Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ravishankar S. Retroplacental hematoma with intraplacental extension (placental abruption). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentaretroplacentalhematoma.html. Accessed November 27th, 2024.
Definition / general
- Loss of maternal vascular integrity, resulting in accumulation of maternal blood between the maternal surface of the placenta and the uterine wall after 20 weeks gestation and before delivery of the fetus / infant
Essential features
- Premature separation of the placenta from the uterine wall by maternal blood; strongly associated with maternal hypertensive disorders of pregnancy and maternal vascular malperfusion of the placenta
- 3 main categories: classic acute abruption, acute marginal abruption and chronic abruption
- Gross features: retroplacental hematoma (acute) / brown membrane staining and circumvallate membrane insertion (chronic)
- Microscopic features: intravillous hemorrhage, hematoma with underlying infarction (acute) / chorioamniotic hemosiderosis (chronic)
Terminology
- Abruptio placentae
- Acute / chronic abruption
- Acute / chronic marginal abruption
- Acute / chronic peripheral separation
ICD coding
- ICD-10: O45 - premature separation of placenta
Epidemiology
- Acute abruption: can occur at any gestational age but is most common between 24 - 26 weeks gestation (Obstet Gynecol 2006;108:1005)
- Rates are generally increasing in the U.S. and are highest in African American women (Am J Obstet Gynecol 2005;192:191)
- Higher incidence in hypertensive patients and those with prior abruption (Obstet Gynecol 1984;63:365, Acta Obstet Gynecol Scand 2011;90:140)
- Strong correlation with maternal vascular malperfusion; may be considered supporting evidence for that diagnosis
Sites
- Placenta
Pathophysiology
- Acute abruption
- Loss of maternal vascular integrity (assumed to be arterial - high pressure / flow) results in rapid, often massive hemorrhage and placental separation
- Acute marginal abruption (Obstet Gynecol Surv 1988;43:577)
- Predilection for venous bleeding at the margin of the placenta for unclear reasons
- Venous disruption at the margin leads to hemorrhage that dissects both retromembranously and subchorionically
