Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Saglam O. Endometrioid carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorendometrioidcarcinoma.html. Accessed May 4th, 2024.
Definition / general
- Ovarian carcinoma resembling endometrioid adenocarcinoma of the endometrium
Essential features
- Most common ovarian endometrioid tumor
- Usually low grade and diagnosed at early stages
- May be associated with endometriosis and adenofibroma
Terminology
- Seromucinous carcinoma is included as a subtype of endometrioid ovarian carcinoma in the 2020 WHO blue book for female genital tumors
ICD coding
- ICD-11: 2C73.01 - endometrioid adenocarcinoma of ovary
Epidemiology
- 10% of primary ovarian carcinomas (J Natl Cancer Inst 2019;111:60)
- Mean patient age is 55 years
- Associated with endometriosis / endometriotic cyst (15%), endometrioid adenofibroma, synchronous endometrial endometrioid adenocarcinoma or endometrial hyperplasia (15 - 30%) (Eur J Gynaecol Oncol 2015;36:21)
- Risk factors: endometriosis, hormone replacement therapy, first degree family history of breast carcinoma (Lancet Oncol 2012;13:385, J Clin Oncol 2016;34:2888)
- May occur in the setting of Lynch syndrome (Gynecol Oncol 2018;150:92, Am J Surg Pathol 2014;38:1173)
Sites
- Ovaries
Pathophysiology
