Table of Contents
Definition / general | ICD coding | Epidemiology | Etiology | Clinical features | Diagnosis | Laboratory findings / pleural fluid measurements | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Immunohistochemical stains (positive and negative stains) | Special stains | Electron microscopy description | Molecular / cytogenetics description | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Vickery J, Husain AN. Mesothelioma versus adenocarcinoma (pleura). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/pleuramesovsadeno.html. Accessed April 2nd, 2025.
Definition / general
- Mesothelial proliferations are a spectrum of benign to malignant lesions of the lining of the serosal cavities
- Adenocarcinoma is a malignant epithelial neoplasm with glandular differentiation
ICD coding
Epidemiology
- Age and gender are unreliable distinguishing factors, as both tumors have a slight male predominance and peak incidence in patients over 65
- History of asbestos exposure should not be taken into consideration by the pathologist when confirming or excluding mesothelioma; diagnosis should be made using morphology and immunohistochemical studies (Arch Pathol Lab Med 2009;133:1317)
- Unlike adenocarcinoma, tobacco is not implicated in the causation of mesothelioma; however, tobacco (especially cigarette) smoke and asbestos can synergistically interact in the causation of lung cancer (Int J Environ Res Public Health 2019;17:258)
- Etiologies and epidemiology for metastases are dependent on site of origin
Etiology
- See epidemiology
Clinical features
- Wide variety of symptoms can lead to a diagnosis of lung cancer and are not specific to a pathologic entity
- Presenting symptoms include chest wall pain (unilateral or bilateral), pleurisy, cough and progressive dyspnea secondary to pleural effusion (Surg Pathol Clin 2020;13:73)
- Both commonly present with insidious onset of chest pain or dyspnea
- Other site specific symptoms may or may not be present in patients with metastatic carcinoma
Diagnosis
- In the initial evaluation of patients with suspected malignant pleural mesothelioma, radiological imaging is essential
- Computed tomography (CT) of the chest is the primary imaging modality but magnetic resonance imaging (MRI) and positron emission tomography (PET) can provide additional information for surgical planning (Radiographics 2004;24:105)
- Further investigation of suspected malignant pleural mesothelioma includes thoracentesis of any existing pleural effusion with cytological examination and closed pleural biopsy
- If there is not enough tissue to reliably distinguish mesothelioma and adenocarcinoma on closed pleural biopsy, surgical intervention via video assisted thoracoscopic, biopsy or open thoracotomy can be pursued (Eur Respir Rev 2016;25:472)
- Concurrent bronchoscopy at the time of surgery can also be considered, as endobronchial lesions are typically not seen in mesothelioma and their presence argues against this diagnosis (Tuberc Respir Dis (Seoul) 2015;78:297)
