Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zhao X, Wei S. Basal cell adenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsbasalcelladenoma.html. Accessed March 30th, 2025.
Definition / general
- Benign salivary tumor composed of nests and cords of small basaloid cells with inner ductal epithelial cells
- First described by Kleinasser and Klein in 1967 (Arch Klin Exp Ohren Nasen Kehlkopfheilkd 1967;189:302)
- Initially included in the group of monomorphic adenoma (unfavored term) along with canalicular adenoma; in 1991, recognized as an independent entity in the second edition of the Salivary Gland Tumors Classification by the WHO
Essential features
- Rare benign epithelial tumor of the salivary gland, displaying monomorphic basaloid cells without a myxochondroid component
Terminology
- Also called monomorphic adenoma, basaloid salivary gland adenoma
- Membranous adenoma also called dermal analogue tumor
ICD coding
Epidemiology
- 1 - 3.7% of all salivary gland tumors (Med Oral Patol Oral Cir Bucal 2006;11:E206)
- Frequent in elderly adults between fifth and seventh decades; uncommon in young adults (J Dent (Shiraz) 2015;16:291)
- Female predilection (2:1) except for the membranous type, which bears an equal M:F distribution (J Laryngol Otol 1989;103:756)
- Membranous type basal cell adenomas can associate with Brooke-Spiegler syndrome (Eur J Dermatol 2004;14:139)
Sites