- Most common molecular alterations: WNT / beta catenin signaling pathway (CTNNB1 - 53%), PI3K pathway (PIK3CA - 40% and PTEN - 17%) (Mod Pathol 2014;27:128)
Etiology
- Unknown
Clinical features
- Most common symptoms are abdominal distention and pain
- Background endometriosis is not associated with survival (J Gynecol Oncol 2018;29:e18)
Laboratory
- Elevated CA-125 (Asian Pac J Cancer Prev 2013;14:4545)
Radiology description
- Most common appearance is a cystic lesion (Acta Radiol 2016;57:758)
Prognostic factors
- Stage is the most important prognostic factor
- Survival rates: > 95% for stage IA and IB and 51% for stage III and IV (J Natl Cancer Inst 2019;111:60)
- Most tumors are confined to the ovary at diagnosis
- CTNNB1 (beta catenin) mutation and low tumor grade are associated with a favorable outcome (Histopathology 2019;74:452, Am J Surg Pathol 2021;45:68)
- Synchronous endometrioid carcinomas of the endometrium and ovaries are often clonally related but typically have indolent clinical behavior (J Natl Cancer Inst 2016;108:djv428, J Natl Cancer Inst 2016;108:djv427, Mod Pathol 2021;34:994)
Case reports
- 39 year old woman with Cowden syndrome incidentally detected from a metachronous ovarian endometrioid carcinoma (BMC Cancer 2019;19:1014)
- 41 year old woman with mixed adenocarcinoma and yolk sac tumor (Int J Clin Exp Pathol 2019;12:3549)
- 45 year old woman with endometrial endometrioid and synchronous bilateral endometrioid ovarian cancer (Anticancer Res 2017;37:969)
