Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross images | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Differential diagnosis | Additional referencesCite this page: Martinez A. Clear cell odontogenic carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxillaclearcellodontogenic.html. Accessed April 18th, 2024.
Definition / general
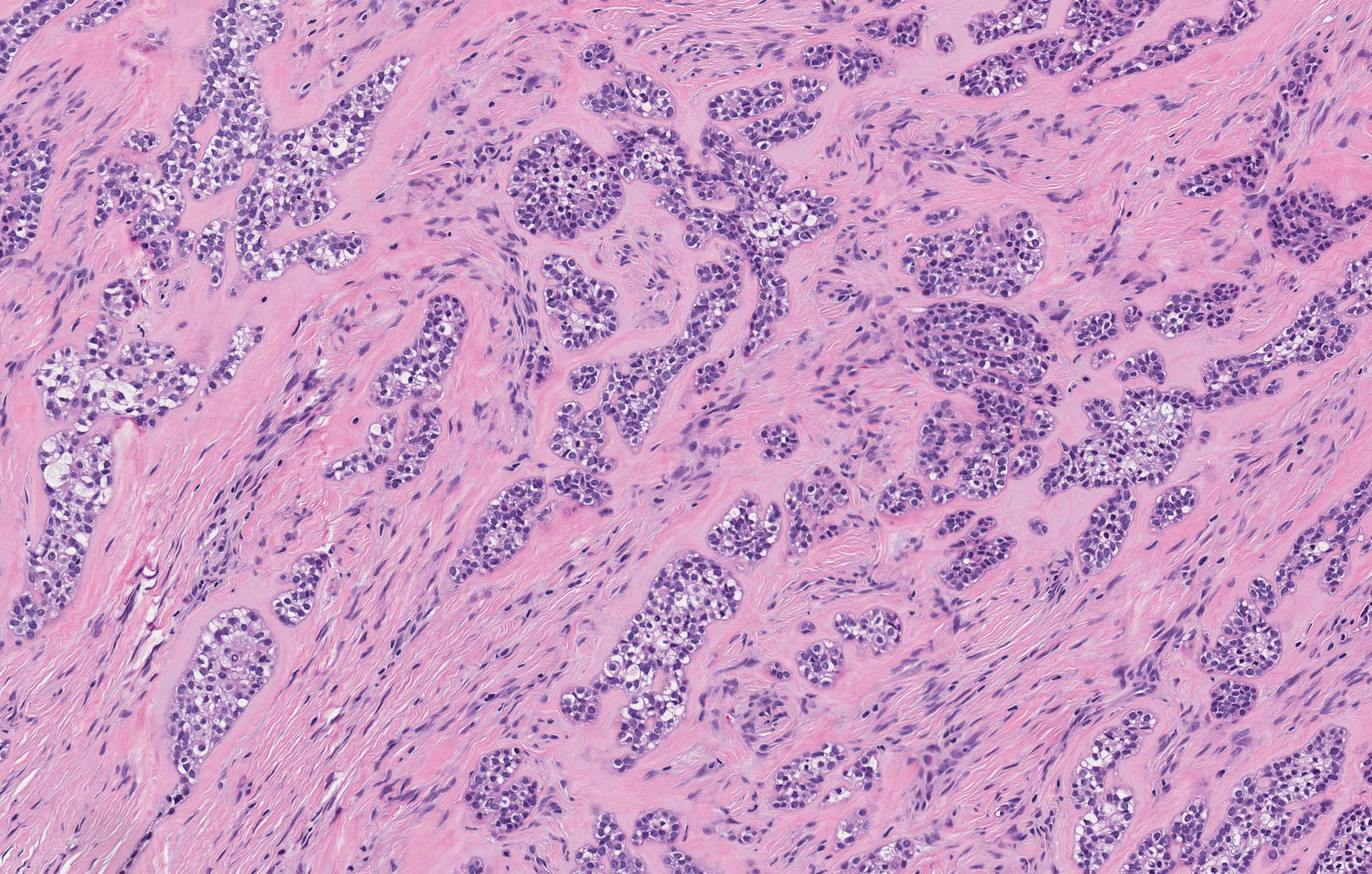
- Rare, malignant, translocation associated odontogenic epithelial neoplasm composed of nest of clear cells and fibrous, hyalinized stroma
- EWSR1 rearrangements found in > 80% of cases (Am J Surg Pathol 2013;37:1001)
Terminology
- Clear cell odontogenic carcinoma (CCOC), clear cell odontogenic tumor
- Previously called clear cell ameloblastoma
- Considered benign by WHO of 1992, but due to its high potential for regional spread and distant metastases, it was reclassified as malignant in 2005
Epidemiology
- Rare, < 100 cases reported
- Most common in 5th to 6th decades
- Mean age ~ 60 years
- More common in females (1.5:1 to 2:1)
- First described in 1980's as jaw tumors that resembled metastatic clear cell renal carcinoma (Head Neck Surg 1985;8:115)
Sites
- Mandible most common site (75%)
- Soft tissue involvement common as lesion often perforates bone
Etiology
- Unknown, as with many translocation tumors, lesion tends to pursue a line of differentiation rather than originate from a particular line of derivation
- However, the tumor cells resemble clear cell rests of primitive dental lamina that are frequently in the same locations
Clinical features
- Often presents as jaw swelling with loosening of the teeth
- Can be painful, asymptomatic or associated with paresthesias
Diagnosis
- Diagnosis dependent on clinical, radiologic and pathologic correlation
Radiology description
- Poorly defined radiolucency
- May show cortical destruction of bone
Prognostic factors
- Recurrence rate of 30% of resected and 87% of curetted/enucleated lesions
- Metastases to lymph nodes, lung and bone
- Up to 25% die of disease
Case reports
- 46 year old with swelling in lower front tooth region for 4–5 months (Contemp Clin Dent 2015; 6: 559)
- 50 year old woman with involvement of mandible and temporomandibuar joint and cervical nodal metastases (Natl J Maxillofac Surg 2014;5:221)
- 55 year old woman with tumor extending from canine to molar region (J Oral Maxillofac Pathol 2013;17:89)
- 64 year old man with CCOC in anterior mandibular region (J Oral Maxillofac Pathol 2014;18:442)
Treatment
- Must tailor surgical treatment to overall clinical and image findings, but often involves a composite / en bloc resection
Clinical images
Microscopic (histologic) images
Positive stains
Negative stains
- S100, SOX10, HMB45, SMA, Mucicarmine, Alcian blue, Congo red
Molecular / cytogenetics description
- > 80% show EWSR1-ATF1 translocations (Am J Surg Pathol 2013;37:1001)
Differential diagnosis
- May vary based on biopsy sample size and whether histology is monophasic (predominantly clear cell), biphasic or ameloblastomatous:
Monophasic (predominantly clear cell) or focal biphasic appearance:
Ameloblastomatous appearance:
- Clear cell carcinoma of salivary gland
- More common in minor salivary glands (~80%), particularly base of tongue, palate, floor of mouth, tongue and buccal mucosa in oral cavity/oropharynx
- The nests or cords lack focal palisading of basal cells ("ameloblastic") seen in CCOC
- Both lesions show EWSR1 rearrangements
- May represent "salivary gland analogue"
