Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Aghighi M, Turner N, Motaparthi K. Reactive granulomatous dermatitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorinterstitialgranulomatous.html. Accessed April 18th, 2024.
Definition / general
- Dermal reaction pattern associated with autoimmune processes more often than infection or malignancy
- Spectrum of clinicopathologic features that vary with lesion age
- Comprises lesions consistent with palisaded neutrophilic granulomatous dermatitis and interstitial granulomatous dermatitis
Essential features
- Dermal reaction pattern associated with a systemic process, most commonly an autoimmune disease
- Variable clinical presentations including crusted pink-brown papules and plaques on extensor extremities, umbilicated papules on acral site, annular plaques on trunk and indurated linear cords on flanks
- Variable pathologic features including degenerated collagen surrounded by palisades of histiocytes, neutrophils and eosinophils, necrobiotic rosettes and leukocytoclastic vasculitis
- Commonly resolves with management of associated systemic disease
Terminology
- Interstitial granulomatous dermatitis, palisaded neutrophilic granulomatous dermatitis, Winkelmann granuloma, superficial ulcerating rheumatoid necrobiosis
ICD coding
- ICD-10: L92.9 - granulomatous disorder of the skin and subcutaneous tissue, unspecified
Epidemiology
- F > M; adults > children
- Associated with autoimmune disorders > malignancies or infections (Hum Pathol 2014;45:598, JAAD Case Rep 2017;3:425)