- 52 year old woman with ovarian mass on computed tomography imaging and a raised CA-125 (Case of the Month #500)
- 65 year old postmenopausal woman with ovarian endometrioid carcinoma presenting as an abdominal wall abscess (J Midlife Health 2018;9:222)
Treatment
- Surgery for early stage cancers
- Adjuvant chemotherapy is associated with survival benefit for patients with inadequately staged and grade 2 stage I cancers (Gynecol Oncol 2020;156:315)
- Patients with advanced stage disease (FIGO III and IV) might benefit from platinum based chemotherapy (Future Oncol 2018;14:123)
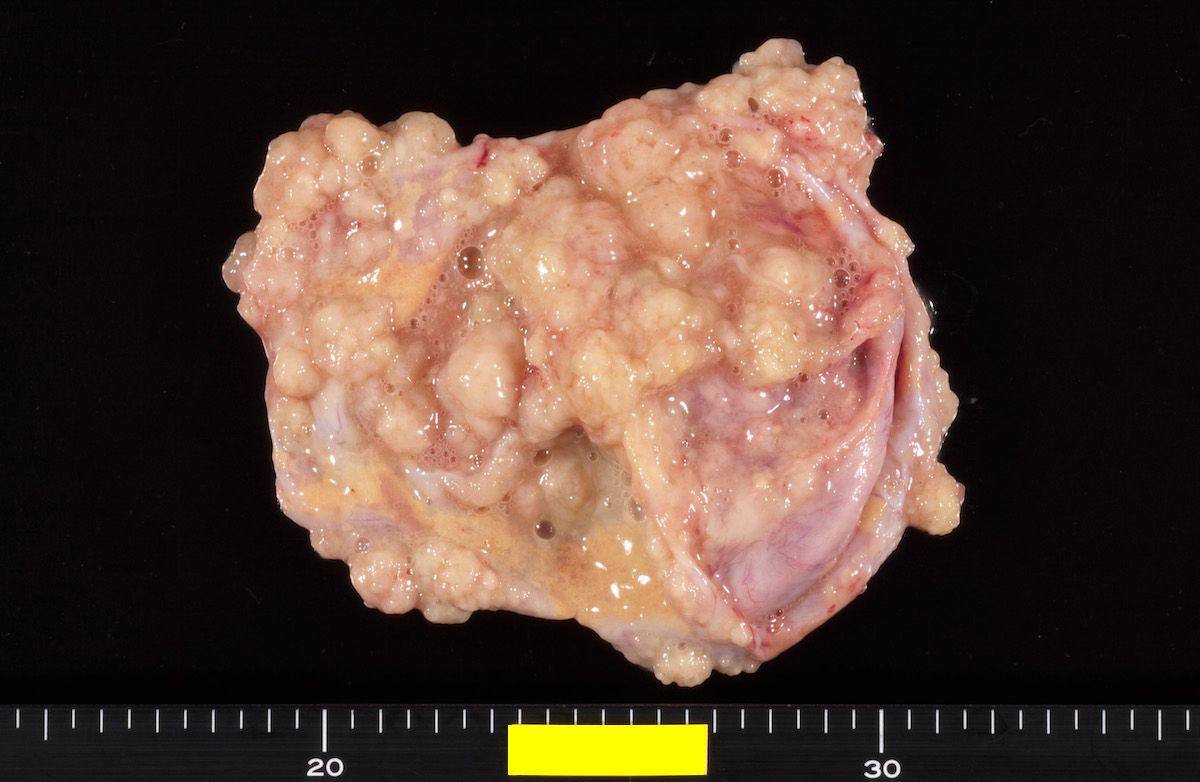
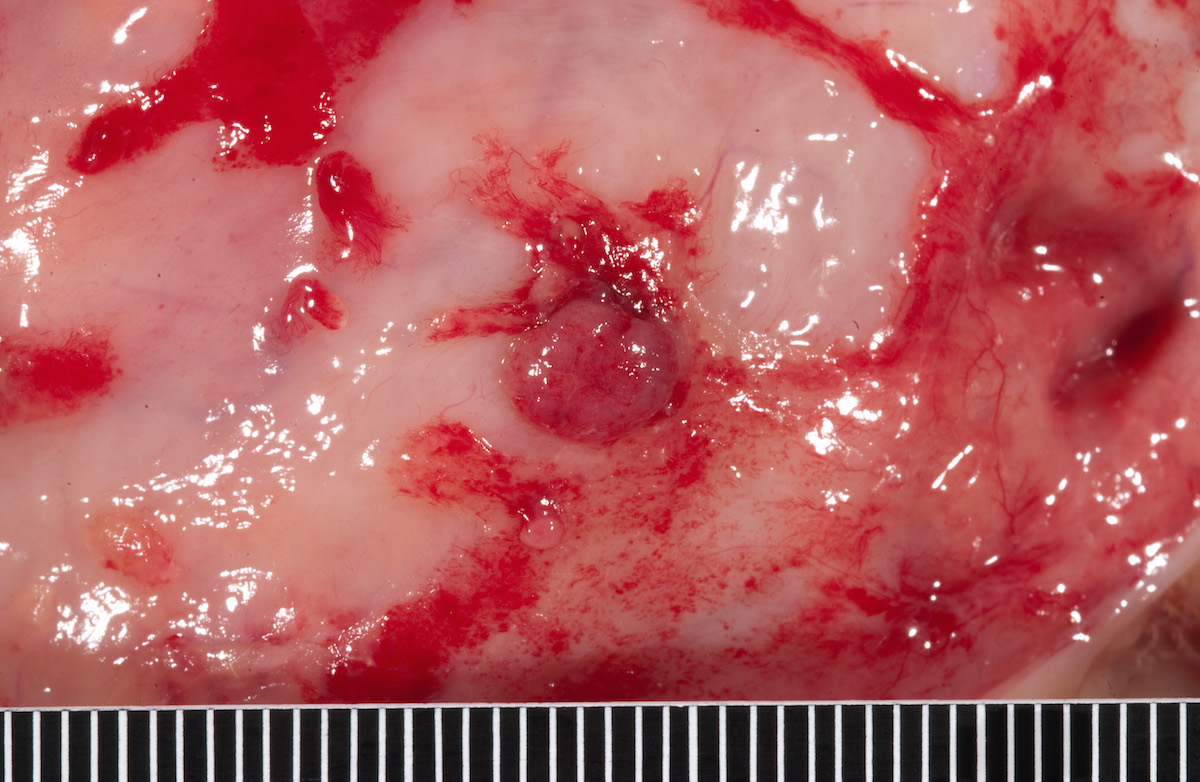
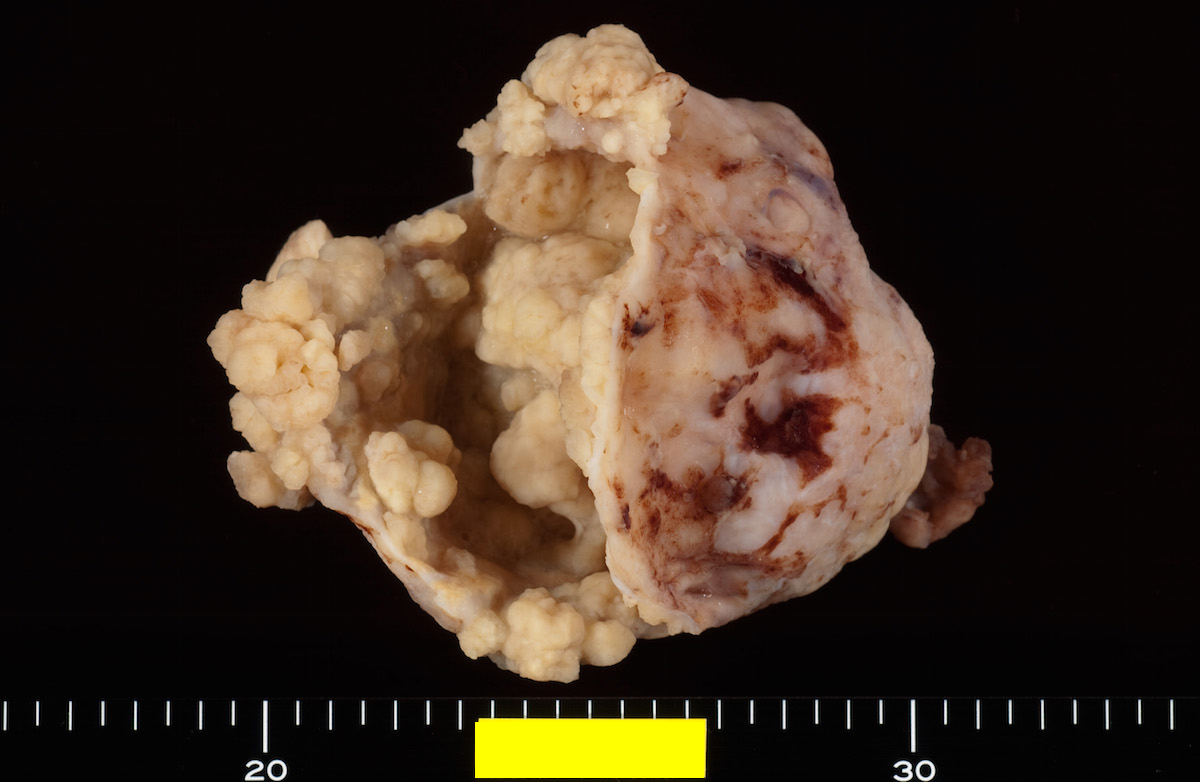
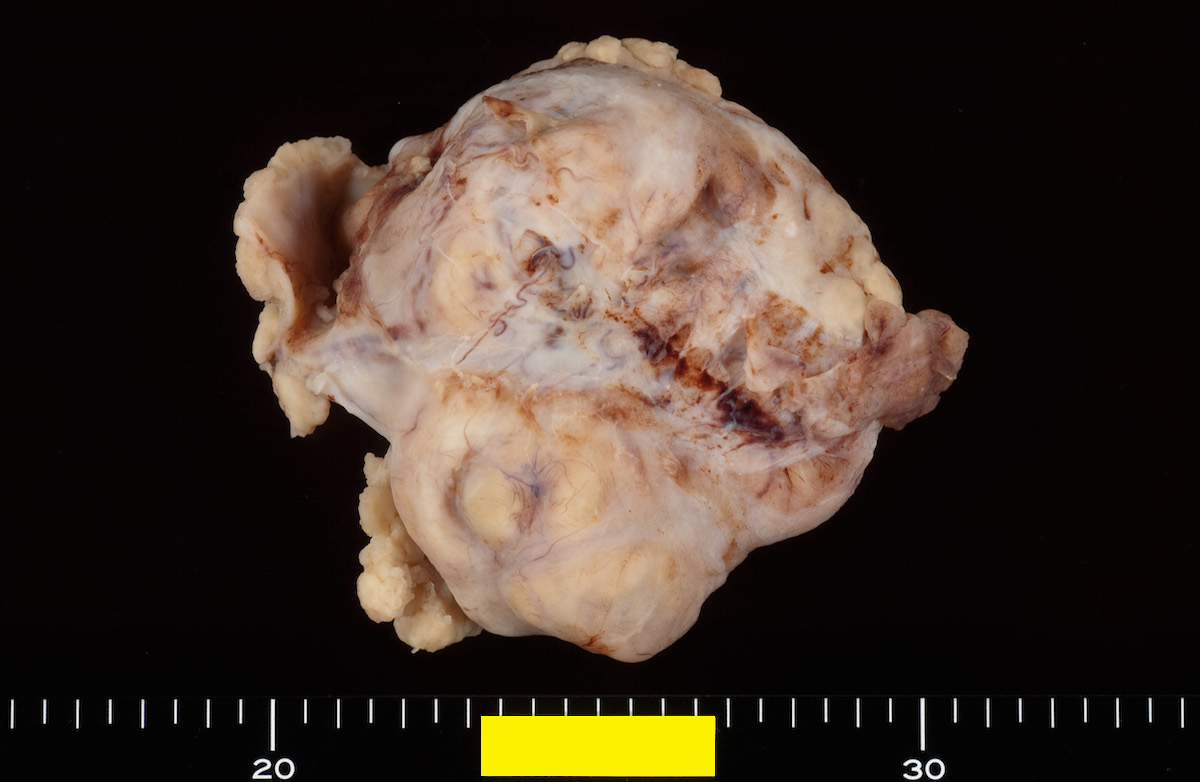
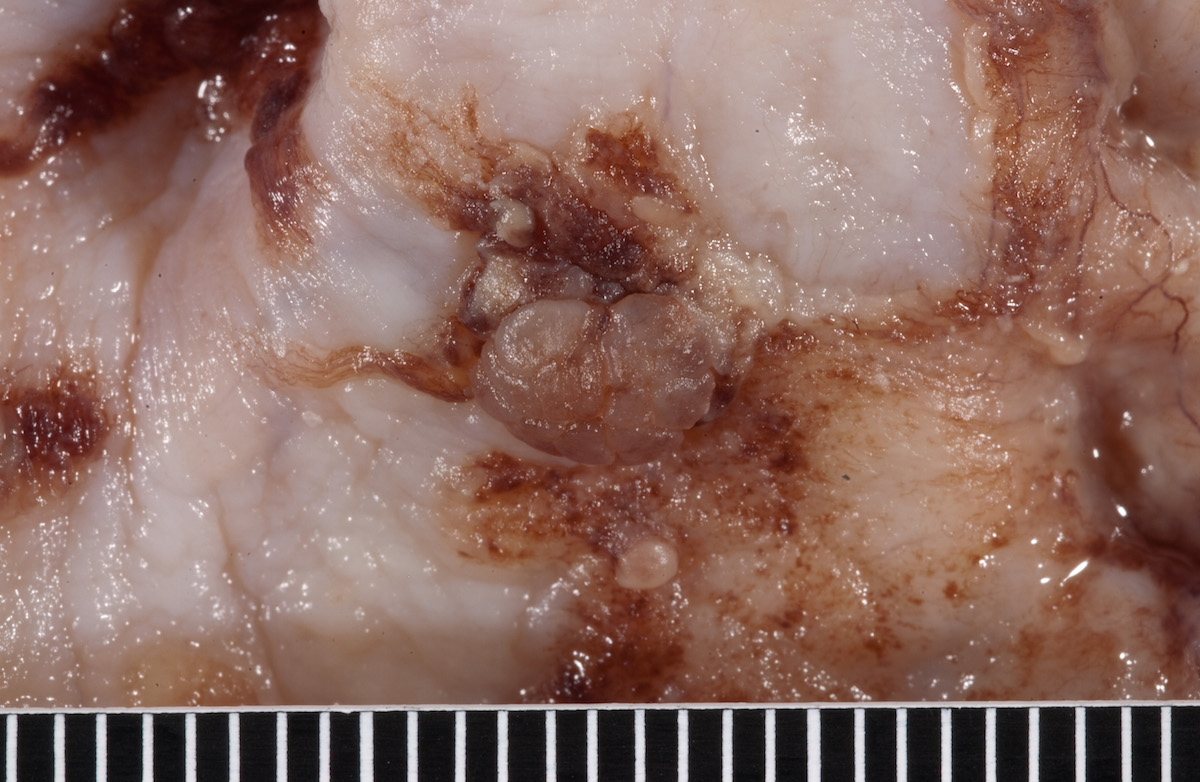
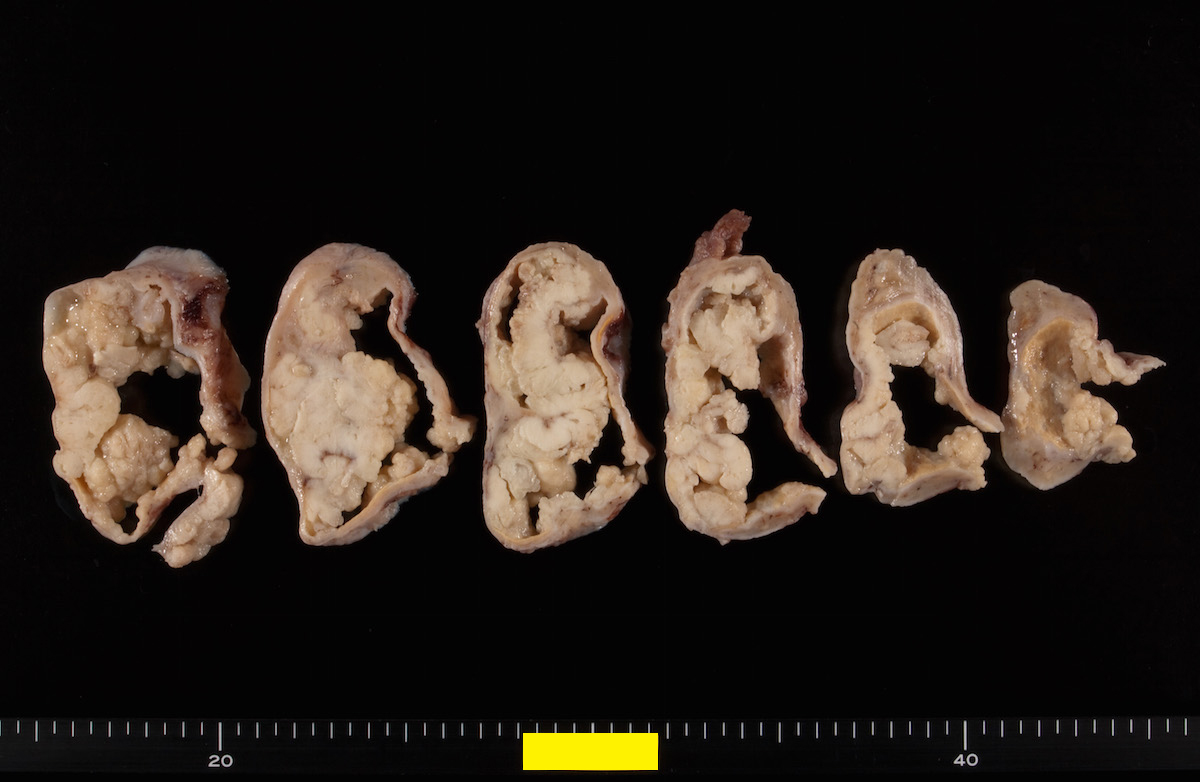
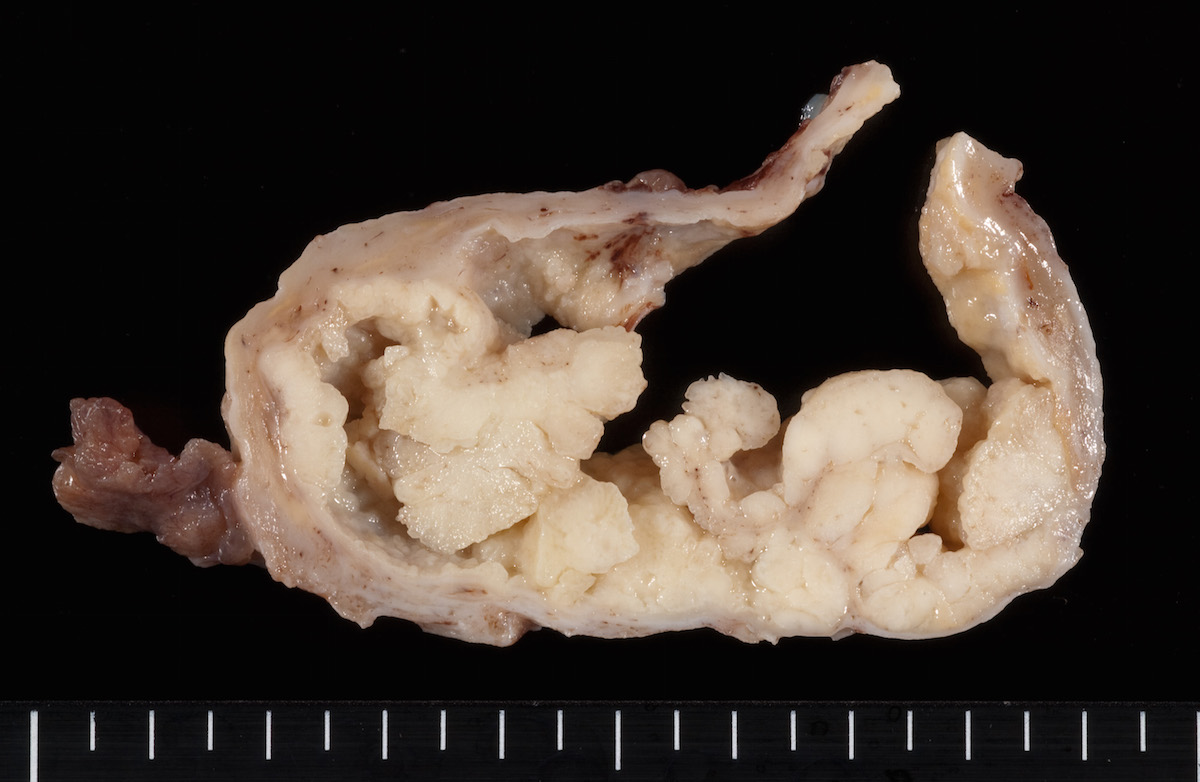
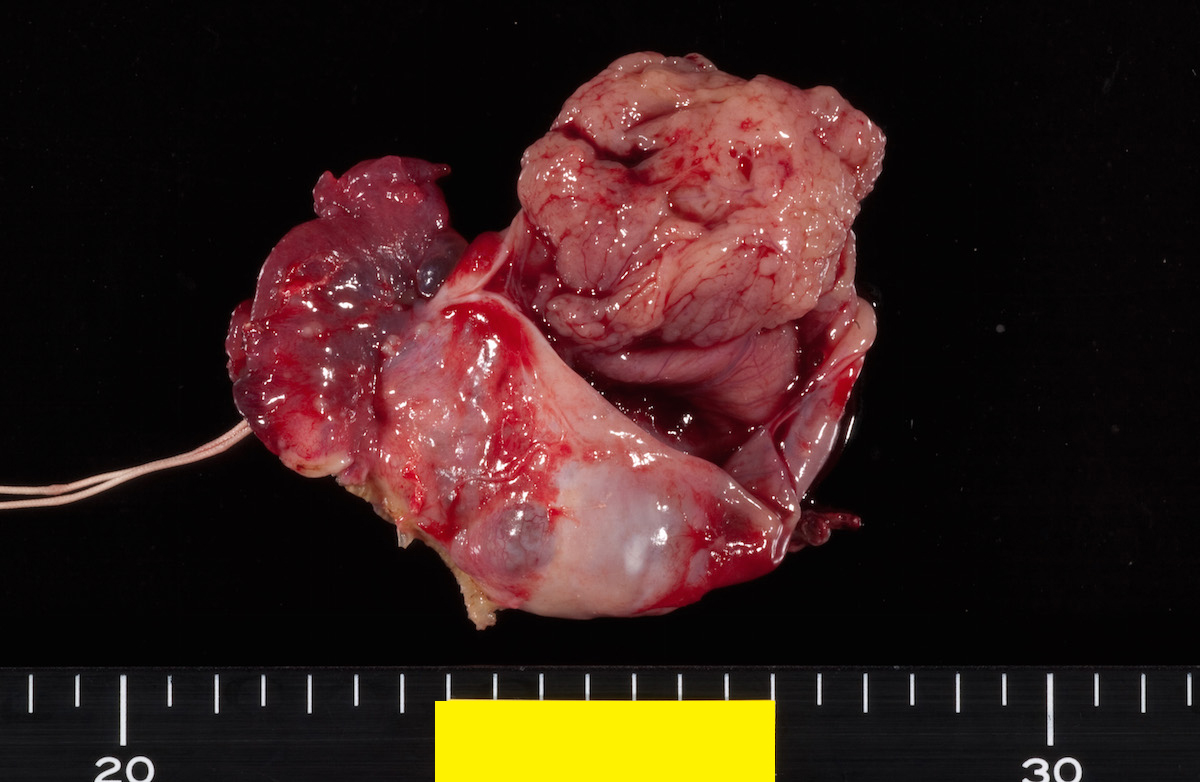
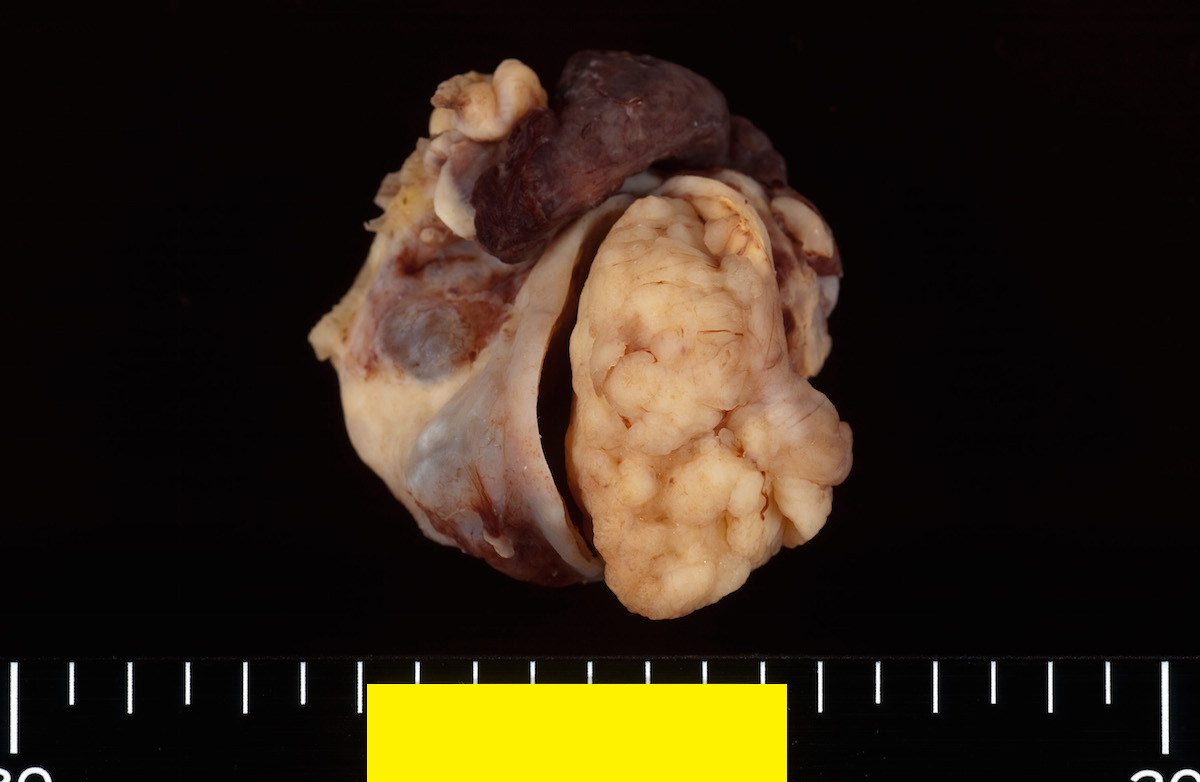
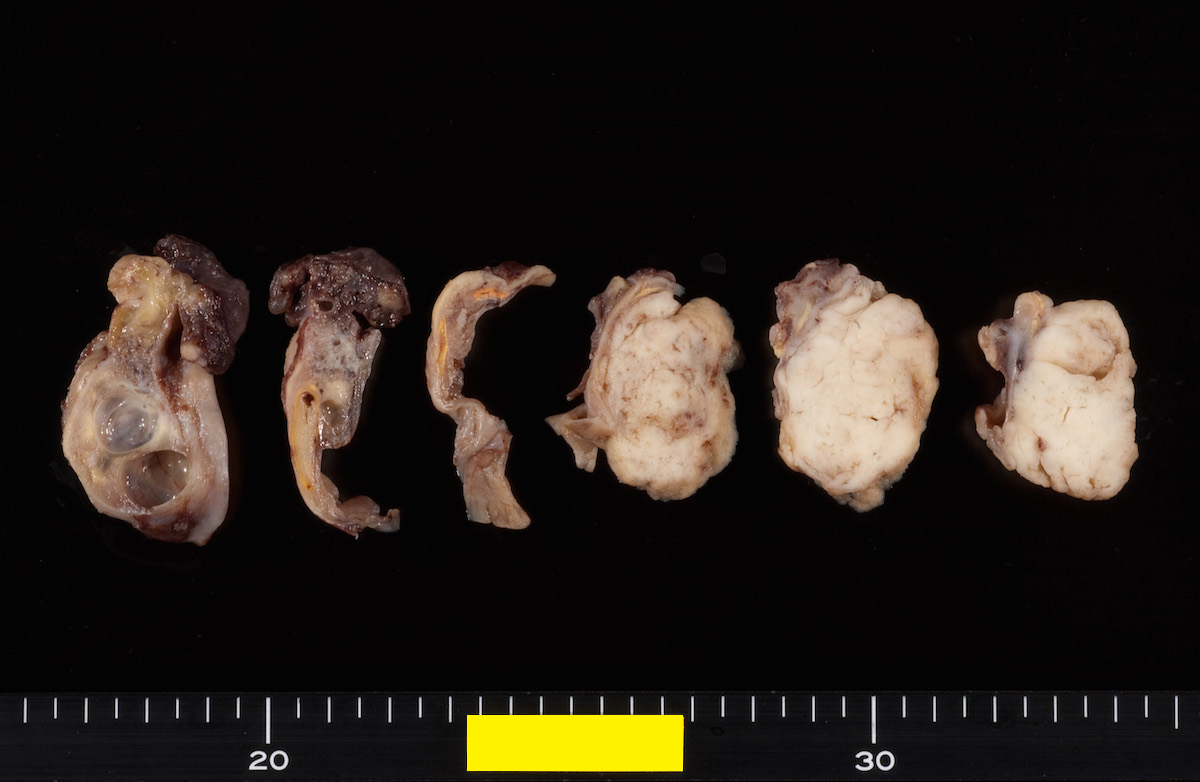
Gross description
- Usually unilateral; only 5% bilateral
- Cystic with solid component and areas of hemorrhage
- With or without polypoid nodule in endometriotic cyst
- Mean tumor size: 11 cm (range: 3 - 22 cm)
- Reference: Arch Gynecol Obstet 2008;278:209
Gross images
AFIP images
Contributed by Ayse Ayhan, M.D.
