Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Czaja R, Iczkowski KA. Malakoplakia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatemalako.html. Accessed April 26th, 2024.
Definition / general
- Rare chronic inflammatory reaction that affects multiple sites, most commonly the bladder and rarely the prostate
Essential features
- Rare inflammatory condition strongly associated with infection (especially gram negative bacilli) and immunosuppression
- Michaelis-Gutmann bodies (intracytoplasmic calcific inclusions) are pathognomonic
- Clinically mimics prostatic adenocarcinoma and histology is definitive
ICD coding
Epidemiology
- Affected men reported between 43 to 85 years old (Ann Diagn Pathol 2016;22:33)
- More common in immunocompromised patients (Ann Diagn Pathol 2016;22:33)
Sites
- May occur in multiple sites, including mucosa, skin and most commonly the bladder; however, has been reported in the prostate
Pathophysiology
- Gram negative bacteria, such as Escherichia coli and Klebsiella pneumoniae, infect the urinary tract
- Undigested bacteria accumulate, which is thought to be secondary to a defect in host macrophage and monocyte lysosomal degradation (Histol Histopathol 2020;35:177)
- Michaelis-Gutmann bodies are formed when iron and calcium accumulate around the undigested bacteria
- Eventually, a mass-like lesion may form in the prostate (Urol Case Rep 2020;32:101222)
Etiology
- Frequently associated with culture positive, predominantly enteric gram negative bacilli, urinary tract infections
Clinical features
- Majority of cases associated with positive urinary cultures, E. coli and K. pneumoniae being the most frequently isolated bacteria (Folia Med Cracov 2019;59:67)
- Affected men may present with an enlarged prostate or bladder outlet obstruction
