Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Vormittag-Nocito E, Kajdacsy-Balla A. Intraductal carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostateidc.html. Accessed April 26th, 2024.
Definition / general
- New addition to the most recent WHO classification of urinary tumors and male genital organs (Moch: WHO Classification of Tumours of the Urinary System and Male Genital Organs, 4th Edition, 2016)
- Intraacinar or intraductal neoplastic epithelial proliferation that has some features of high grade prostatic intraepithelial neoplasia but exhibits much greater architectural or cytological atypia, typically associated with high grade, high pT prostate carcinoma (Eur Urol 2016;70:106)
Essential features
- High degree of cytological atypia, commonly with necrosis that fills prostatic ducts and acini
- Usually associated with high grade and high pT invasive carcinoma
- Should not be included in Gleason pattern scoring
- Appropriate to use immunohistochemistry to demonstrate presence of basal cells if grade of invasive component will be impacted
Terminology
- Intraductal carcinoma of the prostate: currently recognized term
- Ductal carcinoma in situ: less favorable term
- Acinar carcinoma in situ: less favorable term
ICD coding
- ICD-11: 2E67.5 - carcinoma in situ of prostate
Epidemiology
- Seen in ~3% of prostate biopsies (Histopathology 2013;63:574)
Sites
- Prostate ducts and acini
Pathophysiology
- Possible theories include:
- End stage spread of invasive carcinoma into ducts and acini (J Pathol 2016;238:31)
- In situ component of high grade tumor leading to invasive carcinoma (eLife 2014;3:e02224, J Urol 2010;184:1328)
Etiology
- Familial prostatic adenocarcinoma with BRCA2 mutations have higher proportion of intraductal carcinoma (Eur Urol 2015;67:496)
Diagnosis
- Prostate core needle biopsy, prostatectomy or transurethral resection specimens
Laboratory
- Elevated prostate specific antigen
Radiology description
- In situ disease not identified by imaging; microscopic diagnosis only
Prognostic factors
- Associated with higher Gleason grade (patterns 4 or 5) invasive prostatic acinar adenocarcinoma (Urol Oncol 2017;35:673.e9)