- > 80% arise in the major salivary glands, mostly parotid gland (mainly in the superficial lobe), followed by the submandibular gland (5%) and 6% in intraoral location with upper lip being the most common site, followed by the buccal mucosa
Pathophysiology
- Intercalated duct lineage (IDL) could be precursor; IDL, tubular basal cell adenoma (BCA) and nontubular BCA form a continuum of lesions in which IDLs are related closely to tubular BCA (Histopathology 2014;64:880)
- According to some studies, myoepithelial or intercalated duct lineage might be the origin of BCA (J Maxillofac Oral Surg 2010;9:289)
- Epithelial tumor cells of pleomorphic adenoma (PA) may form BCA through certain differentiation mechanisms; basal cells of the epithelium of PA possess reserve cell functions, through epithelial - mesenchymal transdifferentiation, forming the predominant basaloid cell population of basal cell adenoma (Auris Nasus Larynx 2006;33:97)
Etiology
- Etiology and risk factors for BCA are unknown
- Membranous type basal cell adenomas can associate with Brooke-Spiegler syndrome (multiple familial trichoepithelioma) caused by CYLD mutation (Eur J Dermatol 2004;14:139)
Clinical features
- Rare, 1 - 2% of epithelial tumors of salivary glands; 2% of benign salivary gland tumors
- Solitary or part of turban tumor, Brooke-Spiegler syndrome
- Usually adults, 67% female, mean age 58 years
- Rarely is congenital and resembles embryoma
