Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mendoza R, Lanjewar S, Gupta R. Complete hydatidiform mole. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentacompletemole.html. Accessed April 24th, 2024.
Definition / general
- Complete hydatidiform mole is a gestational trophoblastic disease characterized by diffuse hydropic enlargement and trophoblastic proliferation of the chorionic villi
Essential features
- Proliferative disorder of the placenta, resulting in villous hydrops and trophoblastic hyperplasia without embryonic development
- Diploid paternal only genome
- Ultrasonography shows characteristic snowstorm appearance
- Patients typically present with abnormal ultrasound, vaginal bleeding or a missed abortion
- Trophoblastic neoplasia (invasive mole or choriocarcinoma) follows complete mole in 15 - 20% of cases
Terminology
- Molar pregnancy, complete mole
ICD coding
- ICD-10: O01.9 - hydatidiform mole, unspecified
Epidemiology
- 1 - 3 in 1,000 pregnancies in North America and Europe (Geburtshilfe Frauenheilkd 2015;75:1043)
- Incidence is 3 - 4 times higher in Asia, Africa and Latin America (4.2/1,000 in Nepal, 12.5/1,000 in Taiwan, 11.5/1,000 in Indonesia, 5/1,000 in Brazil, 6/1,000 in Nigeria) (BJOG 2003;110:555, Gynecol Oncol Res Pract 2015;2:9, Epidemiol Rev 1984;6:52, Radiol Bras 2016;49:241, Niger Med J 2011;52:223)
- Risk factors:
- Extremes of maternal age, < 20 years old and > 35 years old (Eur J Gynaecol Oncol 2005;26:207)
- Previous molar pregnancy (Hum Reprod 2015;30:2055)
- Previous spontaneous abortions or infertility (Mod Pathol 2020;33:880)
- Diet deficient in carotene (vitamin A precursor) and animal fats (Placenta 2015;36:48, Clinics (Sao Paulo) 2020;75:e1724)
- Smoking (Am J Epidemiol 1985;121:457)
- Genetic predisposition (Mod Pathol 2018;31:1116)
Sites
- Placenta
Pathophysiology
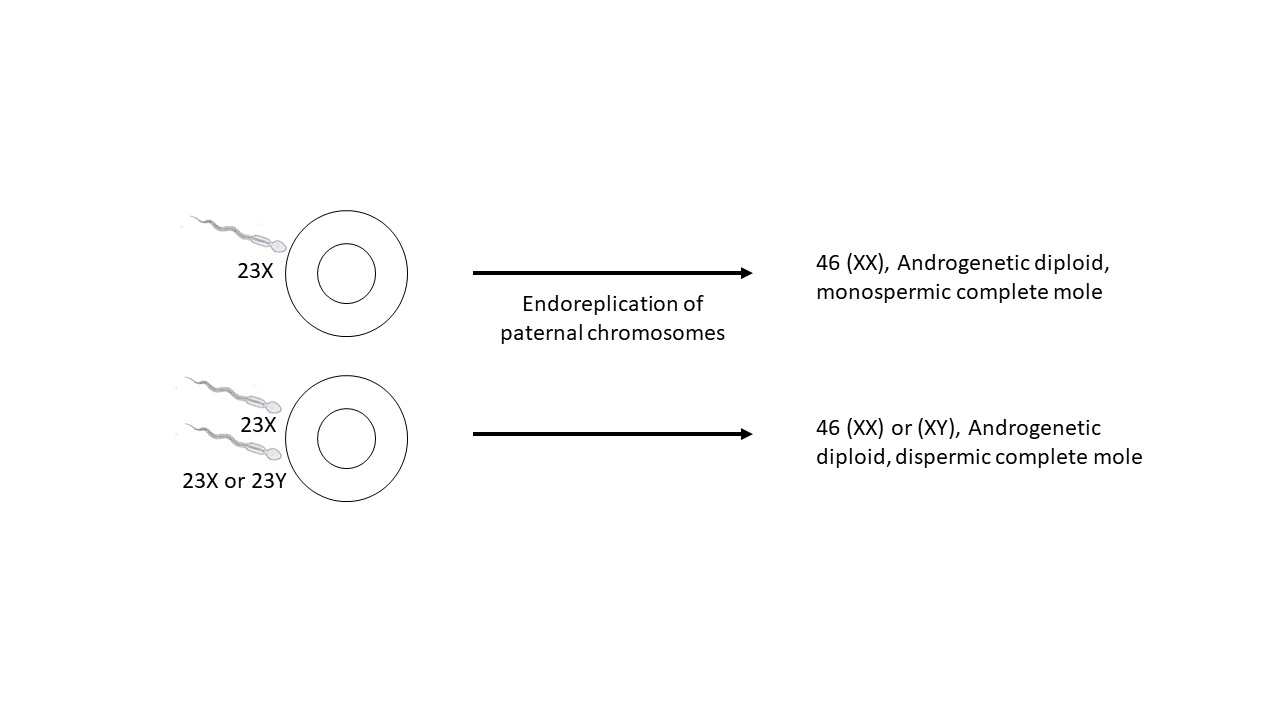
- A complete mole occurs when an empty ovum is fertilized by a sperm
- About 80% of complete hydatidiform moles are 46XX, which originate from duplication of the chromosomes of a haploid sperm; the other 20% are 46XY; all the chromosomes are paternally derived
- Although all chromosomes are paternally derived, mitochondrial DNA remains maternal in origin
- Maternal recessive mutations in NLRP7 (75%) and KHDC3L (5%) are associated with familial biparental recurrent hydatidiform mole (Mod Pathol 2018;31:1116)
Etiology
- Abnormal gametogenesis and fertilization
Diagrams / tables
Clinical features
- Abnormal vaginal bleeding ("prune juice" appearance) during the first trimester
- Ovarian theca lutein cysts > 6 cm in diameter
- The uterus is typically significantly enlarged for gestational age
- Elevated human chorionic gonadotropin level for gestational age
