Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Kisha S, Ahsan B. Acute pancreatitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/pancreasacute.html. Accessed April 26th, 2024.
Definition / general
- Inflammatory disease of the exocrine pancreas that causes acute onset of severe abdominal pain and might lead to pancreatic necrosis
Essential features
- Reversible pancreatic parenchymal injury
- Causes include gallstones, alcohol and hypertriglyceridemia
- Main histological features include acute inflammatory cells with hemorrhage and necrosis
- Treatment is supportive
Terminology
- Interstitial edematous pancreatitis: often referred to simply as acute pancreatitis
- Necrotizing pancreatitis
- Other terminologies: bile pancreatitis, infected pancreatic necrosis and postoperative pancreatitis
ICD coding
Epidemiology
- Incidence of acute pancreatitis is similar among men and women; male sex is associated with higher mortality
- Peak incidence of acute pancreatitis is in the fifth and sixth decades
- In the U.S., incidence has been cited as 600 - 700 per 100,000 people, with 200,000 - 250,000 discharges occurring yearly for acute pancreatitis
- Gallstone disease is the leading cause and accounts for 20 - 70% of all cases in the West
- Alcohol is the second most common cause of acute pancreatitis, accounting for up to 30% of cases
- Hypertriglyceridemia accounts for ~9% of cases, making it the third most common cause
