Table of Contents
Definition / general | Essential features | Terminology | Diagrams / tables | Clinical features | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Singh K, Cohen MC. Anatomy & histology-placenta & umbilical cord. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentanormalhistology.html. Accessed December 25th, 2024.
Definition / general
- Placenta: fetomaternal organ (derived from the Greek word plakoús, which translates as flat cake) that provides gas exchange, nourishment and protection to the fetus
- Also has excretory and endocrine functions; numerous hormones, such as human chorionic gonadotropin (hCG), progesterone, estrone, estradiol, estriol and human placental lactogen (hPL), are secreted by the placenta
- Umbilical cord: anatomic tubular structure that physically connects the developing intrauterine fetus to the placenta, which is anchored to the maternal uterine wall; it is the cable that links the fetus to the placenta
Essential features
- Umbilical cord is the conduit by which oxygenated, nutrient rich blood from the mother (via the intervening placenta) reaches the fetus and deoxygenated, nutrient poor blood from the fetus is returned back to the mother
Terminology
- Umbilicus (or navel) is the attachment site of the umbilical cord to the fetus
- 2 umbilical arteries in the umbilical cord return deoxygenated blood to the mother
- 1 umbilical vein in the umbilical cord carries oxygenated blood to the fetus
- Wharton jelly, in which the 2 umbilical arteries and single umbilical vein are embedded, is a hydrated extracellular matrix gel composed of open chain polysaccharides distributed in a fine network of microfibrils; it provides turgor regulation and protection to the umbilical cord
Clinical features
- Umbilical cord
- Derived from the allantois and yolk sac during the fifth week of fetal development
- Fetoplacental circulation (connection) develops when allantoic vessels establish continuity with the developing villi of the placenta
- Allantoic duct remnant is seen in ~15% of umbilical cords
- Omphalomesenteric duct remnant is seen in ~1.5% of umbilical cords
