Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Duran J, Plaza JA. Lichen simplex chronicus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorlichensimplexchronicus.html. Accessed April 19th, 2024.
Definition / general
- Chronic dermatitis characterized by localized areas of thickened, hyperkeratotic skin resulting from chronic rubbing or scratching
- Absence of underlying dermatologic condition
- These changes, known in conjunction as lichenification, are occasionally superimposed on other dermatoses, inflammatory and neoplastic
Essential features
- Circumscribed (Semin Diagn Pathol 2017;34:220)
- Itch / scratch cycle perpetuates the condition
- Main areas affected are readily accessible to scratching (Semin Diagn Pathol 2017;34:220)
- Clinical: lichenification, excoriations, erythema and hyperpigmentation (Semin Diagn Pathol 2017;34:220, Dermatol Ther 2004;17:8)
- Histopathological: pronounced acanthosis, orthokeratosis, hypergranulosis, papillary dermal fibrosis and perivascular chronic inflammation (Semin Diagn Pathol 2017;34:220, Dermatol Ther 2004;17:8)
Terminology
- Neurodermatitis circumscripta
- Neurodermatitis
ICD coding
Epidemiology
- F:M = 2:1 (Dermatol Ther 2008;21:42)
- Peak incidence: 35 - 50 years of age (Dermatol Ther 2008;21:42)
- Disproportionately affects black patients (Medicines (Basel) 2019;6:98)
- May be seen in children (Dermatol Ther 2008;21:42)
- Incidence and prevalence not well established (Medicines (Basel) 2019;6:98, J Midwifery Womens Health 2012;57:260)
Sites
- Scalp, neck, hands, extensor forearms, ankles, vulva, scrotum, mons pubis and perianal region (Medicines (Basel) 2019;6:98, Dermatol Ther 2008;21:42, J Midwifery Womens Health 2012;57:260)
Pathophysiology
- Uncertain precise pathophysiology (Medicines (Basel) 2019;6:98)
- Persistence and progression correlate with scratching and rubbing (persistent itch / scratch cycle) (Medicines (Basel) 2019;6:98, Dermatol Ther 2008;21:42)