- Early onset of medical complications, such as pregnancy induced hypertension, hyperthyroidism and hyperemesis gravidarum
- Reference: Am J Obstet Gynecol 2010;203:531
Diagnosis
- Pelvic ultrasound
- Dilation and curettage / evacuation
Laboratory
- Elevated serum quantitative human chorionic gonadotropin (hCG) level, typically greater than 100,000 international units (IU)
- Elevated thyroid panel (if signs and symptoms of hyperthyroidism present)
- Elevated liver function tests and proteinuria (if preeclampsia is suspected)
- Anemia and thrombocytopenia in complete blood count (CBC)
- Reference: Am J Obstet Gynecol 2010;203:531
Radiology description
- Pelvic ultrasound shows:
- Heterogeneous, hyperechoic mass in the uterine cavity with multiple anechoic spaces ("snowstorm appearance")
- Absence of embryo or fetus
- Absence of amniotic fluid
- Ovarian theca lutein cyst
- Reference: Radiographics 2017;37:681
Prognostic factors
- 1% recurrence risk (Hum Reprod 2015;30:2055)
- After a molar pregnancy, the risk of a second complete mole rises to 1 - 2%; after two molar pregnancies, the risk of a third mole is 15 - 20%, which is not decreased by having a different partner (Gynecol Oncol 1999;75:224)
- 15 - 20% risk of progressing to gestational trophoblastic neoplasia; 10 - 15% invasive mole, 2 - 3% choriocarcinoma (Gynecol Oncol 2009;112:654)
