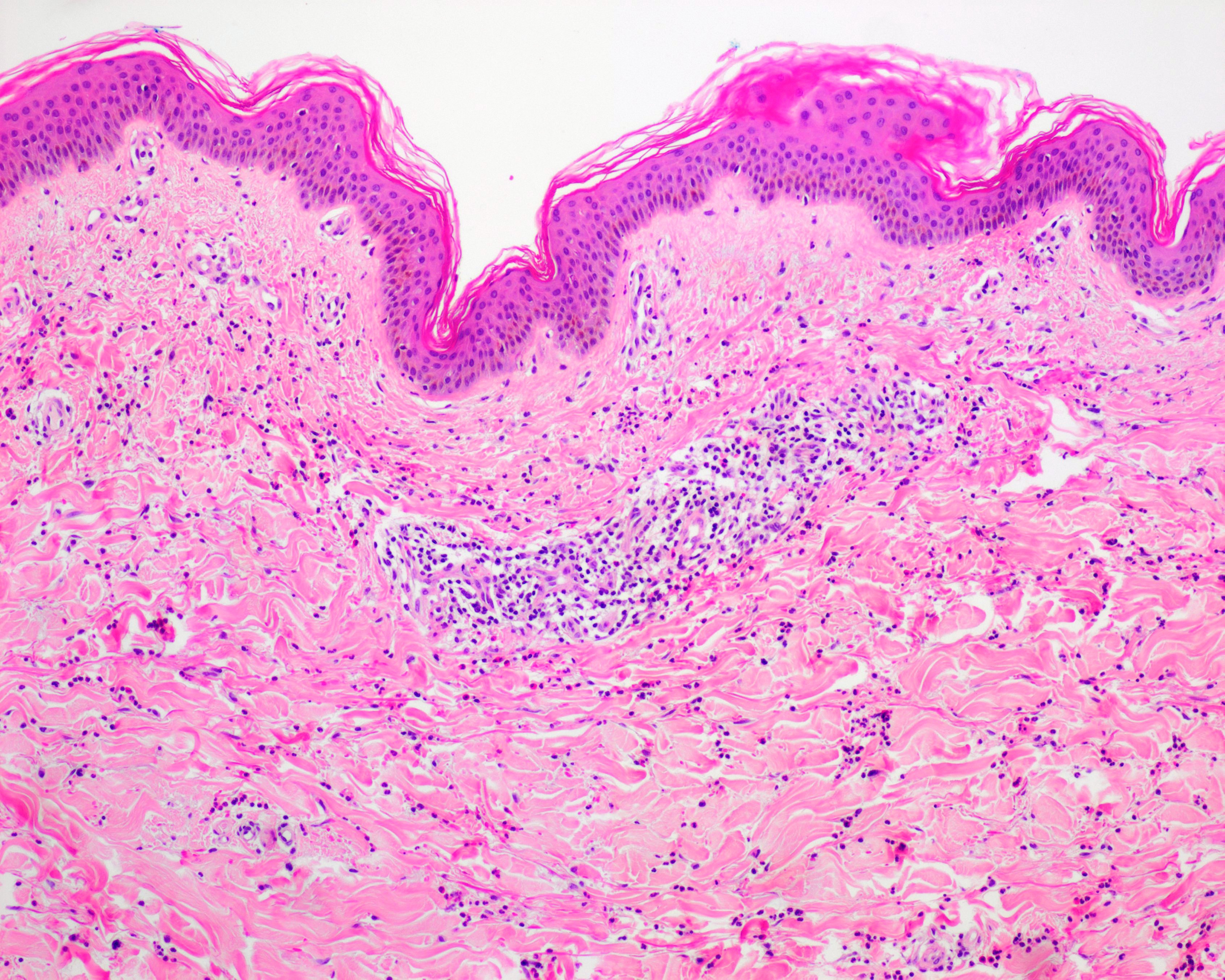
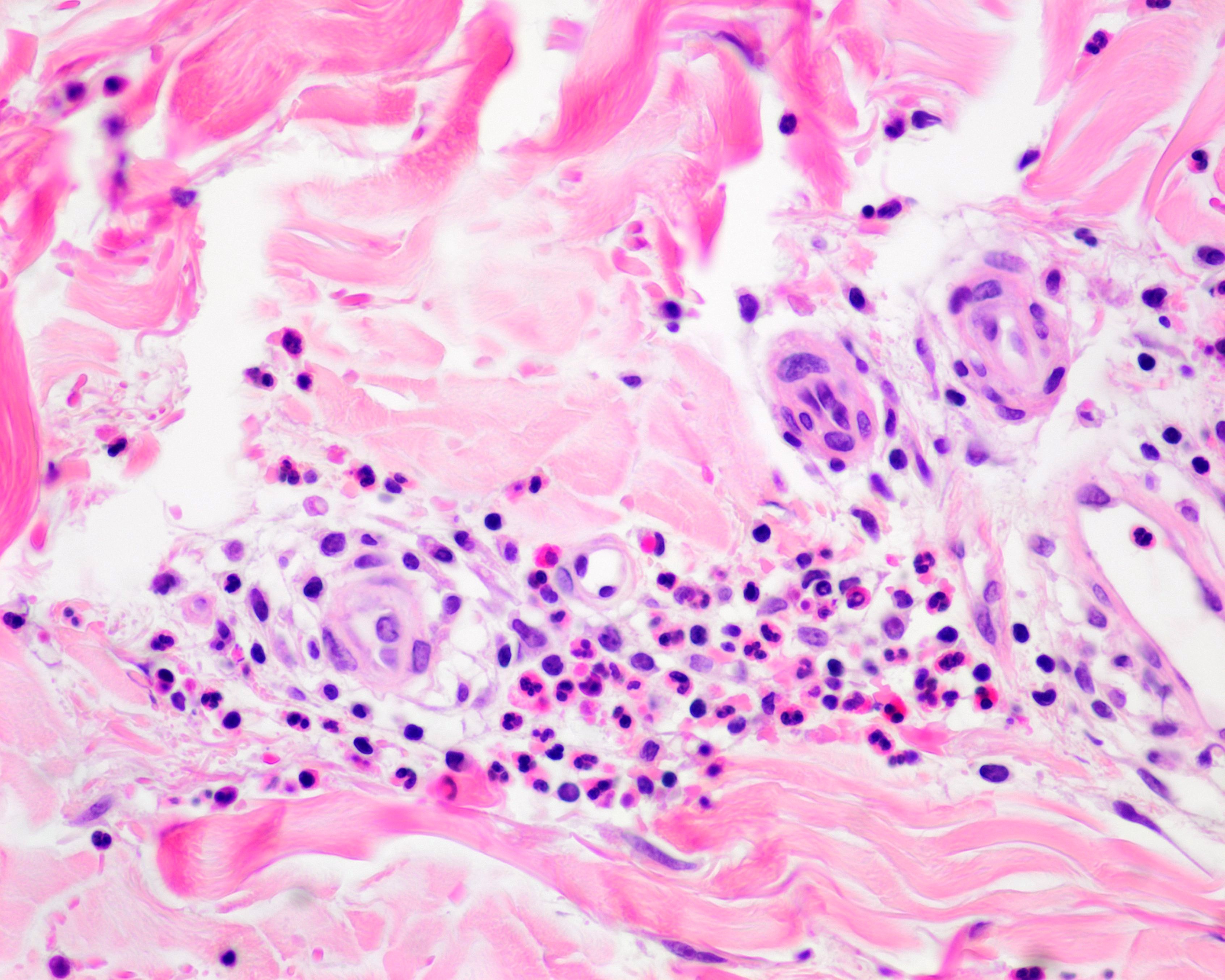
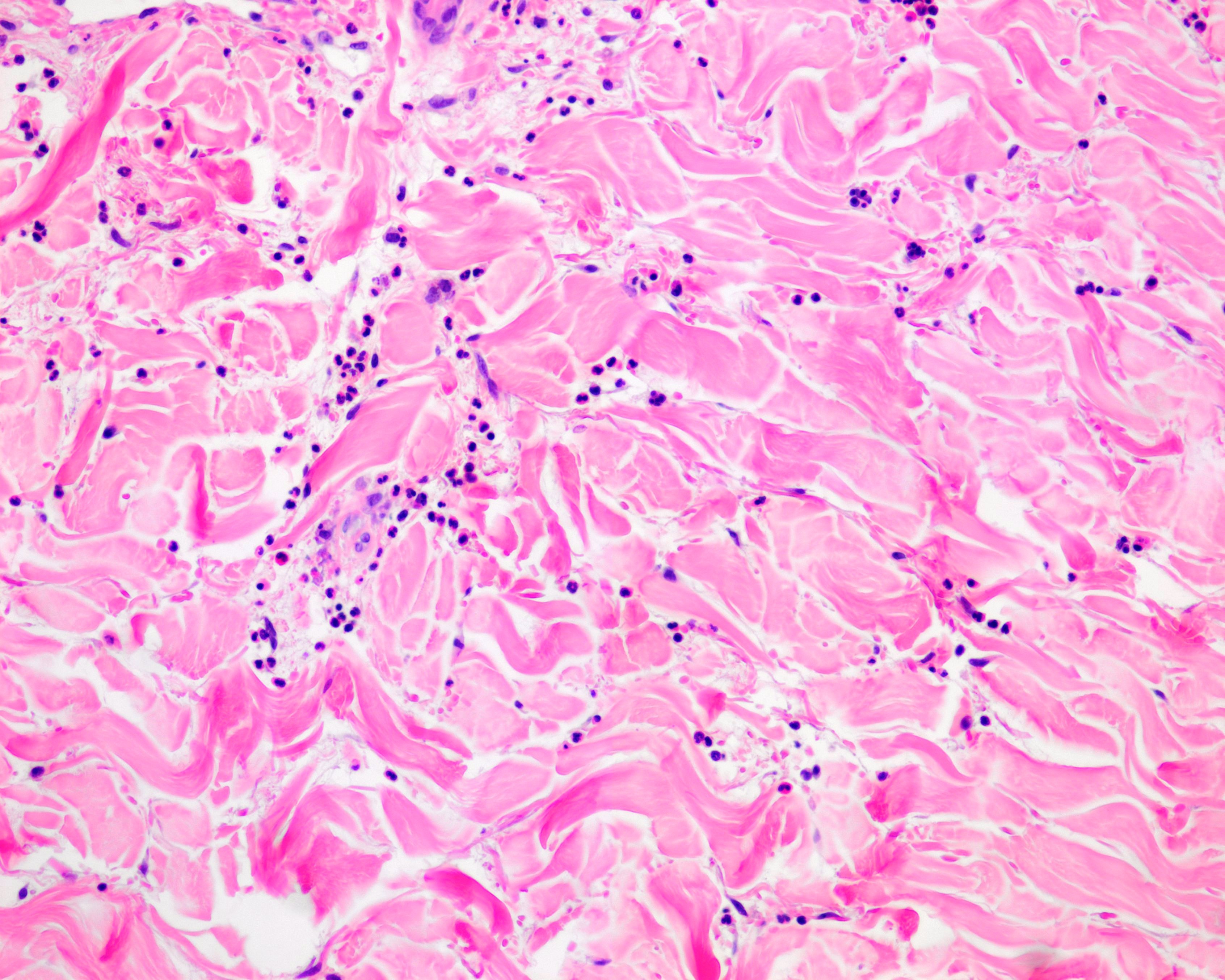
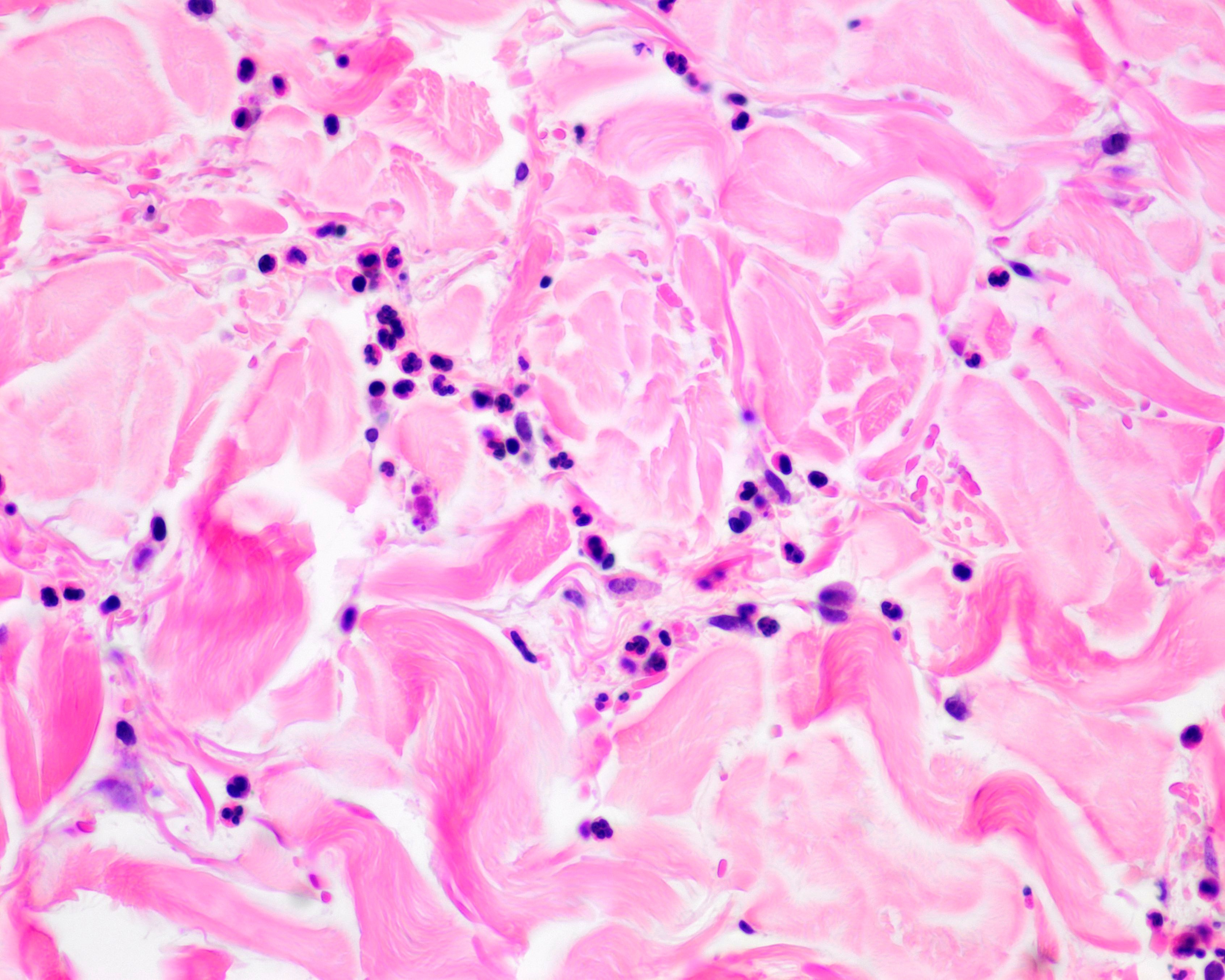
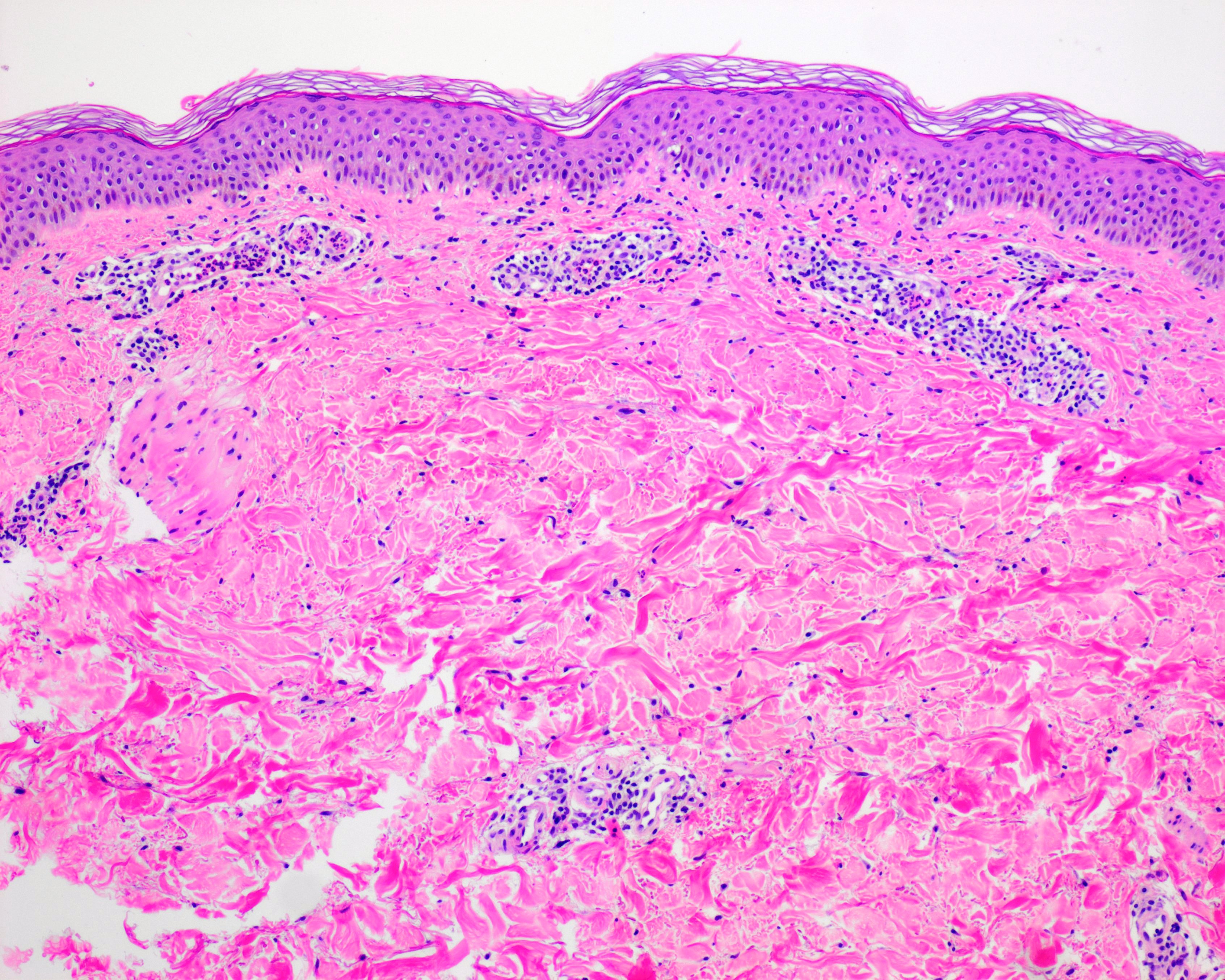