Etiology
- Pruritus
- Underlying stimulus and most important symptom (Dermatol Ther 2008;21:42)
- Hypothesized relation to an increased sensitivity to local neurotransmitters and their neuromodulation, in response to primary stimulus (i.e. temperature, pressure, etc.) (Semin Diagn Pathol 2017;34:220)
- May be secondary to other dermatosis, medical conditions or psychological disorders (Dermatol Ther 2008;21:42)
- Associated with psychiatric disorders, including depression, anxiety, dissociation and obsessive compulsive disorder (Dermatol Ther 2020;33:e14389)
Clinical features
- Circumscribed
- Early lesions may appear erythematous
- Chronicity results in hyperkeratosis with thickened scaly plaques, excoriated papules, leukodermic (hypopigmented) center and increased skin markings (Dermatol Ther 2008;21:42)
- Longstanding lesions may also have depigmentation or hypopigmentation
Diagnosis
- Clinical diagnosis usually sufficient
- Biopsy if the diagnosis cannot be determined clinically or to exclude other dermatoses (J Midwifery Womens Health 2012;57:260, Dermatol Ther 2004;17:8)
Laboratory
- As pertinent, if an underlying medical condition is suspected as the etiology of pruritus
Prognostic factors
- Benign condition
- Challenging symptom control due to its multifactorial nature and unclear physiopathology (Medicines (Basel) 2019;6:98, Dermatol Ther 2004;17:8)
Case reports
- 58 year old woman with foreign body sensation and redness of the left eye (JAMA Ophthalmol 2013;131:816)
- 65 year old woman with severe generalized pruritus (J Med Case Rep 2021;15:80)
- 75 year old woman with scalp pruritus (An Bras Dermatol 2018;93:108)
Treatment
- Topical and intralesional corticosteroids (J Dermatolog Treat 2020 Mar 6 [Epub ahead of print])
- Topical immunomodulators (tacrolimus, pimecrolimus) (J Dermatolog Treat 2020 Mar 6 [Epub ahead of print])
