Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Fielder T, Gupta R. Peripheral ossifying fibroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavityperipheralossifyingfibroma.html. Accessed January 3rd, 2025.
Definition / general
- Reactive gingival proliferation characterized by spindle cell proliferation with calcification or ossification
Essential features
- Reactive gingival lesion; thought to be associated with chronic irritation
- Spindle cell proliferation with calcification or ossification within gingival connective tissue
Terminology
- Other terms include peripheral cementifying fibroma, peripheral cemento-ossifying fibroma, ossifying fibrous epulis, calcifying fibrous epulis (J Indian Soc Periodontol 2014;18:527)
- Should not be confused with odontogenic / central bone tumors, such as ossifying fibroma and cemento-ossifying fibroma
ICD coding
Epidemiology
- More common in females (F:M = ~2:1) (Oral Surg Oral Med Oral Pathol 1987;63:452, Med Oral Patol Oral Cir Bucal 2022;27:e460, J Indian Soc Periodontol 2015;19:83, Pediatr Dent 2001;23:245)
- Second to fourth decades (children and young adults) (Oral Surg Oral Med Oral Pathol 1987;63:452, Med Oral Patol Oral Cir Bucal 2022;27:e460, Br J Oral Maxillofac Surg 2019;57:1081)
- Can occur at any age, reports range from 2 months to 87 years (Oral Surg Oral Med Oral Pathol Oral Radiol 2020;130:e74, Med Oral Patol Oral Cir Bucal 2022;27:e460)
- ~5% of oral hyperplastic lesions (Braz J Otorhinolaryngol 2019;85:399, Indian J Dent Res 2018;29:61, Acta Odontol Latinoam 2015;28:103)
- ~20% of gingival hyperplastic lesions (Quintessence Int 2007;38:103, J Oral Pathol Med 2010;39:631)
Sites
- Arise exclusively on the gingiva
- Maxilla more common than mandible (Oral Surg Oral Med Oral Pathol 1987;63:452, Pediatr Dent 2001;23:245)
- ~67% in incisor cuspid region (Oral Surg Oral Med Oral Pathol 1987;63:452, Med Oral Patol Oral Cir Bucal 2022;27:e460, J Indian Soc Periodontol 2015;19:83)
Pathophysiology
- Unknown, likely a reaction to chronic irritation (J Indian Soc Periodontol 2015;19:83)