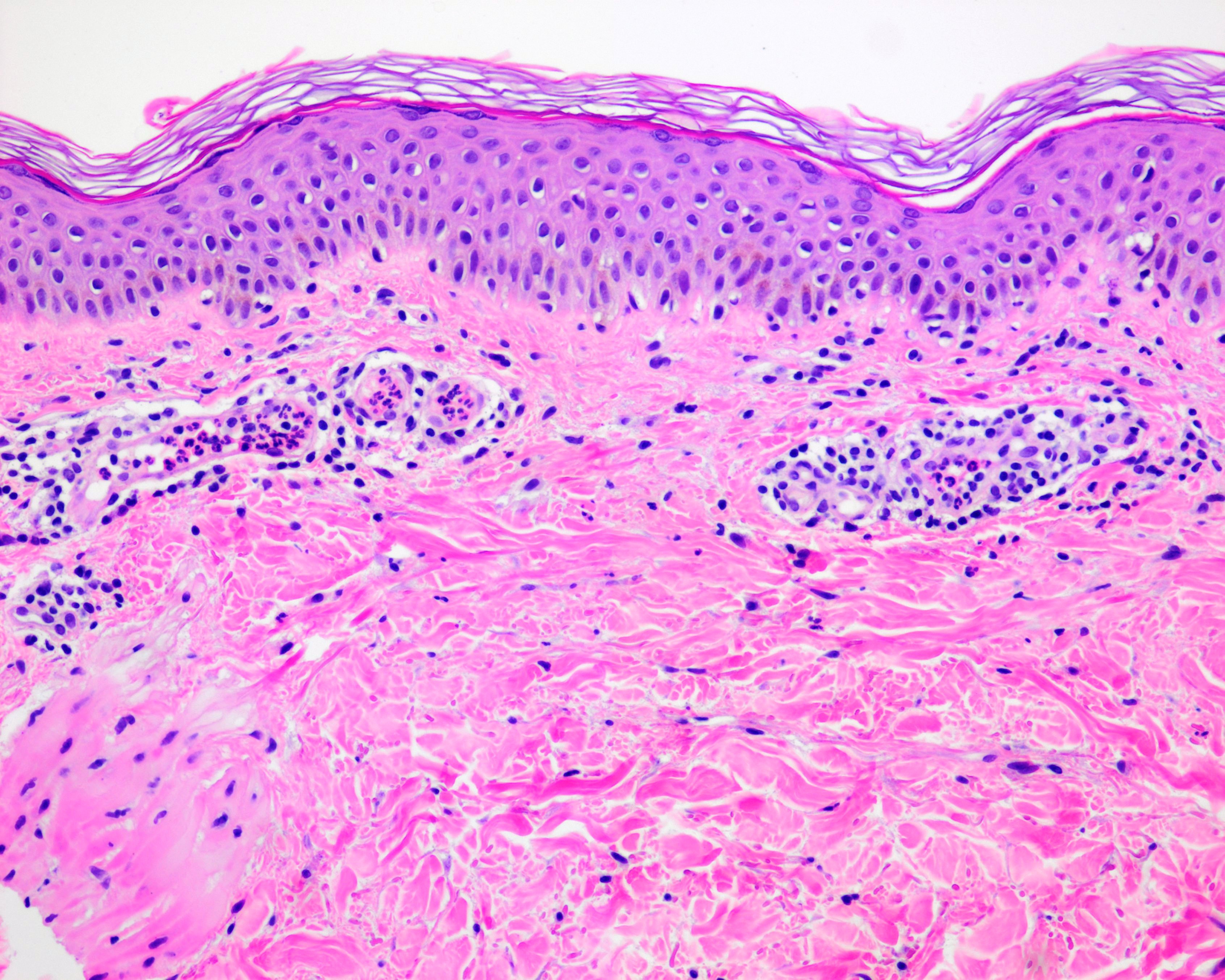
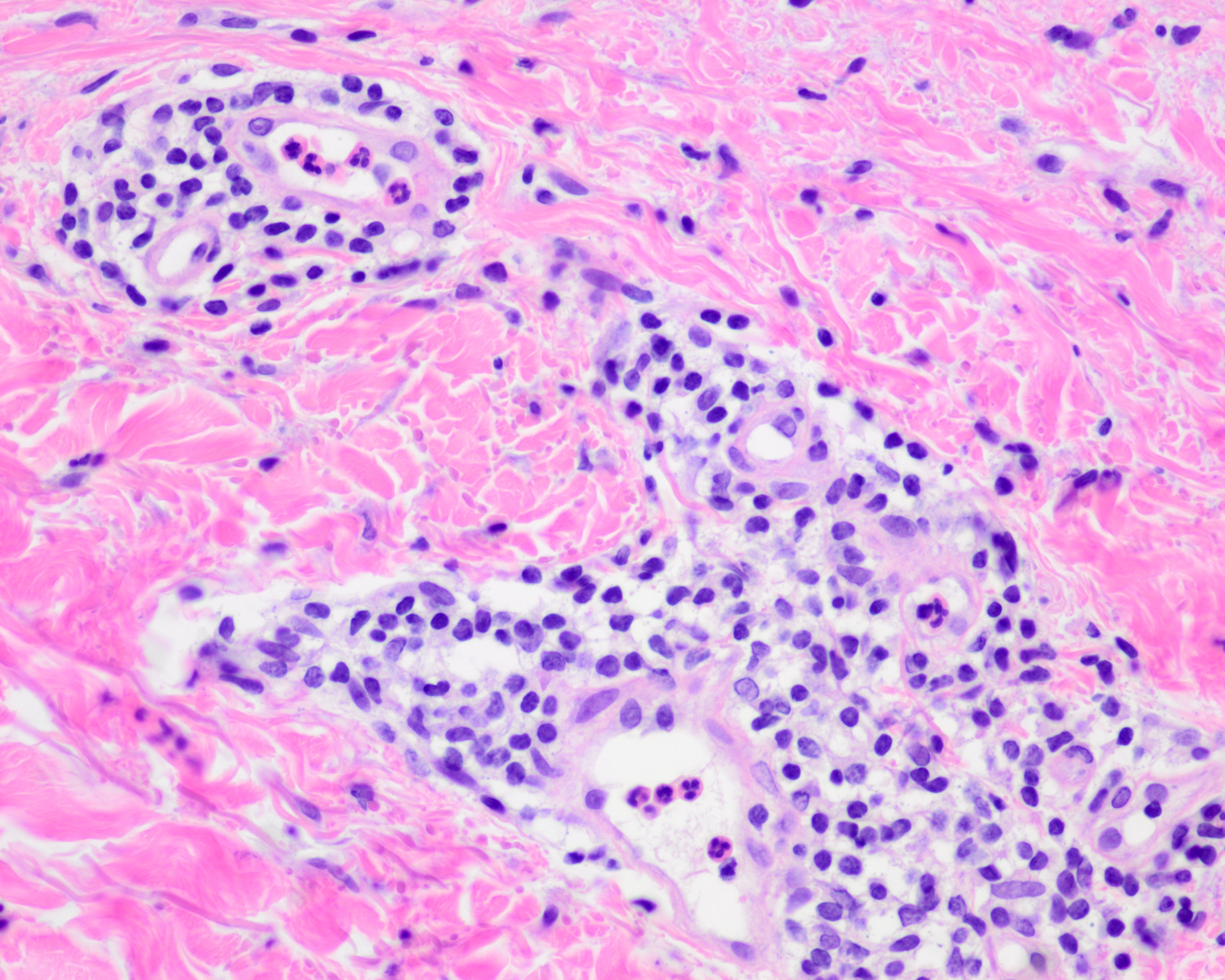
Microscopic (histologic) description
- Age of lesion and nature of evoking stimulus may both influence type and intensity of inflammatory response
- Changes most marked in upper dermis but involvement of the deep dermis may be present
- Mild dermal edema (separation of the collagen bundles)
- Dilatation of small blood vessels, lymphatics and often swelling of their endothelium
- Cellular infiltrate usually mild and perivascular; lymphocytes and few eosinophils in most cases
- Neutrophils are often noted in early lesions but relatively sparse; more prominent in physical urticarias
- Neutrophils and sometimes eosinophils in the lumen of small vessels are seen in early urticarias in the upper dermis
- No fibrinoid changes, hemorrhage or leukocytoclasis
- In neutrophilic urticaria, there is more diffuse interstitial dermal neutrophilia, usually mild in intensity
- In papular urticaria, inflammatory cell infiltrate is usually heavier than in other chronic urticarias
- Reference: Patterson: Weedon's Skin Pathology, 4th Edition, 2015
Microscopic (histologic) images
Contributed by Patricia Muñoz-Hernández, M.D.