- Almost all arise in parotid gland, with submandibular gland being a distant second
- Usually appears as a firm and mobile, slow growing, asymptomatic mass
- Low recurrence rate except for membranous type
- Rarely transforms into malignancy; more likely if membranous type (4% malignant transformation)
- Usually some myoepithelial differentiation using immunostains (Arch Pathol Lab Med 2000;124:401)
- Membranous type may present as multiple nodules; may coexist with dermal cylindromas or trichoepitheliomas
Diagnosis
- Diagnosis is established by the histological study; generally, biopsy is accepted as the most accurate method to obtain the diagnosis, although some authors advocate for fine needle aspiration if physical access to the tumor is available
Radiology description
- Nonspecific
- Oval to round tumor with smooth distinct margin and high incidence of internal macro or microcysts
- Soft tissue components with relative high attenuation on unenhanced CT and enhance well on contrast enhanced CT (AJR Am J Roentgenol 2007;189:W254, AJNR Am J Neuroradiol 2012;33:434)
- Relatively homogenous signal intensity of the solid portion; tumor capsule is low signal intensity on T2 weighted images (Dentomaxillofac Radiol 2010;39:349)
Radiology images
Prognostic factors
- Recurrence rate ~ 2% on average; almost nonexistent for the solid and trabecular - tubular variants
