Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Fletcher CMM, Gupta R. Chondrodermatitis nodularis helicis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorchondrodermatitis.html. Accessed December 18th, 2024.
Definition / general
- Nonneoplastic lesion caused by inflammation and degenerative changes of the skin and the cartilage of the pinna (StatPearls: Chondrodermatitis Nodularis Helicis [Accessed 29 February 2024])
- Characterized by necrobiotic changes of the dermis and perichondrium of the pinna; frequently seen with accompanying ulceration of the skin (StatPearls: Chondrodermatitis Nodularis Helicis [Accessed 29 February 2024])
Essential features
- Painful, nonneoplastic nodule most commonly arising on the helix or antihelix of middle aged to elderly men (Cleve Clin J Med 2023;90:277, StatPearls: Chondrodermatitis Nodularis Helicis [Accessed 29 February 2024])
- Often caused by chronic pressure, solar damage or cold exposure leading to dermal inflammation, followed by impaired wound healing (Cleve Clin J Med 2023;90:277)
- Absence of squamous atypia or other features of malignancy
Terminology
- Chondrodermatitis nodularis chronica helicis
- No longer recommended: Winkler disease (J Clin Pathol 1957;10:46)
ICD coding
- ICD-11: AA12 - chondrodermatitis nodularis
Epidemiology
- Gender
- M > F (up to 4:1 in some studies)
- Mean age for men is 58 - 72 years old; older average age in women (J Dtsch Dermatol Ges 2011;9:287)
- Commonly on the helix or antihelix
- Risk factors
