Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Xu B. Invasive fungal rhinosinusitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/nasalmucor.html. Accessed April 26th, 2024.
Definition / general
- Acute aggressive life threatening invasive fungal infection involving sinonasal tract and adjacent organs (such as orbit or brain); the mortality rate is ~50% (Laryngoscope 2013;123:1112)
Essential features
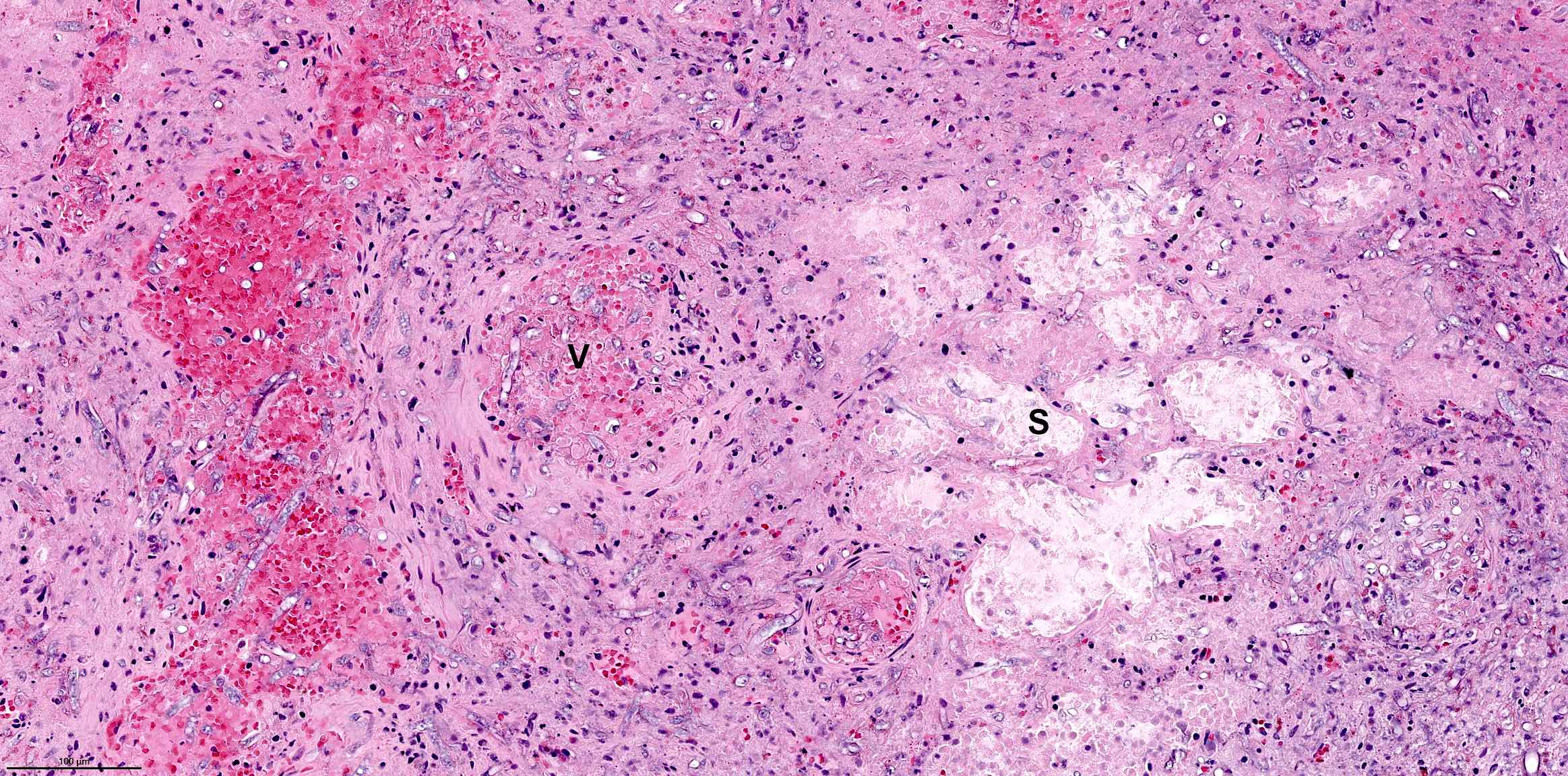
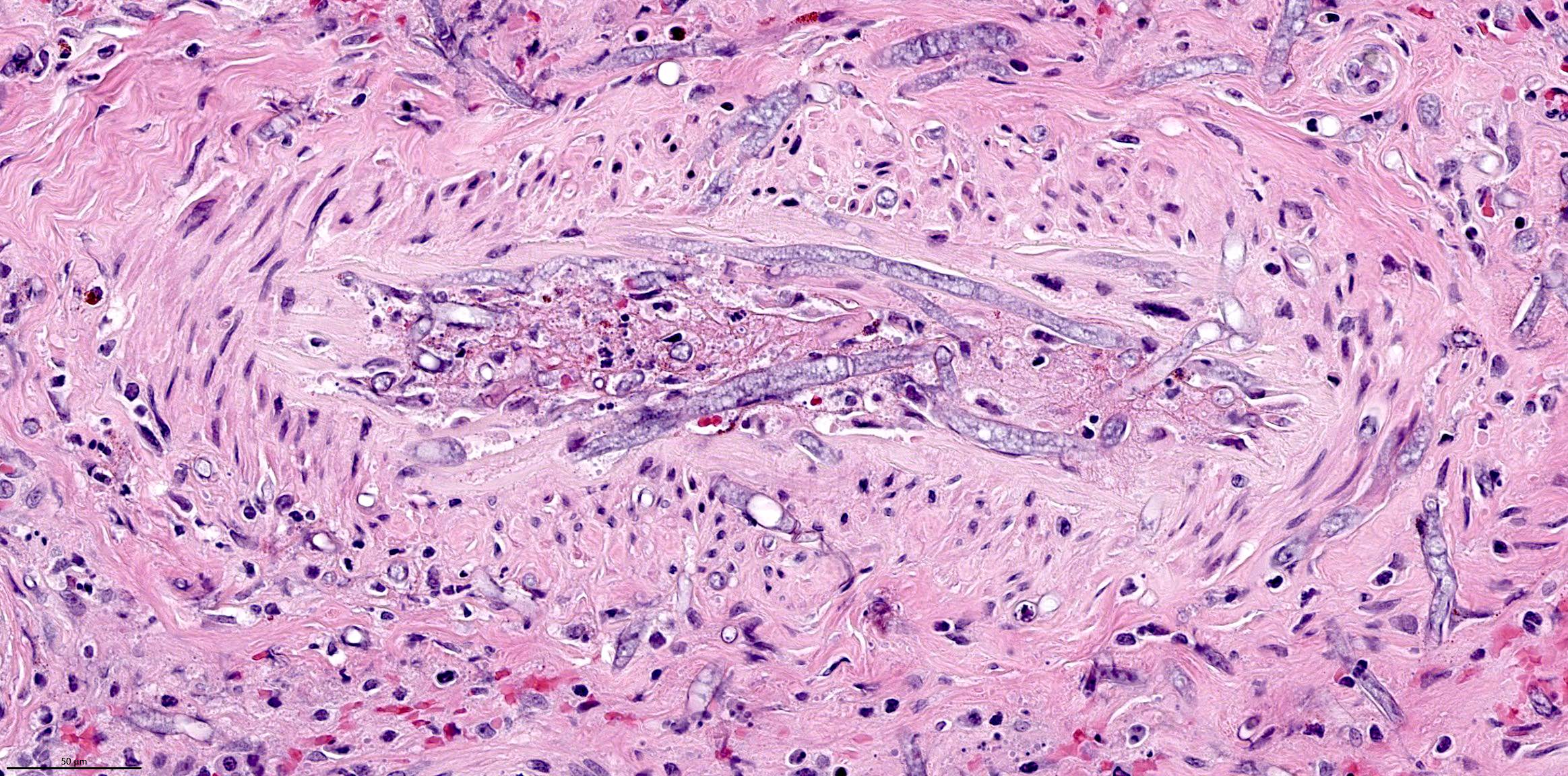
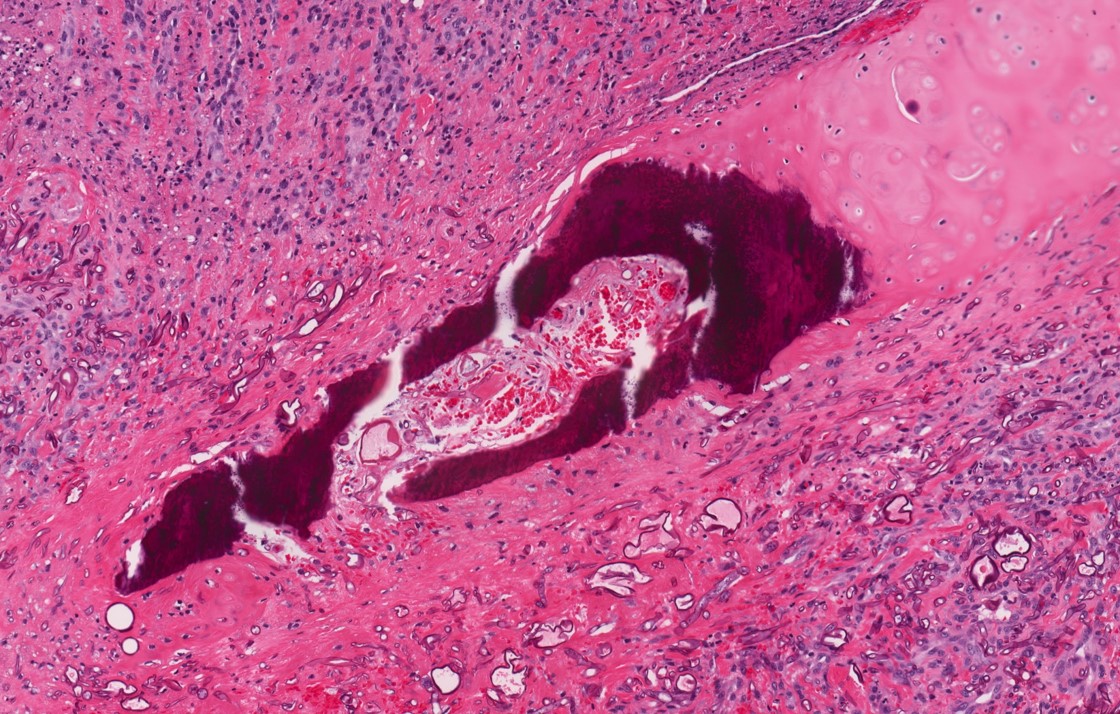
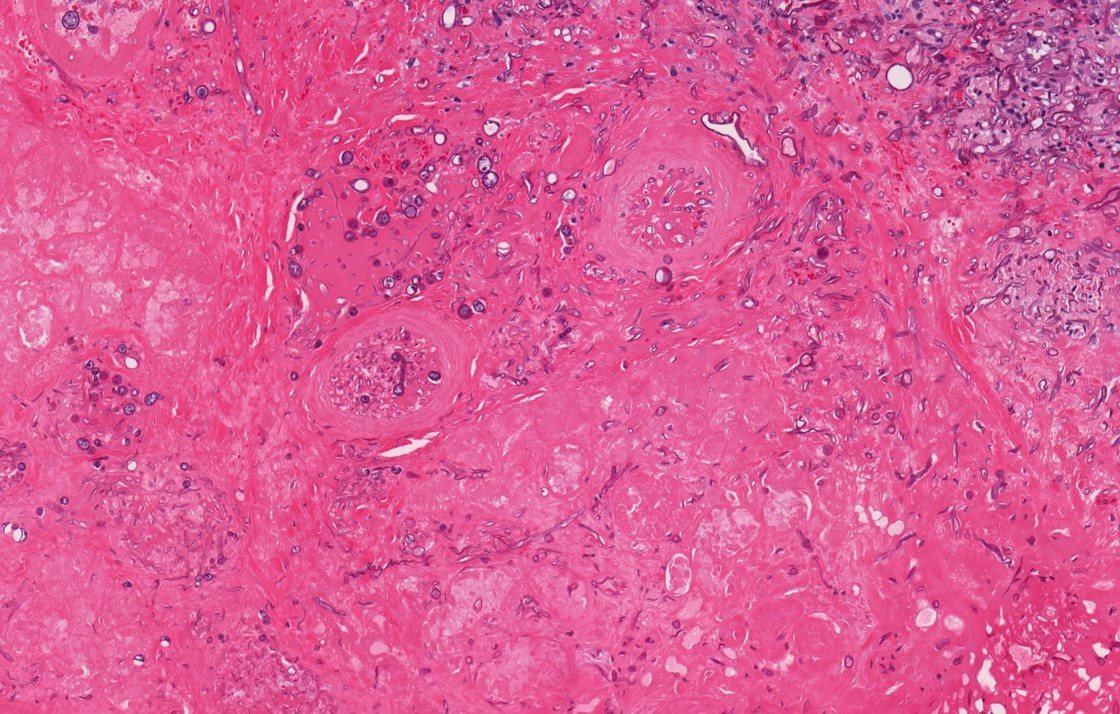
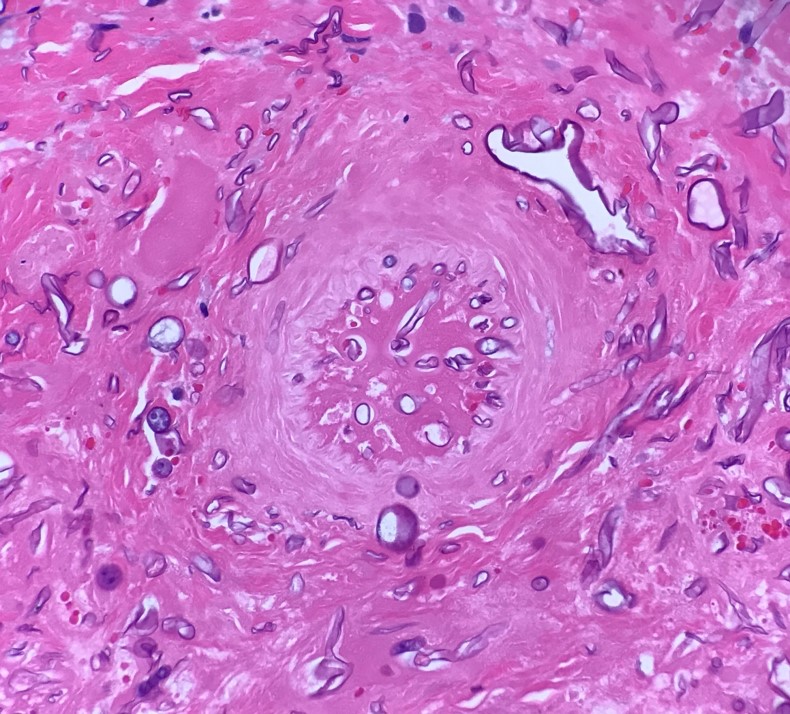
- Definite diagnosis is made on biopsy by identifying the essential histologic feature, which is invasion of tissue and vessels by fungal organisms, often associated with tissue necrosis and infarction
- Mostly occurs in immunocompromised hosts, although immunocompetent patients may also be affected (Laryngoscope 2013;123:1112, Radiographics 2022;42:2075)
- Caused by a diverse group of fungal organisms, most commonly Zygomycetes (such as Mucor and Rhizopus) and Aspergillus (Laryngoscope 2013;123:1112, Radiographics 2022;42:2075)
