Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Laboratory | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Molecular / cytogenetics description | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Totten AH, Farr GA, Leal SM. M. hominis / Ureaplasma spp.. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologymhominis.html. Accessed December 22nd, 2024.
Definition / general
- Atypical bacterial pathogens; stained poorly by the dyes used in Gram stain due to the absence of a cell wall
- Causative agents of urogenital syndromes and infections in transplant patients and neonates
- Taxonomy: class Mollicutes, order Mycoplasmatales, family Mycoplasmataceae
Essential features
- Requires specialized media conditions and does not stain with components of Gram stain
- Etiologic agents of urethritis, pelvic infection and some cases of infertility
- Cause extragenital infections in immunocompromised patients and neonates
Epidemiology
- M. hominis causes chorioamnionitis, urethritis in men and pelvic infection in females
- Ureaplasma urealyticum and Ureaplasma parvum cause chorioamnionitis, urethritis and female infertility
- All 3 species cause hyperammonemia syndrome in immunosuppressed patients (Sci Transl Med 2015;7:284re3)
- Predominantly affects sexually active 18 - 30 year olds but found in all age groups
- Spreads via sexual contact, vaginal birth or direct contact with mucosal surfaces
- Disseminated infections occur in immunocompromised individuals (Semin Fetal Neonatal Med 2009;14:190)
Sites
- M. hominis and Ureaplasma spp.:
- Frequently isolated from the lower urogenital tract of healthy men and women
- Ureaplasma spp. isolated from the vagina up to 50% of healthy women and M. hominis in less than 10% (Clin Microbiol Rev 2005;18:757)