Laboratory findings / pleural fluid measurements
- High levels of hyaluronic acid (concentrations exceeding 100,000 ng/ml) are suggestive of mesothelioma (Respir Investig 2013;51:92)
- Carcinoembryonic antigen elevation (CEA) in both serum and malignant pleural effusions has been associated with pulmonary adenocarcinoma (J Thorac Dis 2018;10:E340)
- When malignant pleural effusions occur in either mesothelioma or adenocarcinoma, they are typically exudative effusions (Dtsch Arztebl Int 2019;116:377)
Radiology description
- Mesothelioma
- Most often presents with unilateral disease
- Diffuse thick rind-like or nodular pleural thickening which may extend into the lung (Indian J Radiol Imaging 2013;23:313)
- May be associated with unilateral pleural effusion and ipsilateral lung volume loss
- Adenocarcinoma of lung / metastatic carcinoma
- Lung primary: main finding is a lung mass / nodule which may extend to the pleura
- Metastatic adenocarcinoma: often multiple nodules in the lung or pleura
- Pitfalls
- Both may have bilateral disease or mediastinal lymph node involvement
- Mesothelial diaphragmatic invasion with liver involvement can mimic a primary liver tumor
Radiology images
Prognostic factors
- 75% of mesotheliomas are detected at stage III - IV at diagnosis
- CT screening detected adenocarcinoma is usually at an earlier stage and has a better prognosis (J Natl Compr Canc Netw 2018;16:412)