- Hormonal influence has been proposed since the lesion is common in adolescents and young women (Niger Med J 2011;52:35)
- However, lesional cells do not express estrogen or progesterone receptors (ER / PR) (J Oral Sci 2010;52:95)
Etiology
- Associated with chronic irritation, poor dentition and dental prosthetics, especially if poorly fitted (J Indian Soc Periodontol 2015;19:83)
- Thought to arise from the periodontal ligament (Ann Diagn Pathol 2020;46:151510)
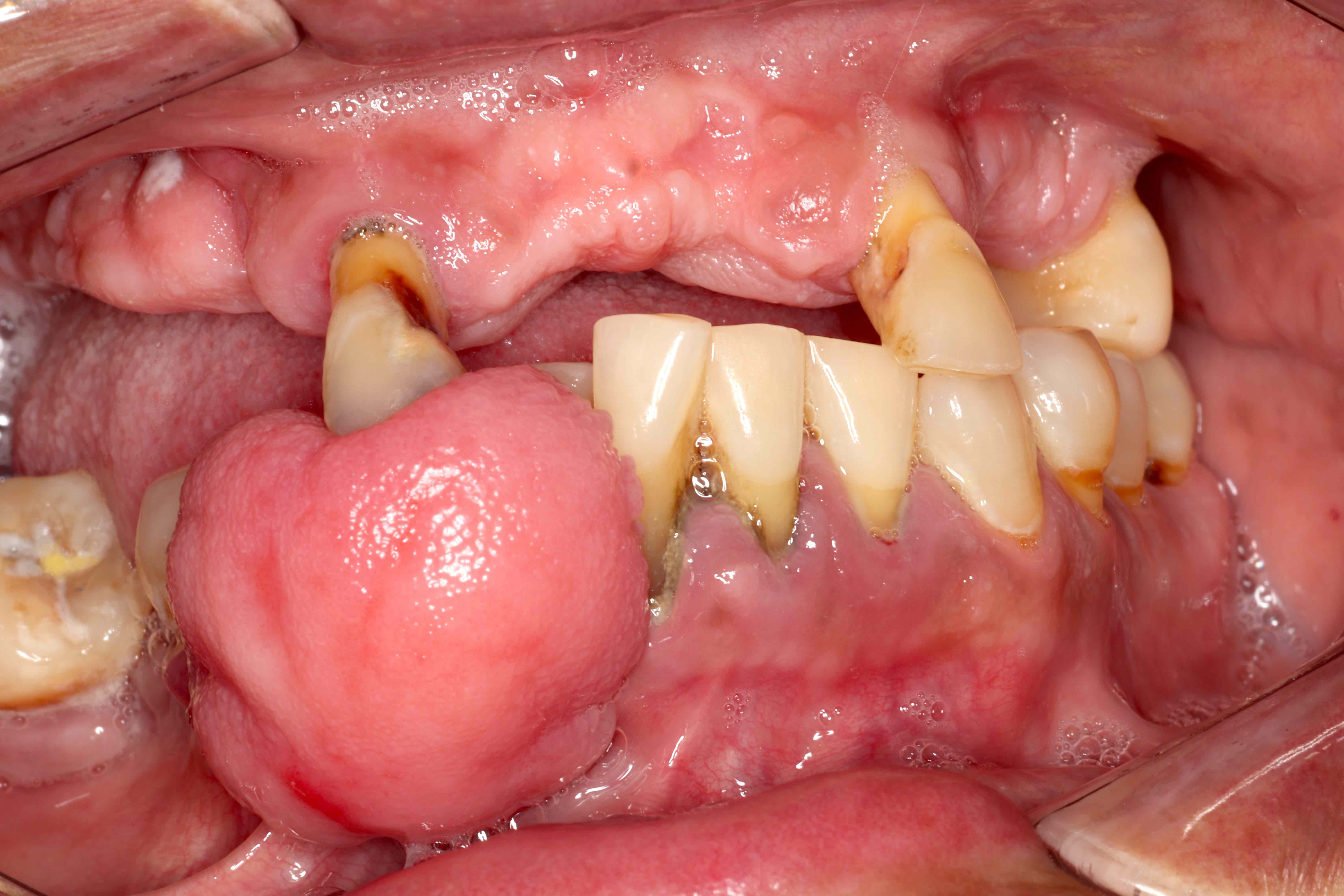
Clinical features
- Slow growing nodule with a mean time to presentation of 16 months (Med Oral Patol Oral Cir Bucal 2022;27:e460)
- Generally painless or causing mild discomfort (J Indian Soc Periodontol 2015;19:83)
- May ulcerate (Oral Surg Oral Med Oral Pathol 1987;63:452)
- Indolent clinical course but in some cases, the size and location may interfere with normal oral function, displace teeth and distort local anatomy (Int J Surg Case Rep 2021;84:106127, Ann Maxillofac Surg 2016;6:300, Head Neck Pathol 2013;7:356)