- Palisaded neutrophilic granulomatous dermatitis pattern is most commonly associated with rheumatoid arthritis, systemic lupus erythematosus, granulomatosis with polyangiitis and eosinophilic granulomatosis with polyangiitis
- Interstitial granulomatous dermatitis pattern is most commonly associated with rheumatoid arthritis (RA), seronegative inflammatory arthritis and autoimmune thyroiditis (Arch Dermatol 1994;130:1278)
- Less common associations include malignant processes (e.g., myelodysplastic syndrome and myeloid leukemia), infections (e.g., human immunodeficiency virus [HIV], Epstein-Barr virus [EBV], parvovirus B19 and Streptococcus), autoimmune diseases (including systemic sclerosis and inflammatory bowel disease) and metabolic diseases (including diabetes) (Dermatol Clin 2015;33:373, Clin Case Rep 2019;7:695)
Sites
- Interstitial granulomatous dermatitis: lateral upper trunk, flanks, buttocks and proximal limbs
- Palisaded neutrophilic granulomatous dermatitis: extensor surfaces of extremities
Pathophysiology
- Poorly understood but thought to be caused by immune complex deposition in small blood vessels → vasculitis, local ischemia and collagen degeneration → lymphohistiocytic response (Am J Clin Dermatol 2010;11:171)
Clinical features
- Palisaded neutrophilic granulomatous dermatitis: red crusted or umbilicated papules, plaques and nodules symmetrically distributed and typically on extensor surfaces
- Interstitial granulomatous dermatitis: firm linear cords or annular erythematous plaques on lateral upper trunk, buttocks and proximal limbs