- Chronic pressure; e.g., sleeping in lateral decubitus position, hearing aids, face masks, headphone use (Dermatol Online J 2021;27:13030, J Eur Acad Dermatol Venereol 2021;35:e506, J Dtsch Dermatol Ges 2011;9:287)
- Cold exposure, solar damage
Sites
- Helix and antihelix; the helix is affected twice as often, typically in the superior aspect as the cartilage changes from vertical to horizontal (StatPearls: Chondrodermatitis Nodularis Helicis [Accessed 29 February 2024])
- However, any part of the pinna may be involved
- Case report of bilevel positive airway pressure (BiPAP) use causing a lesion on the nasal bridge suggests that any cartilage containing, pressure prone area may be susceptible (J Cutan Pathol 2020;47:1046)
Pathophysiology
- Anatomical factors contribute significantly to disease pathogenesis
- Pinna has relatively little subcutaneous tissue to offset pressure or insulate against cold; this is compounded by a paucity of small vessels in the dermis that supply epidermis, dermis, perichondrium and cartilage
- Trauma, pressure, cold weather or solar damage may initiate dermal inflammation, which progresses to necrosis secondary to impaired wound healing (StatPearls: Chondrodermatitis Nodularis Helicis [Accessed 29 February 2024], Medscape: Chondrodermatitis Nodularis Helicis [Accessed 29 February 2024])
Etiology
- Mechanism is not entirely clear but it is believed to be caused by chronic, excessive pressure; commonly attributed to sleeping in lateral decubitus position but also associated with hearing aids, headphones, etc. (Dermatol Online J 2021;27:13030, J Eur Acad Dermatol Venereol 2021;35:e506, J Dtsch Dermatol Ges 2011;9:287)