- 2 umbilical veins are initially present but one atrophies during the second month of pregnancy
- 2 umbilical arteries, in the vast majority of deliveries (96%), anastomose with 1.5 cm of the placental insertion site
Gross description
- Components of the placenta
- Disc
- Oval to circular in shape and devoid any accessory or succenturiate lobes
- Composed of fetal portion (chorionic plate) and maternal portion (basal plate)
- Weight of the trimmed disc is one of the critical measurements of placentas
- Placental weight and fetoplacental ratio should be compared with values expected for gestational age
- Divided into cotyledons from primary stem villi and lobules from secondary stem villi
- Average weight at term: 510 g
- Chorionic plate
- Usually oval and consists of tan-white tissue overlying the villous parenchyma on the fetal side of the placenta
- Basal plate (maternal surface)
- Has slight gray-tan smooth to pebbled appearance at term
- Membranes
- Grossly, normal membranes are thin, tan-pink and semitranslucent; the amnion is clear and glistening while the chorion is thick and can have slight roughness to it, though it is mostly smooth
- Normal placental insertion into the placental disc is marginate
- Circummarginate insertion is a variation with no clinical significance
- Circumvallation is an extrachorial placenta with a raised margin
- Chorionic plate is smaller than the basal plate
- Misalignment causes hematoma retention in the placental margin
- Associated with poor pregnancy outcome (Obstet Gynecol Int 2014;2014:986230)
- Umbilical cord
- Twisted cable that connects the fetus to the placenta and is composed of Wharton jelly covered by a layer of amnion, 2 muscularized umbilical arteries carrying deoxygenated blood away from the fetus to the placenta and a single large, thin walled vein carrying oxygenated blood from the placenta to the fetus
- Pearly white with smooth and glistening surface on gross examination; no surface nodules, ulcerations or deep grooves