- Mortality of acute pancreatitis ranges from 3% in patients with mild edematous pancreatitis to as high as 20% in patients with pancreatic necrosis
- References: StatPearls: Acute Pancreatitis [Accessed 11 July 2023], United European Gastroenterol J 2018;6:649, J Clin Med 2021;10:300
Sites
- Pancreas
Pathophysiology
- Acute pancreatitis is triggered by various factors that disrupt normal intracellular calcium signaling in pancreas cells, which normally maintains stimulus secretion coupling
- Increasing intracellular calcium leads to premature activation of the enzyme trypsinogen to trypsin within the acinar cell instead of the duct lumen
- Intracellular calcium also overwhelms mitochondria leading to impaired production of adenosine triphosphate (ATP)
- Diminished ATP affects cellular process leading cytokine release, cellular necrosis and inflammation
- Proinflammatory cytokines mediate powerful immune response, leading to systemic inflammatory response syndrome, multiorgan dysfunction and higher susceptibility to infections
- References: Drugs 2022;82:1251, StatPearls: Acute Pancreatitis [Accessed 11 July 2023], Int J Mol Sci 2020;21:4005
Etiology
- Gallstone disease: the leading cause of acute pancreatitis worldwide; accounts for 20 - 70% of cases in the West and is more common in women
- Alcohol: second most common cause of acute pancreatitis in North America and Europe, contributing to up to 33% of cases