- Metastatic adenocarcinoma, is, by definition, high stage and has poor prognosis
Case reports
- 45 year old woman with pleural epithelioid mesothelioma and ALK translocation with response to targeted immunotherapy (Lung Cancer 2020;142:47)
- 61 year old man with pleural fluid asbestos bodies and lung adenocarcinoma (Rom J Morphol Embryol 2016;57:1171)
- 70 year old man with concurrent mesothelioma and lung adenocarcinoma (Respir Med Case Rep 2018;26:45)
Treatment
- Surgical management depends on stage and resectability of the tumor
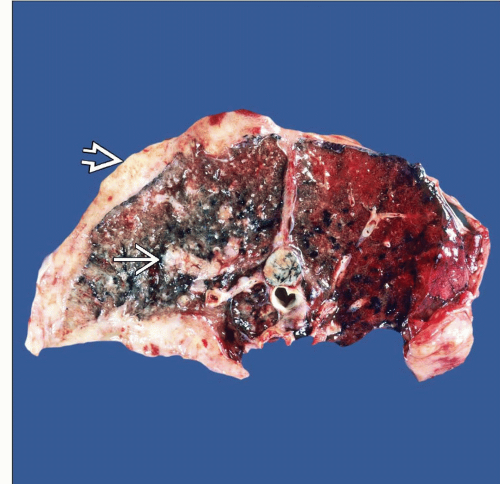
Gross description
- Diffuse pleurotropic growth pattern is most common in mesothelioma (J Carcinog 2008;7:3)
- Peripheral adenocarcinoma encasing the lung, so called pseudomesotheliomatous growth, will usually have a component involving the lung parenchyma
Gross images
Frozen section description
- There are no distinctive features that distinguish mesothelioma and adenocarcinoma on frozen section
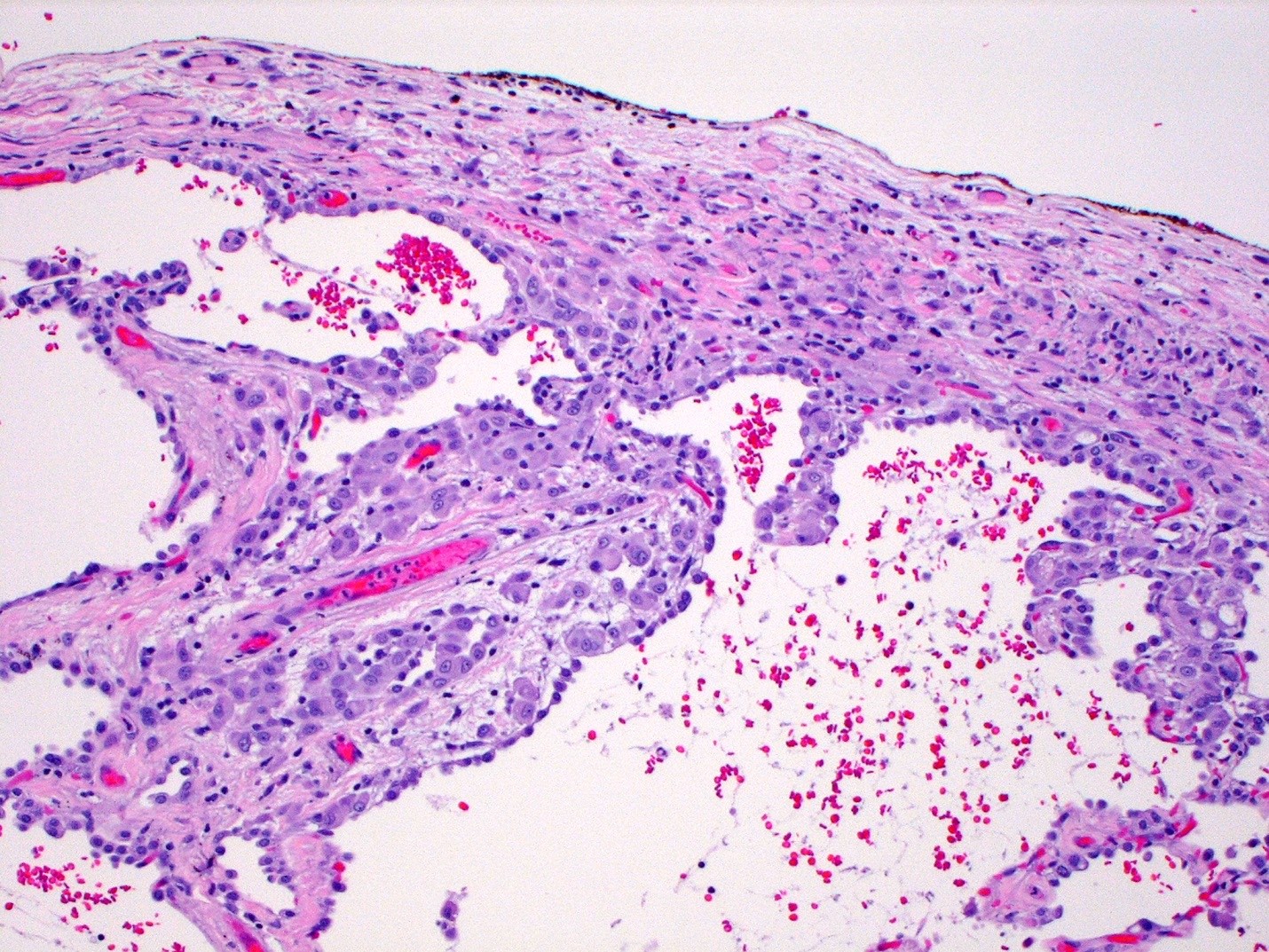
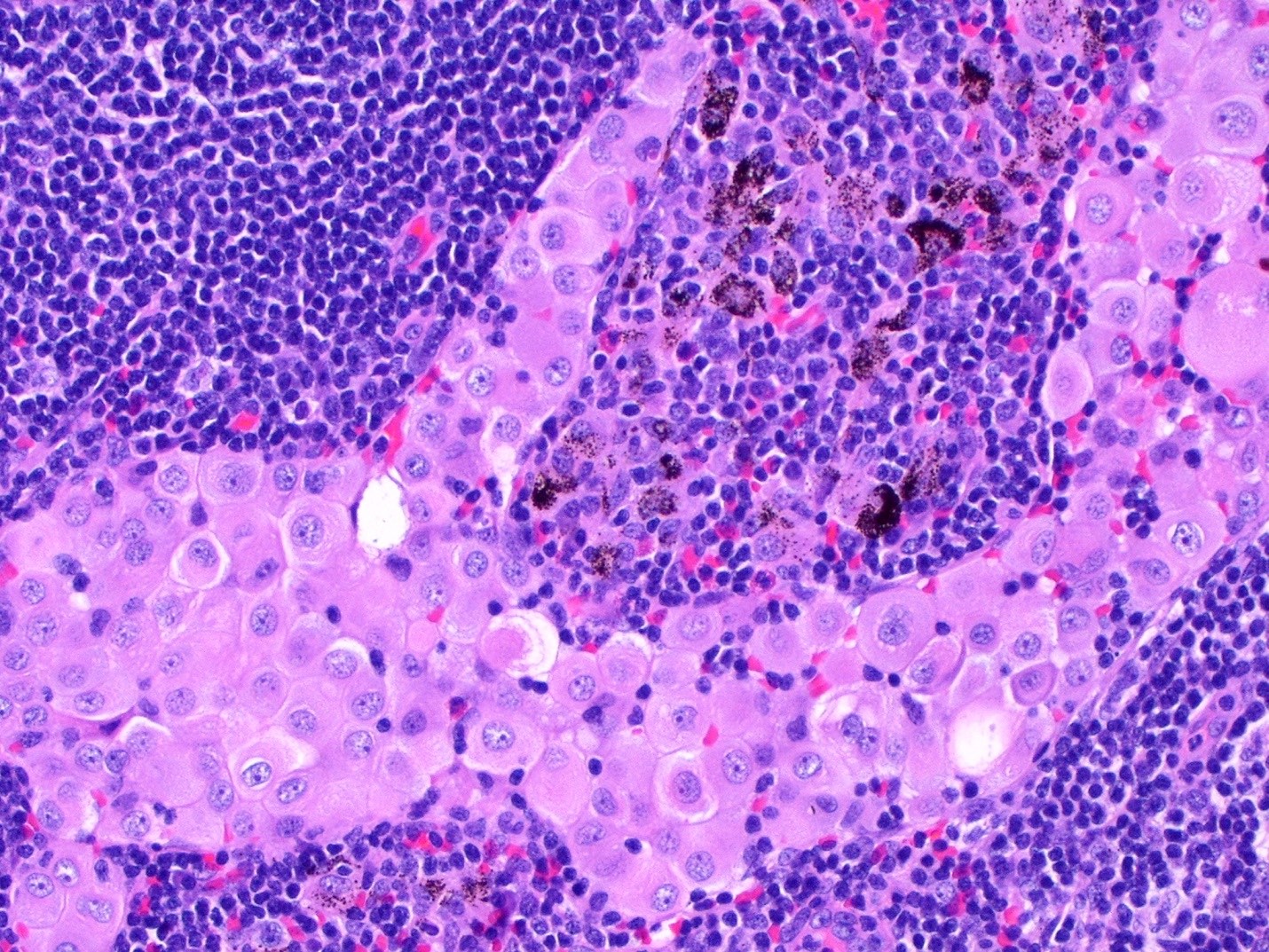
Microscopic (histologic) description
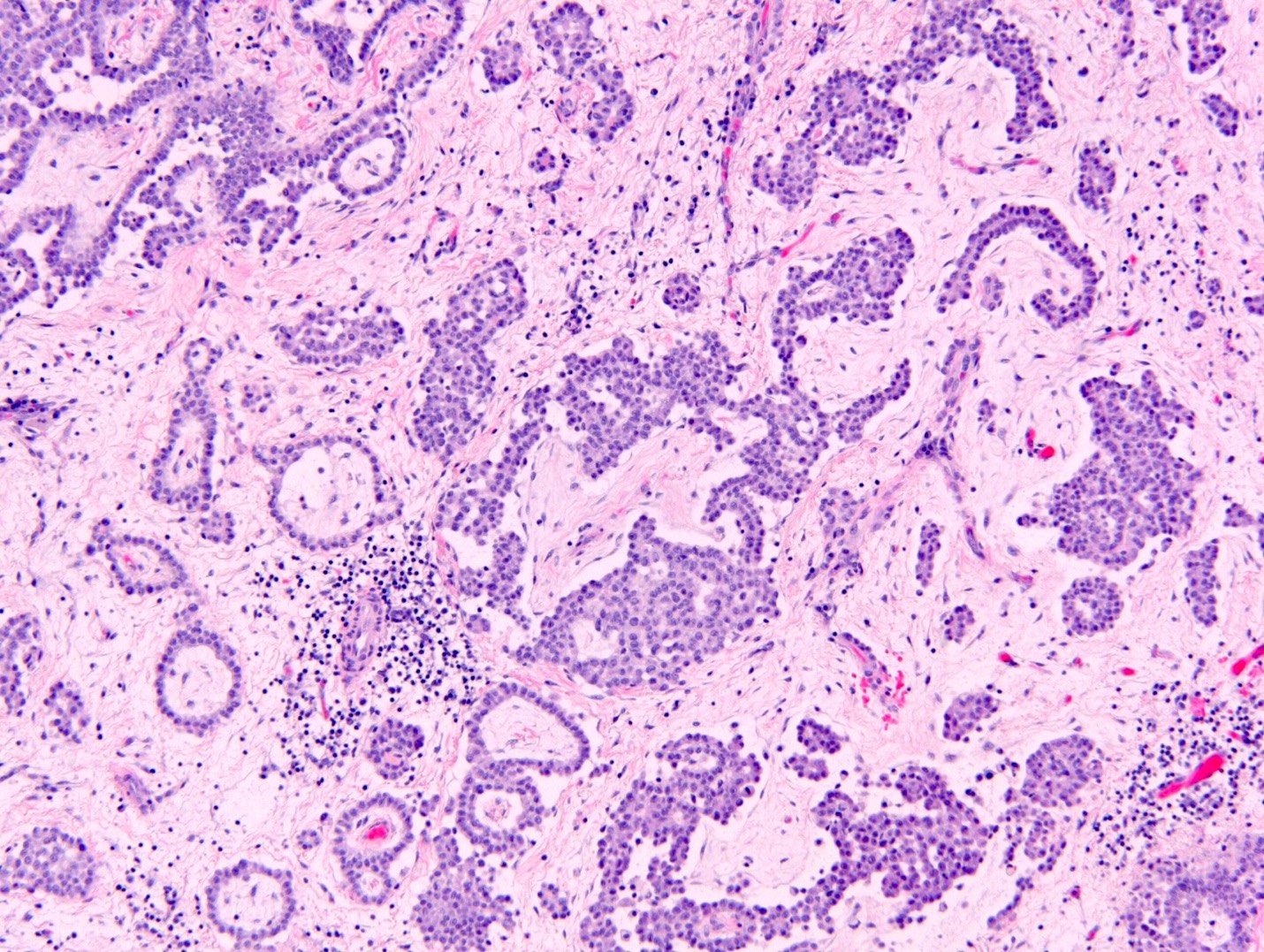
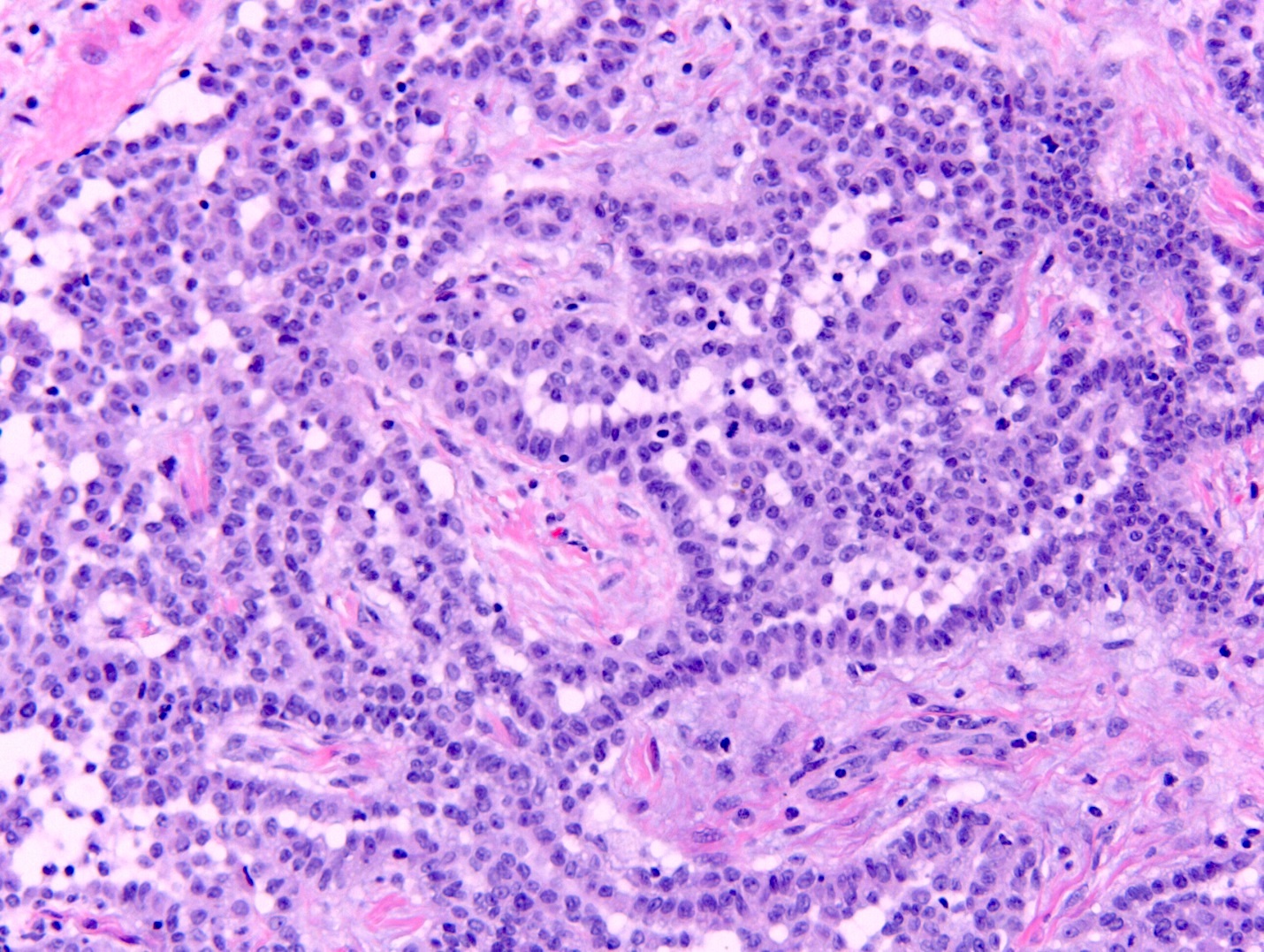
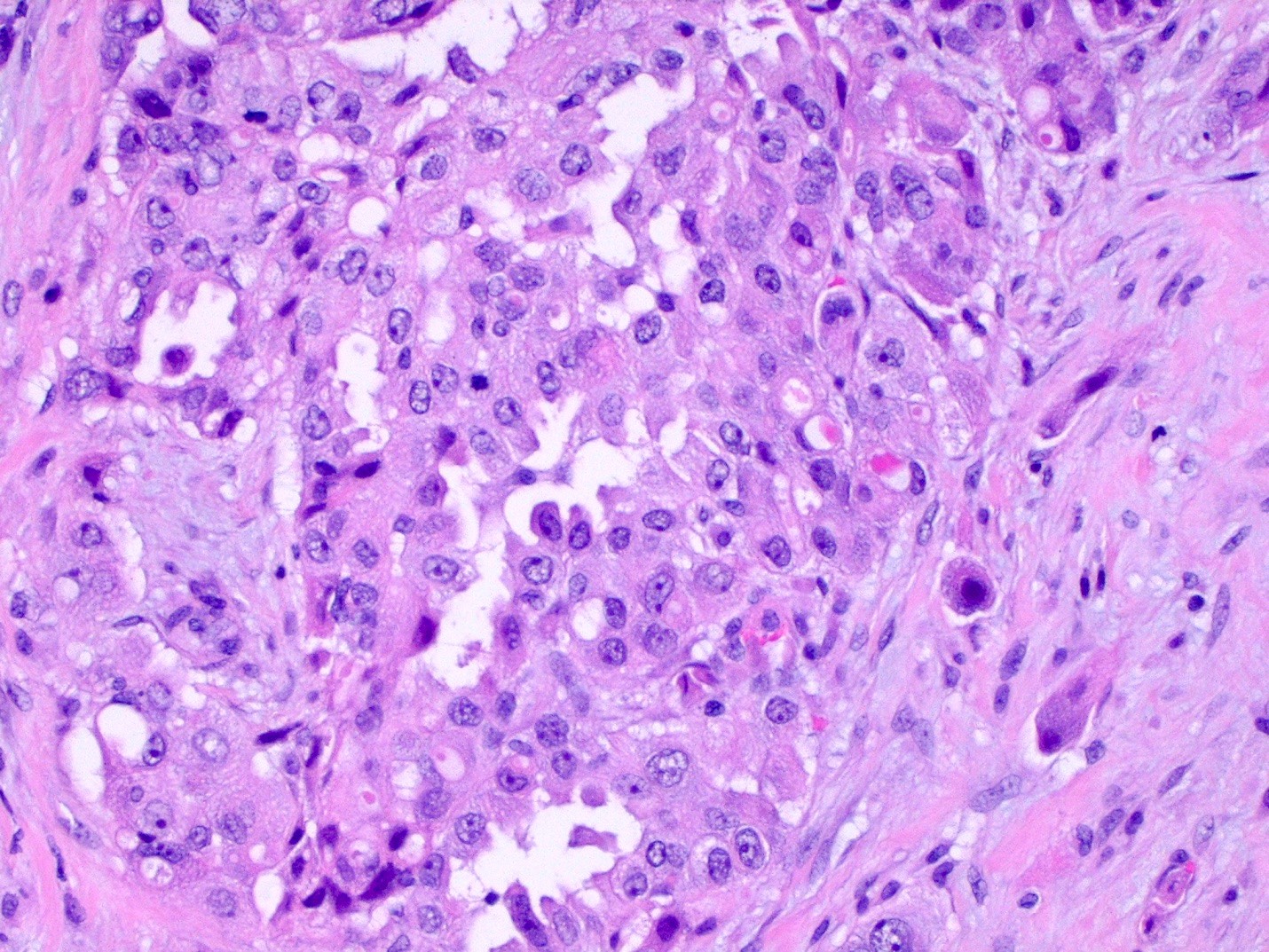
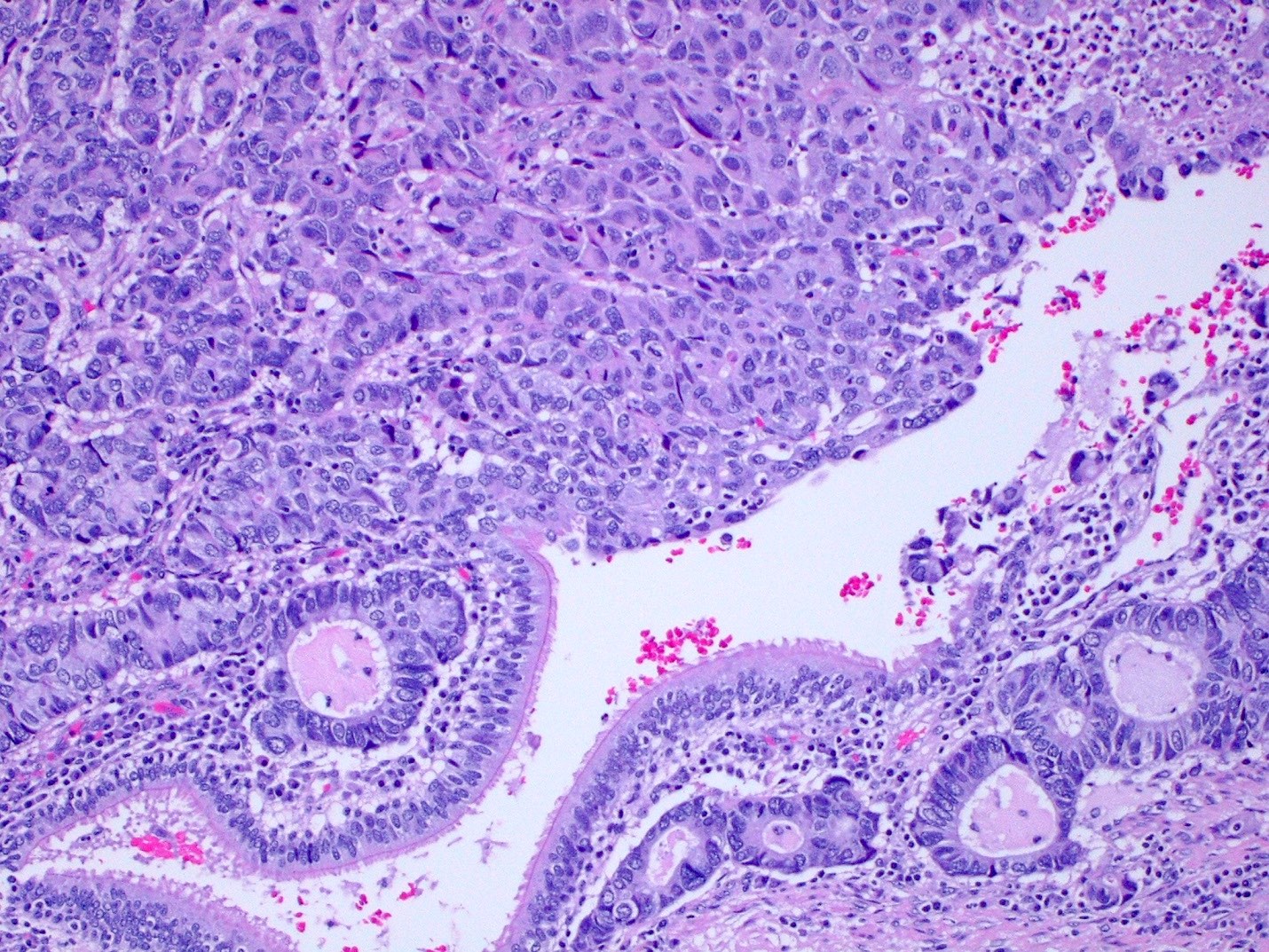
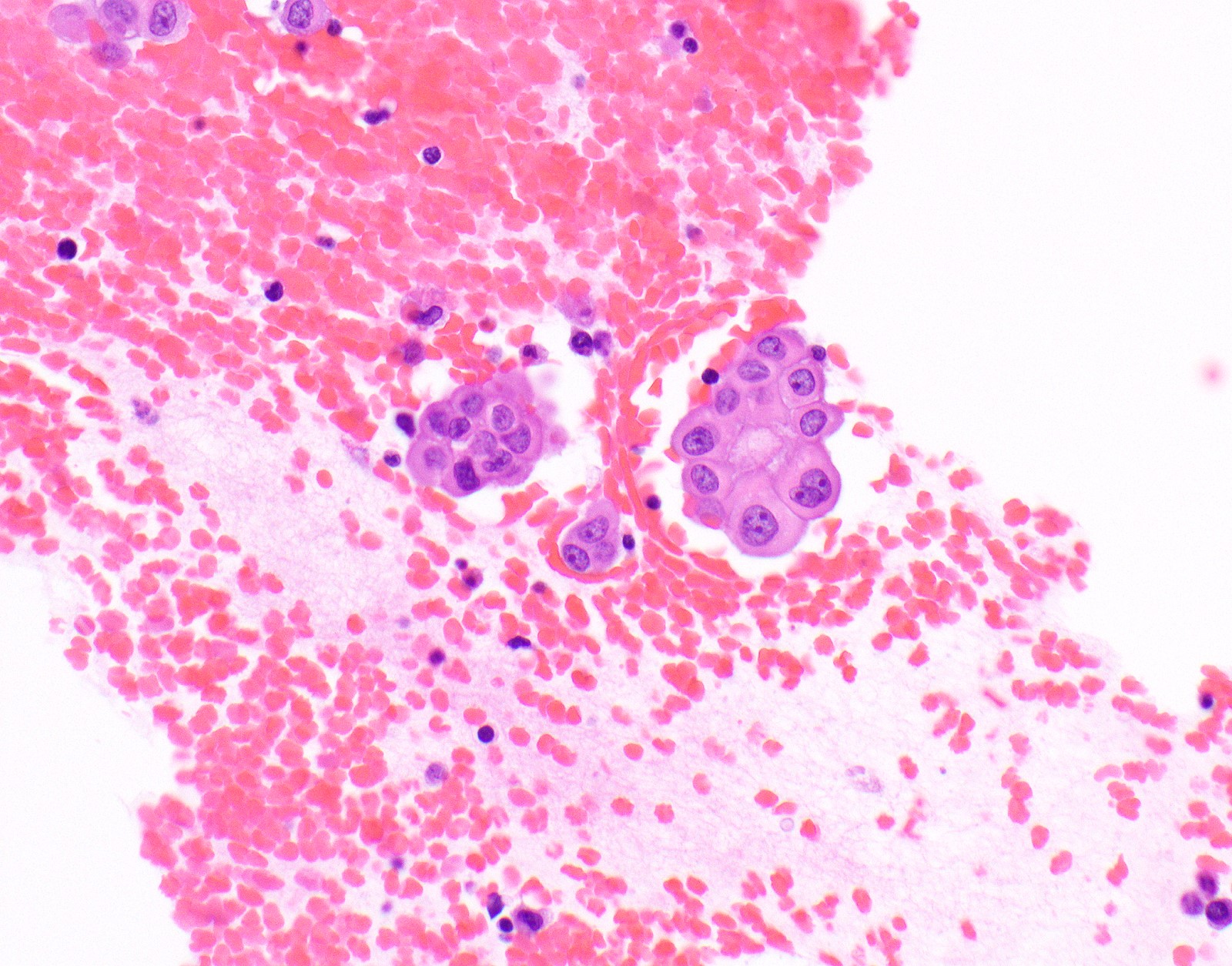
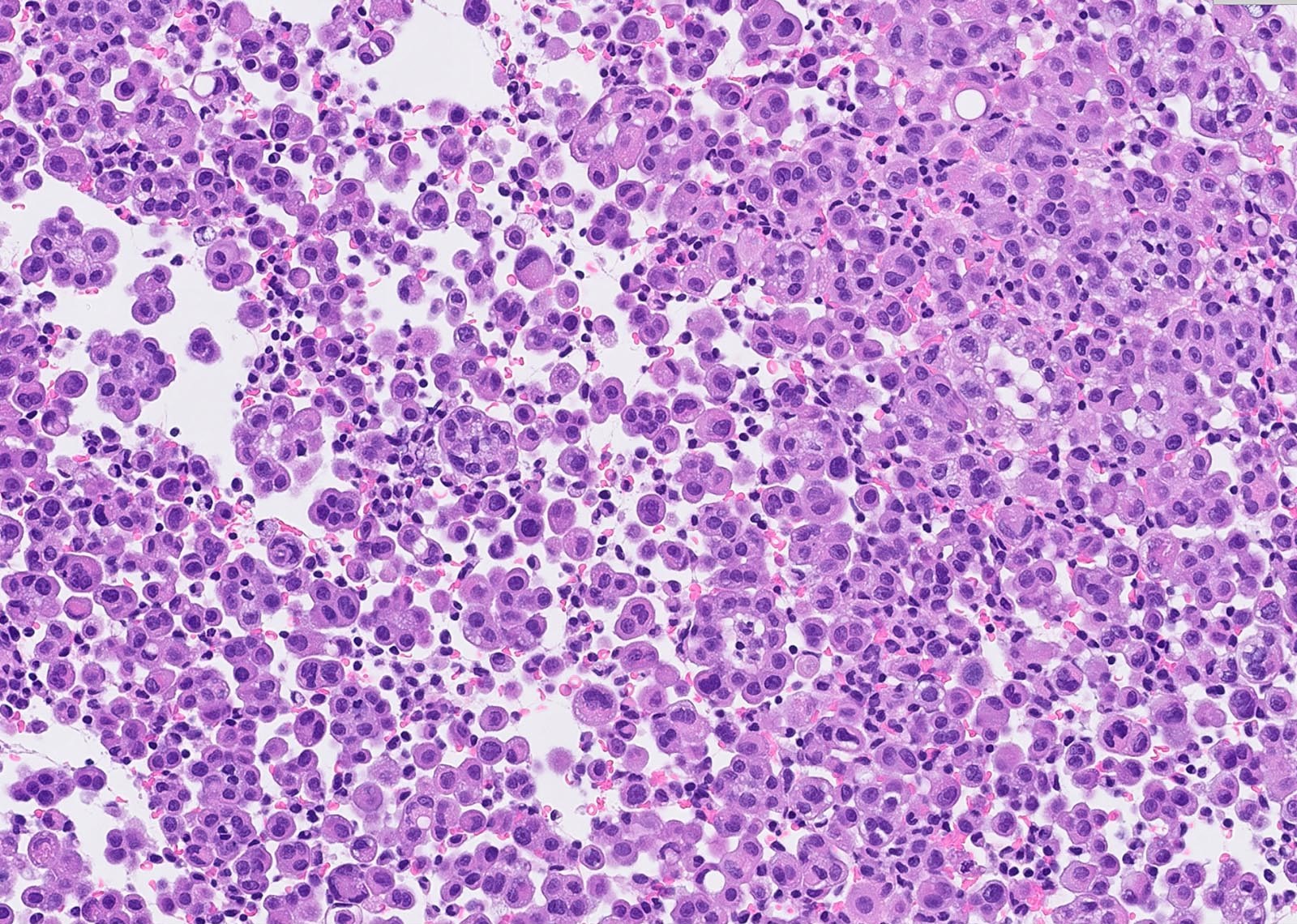
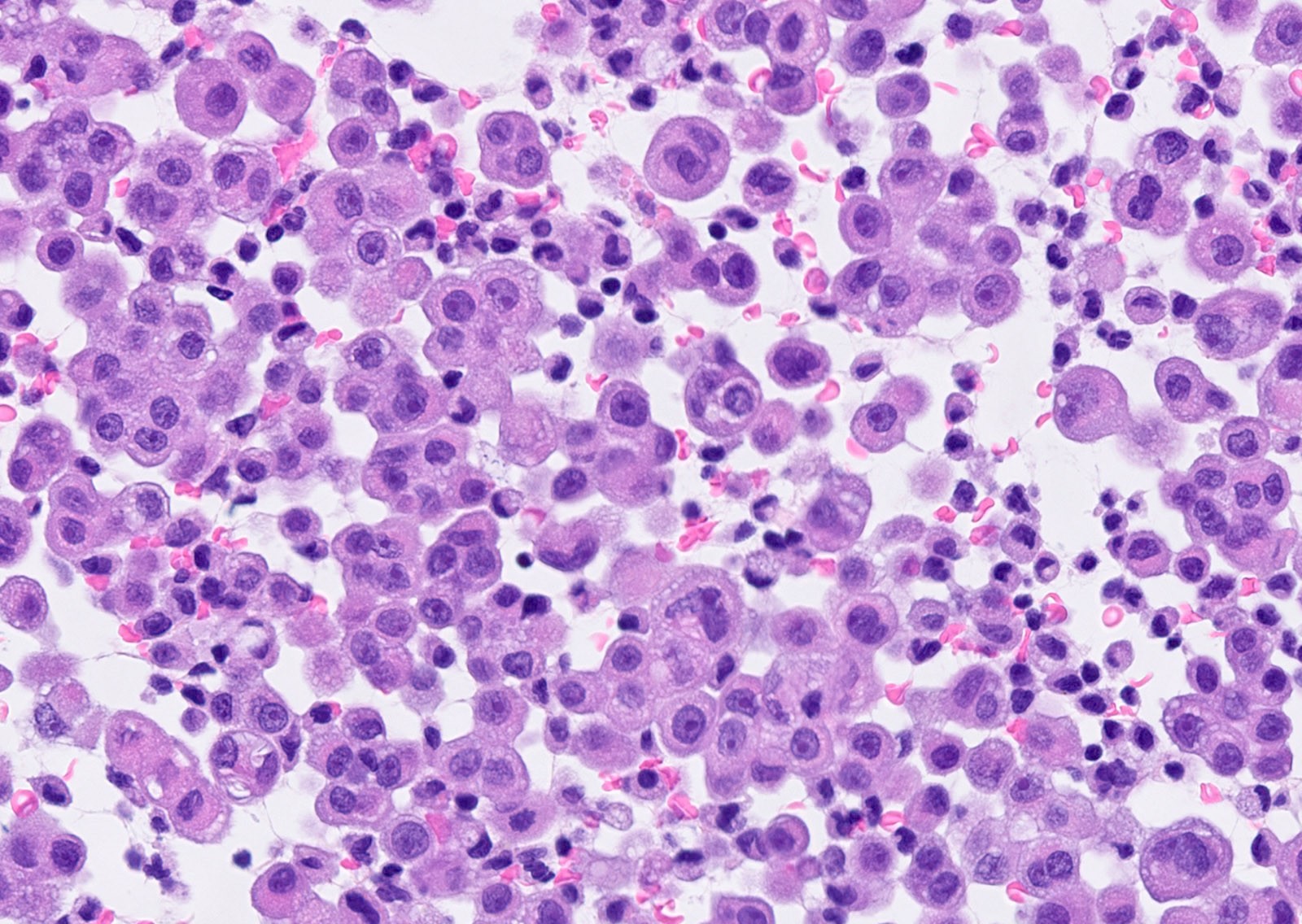
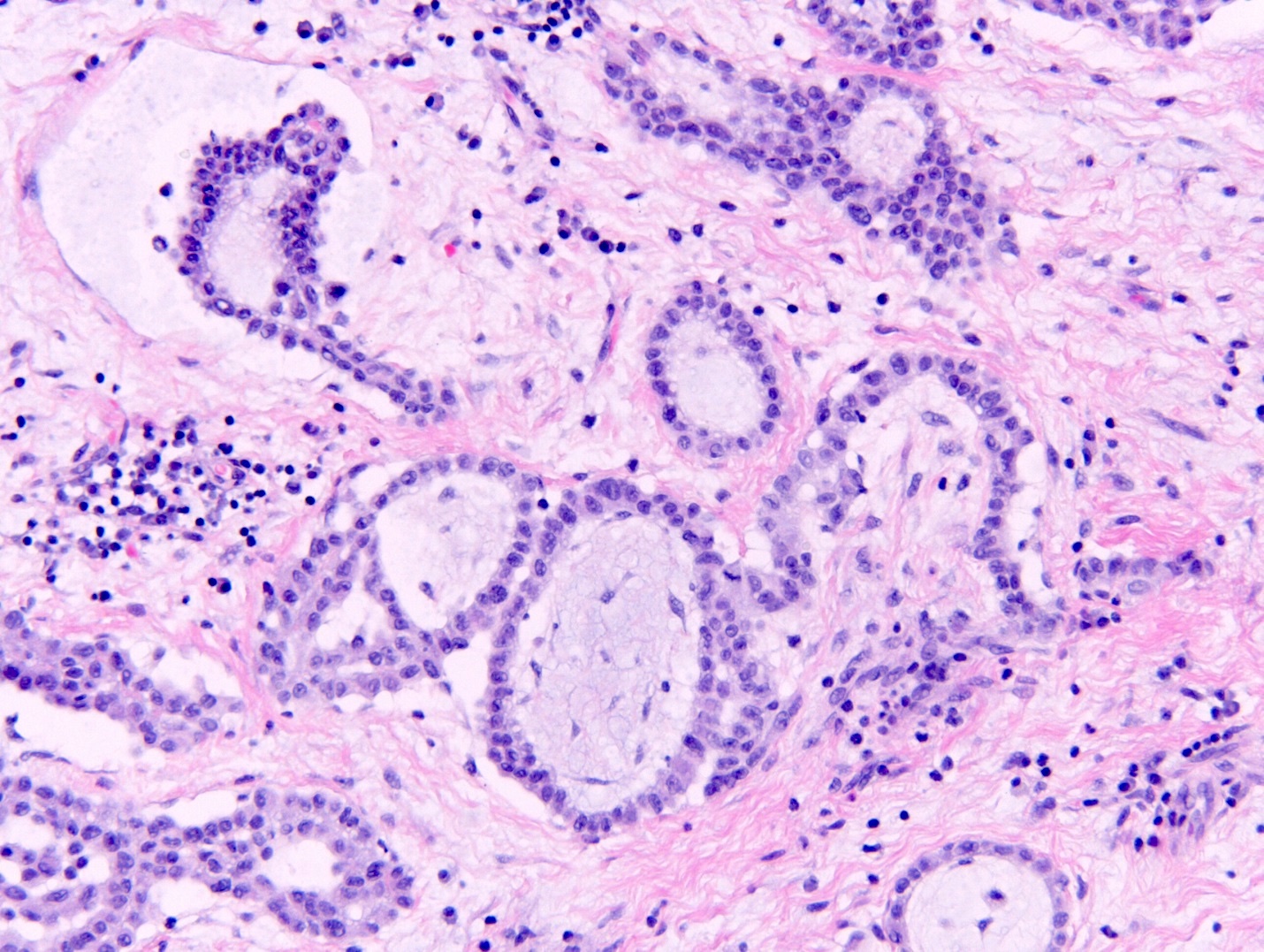