- 50% of choriocarcinoma cases arise from complete mole (Am J Obstet Gynecol 2010;203:531)
- Progression risk is higher:
- Signs of trophoblastic proliferation (uterine size greater than gestational age, serum hCG levels > 100,000 milli-international units/mL, ovarian theca lutein cysts > 6 cm in diameter)
- Age > 40 years
- Dispermic complete mole
Case reports
- 33 year old woman with a history of sudden onset of right iliac fossa pain and mild vaginal bleeding following 8 weeks amenorrhea and a positive pregnancy test (BMJ Case Rep 2018;2018:bcr2018225545)
- 34 year old Japanese woman who was pregnant with a hydatidiform mole and two coexisting fetuses (J Med Case Rep 2019;13:256)
- 42 year old primigravida woman with multiple metastatic gestational trophoblastic disease after a twin pregnancy with complete hydatidiform mole and coexisting fetus, following assisted reproductive technology (Taiwan J Obstet Gynecol 2018;57:588)
Treatment
- Uterine evacuation of gestational tissue (mechanical dilation of the cervix, followed by electric suction aspiration and then sharp curettage to help assure complete evacuation of molar tissue)
- Medication only methods of uterine evacuation (misoprostol, mifepristone, oxytocin) should NOT be used (Gynecol Oncol 2000;78:309)