- 1 of the 3 pathologic manifestations of fungi in the sinonasal tract; the other 2 are allergic fungal sinusitis and mycetoma (fungus ball)
Terminology
- Acute invasive fungal (rhino)sinusitis
- Angioinvasive fungal (rhino)sinusitis
ICD coding
Epidemiology
- Mostly occurs in immunocompromised patients
- Underlying risk factors in a descending order of frequency include (Laryngoscope 2013;123:1112)
- Diabetes (in ~50%), including those with ketoacidosis
- Hematologic malignancy (in ~40%), such as acute lymphoblastic leukemia and acute myeloid leukemia
- Corticosteroid medication
- Renal / liver failure
- Organ transplant (solid organ or allogeneic stem cell transplant)
- HIV / AIDS
- Anaplastic anemia
- Autoimmune disease
- May occur in pediatric patients (J Pediatric Infect Dis Soc 2017;6:S22, Int J Pediatr Otorhinolaryngol 2016;90:231)
Sites
- Sinonasal tract
- Adjacent vital organs, including orbit (in ~50%), intracranial and hard palate (in ~20%) and cavernous sinus (in 9%) (Laryngoscope 2013;123:1112)
Etiology
- Immunocompromised host
- Caused by hyphae form fungi, commonly Zygomycetes (such as Rhizopus and Mucor) and Aspergillus
- Coinfection with COVID-19 and post-COVID-19 infection were reported during COVID-19 pandemic (Laryngoscope Investig Otolaryngol 2022;7:913)
Clinical features
- Most common symptoms presenting in > 50% of patients include facial swelling, fever, nasal congestion and ophthalomoplegia (Laryngoscope 2013;123:1112)
- Other symptoms include proptosis, vision loss, nasal discharge, facial pain, headache, cranial nerve palsy, altered mental status and palatal necrosis / ulcer
Diagnosis
- Diagnosis of invasive fungal rhinosinusitis is rendered on tissue biopsy by identification of fungal hyphae in tissue (such as mucosa, submucosa, bone or vessels)
- Tissue culture is recommended for genus of the fungi and antifungal susceptibility testing (Lancet Infect Dis 2019;19:e405, Clin Infect Dis 2016;63:e1)
- In situ hybridization and RT-PCR for various fungi can be used in formalin fixed tissue for genus of the fungi
Radiology description
- Mucosal thickening
