Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chen IY, Agostini-Vulaj D. Insulinoma (beta cell tumor). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/pancreasinsulinoma.html. Accessed March 30th, 2025.
Definition / general
- Rare neuroendocrine neoplasm of pancreas with functional production of insulin
Essential features
- Tumor secretes insulin (analogous to beta cell production in normal pancreatic islets) and thus clinical hyperinsulinemic hypoglycemia is required for this diagnosis
- Majority of insulinomas are small (< 2 cm) and benign
- Multiple insulinomas associated with multiple endocrine neoplasia type 1 (MEN1) syndrome
Terminology
- Beta cell tumor
ICD coding
Epidemiology
- Usually seen in older adults
- More common in females (Ann Surg 2008;247:165)
- Overall most common functioning pancreatic neuroendocrine neoplasm (J Gastroenterol 2015;50:58)
- Majority are benign; 5 - 10% are malignant (Best Pract Res Clin Gastroenterol 2005;19:783)
Sites
- Pancreas, evenly distributed (Pancreas 2014;43:675, J Hepatobiliary Pancreat Sci 2019;26:383)
- Extrapancreatic sites, such as duodenum or hilum of the spleen, are exceedingly rare (J Hepatobiliary Pancreat Sci 2019;26:383)
Pathophysiology
- Unknown
Etiology
- Mostly sporadic; familial cases are associated with MEN1 or MAFA germline mutations (Endocr J 2012;59:859, Proc Natl Acad Sci U S A 2018;115:1027)
Clinical features