- Hypertriglyceridemia: elevated triglyceride levels in the blood can cause acute pancreatitis, accounting for ~9% of cases
- Drugs such as antiretrovirals, chemotherapeutic agents, antibiotics, steroids and others
- Infectious causes: most commonly mumps, cytomegalovirus (CMV), Epstein-Barr virus (EBV)
- Genetic factors also play a role, such as hereditary pancreatitis associated with specific gene mutations in PRSS1, SPINK1, CFTR and CTRC
- Other causes: there are various less common causes of acute pancreatitis, including trauma, hypercalcemia, tumors, anatomical variants, cardiac bypass surgery, scorpion bites and organophosphate poisoning
- References: Drugs 2022;82:1251, World J Clin Pediatr 2022;11:27
Clinical features
- Symptoms: mild to severe epigastric pain, nausea and vomiting
- Signs: high white blood count, diffuse fat necrosis, peripheral vascular collapse, acute tubular necrosis, shock (blood loss, electrolyte disturbances, endotoxemia, release of cytokines), hypocalcemia, hyperglycemia
- Complications: pancreatic pseudocyst, walled off necrosis, peripancreatic fluid collection
- Systemic complications include: acute respiratory distress syndrome (ARDS), acute kidney injury (AKI), disseminated intravascular coagulation (DIC)
- References: Drugs 2022;82:1251, World J Emerg Surg 2019;14:27
Diagnosis
- Abdominal pain consistent with pancreatitis
- Serum amylase or lipase 3 or more times the upper limit of normal