- Insertion on the placenta is normally centrally located by midgestation but may become more eccentric as gestation proceeds
- Long cords (> 70 cm, with > 95 cm considered extremely long) are associated with knots and fetal entanglements (Pediatr Dev Pathol 2001;4:144)
- A short cord (≥ 45 cm) is associated with adverse pregnancy outcomes (Clin Exp Obstet Gynecol 2017;44:216)
- Most cords have a left coil, with an average of 2 coils per 10 cm; the normal range of coiling is 1 - 3 coils per 10 cm
- Coils are different from twists; twists can be untwisted but coils cannot be uncoiled
- Coiling direction is identified by holding the cord perpendicular to the ground and looking at the coils; if the coils go up towards the left (like the left line of the letter V), then that is a leftward coil
- Pseudoknots are normal variations that have no clinical significance; they are vascular tortuosities (ectatic umbilical vein) that may form a mass-like lesion covered in Wharton jelly
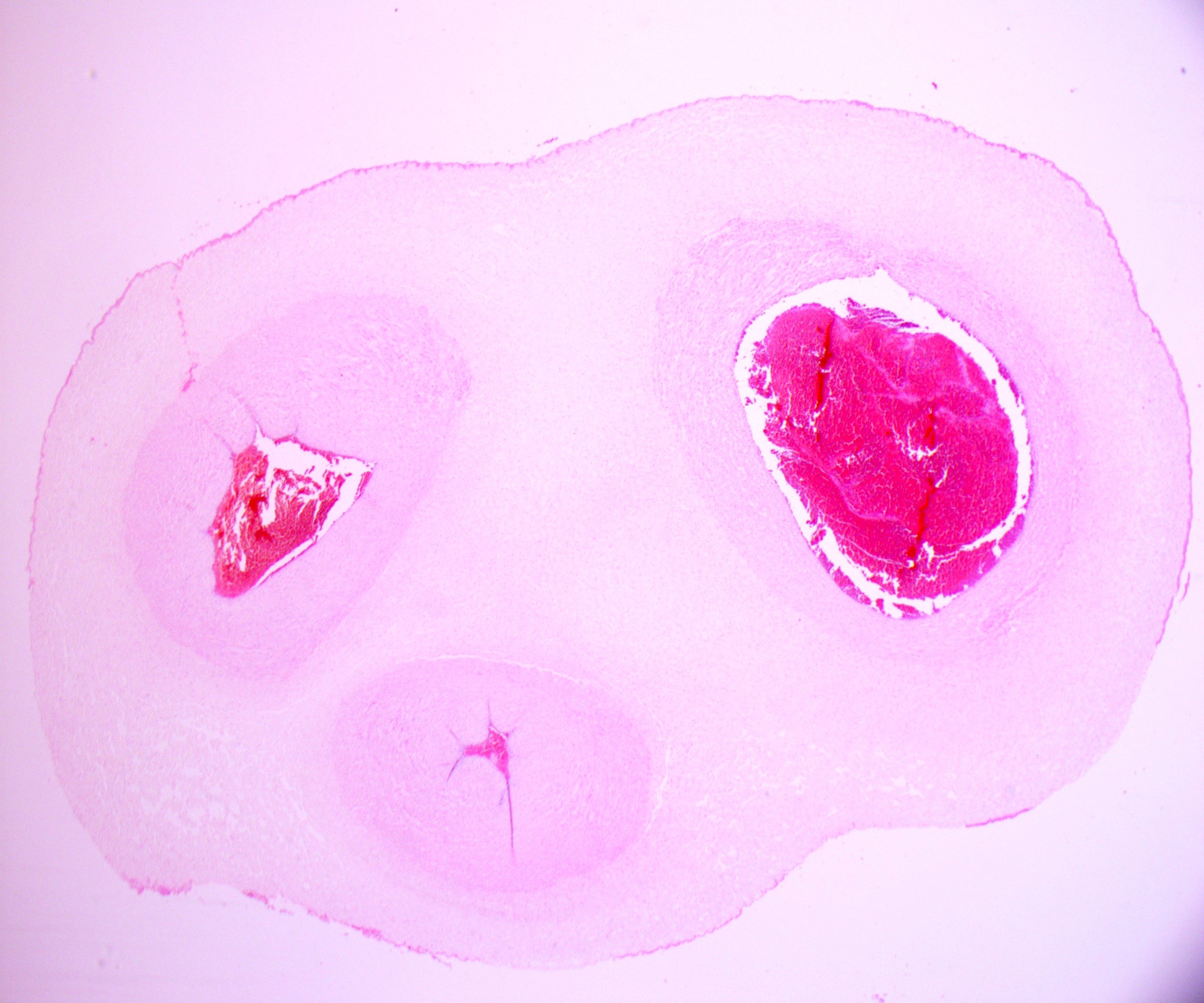
- Disc
Microscopic (histologic) description
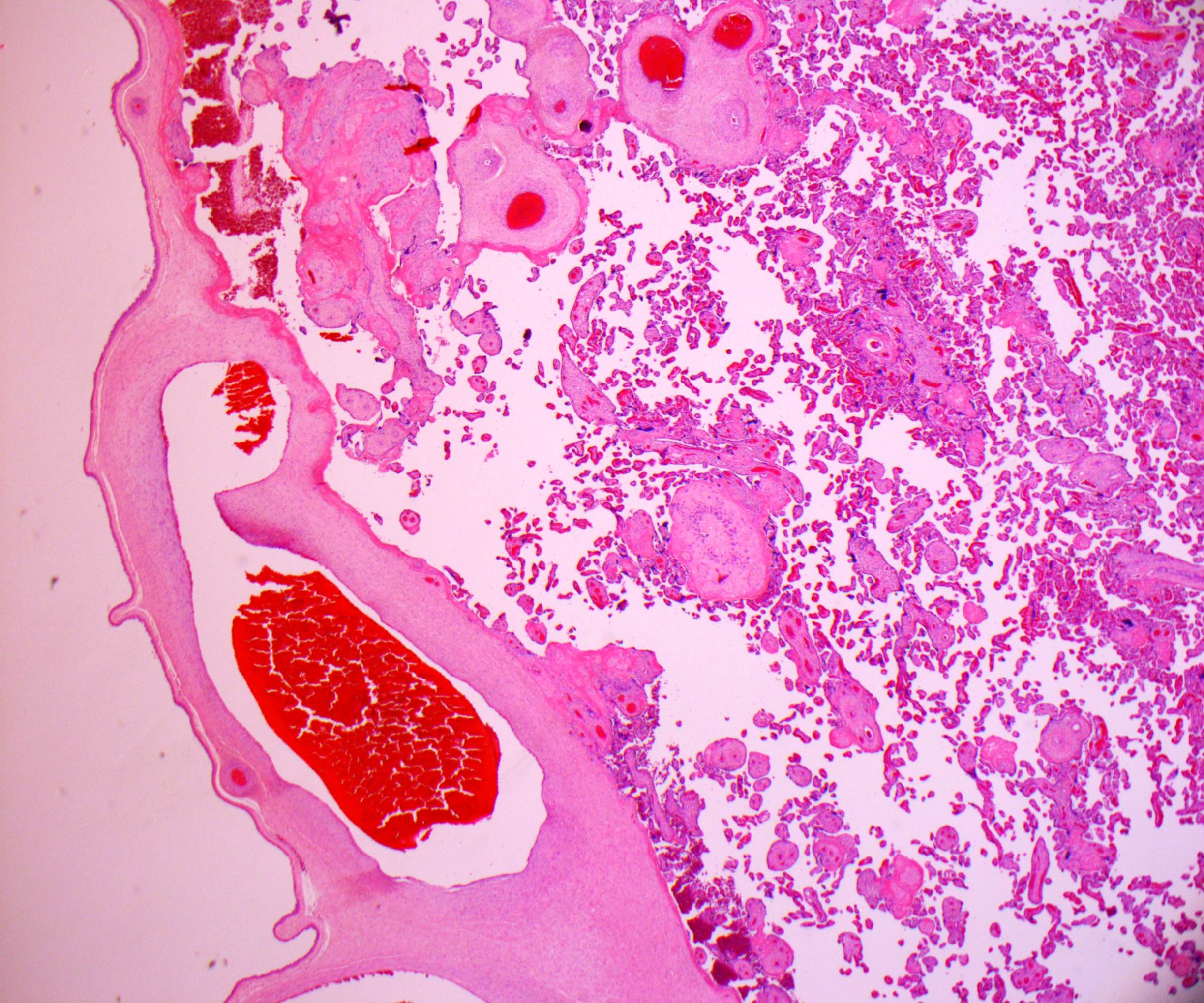
Chorionic plate (fetal surface)
Basal plate (maternal surface)
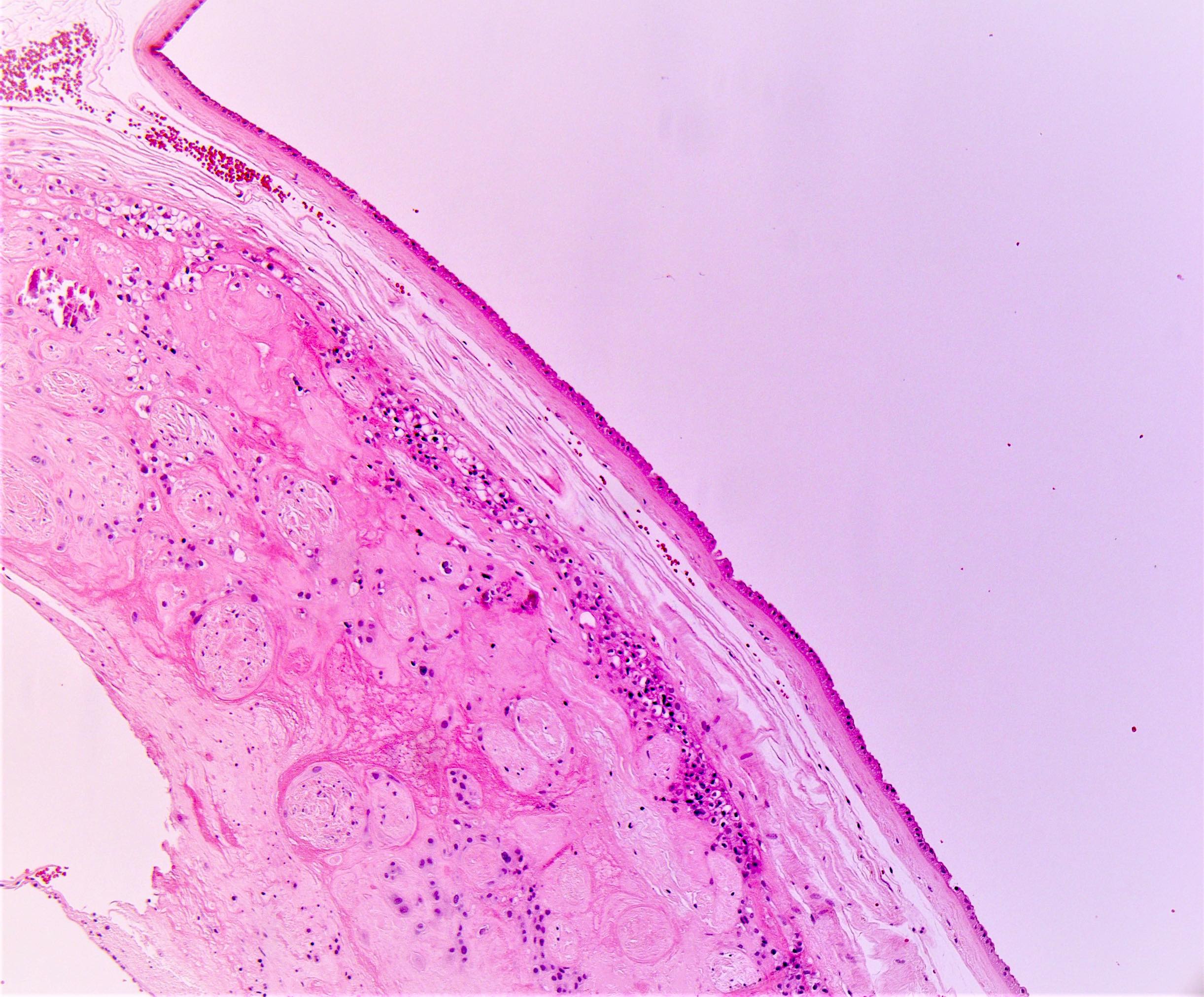
Membranes
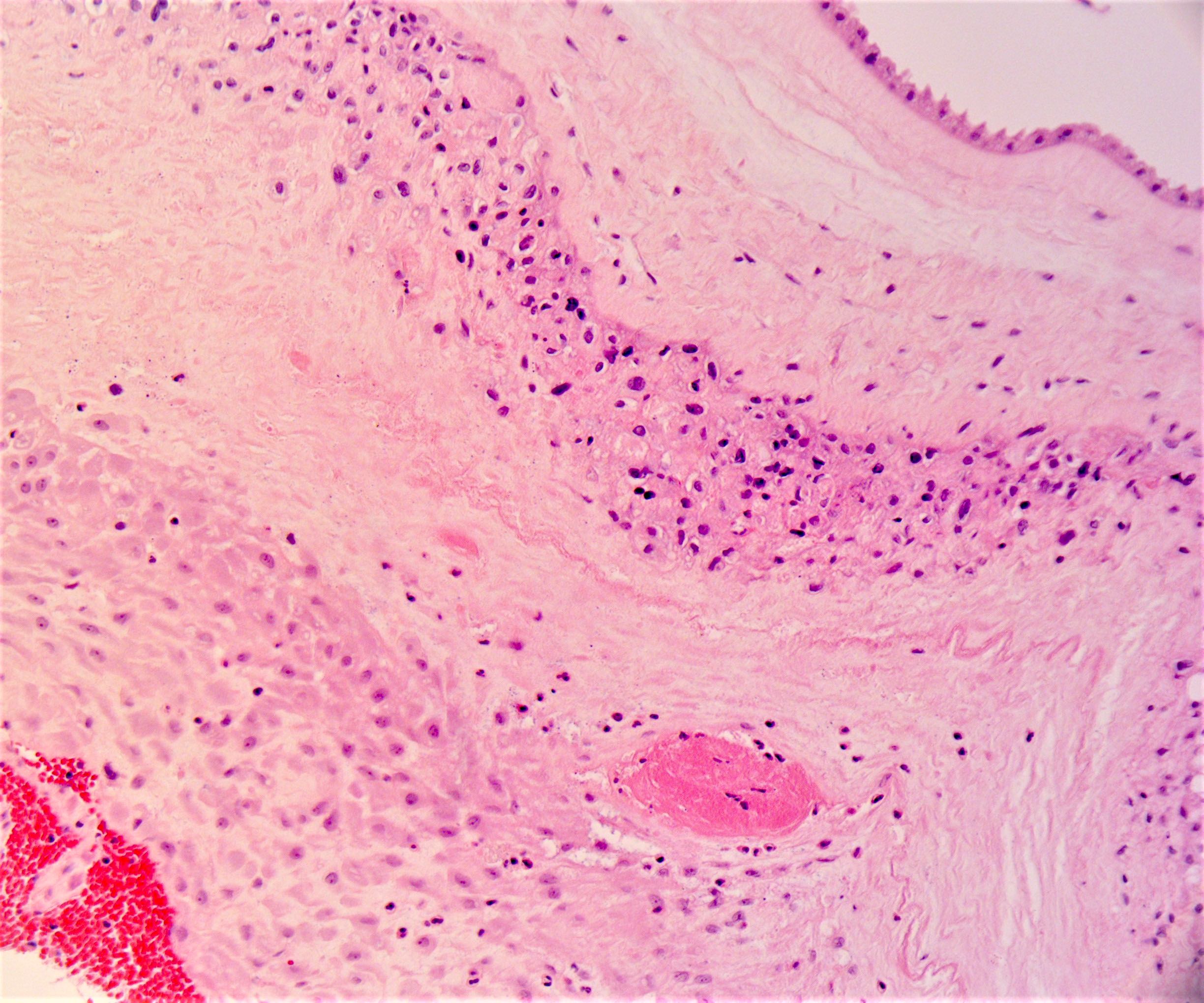
Umbilical cord
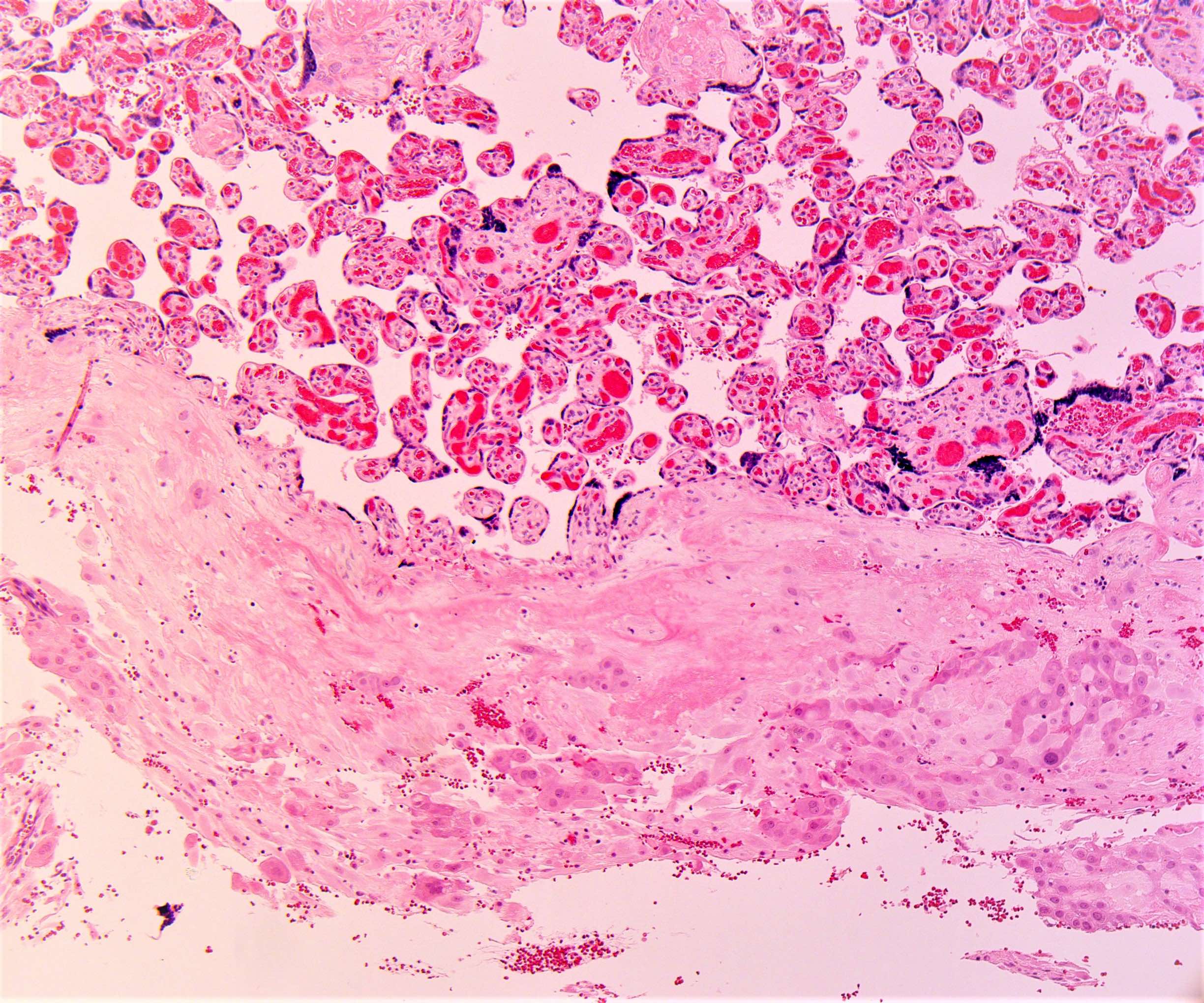
Placental villi
Cytotrophoblast cells
Extravillous (X cells) or intermediate trophoblast cells
Intraplacental trophoblast islands
Syncytiotrophoblast cells
Hofbauer cells
- Covered by a layer of amnion and chorion
- Accumulation of fibrin beneath the chorionic plate is a common finding at term and is visible as tan-white plaques
- Primary stem villi protrude perpendicularly downward from the chorionic plate
- Microscopically, the chorionic plate and stem villi, both primary and secondary, are composed of dense collagenized connective tissue surrounding thick walled arteries and veins
Basal plate (maternal surface)
- Consists of fibrin, extravillous trophoblast cells, decidua basalis and maternal blood vessels