- There have been several cases reported with concomitant prostatic adenocarcinoma (Ann Diagn Pathol 2016;22:33)
Diagnosis
- Clinical findings may prompt follow up imaging or procedures
- Imaging with MRI is suspicious for carcinoma
- Histologic examination for definitive diagnosis
Laboratory
- Elevated prostate specific antigen (PSA) (Folia Med Cracov 2019;59:67)
- Often positive urine culture for gram negative bacilli
Radiology description
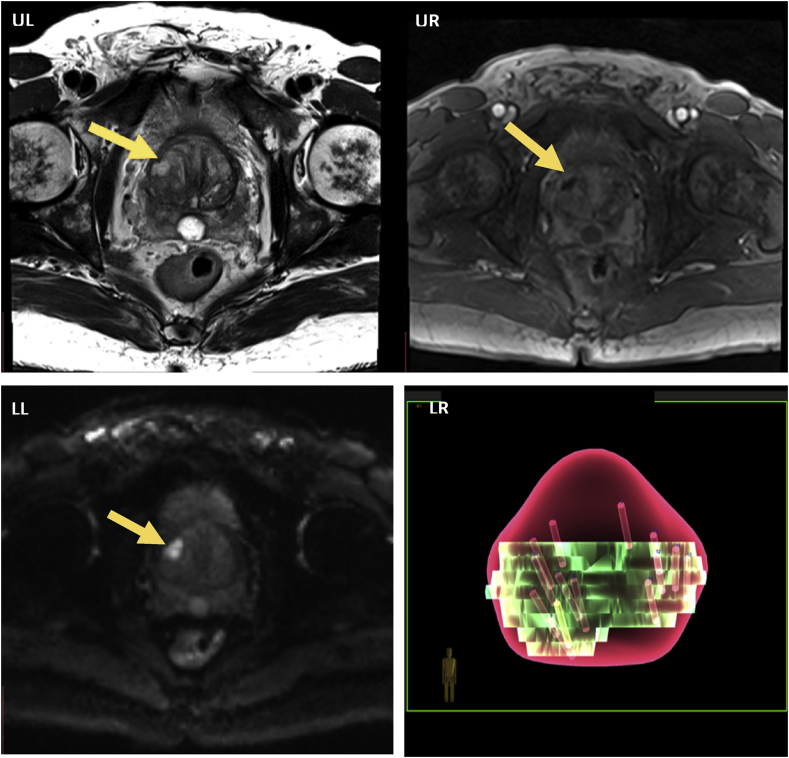
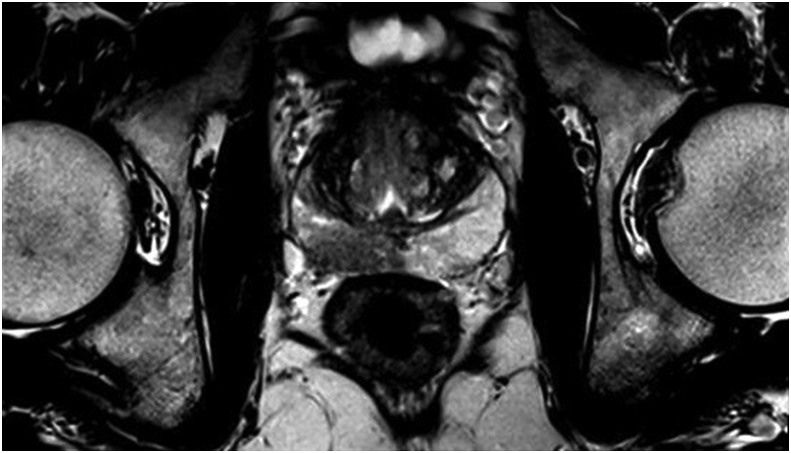
- Multiparametric magnetic resonance imaging (mpMRI) with hypointense lesion(s), which may correspond to higher prostate imaging reporting and data system (PI-RADS) scores (Urol Case Rep 2020;32:101222)
Radiology images
Case reports
- 43 year old man with fever and elevated PSA (Int J Clin Exp Pathol 2018;11:4153)
- 57 year old man with rising PSA over 3 years (Urol Case Rep 2020;32:101222)
- 61 year old man with recurrent E. coli urinary tract infection and months of urinary obstruction symptoms (J Endourol Case Rep 2020;6:231)
- 63 year old man with persistently elevated PSA (Urol Case Rep 2017;18:94)
- 75 year old man with elevated PSA (J Endourol Case Rep 2017;3:74)
Treatment
- Combined medical, such as antibiotics for the background urinary tract infection and surgical approach, depending on extent of disease and anatomic site of involvement (Int J Clin Exp Pathol 2018;11:4153)
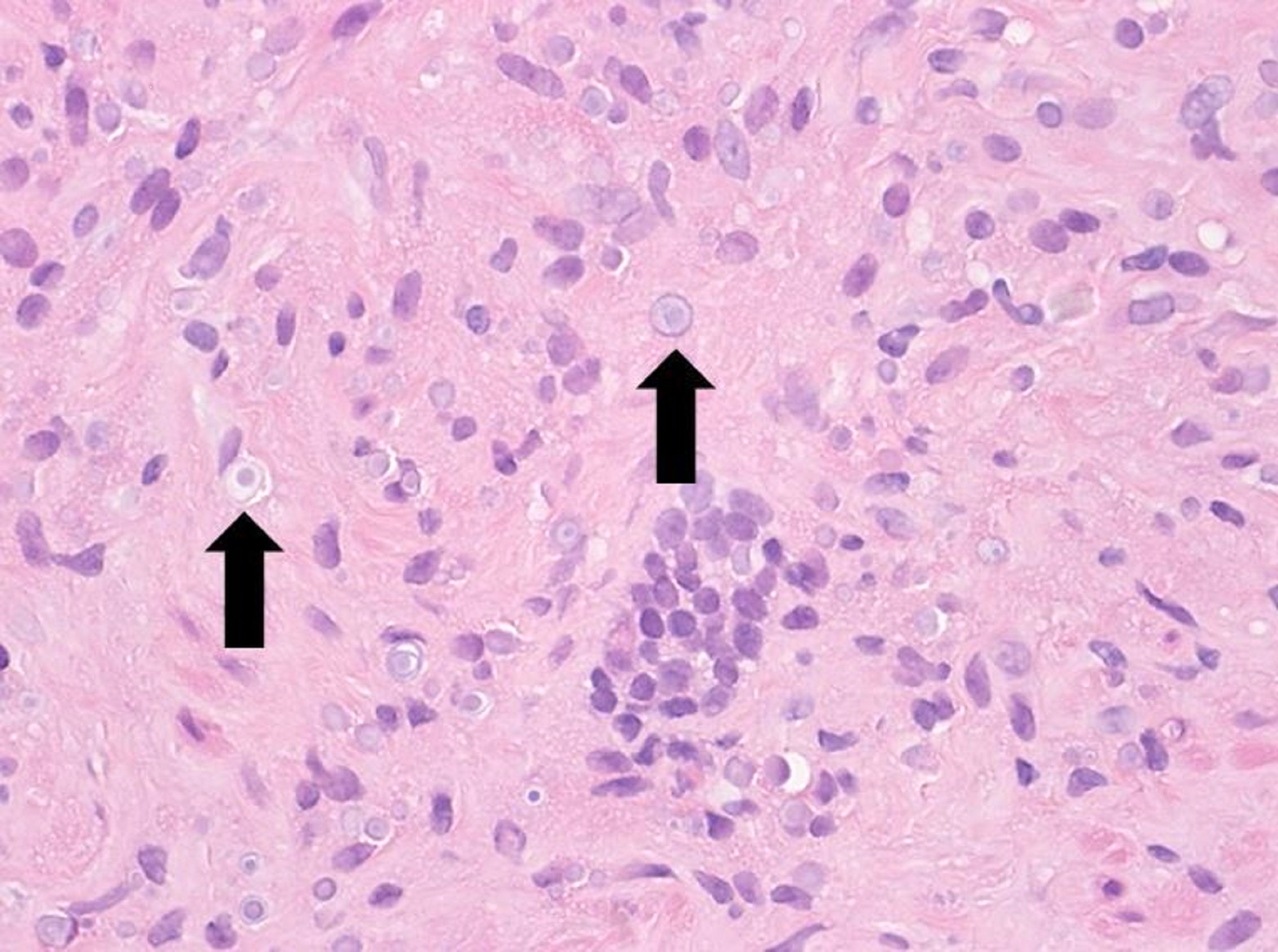
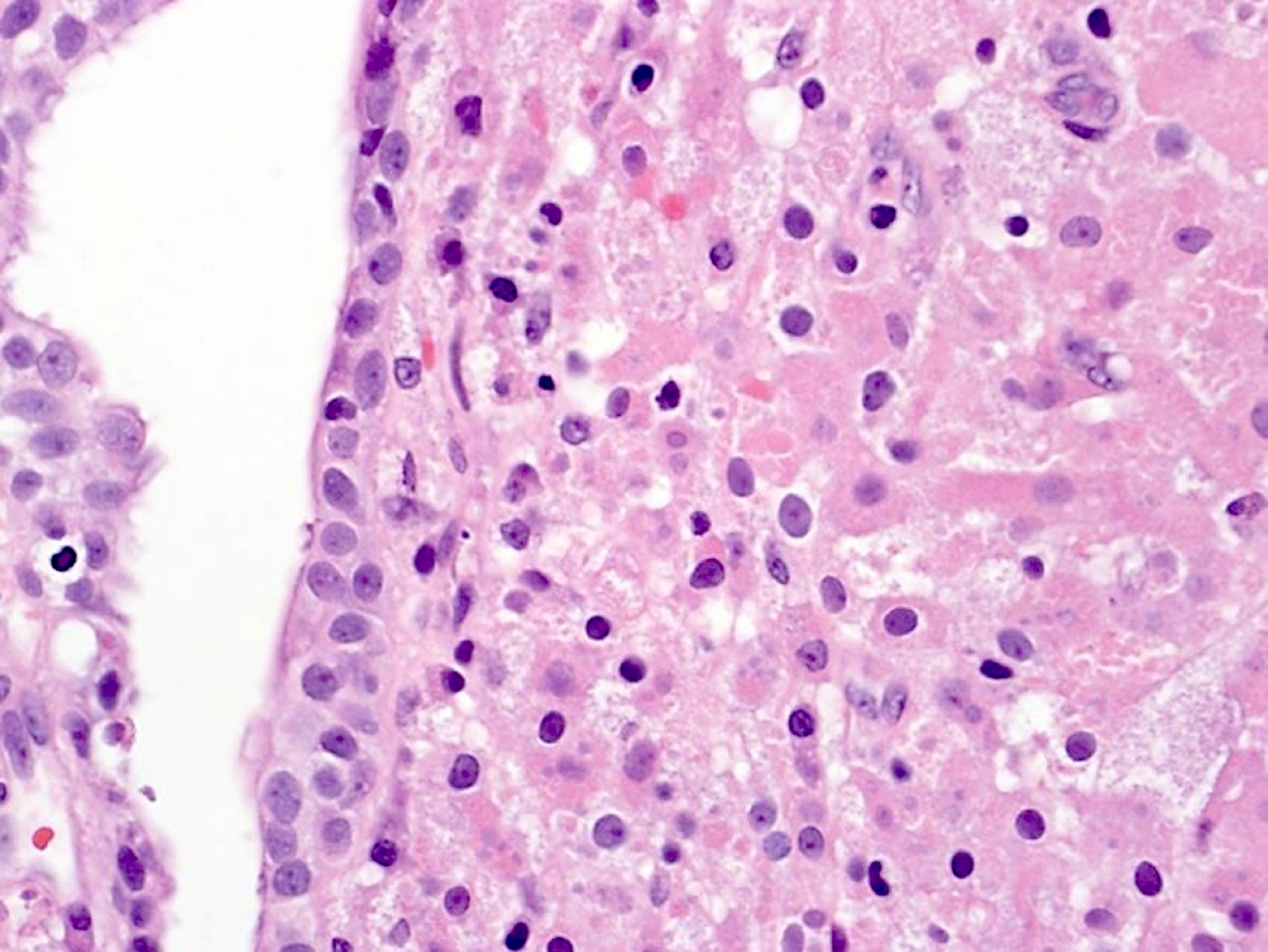
Microscopic (histologic) description
- Prostatic tissue with infiltration by round histiocytes with eosinophilic, granular cytoplasm (von Hansemann cells) (Urol Case Rep 2017;18:94)
- Histiocytes contain round and basophilic intracytoplasmic inclusions with bullseye appearance known as Michaelis-Gutmann bodies