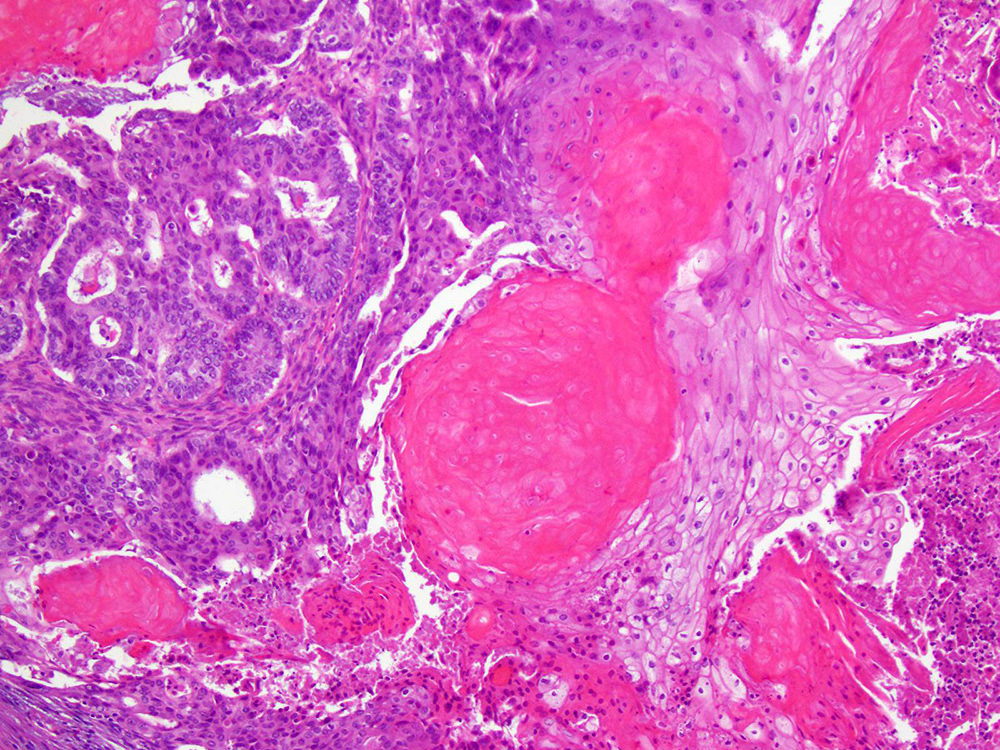
Frozen section description
- Depending on histologic grade, a combination of glandular and solid areas may be seen
- Squamous differentiation may be present
- Differential diagnosis depends on histologic grade but includes metastatic carcinoma, well differentiated Sertoli-Leydig cell tumor and serous carcinoma (Arch Pathol Lab Med 2019;143:47)
Frozen section images
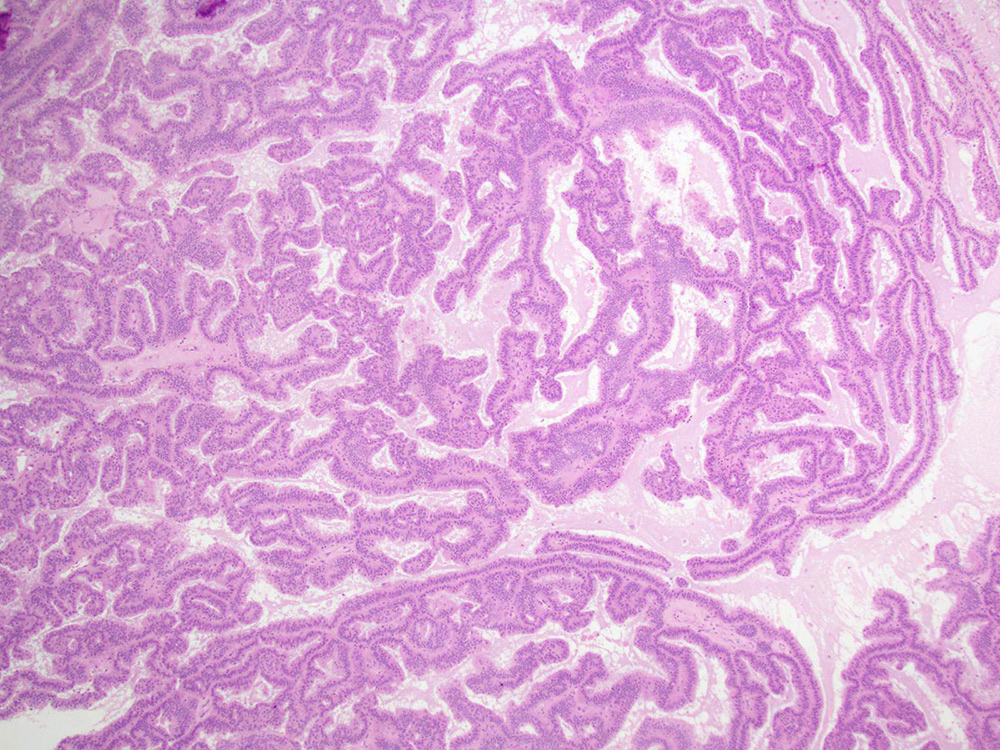
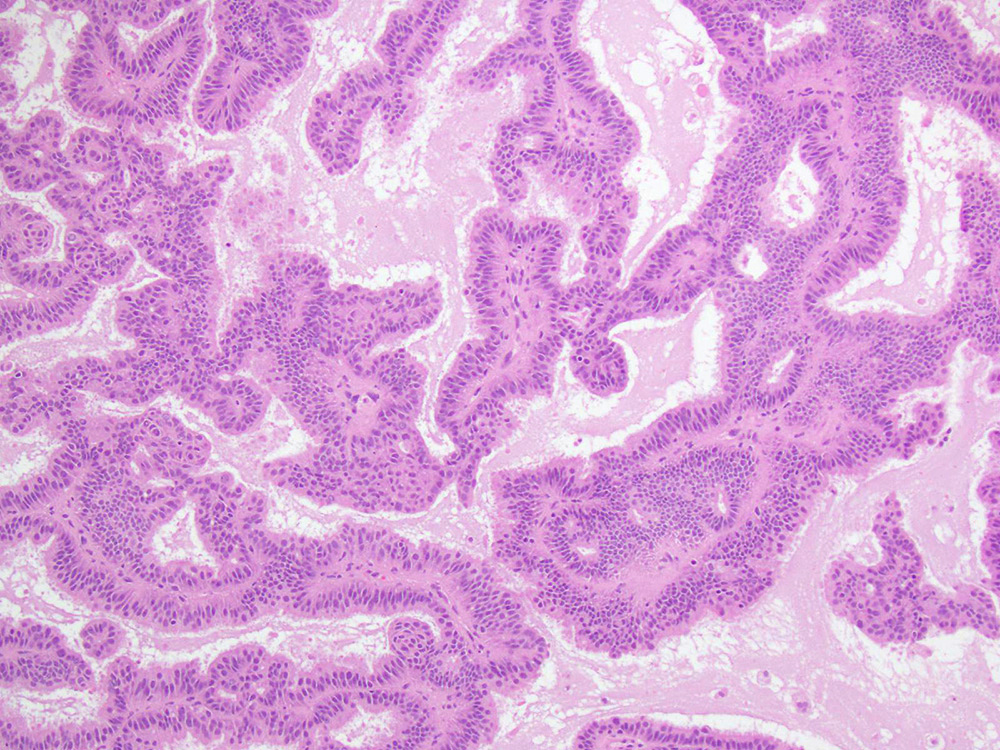
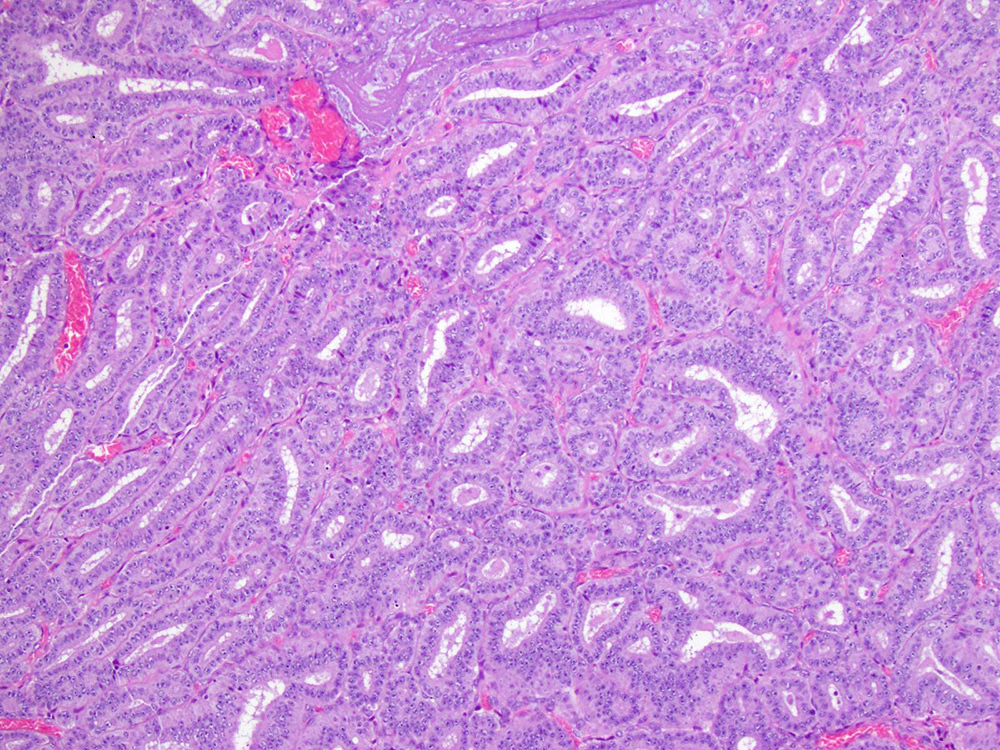
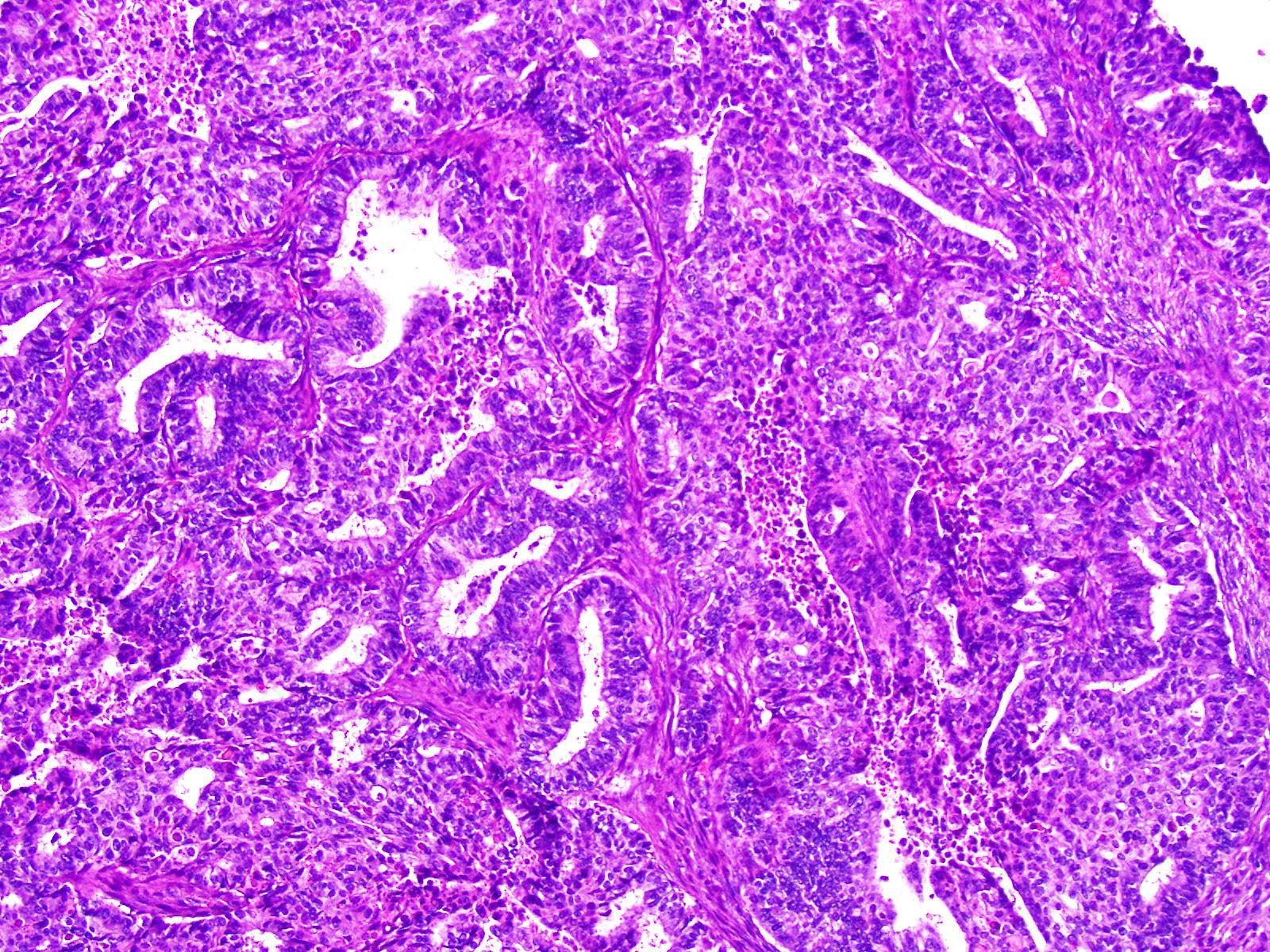
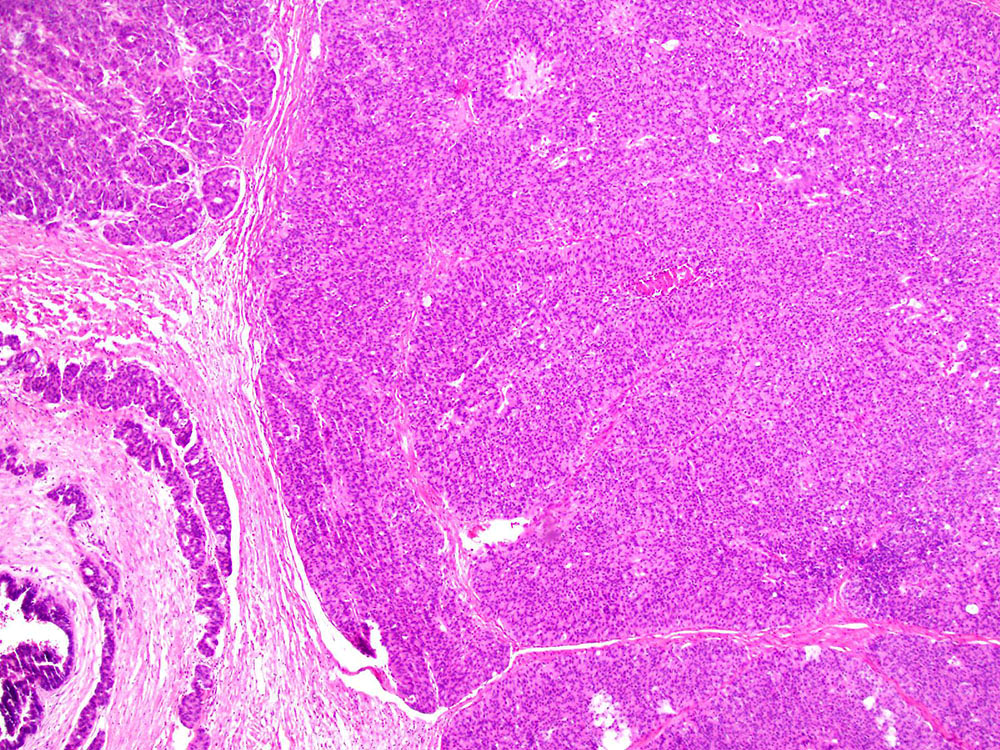
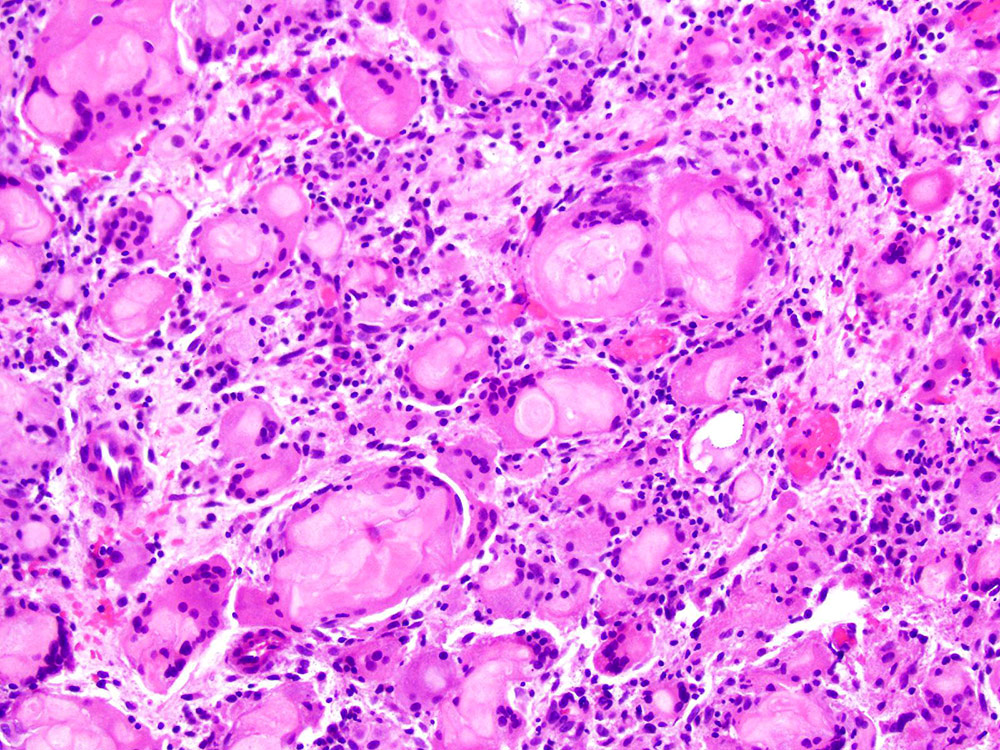
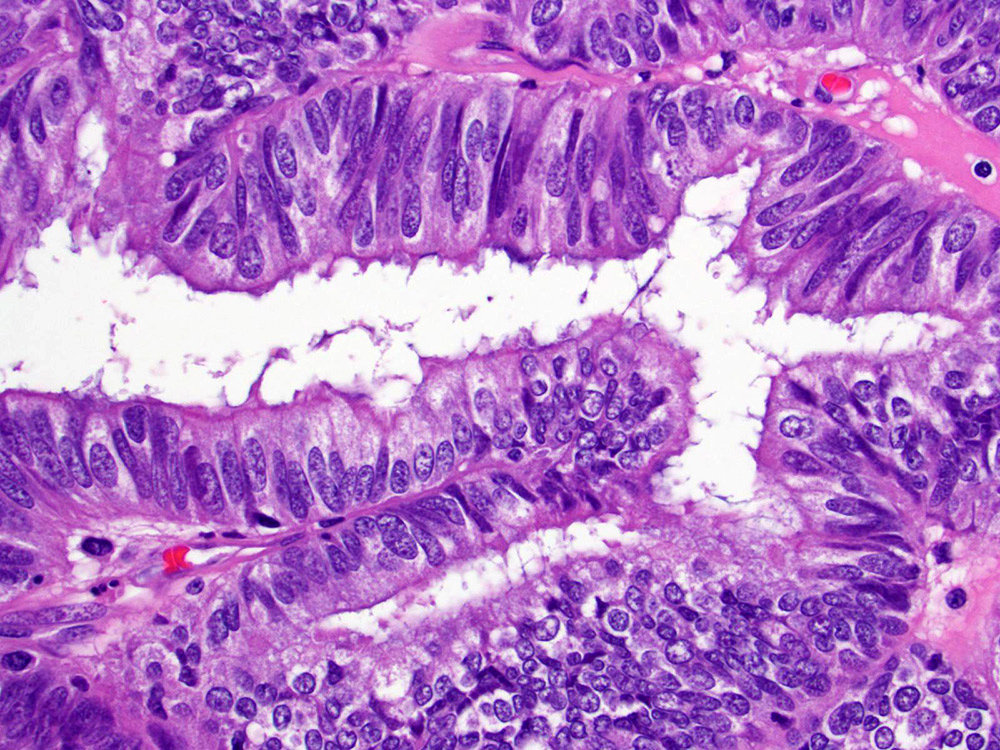
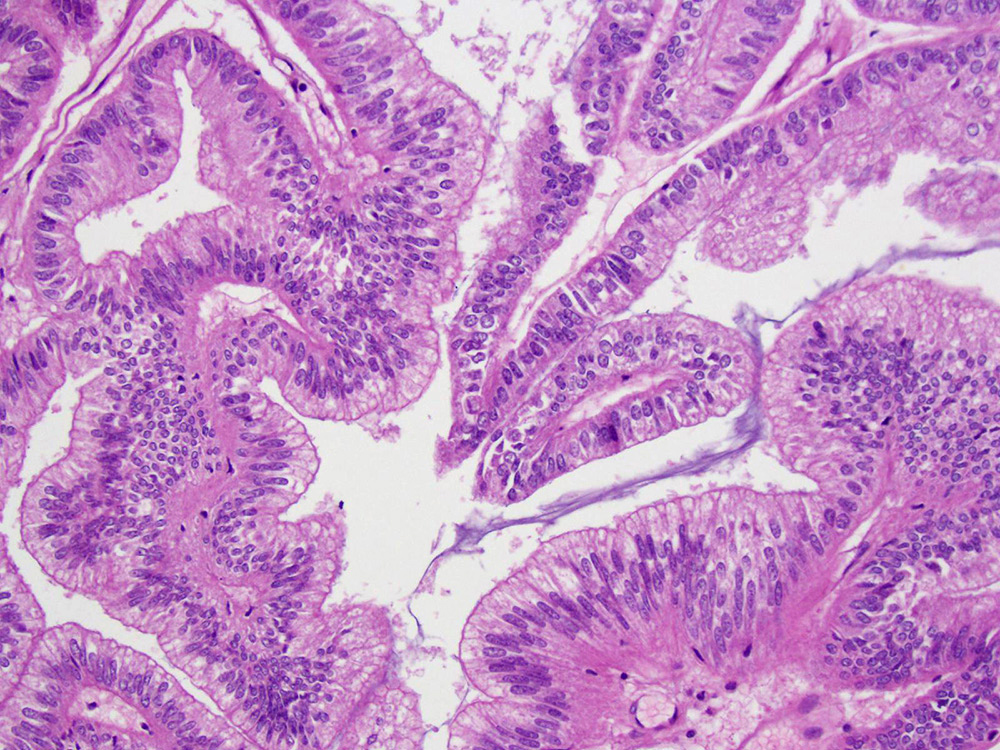
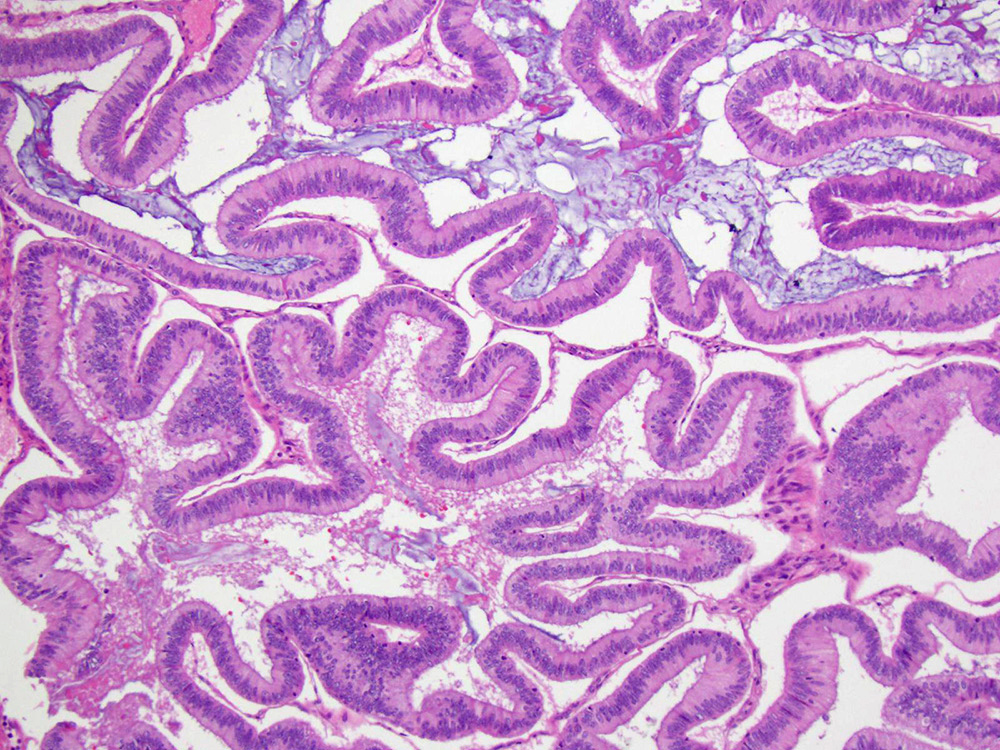
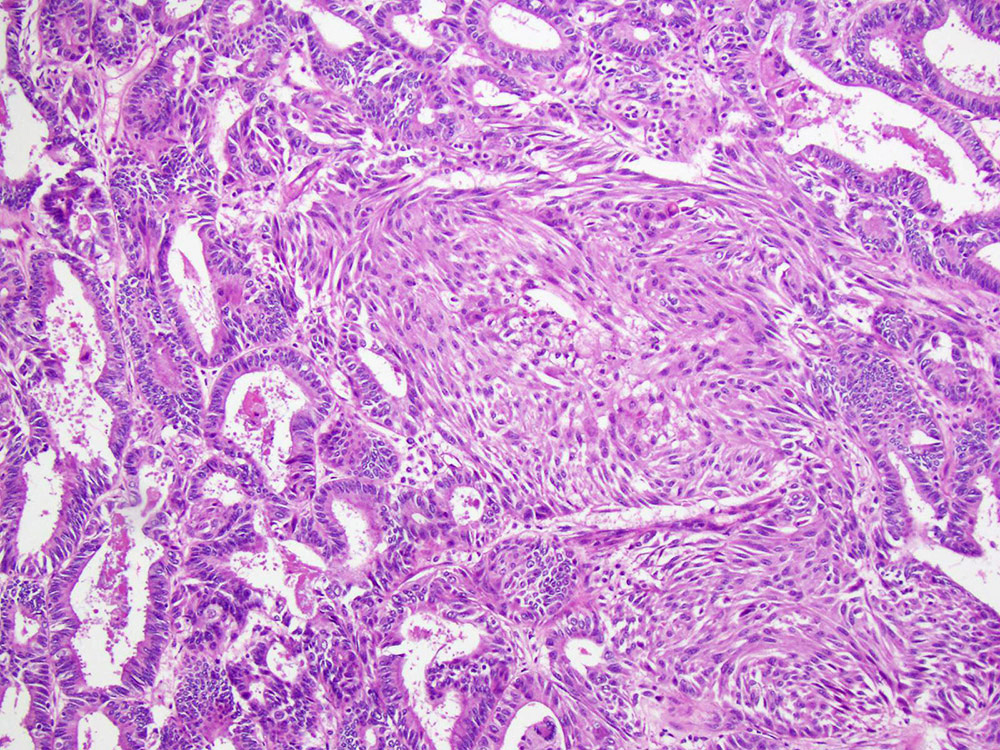
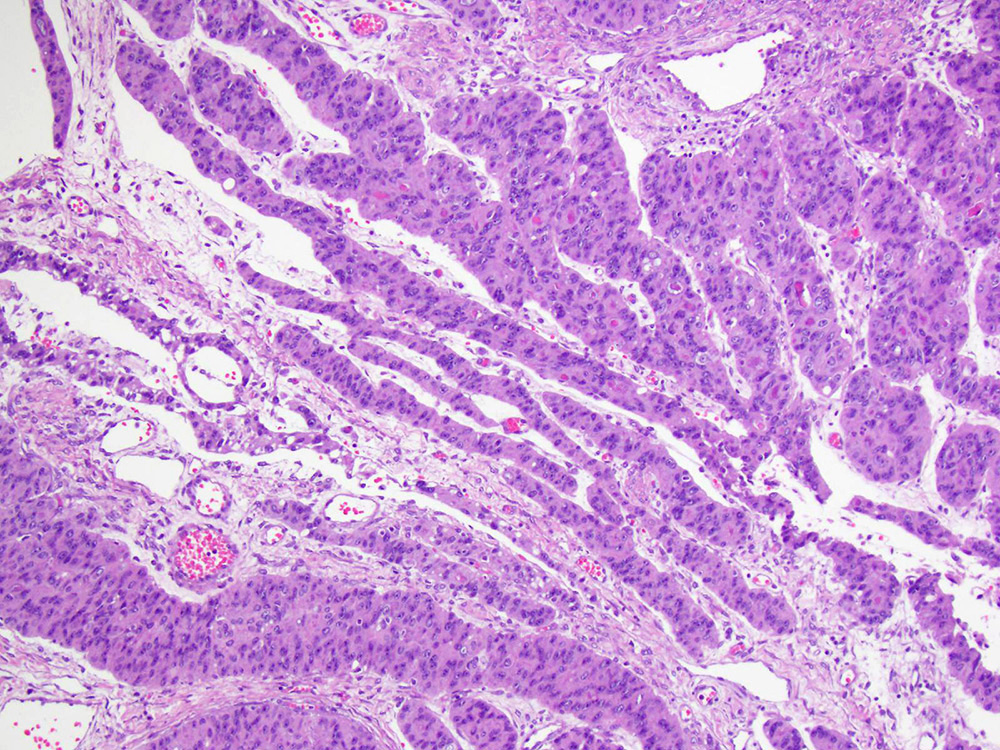
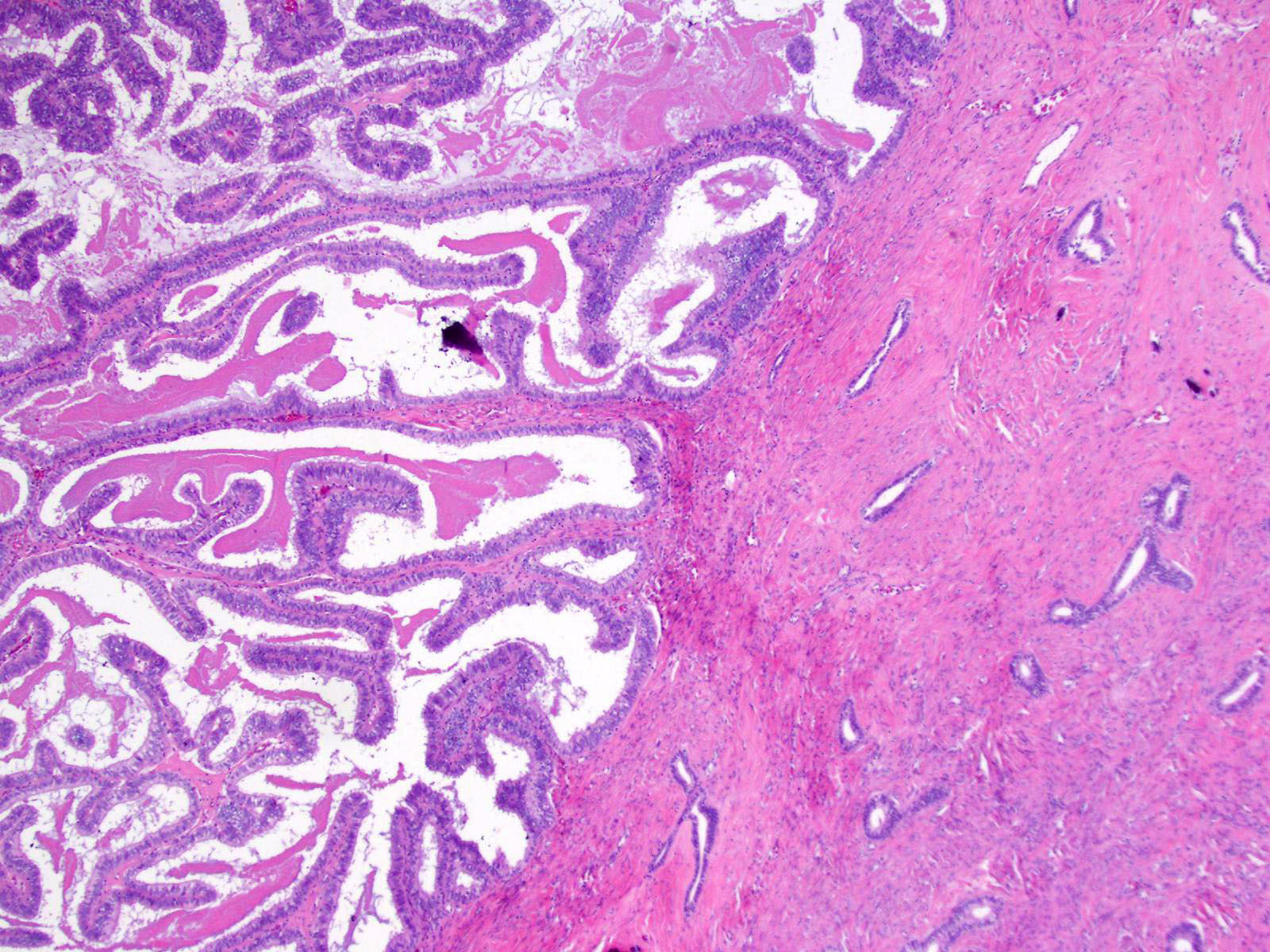
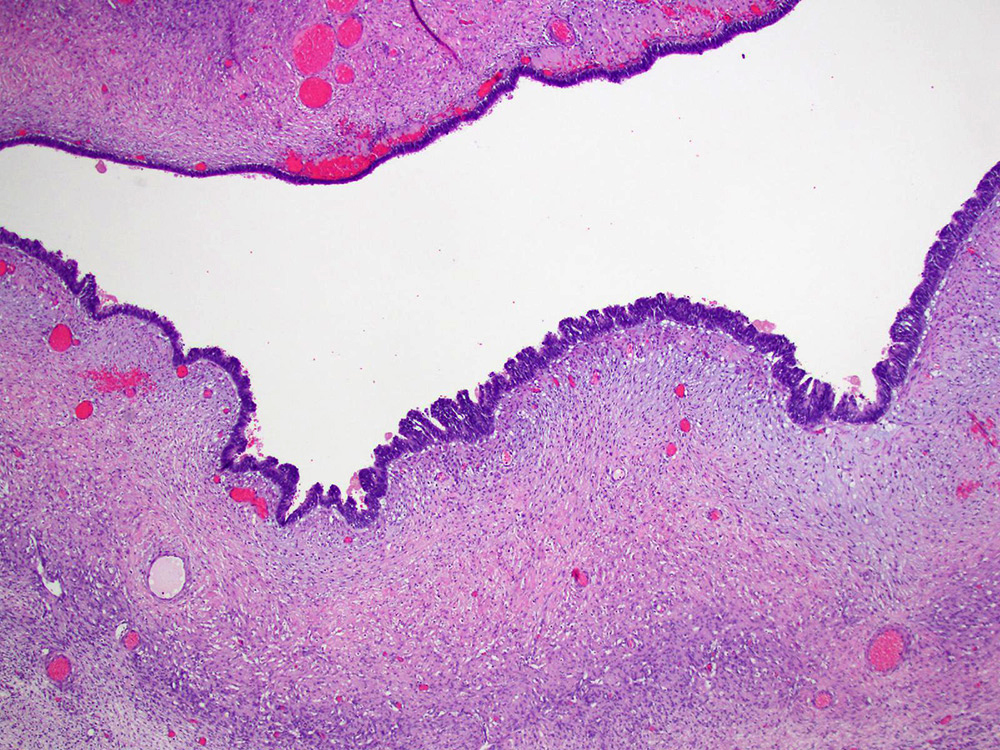
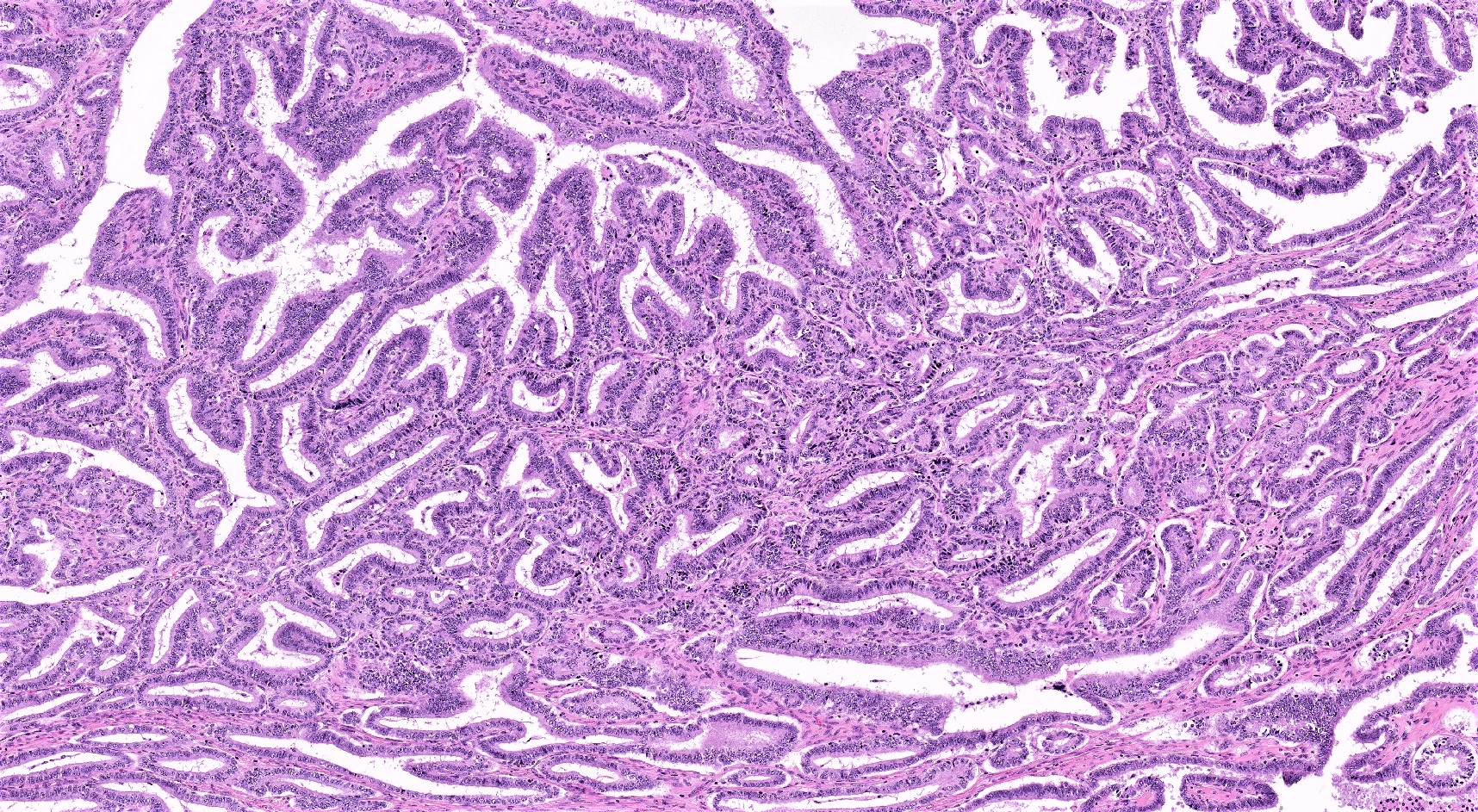
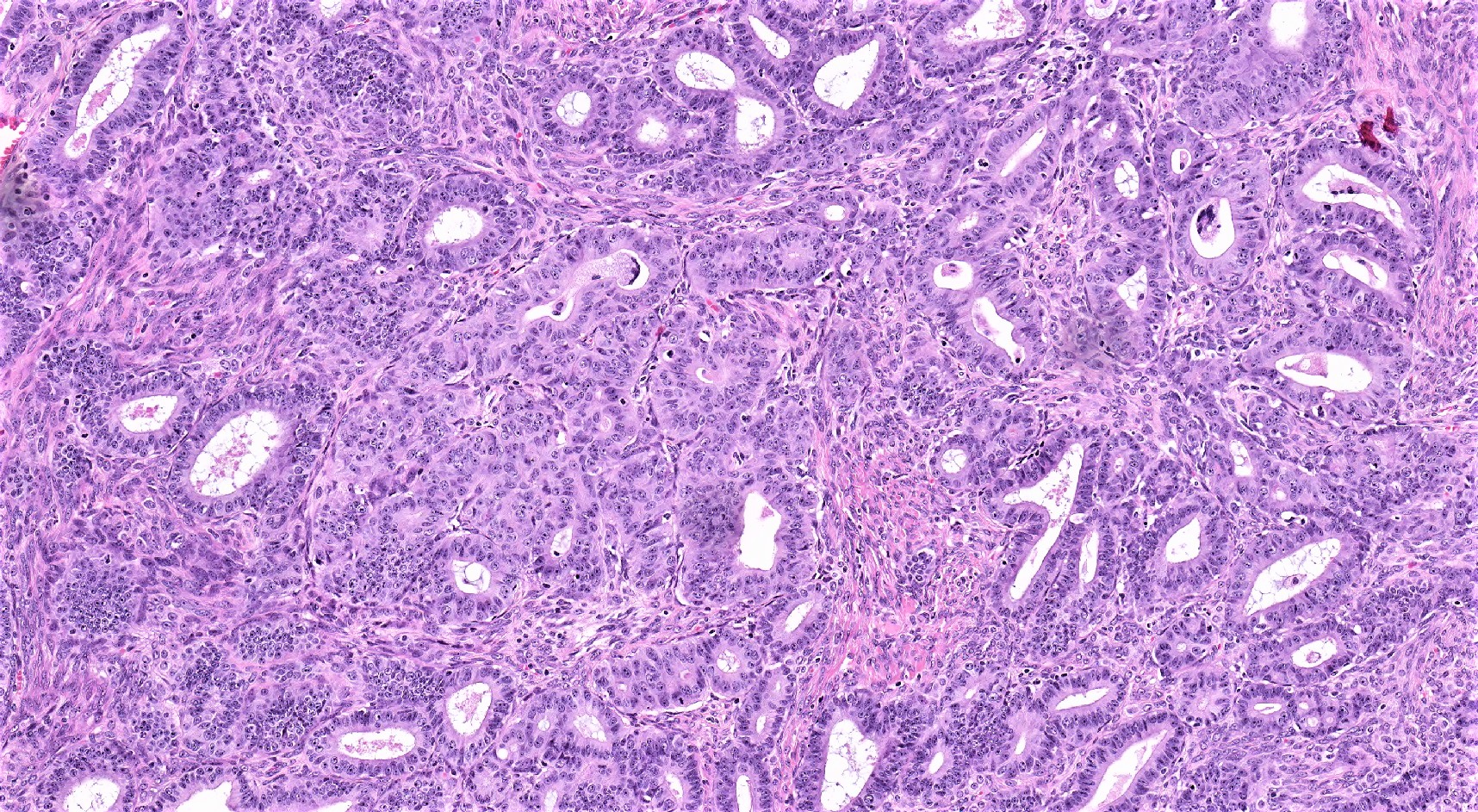
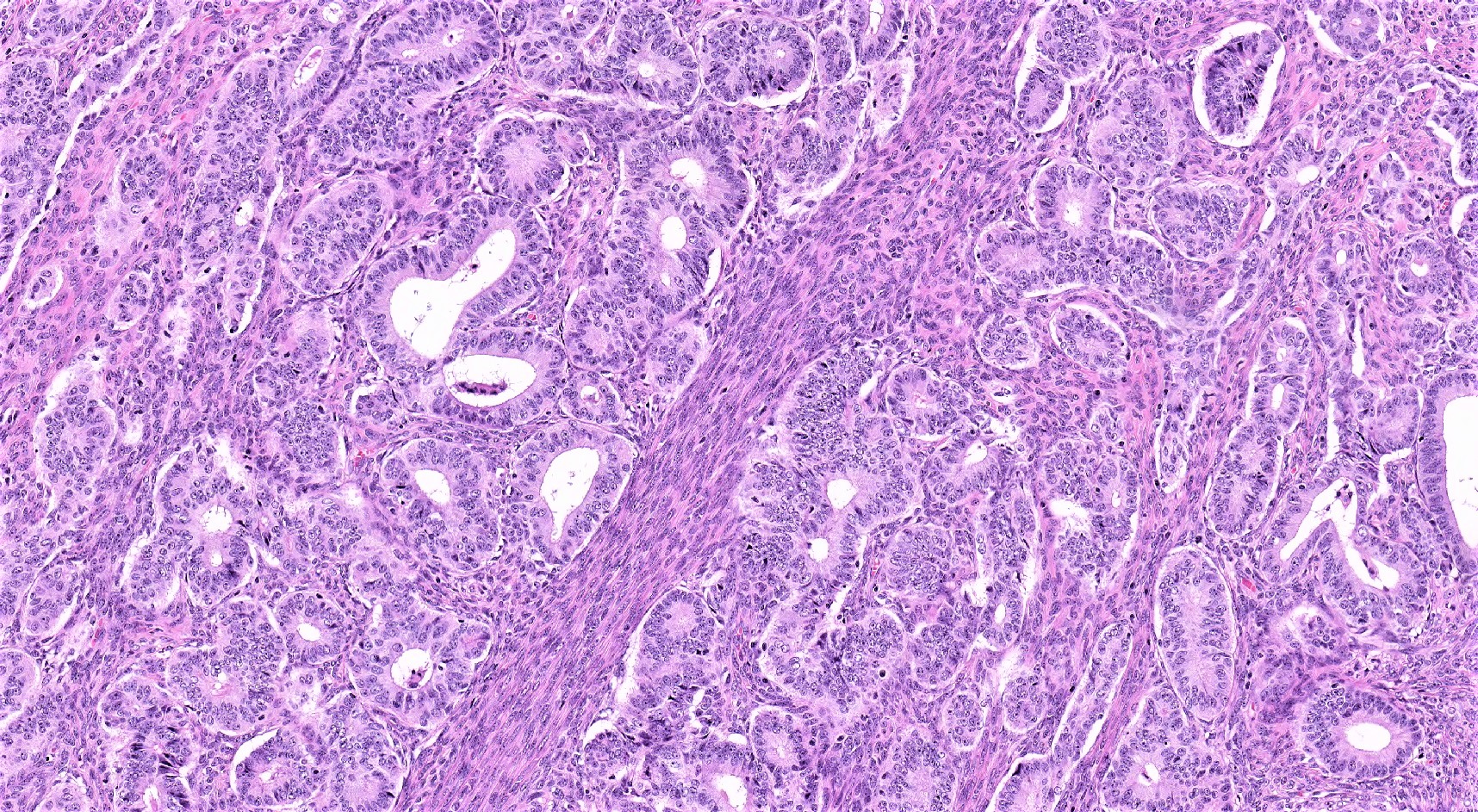
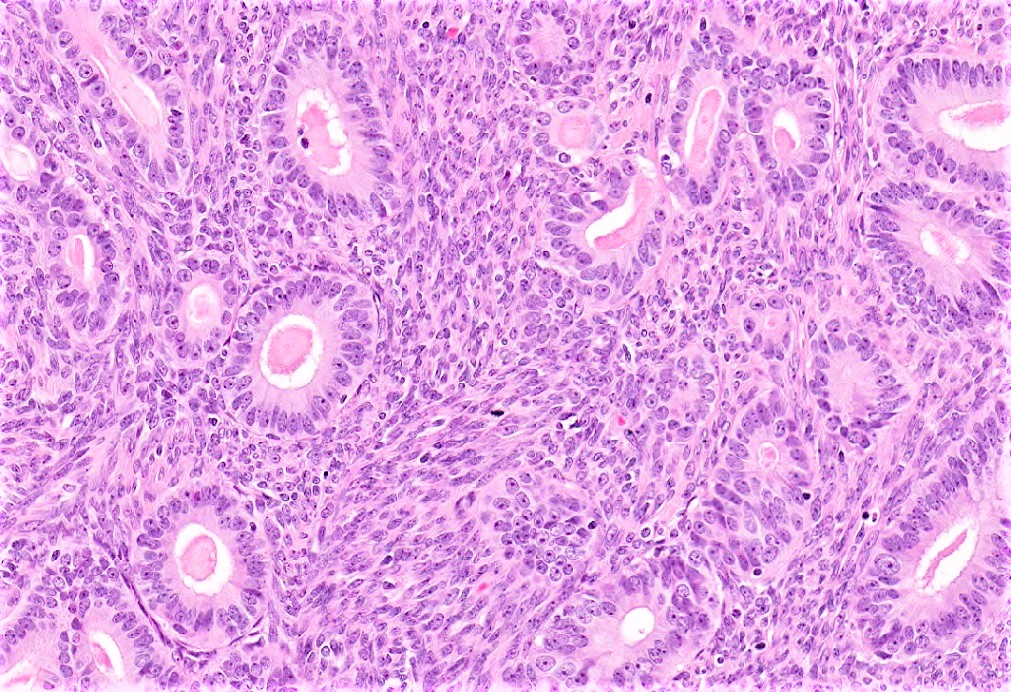
Microscopic (histologic) description
- Most common morphologic pattern is confluent (back to back) glands
- Stromal invasion is usually by expansion; rarely, destructive stromal invasion can be observed