- Endometrial spiral arteries undergo physiological transformation characterized by lumen dilation, extravillous trophoblast invasion of the endothelial lining and fibrinoid replacement of the muscular and elastic tissue of the arterial wall (J Perinat Med 2006;34:447)
- Therefore, maternal spiral arteries transform from high resistance, low capacitance to low resistance, high capacitance vessels
- Maternal veins generally run parallel to the basal plate and are less conspicuous
- Contour of the basal plate is coarsely folded, forming clefts known as placental septa that protrude into the parenchyma and can extend as far as the fetal surface
- Insertion site of the anchoring villi into maternal endometrium
- Invasive intermediate trophoblasts are seen here
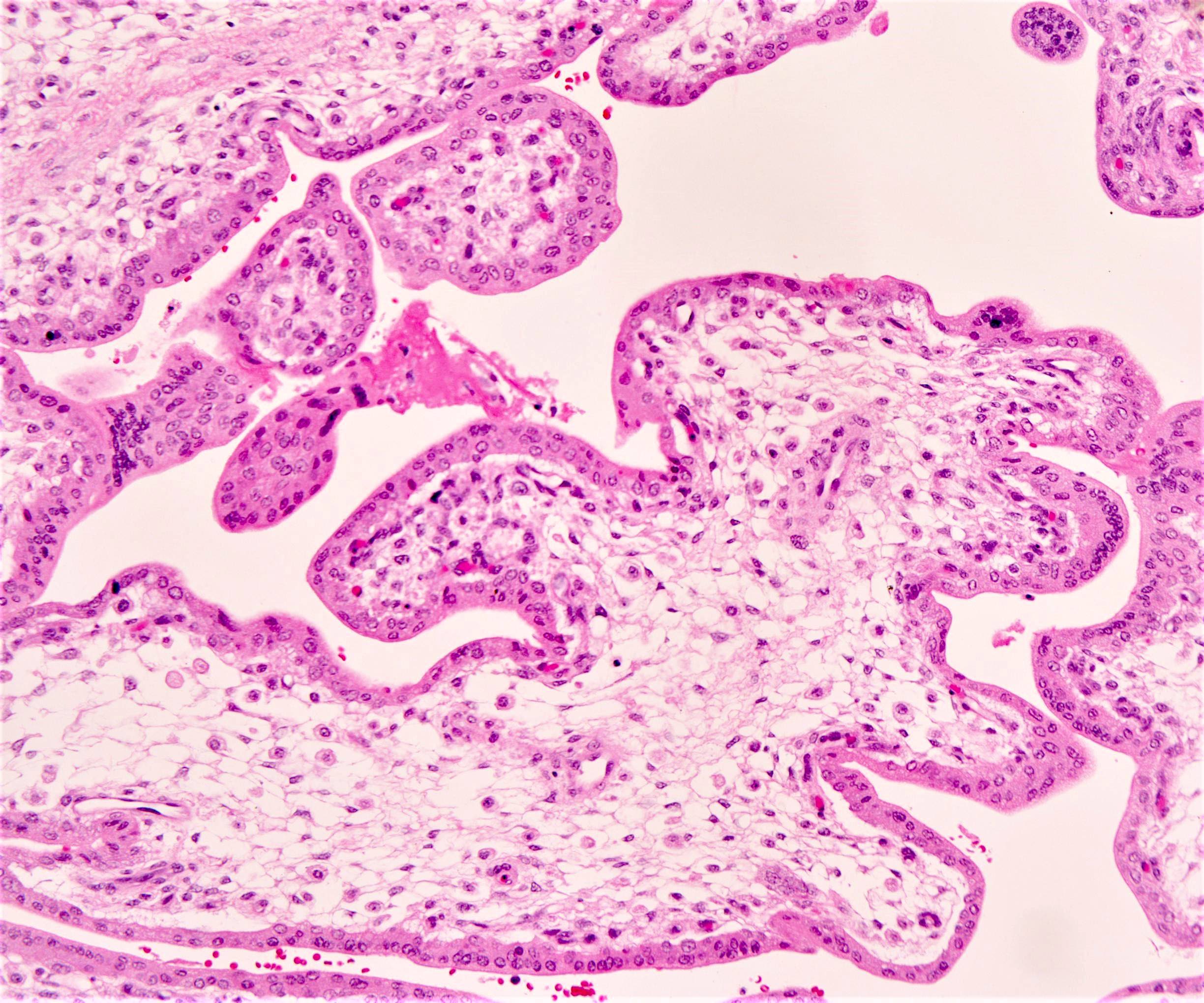
Membranes
- Composed of amnion, intermediate or spongy layer (reticular zone that represents remnants of the coelomic cavity), chorion laeve and chorion frondosum
- Membrane layers adhere together but can be peeled apart with minimal effort
- Amnion: innermost covering of amniotic cavity that is closest to the fetus; thin, avascular layer composed of cuboidal to low columnar epithelial cells that rest on a thin basement membrane with underlying thin band of loose connective tissue (spindled to stellate mesenchymal cells)
- May show squamous metaplasia (plaques of keratinizing, stratified squamous epithelium), especially near umbilical cord insertion
- Present as small gray nodules of 3 - 4 mm in diameter and should be distinguished from amnion nodosum
- Squamous metaplasia is a normal variant (seen in nearly 50% of term placentas), while amnion nodosum is pathological and is strongly associated with longstanding oligohydramnios
- Intermediate or spongy layer: potential space between the amnion and chorion, which results from incomplete fusion of amnionic and chorionic mesoderm during early pregnancy; this intermediate layer is composed of loosely arranged bundles of collagen fibers with a few scattered fibroblasts, separated by a communicating system of clefts and allows the membranes to slide against each other
- Chorion: connective tissue membrane containing fetal vessels, internal to amnion, external to villi
