Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Immunofluorescence description | Immunofluorescence images | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Roy SF, McNiff JM. Lichen planus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorlichenplanus.html. Accessed April 1st, 2025.
Definition / general
- Clinical: the "6 Ps": purple, pruritic, planar (flat), polygonal papules and plaques
- Histologic: prototypic lichenoid infiltrate dermatitis
Essential features
- The "6 Ps": purple, pruritic, planar (flat), polygonal papules and plaques
- Sawtoothed rete ridges, band-like lymphohistiocytic infiltrate at the dermoepidermal junction
- Wedge shaped hypergranulosis
- Civatte bodies (dyskeratotic keratinocytes)
Epidemiology
- Equal gender predilection for cutaneous lichen planus
- Mild female predilection for oral lichen planus (N Engl J Med 2012;366:723)
- Fifth or sixth decade (majority)
- Rare in children
- More common in Asian and the Middle Eastern children than Western (Int J Womens Dermatol 2015;1:140)
- Associated with hepatitis C (may vary geographically) (Br J Dermatol 2004;151:1172)
Sites
- Skin (flexor, wrists and forearms, dorsal hands, shins, presacral area), mucous membranes (oral mucosa, genitalia), hair, nails, esophagus (rare)
- May be confined to oral mucosa (J Dent Res Dent Clin Dent Prospects 2010;4:3)
Pathophysiology
- Possible delayed hypersensitivity reaction (Int J Dermatol 2009;48:682)
- Cytotoxic CD8+ lymphocytes lead to apoptosis of basal keratinocytes
Etiology
- Currently unknown
Clinical features
- The "6 Ps": purple, pruritic, planar (flat), polygonal papules and plaques
- Features may overlap with drug induced lichenoid eruptions; clinical history is key
- Koebner phenomenon: new lesions at trauma sites (e.g. scratching)
- Wickham striae: fine white lines on surface of lesions corresponding to areas of hypergranulosis
- Clinical variants:
- Atrophic (large lichen palnus plaques with central atrophy)
- Hypertrophic (thick, hyperkeratotic plaques)
- Actinic (young adults or children with lichen planus on sun exposed areas occurring during the spring and summer seasons)
- Pigmentosus (lesions are brown, on the face and neck, more common in South Asia, frequent intertriginous involvement)
- Ulcerative (palmoplantar ulcerations)
- Bullous (rare, bullae within preexisting lichen planus lesions)
- Pemphigoides (rare, circulating IgG autoantibodies against BP antigen like bullous pemphigoides)