- Recurrence in ~15% despite surgical excision (Oral Surg Oral Med Oral Pathol 1987;63:452, Br J Oral Maxillofac Surg 2019;57:1081, J Indian Soc Periodontol 2015;19:83)
- Multifocal disease is rare (Indian J Dent Res 2014;25:220)
Diagnosis
- Difficult to distinguish clinically from other entities (pyogenic granuloma, oral irritation fibroma, giant cell fibroma, peripheral giant cell granuloma, metastatic lesions)
- Readily diagnosed histologically with high interobserver concordance (Med Oral Patol Oral Cir Bucal 2022;27:e460)
Radiology description
- May show irregular radiopacity due to calcification / ossification or show mild alveolar bone resorption (Dentomaxillofac Radiol 2007;36:180, Med Oral Patol Oral Cir Bucal 2022;27:e460, Head Neck Pathol 2013;7:356)
Prognostic factors
- Benign but may recur
- Recurrence is more likely if offending irritant is not removed (J Indian Soc Periodontol 2015;19:83)
Case reports
- 2 month old girl with peripheral ossifying fibroma (Oral Surg Oral Med Oral Pathol Oral Radiol 2020;130:e74)
- 24 year old man with multifocal disease (Indian J Dent Res 2014;25:220)
- 25 year old woman with 4 cm tumor interfering with oral function (Int J Surg Case Rep 2021;84:106127)
Treatment
- Surgical excision (J Indian Soc Periodontol 2015;19:83)
- Removal of irritants including plaque / calculus or poorly fitted prosthetics (J Indian Soc Periodontol 2015;19:83)
Clinical images
Gross description
- Exophytic mass that may be sessile or pedunculated (Med Oral Patol Oral Cir Bucal 2022;27:e460, J Indian Soc Periodontol 2015;19:83)
- Mean size of < 2 cm but sizes up to 10 cm have been reported (Med Oral Patol Oral Cir Bucal 2022;27:e460, J Indian Soc Periodontol 2015;19:83, Ann Maxillofac Surg 2016;6:300)
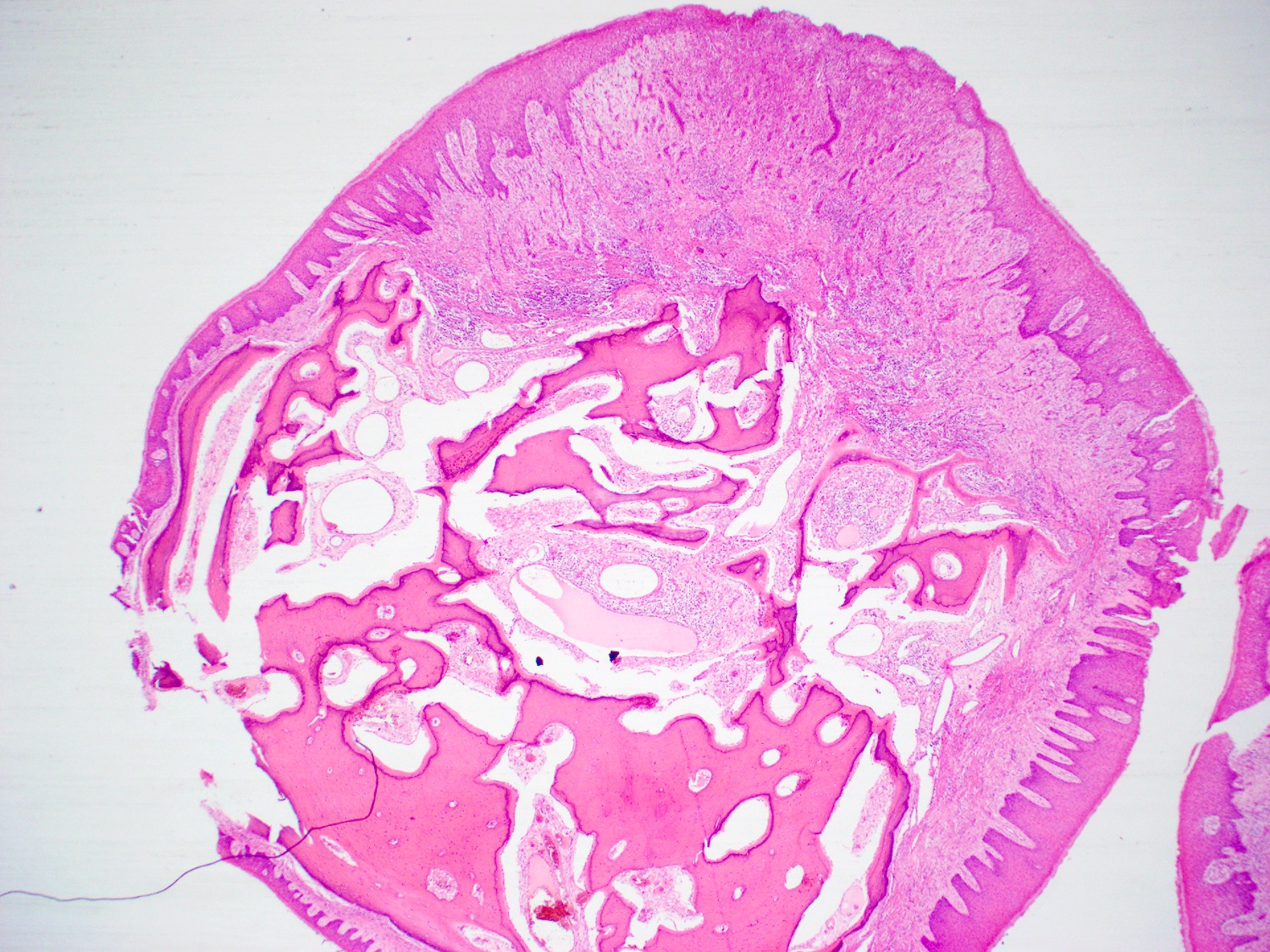
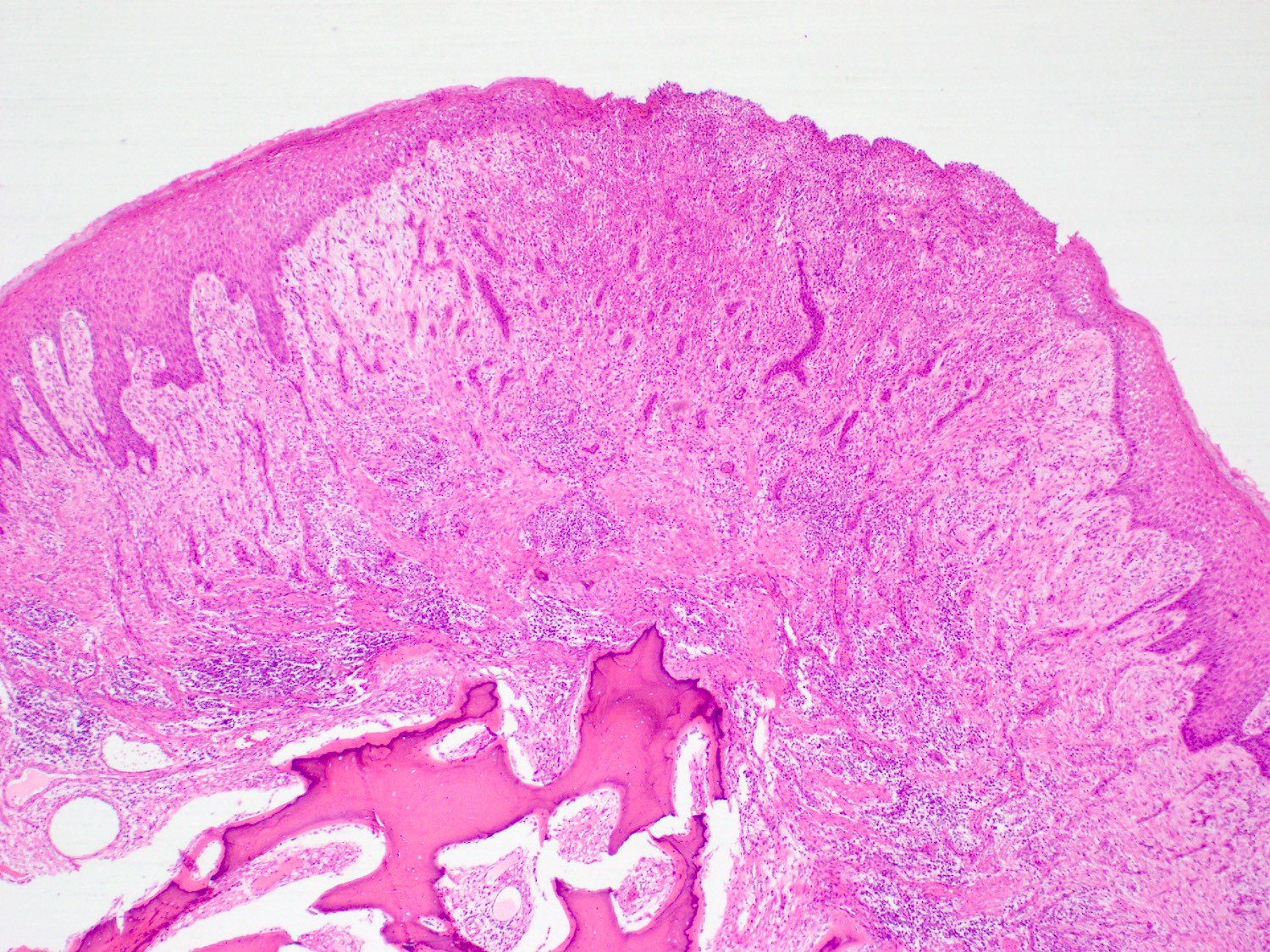
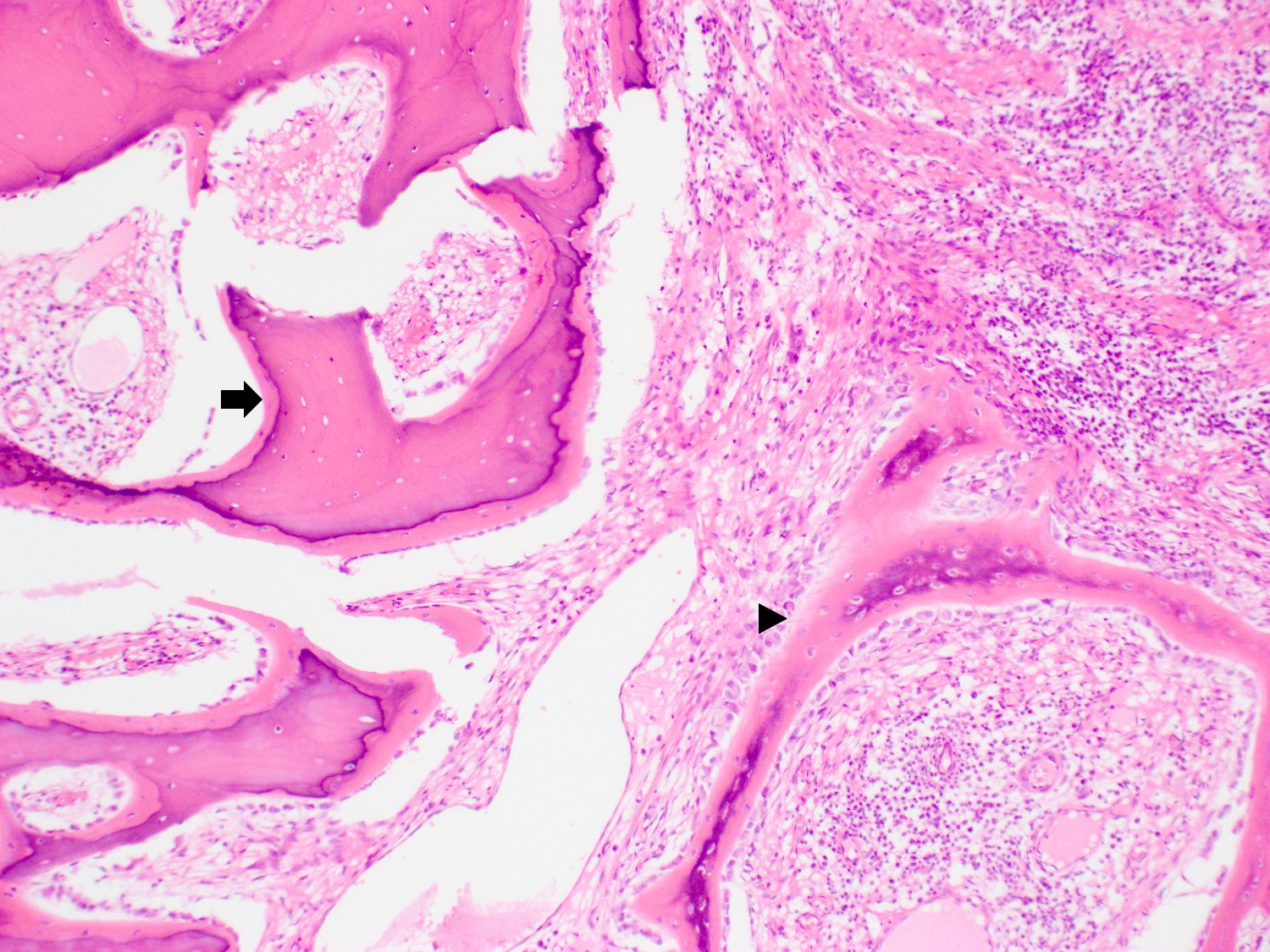
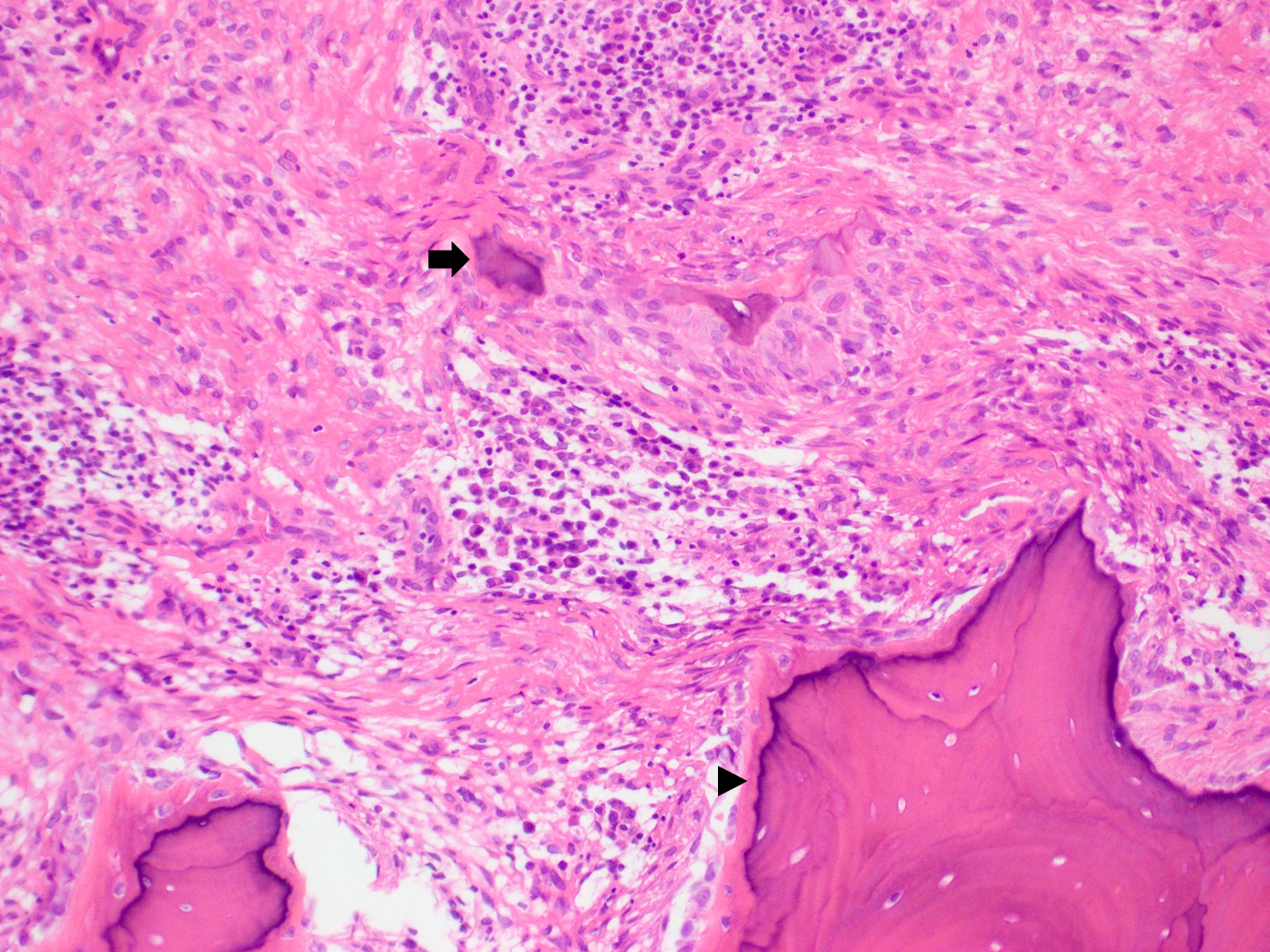
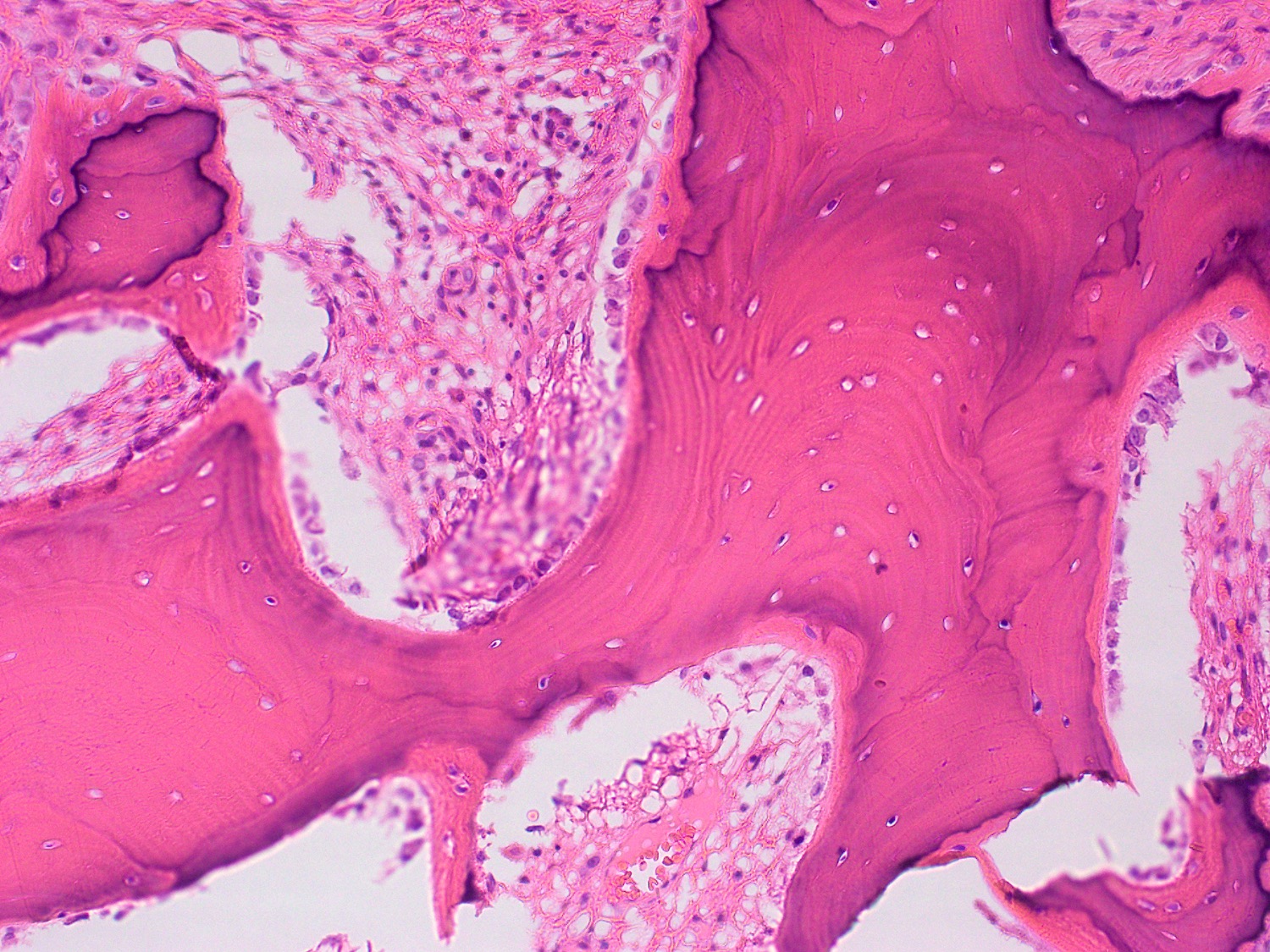
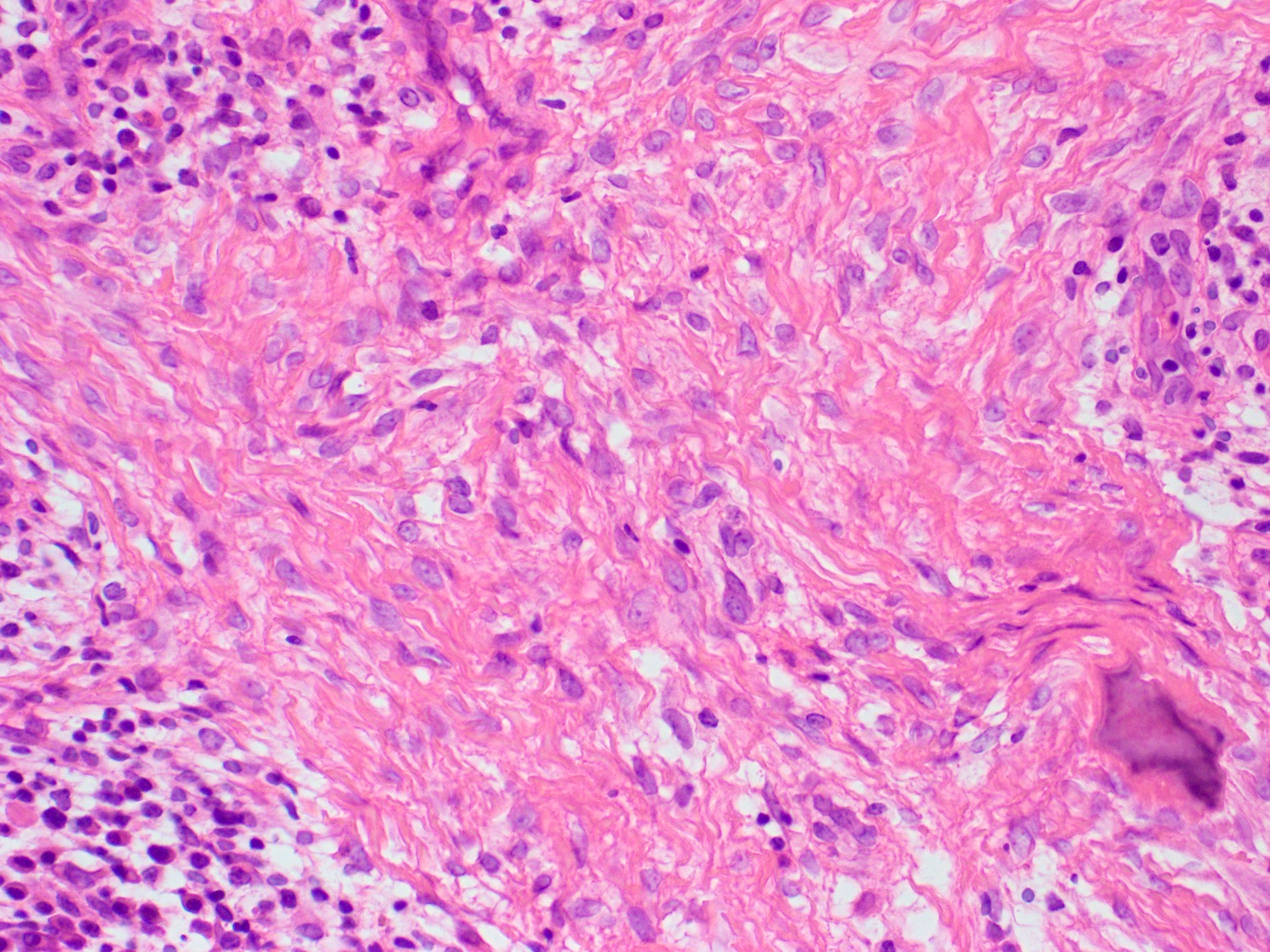
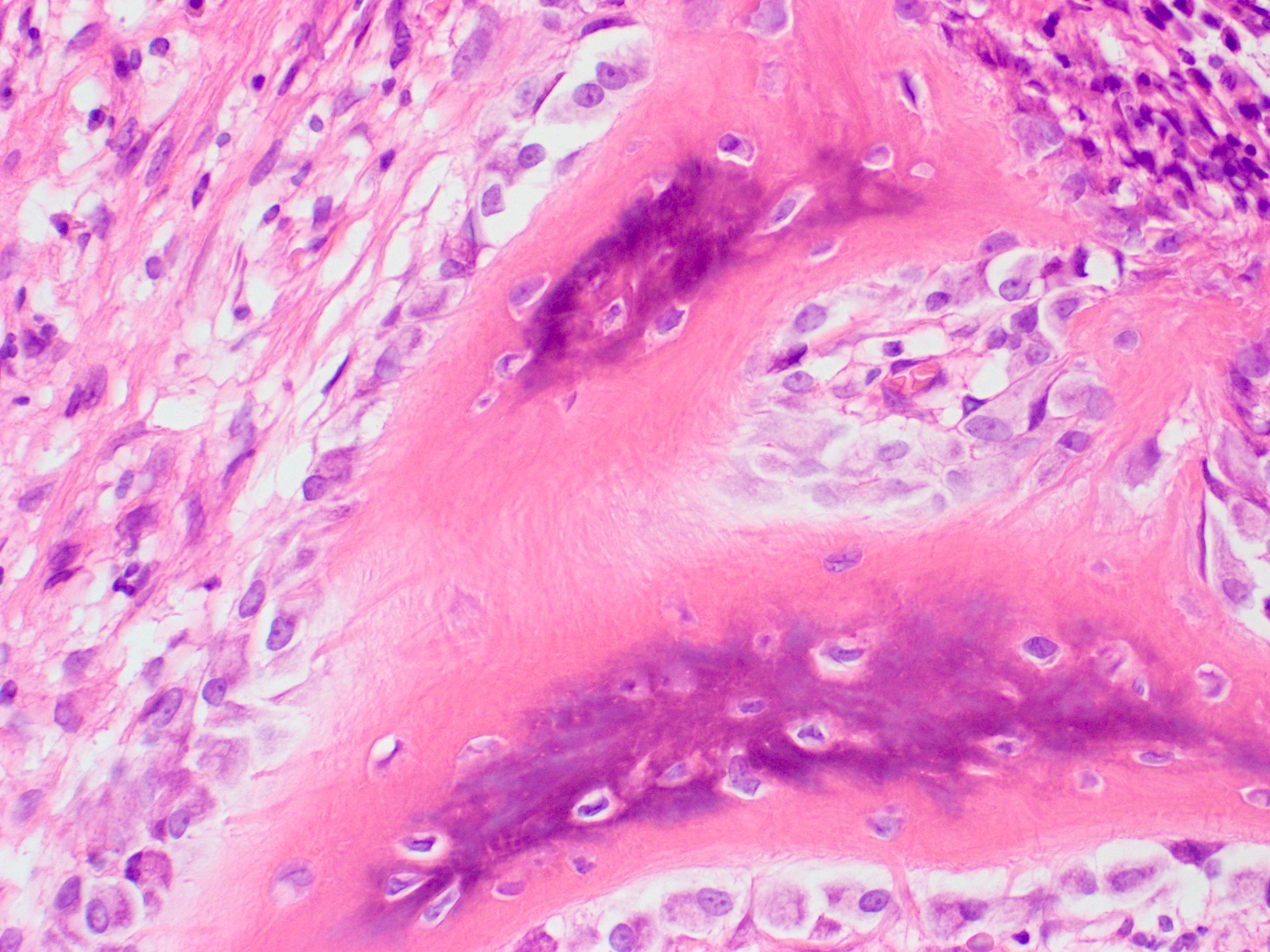