- Inciting injury may also be due to solar damage or cold exposure
- ~15% of patients with chondrodermatitis nodularis helicis may have an underlying autoimmune or connective tissue disease, including but not limited to polymyalgia rheumatica, psoriasis, rheumatoid arthritis, CREST (calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly and telangiectasia) syndrome, vitiligo, chronic dermatitis (Eur J Dermatol 2022;32:347)
Clinical features
- Intensely painful papule on the superior helix, measuring 4 - 5 mm on average (up to 20 mm maximum dimension) (J Dtsch Dermatol Ges 2011;9:287)
- Skin colored, smooth appearance with a central crater or crusted surface
- Chronic changes include prominent central ulceration and raised edges
- Some cases lack nodule formation and instead present as a keratotic plaque with surrounding erythema (StatPearls: Chondrodermatitis Nodularis Helicis [Accessed 29 February 2024])
- Clinically suspicious for malignancy, particularly squamous cell carcinoma and basal cell carcinoma
- Dermoscopic appearance: radially arranged, thick, white lines converging to a central rounded, yellow-brown clod (Arch Dermatol Res 2018;310:551)
- Underlying autoimmune and connective tissue diseases present in up to 15% of cases (Eur J Dermatol 2022;32:347)
Diagnosis
- Diagnosis can be made clinically, dermoscopically or with histological assessment
- WHO essential criteria: cup shaped crater with necrotic debris and fibrin extending to involve the superficial cartilage
