Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sanguedolce F. Nonspecific granulomatous prostatitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostategranprost.html. Accessed April 20th, 2024.
Definition / general
- Granulomatous inflammation of the prostate not associated with specific causes, such as biopsy, transurethral resection, tuberculosis (TB), fungi infection or Bacillus Calmette-Guérin (BCG) treatment
- Though uncommon, nonspecific granulomatous prostatitis (NSGP) is the most frequent granulomatous inflammatory condition of the prostate, accounting for more than half of cases of prostatic granulomatous inflammation (Zhou: Genitourinary Pathology, 2nd Edition, 2015)
Essential features
- Mixed, mostly chronic granulomatous inflammation (epithelioid histiocytes, giant cells, lymphocytes, plasma cells and other inflammatory cells)
- No specific etiology can be established on the basis of clinical and serological findings
ICD coding
Epidemiology
- NSGP accounts for ~70% of all cases of granulomatous prostatitis (Int J Urol 2005;12:474, Ultraschall Med 2005;26:203)
- NSGP is present in < 1% of needle biopsies (Zhou: Genitourinary Pathology, 2nd Edition, 2015)
Sites
- Prostate
Pathophysiology
- Prominent inflammatory reaction to extravasated prostatic fluid containing bacterial toxins and cell debris within the prostate
Etiology
- NSGP is most likely caused by the blockage of prostatic ducts (possibly due to benign prostatic hyperplasia) and associated inflammation, which can cause epithelial disruption and damage
- Cellular debris and prostatic secretion leaking into the stroma induce a granulomatous inflammatory reaction, which is typically centered around the ruptured ducts or acini (Zhou: Genitourinary Pathology, 2nd Edition, 2015)
Clinical features
- May be highly suspicious for prostate cancer (Arch Pathol Lab Med 1997;121:724)
- Serum prostate specific antigen (PSA) is frequently elevated, up to 10 - 15 ng/mL
- Hypoechoic region can be seen on transrectal ultrasound
- ~50% are symptomatic with irritation, fever or chills
- Some patients have symptoms of urinary obstruction or hematuria (Epstein: Biopsy Interpretation of the Prostate, 5th Edition, 2014)
Diagnosis
- Digital rectal examination: the prostate is firm, symmetrically or asymmetrically indurated
- Multiparametric MRI (mpMRI): findings are often suspicious for carcinoma, hence pathology is the gold standard in disease diagnosis (Diagnostics (Basel) 2022;12:2302)
Case reports