- Chronic abruption
- Maternal vascular disruption, usually marginal and venous, for an extended duration leads to accumulation of blood clots and blood breakdown products (fibrin, hemosiderin)
Etiology
- Acute abruption: hypertension / hypertensive disorders of pregnancy (preeclampsia, etc.), smoking, cocaine abuse, trauma
- Acute marginal abruption: acute chorioamnionitis
- Chronic abruption: etiology is poorly understood; no clear risk factors are known
- Reference: Obstet Gynecol 2006;108:1005
Clinical features
- Preterm delivery
- Stillbirth
- Maternal hemorrhage
- Maternal disseminated intravascular coagulation
- Oligohydramnios (chronic abruption)
- Reference: Acta Obstet Gynecol Scand 2011;90:140
Diagnosis
- Clinical and pathologic diagnosis do not necessarily correlate
- Very acute abruptions may not have enough time to leave any placental evidence of their occurrence
- Marginal abruptions are often concealed / clinically silent and are only identified on pathologic examination
- Bloody amniotic fluid
- Couvelaire uterus (N Engl J Med 2020;383:1973)
- Consumptive coagulopathy on laboratory evaluation
Laboratory
- Decreases in maternal fibrinogen, prothrombin, factors V and VIII and platelets
- Elevation in maternal fibrin split products
- Maternal hypofibrinogenemia
- Reference: Int J Obstet Anesth 2011;20:135
Radiology description
- Ultrasound has poor sensitivity for detection of placental abruption (J Ultrasound Med 2002;21:837)
Prognostic factors
- Perinatal mortality of approximately 30% (Acta Obstet Gynecol Scand 2013;92:298)
- Abruption is 10 times more likely to occur in a patient with a previous abruption (Obstet Gynecol 1996;88:309)
Case reports
- 31 year old woman at 28 weeks gestation with thrombotic thrombocytopenic purpura and placental abruption (BMC Pregnancy Childbirth 2020;20:365)
- 32 year old woman at 21 weeks gestation with placental abruption necessitating hysterectomy (BMJ Case Rep 2017;2017:bcr2016218349)
- 35 year old woman at 22 weeks gestation with COVID-19, severe preeclampsia and placental abruption (J Clin Invest 2020;130:4947)
- Woman in her 30s at 25 weeks gestation with placental abruption after multiple amnioreductions for polyhydramnios (BMJ Case Rep 2018;2018:bcr2017222399)