- Topical antipruritics (doxepin, capsaicin, aspirin) (J Dermatolog Treat 2020 Mar 6 [Epub ahead of print])
- Antiepileptics, antihistamines and antidepressants (J Dermatolog Treat 2020 Mar 6 [Epub ahead of print])
- Emerging therapies (phototherapy, transcutaneous electrical nerve stimulation, focused ultrasound) (J Dermatolog Treat 2020 Mar 6 [Epub ahead of print], J Am Acad Dermatol 2018;79:e105)
Clinical images
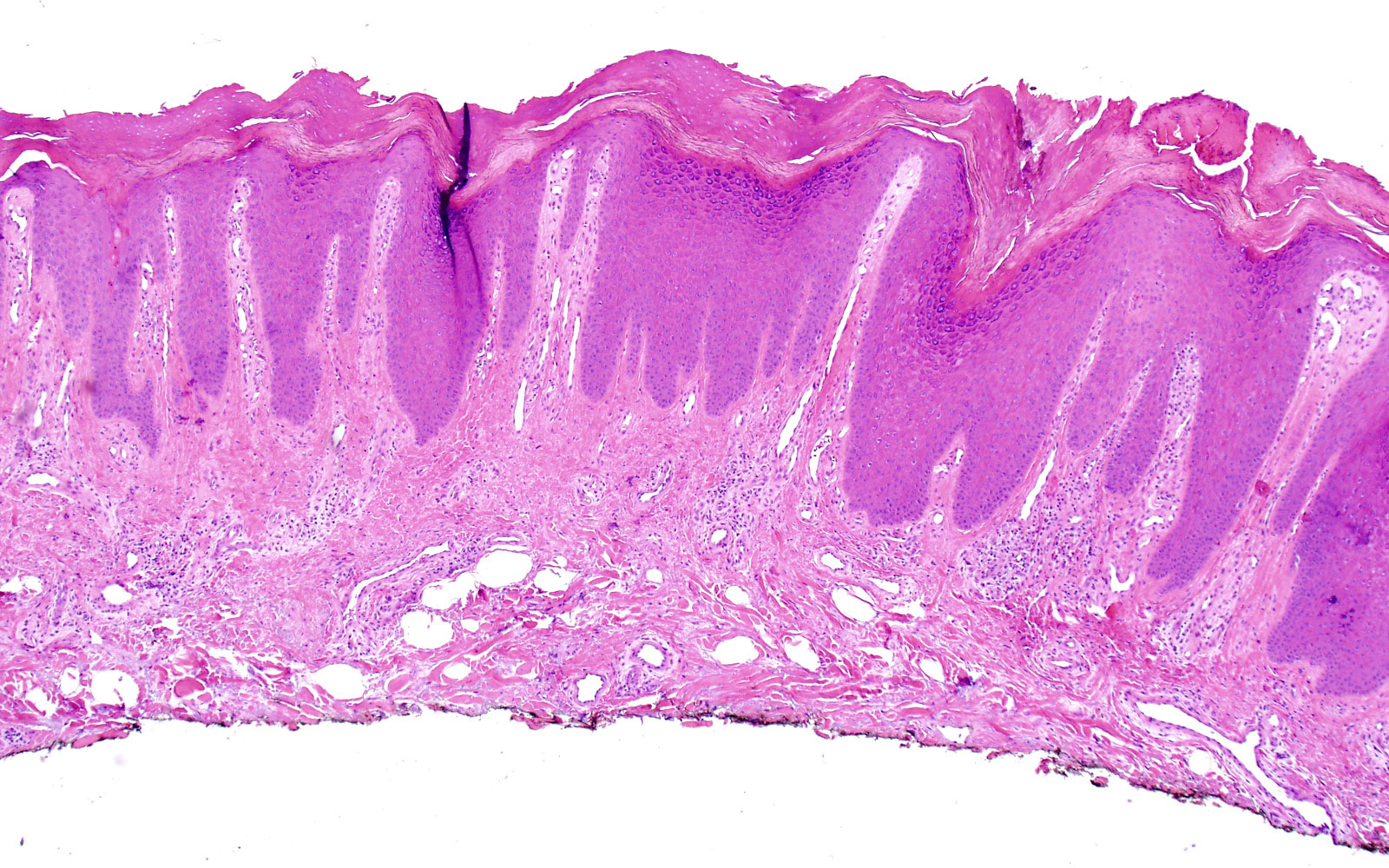
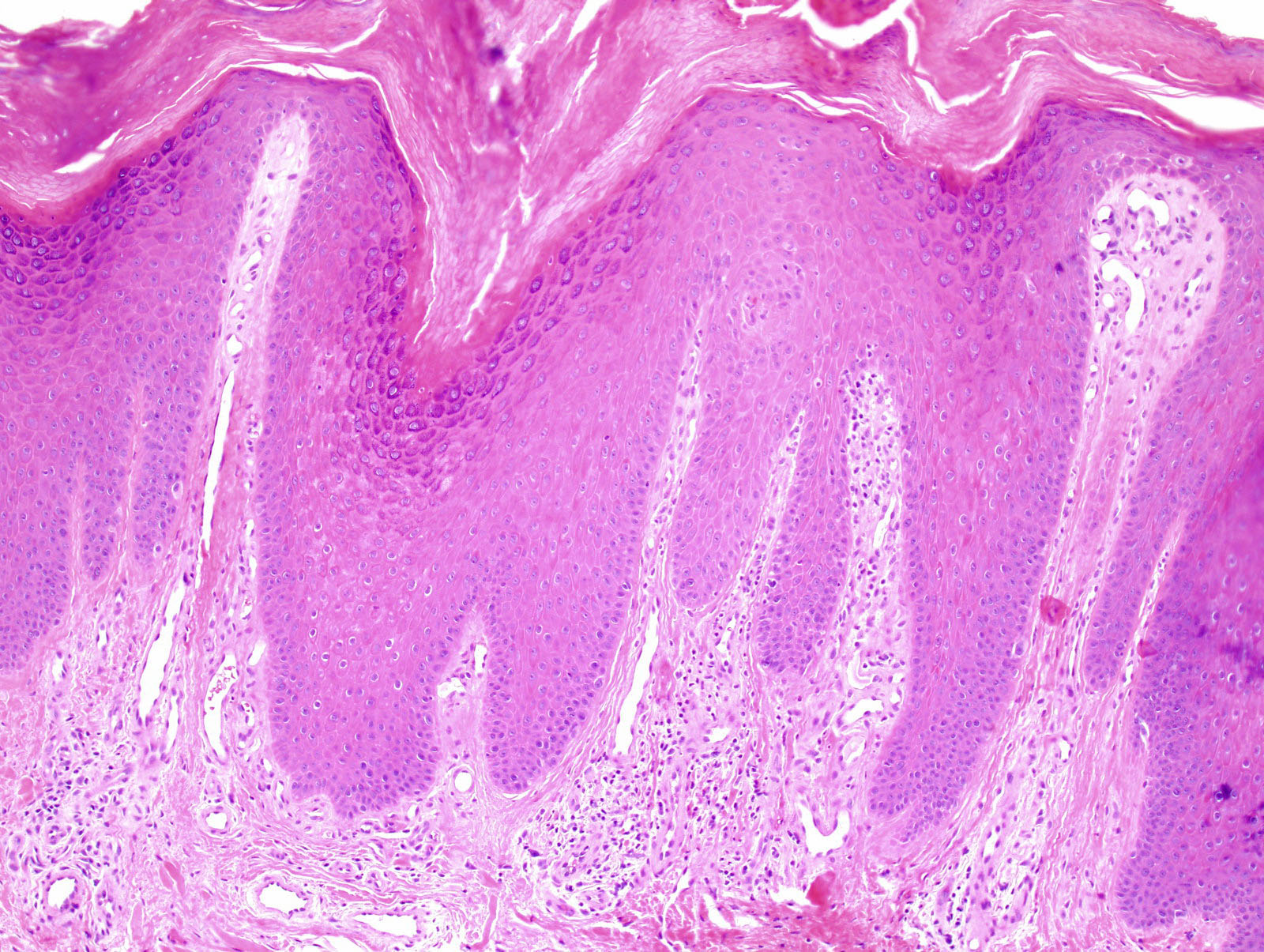
Microscopic (histologic) description
- Early lesions may demonstrate spongiosis (Semin Diagn Pathol 2017;34:220)
- Evolves to demonstrate (Semin Diagn Pathol 2017;34:220)
- Compact orthokeratosis with focal parakeratosis
- Hypergranulosis
- Occasional pseudoepitheliomatous hyperplasia
- Prominent irregular acanthosis with curvilinear, blunt rete ridges
- Papillary dermal fibrosis, with vertically oriented collagen bundles
- Superficial chronic perivascular inflammatory infiltrate
- Rare mast cells and eosinophils
- As lichenification may be superimposed on other dermatoses, careful search for other disorders is advised
Microscopic (histologic) images
Sample pathology report
- Skin, left lower leg, shave biopsy:
- Lichen simplex chronicus (see comment)
- Comment: Sections demonstrate hyperkeratosis, focal parakeratosis, a thickened granular layer and marked acanthosis. Characteristic vertically oriented, thickened collagen bundles are seen in the superficial dermis. The underlying dermis shows mild to moderate chronic inflammation. These findings, in the right clinical setting, are consistent with the above diagnosis.
- Note: Avoid descriptive diagnosis that will not help the clinician to properly treat their patients. Breaking the itch / scratch cycle is essential to treat this entity (Mod Pathol 2020;33:107).
Differential diagnosis
- Psoriasis (Semin Diagn Pathol 2017;34:220, Dermatol Ther 2004;17:8):
- Regular acanthosis with club shaped rete ridges