Prognostic factors
- Recurrence rate: 13.3 - 21.4%
- Lowest rates seen with surgical therapy (Dermatol Surg 2016;42:1125)
- Mean time to recurrence: 9.3 months (Dermatol Surg 2016;42:1125)
Case reports
- 12 year old boy with tender, ulcerating nodule on antihelix after prolonged headphone use (Pediatr Dermatol 2019;36:388)
- 15 year old boy with painful nodule on right antihelix following prolonged headphone use (Dermatol Online J 2021;27:13030)
- 60 year old woman with a painful red papule on antihelix after prolonged cell phone use (BMJ Case Rep 2024;17:e258101)
- 61 year old man with painful red papule on crus of right ear after Mohs surgery and radiation therapy for adjacent squamous cell carcinoma (Cutis 2023;111:E5)
- 68 year old man with painful red papule on bridge of nose from BiPAP mask use (chondrodermatitis nodularis nasi) (J Cutan Pathol 2020;47:1046)
Treatment
- Randomized or blinded trials have not been performed but a systematic review identified surgery as the most effective treatment option (Dermatol Surg 2016;42:1125)
- Surgery
- Highest cure rate (82%) (Dermatol Surg 2016;42:1125)
- Variations in surgical approach: wedge excision, removal of prominent areas, punch excision, curettage followed by cauterization, cartilage removal alone
- Topical nitroglycerin therapy
- Curative in 51% cases (Dermatol Surg 2016;42:1125)
- Can be used in combination with pressure relieving devices with improved success
- Pressure relieving devices
- Curative in 37% (Dermatol Surg 2016;42:1125)