- Associated with higher pT including extraprostatic extension and seminal vesicle invasion (Urol Oncol 2017;35:673.e9)
- Higher rate of biochemical recurrence (Prostate 2019;79:1065)
Case reports
- 56 year old man with firm right lobe of prostate (Arch Pathol Lab Med 2007;131:1122)
- 58 year old man with urinary frequency, urgency and nocturia (Case #286)
- 59 year old man with free floating intraductal tumoral aggregates (Int J Surg Pathol 2016;24:535)
- Man with molecular evidence of intraductal carcinoma clone metastasizing to lymph node (Eur Urol 2015;67:819)
Treatment
- Immediate rebiopsy (within 3 months) or definitive treatment by radiation or radical prostatectomy if only intraductal tumor is present (Yonsei Med J 2016;57:1054)
- If concurrent invasive carcinoma is present, typically definitive treatment is recommended
Gross description
- Not seen on gross examination; microscopic disease entity
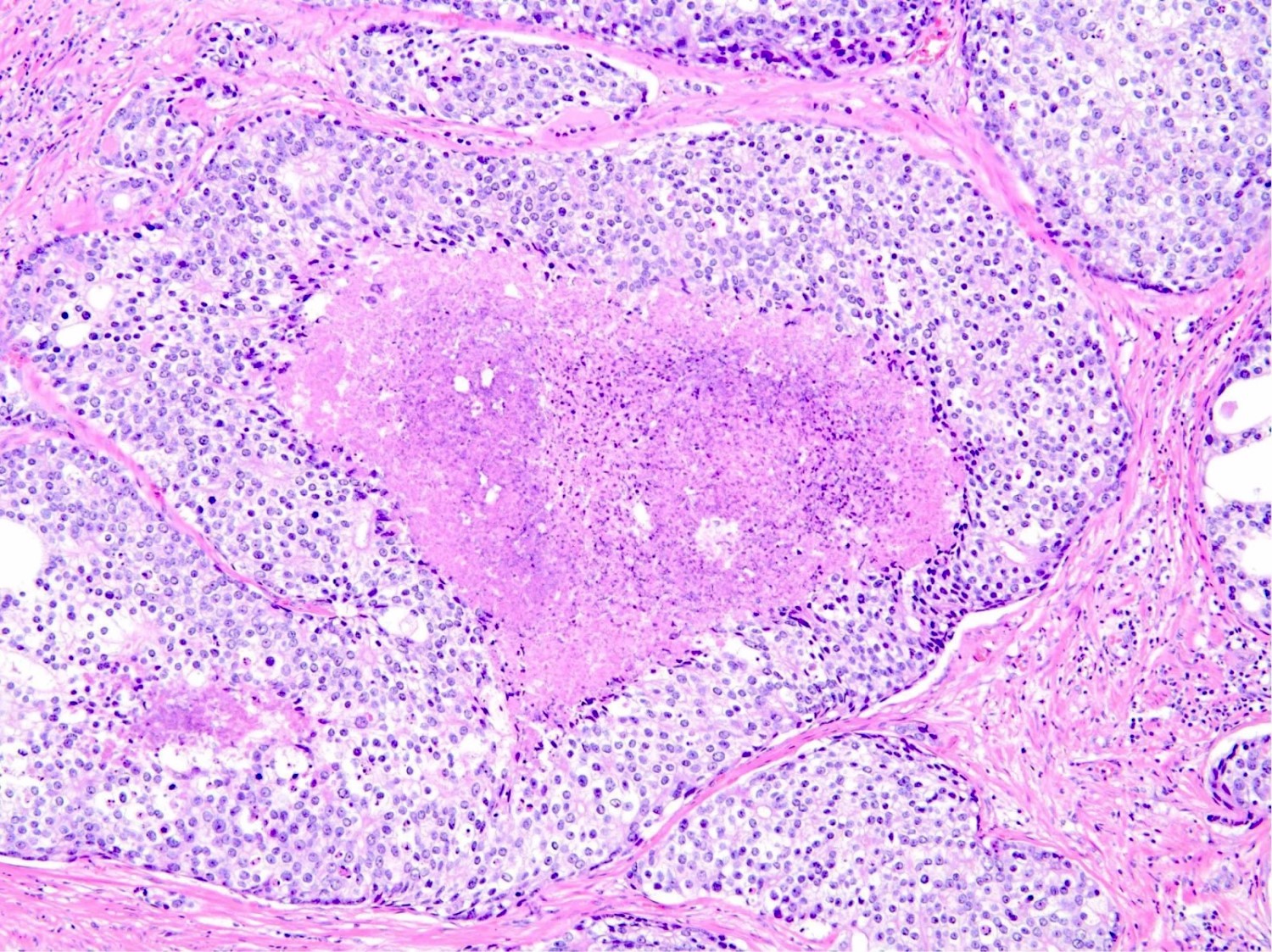
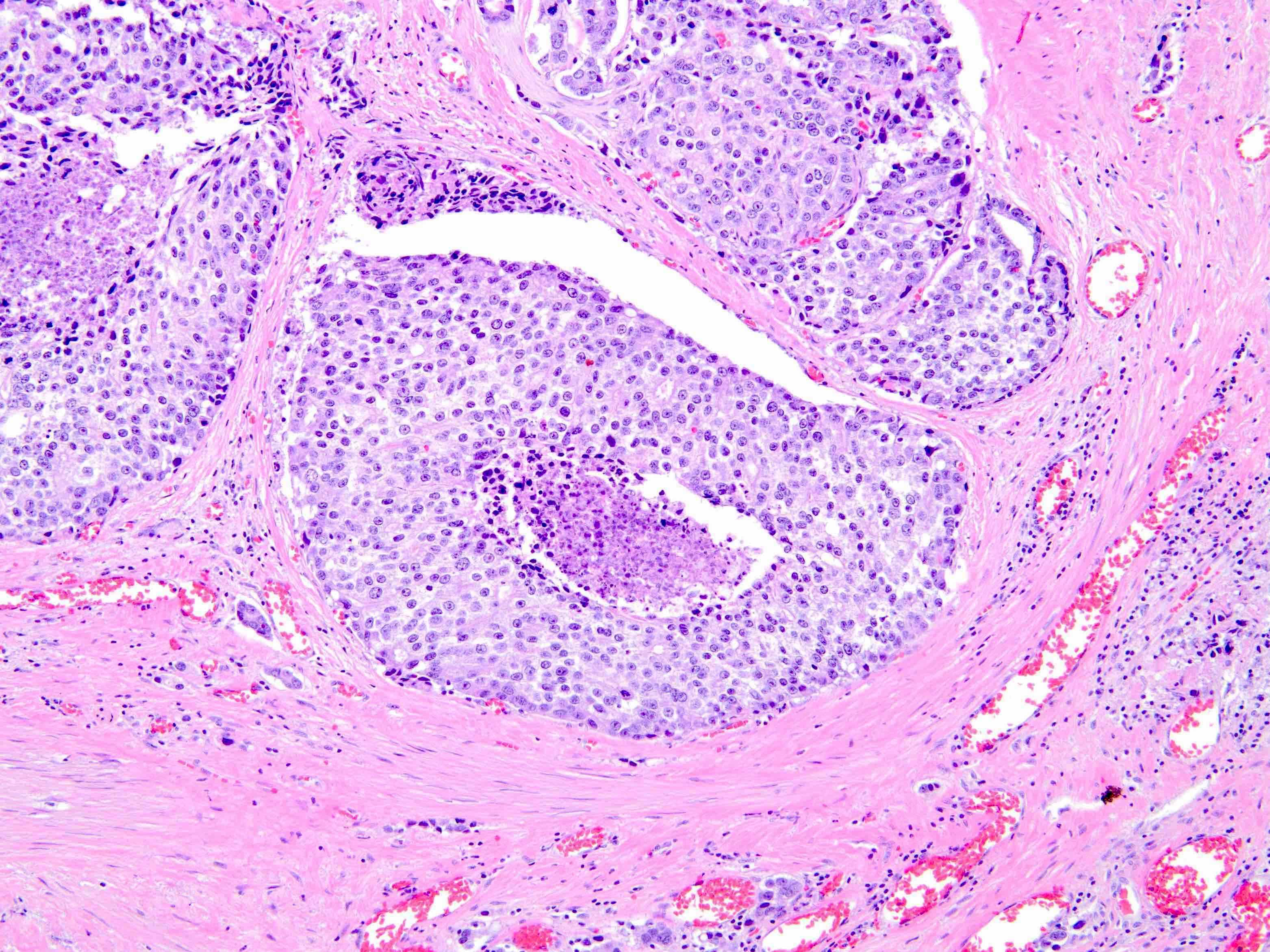
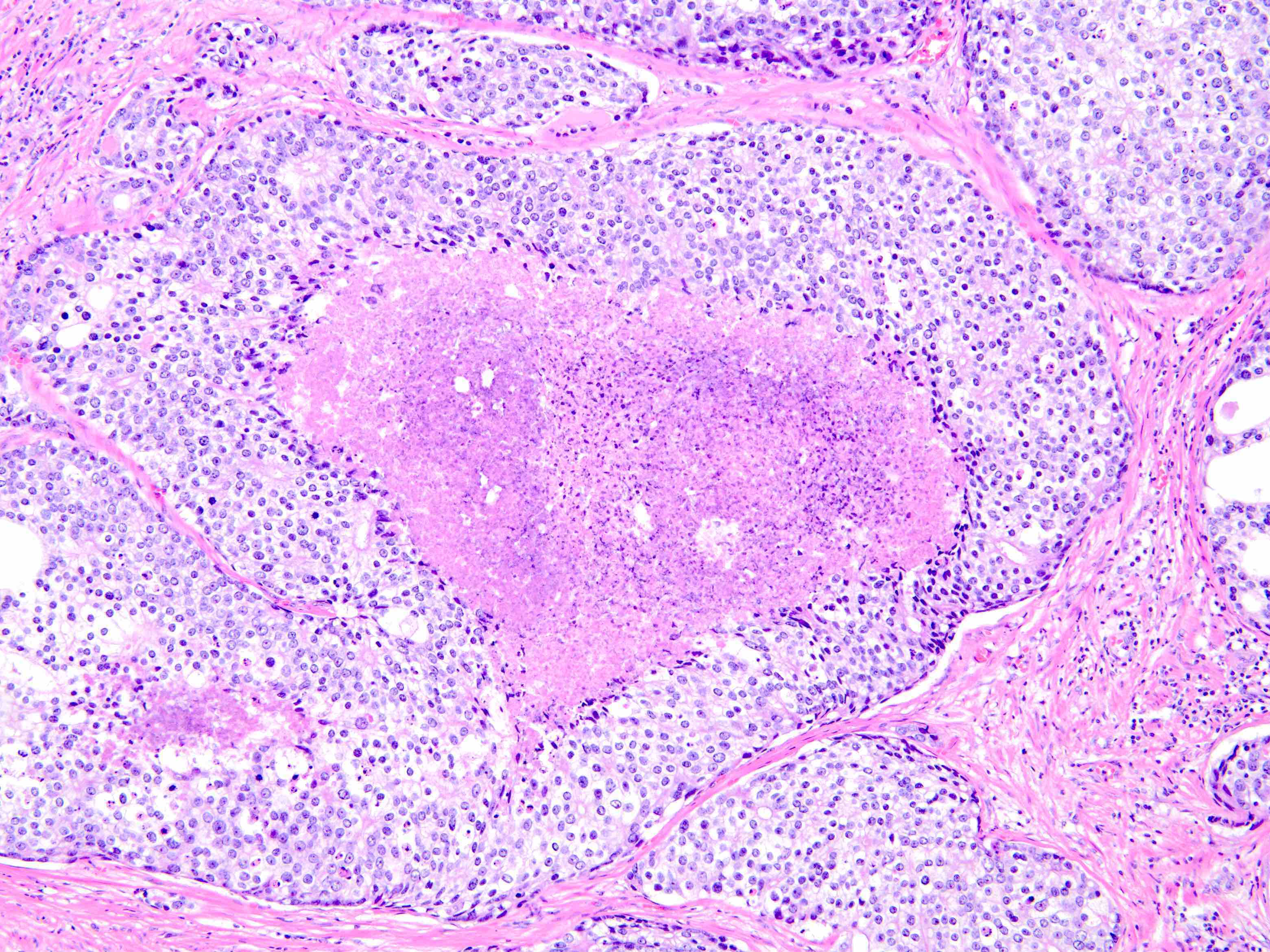