Treatment
- Mild: close observation of maternal stability and reassuring fetal status with preparedness for immediate delivery if either worsens
- Moderate - severe: expedite delivery depending on severity and gestational age (Obstet Gynecol 2006;108:1005)
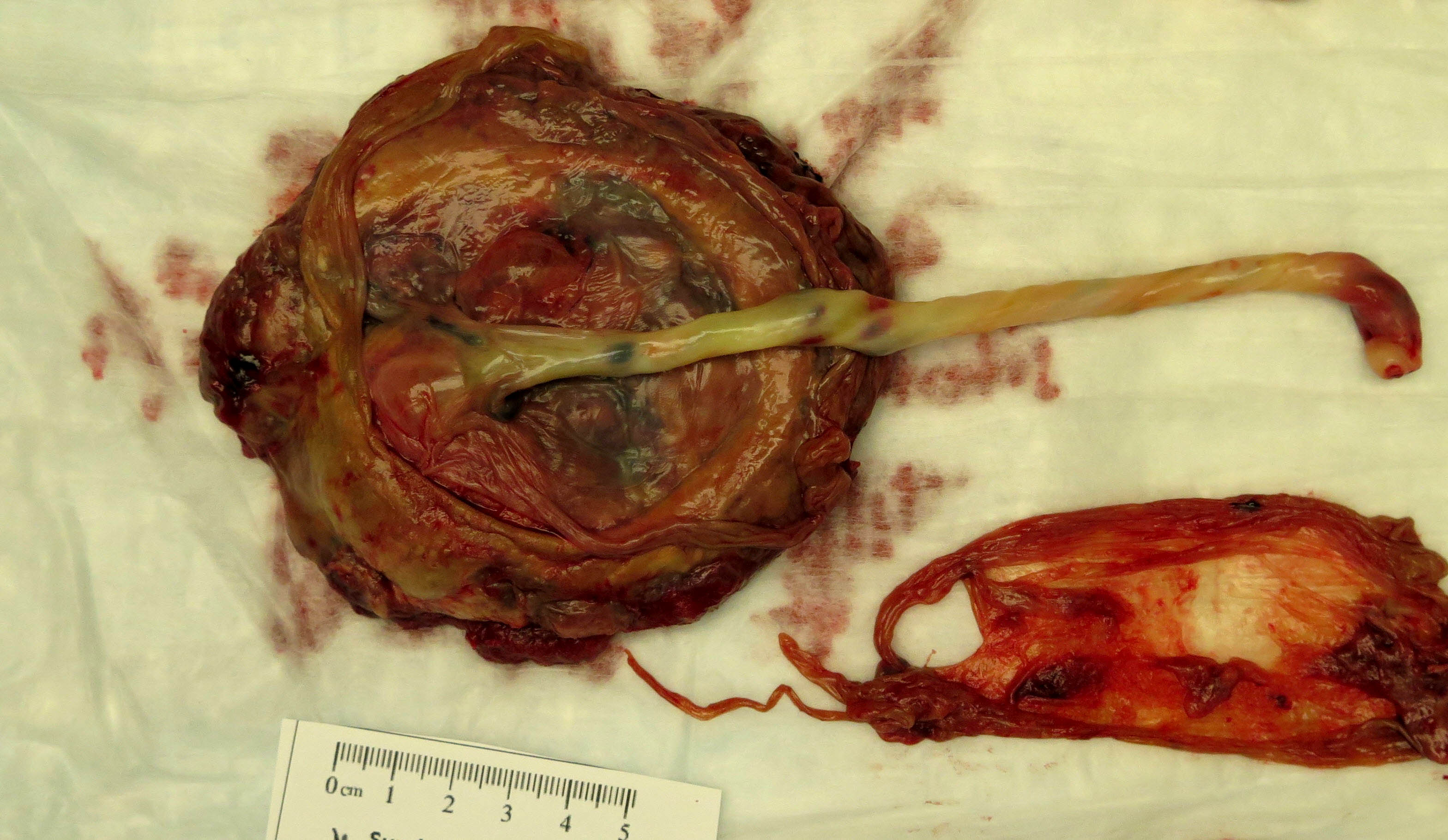
Gross description
- Acute abruption: retroplacental hematoma (central or marginal), with indentation and compression of the surrounding parenchyma
- Very acute abruption may have no gross abnormalities
- Chronic abruption:
- Circumvallate membrane insertion
- Organizing marginal hematoma
- Brown stained membranes (corresponds to hemosiderin deposition)
- Reference: Eur J Obstet Gynecol Reprod Biol 2020;254:188
Gross images
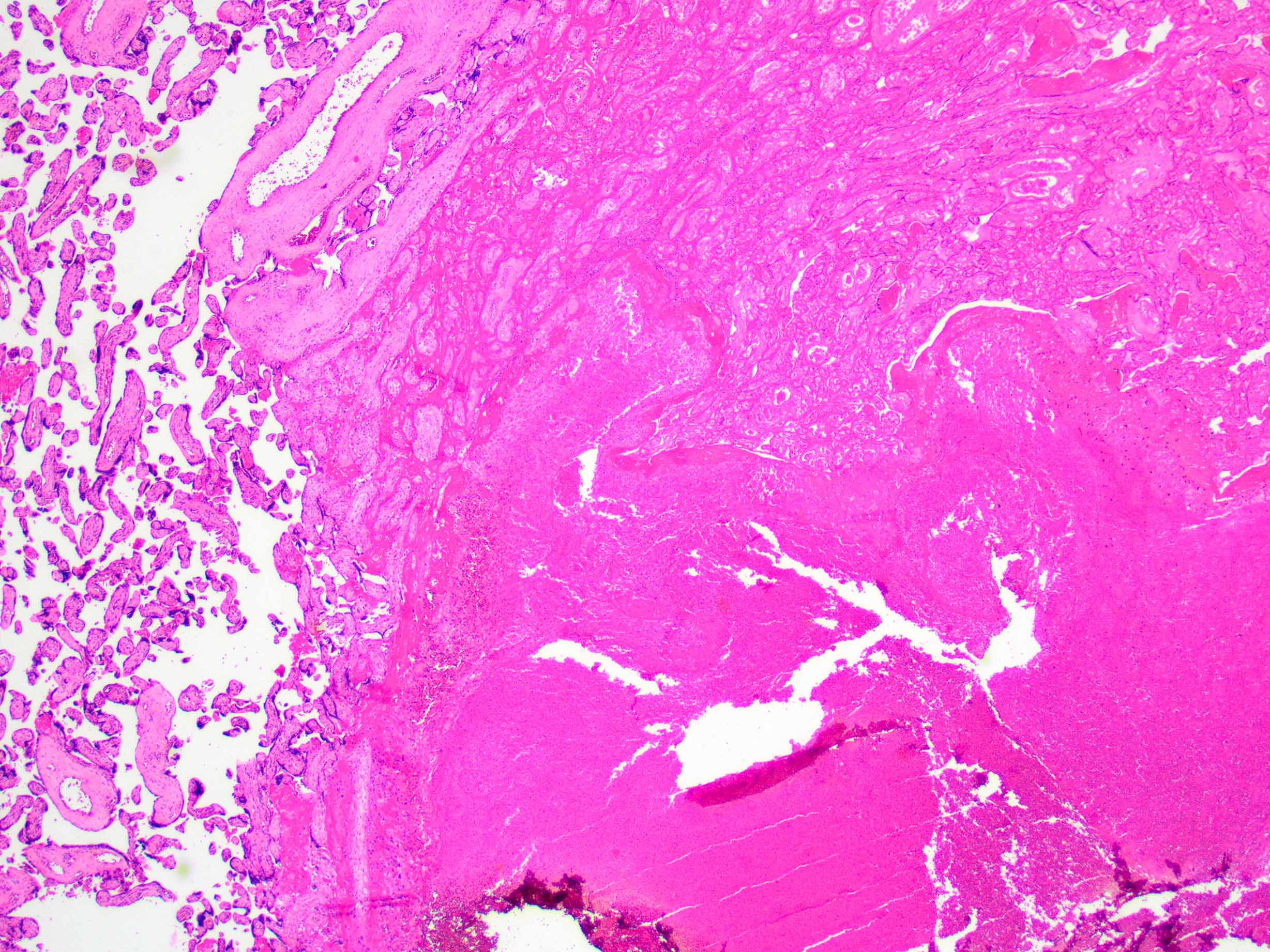
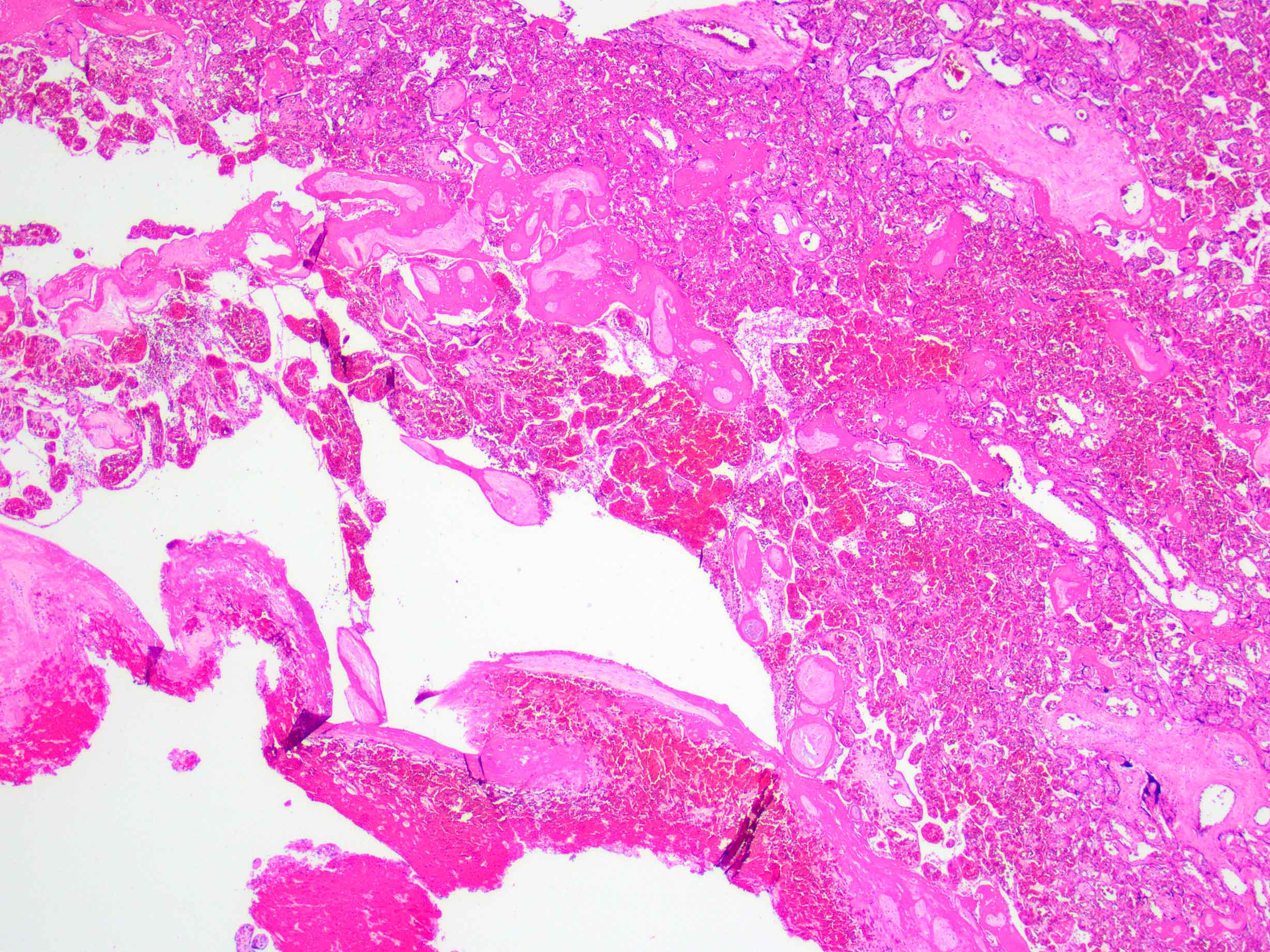
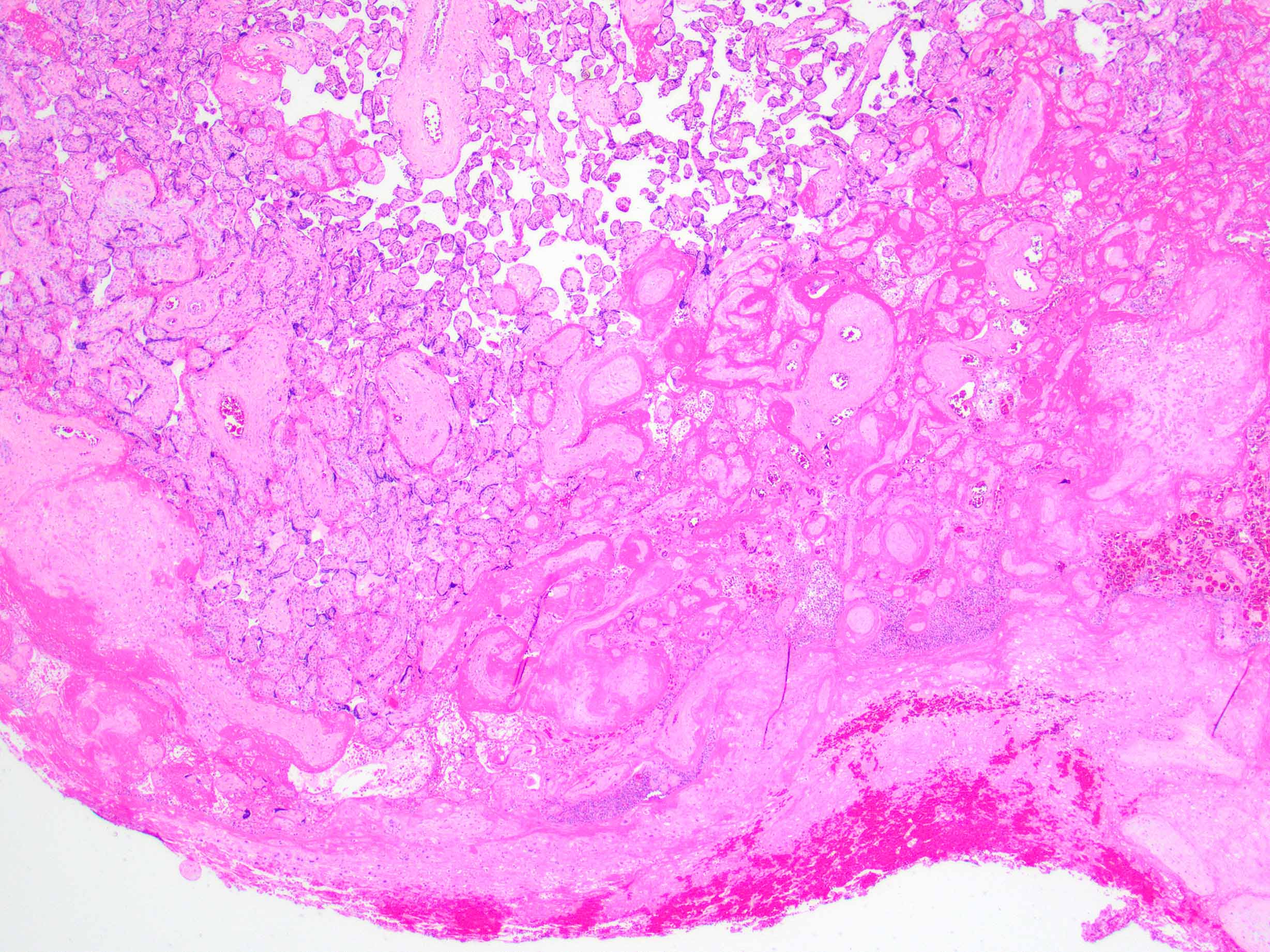
Microscopic (histologic) description
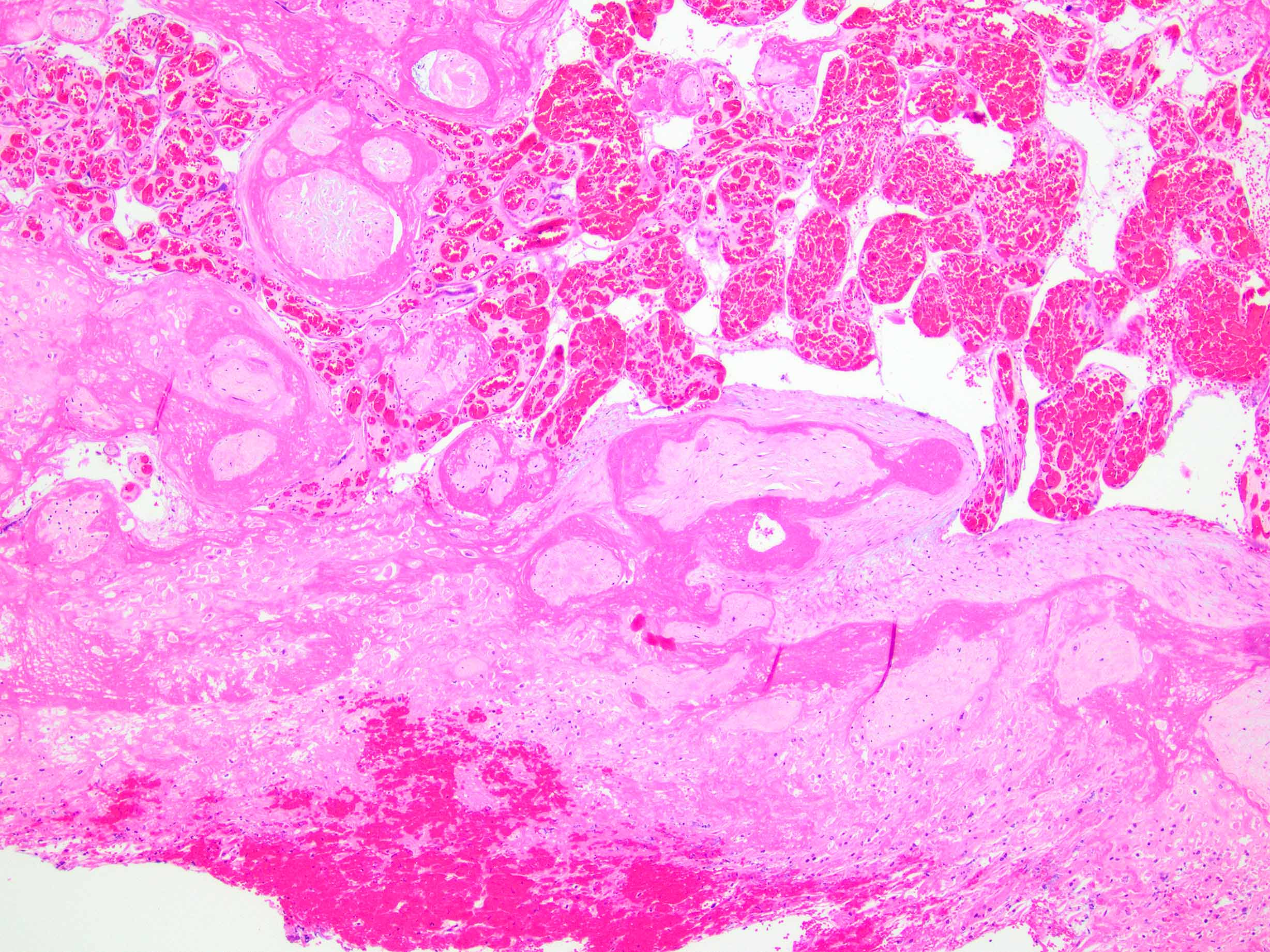
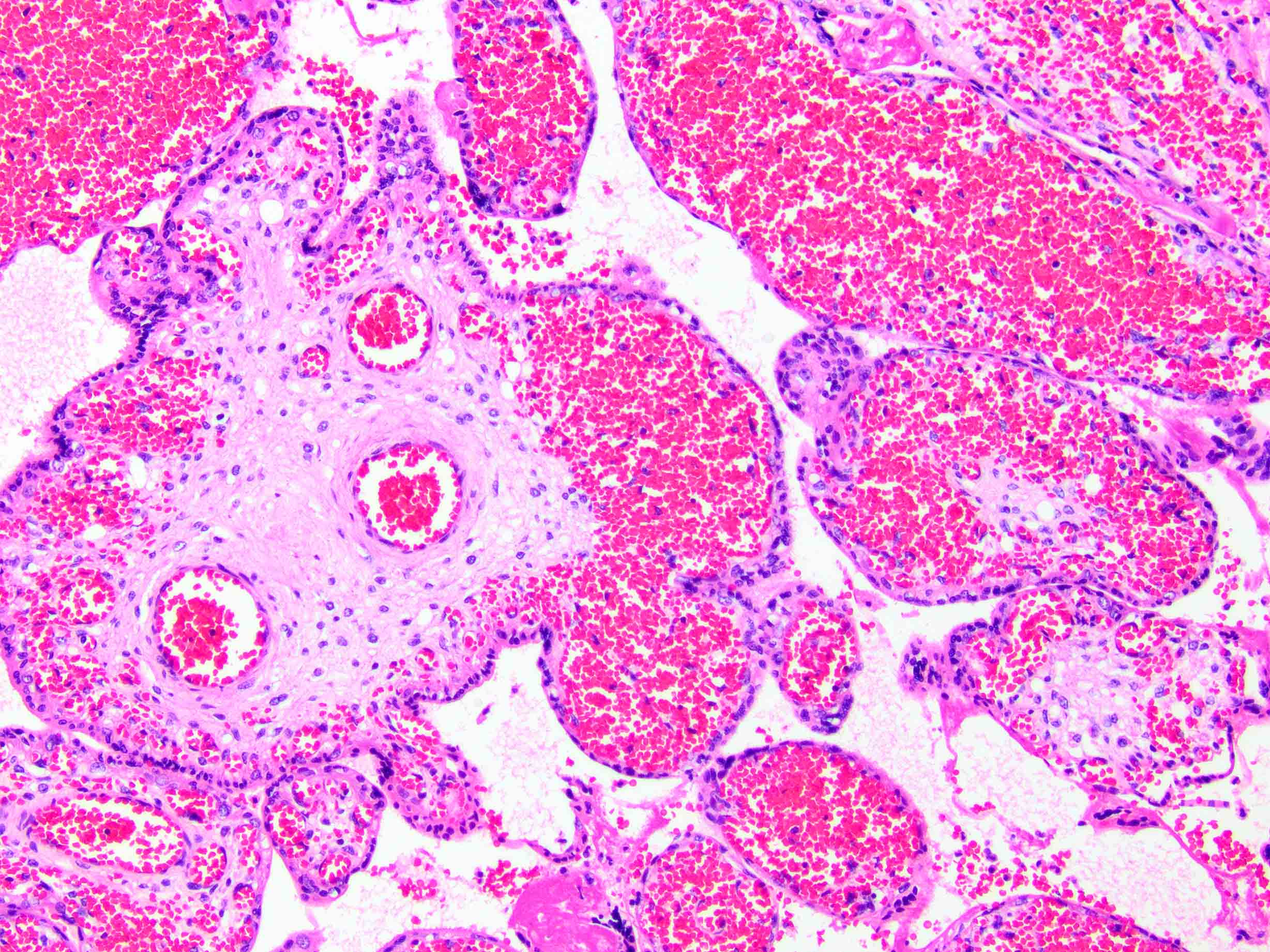
- Acute abruption (Hum Pathol 2017;67:187)
- Decidual or retroplacental hemorrhage / hematoma, with or without extension into the placental parenchyma (intraparenchymal extension)