- Membranous chorion (chorion laeve): formed by the collapse of the intervillous space during development; composed of mononuclear, sometimes vacuolated, extravillous trophoblast and scattered atrophic chorionic villi
- Decidual chorion (chorion frondosum): located in the placenta proper; it eventually fuses with the parietal decidua, thereby obliterating the uterine cavity (Front Bioeng Biotechnol 2020;8:610544)
Umbilical cord
- 2 umbilical arteries have slightly thicker, double layered muscular walls without an elastic layer (Fetal Pediatr Pathol 2005;24:297)
- Single umbilical vein has a thinner muscular wall containing a subintimal elastic layer
- Intervening Wharton jelly contains loose ground substance, a fine network of microfibrils and scattered nucleated cells (predominantly macrophages, myofibroblasts and mast cells)
- Umbilical cord is surfaced by a single layer of amnion, which is continuous with the surface of the placenta and the fetal skin
- A single umbilical artery is present in ~1% of cases
- Vessels branch out over the fetal surface to form the villous tree
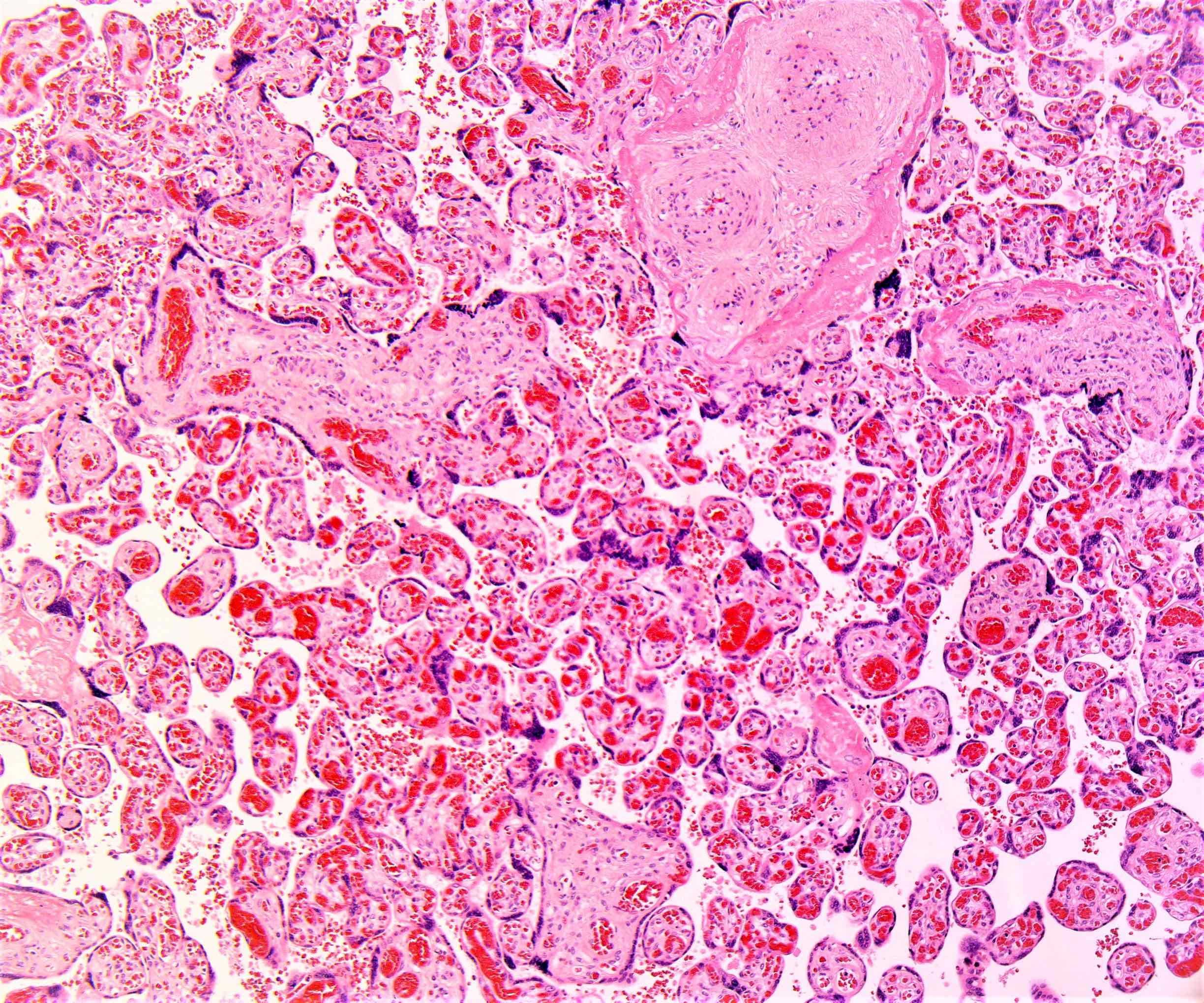
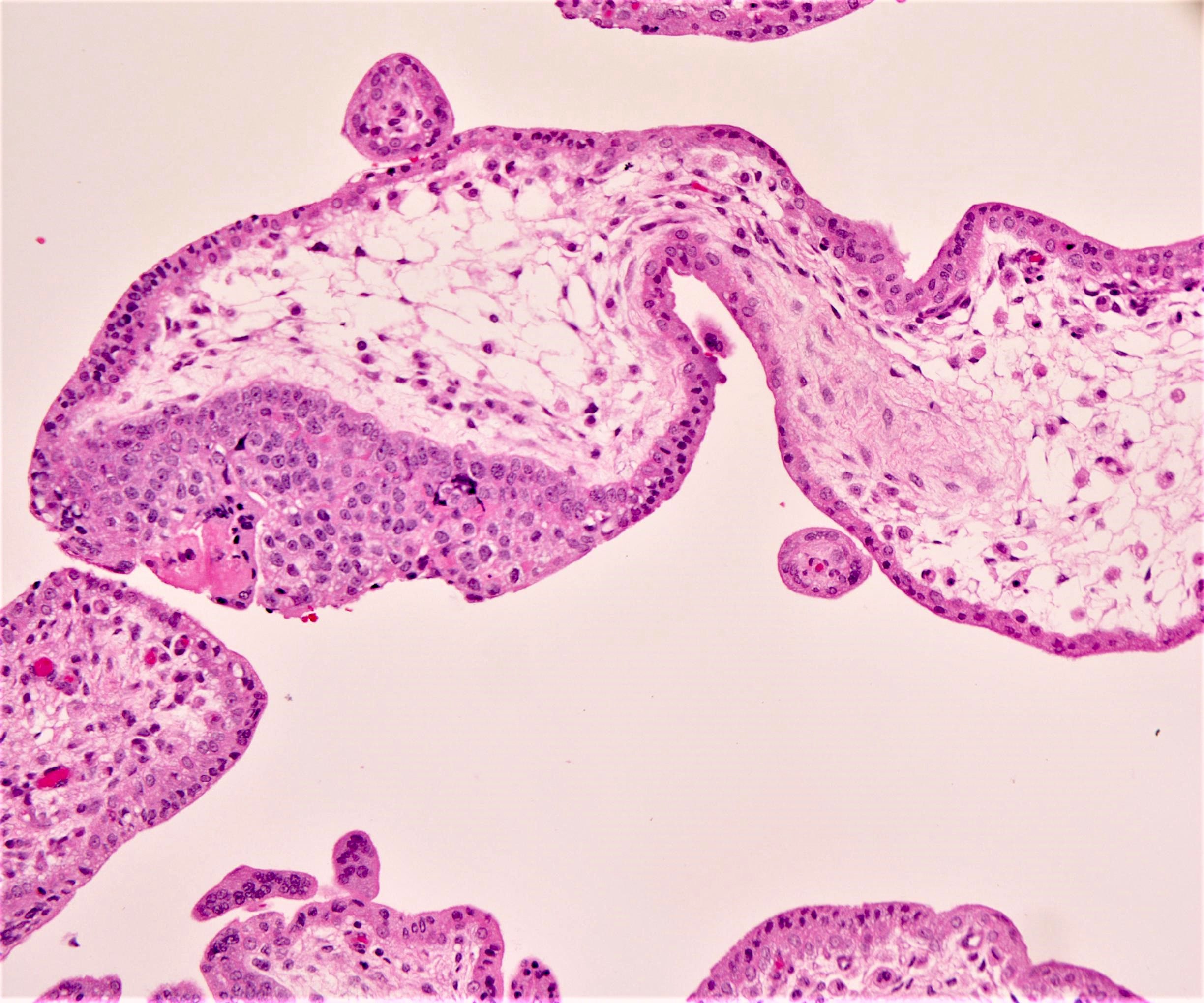
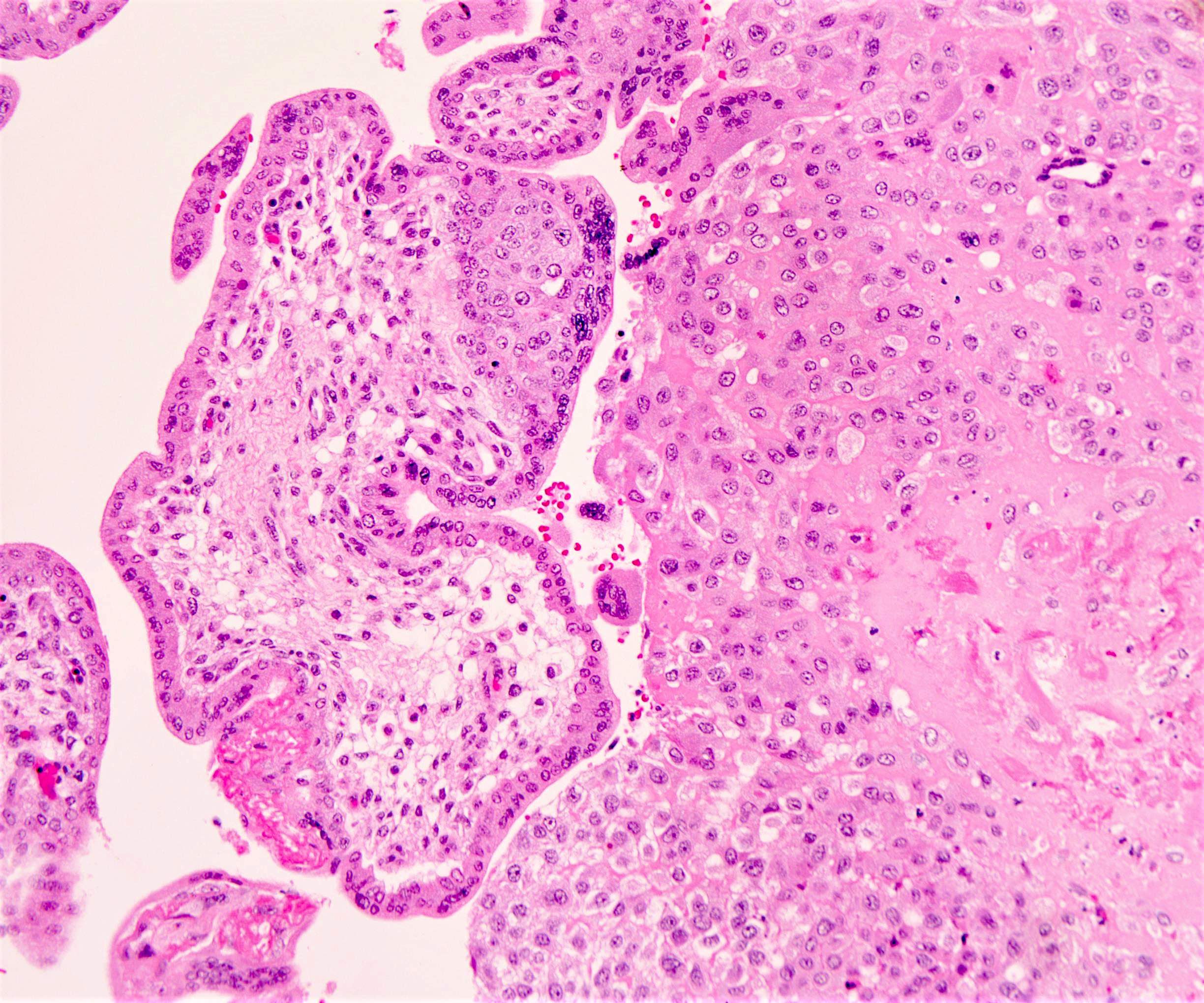
Placental villi
- Comprised of capillaries, fetal macrophages (Hofbauer cells) and perivascular fibroblasts without associated collagen; the surrounding trophoblast bilayer consists of an outer syncytiotrophoblast layer and inner cytotrophoblast layer
- Site of gas exchange, metabolic and endocrine activities
- Dual blood supply from both the fetal and maternal circulations
- Villous trees are made up of ~40 major primary stem villi, each measuring 0.2 - 1.5 mm in diameter, which protrude perpendicularly downward from the chorionic plate; contain arteries, veins, fibrous stroma and capillaries
- Primary villi separate into 4 - 8 secondary stem villi, which travel parallel to the chorionic plate
- These secondary stem villi further divide into tertiary stem villi, which form the placental lobules and insert into the basal plate