- Clear cell variant of calcifying epithelial odontogenic tumor (CEOT)
- Benign epithelial odontogenic neoplasm, clear cell variant may be composed primarily of clear cells
- Occurs in posterior mandible, intra-osseous location
- Variably sized polyhedral eosinophilic epithelial cells with distinct cell borders are arranged in small clusters, trabeculae, islands or a sheet like pattern
- Nuclear pleomorphism is expected, but without appreciable mitotic activity
- Eosinophilic amyloid-like matrix material is haphazardly deposited in association with the tumor islands, and calcified concentric profiles (Liesegang rings) are often identified
- Ancillary studies show the epithelial cells of CEOT highlight with cytokeratin AE1/3, CK5/6 and p63, and amyloid-like material exhibits apple green birefringence when stained with Congo red and viewed with polarized light
- Sclerosing odontogenic carcinoma
- Rare and controversial entity, described in 2008
- Low grade odontogenic carcinoma, locally aggressive
- Infiltrating single file strands, cords and nests of cuboidal or polygonal epithelial cells with cytoplasmic clearing, similar to signet ring change
- No prominent pleomorphism or mitotic figures; no necrosis
- Skeletal muscle and perineural infiltration with stromal sclerosis are characteristic
- Clear cell renal cell carcinoma (metastatic)
- Usually a known history of renal cell carcinoma, which is PAX8+
- Epithelial-myoepithelial carcinoma
- Malignant biphasic tumor with an inner duct-like epithelial component and an outer S100+ myoepithelial component
- Usually occurs in major salivary glands
- CCOC has only a clear cell epithelial component, and is S100 negative
- Mucoepidermoid carcinoma, clear cell variant
- Malignant epithelial tumor with variable amounts of mucous, epidermoid and intermediate cells
- Mucocytes are mucicarmine+
- Can be associatied with MAML2 rearrangement and NOT EWSR1
- Sinonasal renal cell-like adenocarcinoma (SRCLA)
- May be difficult to differentiate, but clear cell tumors involving the maxillary or palatal structures require consideration of a sinonasal neoplasm with secondary involvement of the oral region (Int J Clin Exp Med 2014;7:5469)
- Rare tumor characterized by a clear cell glandular proliferation, most often involving the nasal cavity, associated with a favorable clinical course
- Has round cells with clear cytoplasm and a prominent nucleolus arranged in a follicular pattern
- A tubular arrangement and papillary architecture of the clear cell proliferation have also been described
- No mucinous or myoepithelial differentiation, no necrosis, no hyalinization of stroma
- SRCLA vs. hyalinizing clear cell carcinoma of salivary gland (HCCC): no stromal hyalinization, no stromal vascularity; often has larger clear cells than HCCC and CCOC; has robust CAIX immunostaining vs. focal positive in HCCC; negative for EWSR1 rearrangement
Ameloblastomatous appearance:
- Desmoplastic ameloblastoma
- Dense collagenous stroma with compressed, angular islands of basaloid odontogenic epithelium
- Squamous odontogenic tumor
- Benign tumor of odontogenic squamous epithelium
- Very rare; thought to arise from rests of Malassez in periodontal ligament
- No peripheral palisading or stellate reticulum
- Odontogenic fibroma
- Rare tumor, and poorly described in literature
- Loose to dense collagenous stroma with small, rounded or elongated islands of bland odontogenic epithelial islands
- Islands not elongated, interconnected or arborizing
- Minimal clear cell change
Additional references