- Epithelioid variant is the most common histological subtype of mesothelioma and its principal differential consideration is adenocarcinoma; they are difficult to differentiate histologically if adenocarcinoma does not produce obvious mucin
- Morphologic features of mesothelioma (J Clin Pathol 2006;59:564):
- Round or cuboidal tumor cells, paracentric nuclei, small nucleoli, moderate to abundant amount of cytoplasm with low nuclear to cytoplasmic ratio
- Often deceptively bland cytologic features
- Morphologic features of adenocarcinoma (J Clin Pathol 2006;59:564):
- Tend to have columnar morphology with more pleomorphism, eccentric nuclei, prominent nucleoli, nuclear molding, cellular crowding and variable amount of cytoplasm
- More likely to have high nuclear to cytopasmic ratio
- Background myxoid stromal change favors a diagnosis of mesothelioma but is not a definitive feature
- Pitfalls:
- Papillary formations or psammoma bodies can be seen in reactive and malignant mesothelial proliferations as well as adenocarcinoma
- Intracytoplasmic vacuoles can be seen in both entities
Microscopic (histologic) images
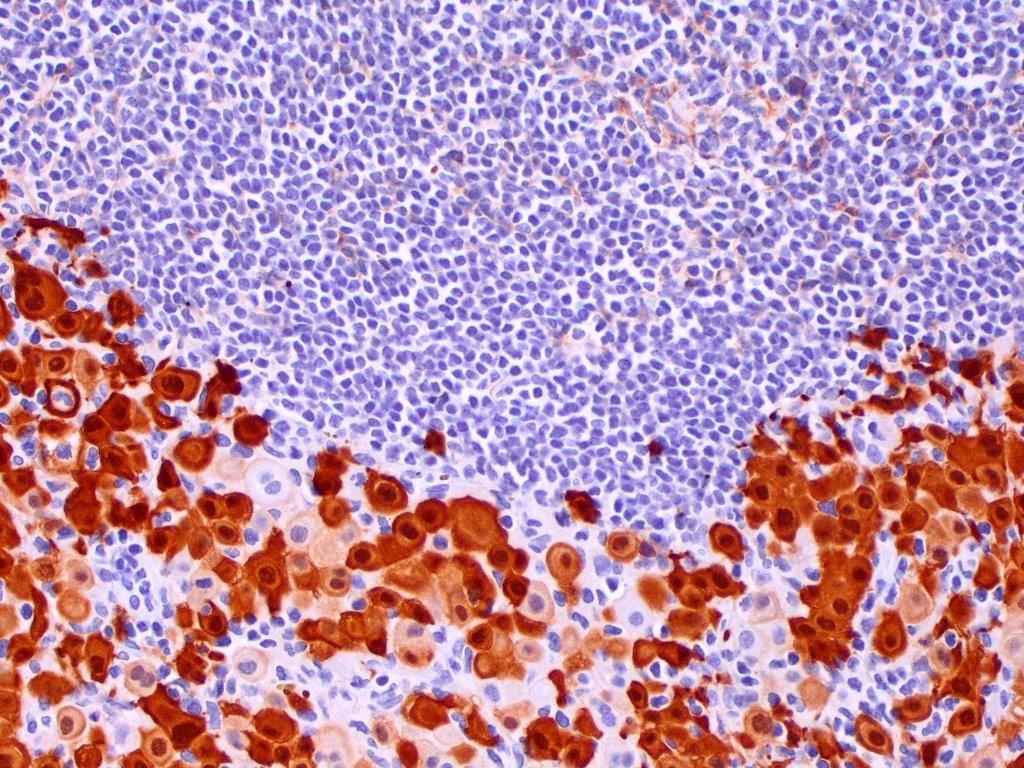
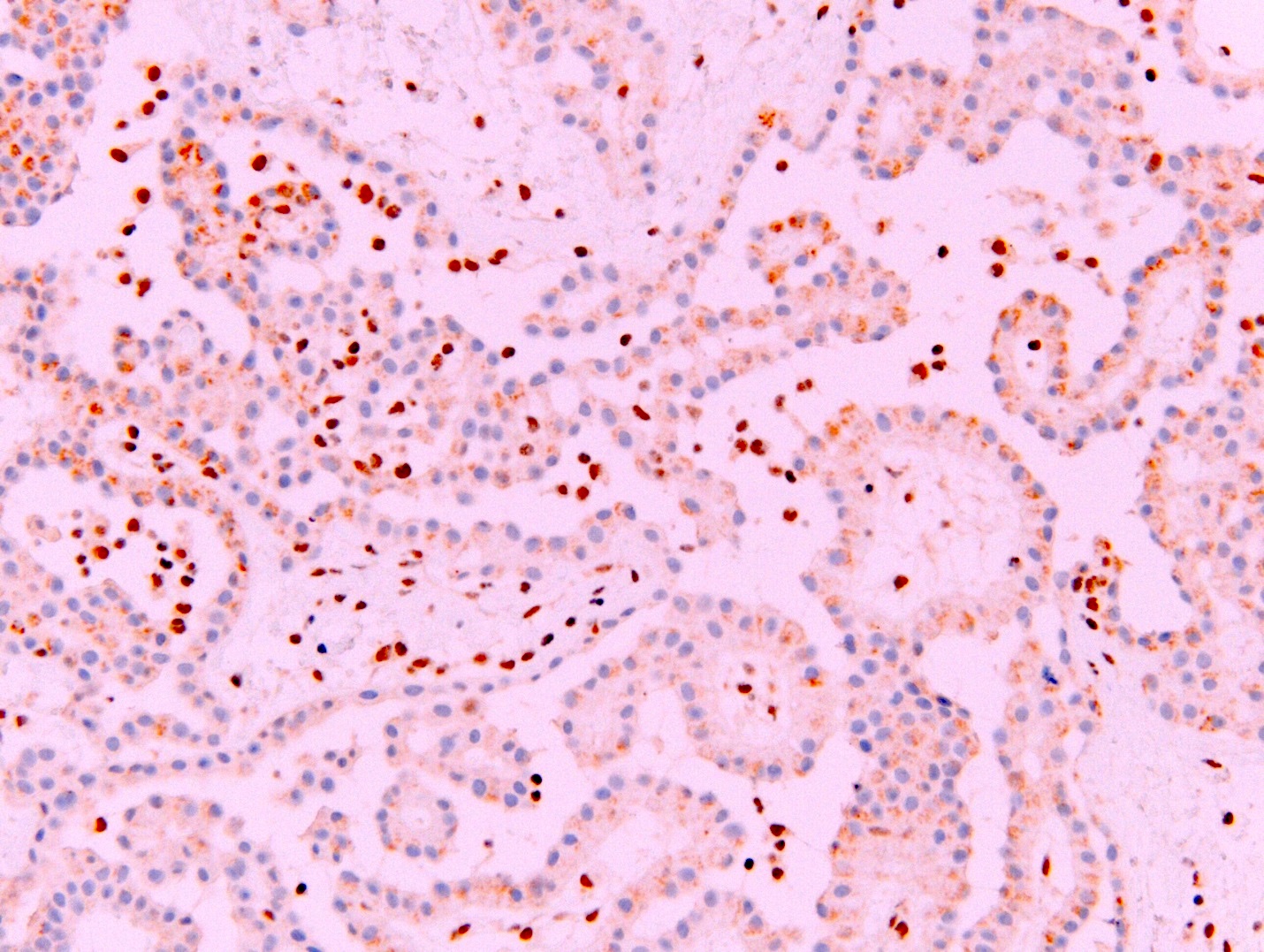
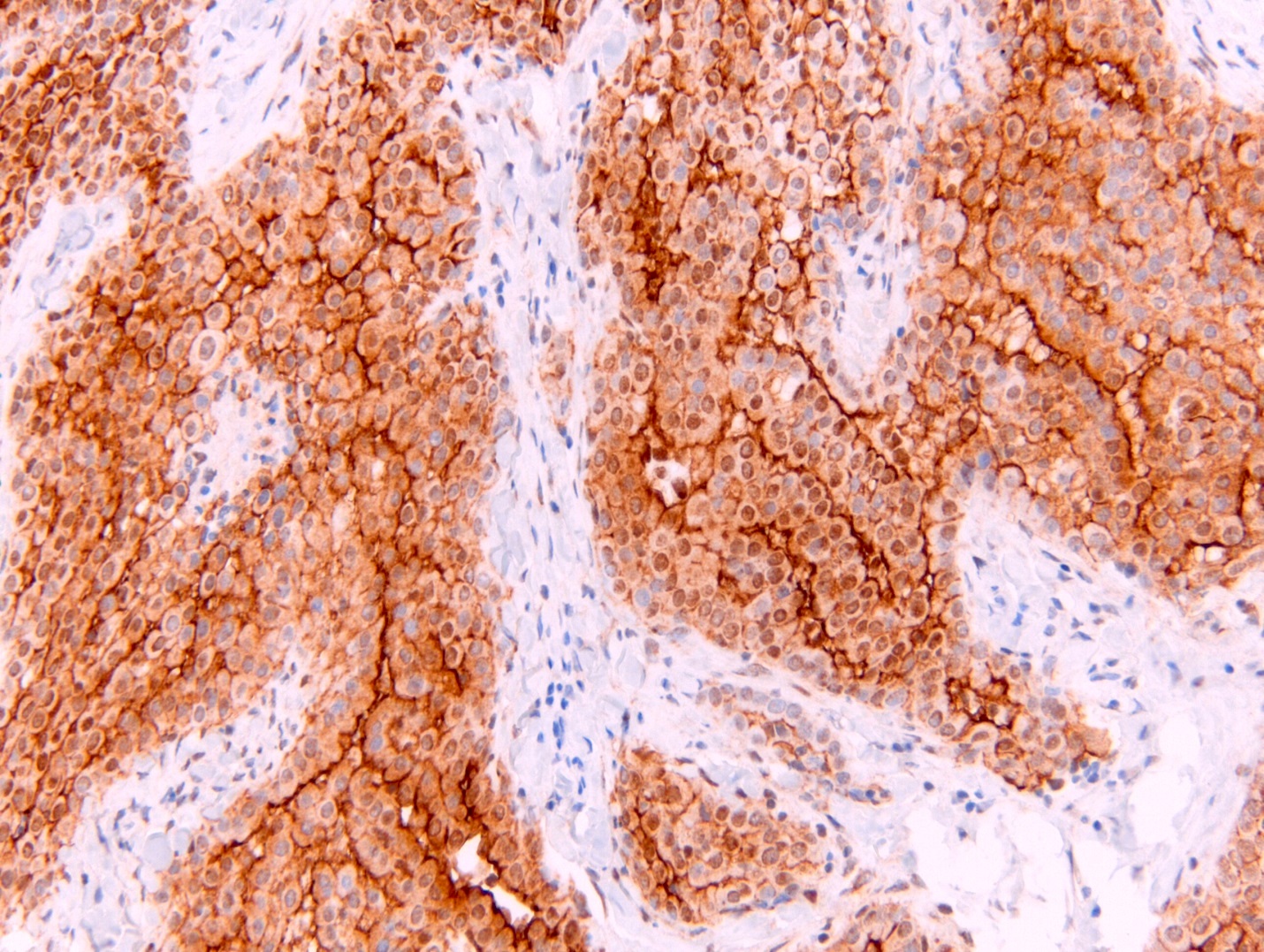
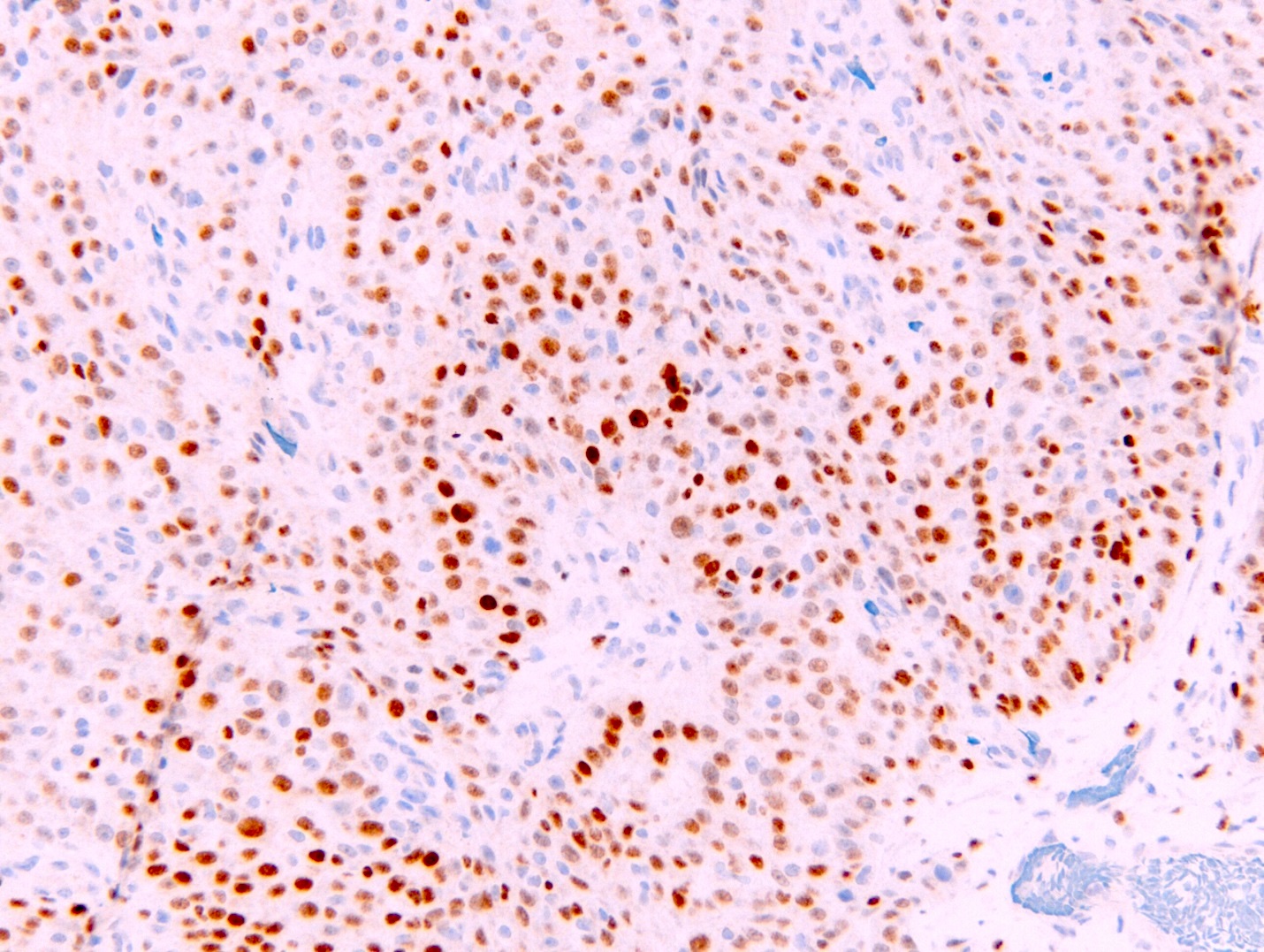
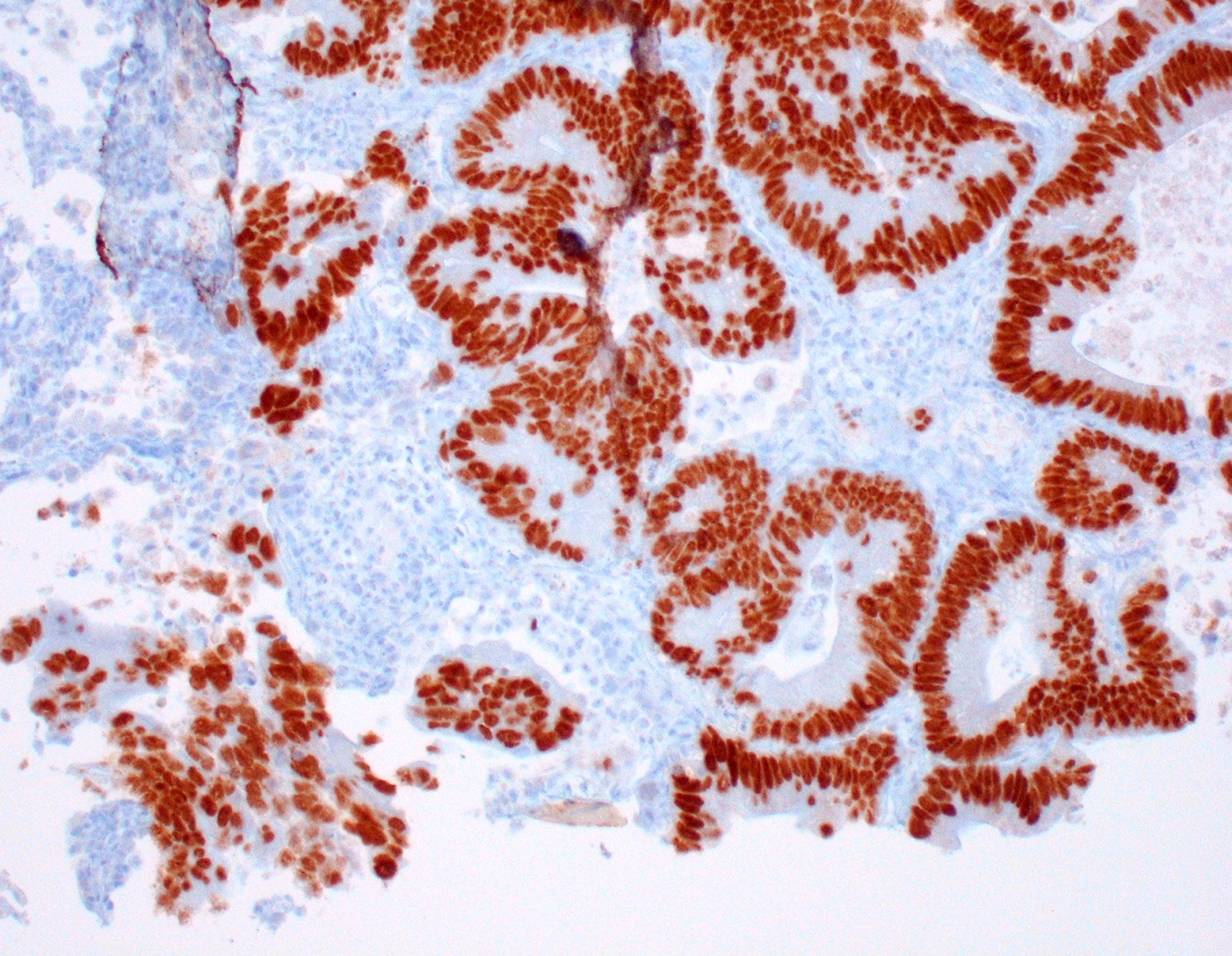
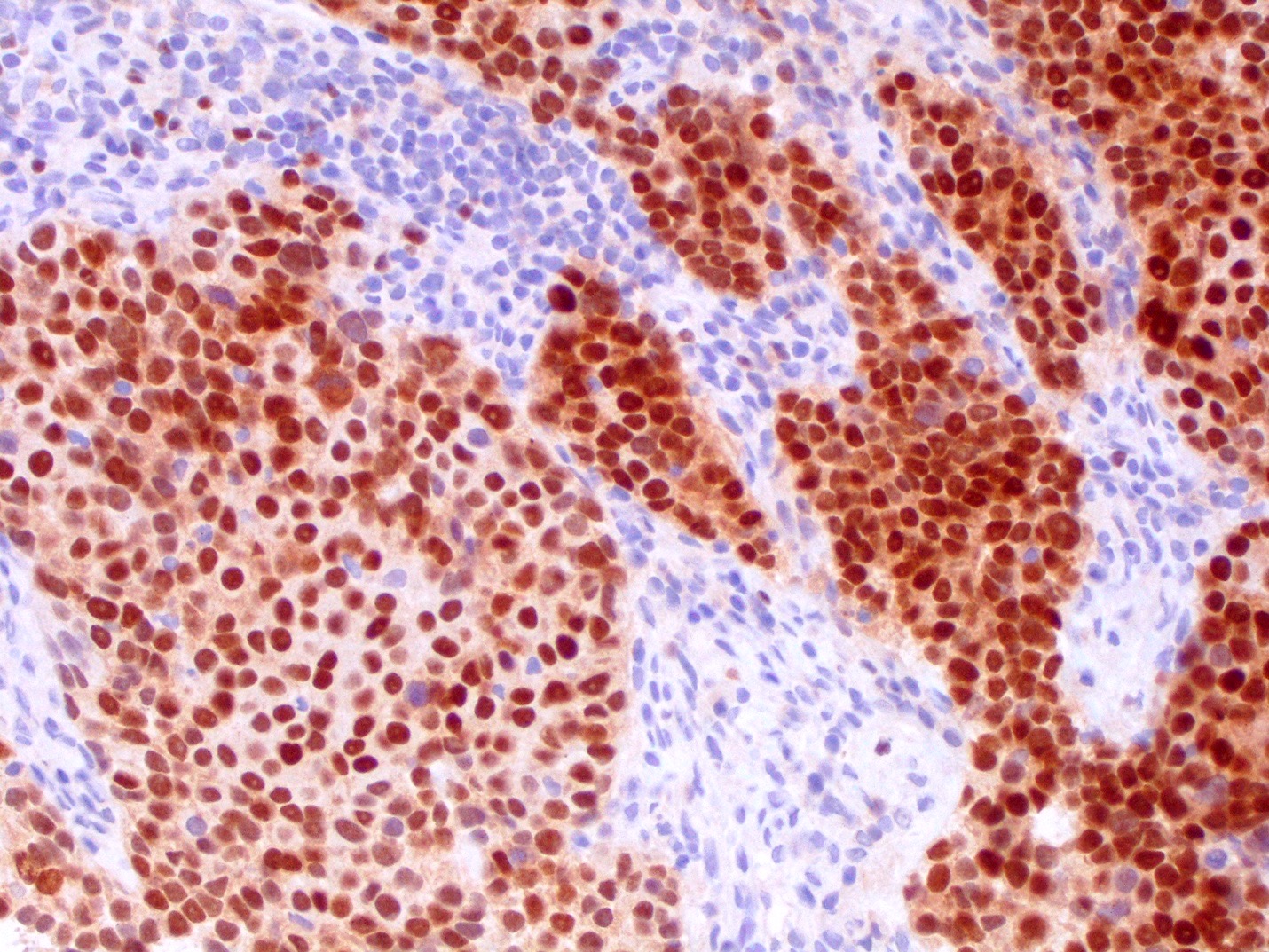
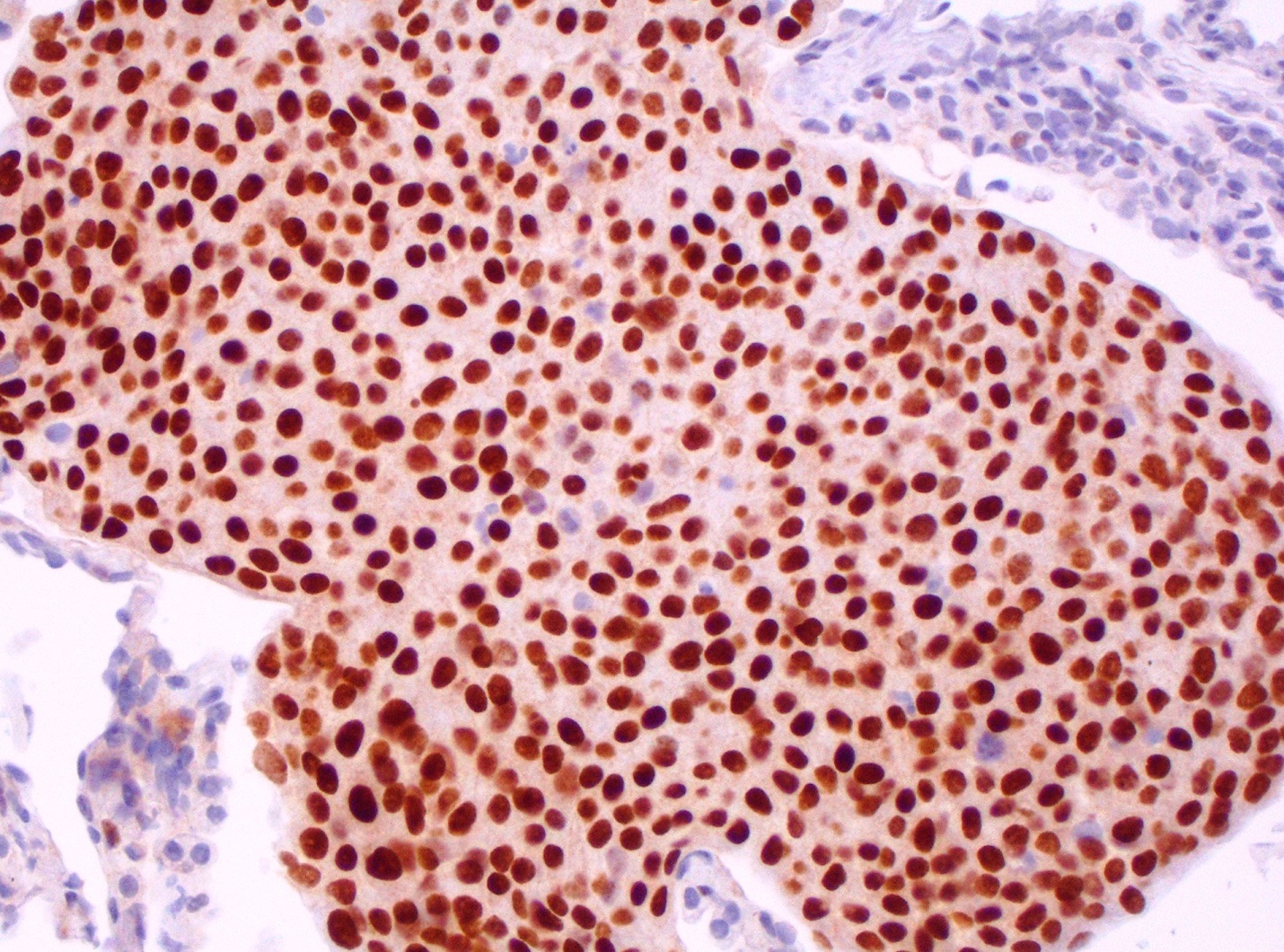
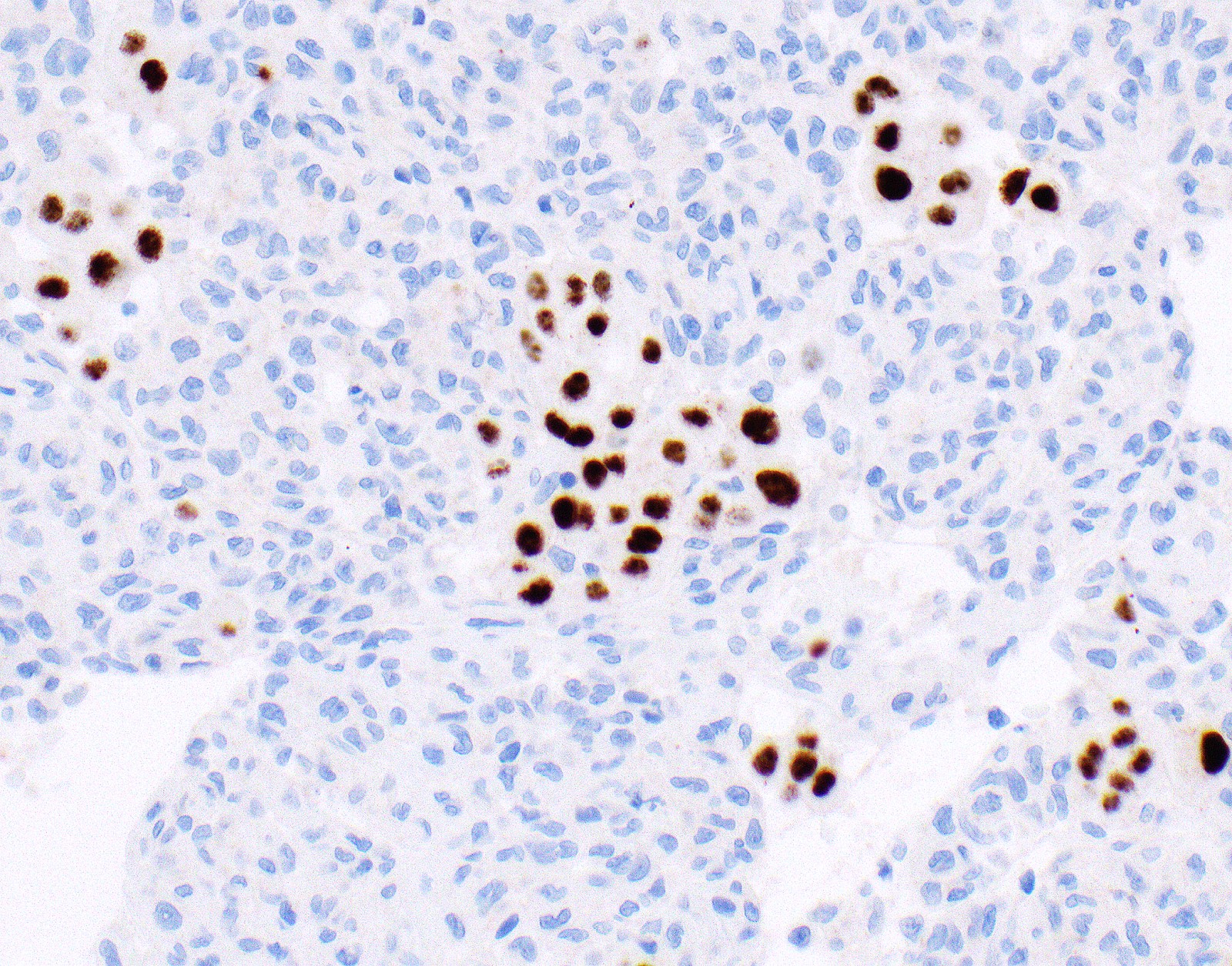
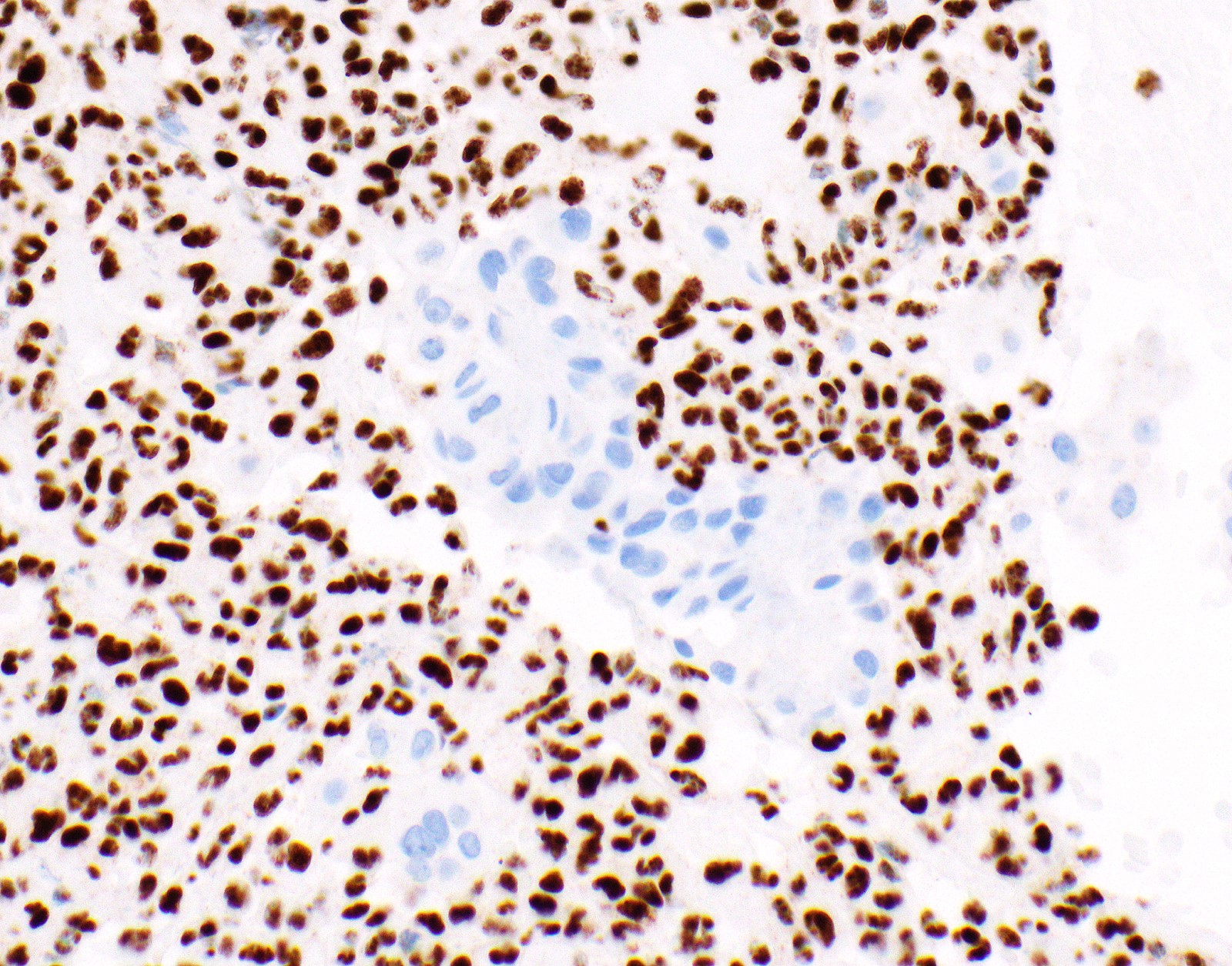
Contributed by Aliya N. Husain, M.D.