- Postevacuation serial serum quantitative hCG measurements, every 1 - 2 weeks until 3 consecutive tests are normal, followed by hCG measurement at 3 month intervals for 6 months
- Hysterectomy
- Prophylactic chemotherapy
- Methotrexate and actinomycin D
Gross description
- Bulky, bloody tissue with hydropic changes in all villi, which appear as semitransparent vesicles of variable size
- Classically described as a "bunch of grapes", the individual vesicles measure anywhere from 1 to 30 mm in diameter and the total weight is usually over 200 g
- Normal placental structures or fetal parts are absent
- Early complete moles may not have gross evidence of abnormal villi
- Reference: APMIS 2018;126:647
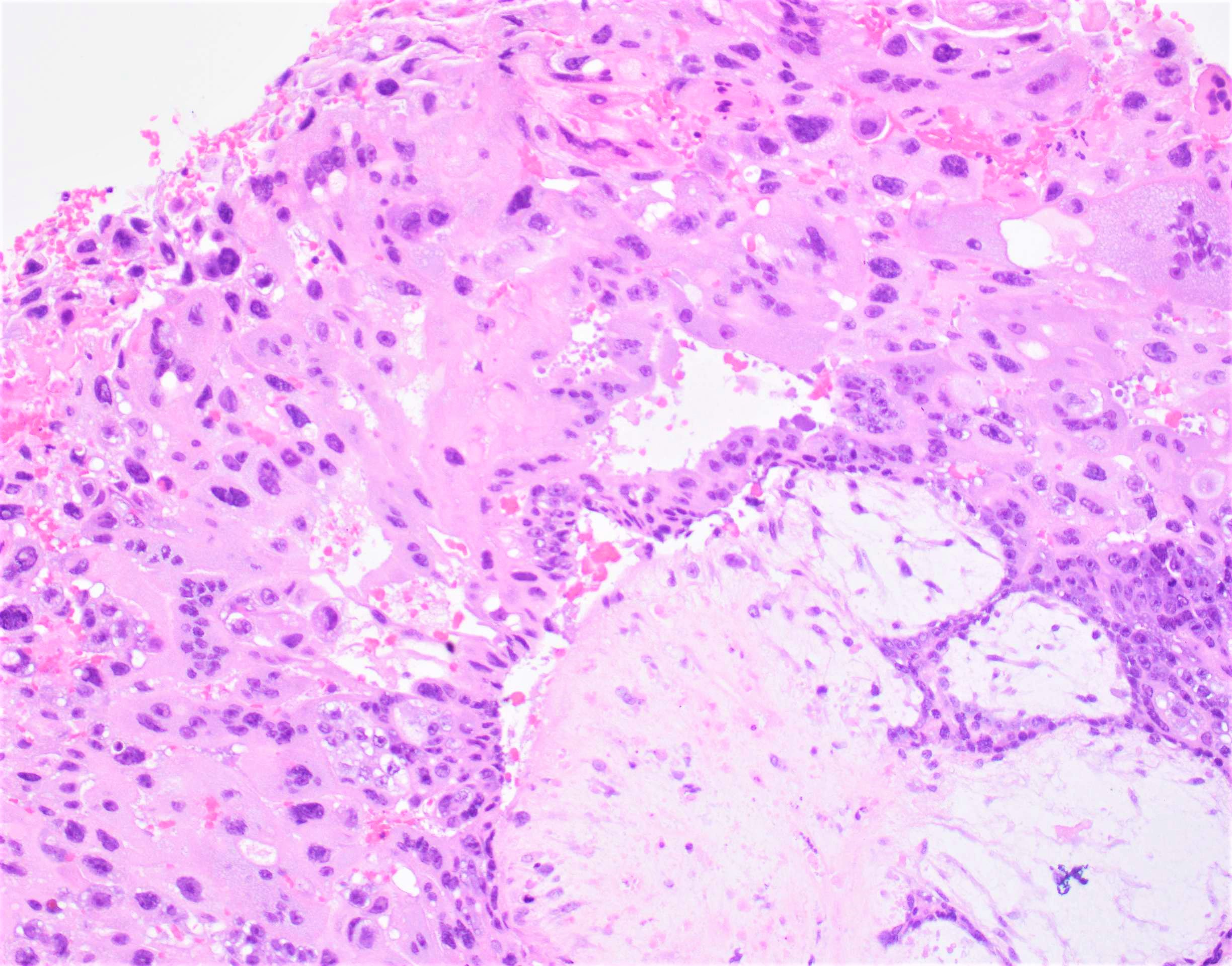
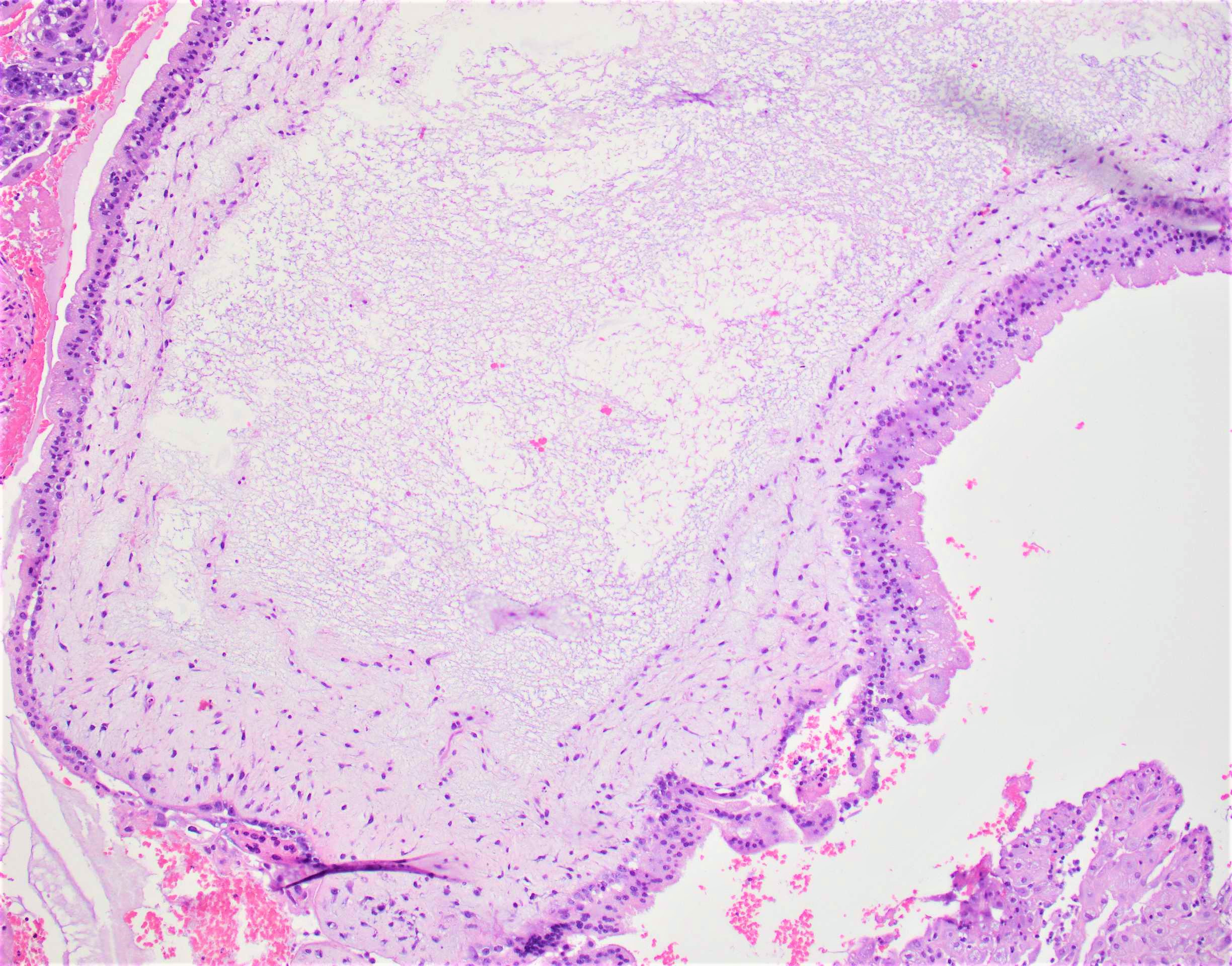
Microscopic (histologic) description
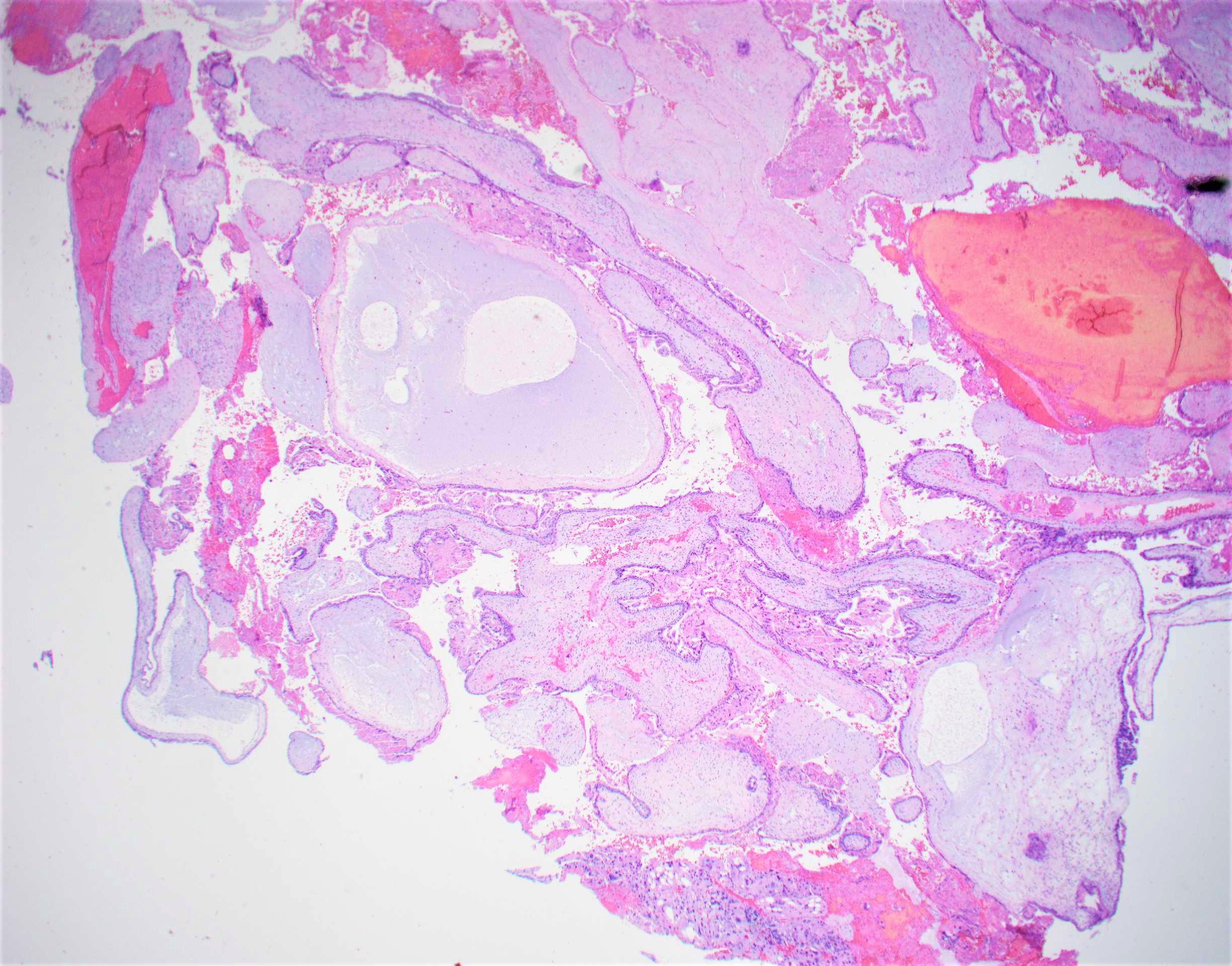
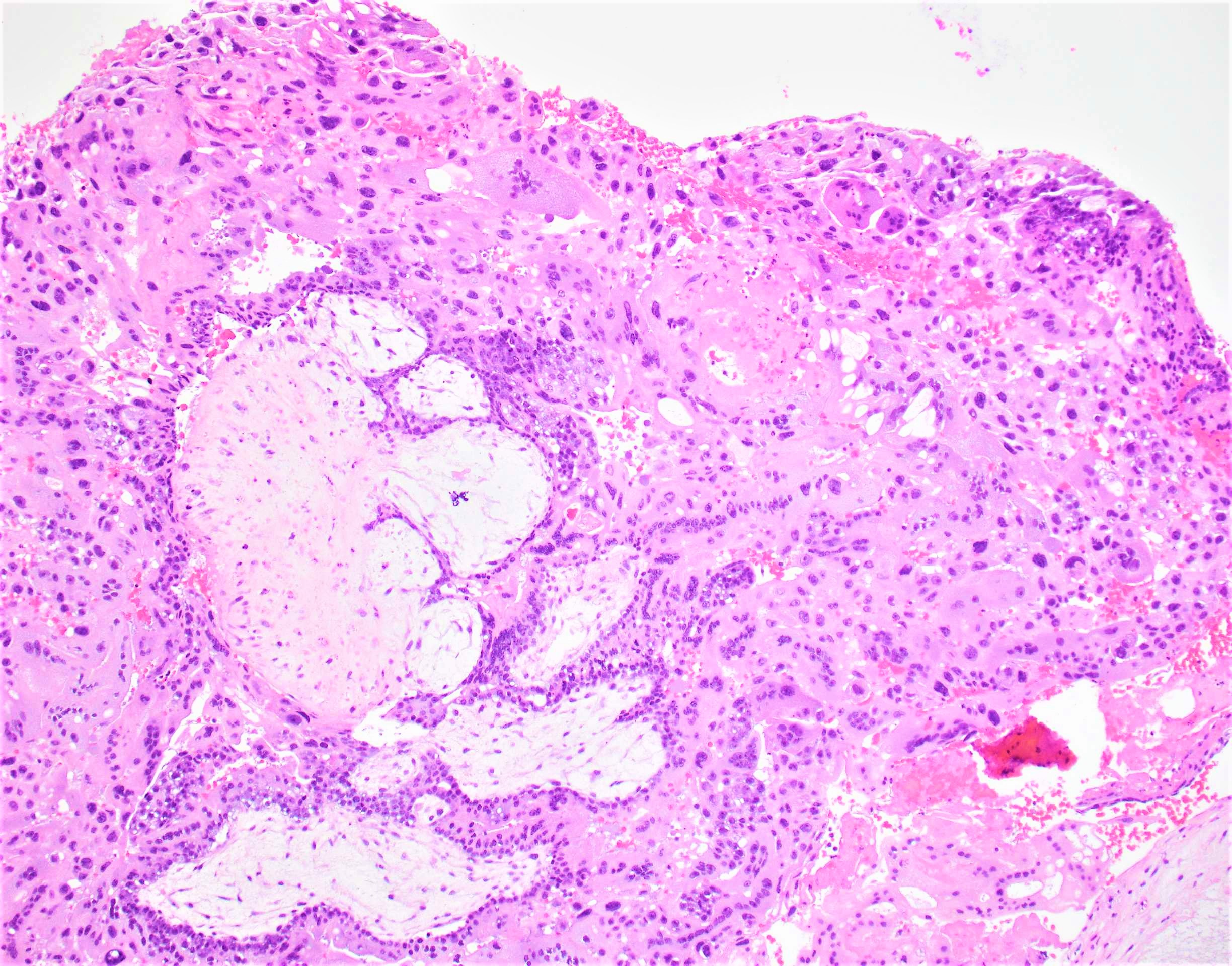
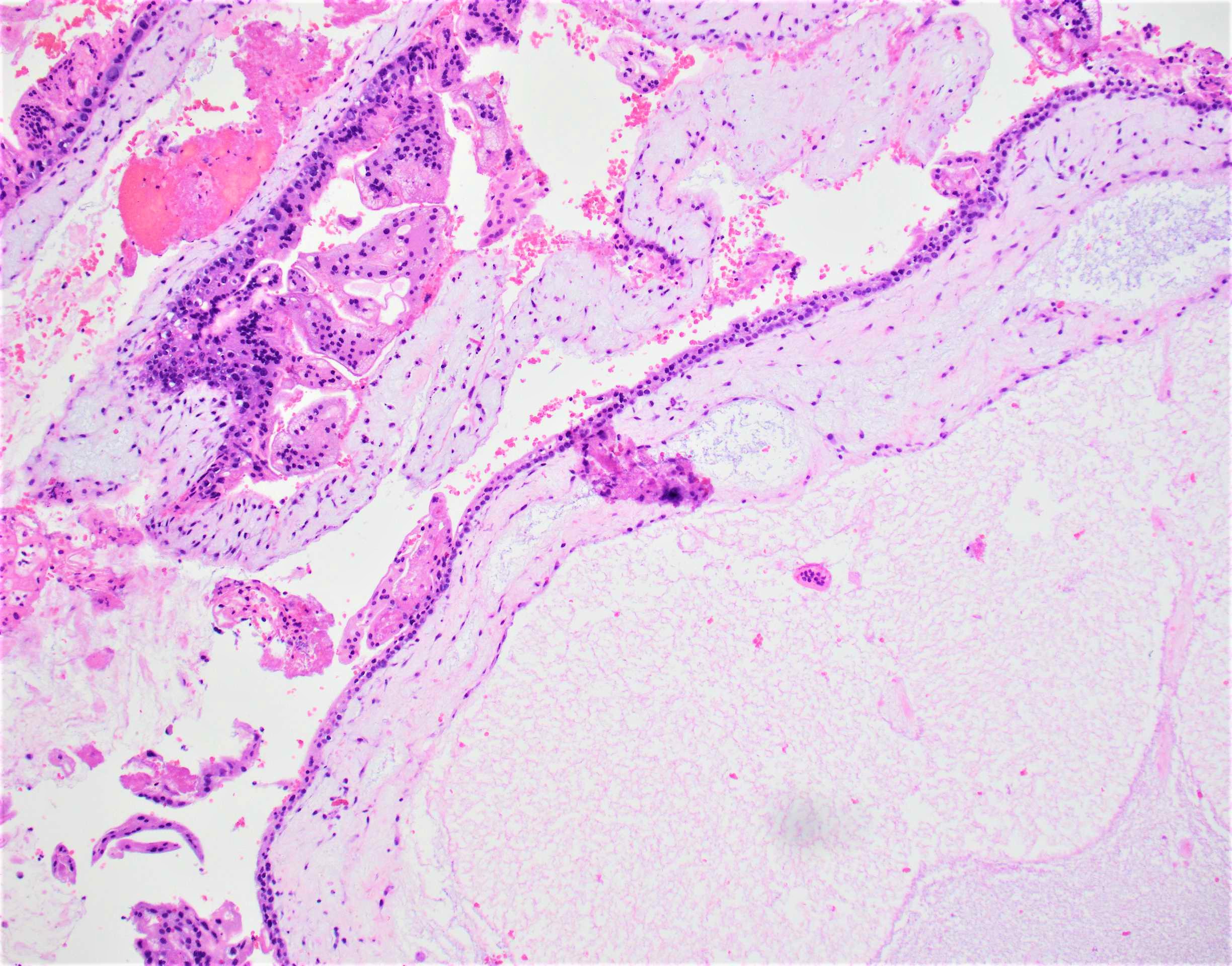
- Diffuse, villous enlargement with marked hydropic changes
- Cistern formation and marked trophoblastic hyperplasia usually in a circumferential pattern
- Remarkable cytologic atypia is almost always present
- Mitoses are common
- Presence of exaggerated placental site
- Distended core of the villus is traversed by widely separated, broken strands of fibrillar material (cistern formation)
- Stromal changes of molar villi, which include stromal mucin and stromal nuclear debris (apoptosis), appear very early and represent a diagnostic clue