- Findings consistent with pancreatitis on CT, MRI or in some cases transabdominal ultrasound (TUS)
- References: Drugs 2022;82:1251
Laboratory
- High amylase and lipase
- High blood glucose
Radiology description
- Abdominal ultrasound (US): first line modality
- Pancreatic enlargement and decreased parenchymal echogenicity due to interstitial edema
- Limitations of US is the inability to make distinction between interstitial and necrotizing pancreatitis
- Computed tomography (CT): gold standard
- Enlargement of the pancreas
- Ill defined parenchymal contours and decreased density and inhomogeneity of the pancreatic parenchyma
- Fluid collections in the peripancreatic region and the inflammatory reaction can produce increased attenuation of the peripancreatic fat tissue commonly described as stranding
- Reference: Diagn Interv Imaging 2015;96:151
Prognostic factors
- Bed side index of severity of acute pancreatitis (BISAP)
- Blood urea and nitrogen level > 8.9 mmol/L
- Systemic inflammatory response syndrome is present
- Age > 60
- Pleural effusion on radiology
- Reference: World J Emerg Surg 2019;14:27
Case reports
- 35 year old man with acute pancreatitis due to over the counter calcium carbonate (J Investig Med High Impact Case Rep 2020;8:2324709620922724)
- 50 year old man with acute pancreatitis with normal lipase and amylase (Medicine (Baltimore) 2019;98:e15138)