- Whipple triad: symptoms of hypoglycemia (stupor, confusion, loss of consciousness), glucose < 45 mg/dL, symptoms relieved by glucose or symptoms caused by fasting or exercise
- 10 - 15% associated with MEN1 syndrome; age < 20 years is suggestive of MEN1 (usually multiple tumors are seen) (Endocr J 2012;59:859, Best Pract Res Clin Gastroenterol 2005;19:783)
Diagnosis
- Clinical diagnosis with demonstration of hyperinsulinemic hypoglycemia
- 72 hour fast is the gold standard for diagnosis (Endocrinol Metab Clin North Am 1999;28:519)
- Imaging based modalities such as CT, ultrasound, MRI, PET or radiolabeled scintigraphy (Neuroendocrinology 2009;90:167, Best Pract Res Clin Endocrinol Metab 2005;19:311, J Clin Endocrinol Metab 2009;94:4398)
- Arteriography was once the gold standard but has been obviated by other, less invasive, modalities and generally is restricted for difficult cases; transhepatic portal venous sampling and selective arterial calcium stimulation with venous sampling are additional more invasive methods (PLoS One 2019;14:e0224928)
Laboratory
- Demonstration of hyperinsulinemic hypoglycemia
- Blood glucose ≤ 45 mg/dL, insulin ≥ 43 pmol/L, C peptide ≥ 200 pmol/L, no sulfonylurea in plasma (Best Pract Res Clin Gastroenterol 2005;19:783)
Radiology description
- CT shows higher attenuation within the lesion than surrounding uninvolved pancreas in venous contrast enhancement phase
- On ultrasound, the lesion is characterized by low echogenicity and hypervascularity