- Reference: APMIS 2018;126:647
Microscopic (histologic) images
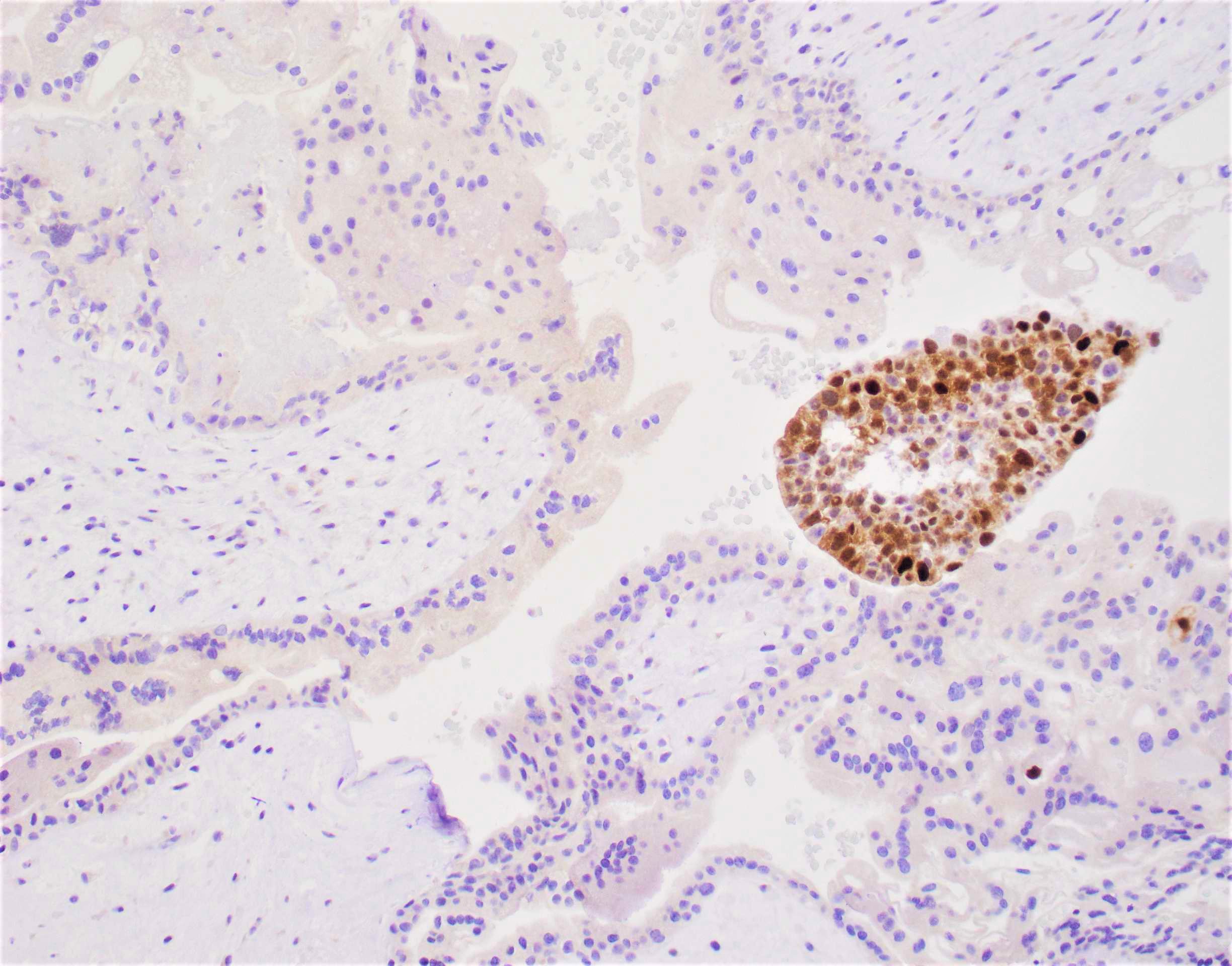
Negative stains
- p57 negative in villous cytotrophoblast and stromal cells
- Paternally imprinted maternally expressed gene
- Complete mole does not have maternal genes and is p57-
- Requires internal positive control in maternal decidua and intervillous trophoblasts
- Rare cases of recurrent complete mole may be biparental (p57+), resulting from mutations of maternal NLRP7 or KHDC3L, shutting down the entire maternal imprinting gene expression
- Reference: Mod Pathol 2014;27:238
Molecular / cytogenetics description
- Karyotyping - 46XX (80%) with homozygous chromosome polymorphisms or 46XY (20%) androgenetic diploidy
- Flow cytometric DNA analysis will show a single peak to denote androgenetic diploidy
- Ploidy FISH - 2 fluorescent signals of androgenetic diploid alleles must be present in > 70% of villous trophoblastic cells
- Genotyping of short tandem repeats / DNA microsatellites will show no maternal alleles and two homozygous (monospermic) or heterozygous (dispermic) paternal alleles
- Mutational analysis may show biallelic NLRP7 or KHDC3L mutations in cases of recurrent complete mole
- References: Mod Pathol 2014;27:238, Arch Pathol Lab Med 2013;137:55, Am J Hum Genet 2011;89:451
Molecular / cytogenetics images