- Admixed acute and chronic inflammation may be present
Microscopic (histologic) images
Positive stains
- von Kossa stain (calcium) highlights Michaelis-Gutmann bodies
- Prussian blue (iron) stains Michaelis-Gutmann bodies blue
- Periodic acid-Schiff (PAS) stain highlights histiocytic eosinophilic cytoplasm
- CD163 and CD68 show extent of histiocytic involvement
- Reference: Urol Case Rep 2014;3:6
Negative stains
Sample pathology report
- Prostate, needle core biopsy:
- Malakoplakia (see comment)
- Comment: The specimen shows diffuse involvement by histiocytes with eosinophilic granular cytoplasm and frequent intracytoplasmic inclusions consistent with Michaelis-Gutmann bodies. The inclusions are emphasized by von Kossa and Prussian blue stains, while PAS highlights the granular cytoplasm of the histiocytes.
Differential diagnosis
- Prostatic adenocarcinoma:
- Small glands with nuclear enlargement, hyperchromasia and prominent nucleoli
- May be associated with acute or chronic inflammation but histiocytic inflammation is not typically identified (Ann Diagn Pathol 2016;24:55)
- Lacks Michaelis-Gutmann bodies
- Positive for AE1 / AE3
- Negative for CD68 and CD163
- Xanthogranulomatous inflammation:
- Collections of histiocytes with abundant foamy cytoplasm
- Lacks Michaelis-Gutmann bodies
- Negative for von Kossa and Prussian blue
- Infectious granulomatous prostatitis, tuberculous prostatitis:
- Central caseous necrosis surrounded by epithelioid histiocytes, plasma cells and multinucleated giant cells
- Negative for von Kossa and Prussian blue
- Nonspecific granulomatous prostatitis:
- Lacks Michaelis-Gutmann bodies
- Negative for von Kossa and Prussian blue
Board review style question #1