- Nonadherence is a large factor to low cure rate, particularly pressure relieving devices to wear during sleep (neck pain, discomfort)
- Other therapies
- CO2 laser, photodynamic therapy, platelet rich plasma, procaine injections, cryoablation, diltiazem cream, hyaluronic acid injection (Dermatol Surg 2016;42:1125, StatPearls: Chondrodermatitis Nodularis Helicis [Accessed 29 February 2024])
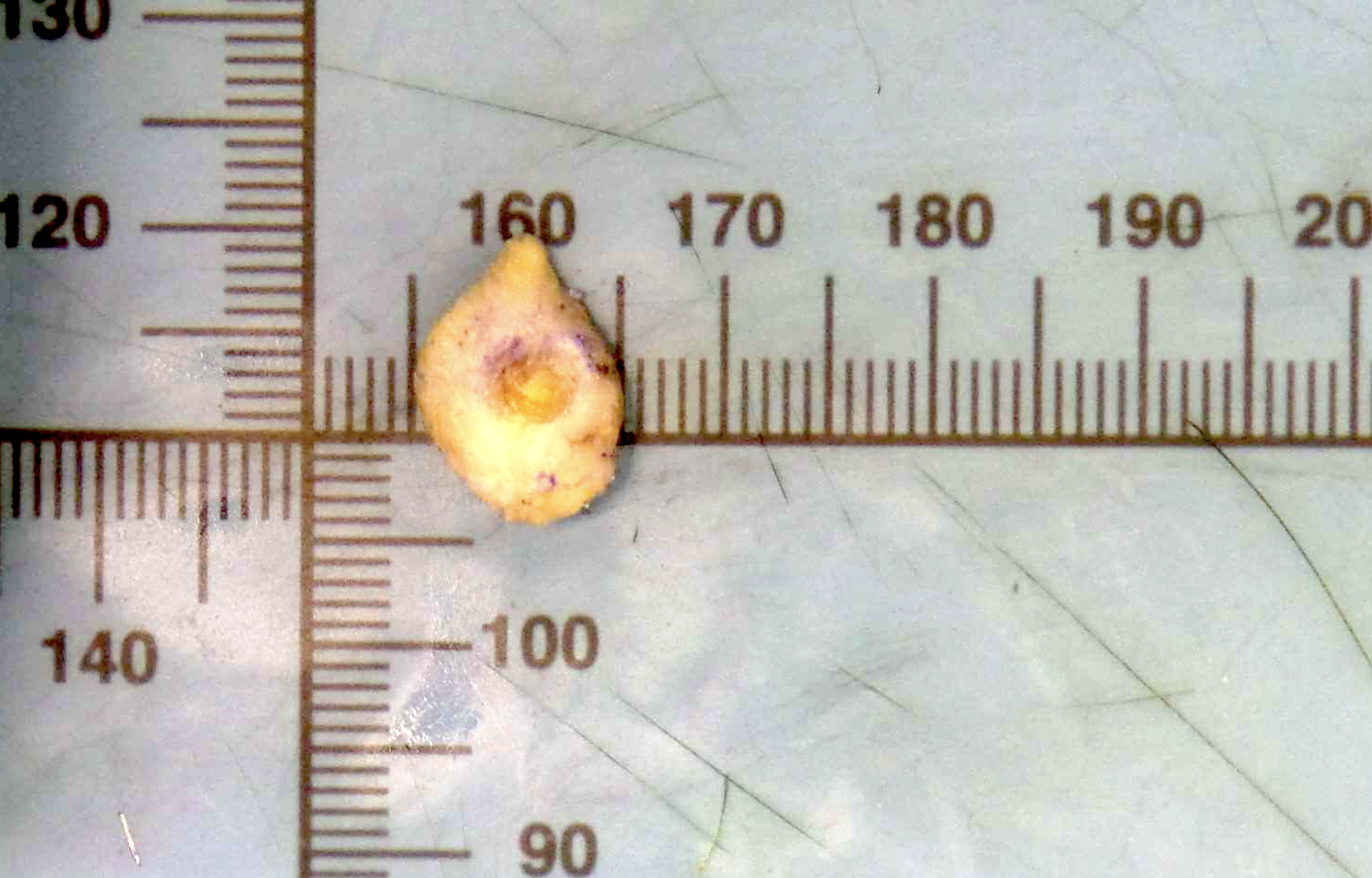
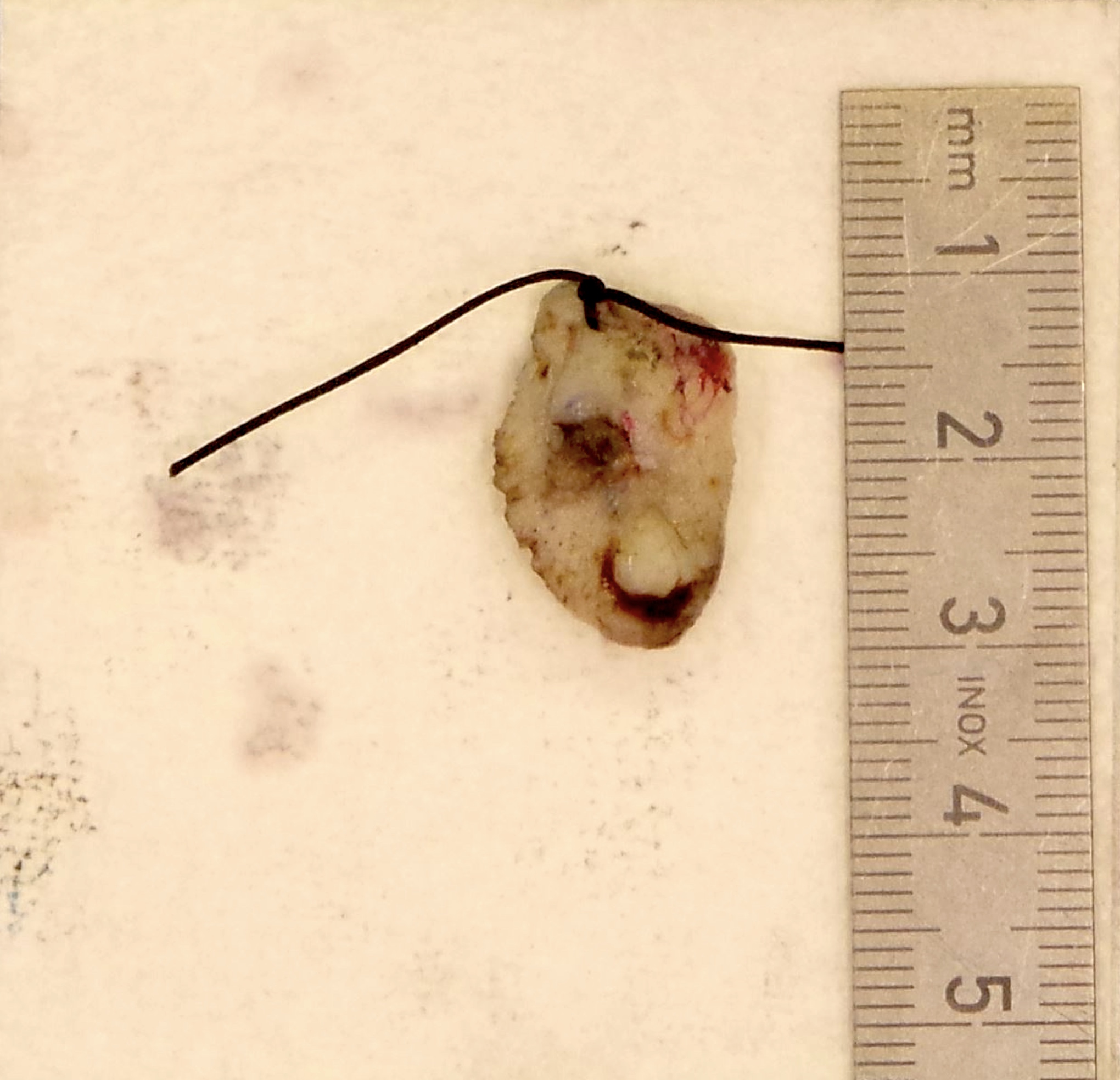
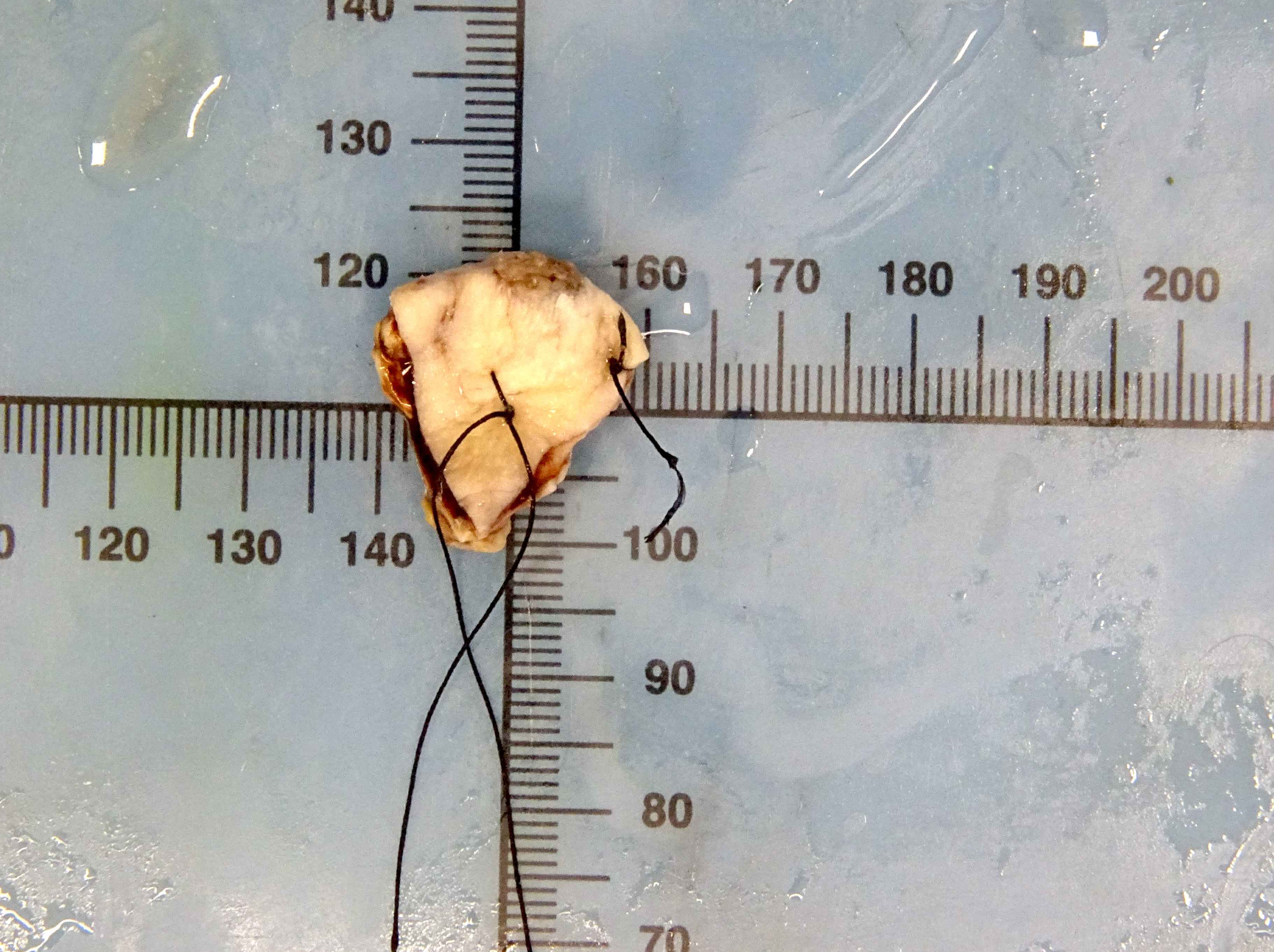
Gross description
- Bears central ulceration with crusting, plus surrounding erythema
Gross images
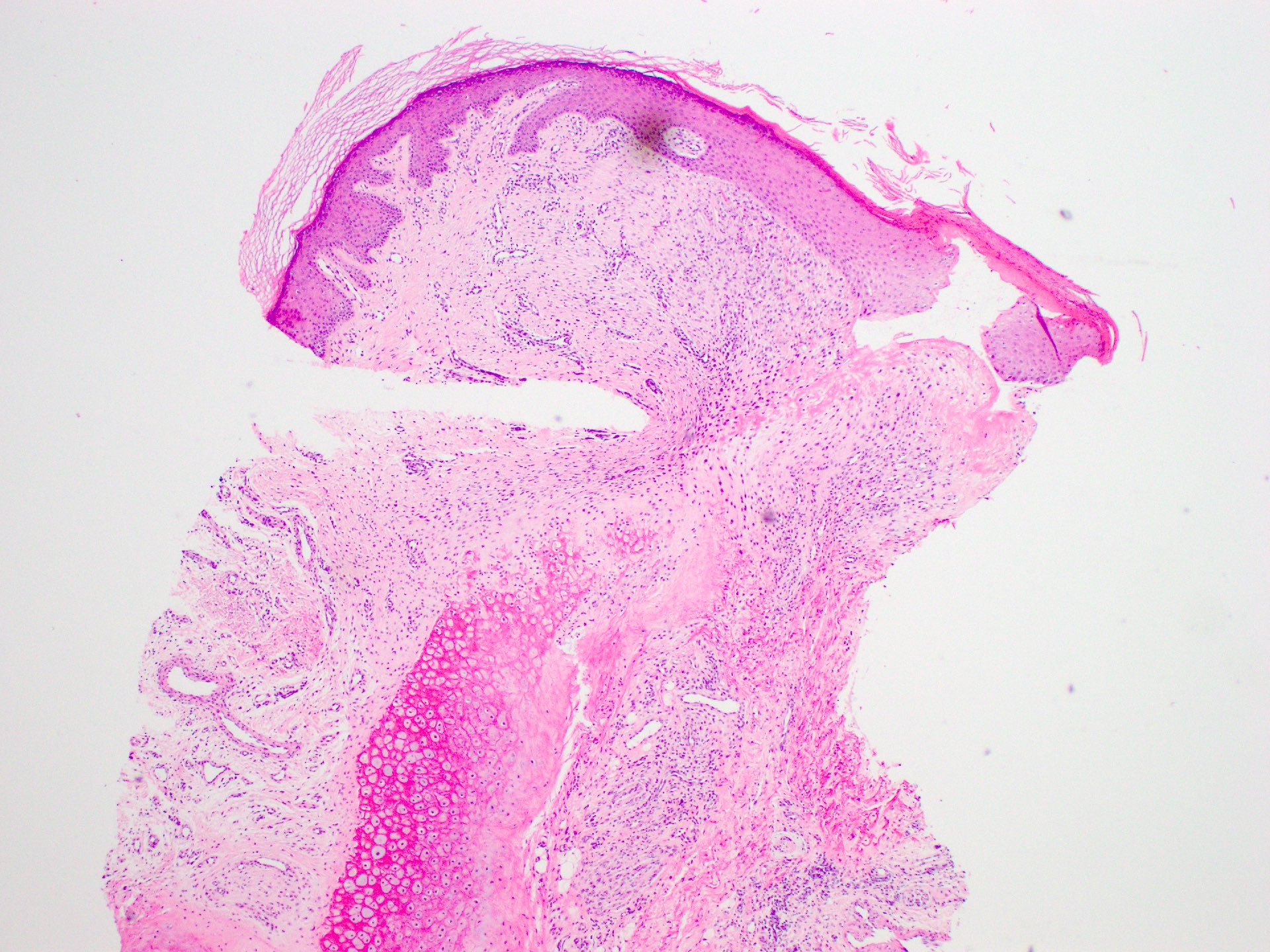
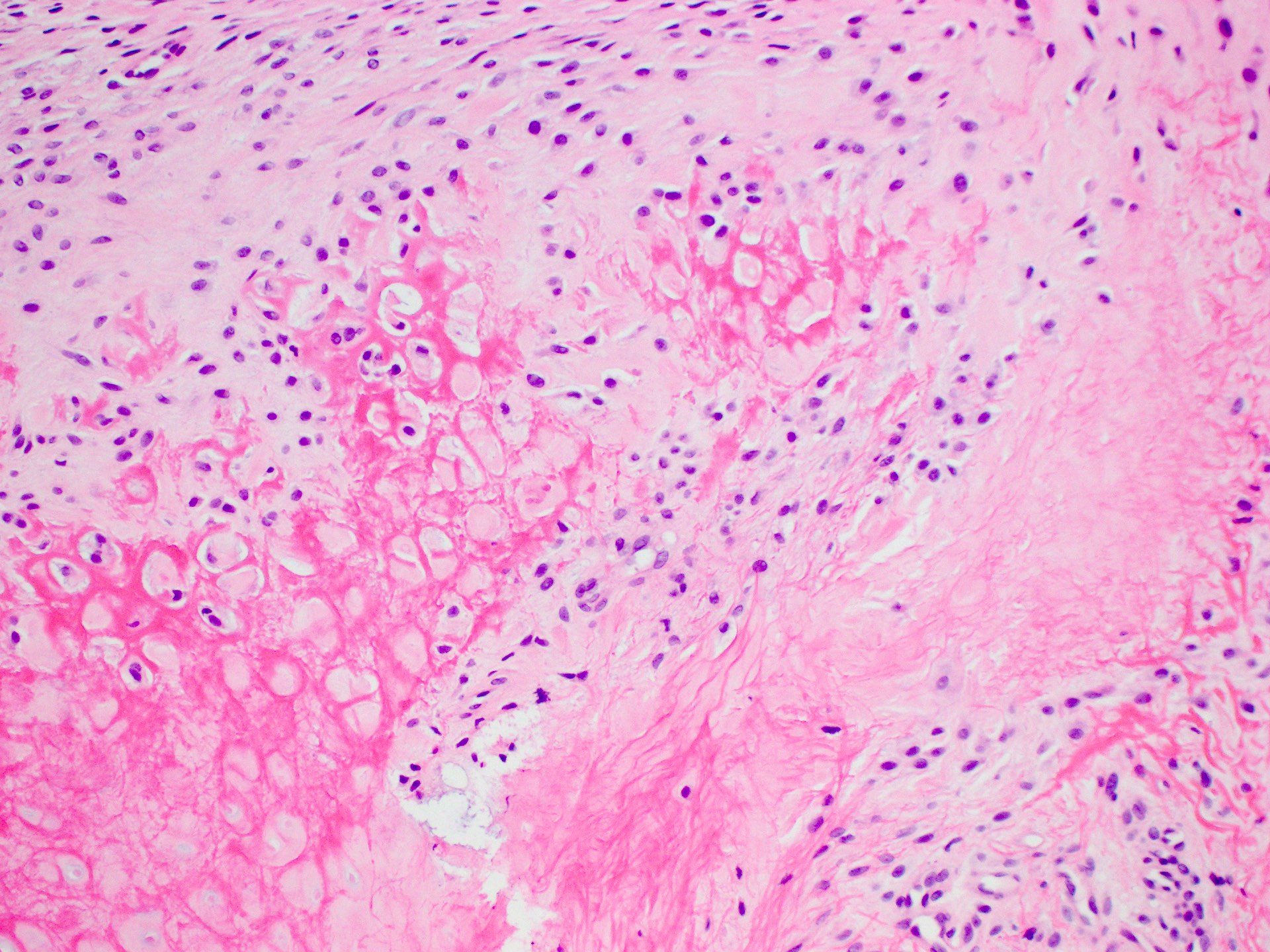
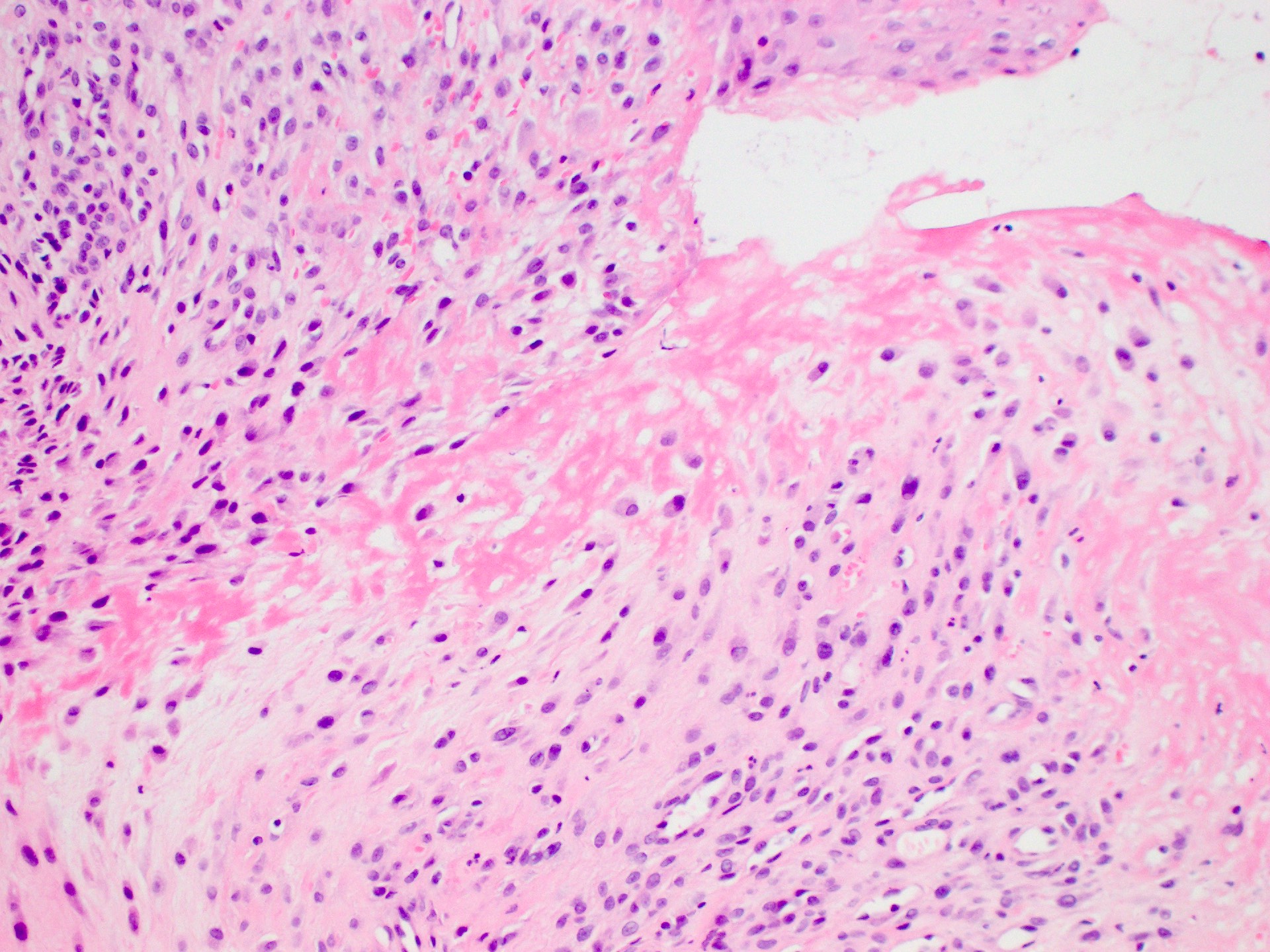
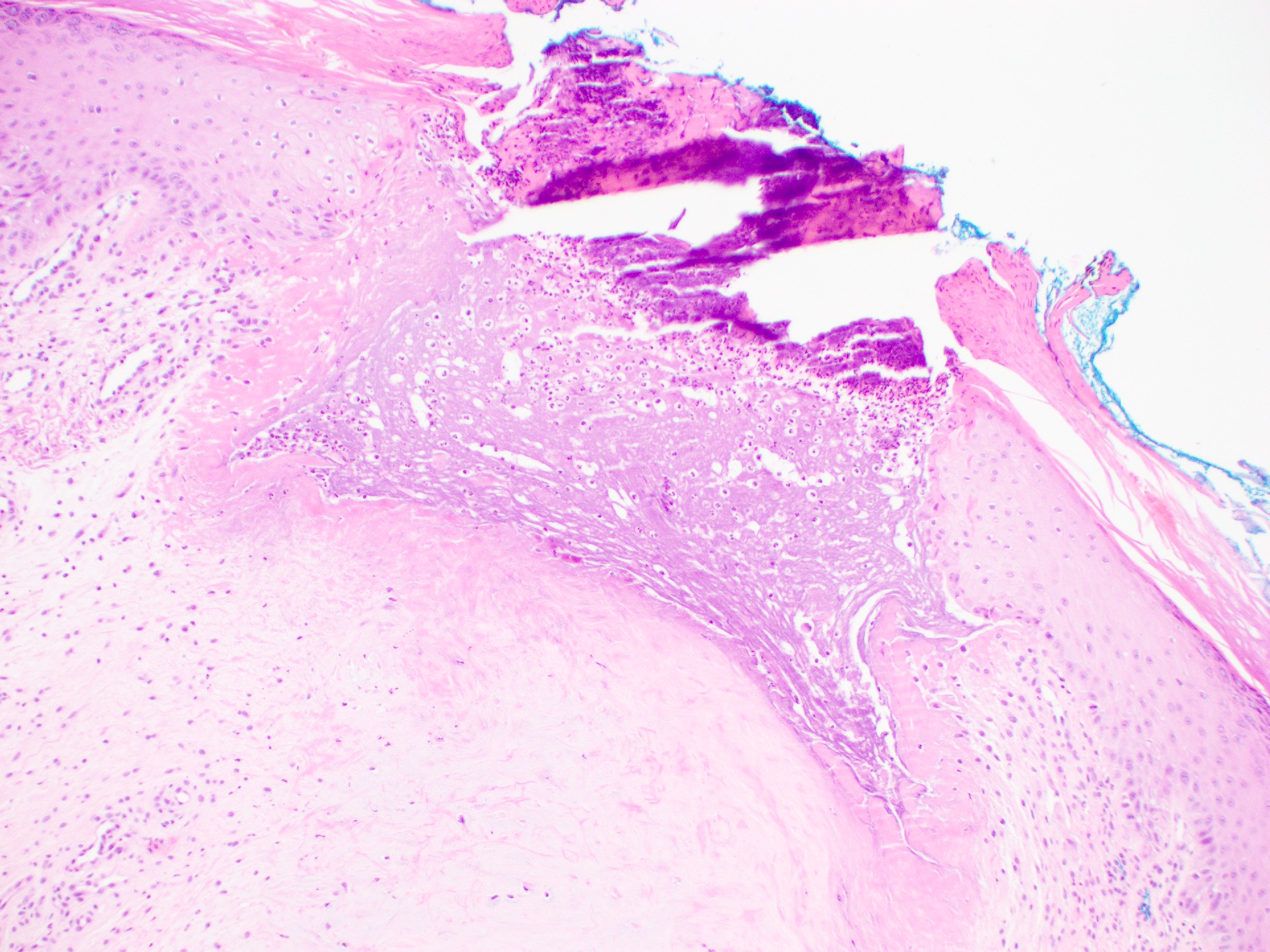
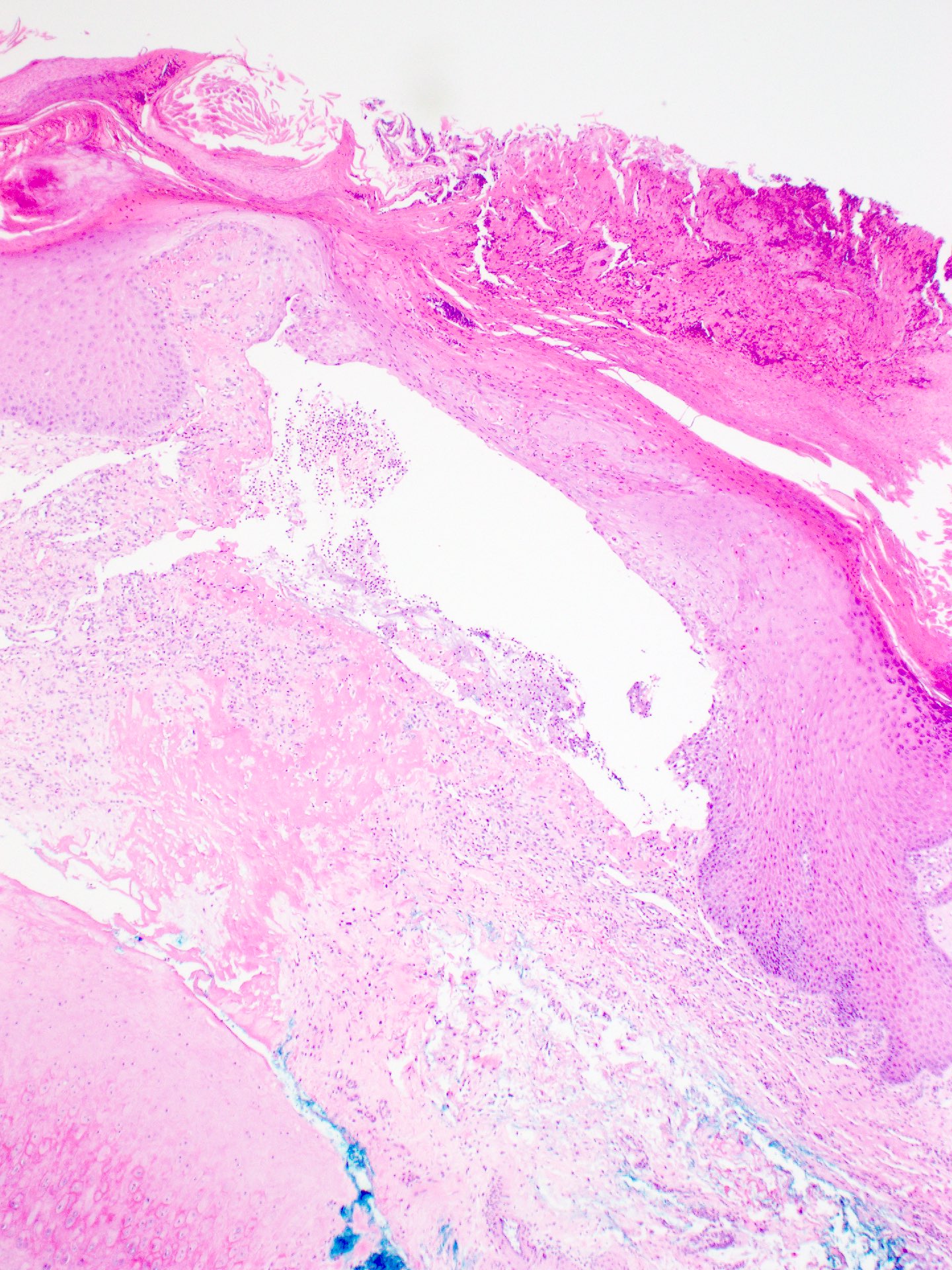
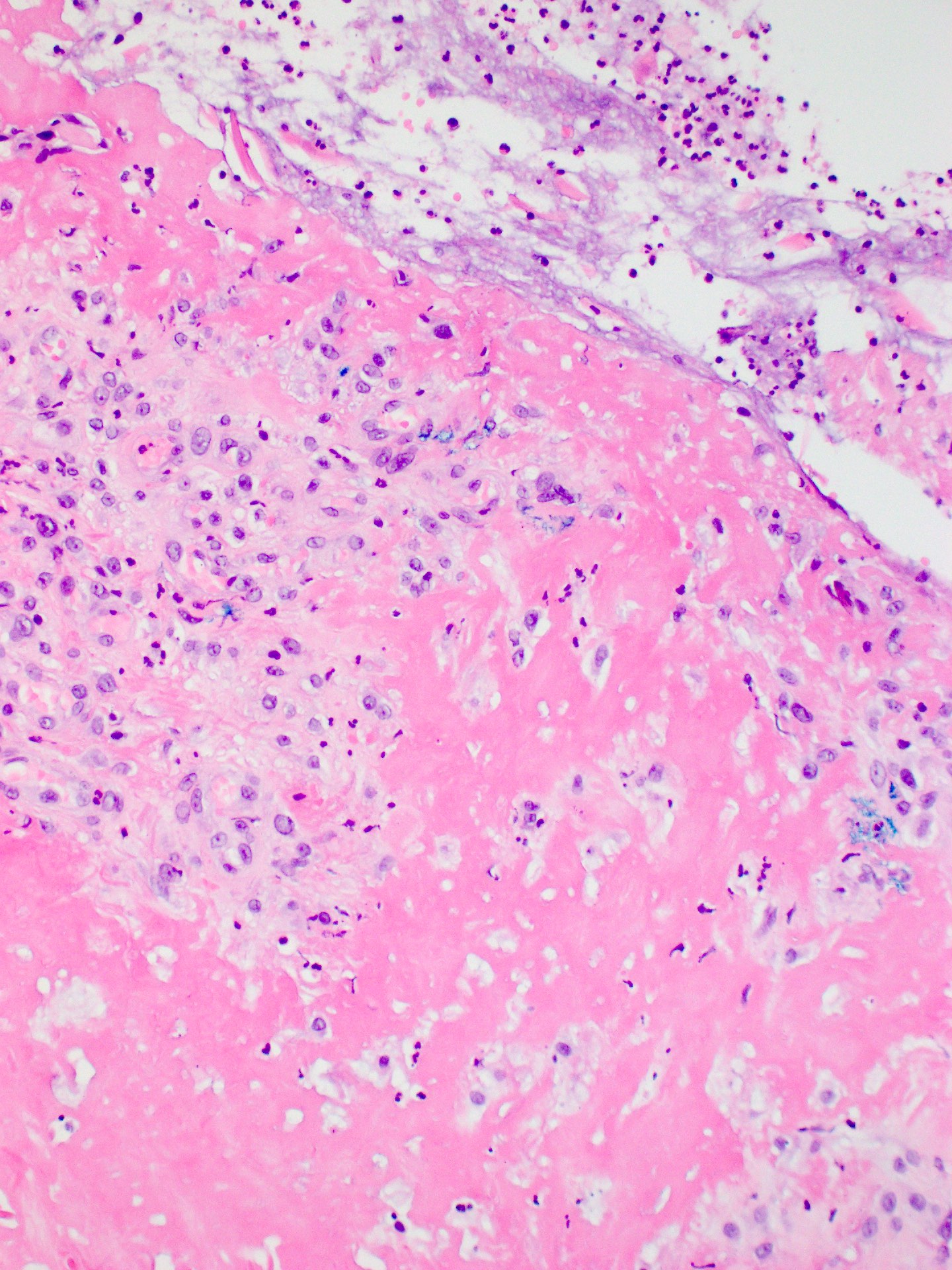
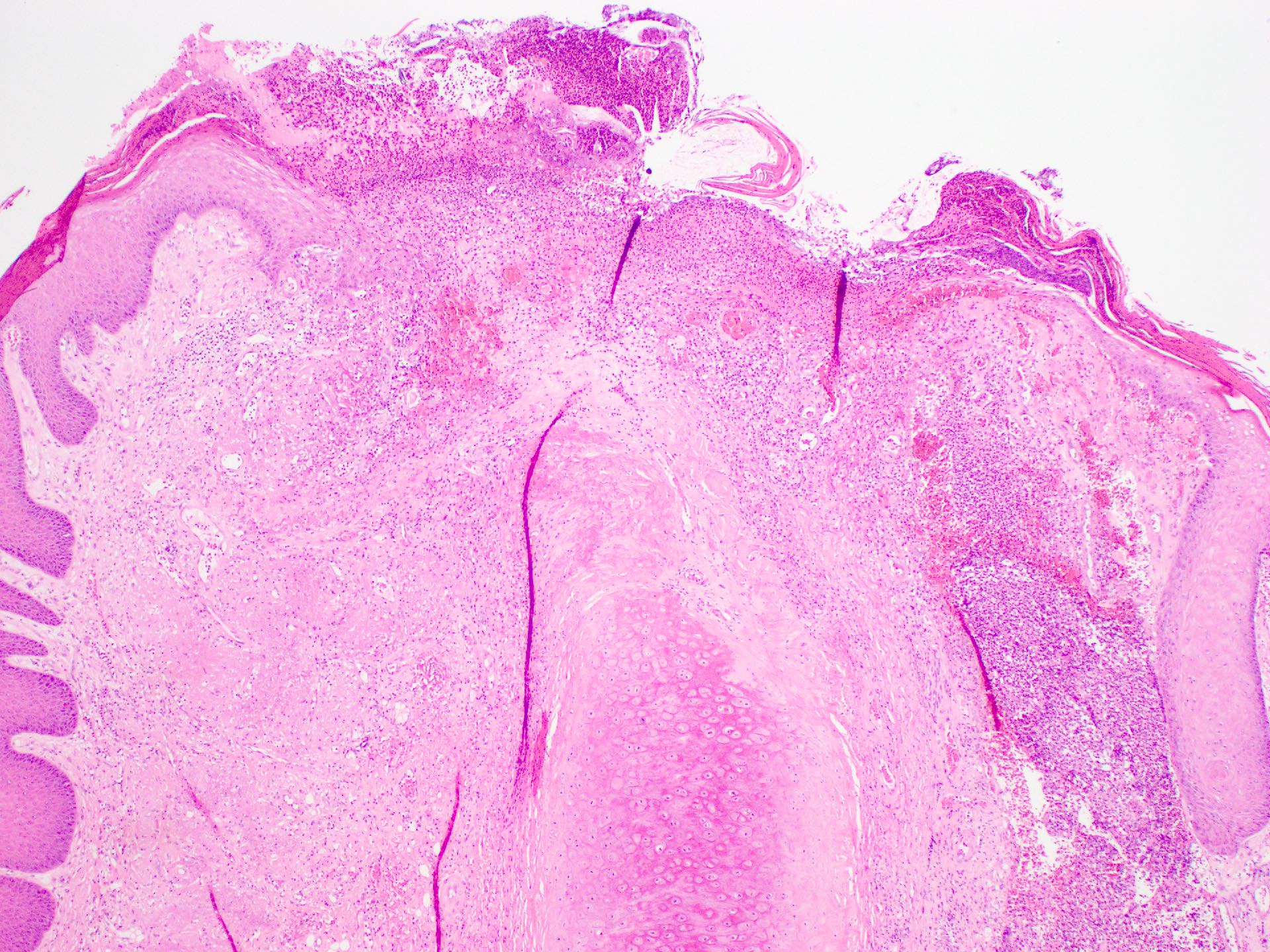
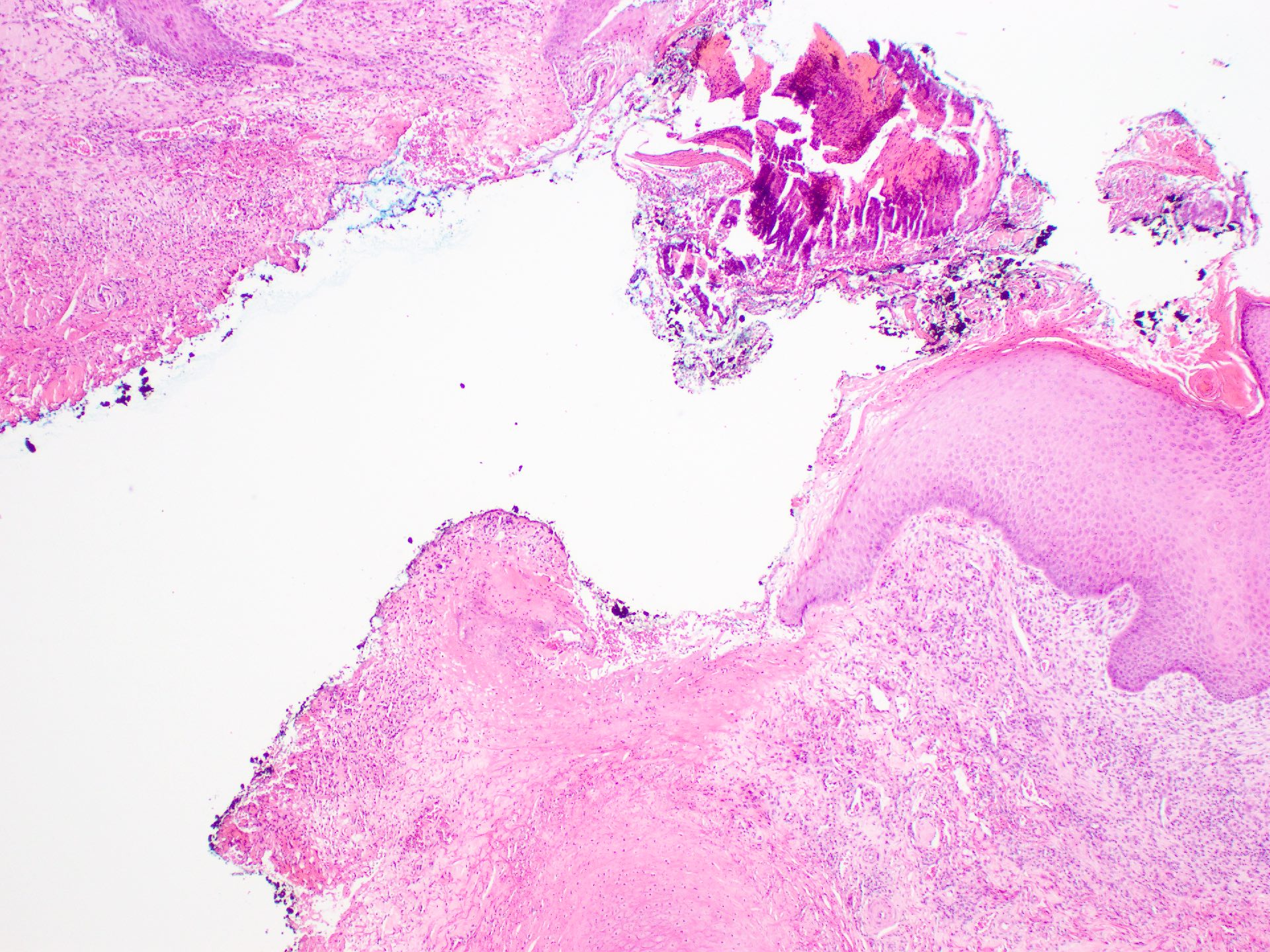
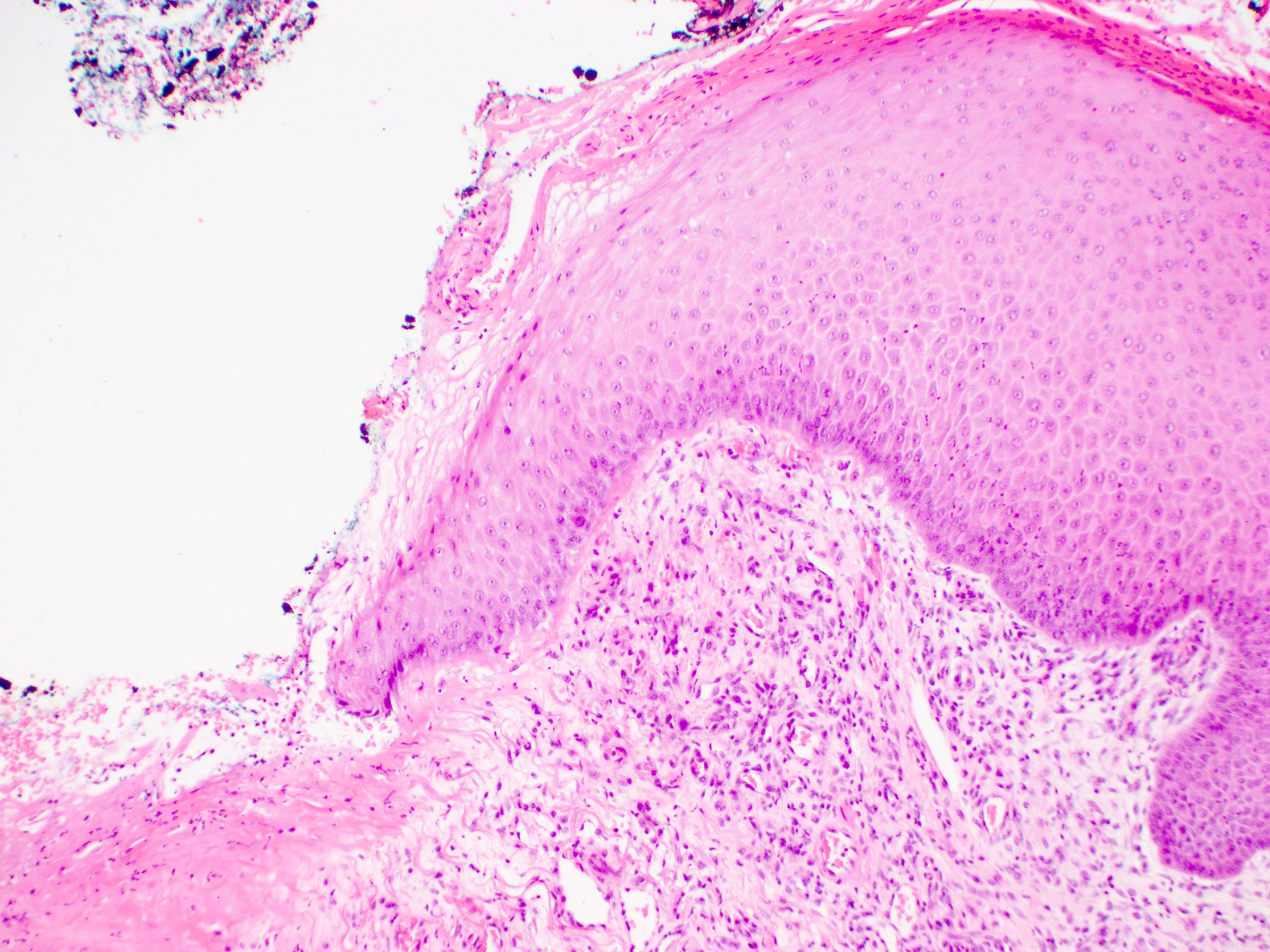
Microscopic (histologic) description
- Essential criteria, as per WHO: cup shaped crater with necrotic debris and fibrin extending to involve the superficial cartilage
- Ulcerating papulonodule filled with necrotic debris, fibrin, variable inflammatory cells
- Hyperkeratotic and parakeratotic crusting of the epidermis with adjacent acanthosis containing acute inflammatory cells
- Inverted funnel shaped defect in dermis, with necrobiosis of underlying collagen; the dermal collagen appears homogenous and eosinophilic with admixed fibrin