Videos
Complete hydatidiform mole histopathology
Sample pathology report
- Endometrium, curettage:
- Complete hydatidiform mole (see comment)
- Comment: Histologic sections show hydropic villi with marked circumferential trophoblastic proliferation and atypia. An exaggerated placental site is also present. p57 immunohistochemical stain shows absent staining in villous cytotrophoblastic and stromal cells, supporting the diagnosis.
Differential diagnosis
- Partial hydatidiform mole:
- Fetal or embryonic tissue may be present
- Chorionic villi with focal edema, scalloping and prominent stromal trophoblastic inclusions
- Functioning villous circulation
- Focal trophoblastic hyperplasia and minimal atypia
- p57 is positive in villous stromal and cytotrophoblast cells
- Cytogenetic studies show diandric triploidy (69XXX, 69XXY)
- Hydropic abortus:
- Polarized trophoblastic proliferation
- No trophoblast atypia
- Only mildly enlarged and edematous villi, occasionally cistern formation
- Biparental diploidy
- Abnormal villous morphology, possibly related to other genetic abnormalities (e.g., trisomy):
- Irregular villous outlines with patchy villous hydropic change
- Complex karyotype (trisomy with combined monosomy, quadriploidy) (Diagn Pathol 2016;11:20)
- Placental mesenchymal dysplasia:
- Fetus is present, may have normal growth
- Absence of trophoblastic proliferation
Additional references
Board review style question #1
A 24 year old woman presents with vaginal bleeding during the 14th week of pregnancy. She reports intractable nausea. Serum beta human chorionic gonadotropin (beta hCG) levels are markedly elevated at 1,780,000 mIU/ml. Ultrasound assessment reveals no visible fetus but a snowstorm pattern is noted by the radiologist. Curettage reveals 510 grams of bloody granular and friable tissue with numerous small vesicles, which contain clear, colorless fluid. No fetal parts are seen grossly. Representative histologic section is as shown above with circumferential trophoblastic proliferation and cistern formation. Which of the following is true about this condition?
- Abnormal karyotype may arise from endoreplication of paternal chromosome
- Immunostaining for p57 should be negative in decidual tissue and syncytiotrophoblasts
- Typical genetic profile is diandric triploidy
- This results from fertilization of a haploid ovum with two haploid sperm cells
Board review style answer #1
A. Abnormal karyotype may arise from endoreplication of paternal chromosome
Comment Here
Reference: Complete hydatidiform mole
Comment Here
Reference: Complete hydatidiform mole
Board review style question #2
The most common karyotype for complete mole is
- 45XX
- 46XX
- 46XY
- 69XXY
Board review style answer #2