- Membranous type most commonly associated with recurrence (25 - 37%), likely due to the multicentricity rather than because of true recurrences (Acta Otolaryngol 1998;118:588)
- Malignant transformation is more common in the membranous type (4%) than in the other types; total parotidectomy rather than superficial parotidectomy is proposed in the membranous type of BCA (J Oral Maxillofac Pathol 2016;20:142, Acta Otolaryngol 1998;118:588)
Case reports
- 22 year old man with cytological diagnosis of basal cell adenoma (J Oral Maxillofac Pathol 2015;19:106)
- 43 year old woman with basal cell adenoma of sublingual gland (Ann Otol Rhinol Laryngol 2003;112:1066)
- 51 year old man with 6 cm parotic mass of 8 years' duration (Case #375)
- 54 year old woman with basal cell adenoma extending to skull base and mastoid (World J Clin Cases 2019;7:1351)
- 55 year old woman with basal cell adenoma of palate (J Dent (Shiraz) 2015;16:291)
- 59 year old Japanese man with basal cell adenoma of upper lip (Case Rep Med 2014;2014:795356)
- 65 year old woman with bilateral parotid basal cell adenoma (J Oral Maxillofac Surg 2010;68:179)
- 19 cases of basal cell adenoma with cribriform pattern (Ann Diagn Pathol 2014;18:5)
Treatment
- Excision: surgical resection with a cuff of normal salivary tissue as the main treatment
Gross description
- Small (mostly < 5 cm), round or oval, encapsulated nodule (Br J Radiol 2005;78:642)
- Membranous subtype often nonencapsulated, multicentric and multilobular (Pilch: Head and Neck Surgical Pathology, 1st Edition, 2001)