- 54 year old man with lower urinary tract symptoms, PSA of 8.0 ng/mL and asymmetric prostate enlargement with a prominent, firm, right prostate lobe on digital rectal examination (Radiol Case Rep 2016;11:78)
- 55 year old man with left flank pain and mild lower urinary tract symptoms, PSA of 12.48 ng/mL and extensive low signal in the peripheral zone bilaterally on mpMRI (J Clin Urol 2020;15:141)
- 71 year old man with PSA of 6.70 ng/mL, a focal area of fixed induration involving the right lobe on digital rectal examination and a 4 cm nodular lesion characterized by low signal intensity on T2 weighted sequences, involving both the peripheral and transition zone of the right lobe with extension to the peripheral zone of the mid basal left lobe on mpMRI (Future Sci OA 2020;6:FSO591)
Treatment
- Can be self limiting
- Generally treated with antibiotics and steroids
- Transurethral prostatic resection (TURP) or other surgical procedures may be needed in case of persistent clinical symptoms of urinary obstruction (Zhou: Genitourinary Pathology, 2nd Edition, 2015)
Gross description
- Prostate is often small, firm, gray-yellow and nodular
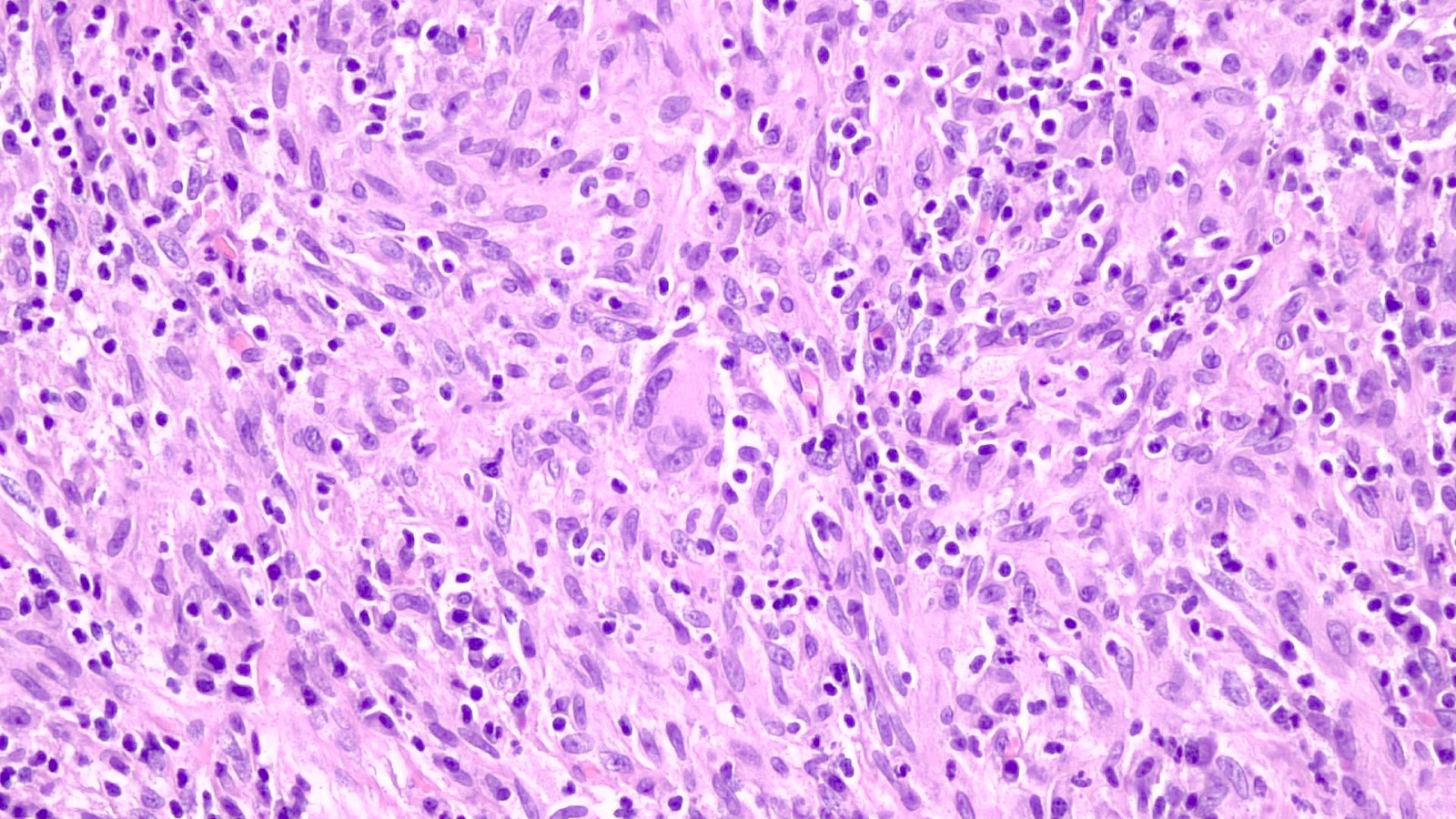
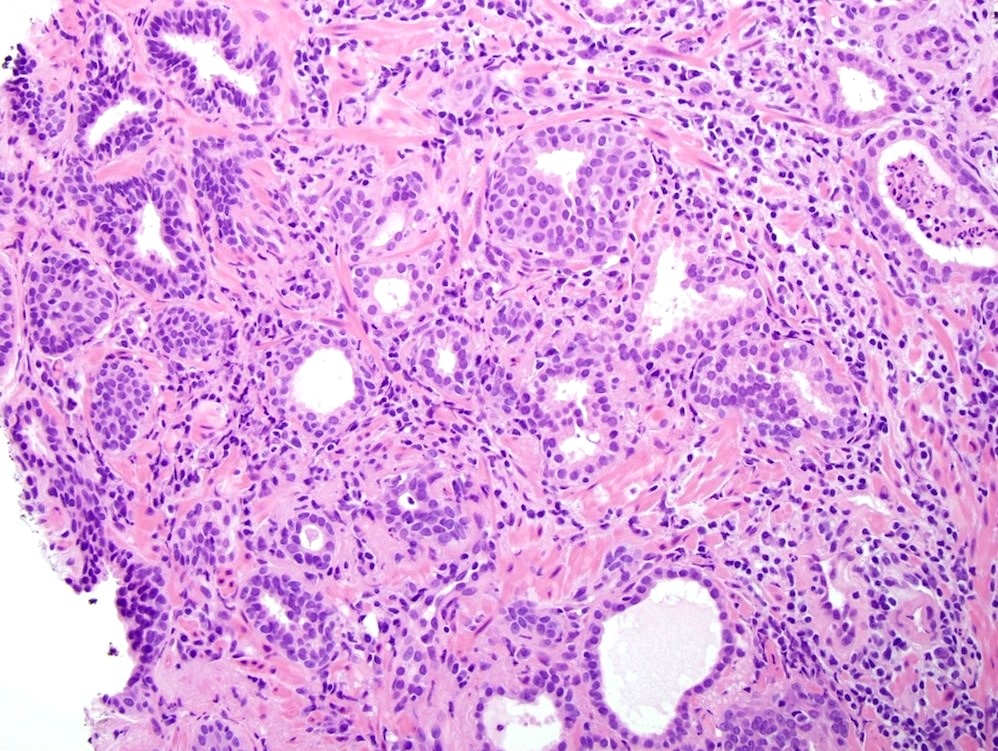
Microscopic (histologic) description
- NSGP is generally a diffuse process
- Inflammation often presents as poorly defined, expansile nodular infiltrates, usually involving entire lobules
- In the early phase, acute inflammation or microabscesses are present within the ducts or acini, which in turn are often filled with sloughed epithelial cells
- Subsequently, rupture and destruction of the epithelial lining occur, hence the inflammatory reaction is centered on ruptured glandular structures
- In the later stage, parenchymal loss, stromal fibrosis and sclerosis and chronic inflammation become prominent and giant cells are occasionally seen
- Granulomas are composed predominantly of epithelioid histiocytes, lymphocytes and plasma cells, with sometimes intermixed scattered neutrophils and eosinophils, foamy macrophages and multinucleated foreign body giant cells
- These granulomas are typically poorly formed and noncaseating
- Cytologic atypia can be seen in the reactive glandular cells, which may resemble adenocarcinoma (Am J Clin Pathol 1991;95:330)
- In rare cases, adenocarcinoma may coexist with NSGP and tumor cells and glands may be obscured by the overt inflammation (Ann Diagn Pathol 2004;8:242)
Microscopic (histologic) images
Positive stains
- CD68 (KP1), CD163 stain the histiocytes