- Early or well developed infarction of the surrounding placental parenchyma
- Intravillous hemorrhage / villous stromal hemorrhage - red blood cells leak from the villous capillaries and into villous stroma
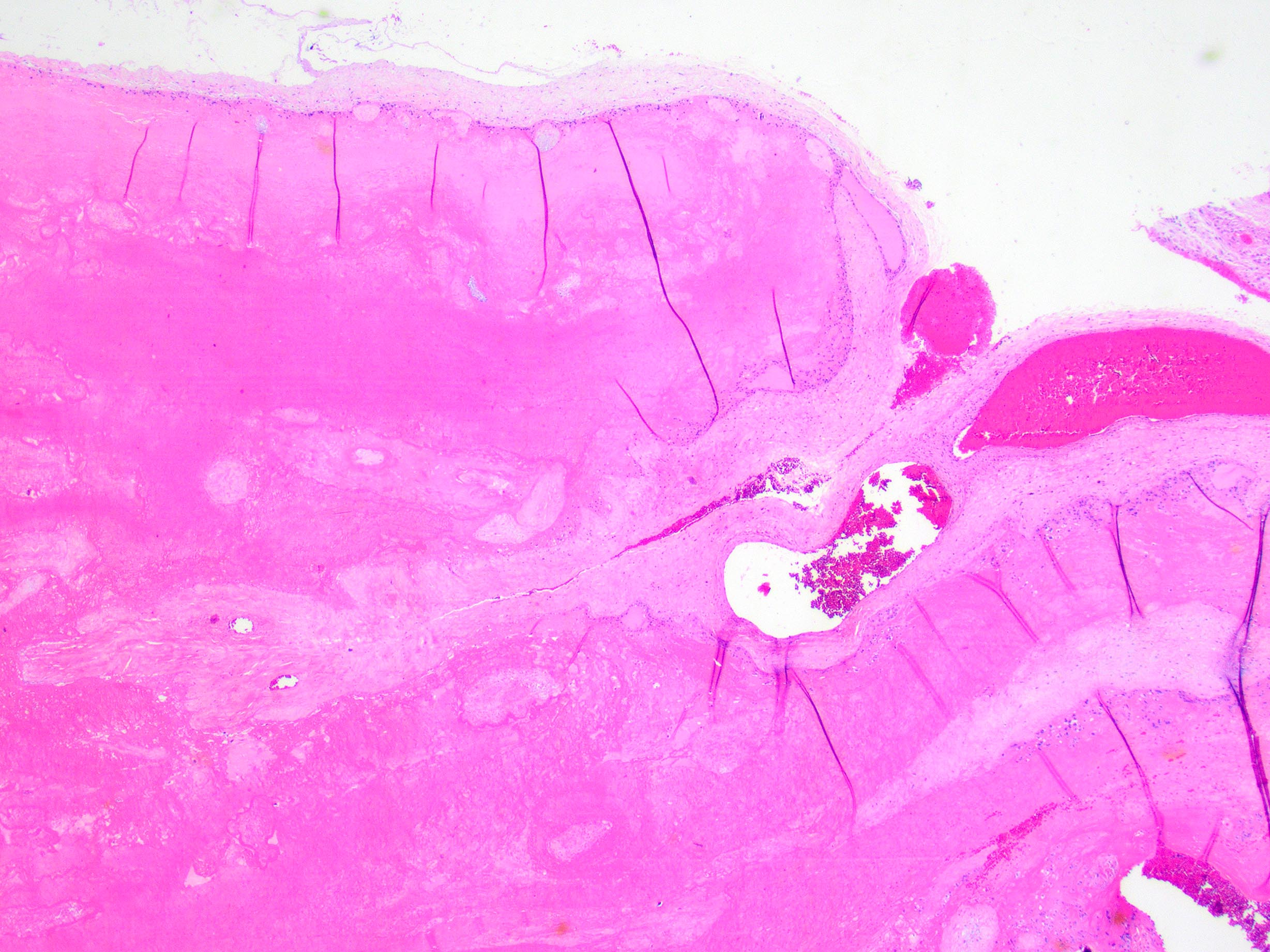
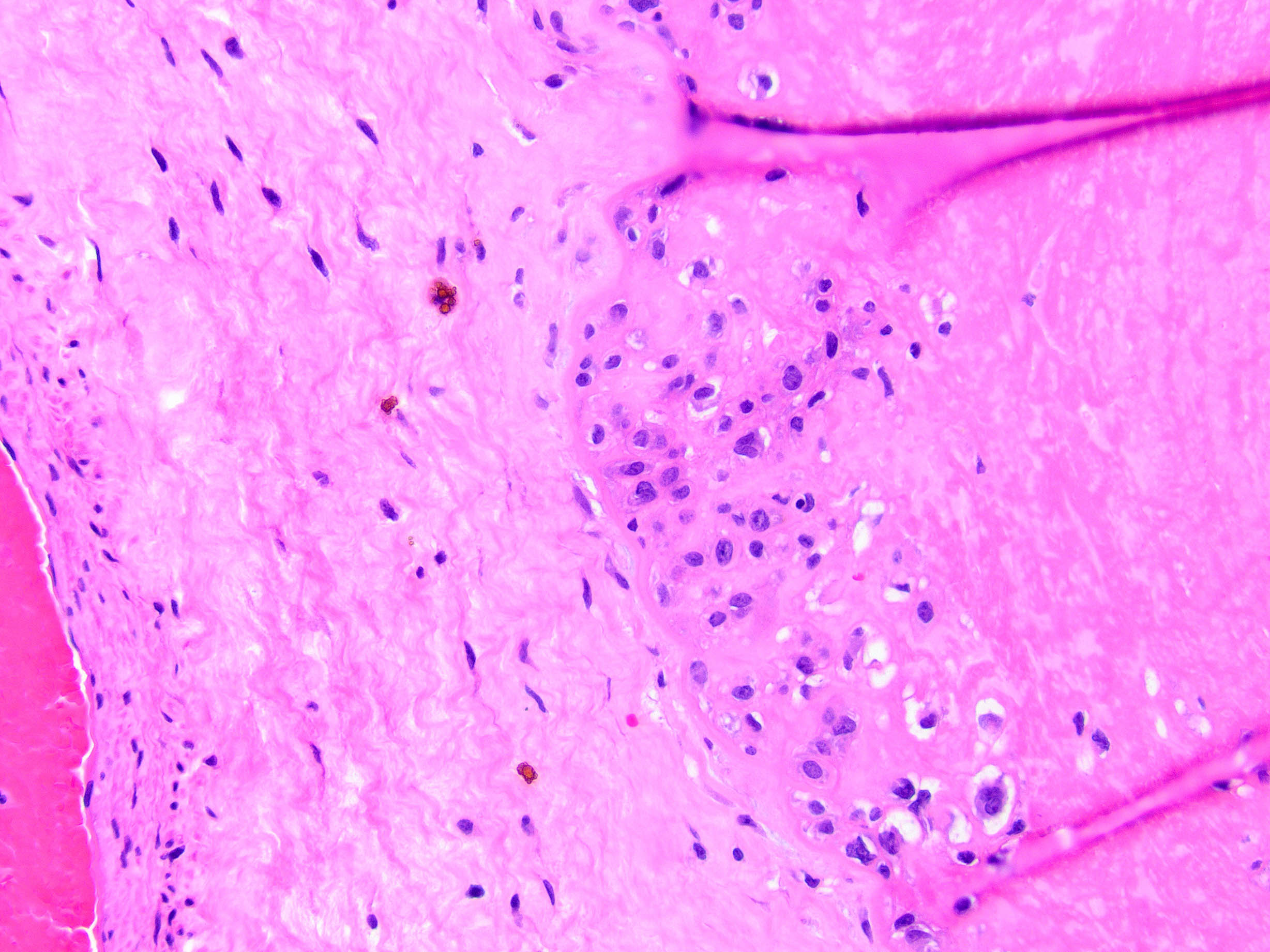
- Chronic abruption (Am J Clin Pathol 1999;111:804)
- Diffuse chorioamniotic hemosiderosis - accumulation of hemosiderin laden macrophages in the free membranes or chorionic plate
- May be confirmed with special stain for iron
- Accumulation of organized clot or fibrin at the margin of the placenta
- Diffuse chorioamniotic hemosiderosis - accumulation of hemosiderin laden macrophages in the free membranes or chorionic plate
Microscopic (histologic) images
Videos
Disseminated intravascular coagulation and placental abruption
Sample pathology report
- Placenta:
- (Immature / slightly immature / mature) placenta (_ g)
- Findings consistent with acute abruption:
- Recent marginal retroplacental hematoma with intraparenchymal extension
- Underlying villous infarction
- Intravillous hemorrhage