- Squamous metaplasia (morules or keratin pearls), cytoplasmic mucin, intracytoplasmic vacuoles, oncocytic changes, clear cell changes and cilia and sex cord-like elements (sertoliform) can be observed; none of these morphologic features affect the histologic grade (Am J Surg Pathol 2007;31:1203)
- Histologic grading: same as for endometrial endometrioid adenocarcinoma
- FIGO grade 1: less than 5% solid component
- FIGO grade 2: 6 - 50% solid component
- FIGO grade 3: more than 50% solid component
- Endometriosis or adenofibroma may be present in the background
- Vascular invasion is rare
- Might be associated with serous, undifferentiated carcinoma and yolk sac tumor (mixed carcinoma) (Am J Surg Pathol 1994;18:687, Am J Surg Pathol 1996;20:1056)
- Morphologic features in favor of synchronous endometrial and ovarian tumors:
- Both tumors are low grade
- No myometrial invasion or less than 50% myometrial inivasion
- There is no involvement in any other anatomical sites
- No lymphovascular involvement in either tumor
- Background atypical endometrial hyperplasia in the endometrium
- Unilateral ovarian involvement and unifocal parenchymal distribution of tumor
- Lack of ovarian capsular, multifocal or hilar involvement
- Presence of endometriosis or adenofibroma in the ovary (Int J Gynecol Pathol 2019;38:S75)