Microscopic (histologic) description
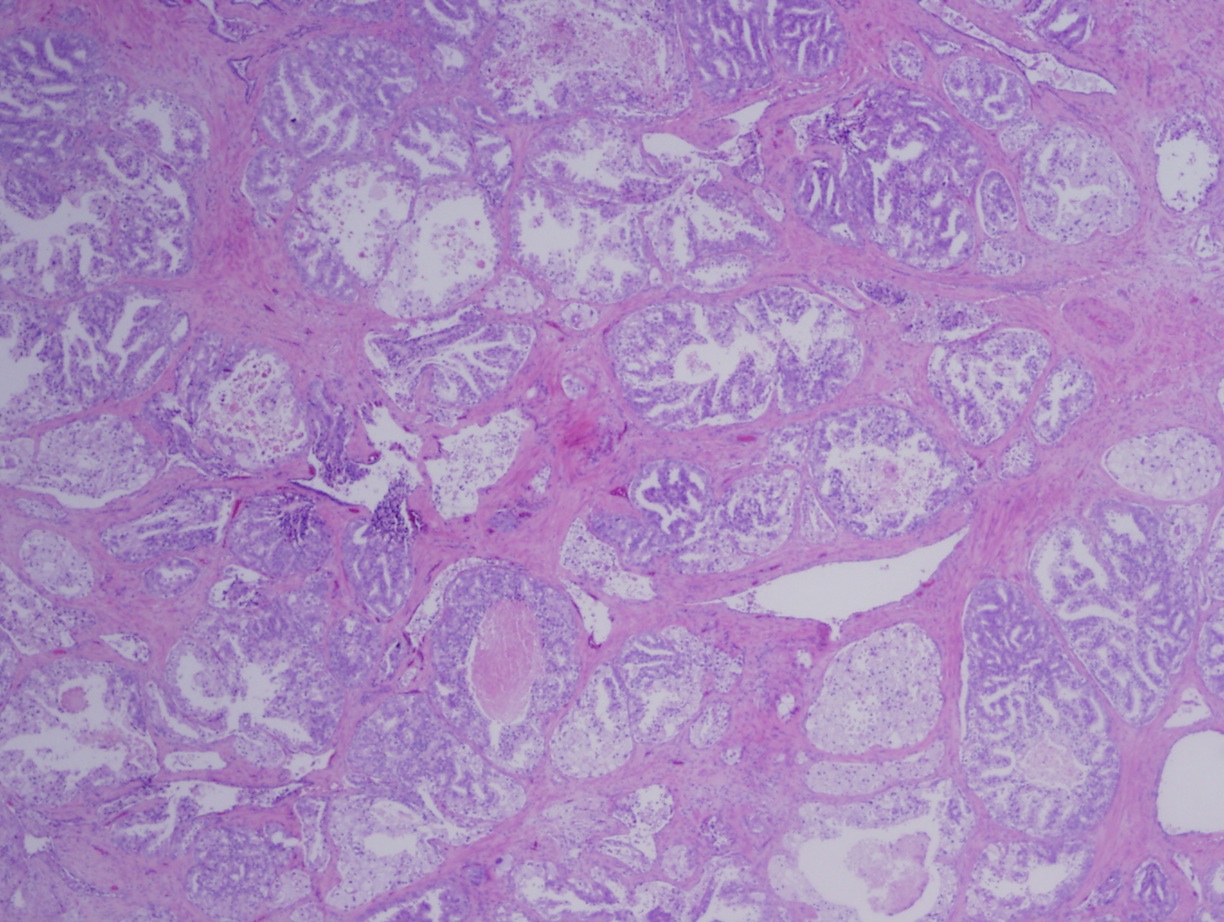
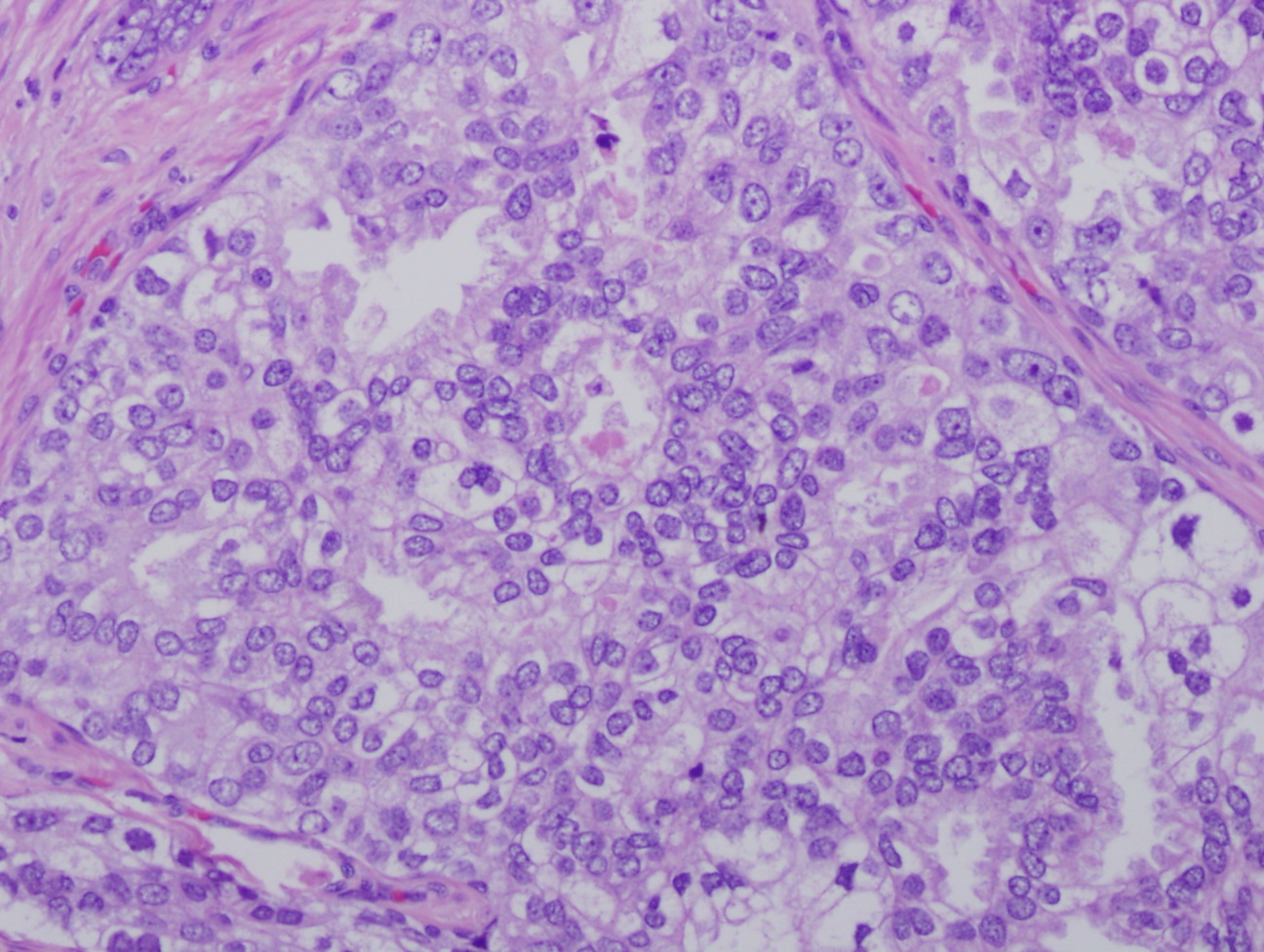
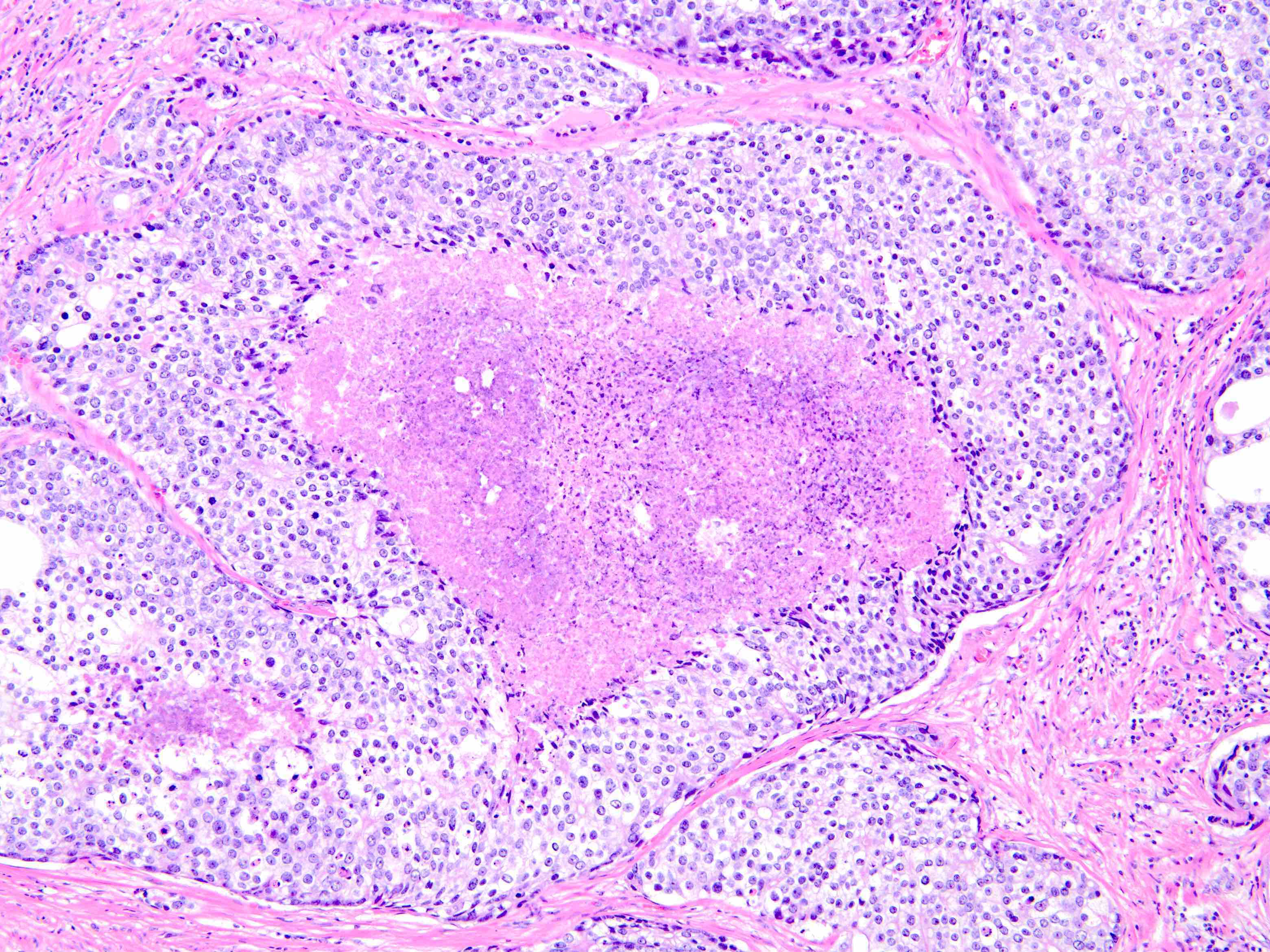
- Basal cells present at periphery of lesion
- Dense cribriform, loose cribriform, solid and micropapillary patterns possible (Mod Pathol 2006;19:1528)
- Various shapes also possible including round, irregular and branching; if diffuse, it is more likely invasive (Pathol Res Pract 2018;214:1681)
- Major criteria (Arch Pathol Lab Med 2015;139:1234):
- Markedly enlarged nuclei (6x normal)
- Nonfocal comedonecrosis
- Solid or dense cribriform architecture
- Minor criteria (Arch Pathol Lab Med 2015;139:1234):
- > 6 glands involved
- Irregular shaped glands with right angle branching
- Frequent / easily identifiable mitoses
- 2 cell populations (mitotically active at periphery and quiescent cells in the center)
- Important to distinguish from invasive carcinoma as this should not be graded
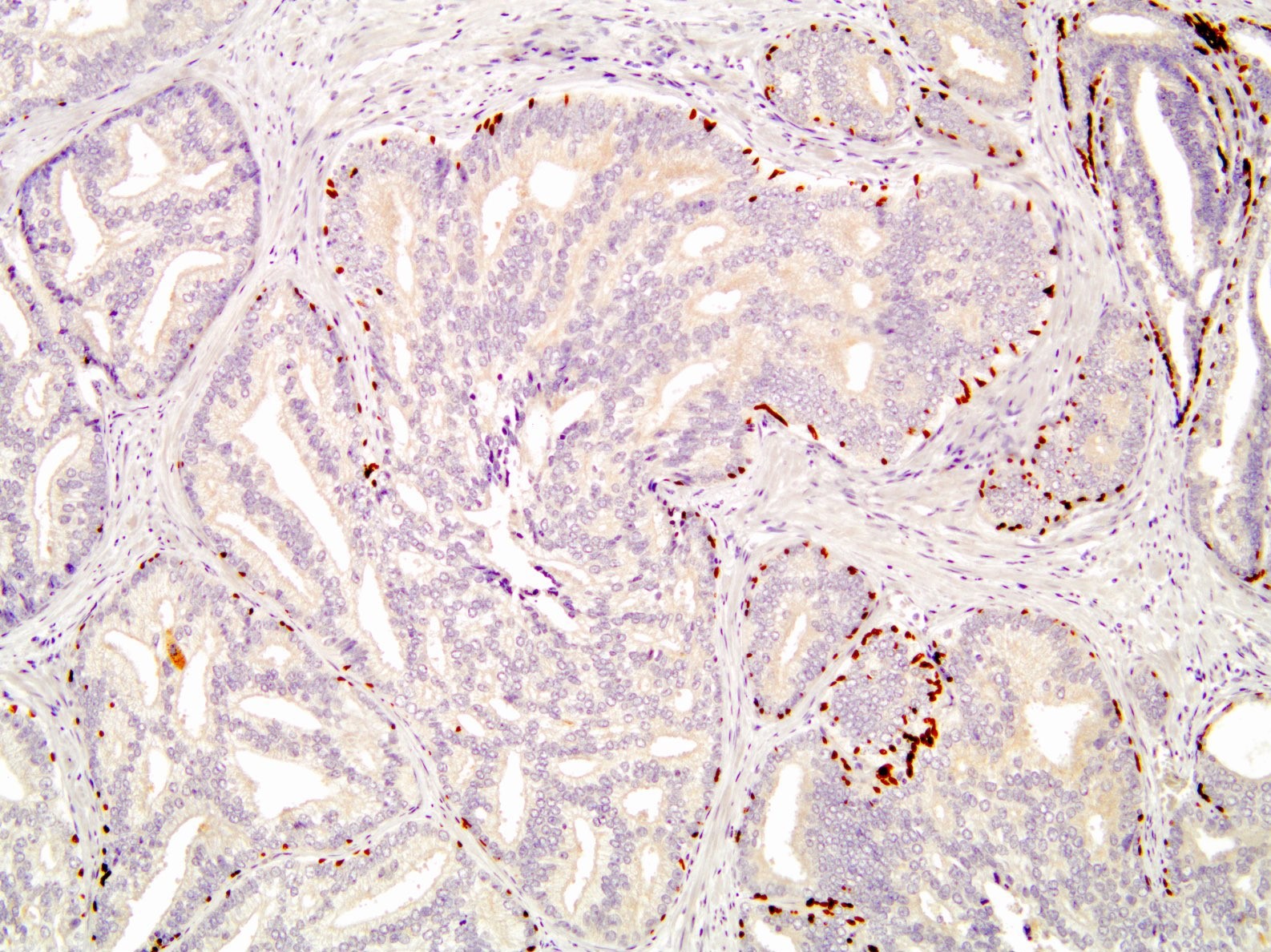
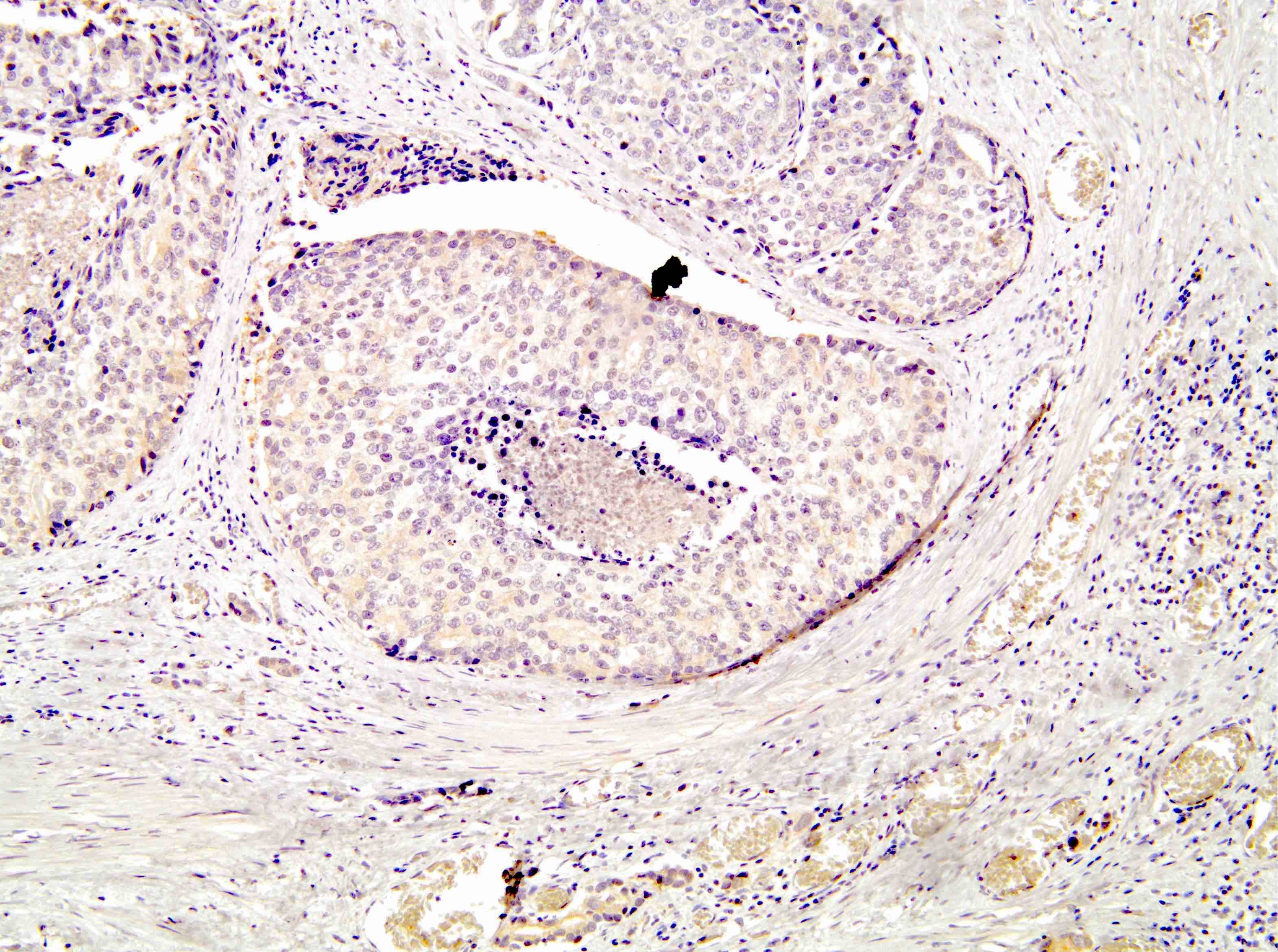