- Usually brownish appearance; typically uniform and solid, without necrosis; can be cystic (Arch Otolaryngol 1974;99:84)
Frozen section description
- Adequate sectioning including the capsule should be made on frozen section
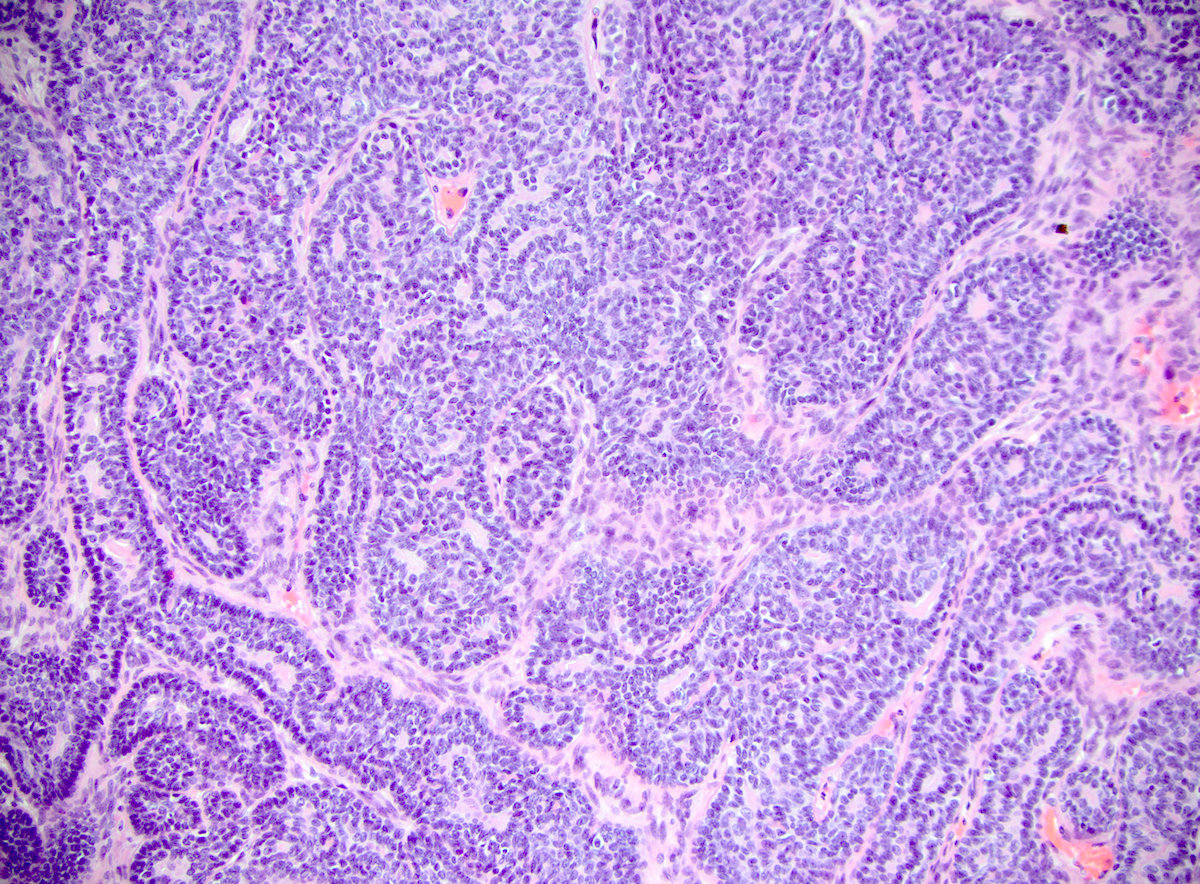
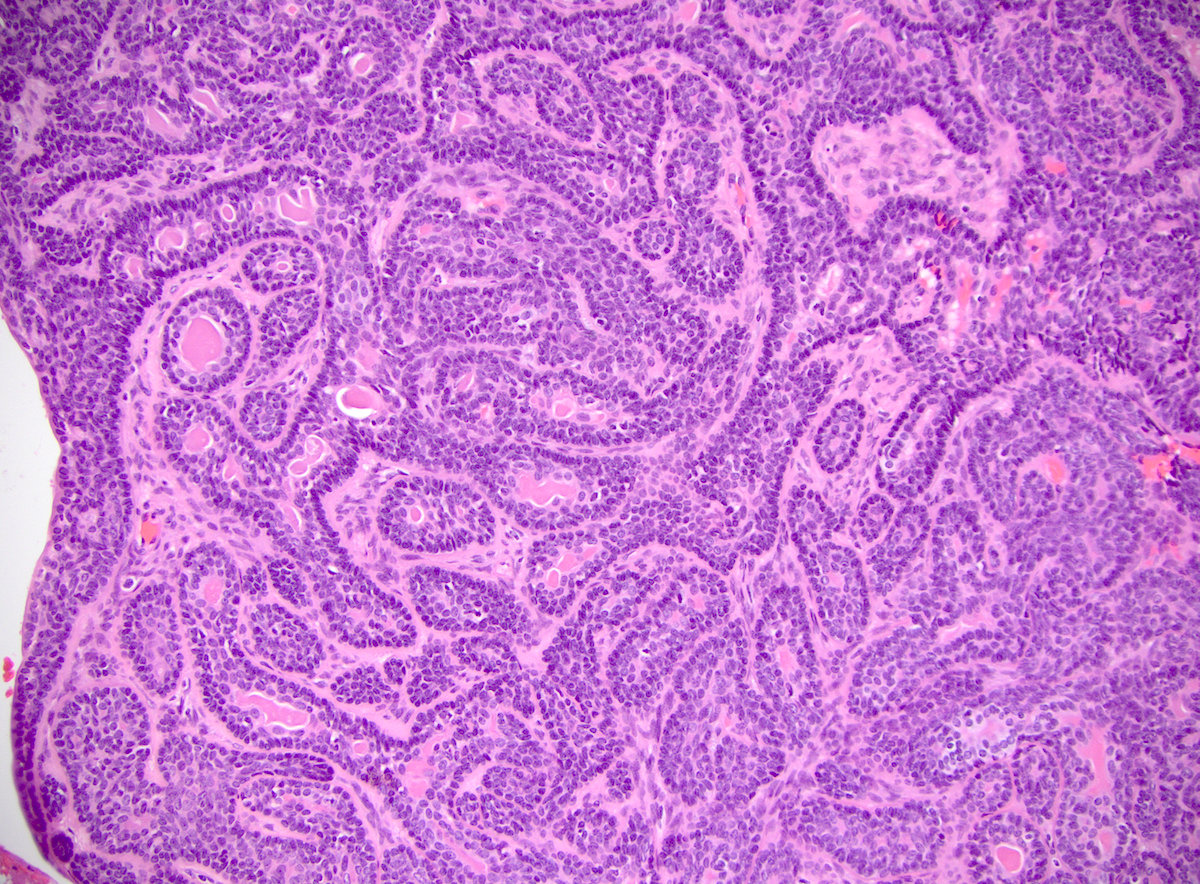
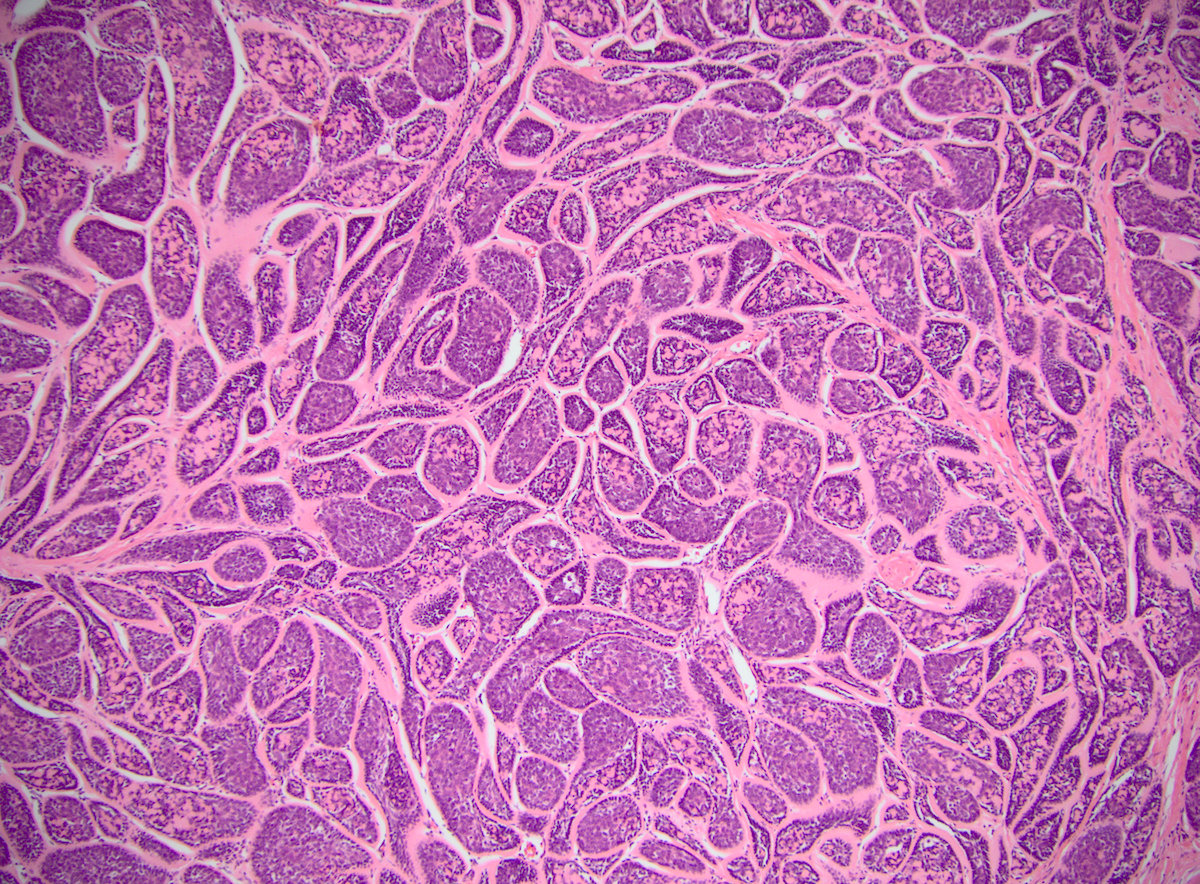
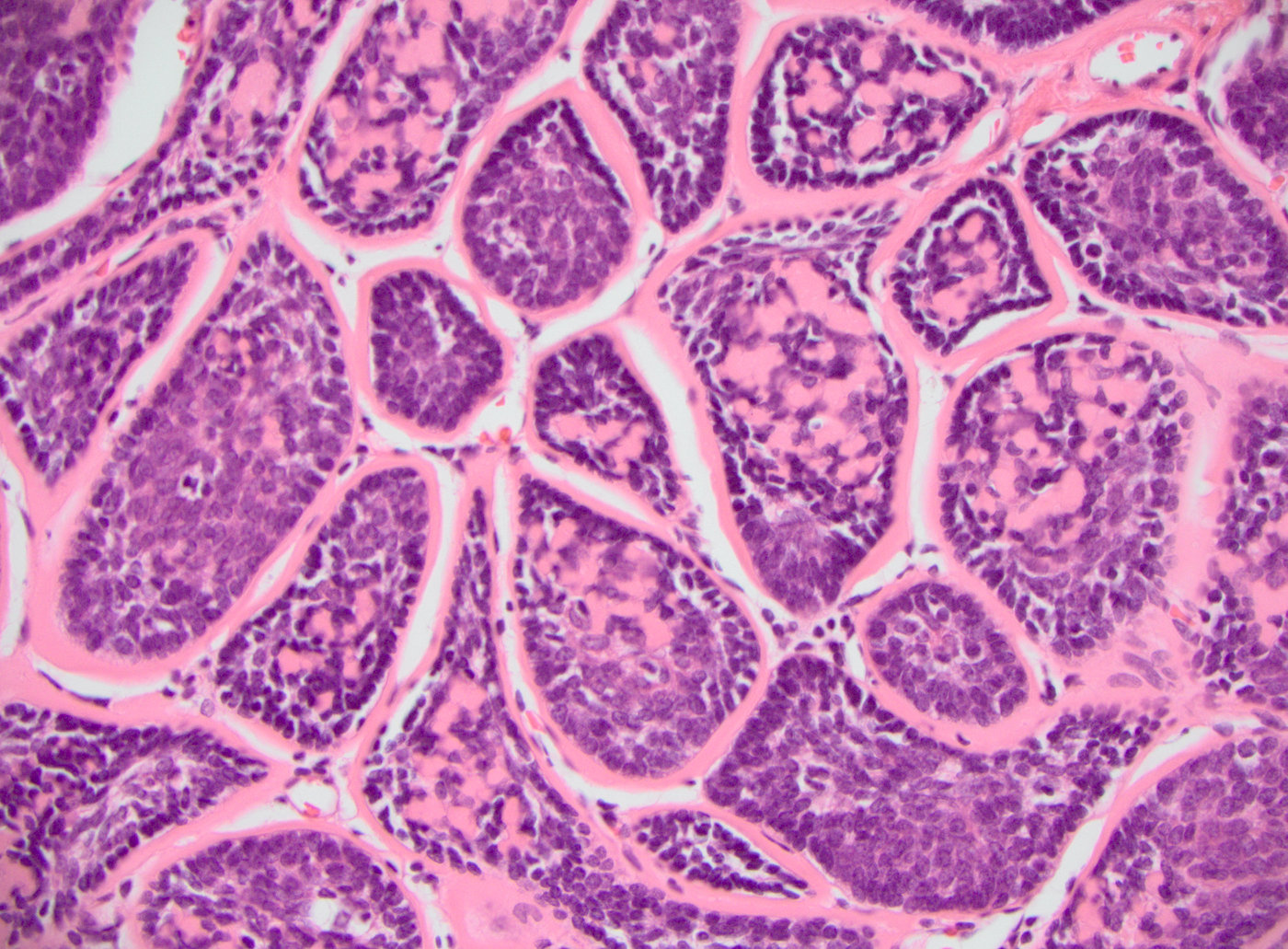
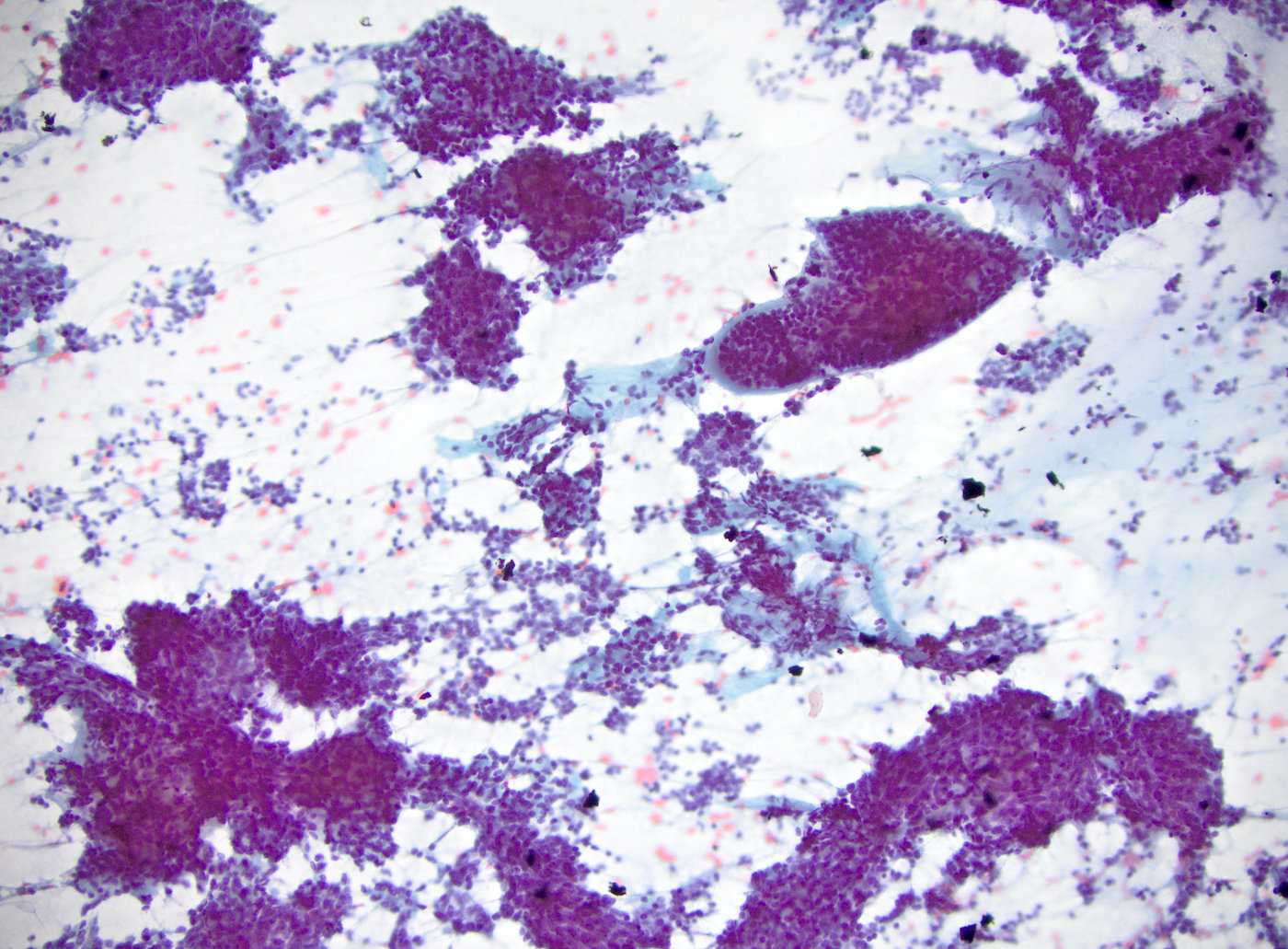
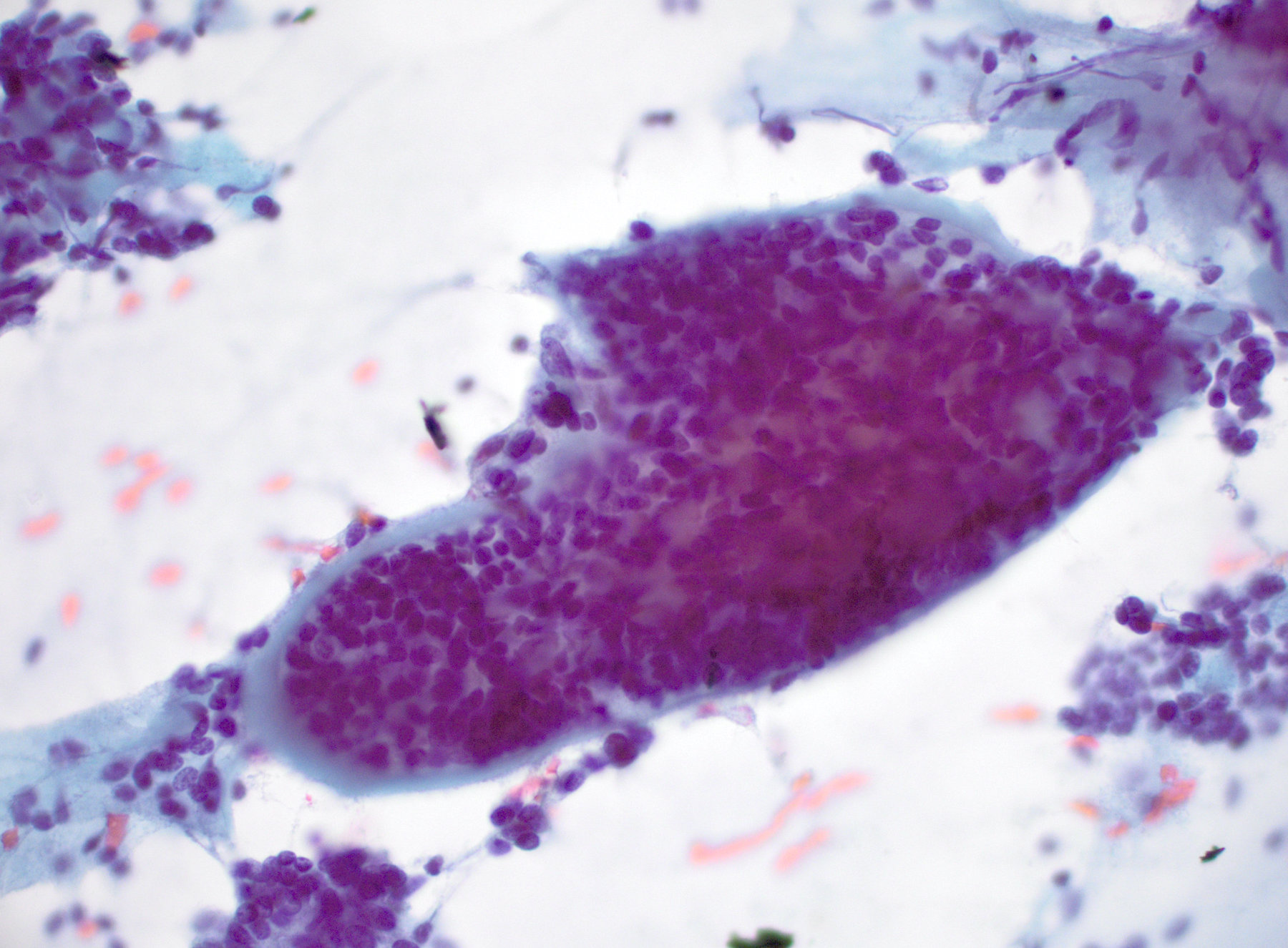
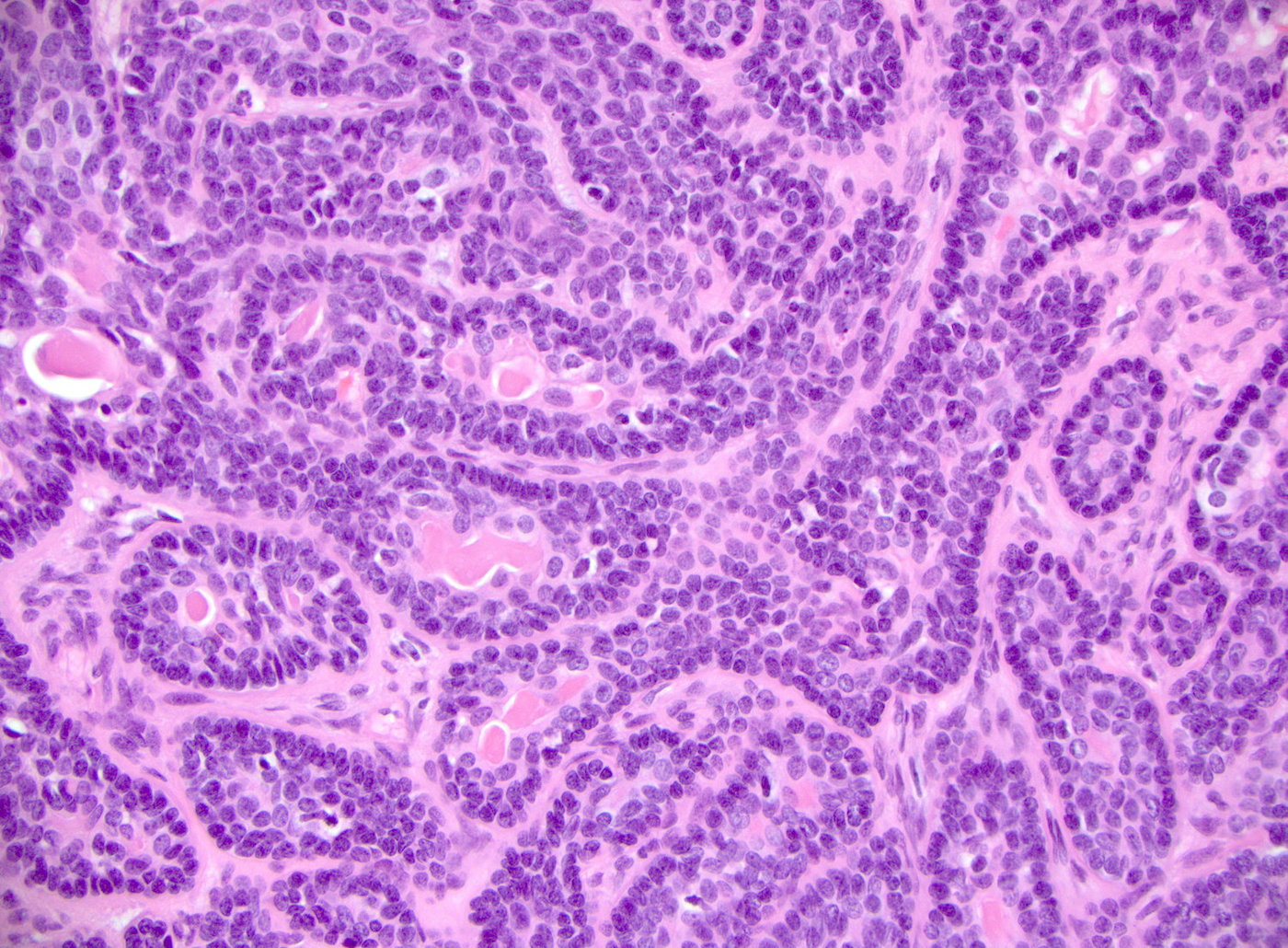
Microscopic (histologic) description
- 2 types of tumor cells:
- Basaloid cells with basal cells or myoepithelial phenotype
- Luminal cells
- Fibrocellular stroma can be present
- 4 histologic patterns: mixture of at least 2 patterns is common (Ellis: Surgical Pathology of the Salivary Glands, 1st Edition, 1991)
- Solid pattern: most common, basaloid cells are present in the form of solid masses which may show peripheral palisading
- Trabecular pattern: narrow or broad trabeculae which may get interconnected with each other creating a reticular pattern
- Tubular pattern: numerous tubules consisting of a central lumen and an outer single layer or double layered lining of cuboidal and basaloid cells is seen; the lumen often contains an eosinophilic secretion / mucin which is PAS positive