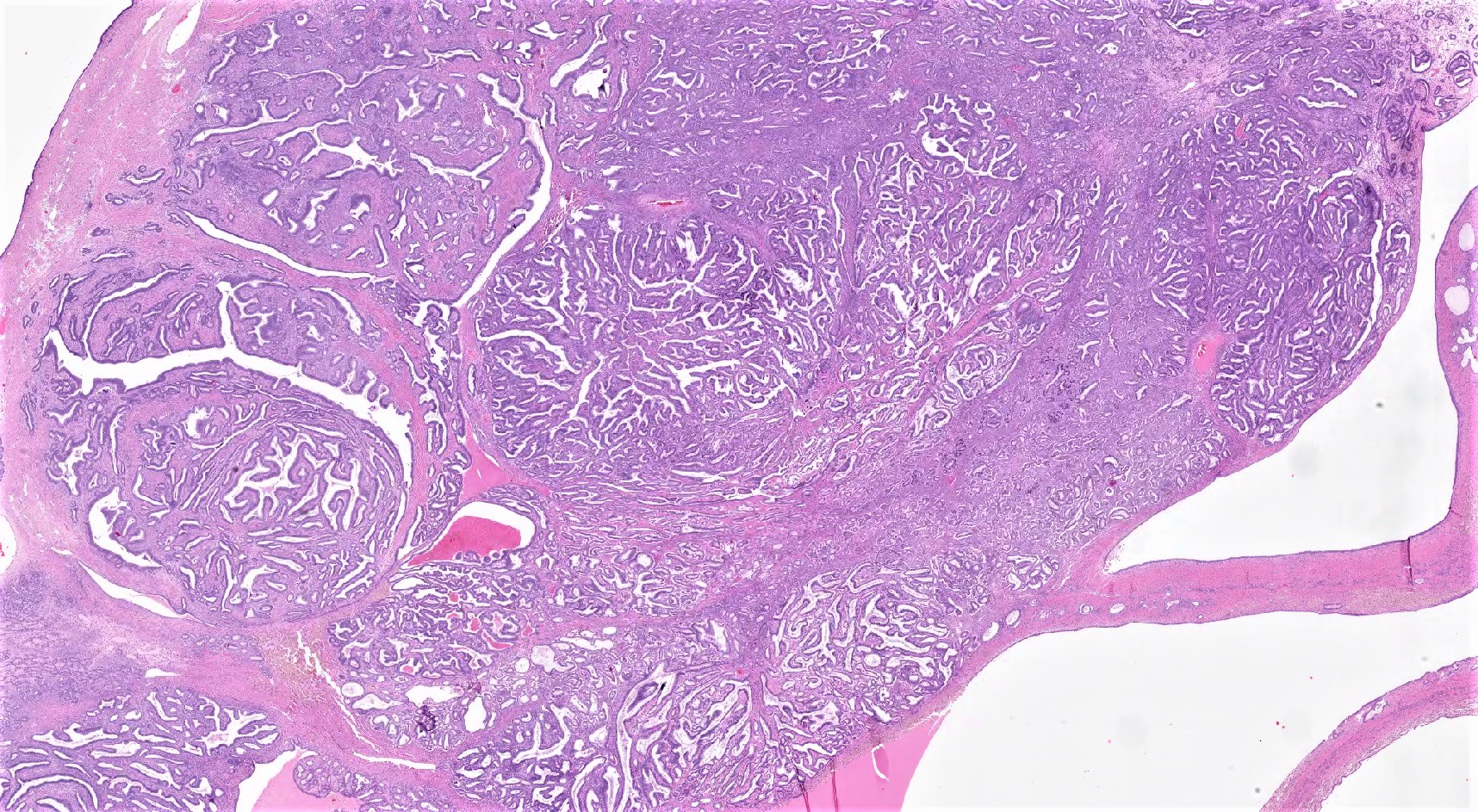
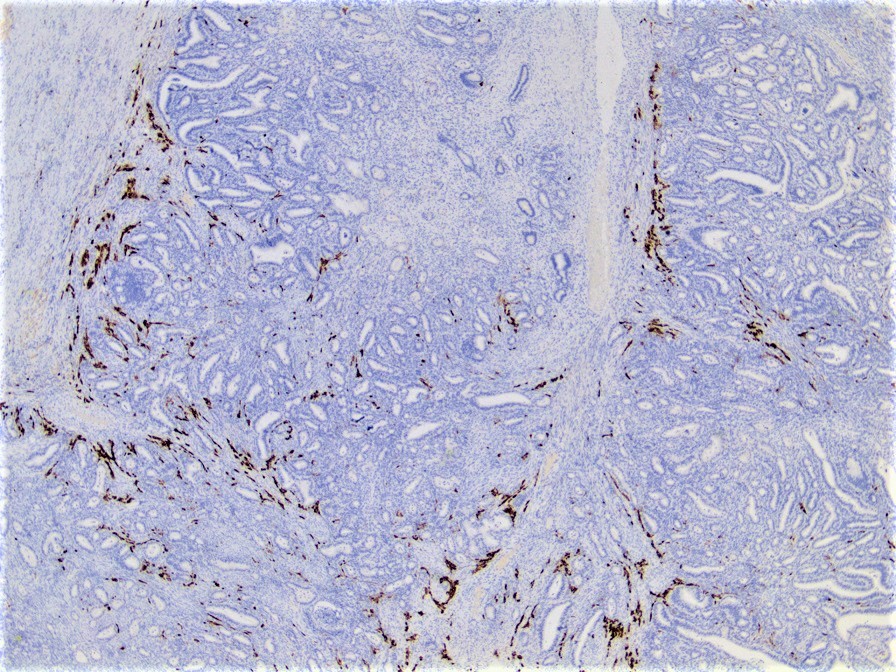
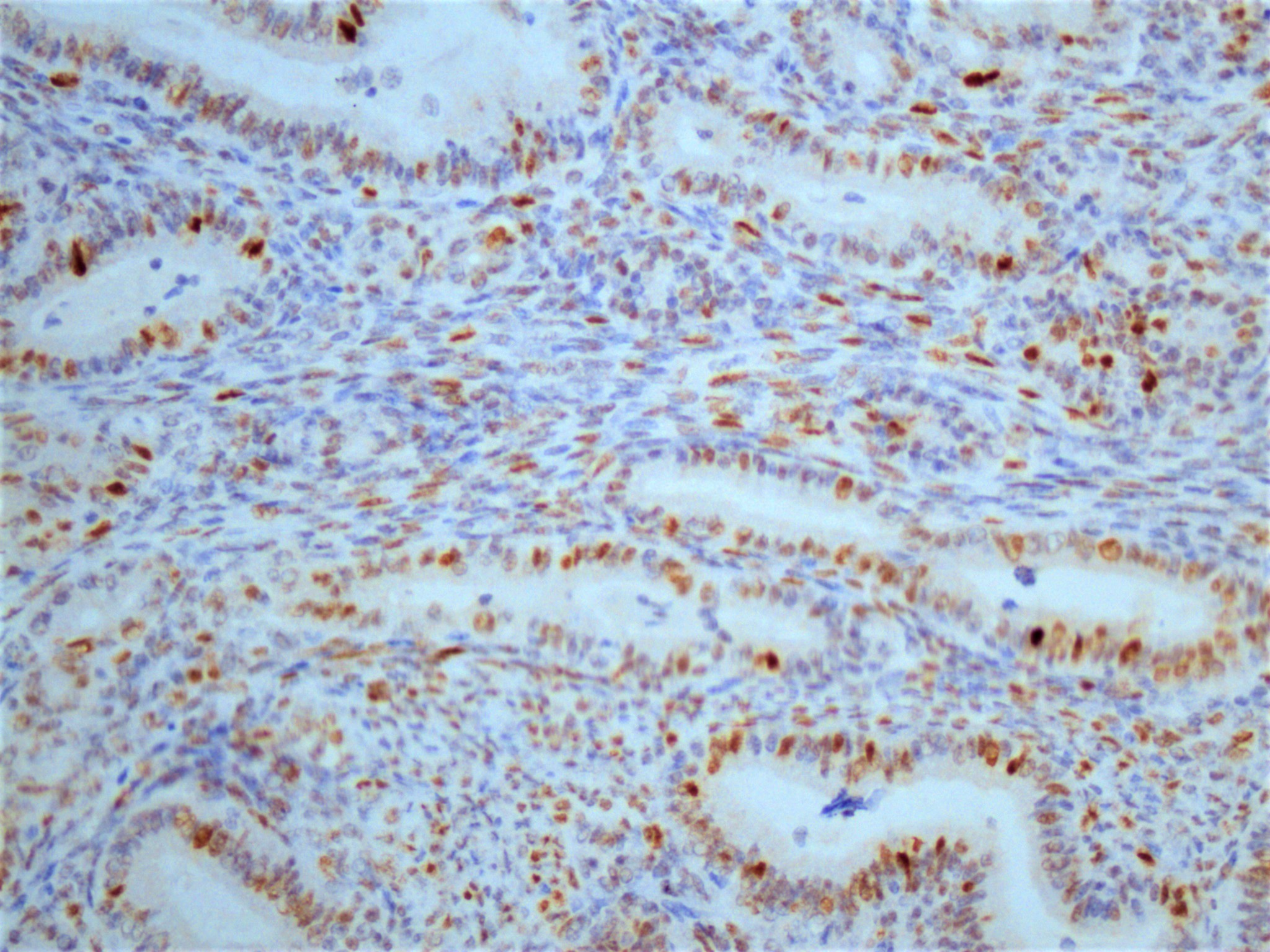
Microscopic (histologic) images
Contributed by Ozlen Saglam, M.D.
Contributed by Sakinah A Thiryayi, M.D. and Gulisa Turashvili, M.D., Ph.D. (Case #500)
Cytology description
- Large cohesive cell clusters
- Mild nuclear membrane irregularities
- May see squamous differentiation
- Detection in pelvic washing: sensitivity 58%, specificity 89% Cancer 2004;102:150
Positive stains
- Keratin cocktails, EMA, CK7, PAX8 (15% negative), ER and PR (Semin Diagn Pathol 2005;22:3, Int J Gynecol Pathol 2016;35:430)
- p53: wild / normal type expression (most tumors) (Int J Gynecol Pathol 2016;35:430, Am J Surg Pathol 2018;42:534)
- High grade endometrioid cancers might demonstrate mutational pattern (nuclear staining in > 80% of cells, complete absence of staining, diffuse cytoplasmic staining)
- Mismatch repair protein deficiency has been reported in up to 23% of tumors (Gynecol Oncol 2020;156:669, Am J Surg Pathol 2019;43:235)
Negative stains
Molecular / cytogenetics description
- Ovarian endometrioid cancers and associated endometriosis share mutations in majority of cases (85 - 90%) (J Pathol 2018;245:265)
- CTNNB1 (53%), PIK3CA (40%), KRAS (33%), ARID1A (30%) and PTEN (17%) are common mutations (Cancer Cell 2007;11:321, Mod Pathol 2014;27:128)