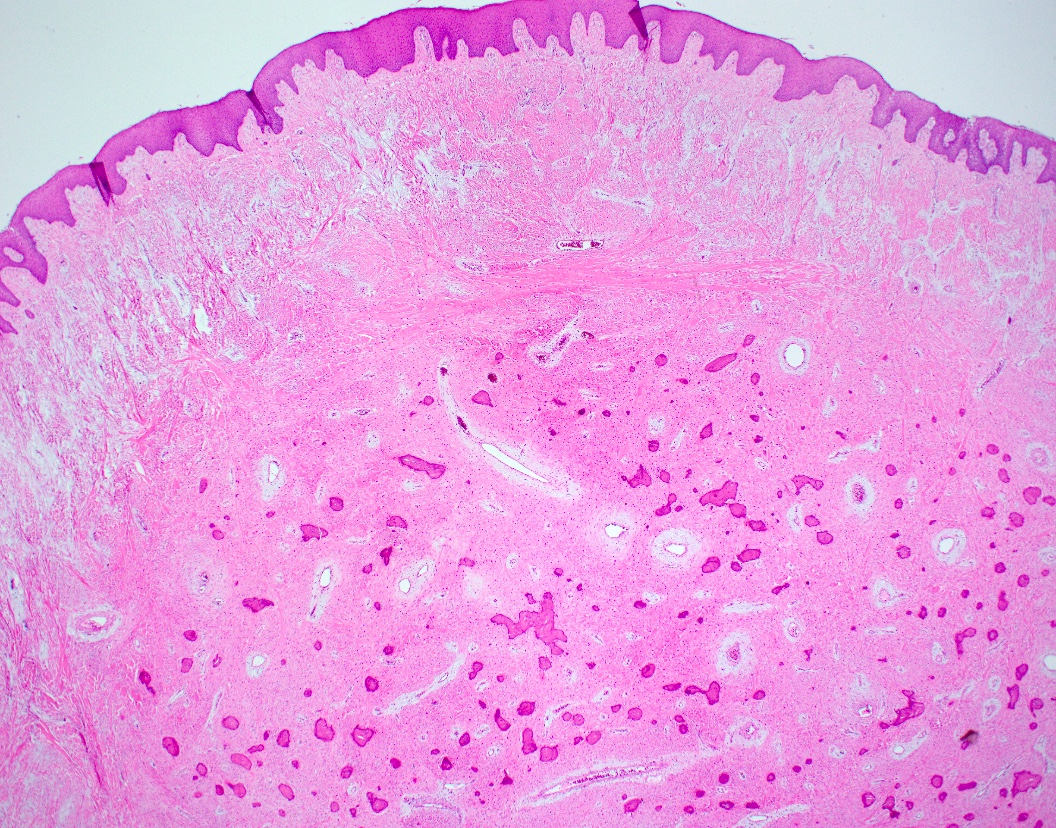
Microscopic (histologic) description
- Variably cellular fibroblastic spindle cell proliferation in subepithelial connective tissue in variably collagenous background (J Indian Soc Periodontol 2015;19:83)
- Collagen deposition is more prominent in the deep aspect (J Indian Soc Periodontol 2015;19:83)
- Dystrophic calcification, lamellar or woven bone formation is essential for diagnosis (J Indian Soc Periodontol 2015;19:83)
- Overlying hyperplastic epithelium with hyperkeratosis (J Indian Soc Periodontol 2015;19:83)
- Surface epithelium may be ulcerated (J Indian Soc Periodontol 2015;19:83, Oral Surg Oral Med Oral Pathol 1987;63:452)
- Background contains variable chronic inflammatory infiltrate, predominantly lymphoplasmacytic and proliferating small capillary sized vessels (J Indian Soc Periodontol 2015;19:83, Med Oral Patol Oral Cir Bucal 2022;27:e460)
Microscopic (histologic) images
Contributed by Timothy Fielder, M.B.B.S., B.Med.Sci., Ruta Gupta, M.D. and Molly Housley Smith, D.M.D.
Positive stains