- Usually asymptomatic but may be pruritic or tender
- Significant overlap between palisaded neutrophilic granulomatous dermatitis and interstitial granulomatous dermatitis; lesions consistent with both entities may present in the same patient
- Reference: Dermatol Clin 2015;33:373
Diagnosis
- Clinical features including history of systemic disease
- Punch biopsy
- Reference: Dermatol Clin 2015;33:373
Prognostic factors
- Self resolving (up to 80%) more often than a chronic course (J Eur Acad Dermatol Venereol 2021;35:988)
- Related to activity of underlying systemic process
Case reports
- 47 year old woman with palisaded neutrophilic granulomatous dermatitis and Hodgkin lymphoma (Am J Dermatopathol 2019;41:835)
- 70 year old woman with reactive granulomatous dermatitis and rheumatoid arthritis (JAAD Case Rep 2016;2:67)
- 72 year old woman with reactive granulomatous dermatitis and myelodysplastic syndrome (Ann Hematol 2017;96:1037)
- 3 cases of generalized palisaded neutrophilic granulomatous dermatitis associated with chronic myelomonocytic leukemia (Hum Pathol 2017;64:198)
- 52 patients with reactive granulomatous dermatitis (J Eur Acad Dermatol Venereol 2021;35:988)
Treatment
- Management is focused on treatment of the underlying, triggering disorder
- No standardized lesion directed therapy
- Reports of improvement with topical corticosteroids, topical calcineurin inhibitors, systemic corticosteroids, tetracyclines, hydroxychloroquine, cyclosporin, etanercept and phototherapy (J Eur Acad Dermatol Venereol 2021;35:988)
Clinical images
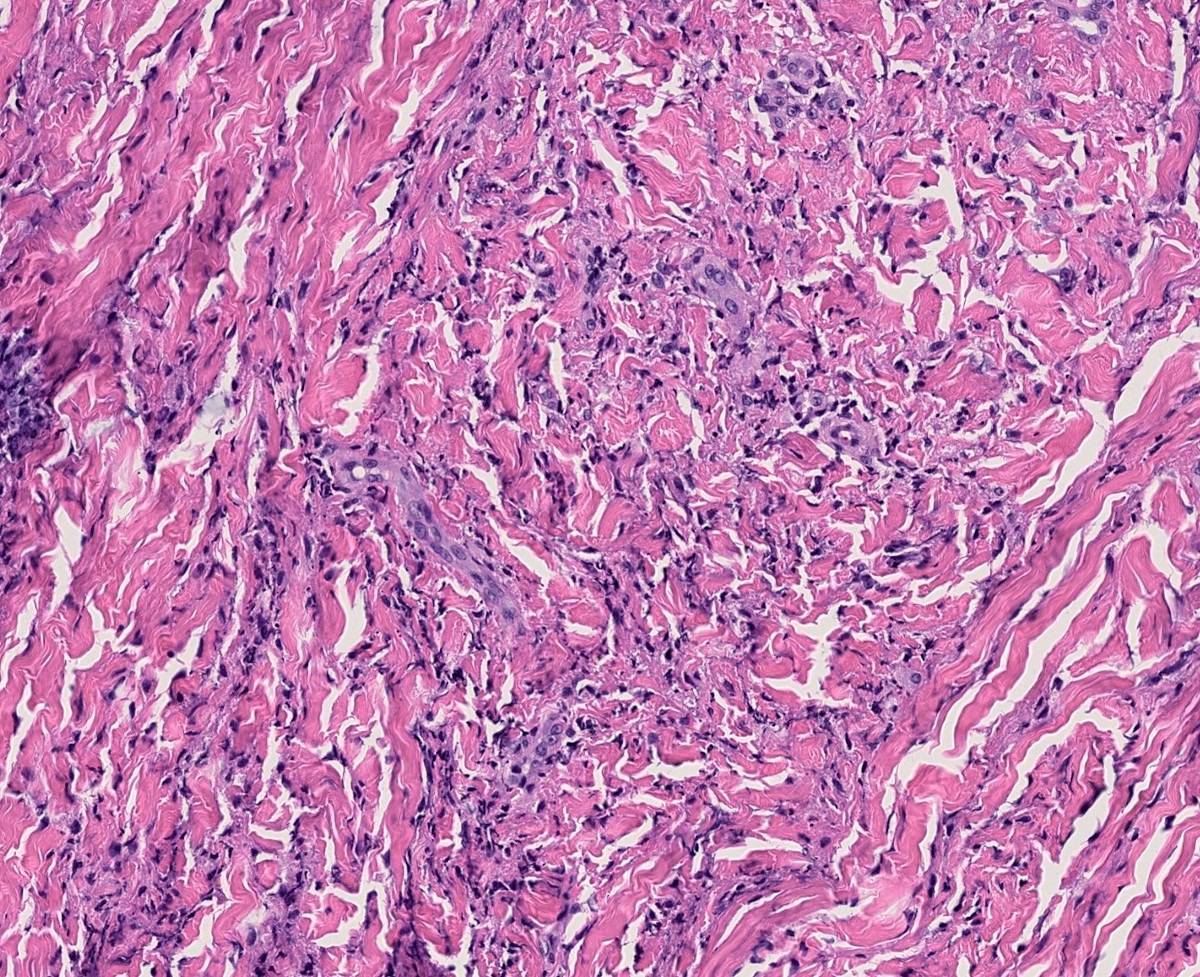