- 57 year old woman with steroids induced acute pancreatitis (Cureus 2021;13:e19132)
- 71 year old woman with acute pancreatitis following COVID-19 vaccination (Medicine (Baltimore) 2022;101:e28471)
- 75 year old woman with acute pancreatitis due to cytomegalovirus infection (IDCases 2020;22:e00932)
Treatment
- Oxygen supplementation
- Intravenous fluid resuscitation to correct third space volume loss and tissue hypoperfusion
- Pain management: NSAIDs or opioids, depending on the severity
- Reference: Drugs 2022;82:1251
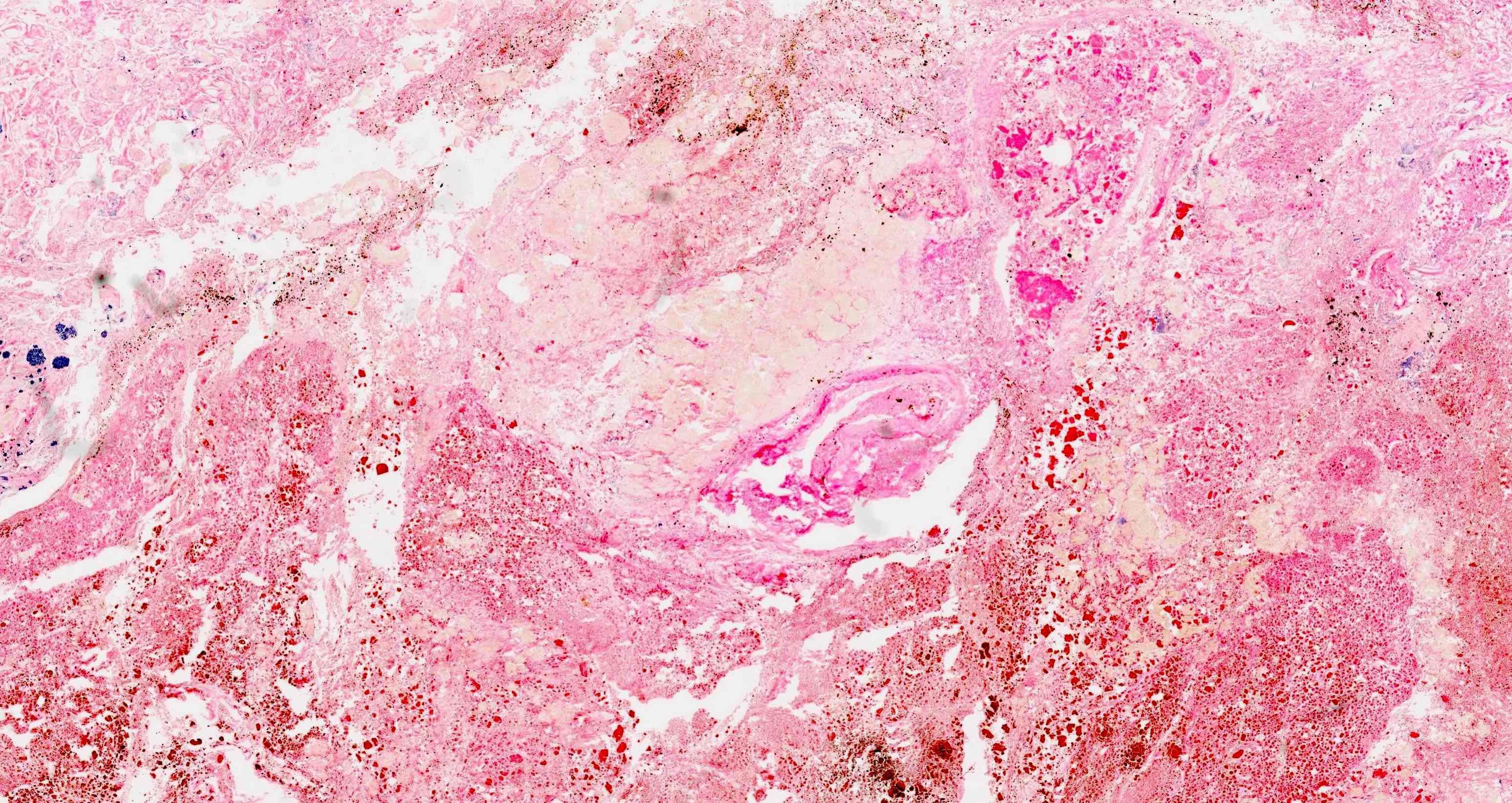
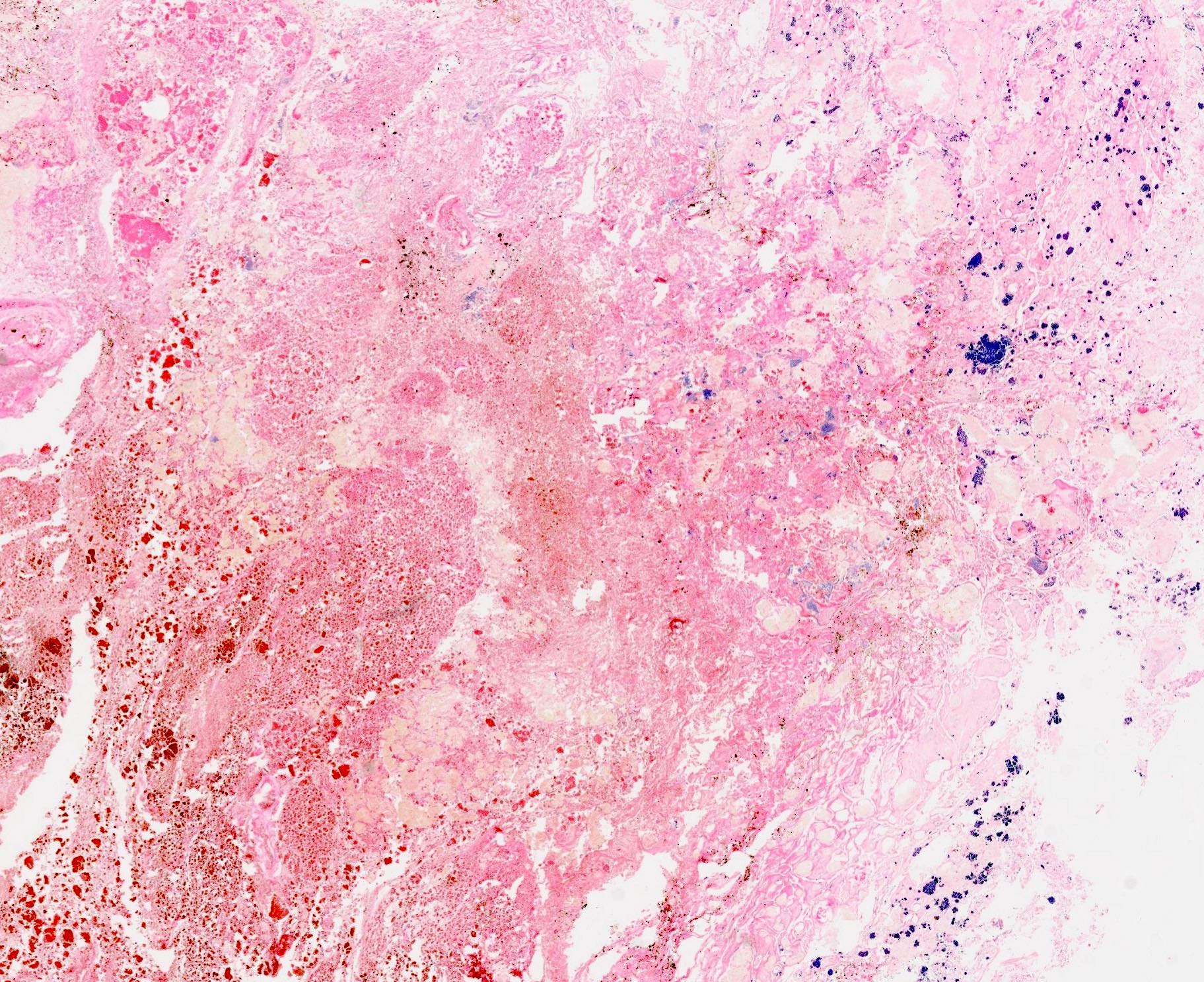
Gross description
- Diffuse stippled necrosis of the pancreatic parenchyma and peripancreatic fat
- Hemorrhagic, black-brown necrosis of the pancreatic parenchyma and peripancreatic fat
Gross images
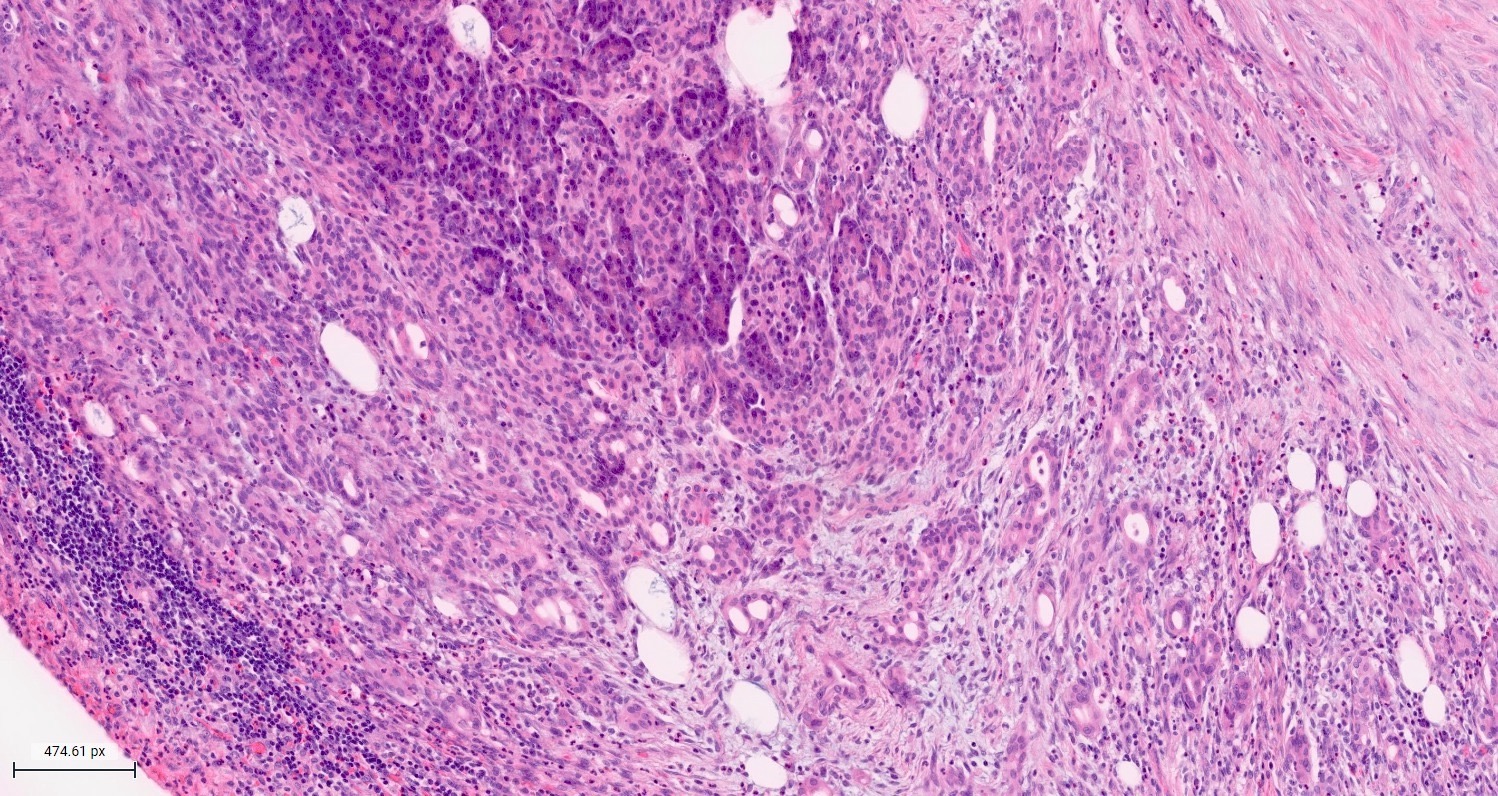
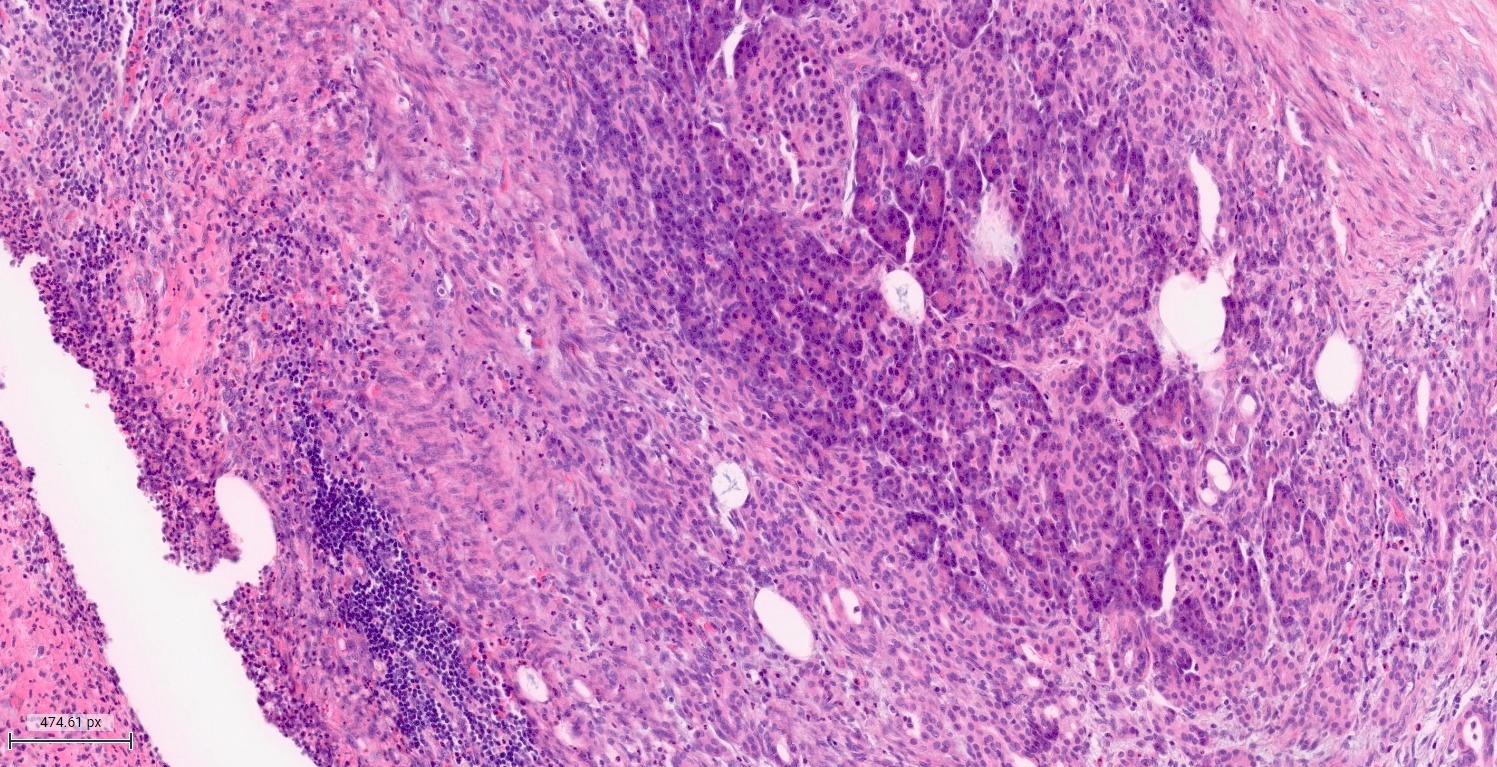
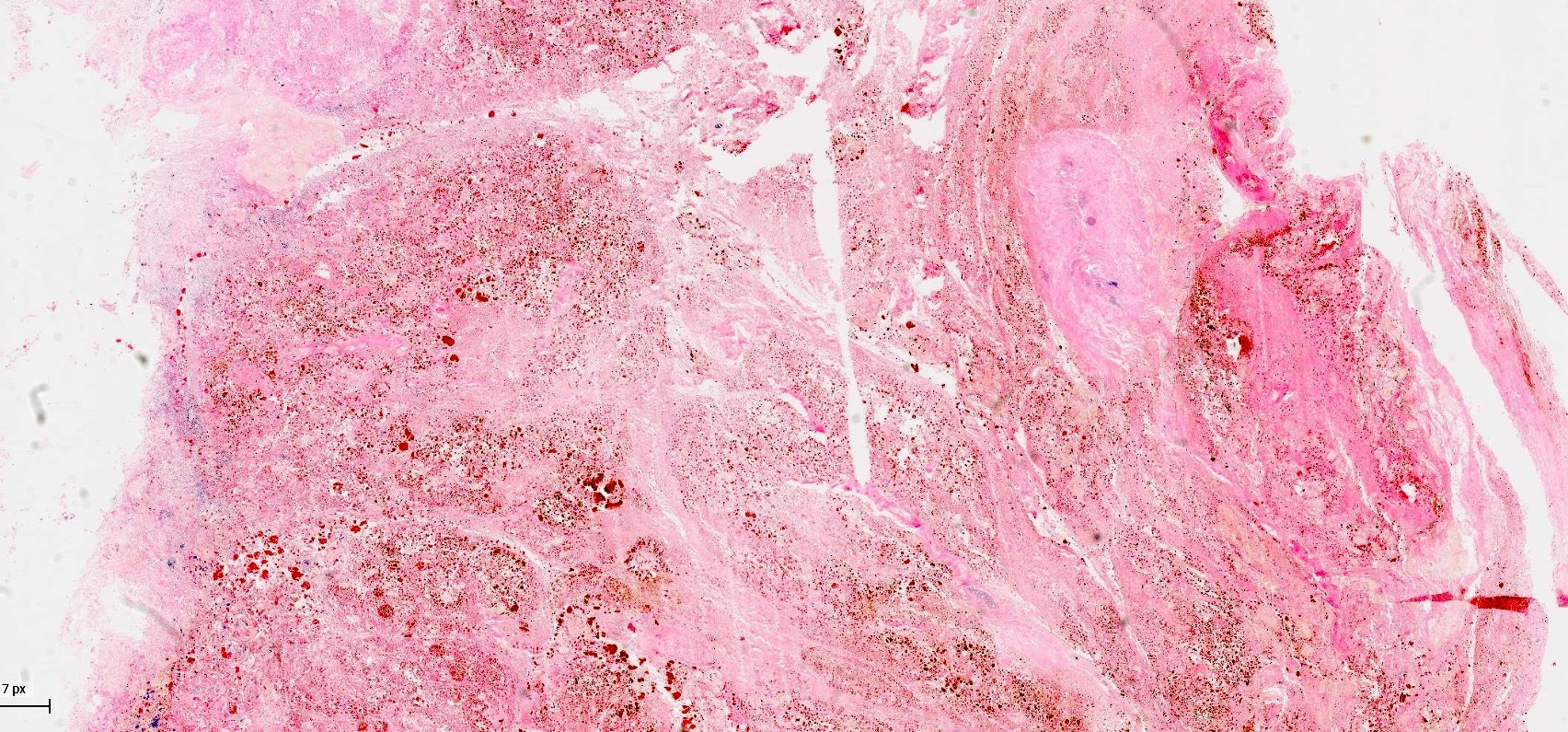
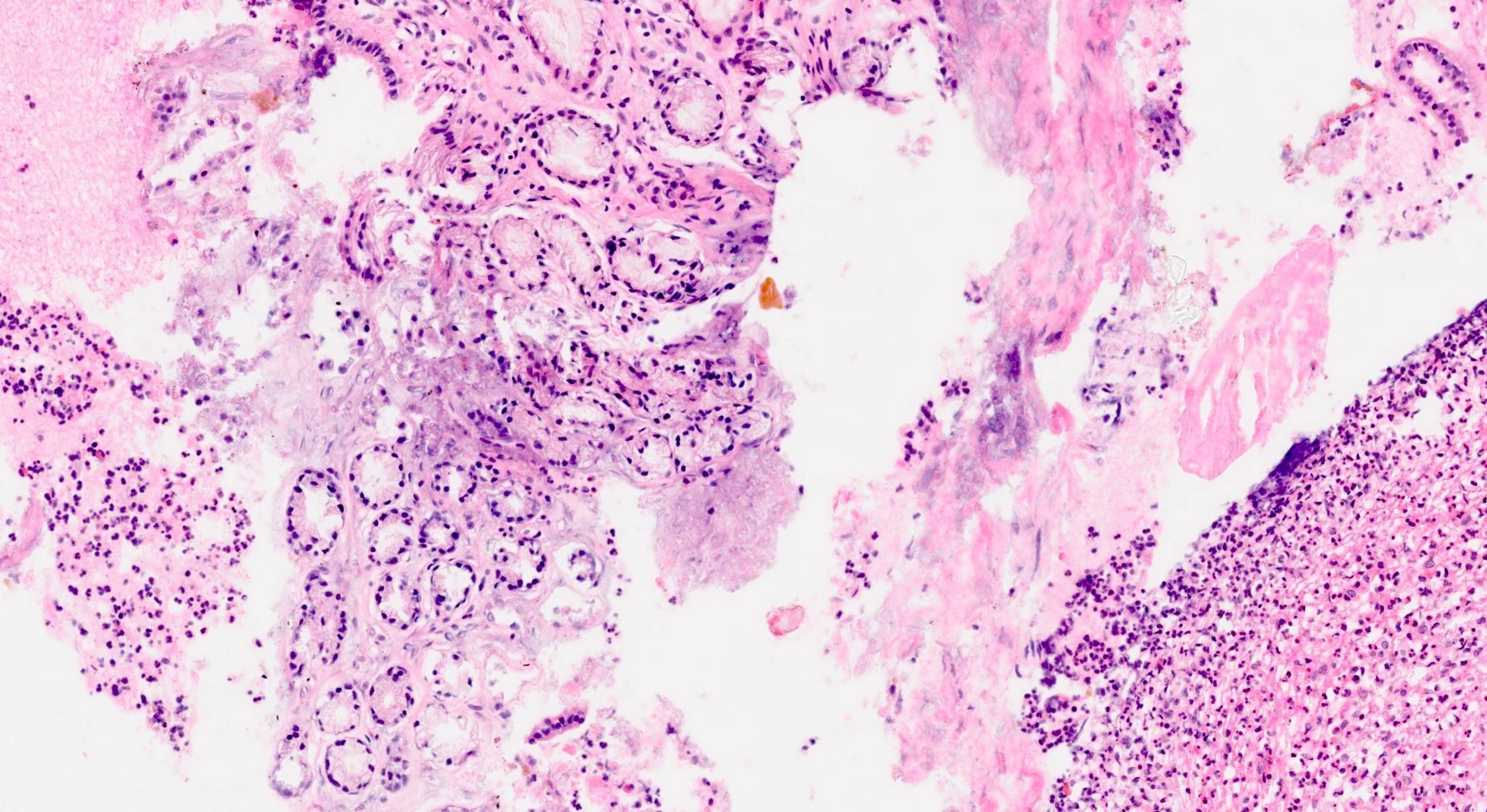
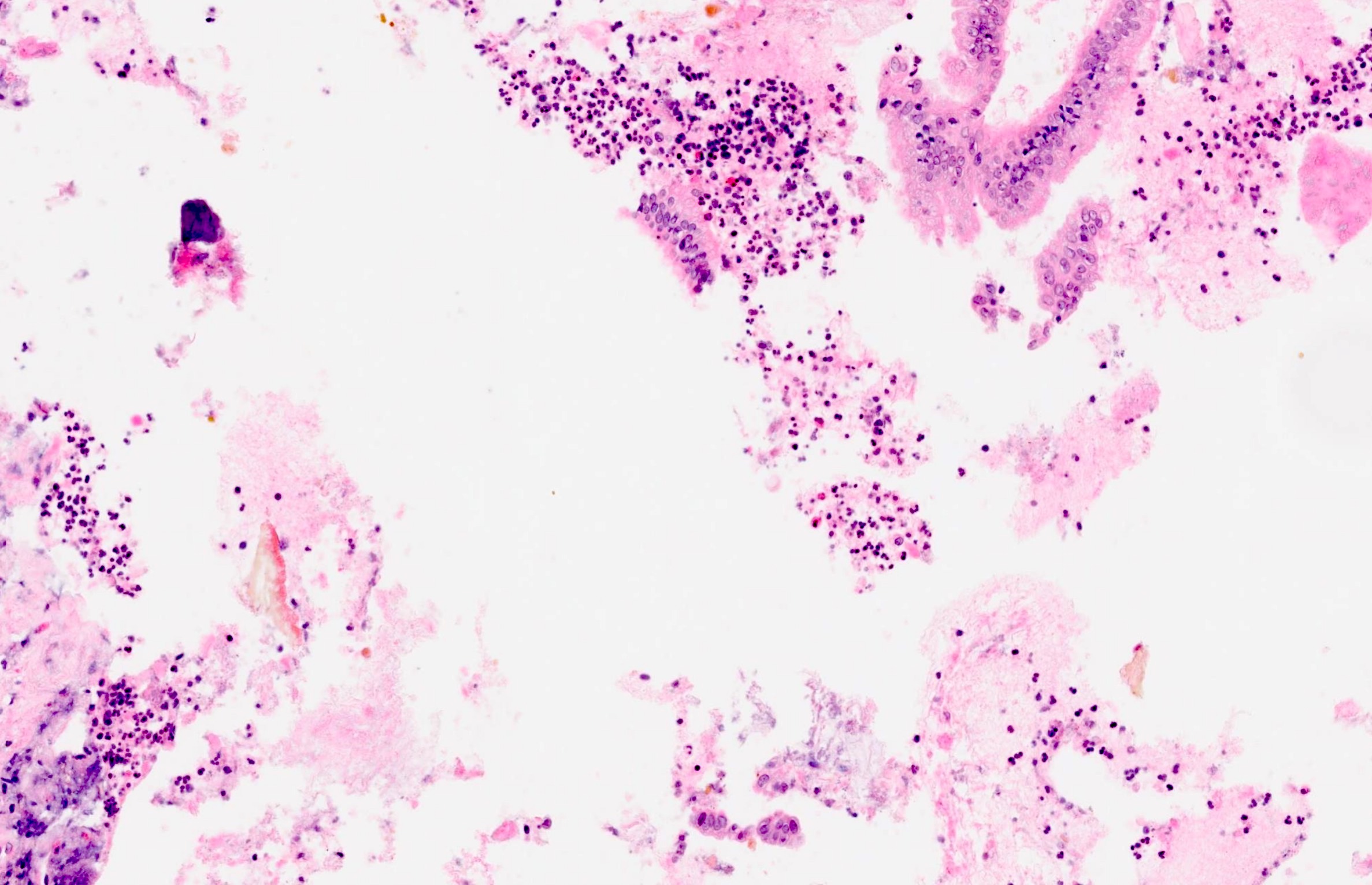
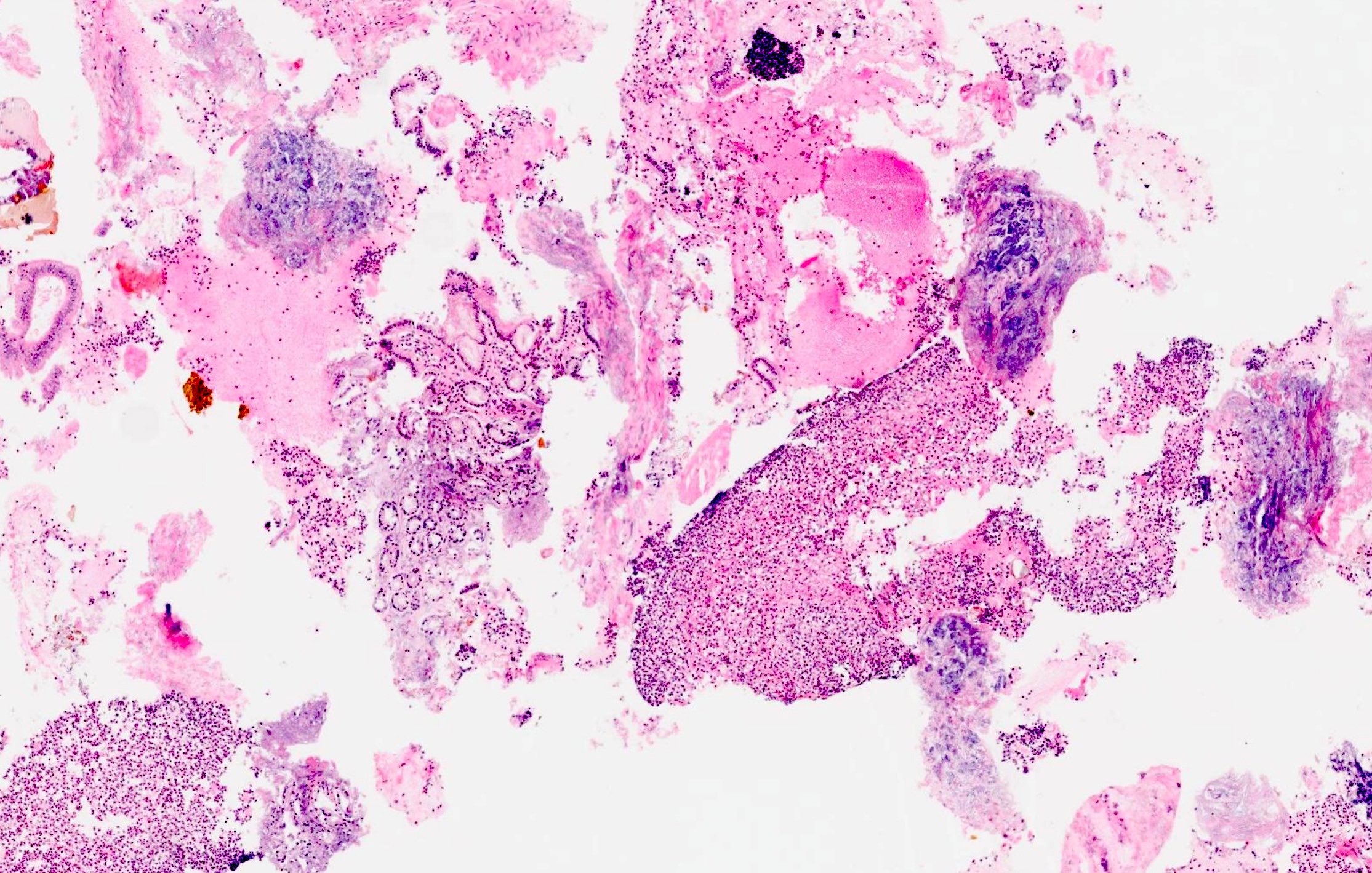
Microscopic (histologic) description
- Acute interstitial or edematous: the interstitial fibrous tissue, adipose tissue and pancreatic parenchyma are edematous and contain acute inflammatory cells with limited fat necrosis
- Acute necrotizing: marked hemorrhage, panlobular coagulative necrosis and extensive fat necrosis of peripancreatic tissues, presence of intravascular thrombi