- Villi types evolve during pregnancy: immature intermediate villi are dominant in early pregnancy; mature intermediate branch into terminal villi represent the main exchange area of the third trimester placenta
Cytotrophoblast cells
- Present in early gestation; differentiates into villous or extravillous trophoblast and forms syncytiotrophoblasts by fusing on villous surface
- During early pregnancy, this layer is nearly complete but later in gestation it becomes discontinuous and is inconspicuous in term placenta
- Cuboidal, polyhedral or ovoid cells with well demarcated cell borders and large, lightly staining nuclei containing finely dispersed chromatin
- Cytoplasm is usually clear to slightly granular and somewhat basophilic
- Mitotic figures are occasionally found
Extravillous (X cells) or intermediate trophoblast cells
- Old literature described extravillous trophoblast as intermediate trophoblast, as the morphology appeared intermediate between cytotrophoblast and syncytiotrophoblast
- Infiltrate decidua and myometrium of placental site, invade and replace spiral arteries of the basal plate to establish maternal - fetal circulation and keep vessels patent (Cell Mol Life Sci 2019;76:3479)
- Form trophoblastic shell
- Secrete parathyroid hormone (PTH) related protein
- Located in the basal plate, septa and chorion laeve; morphology varies by location
- In the basal plate, they are enlarged polyhedral to spindle cells with abundant amphophilic and vacuolated cytoplasmic and large, hyperchromatic nuclei; may resemble adjacent decidua
- In myometrium, they are more spindled and resemble adjacent smooth muscle cells; may fuse to become multinucleated cells
Intraplacental trophoblast islands
- Form the inner layer of the villous trophoblastic mantle and play an important role in maintaining the structural integrity of the villi
- Serve as a source from which implantation site and chorionic type intermediate trophoblast cells are derived
- Larger than cytotrophoblasts, mononucleate, polygonal, abundant pale to clear cytoplasm, distinct cell borders and single nuclei