- The Cancer Genome Atlas (TCGA) molecular classifiers for endometrial carcinoma has categorized ovarian endometrioid carcinoma into prognostically significant groups (Mod Pathol 2017;30:1748)
Sample pathology report
- Left ovary and fallopian tube, salpingo-oophorectomy:
- Endometrioid adenocarcinoma, FIGO grade 1 (see synoptic report)
- Tumor size: 8.5 cm
- Ovarian surface: not involved by carcinoma
- Fallopian tube: not involved by carcinoma
- Additional findings: background endometriotic cyst
Differential diagnosis
- Adult granulosa cell tumor:
- Sertoli cell tumor / Sertoli-Leydig cell tumor:
- High grade serous carcinoma:
- Architecture: solid, papillary, labyrinthine, glandular
- Nuclei are large
- Nuclear size variability > 3 fold
- High mitotic activity (> 12 mitoses per 10 high power fields)
- Metastatic colonic carcinoma:
- Metastatic endometrial endometrioid adenocarcinoma:
- Metastatic endometrial endometrioid adenocarcinoma is usually high grade (FIGO grade 3)
- Bilateral involvement
- Multinodular growth
- No endometriosis / adenofibroma background
- Clear cell carcinoma:
Board review style question #1
A 48 year old woman with endometrial carcinoma underwent laparoscopic staging procedure and a right ovarian adenocarcinoma was identified. Endometrial and ovarian lesions have identical morphology (see image). The ovarian lesion is confined to the right ovary and endometrial cancer has superficial myometrial invasion. Which immunostain can be useful to rule out metastatic endometrial adenocarcinoma?
- Immunostains are not contributory in differential diagnosis
- Napsin A
- PAX8
- Vimentin
- WT1
Board review style answer #1
A. Immunostains are not contributory in a differential diagnosis
Comment Here
Reference: Endometrioid carcinoma
Comment Here
Reference: Endometrioid carcinoma
Board review style question #2
Which of the following is associated with favorable disease outcome in patients with ovarian endometrioid carcinoma?
- Strong PAX8 expression
- WT1 expression
- Vimentin expression
- Cytoplasmic napsin A expression
- Low grade tumor and nuclear beta catenin expression
Board review style answer #2
E. Low grade tumor and nuclear beta catenin expression
Comment Here
Reference: Endometrioid carcinoma
Comment Here
Reference: Endometrioid carcinoma
Board review style question #3
What clinical manifestations have most commonly been associated with functioning stroma in ovarian tumors?
- Adrenergic manifestations
- Androgenic manifestations
- Estrogenic manifestations
- Progestogenic manifestations
Board review style answer #3