- Colonization is linked to younger age, lower economic status, sexual activity with multiple partners and is greater among women during pregnancy
Pathophysiology
- Attachment proteins (adhesins) are debated in importance but implicated in infection
- Ureaplasma spp. produce IgA proteases and produce ammonia to alkalinize microenvironments (J Clin Microbiol 1984;19:255)
- M. hominis exhibits intrinsic resistance to macrolides
Clinical features
- Typically asymptomatic colonization of urogenital tract but can be disease causing
- Male and female urethritis / urinary calculi (Ureaplasma spp.)
- Female reproductive tract (M. hominis and Ureaplasma spp.)
- Chorioamnionitis / infertility (Semin Fetal Neonatal Med 2009;14:190)
- Adverse pregnancy outcomes, including preterm birth and miscarriage
- Bacterial vaginosis (M. hominis > Ureaplasma spp.)
- Pelvic inflammatory disease which may be multibacterial (M. hominis)
- Neonatal infection (intrauterine) (Semin Fetal Neonatal Med 2009;14:190)
- Chorioamnionitis / bronchopulmonary dysplasia
- Fever / congenital pneumonia
- Meningoencephalitis
- Disseminated infection
- Hyperammonemia syndrome in immunocompromised (transplant) patients (Ann Thorac Surg 2017;103:670)
- Pulmonary / respiratory / nasopharyngeal infections
- Septic arthritis
- Meningitis
Laboratory
- Does not stain on a Gram stain due to the lack of a cell wall
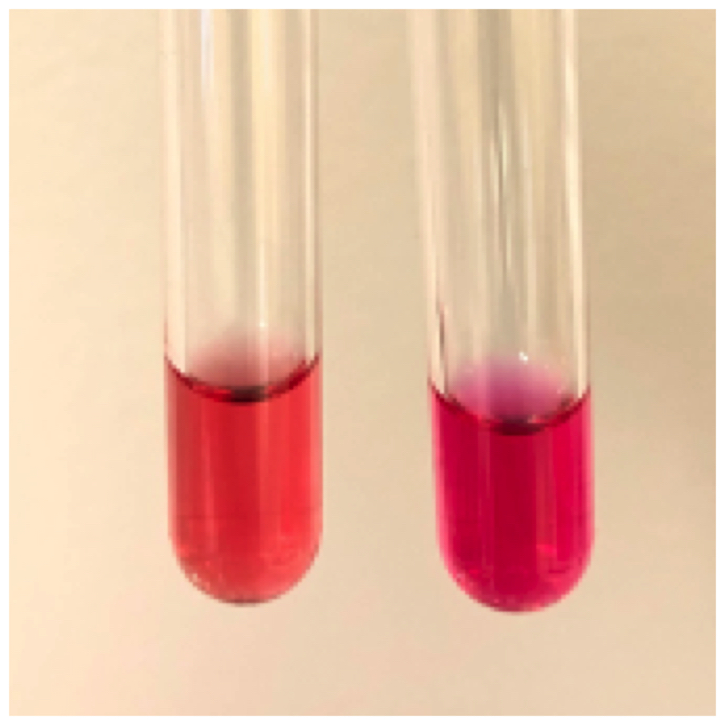
- M. hominis will grow on standard microbiology media (J Clin Microbiol 2012;50:3542)
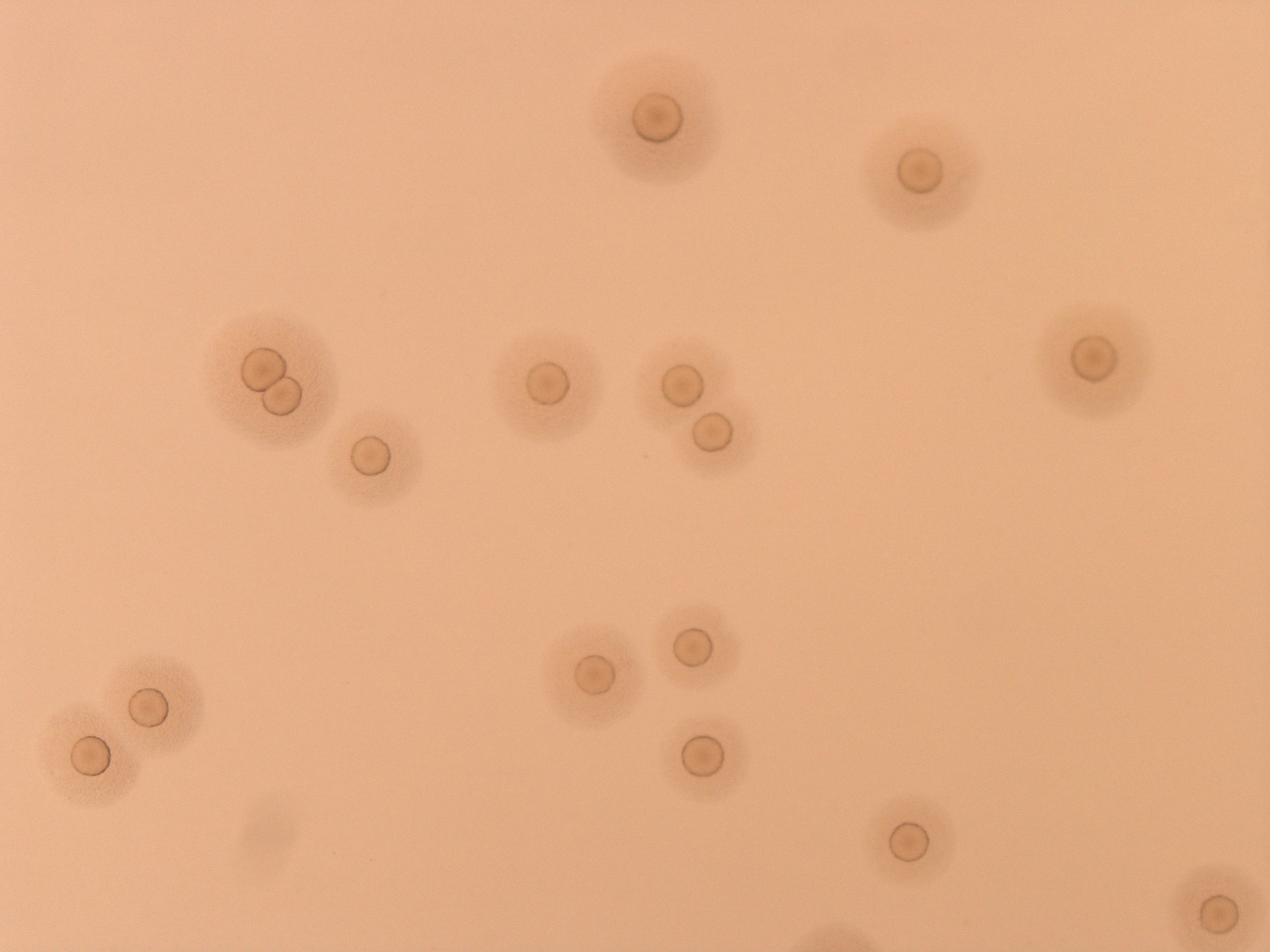
- Small, fried egg colonies (dissection scope needed) on SP4 or A8 agar within 2 - 4 days; aerobically at 37°C
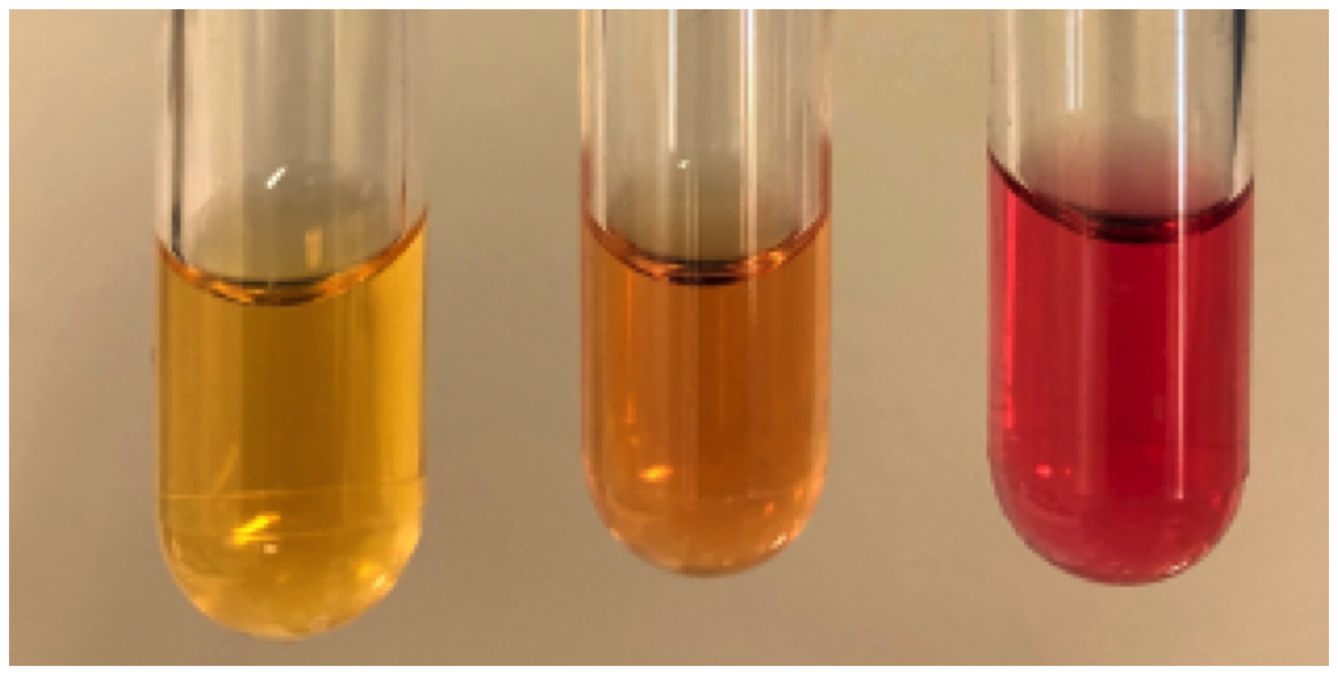
- Ureaplasma species do not grow on standard media (J Clin Microbiol 2012;50:3542)