- Frequently, the islands contain villous remnants with perivillous fibrin
Syncytiotrophoblast cells
- Single, continuous, normally uninterrupted layer that extends over the surfaces of all villous trees and chorionic villi as well as over parts of the inner surfaces of chorionic and basal plates
- Synthesize and secrete hCG, hPL
- Multinucleated giant cells with abundant homogeneous to finely granular, somewhat basophilic cytoplasm, often with multiple intracytoplasmic vacuoles and small dense pyknotic nuclei with moderately dense chromatin
Hofbauer cells
- Fetal macrophages located in villous stroma
- 10 - 35 μm in diameter
- Present from 18 days postconception and throughout gestation
- 4 subtypes according to differences in the expression of major histocompatibility complex (MHC) type II complement receptors, lectins, lipopolysaccharide coreceptor (CD14) and CD68 (Anal Quant Cytopathol Histpathol 2013;35:283)
- Round to ovoid cells with eccentric nuclei and granular cytoplasm with many vacuoles containing flocculent material and occasional osmiophilic bodies
- Their most important function is the immunological defense of the fetus and the prevention of vertical transmission of pathogens
Microscopic (histologic) images
Positive stains
- Cytotrophoblast cells (early placenta): AE1 / AE3 (keratin), Ki67 (25 - 50%), p63, cyclin E, beta catenin (nuclear), SALL4, EGFR, E-cadherin and integrins alpha 6 and beta 4
- Extravillous (X cells) or intermediate trophoblast cells: cytokeratin, HSD381, HLA-G, HLA-C, HLA-E, hPL, beta hCG (positive in multinucleated cells), cyclin E, MEL-CAM, beta catenin (weak), MUC4, ASCL2, integrin alpha 5, integrin beta 1, inhibin alpha, PLAP (weak)
- Intraplacental trophoblast islands: cytokeratin, EMA, HNK1, HLA-G, hPL (increased expression towards the implantation site) and MEL-CAM (in cells with eosinophilic cytoplasm; towards distal end only), PLAP (in clear cells), MUC4, cyclin E (increased expression towards the implantation site), beta catenin (membranous)
- Syncytiotrophoblast cells: beta hCG, hPL, inhibin alpha, HSD381, ER, PR, PDL1
Negative stains