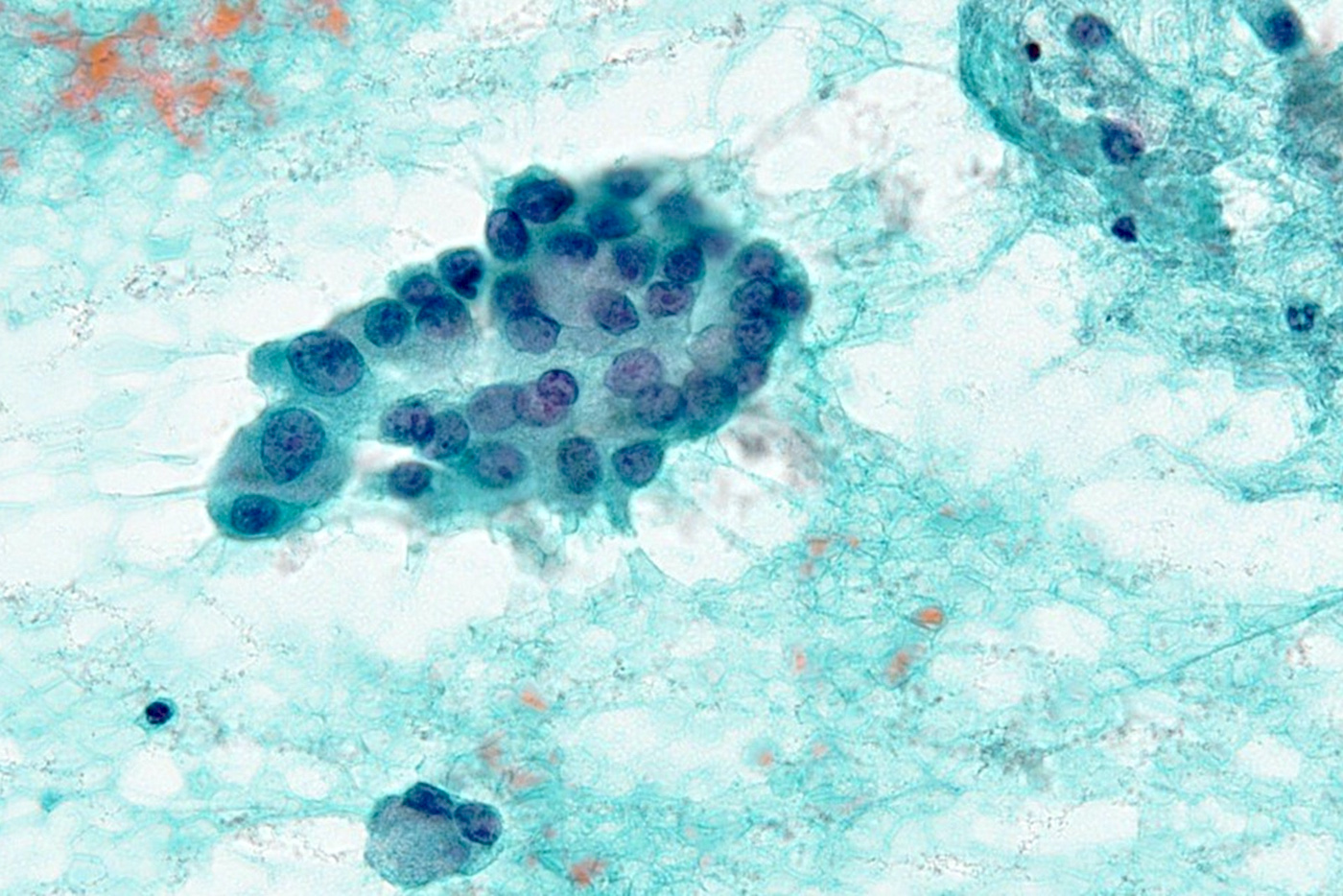
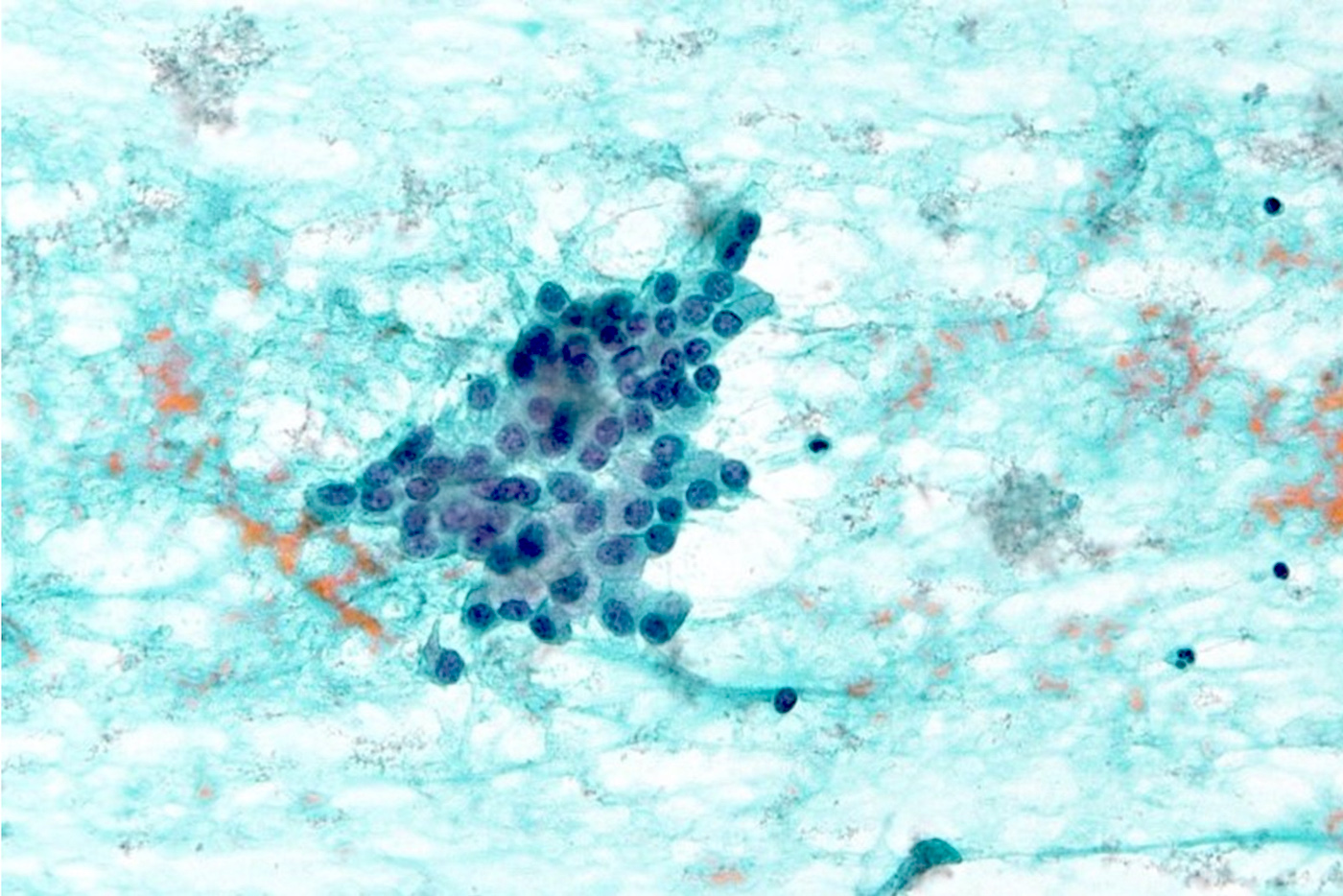
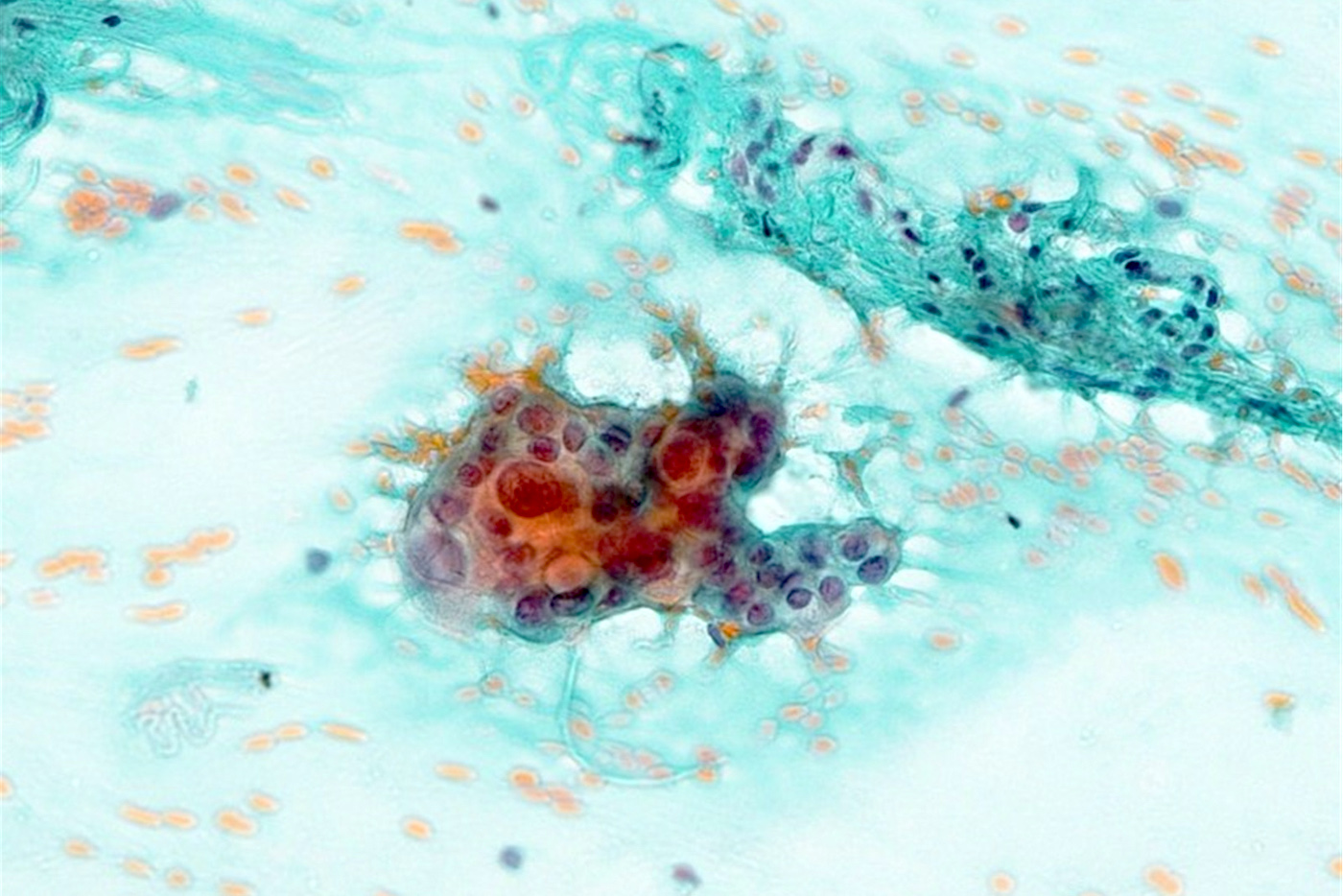
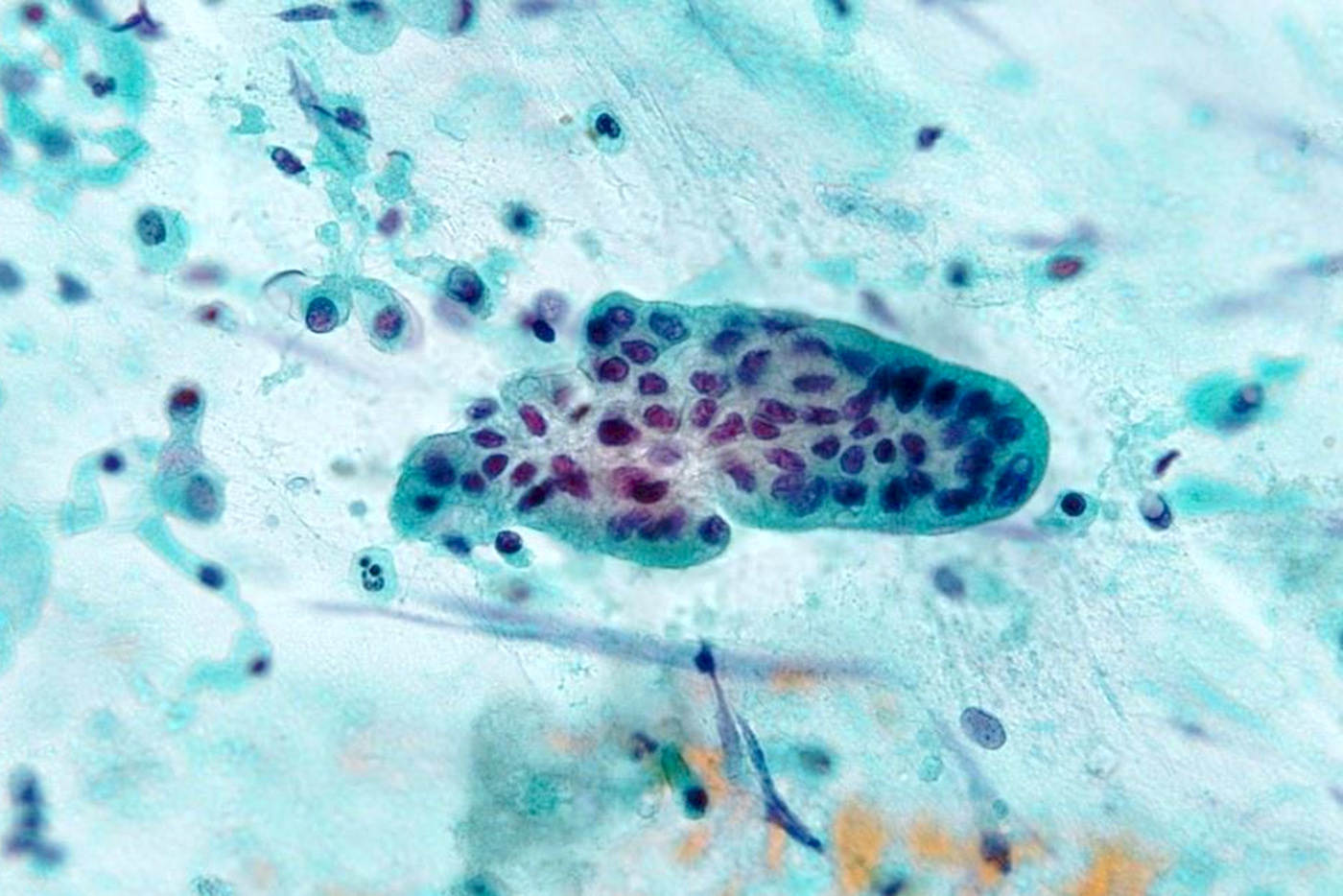
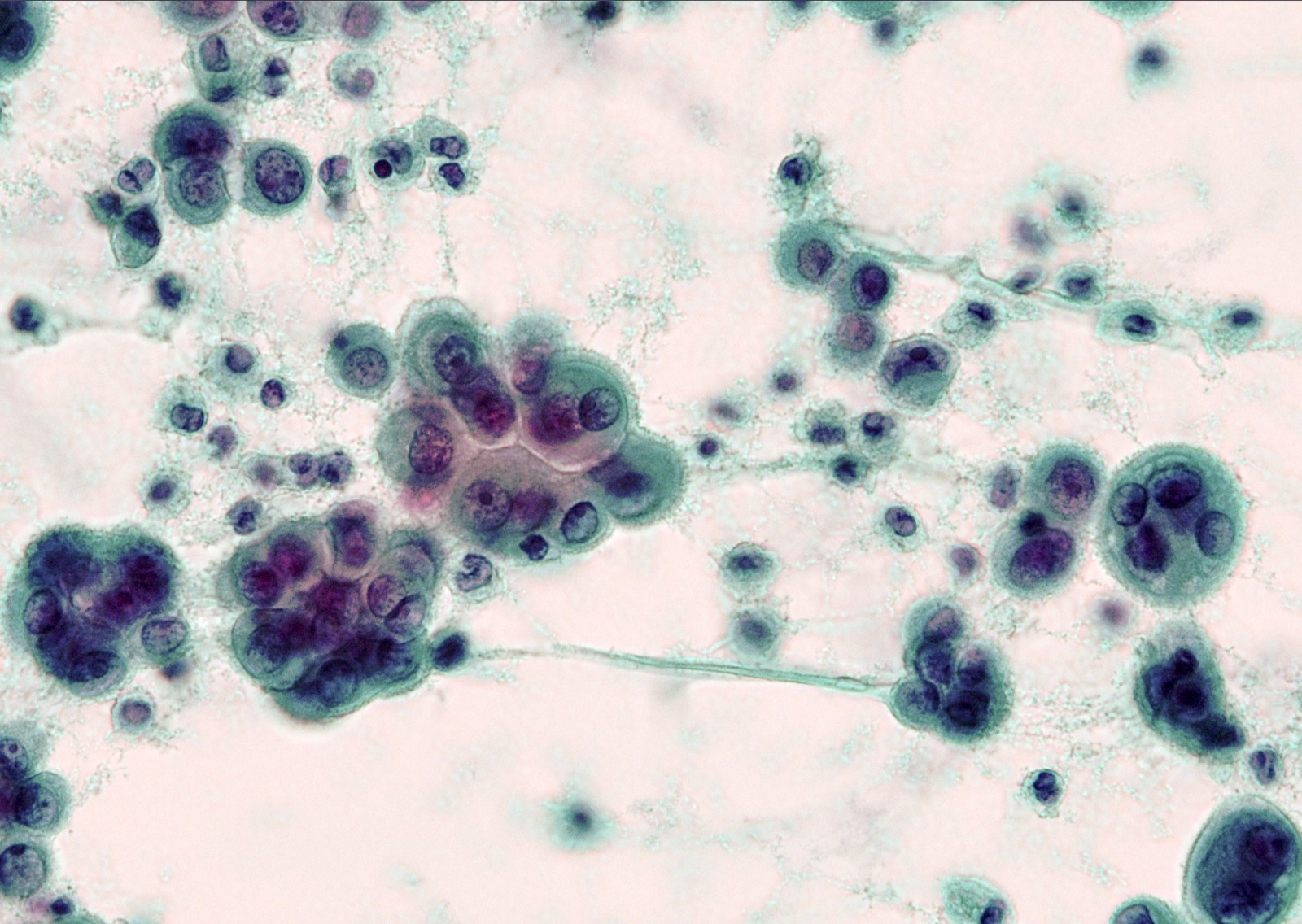
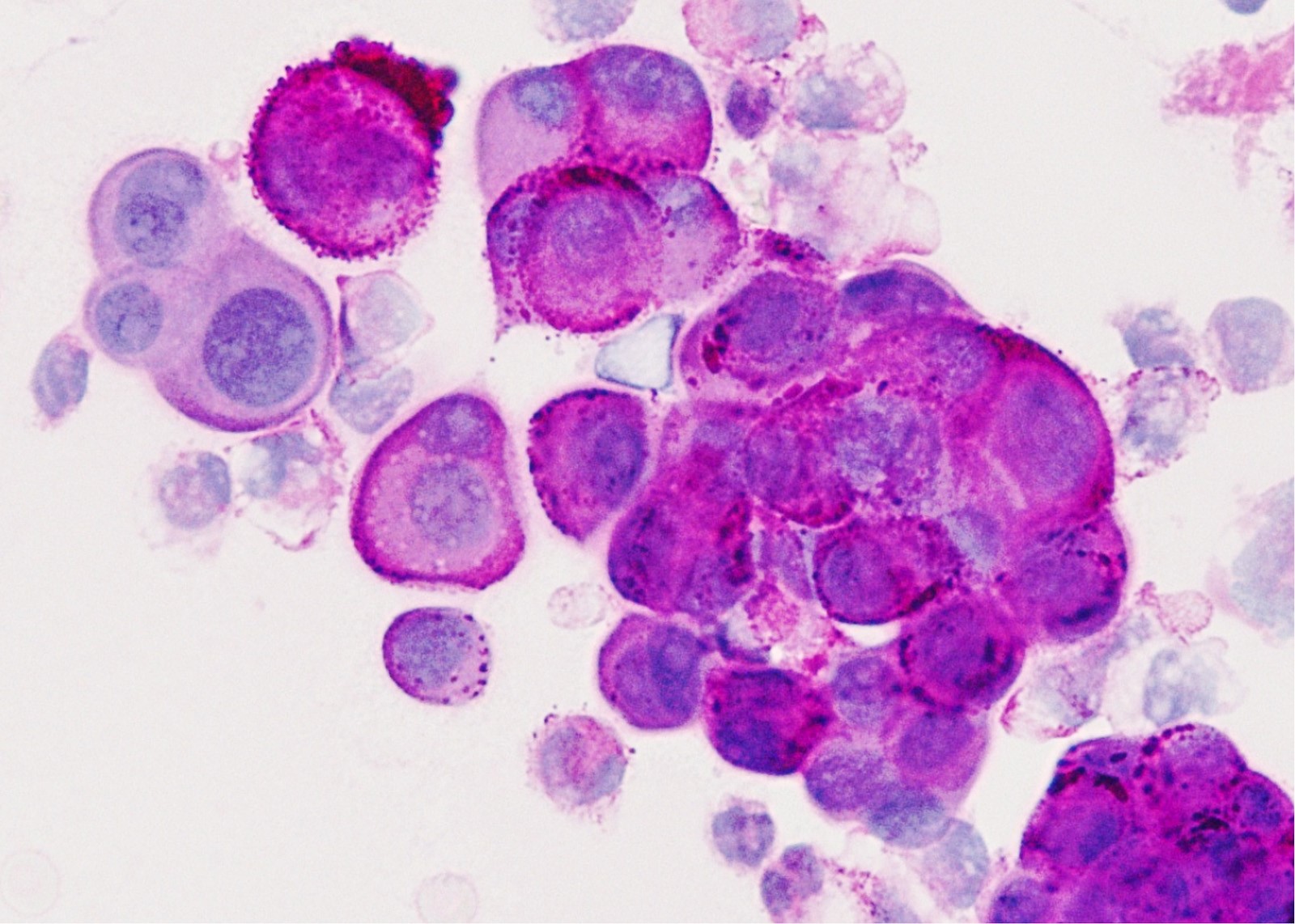
Cytology description
- Adenocarcinoma appears as a distinct population from background mesothelial cells, while mesothelioma appears as a uniform population
- Adenocarcinoma is the likeliest lung cancer cell type to generate a malignant pleural effusion and it is also associated with the highest cytological yield (Ann Transl Med 2019;7:352)
- In adenocarcinoma, the cells may line up to form a picket fence arrangement
- Cytomorphology of mesothelial cells consists of sheets or individual cells with windows between the cells
- In 1 study, the 3 features that were statistically significant to distinguish mesothelioma from adenocarcinoma were: a giant atypical mesothelial cell being indicative of mesothelioma, in contrast to increased nuclear pleomorphism and acinar structures being indicative of adenocarcinoma (Diagn Cytopathol 2009;37:4)
- Cytoplasmic vacuoles in reactive mesothelial cells tend to be paranuclear without indentation of the nuclear membrane, unlike in adenocarcinoma
- Cytoplasmic vacuoles of mesothelial cells contain hyaluronic acid, while those of adenocarcinoma contain epithelial mucin
- Pitfalls: both entities can occur as cell balls with smooth or knobby contours
Cytology images
Contributed by Takashi Hori, C.T., Akira Yoshikawa, M.D., Anja C. Roden, M.D. and Andrey Bychkov, M.D., Ph.D.
Images hosted on other servers:
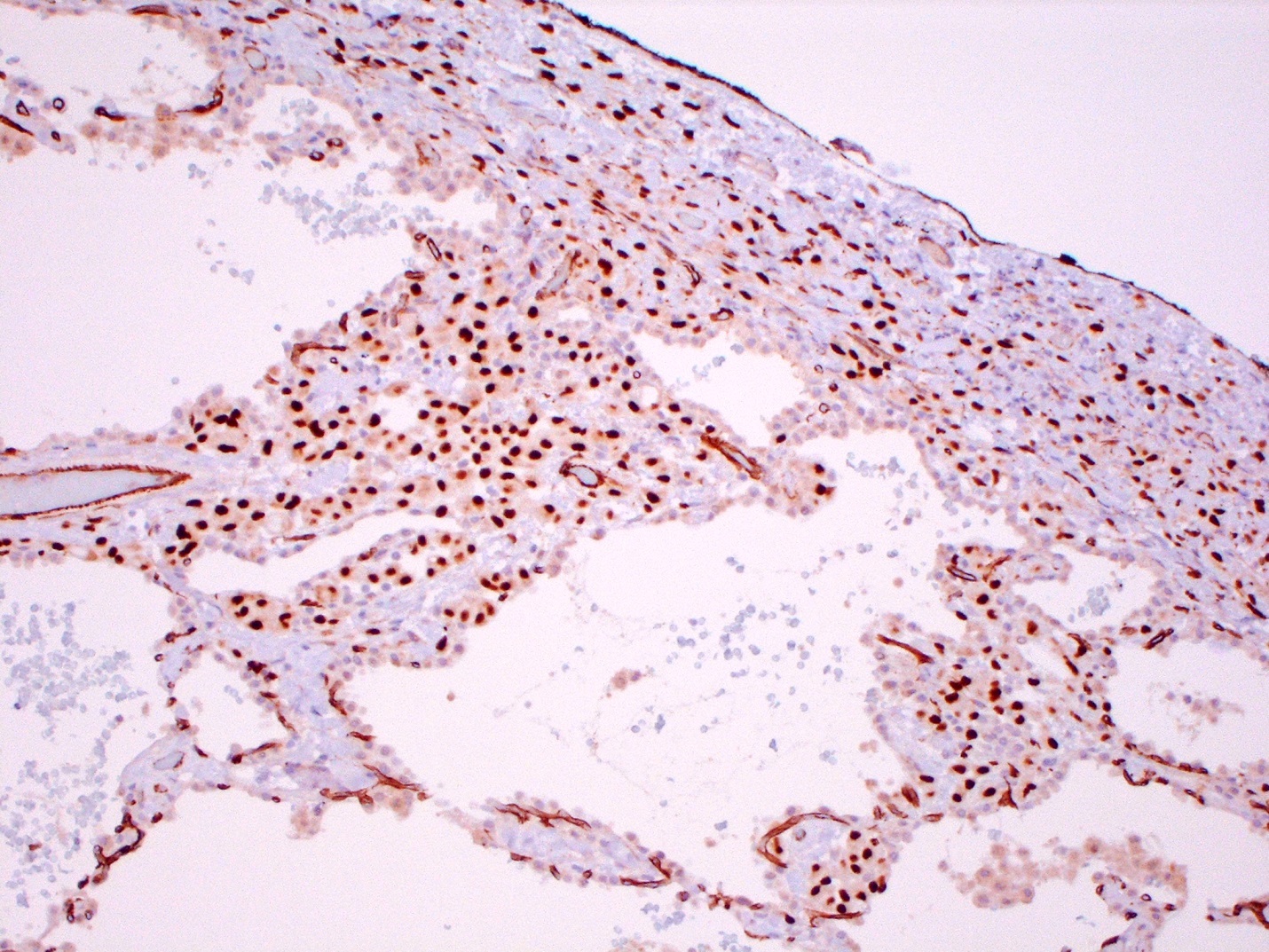
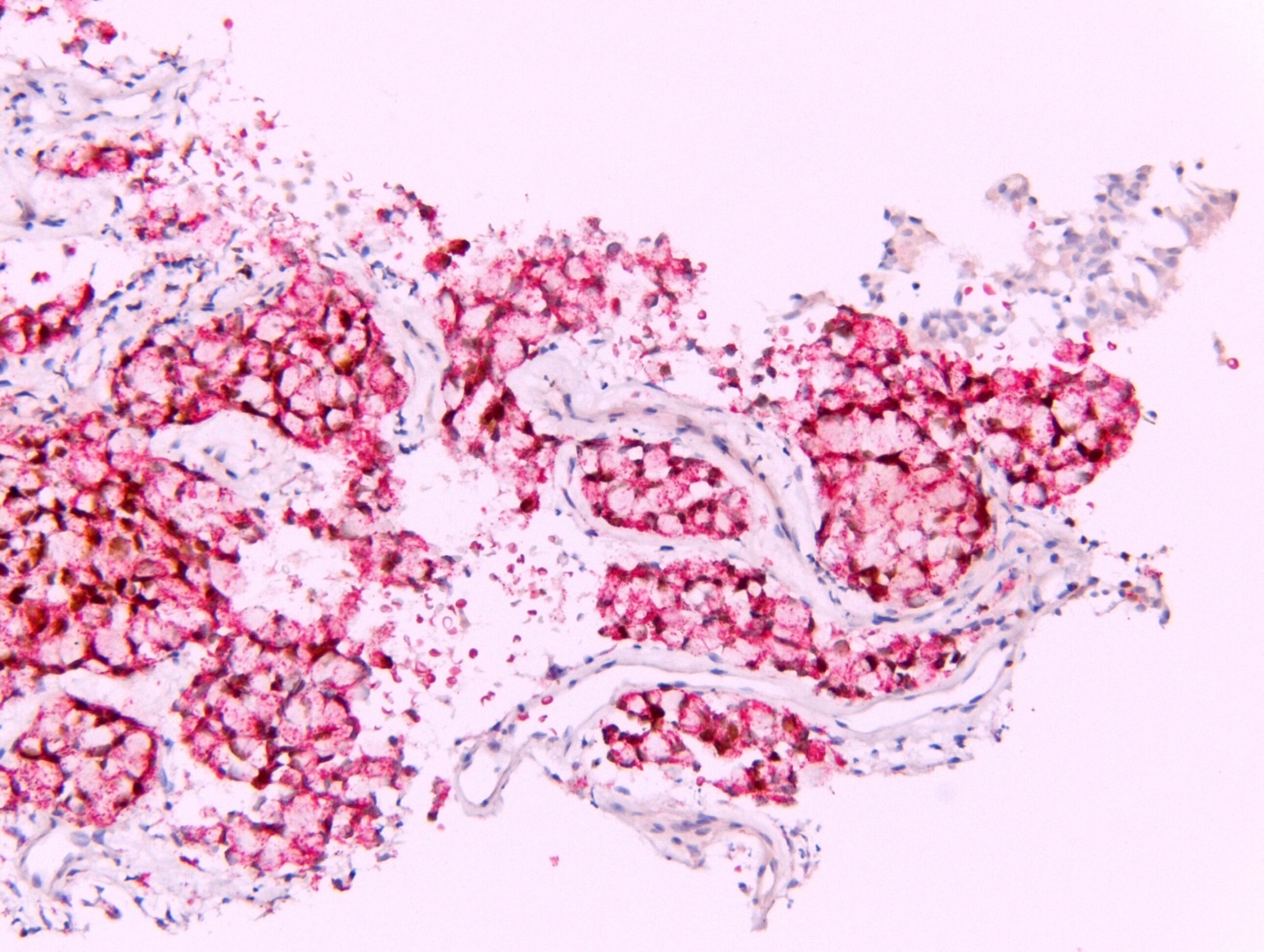
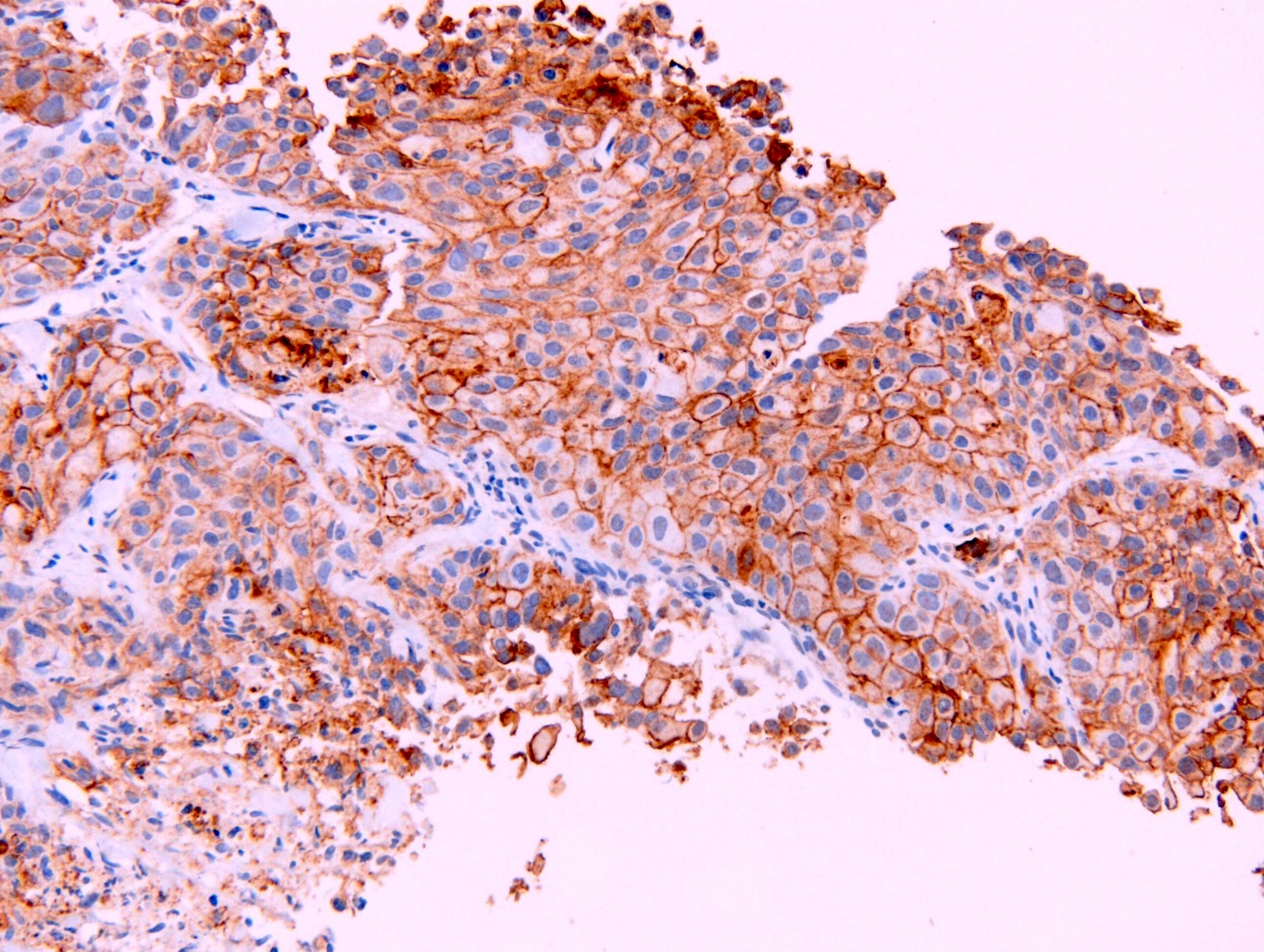
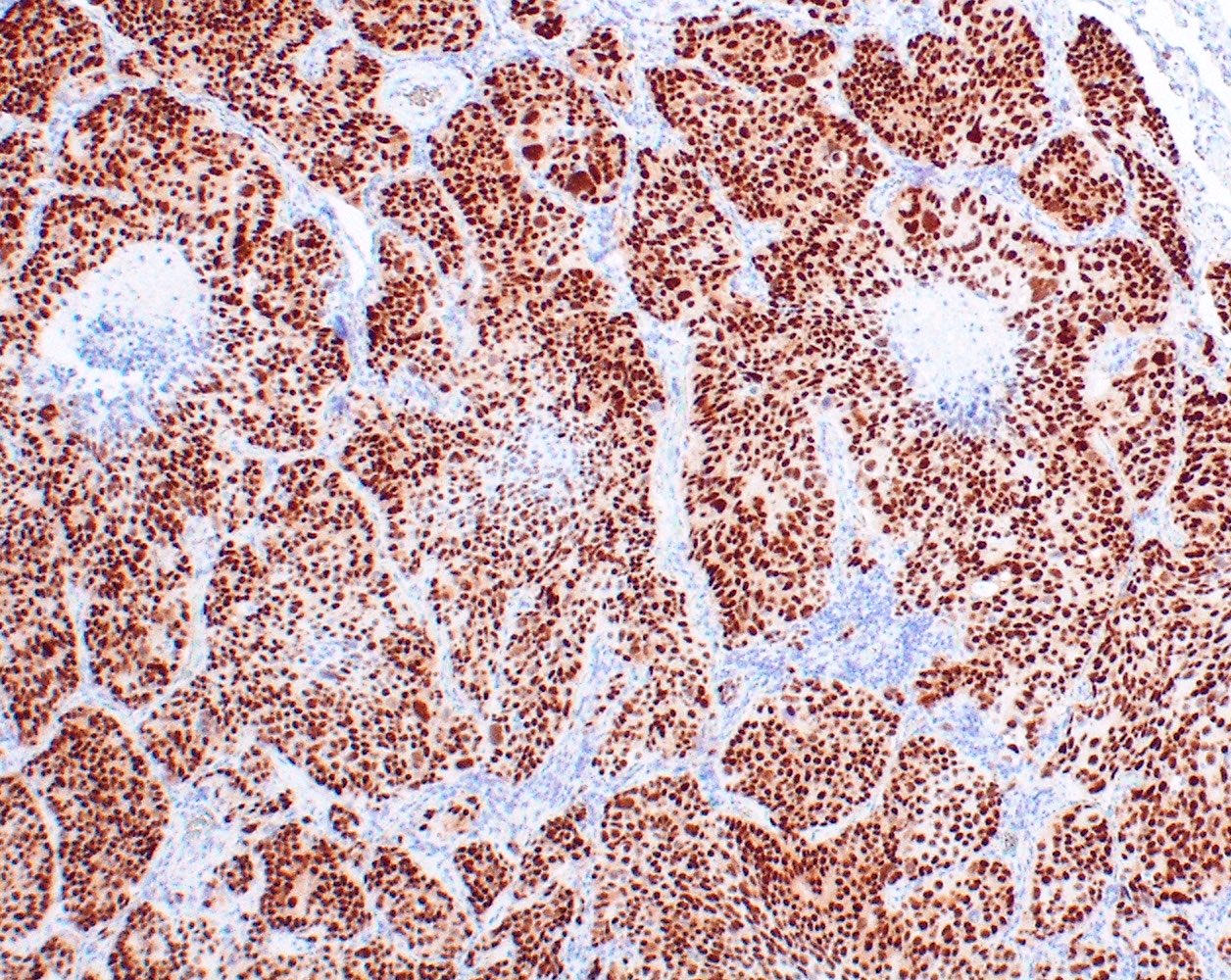
Immunohistochemical stains (positive and negative stains)
- International Mesothelioma Interest Group recommends the initial diagnostic immunohistochemical panel should include at least 2 mesothelial markers and 2 general epithelial markers
- For other tumors in the differential diagnosis, on the basis of morphology, specific markers can be added (e.g. TTF1, PAX8, etc.)
- Use more markers if results inconclusive
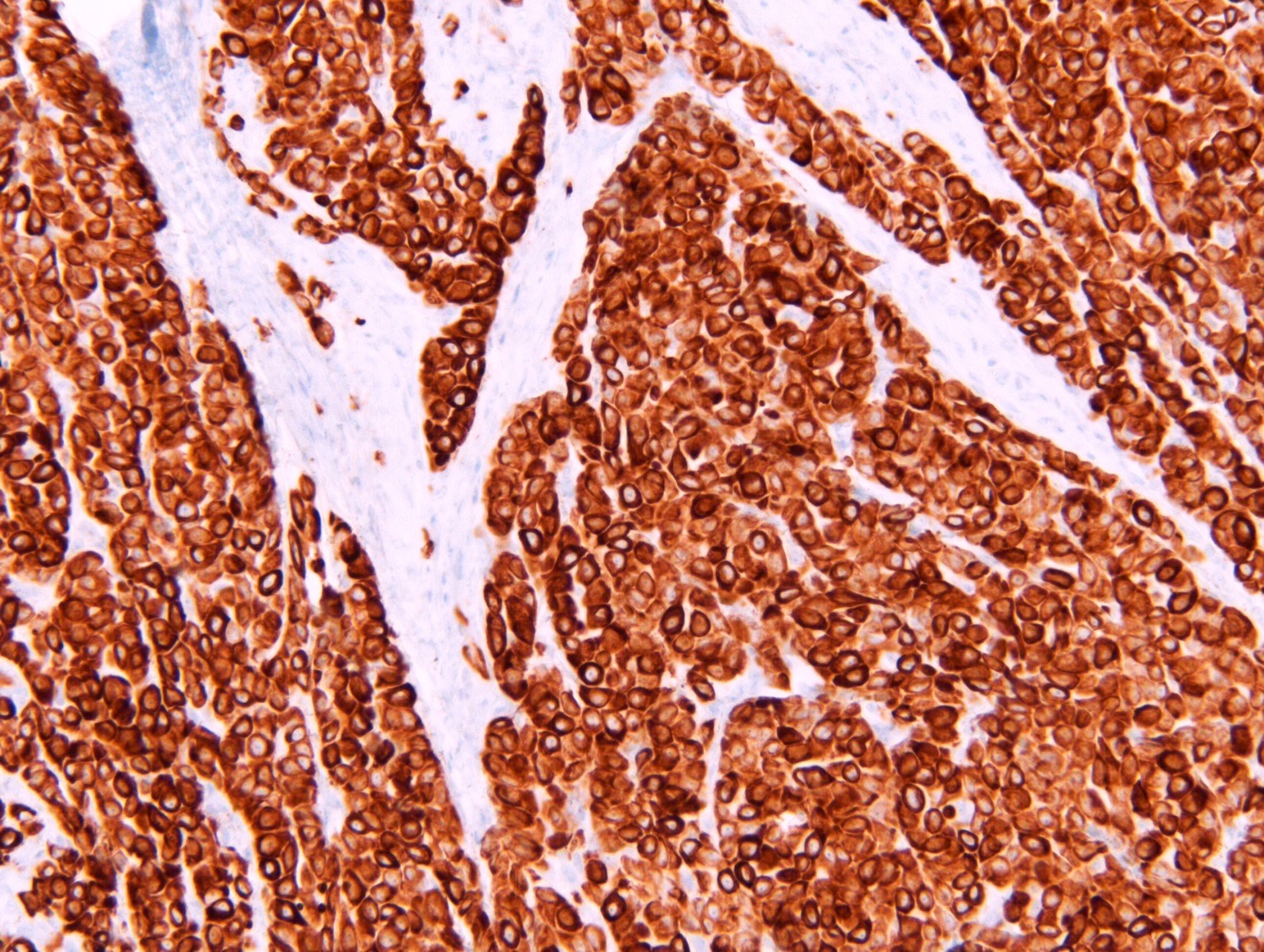
- Best positive mesothelioma markers: calretinin, CK5 or CK5/6, WT1, D2-40
- Best positive carcinoma markers: claudin 4, MOC31, BerEP4, CEA and BG8 (Lewis antigen blood group)