- Soft tissue invasion into adjacent tissue / organ(s), such as orbit and intracranial extension
Radiology images
Prognostic factors
- Unfavorable prognostic factors include older age, altered mental status, underlying conditions of anaplastic anemia or renal / liver failure, intracranial or cavernous sinus involvement, neutropenia and treatment delay (Laryngoscope 2013;123:1112, Otolaryngol Head Neck Surg 2018;159:386)
- Favorable prognostic factors are surgery and liposomal amphotericin B antifungal therapy
Case reports
- 27 year old woman with acute lymphoblastic leukemia developed rhinosinusitis after induction chemotherapy (Clin Hematol Int 2022;4:60)
- 29 year old man post-bone marrow transplant with psychosis and a gingival lesion (Arch Pathol Lab Med 2000;124:883)
- 33 year old male intranasal cocaine user presented with facial and nasal pain and was found to have invasive Aspergillus flavus sinusitis (IDCases 2021;26:e01327)
- 36 year old woman, 45 year old woman and 62 year old man with acute invasive fungal sinusitis associated with COVID-19 infection (Indian J Otolaryngol Head Neck Surg 2022;74:3359)
Treatment
- Combination of surgery and antifungal treatment (Laryngoscope 2013;123:1112)
- Surgery can be performed via endoscopic or open approach
- The most common antifungal treatment is amphotericin B
- Correcting the source of immunosuppression may also be useful
Gross description
- Necrotic and hemorrhagic tissue fragments
Frozen section description
- Fungal hyphae in tissue are diagnostic for invasive fungal sinusitis on frozen sections
- Free floating fungal elements with or without mucus, blood, debris or fibrin are insufficient to confirm the invasive nature of the fungi and are therefore insufficient for the diagnosis
Microscopic (histologic) description
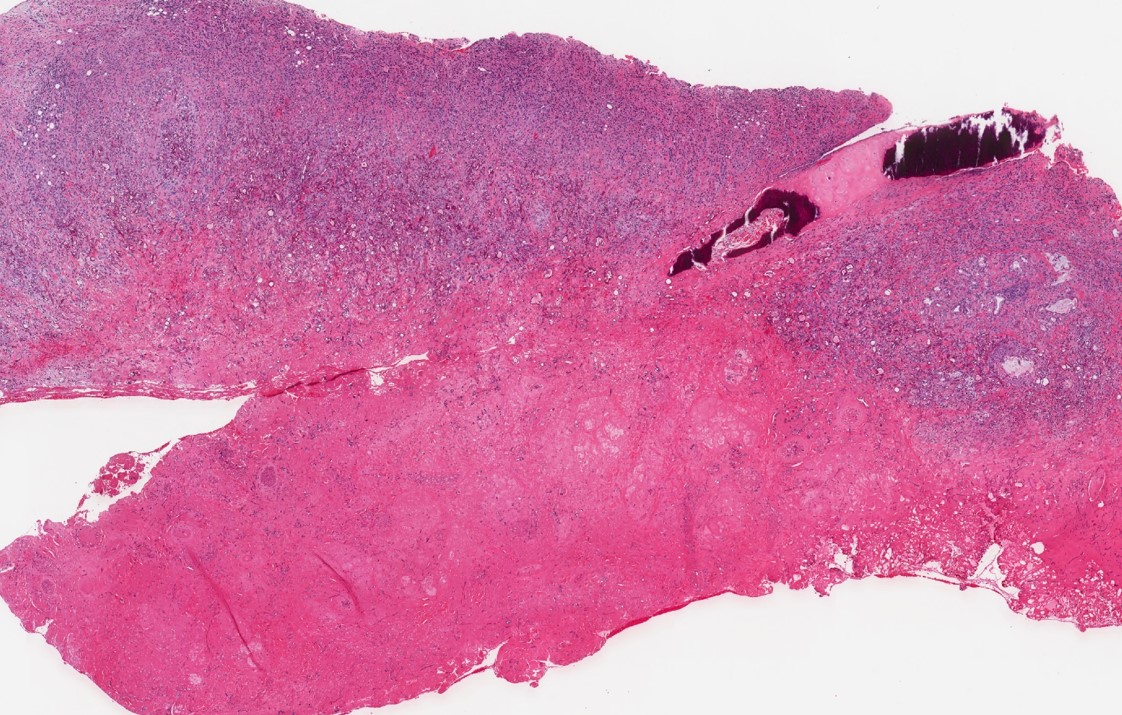
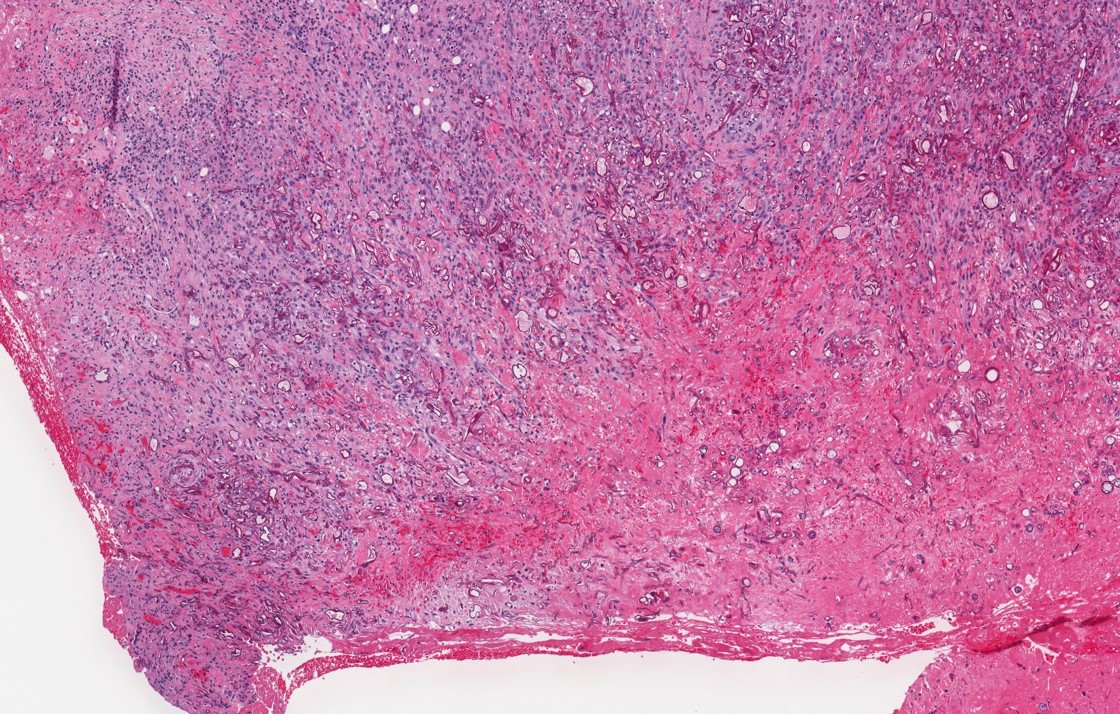
- Fungal hyphae in mucosa, submucosa, vessels and bone
- Zygomycetes: broad nonseptate hyphae branching at 90 degrees
- Aspergillus: slender septate hyphae branching at 45 degrees
- Preoperative antifungal treatment may significantly alter the morphology of the hyphae