Virtual slides
Sample pathology report
- Left arm, biopsy:
- Superficial perivascular dermatitis with dermal edema and eosinophils; the histologic features are consistent with urticaria (see comment)
- Comment: The upper dermis shows interstitial edema with mild perivascular infiltrate of lymphocytes and relatively numerous eosinophils. Neutrophils are seen within vessels lumens without vasculitis. Clinical correlation is recommended.
Differential diagnosis
- Histology of urticaria is nonspecific, clinicopathological correlation is needed
- Polymorphous light eruption:
- More edema in upper or papillary dermis
- Drug induced exanthem:
- Mild spongiosis and discrete basal layer vacuolization
- Arthropod reaction:
- Epidermal changes, wedge shaped superficial and deep mixed inflammatory infiltrate
- Viral exanthem:
- Can have very similar appearance to urticaria; clinical correlation is required
- Urticarial vasculitis:
- Endothelial swelling, leukocytoclasis, extravasated erythrocytes and fibrin deposition
- The main differential feature in urticarial vasculitis is the presence of fibrinoid necrosis of the dermal capillaries in contrast to the absence of vascular wall damage in urticaria
Additional references
Board review style question #1
Urticaria is shown in the image above. Which is true of this lesion?
- Individual lesions fade within 100 hours, although episodes may last days to months
- This disease is characterized by transient skin or mucosal swellings due to plasma leakage
- Vasculitis with fibrin deposition is characteristically seen
- Typical lesions known as wheals are not usually pruritic
- The biopsy commonly shows epidermal changes, such as parakeratosis, acanthosis, spongiosis and vacuolar basal degeneration
Board review style answer #1
B. This disease (urticaria) is characterized by transient skin or mucosal swellings due to plasma leakage. Due to a stimulus, there is mast cell degranulation with release of histamine and other proinflammatory mediators, which results in vasodilation and increased permeability of postcapillary venules to large plasma proteins, including albumin and inmmunoglobulins. Option A is incorrect since individual lesions fade within 24 hours, although episodes may last days to months. Option C is incorrect since there is no vasculitis in urticaria. No fibrinoid changes, hemorrhage or leukocytoclasis are seen.
Option D is incorrect because wheals are characteristically pruritic and pink or pale in the center, whereas angioedema is often painful, less well defined and shows no color change. Option E is incorrect since epidermal changes are not usually seen. In urticaria, typical changes include dermal edema and lymphocytes perivascular infiltrate with few eosinophils.
Comment Here
Reference: Urticaria (hives)
Comment Here
Reference: Urticaria (hives)
Board review style question #2
Which of the following is true about the pathology of urticaria?
- Neutrophils are never found on biopsies
- Perivascular infiltrate is due only to eosinophils
- When neutrophils are found, they are perivascular
- Neutrophils can be found interstitially
- Lymphocytes appear only rarely in biopsies of urticaria
Board review style answer #2
D. Neutrophils can be found interstitially. Option A is incorrect since lymphocytes, neutrophils and eosinophils can all appear on biopsies. Option B is incorrect since lymphocytes, neutrophils and eosinophils can all appear in the perivascular infiltration. Option C is incorrect because neutrophils can be perivascular or interstitial. Option E is incorrect since lymphocytes, neutrophils and eosinophils can all appear frequently.
Comment Here
Reference: Urticaria (hives)
Comment Here
Reference: Urticaria (hives)