- Small, punctate colonies (dissection scope needed) on A8 agar within 2 - 5 days; aerobically at 37°C
- Nucleic acid amplification test (NAAT) required to differentiate Ureaplasma species
Case reports
- 11 day old neonate with meningoencephalitis caused by M. hominis infection (Lancet Infect Dis 2016;16:e261)
- 32 and 49 year old women with fatal hyperammonemia syndrome following lung transplantation and subsequent infection with M. hominis and Ureaplasma urealyticum (Open Forum Infect Dis 2019;6:ofz033)
- 35 year old man with oropharyngeal U. urealyticum infection and coinfection with HIV, HPV and Treponema pallidum (JMM Case Rep 2018;5:e005132)
- 62 year old man with M. hominis infection after total knee replacement (Chin J Traumatol 2017;20:243)
- Report of 5 cases of post transplant infections with Ureaplasma and M. hominis (Transpl Infect Dis 2018;20:e12937)
Treatment
- M. hominis: quinolones, tetracyclines and clindamycin (Carroll: Manual of Clinical Microbiology, 12th Edition, 2019)
- Resistance: quinolone (~ 10%), tetracycline (< 5%), macrolide (100%)
- Ureaplasma species: macrolides or tetracyclines
- Resistance: quinolone (~ 5%), tetracycline (8%), macrolide (< 5%)
Clinical images
Microscopic (histologic) description
- Not known
- Organism not seen on H&E; expect a chronic inflammatory response
Molecular / cytogenetics description
- FDA approved diagnostic tests are not available
- Laboratory developed nucleic acid amplification tests (NAAT) for M. hominis and Ureaplasma species have been published:
- Urease gene for Ureaplasma spp. (J Clin Microbiol 1998;36:3211)
- Multibanded antigen, MBA gene for Ureaplasma spp. (Diagn Microbiol Infect Dis 2007;57:373)
- Gap gene (BMC Microbiol 2004;4:35)
- RpoB gene for M. hominis (J Mol Diagn 2012;14:437)
- Detection by multiplex assay NAAT like ELITech InGenius