- MRI and radiolabeled glucagon-like peptide 1 receptor (GLP-1R) scintigraphy has been used to localize small insulinomas (J Clin Endocrinol Metab 2009;94:4398)
- Reference: Neuroendocrinology 2009;90:167
Prognostic factors
- Stage and grade are important prognostic factors (Neoplasma 2015;62:484)
- Increased risk for metastasis and reduced survival in the following:
- Tumor ≥ 2 cm (Neoplasma 2015;62:484, Endocr Pathol 2020;31:108)
- ARX immunohistochemical (IHC) protein expression (Endocr Pathol 2020;31:108)
- Loss of DAXX or ATRX by IHC stain and alternative lengthening of telomeres (ALT) (Gastroenterology 2014;146:453, Endocr Pathol 2020;31:108)
- High Ki67 labeling index and high mitotic count are unfavorable prognostic factors (see well differentiated neuroendocrine tumor for additional details on grading)
- Insulinomas generally have a more favorable prognosis compared with nonfunctional tumors, as well as other functioning tumors (Surg Pathol Clin 2016;9:595, Front Med 2016;10:444)
- Proteomic study revealed low tumor protein D52 expression as a strong independent prognostic factor for both recurrence free and overall disease related survival (Mod Pathol 2015;28:69)
Case reports
- 20 year old slender, lean man complained of increased hunger, tremor and frequent seizures with worsening symptoms for 4 months (Cureus 2022;14:e23414)
- 32 year old woman with long history of prolactinoma and secondary amenorrhea presented with hypoglycemia (BMC Endocr Disord 2022;22:108)