- Placenta:
- (Immature / slightly immature / mature) placenta (_ g)
- Findings consistent with chronic marginal abruption:
- Circumvallate membrane insertion
- Remote marginal retroplacental hematoma
- Diffuse chorioamniotic hemosiderosis
Differential diagnosis
- Nonadherent or loosely adhered retroplacental blood clot:
- Easily peeled off the maternal surface - more likely to represent nonpathologic clot
- Parenchymal atrophy or container artifact:
- Areas that may appear grossly similar to parenchymal compression / indentation but are actually areas of atrophy or artifact from the specimen container (especially postfixation)
- Look for gross evidence of infarction or congestion in the area; if in doubt, describe and submit a section
- Villous congestion:
- Look closely at high power to see if the red blood cells are still within the capillary spaces or are in the stroma itself
Additional references
Board review style question #1
A 35 year old woman at 25 weeks gestation presents with vaginal bleeding and nonreassuring fetal heart tracings and undergoes an urgent cesarean section. Gross examination of the placenta demonstrates a large retroplacental hematoma with indentation (see image above). What finding might you expect to see microscopically?
- Chronic villitis
- Delayed villous maturation
- Maternal floor infarction
- Villous stromal vascular karyorrhexis
- Villous infarction
Board review style answer #1
E. Villous infarction
Comment Here
Reference: Retroplacental hematoma with intraplacental extension (abruption)
Comment Here
Reference: Retroplacental hematoma with intraplacental extension (abruption)
Board review style question #2
A 24 year old woman at 23 weeks gestation presents with intrauterine fetal demise. Pathologic examination of the placenta demonstrates a small placenta with foci of intravillous hemorrhage. What clinical syndrome is the mother likely to have?
- Cholestasis of pregnancy
- Gestational diabetes
- Maternal fever
- Placenta previa
- Preeclampsia
Board review style answer #2
E. Preeclampsia
Comment Here
Reference: Retroplacental hematoma with intraplacental extension (abruption)
Comment Here
Reference: Retroplacental hematoma with intraplacental extension (abruption)