- Initially neutrophils are present, then macrophages and lymphocytes
- Calcification occurs early and extensively
- Fat necrosis, which is characterized by lipid laden macrophages and foreign body giant cells, can progress to fat saponification, which involves calcium deposition
Microscopic (histologic) images
Cytology description
- Benign pancreatic acinar tissue and ducts
- Fat necrosis, fibrotic stromal tissue
- Acute and chronic inflammatory infiltrate
Molecular / cytogenetics description
- Most common genes associated with acute pancreatitis include
- PRSS1 mutations: inhibits trypsin self destruction, mutations lead to pancreatic autodigestion and pancreatitis
- SPINK1 mutations: encodes a trypsin inhibitor and mutations lead to increased intrapancreatic trypsin activity
- References: Diagnostics (Basel) 2020;11:31, Gastroenterology 2019;156:1951
Videos
Pancreas: acute pancreatitis, gross and microscopy
Sample pathology report
- Pancreas, resection:
- Fragments of necrotic pancreatic and adipose tissues with fat necrosis, hemorrhage, bacterial colonies and fibrinopurulent exudate, consistent with acute hemorrhagic pancreatitis
Differential diagnosis
- Acute cholecystitis:
- Severe abdominal pain with jaundice
- Imaging studies are utilized to make a definite diagnosis
- Acute mesenteric ischemia:
- Severe, sudden abdominal pain in patients with history of atherosclerotic disease
- Angiography
- Acute cholangitis:
- Clinical features include right upper quadrant pain, fever, malaise, chills and jaundice
- Imaging studies including US, CT scan and magnetic resonance cholangiopancreatography (MRCP)
- Chronic pancreatitis:
- Less severe pain
- Malabsorption syndrome (fatty stool and weight loss)
- Histological features of chronic pancreatitis include loss of acinar cells, islet cell hyperplasia, presence of intralobular fibrosis and periductal chronic inflammation
- Myocardial infarction:
- Chest and upper abdominal pain in patients with history of atherosclerotic disease
- ECG with characteristic changes of ischemic injury
- Peptic ulcer disease:
- Bouts of mid epigastric pain associated with eating
- Upper gastrointestinal endoscopy
Board review style question #1
Board review style answer #1
C. Elevated serum lipase and amylase levels. Amylase and lipase are digestive enzymes normally released from the acinar cells of the exocrine pancreas into the duodenum. Following injury to the pancreas, these enzymes are released into the circulation and the pancreas will continue to release these enzymes form injured cells even when the normal outflow of these enzymes is obstructed. This will result in elevated serum lipase and amylase levels in the blood. Answer A is incorrect because elevated bilirubin is associated with gall stones and acute cholecystitis. Answer B is incorrect because high blood alcohol levels have no immediate association with acute pancreatitis and only indicate recent drinking. Answer C is incorrect because acute pancreatitis is an inflammatory condition that leads to high white blood count.
Comment Here
Reference: Acute pancreatitis
Comment Here
Reference: Acute pancreatitis
Board review style question #2
Why is the body more susceptible to secondary infections during cases of pancreatitis?
- Activation of leukocytes in response to proinflammatory cytokine production
- Formation of pseudocysts
- Production of anti-inflammatory cytokines and specific cytokine inhibitors
- Release of cortisol in response to stress
Board review style answer #2
C. Production of anti-inflammatory cytokines and specific cytokine inhibitors.
As a result of the systemic inflammatory response during acute pancreatitis, anti-inflammatory cytokines and specific cytokine inhibitors are produced, increasing the body's risk for infection. Answer A is incorrect because increased leucocytes lead to activation of the immune response and less susceptibility to infections. Answer B is incorrect because pseudocyst cyst formation is a result of the ongoing inflammation and has no relation with susceptibility to infections. Answer D is incorrect because cortisol is ordinarily anti-inflammatory and contains the immune response, so acute increase does not increase infection susceptibility.
Comment Here
Reference: Acute pancreatitis
Comment Here
Reference: Acute pancreatitis