- 50 year old man transiently lost consciousness while piloting a helicopter rescue (Med Lav 2022;113:e2022007)
- 83 year old woman with recurrent episodes of delirium occurring overnight, associated with hypoglycemia (Age Ageing 2022;51:afac055)
- 84 year old nondiabetic woman presented with recurrent falls and hypoglycemic episodes (Clin Med (Lond) 2022;22:90)
Treatment
- Definitive surgical resection, enucleation is preferred if possible (J Laparoendosc Adv Surg Tech A 2022 Apr 19 [Epub ahead of print])
- Symptomatic control with somatostatin analogs (octreotide) (Neoplasma 2015;62:484)
Gross description
- Most commonly a solitary, well delineated lesion with tan-yellow homogenous cut surface, with or without hemorrhage (Surg Pathol Clin 2016;9:595)
Gross images
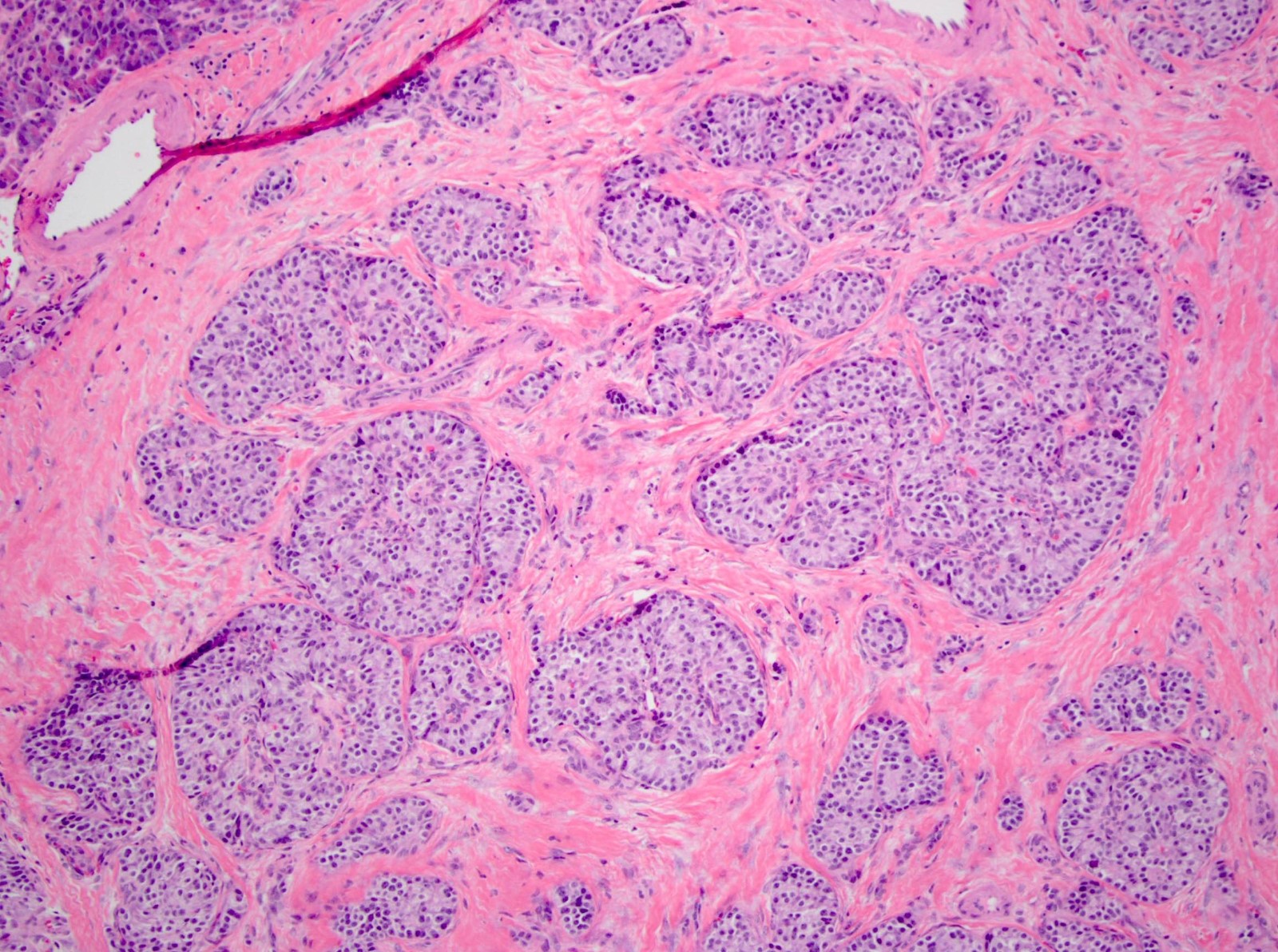
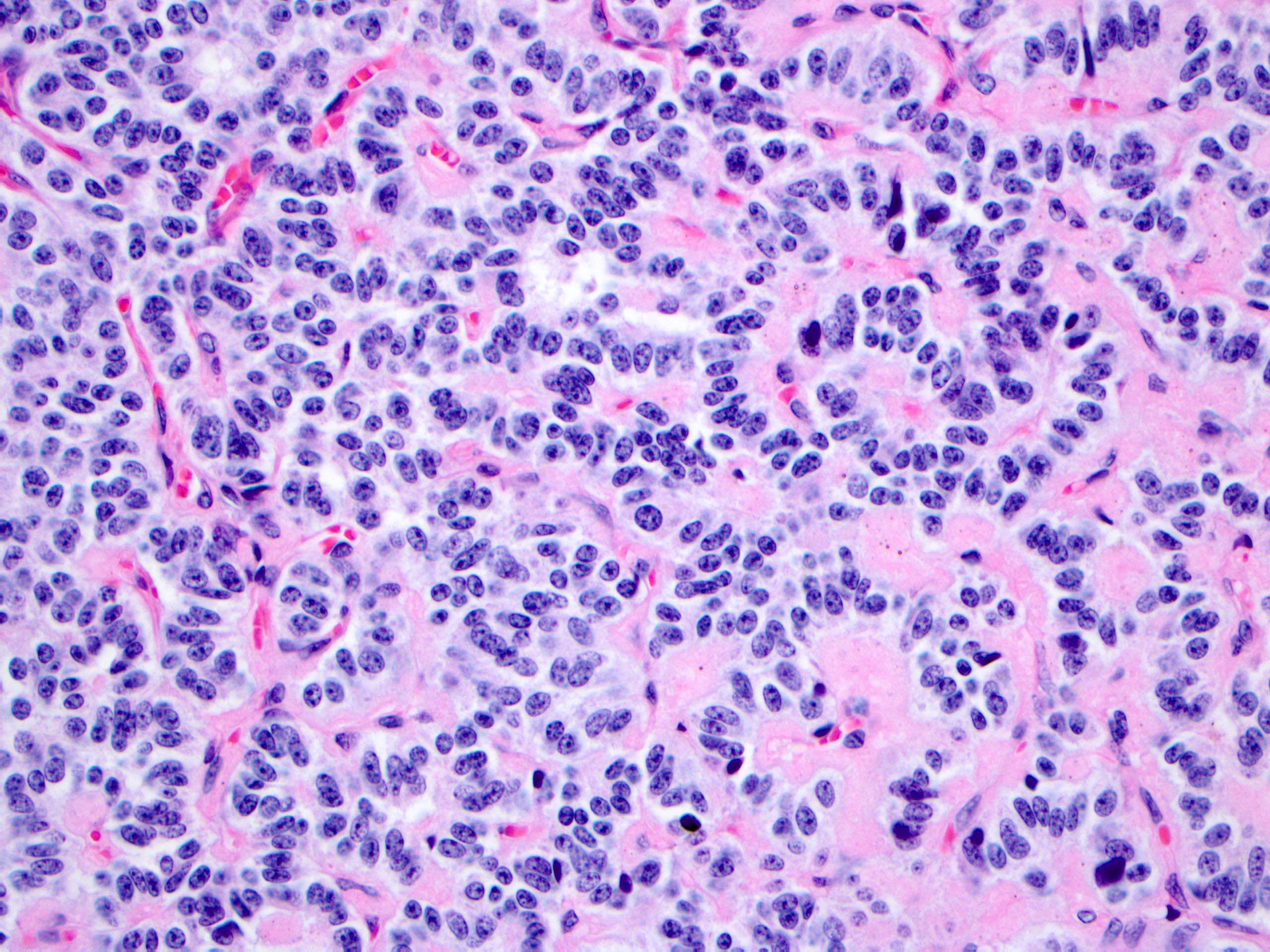
Microscopic (histologic) description
- Trabecular, nested, gyriform or solid architecture
- Monotonous cells demonstrating round nuclei with salt and pepper-like chromatin and abundant cytoplasm
- Amyloid stromal deposition may be seen (nonspecific) (Arch Pathol Lab Med 1978;102:227, Endocr Pathol 2021;32:318)
Microscopic (histologic) images
Cytology description
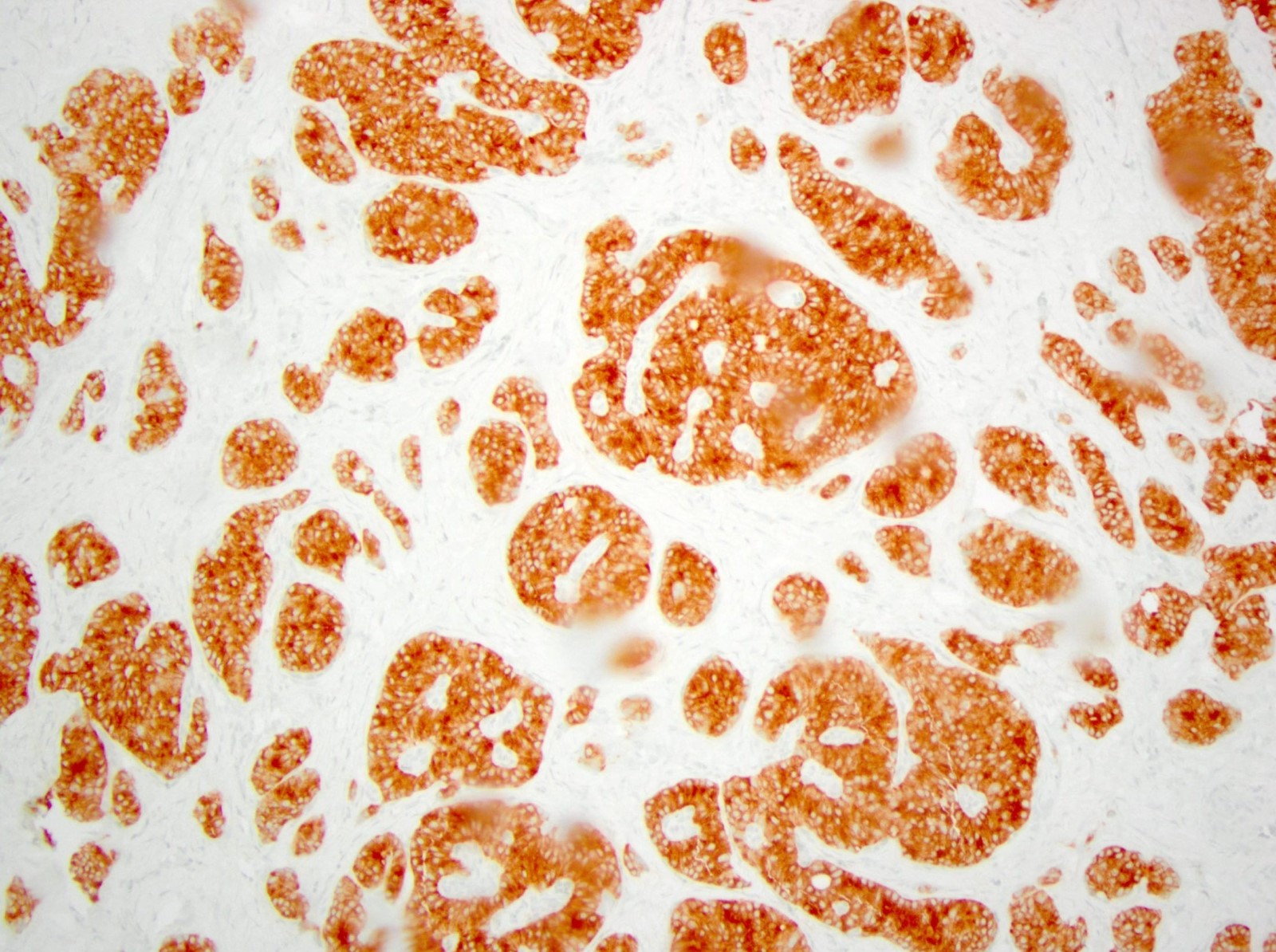
Positive stains
- Synaptophysin, chromogranin, ISL1, INSM1 (Am J Surg Pathol 2013;37:399)
- Insulin (positivity is not required for diagnosis), proinsulin (50%), amylin, islet amyloid polypeptide (Am J Surg Pathol 2013;37:399)