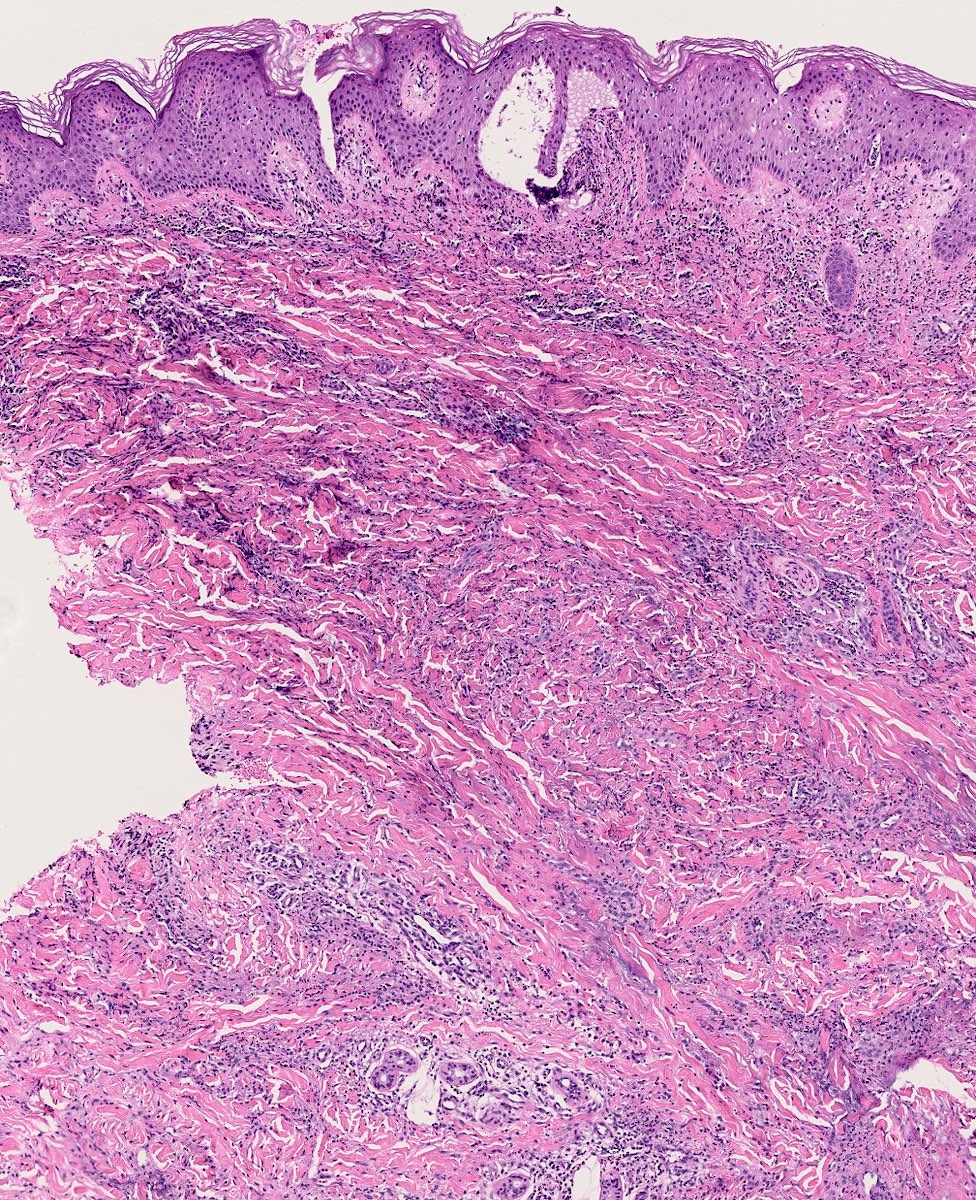
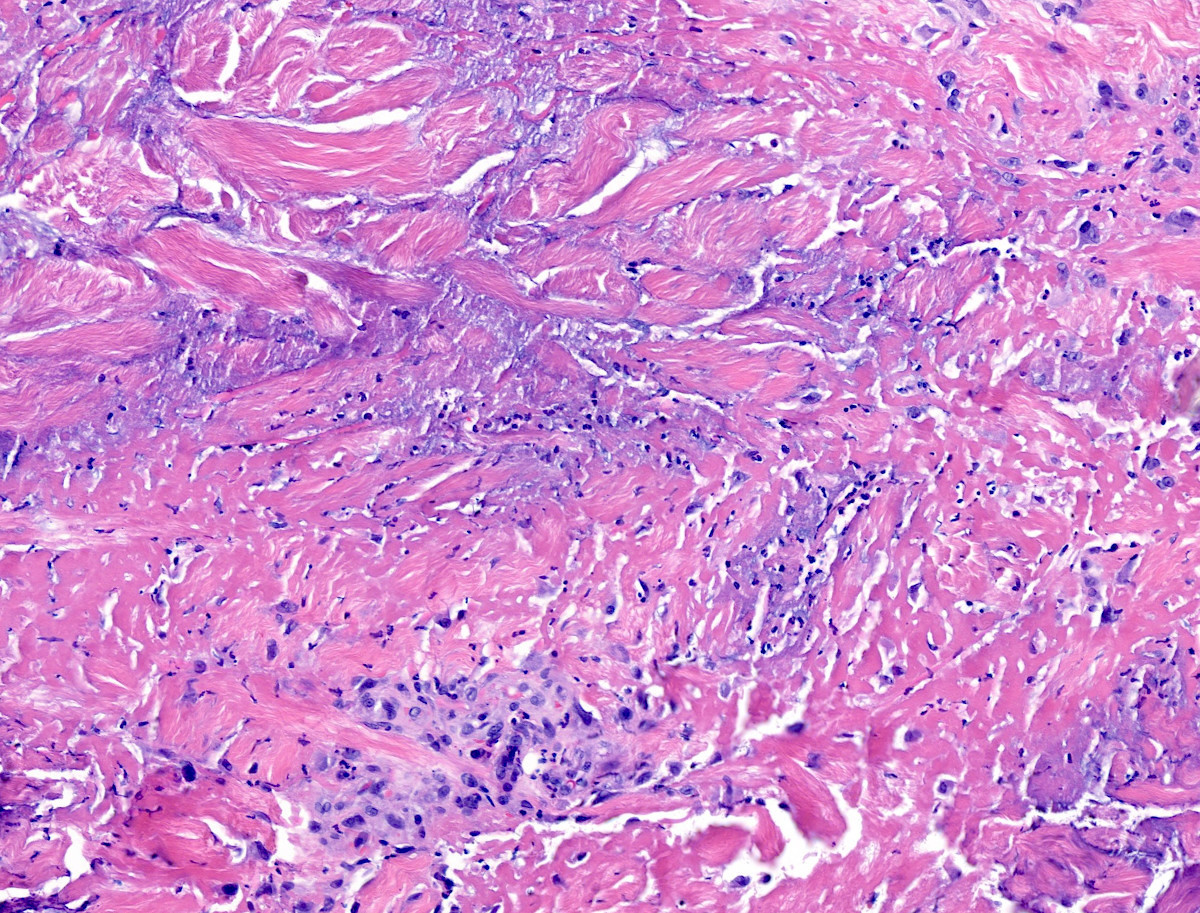
Microscopic (histologic) description
- Inflammatory infiltrate is variable among lesions and as the lesions age (J Eur Acad Dermatol Venereol 2021;35:988, JAAD Case Rep 2017;3:425, Am J Dermatopathol 2015;37:614, Lupus 2016;25:209)
- May be consistent with classical palisaded neutrophilic granulomatous dermatitis or interstitial granulomatous dermatitis (see below) or may be neutrophil predominant, eosinophil predominant or histiocyte predominant
- Interstitial granulomatous dermatitis: small rosettes of necrobiotic collagen surrounded by histiocytes and lymphocytes (floating sign)
- Absent leukocytoclastic vasculitis and minimal or absent mucin deposition
- Scarce neutrophils and eosinophils
- Palisaded neutrophilic granulomatous dermatitis: large foci of necrobiotic collagen surrounded by palisades of histiocytes, lymphocytes and prominent neutrophils
- Leukocytoclastic vasculitis may be present in early lesions
- Mucin deposition is minimal or absent
Microscopic (histologic) images
Sample pathology report
- Upper trunk, punch biopsy:
- Reactive granulomatous dermatitis, eosinophil rich (see comment)
- Comment: There are palisades of histiocytes and eosinophils surrounding degenerated collagen in the superficial to mid-dermis. Special stains for bacteria, fungi and mycobacteria are negative. No vacuolar interface dermatitis is present to suggest interstitial granulomatous drug reaction and no mucin deposition is seen to suggest granuloma annulare.