- Superficial cartilage erosion characterized by loss of basophilia, fibrosis and chondrocyte dropout
- Banal angioplasia is often seen in the dermis adjacent to fibrin deposition
- References: J Clin Pathol 1959;12:179, StatPearls: Chondrodermatitis Nodularis Helicis [Accessed 29 February 2024]
Microscopic (histologic) images
Contributed by Cale Michael Max Fletcher, B.Med., M.P.H. and Ruta Gupta, M.D.
Virtual slides
Videos
Chondrodermatitis nodularis helicis by Dr. Jerad Gardner
Sample pathology report
- Skin, left helix, punch biopsy:
- Chondrodermatitis nodularis helicis (see comment)
- Comment: Punch biopsy of squamous epithelium to underlying cartilage shows a funnel shaped ulcer with adjacent acanthosis. Skin surface bears a parakeratotic crust. The underlying dermis is homogenized and eosinophilic with fibrin deposition extending to involve the superficial cartilage. Chondrocyte dropout and loss of basophilia is seen. There is a mild accompanying population of mixed inflammatory cells and ectatic vessels.
- No squamous atypia is seen. There are no features of malignancy.
- The features are those of chondrodermatitis nodularis helicis.
Differential diagnosis
- Keratinocyte proliferative lesions:
- Squamous cell carcinoma:
- Macroscopic: resembles chondrodermatitis nodularis helicis (ulcerated or keratotic papule or nodule)
- Microscopic: squamous atypia with nuclear hyperchromasia, pleomorphism, mitoses and incomplete maturation and paradoxical keratinization
- Adjacent epidermis may show actinic keratosis
- Basal cell carcinoma:
- Macroscopic: pearly telangiectatic papule, which may be ulcerated
- Microscopic
- Nodules of basaloid cells with scanty cytoplasm and angulated, hyperchromatic nuclei
- Mitoses and apoptosis are easily found
- There is palisading of nuclei at the periphery of the nests and retraction artifact
- Squamous cell carcinoma:
- Inflammatory:
- Granuloma annulare:
- Interstitial granulomatous inflammation centered around necrobiotic collagen, with mucin deposition between collagen fibers
- Gouty tophi:
- Nodular aggregates of acellular, amorphous pale eosinophilic material with granulomatous inflammation
- Granuloma annulare:
- Painful nodular tumors, which occur rarely on the pinna (J Dtsch Dermatol Ges 2011;9:287):
- Eccrine spiradenoma:
- Circumscribed basaloid tumor within the dermis
- Composed of tubules and ductules containing basement membrane-like material
- 2 cell populations are seen (central pale cells and more peripheral basaloid cells)
- Glomus tumor:
- Well circumscribed mass comprising glomus cells, vessels and smooth muscle cells
- Leiomyoma:
- Well circumscribed soft tissue mass composed of intersecting fascicles of bland smooth muscle
- Neuroma:
- Circumscribed, unencapsulated spindle cell proliferation comprising axons, Schwann cells, endoneurial and perineurial cells
- Eccrine spiradenoma:
Additional references
Board review style question #1
Board review style answer #1