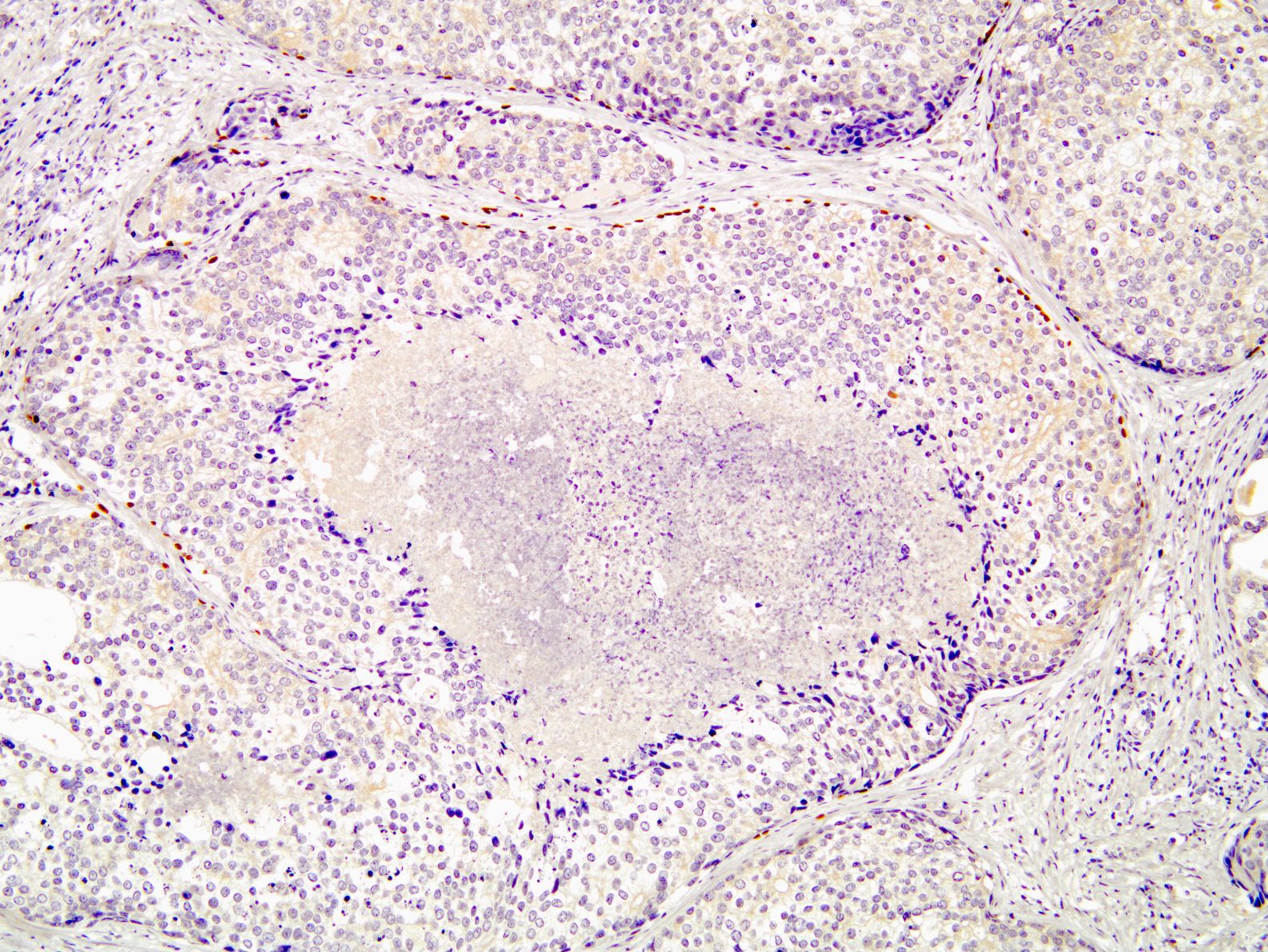
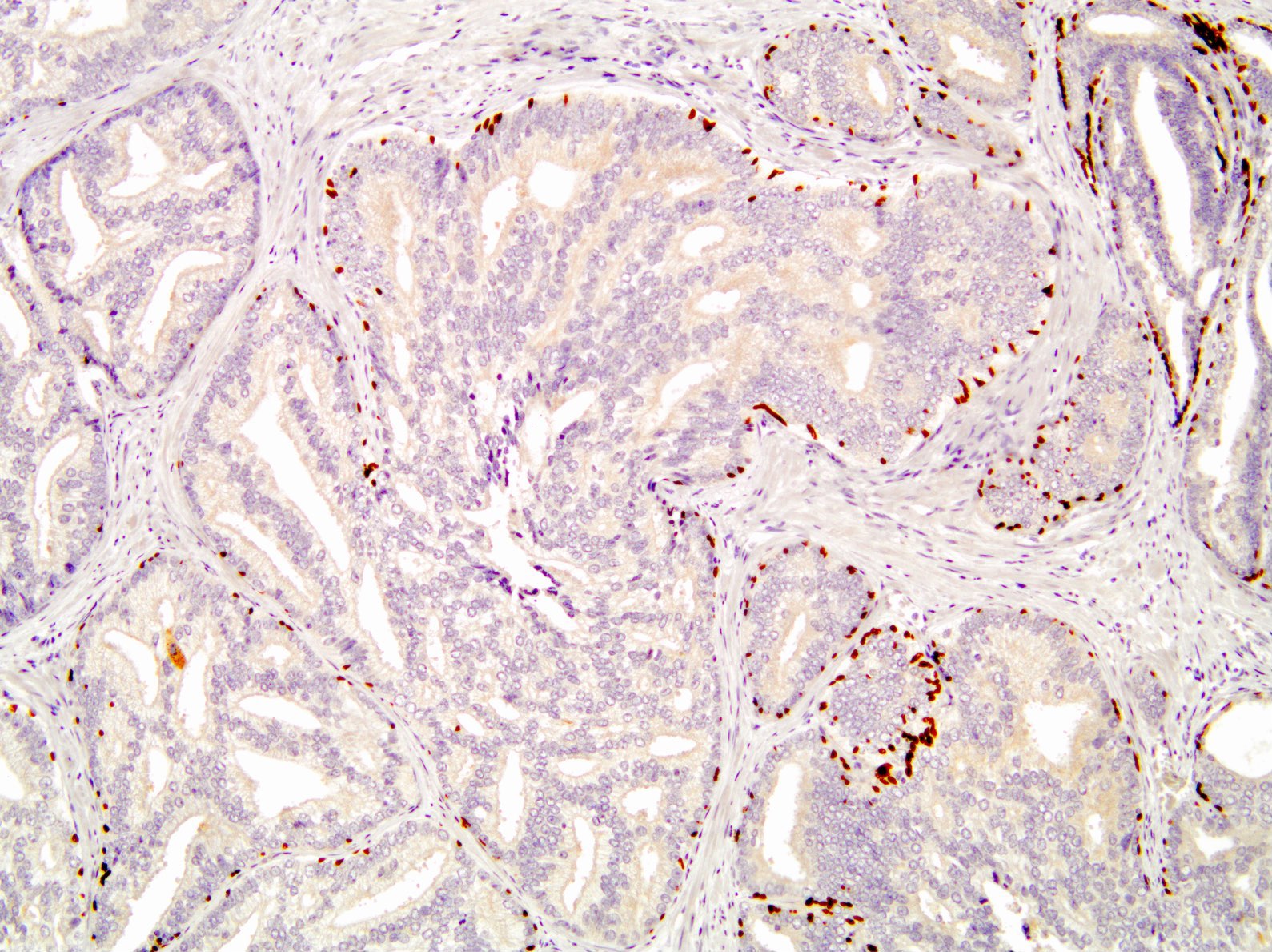
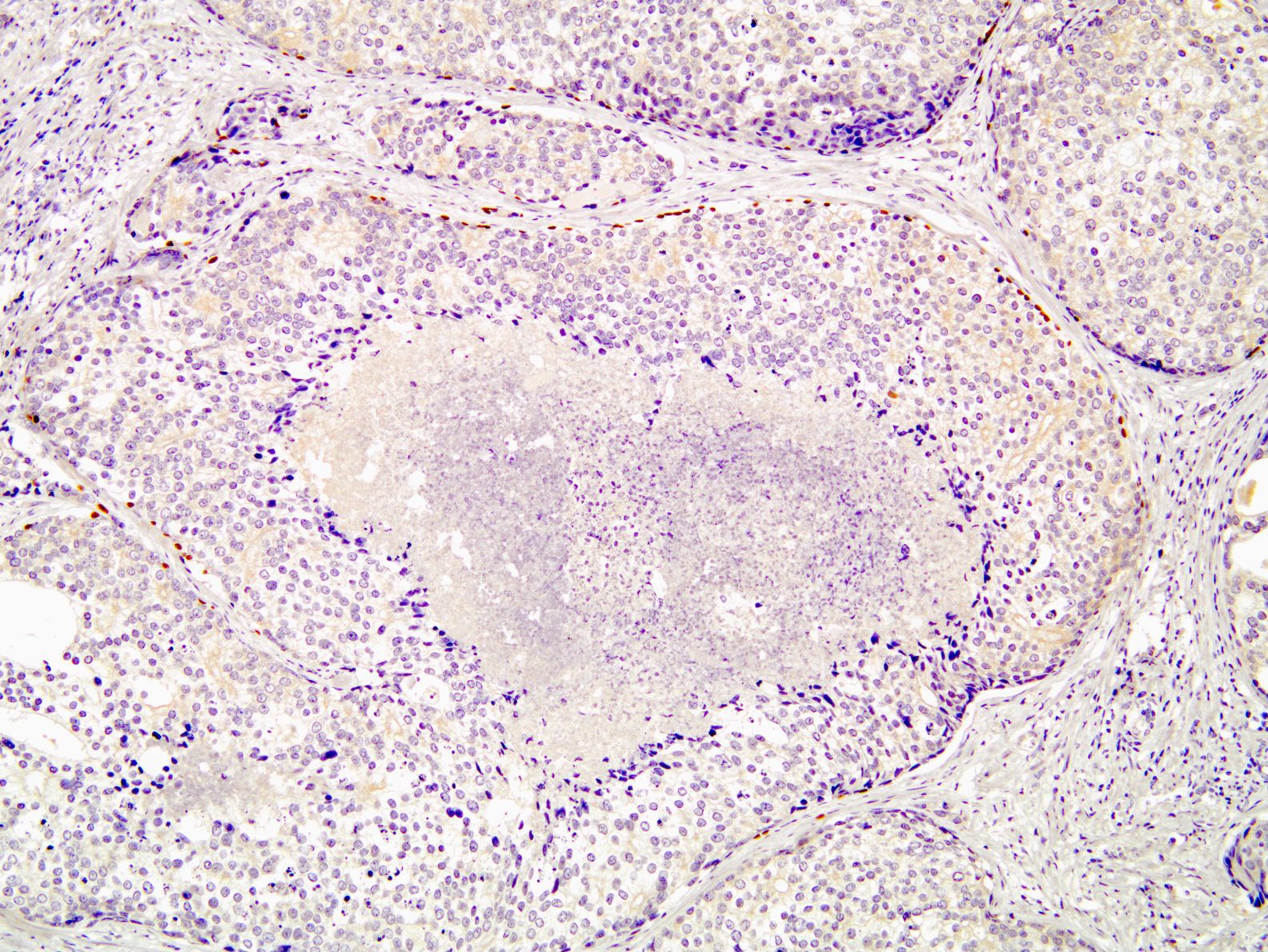
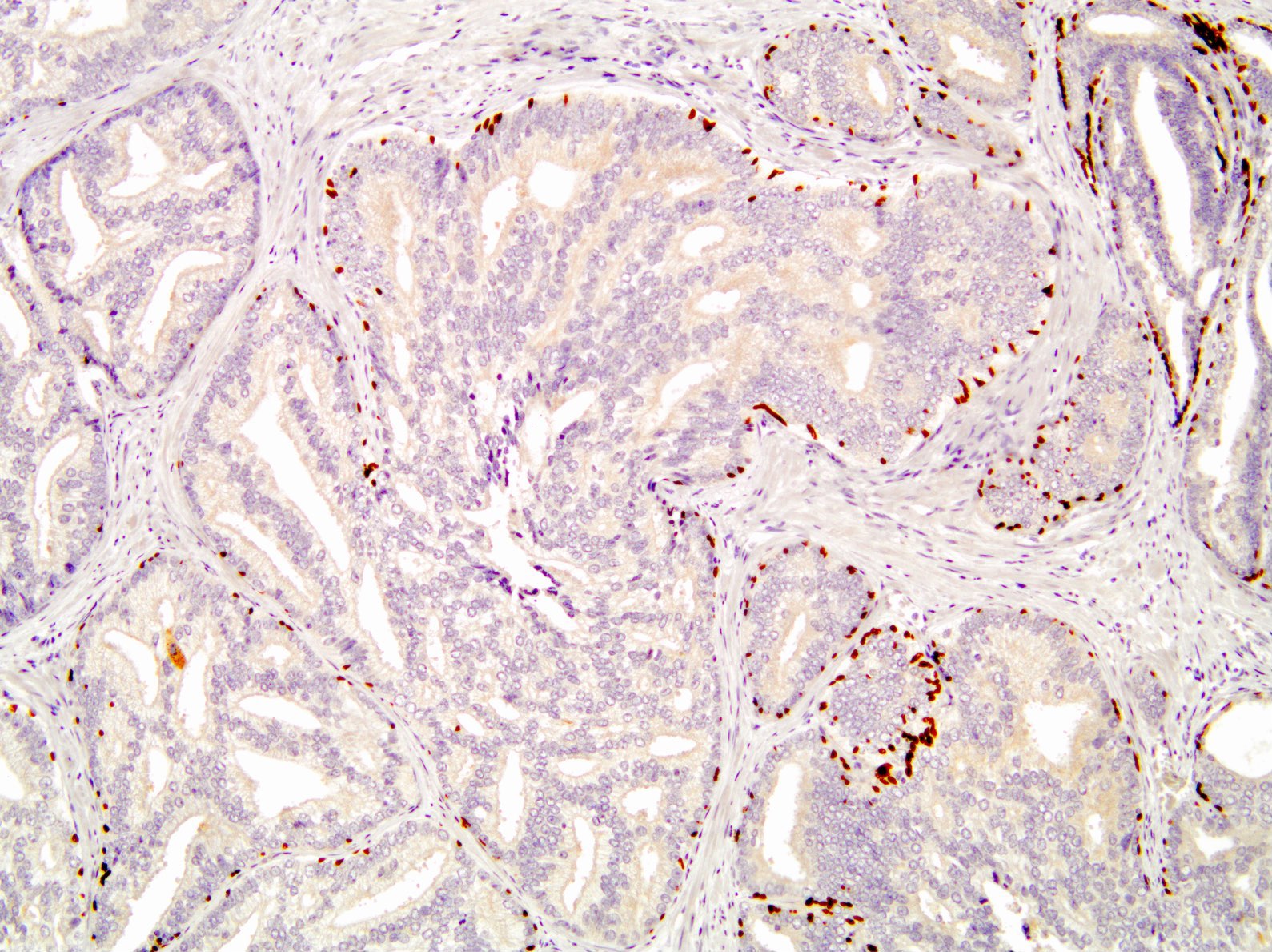
Microscopic (histologic) images
Cytology description
- Cytology not performed for the diagnosis of this disease entity
Positive stains
- p63, CK5/6 and 34betaE12 / HMWCK / high molecular weight highlights basal cells in 100% of cases
- Prostate specific markers such as PSA and PSAP stain acinar cells (Moch: WHO Classification of Tumours of the Urinary System and Male Genital Organs, 4th Edition, 2016)
- Ki67 increased in acinar cells
Negative stains
- PTEN: cytoplasmic loss in 79 - 89% (Mod Pathol 2013;26:587, Prostate 2016;76:394)
Electron microscopy description
- Electron microscopy not used to diagnose this disease entity
Molecular / cytogenetics description
- PTEN deletions detected by molecular analysis in ~50% (Mod Pathol 2013;26:587, Virchows Arch 2019;474:525, J Pathol 2019 Apr 16 [Epub ahead of print])
- ERG fusions detected in ~7% (J Pathol 2019 Apr 16 [Epub ahead of print])
Sample pathology report