Differential diagnosis
- Neisseria gonorrhea:
- Gram negative diplococci, oxidase positive; NAAT recommended
- Chlamydia trachomatis:
Board review style question #1
- A 78 year old man is experiencing confusion and lethargy with elevated ammonia levels two weeks after lung transplant. Blood cultures, microbiology tests and liver function tests appear normal. Which organism may be contributing to the hyperammonemia?
- Human papillomavirus
- Mycoplasma fermentans
- Neisseria meningitidis
- Ureaplasma urealyticum
Board review style answer #1
D. Ureaplasma urealyticum is associated with hyperammonemia due to cleavage of urea and production of ammonia. M. fermentans, HPV and N. meningitidis do not cleave urea and are not associated with this syndrome.
Comment Here
Reference: M. hominis / Ureaplasma spp.
Comment Here
Reference: M. hominis / Ureaplasma spp.
Board review style question #2
- Pure isolation of pinpoint colonies on sheep blood agar were seen 48 hours after planting joint fluid on sheep blood agar. After picking a colony and performing a Gram stain, the technologists did not see any organism on the slide so she repeated the procedure with the same result. Which organism is most likely the causative agent of this patient’s joint infection?
- Mycoplasma genitalium
- Mycoplasma hominis
- Mycoplasma pneumoniae
- Mycoplasma synoviae
Board review style answer #2
B. Mycoplasma hominis is the only known Mycoplasma species causing infection in humans that grows rapidly on standard microbiology media. M. pneumoniae and M. genitalium require longer incubation and special media. M. synoviae is a poultry pathogen that does not cause human disease.
Comment Here
Reference: M. hominis / Ureaplasma spp.
Comment Here
Reference: M. hominis / Ureaplasma spp.