- Best positive lung adenocarcinoma markers: TTF1 and napsin (Arch Pathol Lab Med 2013;137:647)
- Metastatic adenocarcinoma (Arch Pathol Lab Med 2009;133:1317)
- PAX8 is very useful for renal cell carcinoma; about 85 - 100% of renal cell carcinomas are positive; mesotheliomas are mostly negative
- Claudin 4 is positive in almost all lung adenocarcinomas, 90% of renal cell carcinomas, 98% of papillary serous carcinomas, 100% of gastric, pancreatic, colonic and biliary adenocarcinomas; mesotheliomas are always negative
- CDX2 is positive in 90 - 100% of colon, 80% of small intestine and 70% of gastric carcinomas and negative in mesothelioma
- PSA is often positive in metastatic prostatic adenocarcinoma and is always negative in mesothelioma
- Estrogen receptor is positive in 60 - 93% in serous and breast carcinomas and negative or has a very low positive rate (0 - 8%) in mesothelioma
- GATA3 is frequently positive in breast and urothelial carcinomas; however, 33 - 50% of epithelioid mesotheliomas also express GATA3
- Strong diffuse staining for GATA3 favors a diagnosis of sarcomatoid / desmoplastic mesothelioma over metastatic sarcomatoid carcinoma of the lung (Am J Surg Pathol 2017;41:1221)
| IHC stain | Mesothelioma | Adenocarcinoma | Staining pattern in positive cells |
| Calretinin | Positive | Negative | Nuclear and cytoplasmic |
| D2-40 (podoplanin) | Positive | Negative | Membranous |
| WT1 | Positive | Negative | Nuclear |
| Cytokeratin 5 / 6 | Positive | Negative | Cytoplasmic |
| Claudin 4 | Negative | Positive | Membranous |
| MOC31 | Negative | Positive | Membranous |
| TTF1 | Negative | Positive | Nuclear |
| Napsin A | Negative | Positive | Granular cytoplasmic |
| B72.3 | Negative | Positive | Membranous, cytoplasmic or both |
| BG8 | Negative | Positive | Cytoplasmic |
| CEA (monoclonal) | Negative | Positive | Cytoplasmic with membrane enhancement |
| BerEP4 | Negative | Positive | Membranous |
| BAP1 | Loss in 60% of epithelioid MM | Retained | Nuclear |
Special stains
- With the advent of specific histochemical markers, these are now mostly historical and not useful in everyday practice
- PAS after pretreatment with diastase or Alcian blue after hyaluronidase, positivity indicates neutral mucin which favors adenocarcinoma (Alcian blue without hyalurinadase is not helpful) (J Surg Oncol 1987;35:30)
- Mucicarmine should not be used as it sometimes cross reacts with hyaluronic acid