- Prostate, core needle biopsy:
- Intraductal carcinoma, involving 1 of 2 cores, 10 mm of 20 mm and 50% of the tissue (see comment)
- Comment: No invasive carcinoma is present. Intraductal carcinoma without evidence of invasive carcinoma is associated with high grade invasive prostatic carcinoma at prostatectomy or repeat biopsy. Clinical and serologic follow up is recommended and a repeat biopsy may be clinically indicated.
- Prostate, core needle biopsy:
- Prostatic adenocarcinoma, Gleason score 3+4=7, involving 1 of 2 cores, measuring 8 mm of 16 mm and 50% of the tissue
- Intraductal carcinoma is present
Differential diagnosis
- High grade prostatic intraepithelial neoplasm:
- Also has retained basal cell layer
- No high grade cytologic atypia
- Clear / vesicular nuclei
- Smaller nuclear size
- Ductal carcinoma of prostate:
- Lacks basal cell layer
- Pseudostratified columnar epithelium with more cytoplasm and tufting
- Infiltrative growth and pagetoid spread common
- High grade invasive acinar prostatic adenocarcinoma:
- Lacks basal cell layer
- Also can have necrosis and cribriform architecture and may grow admixed with intraductal carcinoma
- Urothelial carcinoma in situ within prostatic ducts:
- Also has retained basal cell layer
- Solid growth pattern, lacks cribriform architecture
- Diffusely positive for CK7, p63, GATA3, uroplakin III and negative for PSA (Hum Pathol 2002;33:1136)
- Urothelial carcinoma:
- Lacks basal cell layer
- Solid growth pattern, lacks cribriform architecture
- Greater cytologic atypia and pleomorphism
- More nuclear pleomorphism; nucleoli less uniform; more frequent mitoses
- Diffusely positive for CK7, p63, GATA3, uroplakin III and negative for PSA (Hum Pathol 2002;33:1136)
Board review style question #1
Which of the following is true regarding intraductal carcinoma of the prostate?
- A basal cell layer is not present in intraductal carcinoma
- Intraductal carcinoma is a common finding in prostate biopsies
- Intraductal carcinoma should be graded based on the Gleason pattern scoring system
- PTEN alterations are common in intraductal carcinoma
Board review style answer #1
D. Intraductal carcinoma commonly has loss of PTEN expression seen by immunohistochemistry.
Comment Here
Reference: Intraductal carcinoma
Comment Here
Reference: Intraductal carcinoma
Board review style question #2
A 65 year old man had a radical prostatectomy for invasive carcinoma found on prostate biopsy. What does the following finding on histology predict about this patient's clinical course?
- The patient has a higher probability of biochemical recurrence
- The patient is cured with prostatectomy alone
- The patient was overtreated as he did not need a prostatectomy
- The patient will do the same as other patients within his same grade group without this finding
Board review style answer #2
A. This is prostatic intraductal carcinoma. The patient has a higher probability of biochemical recurrence. Patients with intraductal carcinoma have higher pT category, higher grade tumors with higher likelihood of biochemical recurrence when matched for grade group.
Comment Here
Reference: Intraductal carcinoma
Comment Here
Reference: Intraductal carcinoma