- Membranous types: histologically identical to dermal cylindroma, eosinophilic hyaline membranes separating cell nests; BCA with greater than 50% membranous pattern should be designated as membranous type
- Cyst formation is common and can be a main histopathologic feature of basal cell adenoma
- Occasionally has acinar cells, squamous whorls or keratinization
- No invasion, no perineurial invasion, no chondromyxoid matrix
Microscopic (histologic) images
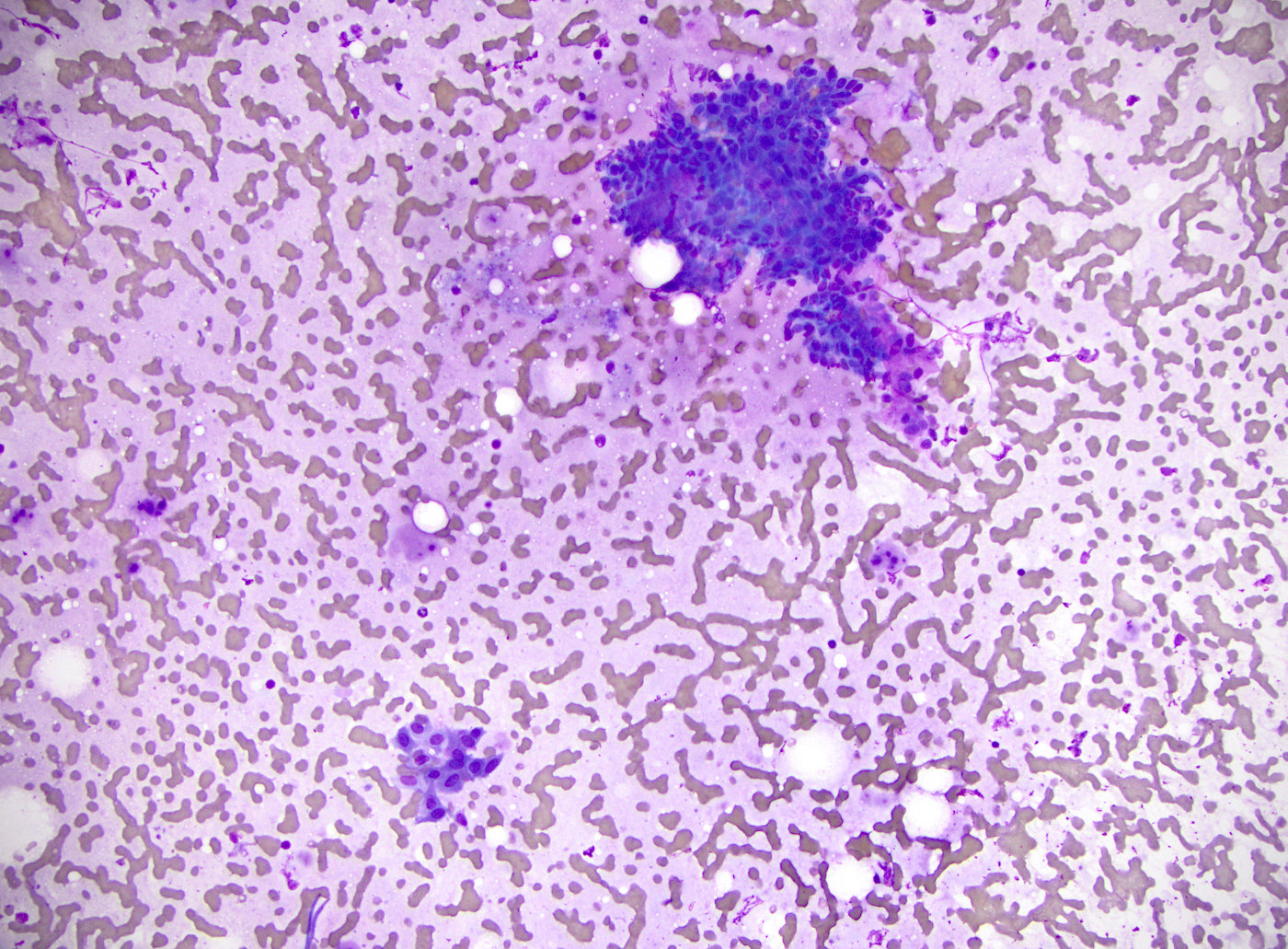
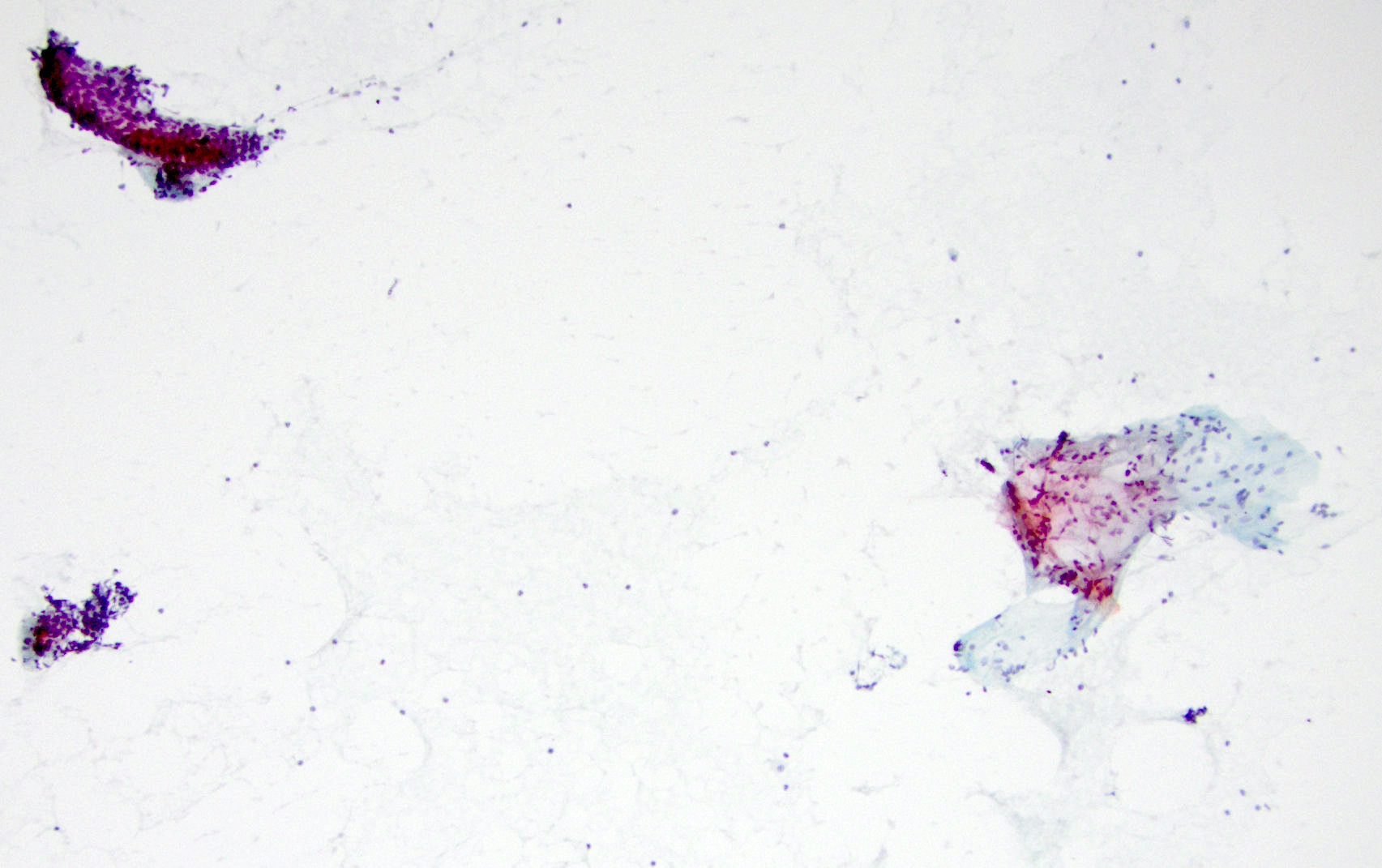
Cytology description
- Monomorphic basaloid cels with round nuclei and scant cytoplasm (Diagn Cytopathol 2007;35:85)
- Irregular nests and trabecula, tubular or peripheral palisading architecture
- Benign mimickers: cellular pleomorphic adenoma (with chondromyxoid stroma) and myoepithelioma
- Malignant mimickers: basal cell adenocarcinoma and basaloid squamous cell carcinoma (with significant cytological atypia, mitosis and necrosis) (Am J Clin Pathol 2002;118:S100)
- Membranous basal cell adenoma simulates adenoid cystic carcinoma (J Cytol 2018;35:55)
Cytology images
Positive stains
- Ductal cells: keratin, alpha-1-antichymotrypsin, CEA, EMA, CD117 (Pathol Res Pract 1991;187:145)
- Basaloid cells: vimentin, actin, calponin, S100, p63, GFAP
- Spindle cell in the stroma is positive for S100, negative for p63
- Can be positive for BCL2 and nuclear beta catenin (Am J Surg Pathol 2016;40:1143)
Electron microscopy description