- References: N Engl J Med 2012;366:723, J Dtsch Dermatol Ges 2013;11:309, Int J Dermatol 2009;48:682
Diagnosis
- Made on H&E stain with light microscopy
Prognostic factors
- Disease course depends on variant:
- Conventional (exanthematous) lichen planus: self limiting, resolves 1 - 2 years
- Hypertrophic, oral, hair and nail lichen planus: longer, chronic course
- Hyperpigmentation after resolution is common (postinflammatory hyperpigmentation) (Acta Derm Venereol 1991;71:242)
- Oral lichen planus: associated with squamous cell carcinoma (oral lichen planus patients 4.8 times more likely to develop oral squamous cell carcinoma than patients without oral lichen planus) (Int J Dermatol 2019;58:296)
Case reports
- 8 year old boy with oral lichen planus (J Oral Maxillofac Pathol 2020;24:S128)
- 38 year old man with grey macular pigmentation on sun exposed head and neck areas (An Bras Dermatol 2019;94:378)
- 63 year old man with a pruritic eruption following a Blaschkoid distribution (JAAD Case Rep 2020;6:237)
- 66 year old man with a pruritic eruption following radiation therapy (Dermatol Online J 2019;25:13030)
Treatment
- Topical corticosteroids
- Intralesional corticosteroids
- Oral glucocorticoids
- Phototherapy
- Oral retinoids
- Oral antihistamines (for symptoms) (J Am Acad Dermatol 2019;81:1397)
Clinical images
Gross description
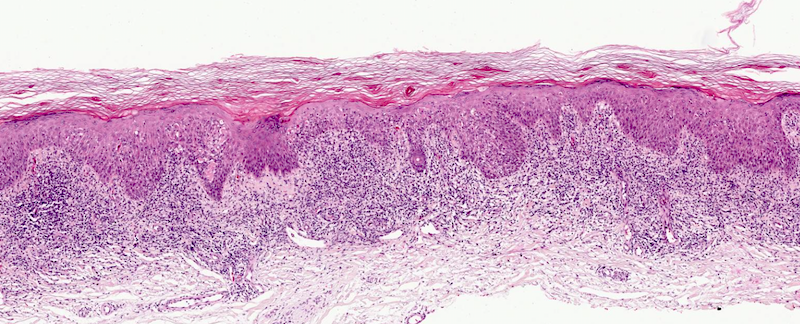
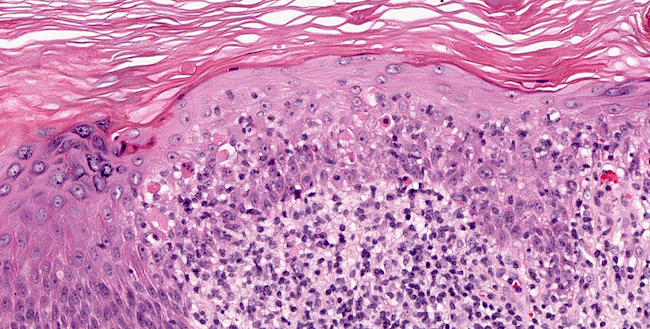
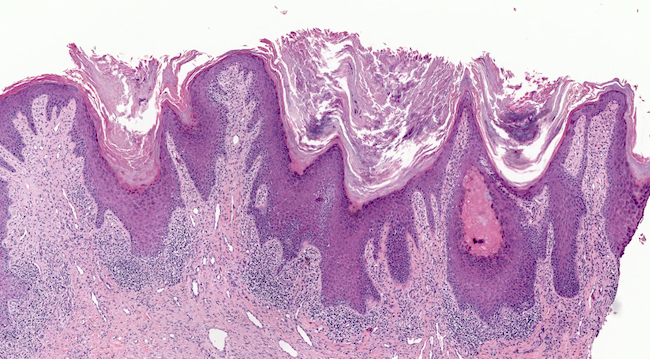
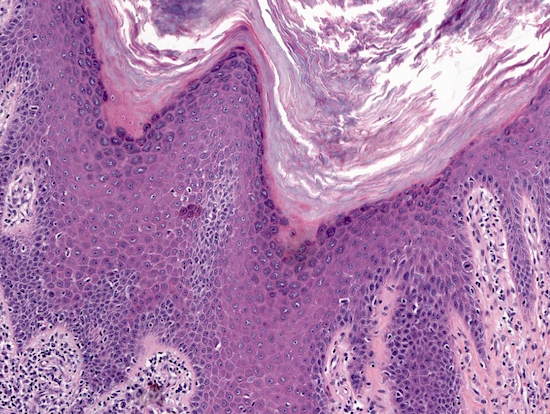
Microscopic (histologic) description
- Classic lichenoid dermatitis
- Hyperkeratosis, acanthosis, wedge shaped hypergranulosis, sawtoothing of rete ridges, band-like lymphohistiocytic infiltrate obscuring the dermoepidermal junction (Int J Dermatol 1982;21:203)
- Civatte / cytoid bodies (apoptotic basal keratinocytes, PAS+)
- Basal cell squamatization (flattening of cells)
- Parakeratosis: generally absent, think twice before diagnosing lichen planus
- Artifactual cleft formation between epidermis and papillary dermis (Max Joseph space) (ScienceDirect: A clinicopathological study of cutaneous lichen planus [Accessed 16 October 2020])
- Melanin pigment within macrophages of the dermis (pigment incontinence)
- Occasional subepidermal bullae
- Presence of eosinophils favors lichenoid drug reaction in conventional lichen planus (eosinophils can be seen in hypertrophic lichen planus) (J Cutan Pathol 2014;41:347)
- Atrophic lichen planus: no acanthosis, fewer Civatte bodies, more pigment incontinence and minimal inflammation (Int J Dermatol 2007;46:1237)