- Not used in routine diagnosis
- SMA in 73% (Br J Oral Maxillofac Surg 2019;57:1081)
- CD68 in 54% (Br J Oral Maxillofac Surg 2019;57:1081)
- SATB2 in 100% (Head Neck Pathol 2022;16:339, Ann Diagn Pathol 2020;46:151510)
- Positive for osteoblastic / cementoblastic proteins RUNX2, BMP2, CAP in one study and osterix (OSX) in another (J Oral Pathol Med 2015;44:628, Braz Oral Res 2017;31:e53)
Negative stains
Sample pathology report
- Gingiva, excision:
- Peripheral ossifying fibroma (see comment)
- Comment: Sections include oral squamous mucosa with underlying connective tissues and show features of a peripheral ossifying fibroma. The mucosa shows focal ulceration with organizing granulation tissue. The submucosal tissues show a well demarcated but unencapsulated lesion composed of areas of fibrosis and metaplastic ossification. There is no dysplasia or malignancy.
Differential diagnosis
- Oral irritation fibroma:
- Clinically difficult to distinguish
- Histologically lacks calcification or bone formation
- Peripheral giant cell granuloma:
- Clinically difficult to distinguish
- Stromal multinucleated giant cells are seen on histology
- Pyogenic granuloma:
- Clinically difficult to distinguish
- Lobulated vascular proliferation on histology
- Giant cell fibroma:
- Clinically difficult to distinguish
- Lacks bone formation
Board review style question #1
Which of the following is true regarding peripheral ossifying fibroma?
- It is a reactive gingival proliferation thought to occur in response to irritation or trauma
- It is histologically characterized by lobulated growth of capillary sized vessels with a central feeder vessel
- It is molecularly characterized by recurrent internal tandem duplication of BCOR
- It is most common in males over 50
Board review style answer #1
A. It is a reactive gingival proliferation thought to occur in response to irritation or trauma
Comment Here
Reference: Peripheral ossifying fibroma
Comment Here
Reference: Peripheral ossifying fibroma
Board review style question #2
Board review style answer #2