Board review style answer #1
B. Escherichia coli. E. coli is one of the most commonly associated organisms which have been associated with prostatic malakoplakia and is an enteric gram negative bacillus. Prevotella bivia is another gram negative bacillus; however, is typically recovered from oral and vaginal sites. P. bivia may cause urinary tract infections; however, there has not, as of the drafting of this article, been a case associated with malakoplakia. Chlamydia trachomatis is a gram negative bacteria that is transmitted through infected secretions, infects mucosal membranes and is most commonly associated with sexually transmitted infections. Staphylococcus saprophyticus is a gram positive coccus and is associated with urinary tract infections in young women.
Comment Here
Reference: Malakoplakia
Comment Here
Reference: Malakoplakia
Board review style question #2
A 49 year old man presents with urinary obstructive symptoms and imaging is concerning for malignancy. On histopathology, several intracytoplasmic inclusions are noted in the histiocytes. Which of the following groups of special stains would help the most with the diagnosis?
- Prussian blue, PAS, reticulin
- Prussian blue, PAS, von Kossa
- Prussian blue, trichrome, von Kossa
- Prussian blue, trichrome, reticulin
Board review style answer #2
B. Prussian blue, PAS, von Kossa. Prussian blue (iron) and von Kossa (calcium) highlight Michaelis-Gutmann bodies, as they are formed from the accumulation of iron and calcium. Trichrome stains connective tissue, including collagen, while reticulin highlights reticular fibers and basement membrane materials; neither is utilized in supporting the diagnosis of malakoplakia.
Comment Here
Reference: Malakoplakia
Comment Here
Reference: Malakoplakia