Differential diagnosis
- Interstitial granulomatous drug reaction:
- Firm papules, plaques and nodules that arise in response to exposure to medications, including antihypertensives, statins and tumor necrosis factor alpha inhibitors
- Presence of vacuolar interface dermatitis helps to differentiate from reactive granulomatous dermatitis
- Granuloma annulare:
- Firm, red-brown smooth or umbilicated papules, patches and subcutaneous nodules that arise most commonly on the extremities but may also be generalized
- Perforating variant may resemble umbilicated lesions of palisaded neutrophilic granulomatous dermatitis
- No clear association with autoimmune disease
- Abundant mucin and scarce neutrophils help to differentiate from reactive granulomatous dermatitis
- Infectious granuloma:
- Suppurative, sarcoidal or diffuse (interstitial) granulomas with positive infectious stains
- Rheumatoid nodules:
- Large nodules overlying extensor surfaces of joints in patients with rheumatoid arthritis
- Palisading granulomas with fibrinoid necrosis, prominent neutrophilic infiltrate and absent mucin deposition in deep dermis or subcutaneous fat
- Leukemia cutis:
- Reactive granulomatous dermatitis has been described in the setting of myelodysplastic syndrome and myeloid leukemia
- Distinguishing myeloid precursors from histiocytes enables differentiation
- Leukocytoclastic vasculitis:
- Purpuric macules and papules, petechiae, urticarial wheals and targetoid papules that favor dependent skin, are seen in small vessel vasculitis
- Small or medium sized vessels with fibrinoid necrosis, erythrocyte extravasation and neutrophilic perivascular infiltrate with karyorrhexis
- Lesions of palisaded neutrophilic granulomatous dermatitis may demonstrate leukocytoclastic vasculitis
- Reactive granulomatous dermatitis may occur in the setting of systemic vasculitides including granulomatosis with polyangiitis and eosinophilic granulomatosis with polyangiitis
- Acute febrile neutrophilic dermatosis (Sweet syndrome):
- Pink, tender edematous papules and plaques that favor the upper trunk; often with concomitant fever and variable systemic involvement
- Papillary dermal edema, dense neutrophilic infiltrate and karyorrhexis without vasculitis
Board review style question #1
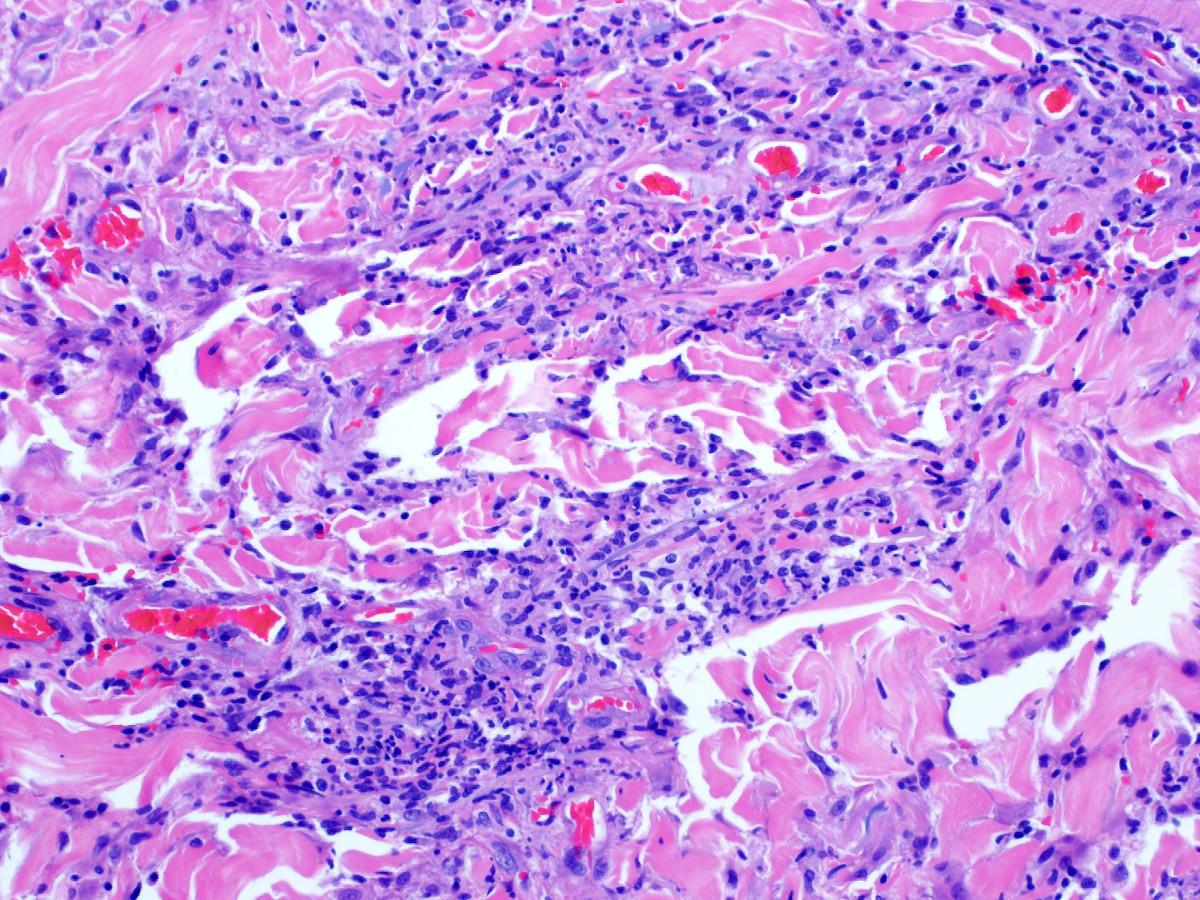
A 55 year old woman with systemic lupus erythematosus presents with a 2 month history of pink-brown, crusted papules on the extensor surfaces of her bilateral arms. Punch biopsy findings are presented in the image above. Grocott methenamine silver and Ziehl-Neelsen stains are negative. Which of the following is the best diagnosis?
- Acute febrile neutrophilic dermatosis (Sweet syndrome)
- Erythema elevatum diutinum
- Granuloma annulare
- Reactive granulomatous dermatitis
- Rheumatoid nodule
Board review style answer #1