- Hypertrophic lichen planus: striking hyperkeratosis and acanthosis (pseudoepitheliomatous hyperplasia) (J Cutan Pathol 2014;41:347)
- Ulcerative (erosive) lichen planus: epidermal ulceration with lichen planus changes at the ulcer margins; frequent plasma cells (Clin Exp Dermatol 1993;18:169)
- Lichen planus pigmentosus: lymphocytic infiltrate tends to be deeper, with dermal melanin incontinence (Int J Dermatol 1992;31:90)
- Actinic lichen planus: dermal melanin incontinence and focal parakeratosis; milder lymphocytic infiltrate (Clin Exp Dermatol 1989;14:65)
- Bullous lichen planus: vesicle or bullae in conventional lichen planus (Clin Exp Dermatol 1989;14:150)
- Lichen planus pemphigoides: bulla with mild perivascular lymphocytic infiltrate, may show neutrophils (J Am Acad Dermatol 1983;8:331)
- Oral lichen planus: occasional parakeratosis, less acanthosis than in the skin, plasma cells in infiltrate
- Lichen planopilaris: scarring alopecia with lichenoid interface dermatitis of the hair infundibulum, with fibrous tracts and Civatte bodies
- Perifollicular lichenoid infiltrate around infundibulum (Arch Dermatol 1966;93:684)
Microscopic (histologic) images
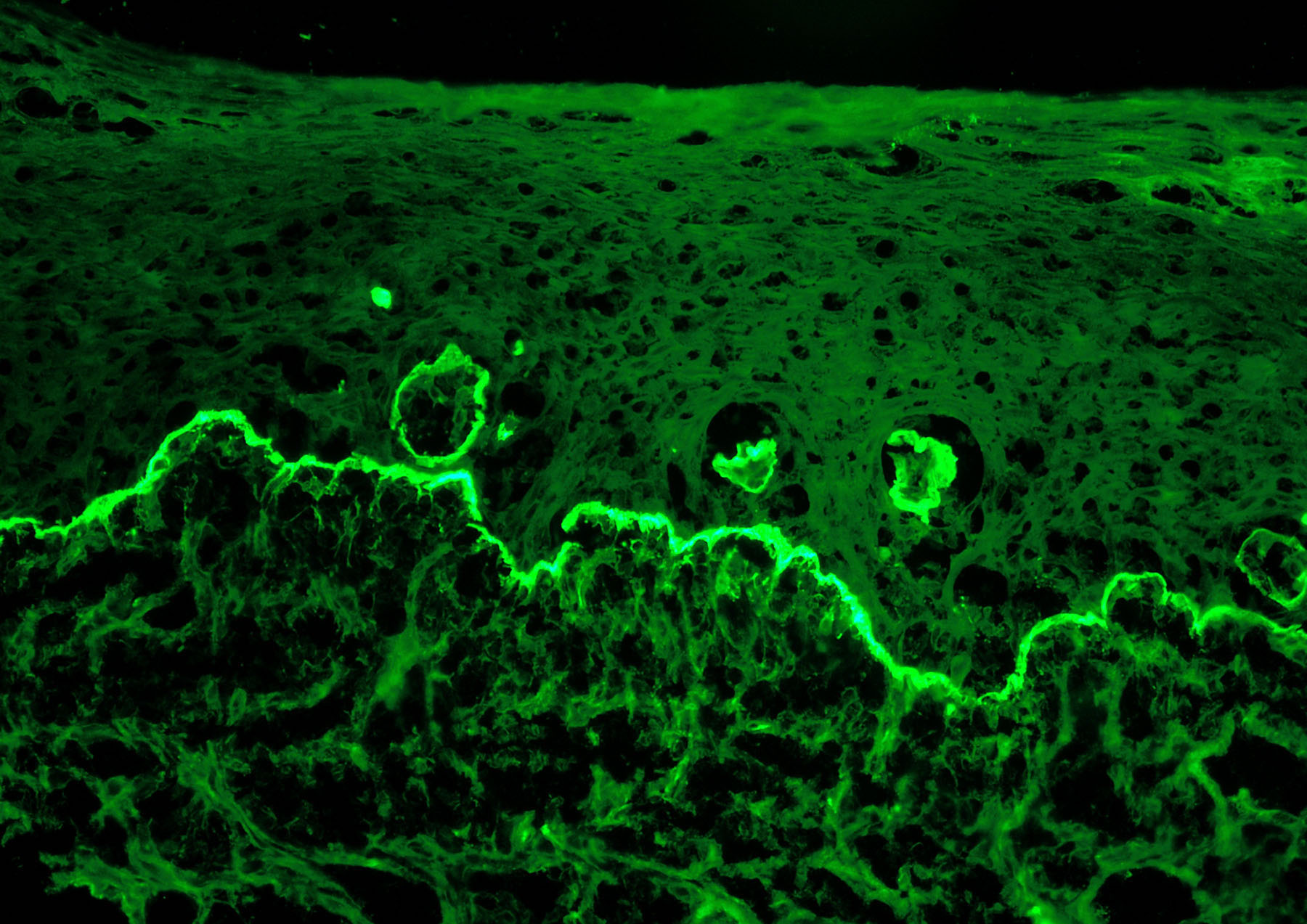
Immunofluorescence description
- Direct immunofluorescence:
- Fibrillar band of fibrin along dermoepidermal junction
- Civatte bodies highlighted with IgM, IgA and C3 (Int J Dermatol 2007;46:1237)
Immunofluorescence images
Positive stains
- PAS: Civatte bodies
Videos
Hypertrophic lichen planus
Sample pathology report
- Skin, left forearm, punch biopsy:
- Lichen planus (see comment)
- Comment: Sections show acanthosis, hypergranulosis and a lichenoid infiltrate with Civatte bodies. The histologic features are consistent with lichen planus. If this is a solitary lesion, a benign lichenoid keratosis is favored. Clinicopathologic correlation is recommended.
Differential diagnosis
- Lichenoid drug reaction:
- Lichenoid interface infiltrate with basal cell squamatization and Civatte bodies
- Distinguishing features from lichen planus: clinical history of potential culprit medication present and eosinophils generally, sometimes plasma cells and parakeratosis
- Benign lichenoid keratosis:
- Lichenoid interface infiltrate with basal cell squamatization and Civatte bodies
- Distinguishing features from lichen planus: diagnose only if solitary lesion rather than several papules and plaques
- Chronic discoid lupus:
- Vacuolar interface dermatitis with adnexal involvement, follicular plugging, hyperkeratosis, hypergranulosis and dermal mucin deposition
- Distinguishing features from lichen planus: can resemble hypertrophic variant of lichen planus, although presence of epidermal atrophy, follicular plugging and adnexal involvement are in favor of lupus
- Secondary syphilis:
- Several histopathological patterns possible but classically a psoriasiform dermatitis, demonstrating slender acanthosis of the rete pegs and a prominent plasma cell infiltrate in the dermis
- Distinguishing features from lichen planus: plasma cells and psoriasiform acanthosis
- In rare occurences, syphilis may show a lichenoid interface dermatitis, although spirochetes would be absent by Warthin-Starry stain or Treponema pallidum immunohistochemistry
- Squamous cell carcinoma (keratoacanthoma type):
- Crateriform well differentiated epithelial proliferation with central keratinization, enlarged keratinocyte cells with ample eosinophilic cytoplasm, dyskeratosis and mitoses
- Distinguishing features from lichen planus: absent wedge shaped hypergranulosis, present cytologic atypia, marked solar elastosis, lymphovascular or perineural invasion, perforating elastic fibers upon elastic staining and absence of eosinophils
- P53 overexpression in keratoacanthoma or squamous cell carcinoma (JAAD Case Rep 2017;3:151)
Additional references
Board review style question #1
- Which of the following is true about cutaneous lichen planus?
- Civatte bodies are PAS negative
- Eosinophils are common
- Dyskeratotic keratinocytes are frequently seen at the basal layer
- Mucosal involvement is seldom seen
Board review style answer #1
C. Dyskeratotic keratinocytes are frequently seen at the basal layer. Dyskeratotic keratinocytes (so called Civatte bodies) are frequently seen at the basal layer. Civatte bodies are PAS positive. Eosinophils are uncommon in conventional cutaneous lichen planus. Lichen planus may occur on mucosal surfaces such as the oral mucosa or genitalia.
Comment Here
Reference: Lichen planus
Comment Here
Reference: Lichen planus
Board review style question #2
Board review style answer #2
B. Eosinophils. Classic lichen planus and lichenoid drug eruption both share similar histopathological features (civatte bodies, wedge shaped hypergranulosis and hyperkeratosis). However, eosinophils favor a lichenoid drug eruption.
Comment Here
Reference: Lichen planus
Comment Here
Reference: Lichen planus