- Myoepithelial cells show microfilaments, desmosomes, junctional complexes, reduplicated basal lamina (Dardick: Salivary Gland Tumor Pathology, 1st Edition, 1996)
- Ductal cells show microvilli, tight junctions, desmosomes (Acta Otorhinolaryngol Ital 2005;25:150)
Molecular / cytogenetics description
- CTNNB1 mutations are common in BCA, especially those with tubular or tubulotrabecular patterns (Am J Surg Pathol 2016;40:1143)
- CYLD1 mutations and loss in sporadic and Brooke-Spiegler syndrome associated basal cell adenoma (Mod Pathol 2018;31:1064, Am J Surg Pathol 2002;26:778)
Sample pathology report
- Parotid, left, parotidectomy:
- Basal cell adenoma, 1.6 cm, membranous type, margins negative for tumor
Differential diagnosis
- Adenoid cystic carcinoma:
- Infiltrative growth pattern, perineural invasion
- Basal cell adenocarcinoma:
- Invasive growth pattern
- Pleomorphic adenoma:
- Chondromyxoid stroma blended with epithelial cells, BCA with prominent myoepithelial derived stroma and stroma in BCA does not blend into the epithelial nests
- Canalicular adenoma:
- Double columns of cells forming anastomosing canaliculi with paucicellular stroma
Additional references
Board review style question #1
A 56 year old woman presents with a nodule close to the left ear. Imaging reveals a well circumscribed 1.6 cm nodule in parotid gland. Biopsy findings are shown in the picture above. Which of the following statements is true about this entity?