Negative stains
- Cytokeratin AE1 / AE3, CAM5.2, pancytokeratin, PSA, PSAP, AMACR (in order to rule out carcinoma) (Zhou: Genitourinary Pathology, 2nd Edition, 2015)
- PAS, Grocott methenamine silver (GMS) and acid fast bacilli (AFB) histochemical stains (in order to rule out infections)
- Calcium and iron histochemical stains (in order to rule out malakoplakia)
Sample pathology report
- Prostate, biopsy / transurethral resection:
- Idiopathic (nonspecific) granulomatous inflammation
Differential diagnosis
- Prostate adenocarcinoma:
- Prostatic epithelial cells may feature reactive and regenerative changes
- Tumor cells with foamy cytoplasm may mimic lipid laden epithelioid histiocytes (Mod Pathol 2018;31:S64)
- Tumor cells show nuclear atypia, lack basal cells and are positive for AMACR
- BCG induced granulomas (Clin Imaging 2012;36:413):
- History of high grade nonmuscle invasive bladder cancer treated with BCG instillations
- Caseating granulomas
- Postbiopsy / posttransurethral resections granulomas:
- Fibroid central geographic necrosis, foreign body giant cells
- Infectious prostatitis:
- Positive Grocott methenamine silver (GMS) / AFB stains
- Malakoplakia:
Additional references
Board review style question #1
Board review style answer #1
A. Multinucleated giant cell. Such cells result from the fusion of several histiocytes within a granulomatous inflammation. Answers B - D are incorrect because osteoclasts, syncytiotrophoblasts and sometimes neoplastic cells may be multinucleated, yet they would be found in different places (bone tissue, placenta and tumors, respectively).
Comment Here
Reference: Nonspecific granulomatous prostatitis
Comment Here
Reference: Nonspecific granulomatous prostatitis
Board review style question #2
In cases of nonspecific granulomatous prostatitis (NSGP), which stain(s) can be used to rule out malakoplakia?
- AMACR
- Calcium and iron histochemical stains
- Grocott methenamine silver (GMS) and acid fast bacilli (AFB) stains
- Pancytokeratins
Board review style answer #2
B. Calcium and iron histochemical stains. Malakoplakia is positive for calcium and iron histochemical stains, while NSGP is not. Answers D and A are incorrect because immunohistochemical markers (pancytokeratins and AMACR) may be useful to distinguish NSGP from carcinoma. Answer C is incorrect because negativity for GMS and AFB stains rule out infective prostatitis.
Comment Here
Reference: Nonspecific granulomatous prostatitis
Comment Here
Reference: Nonspecific granulomatous prostatitis