- Histochemical methods are most useful in epithelioid mesotheliomas and not useful in nonepithelioid mesotheliomas
Electron microscopy description
| EM features | Mesothelioma | Adenocarcinoma |
| Apical microvilli | Long and thin, no glycocalyx | Shorter and have microvilli |
| Perinuclear tonofilament bundles | Present | Absent |
| Basal lamina | Present | Absent |
| Long desmosomes | Present | Absent |
- Helpful in distinguishing mesothelioma from adenocarcinoma in well differentiated tumors
- Not helpful in distinguishing benign / reactive from malignant mesothelial proliferations
- Reference: Ultrastruct Pathol 2006;30:3
Molecular / cytogenetics description
- Most mesotheliomas (> 80%) harbor somatic alterations of the CDKN2A locus, 60% harbor somatic mutations and exonic deletions of the BAP1 gene and 30 - 50% show inactivation of NF2 (Transl Lung Cancer Res 2017;6:270)
- Several driver gene alterations are known in lung adenocarcinomas including EGFR, KRAS and ALK
Additional references
Board review style question #1
Board review style answer #1
C. WT1, calretinin, claudin 4, MOC31 is the only answer choice that has 2 mesothelioma markers (WT1, calretinin) and 2 adenocarcinoma markers (claudin 4, MOC31). BAP1 is lost in the majority of epithelioid mesotheliomas and is indicative of malignancy but is not a sensitive initial diagnostic marker. GATA3 and p16 are not specific to mesothelioma. ER and CDX2 are specific to certain metastatic adenocarcinomas but not other adenocarcinomas.
Comment Here
Reference: Mesothelioma versus adenocarcinoma
Comment Here
Reference: Mesothelioma versus adenocarcinoma
Board review style question #2
Molecular alterations of which of the following genes is least likely to be occur in pleural mesothelioma?
- ALK
- BAP1
- CDKN2A
- NF2
Board review style answer #2
A. ALK. Genetic alterations in NF2, CDKN2A and BAP1 are commonly associated with epithelioid mesothelioma of the pleura. ALK-EML4 translocations are seen in 3 - 7% of lung adenocarcinomas. ALK alterations rarely occur in a subset of peritoneal mesotheliomas. Rare case reports of pleural mesothelioma with ALK translocations have now recently been described and although very uncommon are important to recognize because they may impact treatment options. (JCO Precis Oncol 2019;3:PO.19.00048, Transl Lung Cancer Res 2018;7:537)
Comment Here
Reference: Mesothelioma versus adenocarcinoma
Comment Here
Reference: Mesothelioma versus adenocarcinoma