- PDX1 (beta cell marker) (Endocr Pathol 2020;31:108):
- Positive in indolent insulinoma; variable staining pattern in aggressive insulinoma
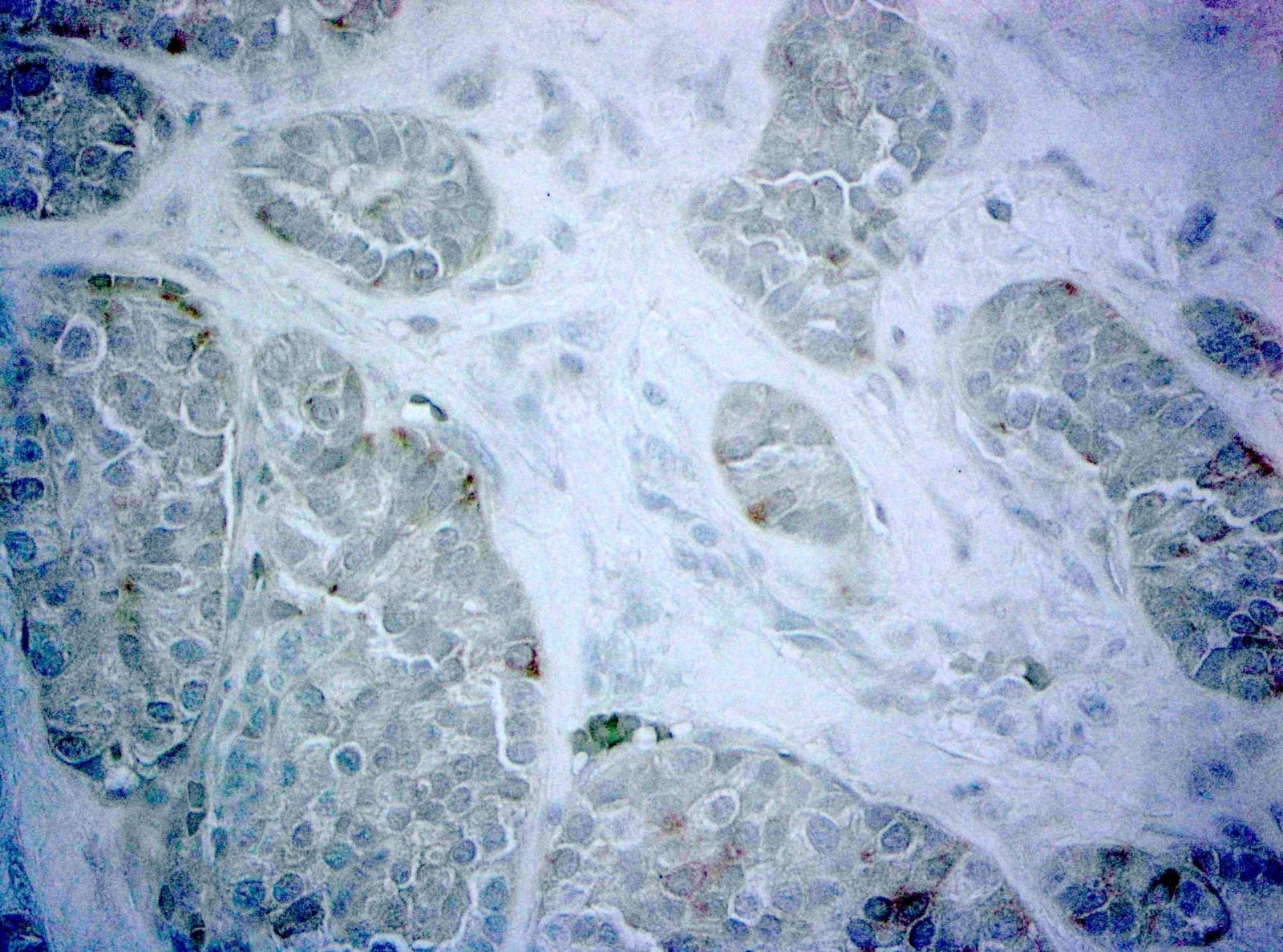
- ARX (alpha cell marker) (Endocr Pathol 2020;31:108):
- Negative in indolent insulinoma; positive in aggressive insulinoma
Negative stains
- Beta catenin (normal membranous expression)
- PDX1 (beta cell marker) (Endocr Pathol 2020;31:108):
- Positive in indolent insulinoma; variable staining pattern in aggressive insulinoma
- ARX (alpha cell marker) (Endocr Pathol 2020;31:108):
- Negative in indolent insulinoma; positive in aggressive insulinoma
Electron microscopy description
- Round secretory granules with paracrystalline content (similar to granules seen in beta cells of normal pancreatic islets) (Nouv Presse Med 1977;6:3713)
Molecular / cytogenetics description
- MEN1, DAXX, ATRX, PTEN and TSC2 mutations as those seen in PanNET, are rare in insulinoma (J Hepatobiliary Pancreat Sci 2019;26:383)
- A subset (30%) showed recurrent p.T372R mutation in YY1 gene (Nat Commun 2013;4:2810, J Clin Endocrinol Metab 2015;100:E776)
- A subset showed alternative lengthening of telomere phenotype, loss of DAXX / ATRX and loss of CDKN2A, which is associated with metastatic disease and closely related to PanNET (Endocr Pathol 2020;31:108)
Sample pathology report
- Pancreas, distal pancreatectomy:
- Well differentiated neuroendocrine tumor, WHO grade __, functional, clinically consistent with insulinoma