D. Reactive granulomatous dermatitis. The image shows necrobiosis surrounded by palisades of histiocytes and neutrophils, consistent with a diagnosis of reactive granulomatous dermatitis (answer D). Biopsy of acute febrile neutrophilic dermatosis (answer A) would be expected to show superficial dermal edema and exuberant neutrophilic infiltrate with karyorrhexis but without true vasculitis; additionally, Sweet syndrome classically presents with an acute eruption of edematous papules and plaques that may ulcerate rather than a subacute to chronic eruption of crusted papules, as is described in this case. Biopsy of erythema elevatum diutinum (answer B) would be expected to show leukocytoclastic vasculitis with onion skin fibrosis. Histologic variants of granuloma annulare (answer C) include palisading granuloma annulare, in which histiocytes surround areas of necrobiosis and mucin deposition, as well as interstitial granuloma annulare, in which histiocytes and mucin intercalate between dermal collagen bundles; significant neutrophilic infiltrate is not characteristic. Rheumatoid nodules (choice E) are characterized by palisading granulomas with fibrinoid necrosis in the deep dermis and subcutis.
Comment Here
Reference: Reactive granulomatous dermatitis
Comment Here
Reference: Reactive granulomatous dermatitis
Board review style question #2
A 42 year old woman with poorly controlled rheumatoid arthritis presents with pink-brown, indurated, cord-like plaques on her trunk and flanks. A punch biopsy is performed and is shown above. Which of the following histopathologic features is characteristic of this entity?
- Degenerated collagen and fibrin surrounded by palisading histiocytes in the subcutaneous fat
- Degenerated collagen surrounded by palisades of histiocytes and neutrophils in the superficial to mid-dermis
- Foci of degenerated collagen with dense mucin deposition surrounded by palisades of histiocytes
- Naked granulomas with Langhans type giant cells and asteroid bodies
- Papillary dermal edema with dense neutrophilic infiltrate and karyorrhexis
Board review style answer #2
B. Degenerated collagen surrounded by palisades of histiocytes and neutrophils in the superficial to mid-dermis. The vignette describes the rope sign of interstitial granulomatous dermatitis (a subtype of reactive granulomatous dermatitis), in which indurated cord-like plaques develop on the trunk and flanks. The histologic image demonstrates degenerated collagen surrounded by palisades of histiocytes and neutrophils (answer B), further supporting the diagnosis of reactive granulomatous dermatitis. Answer A describes the histologic features of rheumatoid nodules. Answer C describes the histologic features of palisading granuloma annulare. Answer D describes the histologic features of sarcoidosis. Answer E describes the histology features of acute febrile neutrophils dermatosis (Sweet syndrome).
Comment Here
Reference: Reactive granulomatous dermatitis
Comment Here
Reference: Reactive granulomatous dermatitis