- Cytotrophoblast cells (early placenta): EMA, beta hCG, HLA-G, HNK1, hPL, inhibin alpha, MEL-CAM (CD146), PLAP, HSD381, MUC4, ER, PR, PDL1
- Extravillous (X cells) or intermediate trophoblast cells: EMA (usually), Ki67, p63, EGFR, E-cadherin, HNK1, integrins alpha 6 and beta 4
- Intraplacental trophoblast islands: EMA, beta hCG, PLAP, p63
- Syncytiotrophoblast cells: HLA-G, Ki67, MEL-CAM, PLAP, E-cadherin, HNK1, beta catenin, p63, cyclin E
Electron microscopy description
- Syncytiotrophoblast cells: vacuoles are due to dilated endoplasmic reticulum and lacunae from plasma membrane infoldings
Additional references
Board review style question #1
Placenta product of a concealed pregnancy is submitted for assessment of the gestational age. The trimmed placental weight is 51 grams. The histology shows a prevalence of intermediate immature villi with presence of extravillous (intermediate) trophoblast. What is the most likely gestational age of the placenta?
- 12 weeks
- 26 weeks
- 36 weeks
- 40 weeks
- 42 weeks
Board review style answer #1
A. 12 weeks gestation. Immature intermediate villi are dominant in early pregnancy (first trimester). The presence of extravillous trophoblast invades the uterus during implantation. Answers B - E are incorrect because these features would likely not be present by the gestational age listed.
Comment Here
Reference: Anatomy & histology-placenta & umbilical cord
Comment Here
Reference: Anatomy & histology-placenta & umbilical cord
Board review style question #2
In which placental compartment is the Wharton jelly present?
- Basal plate
- Chorionic plate
- Membranes
- Umbilical cord
- Villi
Board review style answer #2
D. Umbilical cord. Intervening Wharton jelly contains loose ground substance, a fine network of microfibrils and scattered nucleated cells (predominantly macrophages, myofibroblasts and mast cells). Answers A - C and E are incorrect because Wharton jelly is not present in these placental compartments.
Comment Here
Reference: Anatomy & histology-placenta & umbilical cord
Comment Here
Reference: Anatomy & histology-placenta & umbilical cord