Differential diagnosis
- Noninsulin secreting pancreatic neuroendocrine tumor (see well differentiated neuroendocrine tumor and neuroendocrine neoplasms - general):
- Does not demonstrate clinical hyperinsulinemic hypoglycemia (i.e., are nonfunctional)
- Histologic features are essentially identical
- Solid pseudopapillary neoplasm:
- Usually seen in young females
- No associated clinical syndrome of hyperinsulinemic hypoglycemia
- Pseudopapillae formation
- Positive nuclear beta catenin
Additional references
Board review style question #1
Which syndrome is associated with multiple insulinomas?
- MEN1
- MEN2A
- MEN2B
- NF2
- Peutz-Jeghers
Board review style answer #1
Board review style question #2
A midbody pancreatic enucleation is performed (see image above). Histologically, the neoplasm is positive for insulin, chromogranin and synaptophysin, with a Ki67 of < 2%. The patient has no clinical syndrome of hyperinsulinemic hypoglycemia. What is the most appropriate diagnosis?
- Glucagonoma
- Insulinoma
- VIPoma
- Well differentiated neuroendocrine tumor, G1
- Well differentiated neuroendocrine tumor, G2
Board review style answer #2
D. Well differentiated neuroendocrine tumor, G1. In the absence of a clinical syndrome, the term insulinoma should not be used; the Ki67 of < 2% classifies this as a grade 1 neuroendocrine tumor.
Comment Here
Reference: Insulinoma
Comment Here
Reference: Insulinoma