- Classification of the fungal genus is not reliable on histology: tissue fungal culture or RT-PCR test using paraffin blocks are more reliable tools
- Often associated with tissue necrosis, acute inflammation, ulceration or granulation tissue
- Grocott-Gomori methenamine silver (GMS) and periodic acid-Schiff (PAS) stains are useful special stains to highlight fungal organisms
Microscopic (histologic) images
Cytology description
- Cytology (such as nasal swab) can only detect the presence of fungal hyphae
- Invasive nature of the fungal elements cannot be established in cytologic samples
Sample pathology report
- Maxillary sinus, biopsy:
- Invasive and angioinvasive fungal rhinosinusitis associated with tissue necrosis, acute inflammation and ulceration (see comment)
- Comment: GMS and PAS stains highlight fungal hyphae.
Differential diagnosis
- Key differential diagnosis is noninvasive fungal infection of the sinonasal tract, including
- Allergic fungal sinusitis:
- Mycetoma (fungus ball):
- Mass forming growth of densely packed fungal hyphae in sinus cavity
- Tissue invasion by fungi is absent
Board review style question #1
Board review style answer #1
C. Invasive fungal sinusitis. The H&E shows invasive fungal infection with fungal hyphae in a blood vessel and fibrous tissue (i.e., invasive fungal sinusitis). Answers A and D are incorrect as both are noninvasive fungal diseases. Answer B is incorrect because the presence of fungal organisms excludes the diagnosis of granulomatosis with polyangiitis.
Comment Here
Reference: Invasive fungal rhinosinusitis
Comment Here
Reference: Invasive fungal rhinosinusitis
Board review style question #2
What is the most common causal fungal organism for invasive fungal sinusitis?
- Candida albicans
- Cryptococcus
- Histoplasma capsulatum
- Mucor
Board review style answer #2
D. Mucor. The most common causal fungal organisms for invasive fungal sinusitis are Zygomycetes (such as Mucor and Rhizopus) and Aspergillus. Answers A - C are incorrect because Cryptococcus, Histoplasma and Candida are all fungal organisms but are not the common cause for invasive fungal sinusitis.
Comment Here
Reference: Invasive fungal rhinosinusitis
Comment Here
Reference: Invasive fungal rhinosinusitis