- Cystic change is uncommon
- Due to the high recurrence rate, total excision is required for all of these neoplasms
- It is one of the most common neoplasms in the salivary glands
- It occurs more often in younger patients
- It can be associated with Brooke-Spiegler syndrome
Board review style answer #1
E. It can be associated with Brooke-Spiegler syndrome. Brooke-Spiegler syndrome is a rare genetic disease characterized as an inherited skin tumor predisposition syndrome presenting with skin appendage tumors (cylindromas, spiradenomas and trichoepitheliomas) and salivary gland tumor. Some patients can have a membranous basal cell adenoma of the salivary gland. It is caused by germline mutations in the CYLD gene (16q12-q13).
Comment Here
Reference: Basal cell adenoma
Comment Here
Reference: Basal cell adenoma
Board review style question #2
Which of the following markers is most useful to differentiate tubular / trabecular predominant basal cell adenoma from pleomorphic adenoma?
- Beta catenin
- Calponin
- CMA
- p63
- S100
Board review style answer #2
A. Beta catenin. Jo et al. reported that nuclear beta catenin staining can be present in 83% of basal cell adenomas. All adenoid cystic carcinomas (0/20) and pleomorphic adenomas (0/20) were negative. 4 of 5 basal cell adenomas had exon 3 CTNNB1 mutations (Am J Surg Pathol 2016;40:1143).
Comment Here
Reference: Basal cell adenoma
Comment Here
Reference: Basal cell adenoma