B. Chondrodermatitis nodularis helicis. No neoplastic proliferation is present. Inflammatory changes, including a funnelshaped ulcer and fibrinous sinus tract, can be seen extending to the underlying cartilage. Answers A and D are incorrect because they require the presence of a neoplastic population of epithelial cells. Answer C is incorrect because it requires the presence of an amorphous, eosinophilic nodule with associated granulomatous inflammation.
Comment Here
Reference: Chondrodermatitis nodularis helicis
Comment Here
Reference: Chondrodermatitis nodularis helicis
Board review style question #2
Which of the following is true regarding chondrodermatitis nodularis helicis?
- Most cases occur in patients with an autoimmune or connective tissue disease
- Most commonly found on the helix and antihelix of older men
- Neoplastic lesion characterized by necrobiotic dermal collagen and erosion of superficial cartilage
- Precipitating injury is believed to be microbial infection
Board review style answer #2
B. Most commonly found on the helix and antihelix of older men. The helix and antihelix are the most common sites for this lesion; however, any cartilage containing, pressure prone area may be susceptible. Answer A is incorrect because ~15% of cases occur in patients with an autoimmune or connective tissue disease (e.g., polymyalgia rheumatica). Answer C is incorrect because chondrodermatitis nodularis helicis is a nonneoplastic lesion. Answer D is incorrect because the precipitating injury is believed to be solar / actinic damage or cold exposure.
Comment Here
Reference: Chondrodermatitis nodularis helicis
Comment Here
Reference: Chondrodermatitis nodularis helicis