- Confluent parakeratosis
- Hypogranulosis
- Intracorneal neutrophils
- Acanthosis
- Vascular congestion of papillary dermis
- Other chronic spongiotic dermatitides:
- Spongiosis
- Acanthosis
- Exocytosis
- Perivascular inflammatory infiltrate, predominantly lymphohistiocytic and occasional neutrophils and eosinophils (the latter may be numerous in allergic contact dermatitis)
- Their differentiation may not be possible if superimposed lichenification is present
- Prurigo nodularis
- Same findings as in lichen simplex chronicus but in nodular configuration rather than plaque-like
Additional references
Board review style question #1
A pathologist is reviewing a skin case. The clinical history field on the requisition indicates chronic pruritus. Hematoxylin and eosin stained sections of a punch skin biopsy submitted as lower leg lesion demonstrate the features shown in the photomicrograph. This entity most likely represents:
- Dermatophyte infection
- Lichen simplex chronicus
- Mycosis fungoides
- Psoriasis
Board review style answer #1
Board review style question #2
Which clinical scenario best fits a diagnosis of lichen simplex chronicus?
- 30 year old man with buttocks and scalp lesions (white / silver scaly, well demarcated plaques with underlying erythema)
- 45 year old woman with dorsal hand lesion (circumscribed, erythematous pruritic plaque with leukodermic center and increased skin markings)
- 50 year old woman with neck lesion (annular plaque of erythema, scale at advancing border)
- 60 year old man with numerous trunk lesions (initially pruritic patches with minimal scaling with evolution to erythematous plaques)
Board review style answer #2
B. 45 year old woman with dorsal hand lesion (circumscribed, erythematous pruritic plaque with leukodermic center and increased skin markings)
Comment Here
Reference: Lichen simplex chronicus
Comment Here
Reference: Lichen simplex chronicus