Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: LeBlanc RE. Mycosis fungoides. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticmycosisfungoides.html. Accessed April 2nd, 2025.
Definition / general
- Peripheral T cell lymphoma derived from mature, post-thymic T lymphocytes
- Presents as cutaneous patches and can progress to plaques, tumors and erythroderma
- While most patients experience an indolent course, the lymph nodes, bone marrow and viscera can become involved in advanced stage disease
Essential features
- Mycosis fungoides (MF) is a clinical diagnosis that requires strong correlation with histopathologic and sometimes molecular findings to exclude benign inflammatory diseases, more aggressive primary cutaneous lymphomas, and extracutaneous lymphomas that can involve the skin
- Conventional MF begins as eczematoid or psoriasiform patches and plaques that arise in a "bathing trunk" distribution
- MF often behaves as an indolent lymphoma with excellent overall survival; however, a minority of patients experience disease progression with fungating tumors, erythroderma and extracutaneous spread
- Biopsies from developed patches and plaques of MF show band-like papillary dermal lymphoid infiltrates with background fibroplasia, lymphocytes tagging the junction and migrating to the epidermis as single cells and Pautrier microabscesses, lymphoid cytologic atypia and an absence of findings that would otherwise suggest a spongiotic, psoriasiform or interface dermatitis; there are many histologic variants
- Immunohistochemistry is generally more useful to exclude other lymphomas than to confirm a diagnosis of MF
- Clonality testing can sometimes solidify a diagnosis when findings from pairs of temporally or anatomically separate samples are compared together
Terminology
- Mycosis fungoides (MF)
- Cutaneous T cell lymphoma
ICD coding
Epidemiology
- Higher incidence among men than women
- Median age at diagnosis in 50s
- Wide age range, predominantly older adults
- Children more likely to have the hypopigmented variant
Sites
- Photoprotected "bathing trunk" distribution involving the buttock, trunk and proximal limbs is found in most cases; however, mycosis fungoides can arise anywhere on the body
Pathophysiology
- Pathophysiology is incompletely understood due to the clinical and immunophenotypic heterogeneity of this entity
- Cells of origin are skin honing, effector memory T cells in contrast with the central memory T cell phenotype encountered in Sézary syndrome
- In skin limited disease, the cells most often show a tissue resident memory T cell phenotype and less frequently a migratory memory T cell phenotype (Sci Transl Med 2015;7:308ra158)
- Immunological milieu of mycosis fungoides (MF) is enhanced for Th2 gene expression and Th2 associated cytokine production (Am J Hematol 2016;91:151)
- NFkB has been associated with B cell lymphomagenesis and is constitutively activated in MF (Am J Hematol 2016;91:151)
- STAT activation, cyclin upregulation and loss of RB1 have been identified in some MF cohorts (Am J Hematol 2016;91:151)
- Cytogenetic and comparative genomic hybridization have demonstrated loss of 9p21 (including the CDKN2a - CDKN2B locus) in some cases of large cell MF and tumor stage MF (Am J Hematol 2016;91:151)
- Recurrent chromosomal translocations are rare in comparison with B cell lymphomas (Am J Hematol 2016;91:151)
Etiology
- Must exclude HTLV1 infection because some cases of adult T cell leukemia / lymphoma closely mimic mycosis fungoides (MF) at presentation
- Human leukocyte antigen (HLA) type associations and rare familial cases suggest genetic predisposition in some patients
- Some medications are associated with the development of T cell dyscrasias that resemble MF and resolve when the offending drug is withdrawn
- Infrequently, drug associated T cell infiltrates persist and behave as MF following agent withdrawal, suggesting that some medications can actually induce MF
Clinical features
- Must avoid overdiagnosis if equivocal findings, but underdiagnosis may lead to treatments that suppress antitumor immunity and foster disease development
- Can mimic spongiotic or psoriasiform dermatitis, wax and wane and elude a definitive diagnosis for years to decades
- Begins as a skin limited disease
- Classic patches are erythematous and heterogeneous in size and shape with fine scale and variable atrophy
- Increased risk of other malignancies including synchronous lymphoma
- Usually indolent, but may progress to infiltrative plaques, tumors and erythroderma reminiscent of Sézary syndrome
- Lymph node involvement, visceral involvement and rarely bone marrow involvement can occur with disease progression
- Advanced stage disease is associated with loss of T cell repertoire causing infection and death
- Variants include poikilodermatous, hypopigmented, granulomatous, folliculotropic, syringotropic and palmoplantar mycosis fungoides
Diagnosis
- Mycosis fungoides (MF) is a clinical diagnosis and a diagnosis of exclusion, using clinical, histologic and molecular data
- Must exclude inflammatory dermatitis (in particular spongiotic, psoriasiform and lichenoid diseases),drug induced reactions and dyscrasias, cutaneous dissemination of extracutaneous peripheral T cell lymphoma, indolent cutaneous lymphoproliferative disorder or aggressive primary cutaneous lymphoma
Laboratory
- Elevated lactate dehydrogenase (LDH) is an independent prognostic marker of worse survival
- Smear, flow cytometry and clonality testing can detect involvement in the peripheral blood
- HTLV1 serologic studies may be required to exclude adult T cell leukemia / lymphoma
Prognostic factors
- Independent prognostic markers of worse survival include clinical stage IV disease, age older than 60 years, large cell transformation and elevated lactate dehydrogenase (LDH) (J Clin Oncol 2015;33:3766)
- T category is based on the percentage of skin surface involvement and the lesional morphology (patchy, plaque, tumor or erythroderma)
- N category is based on the presence of dermatopathic lymphadenopathy, lymphoma cells and evidence of clonality in addition to the extent of nodal involvement by lymphoma
- M category is based on the presence or absence of visceral involvement
- Peripheral blood staging is based on the quantity of abnormal lymphocytes (blood tumor burden) and presence or absence of clonality
- Median survival for stage IA (< 10% skin surface involvement by patches or plaques) is ≥ 20 years
- Median survival beyond stage III (> 80% skin surface confluence / erythroderma) is approximately 5 years
Case reports
- 33 year old woman with a 7 year history of alopecia (J Cutan Pathol 2016;43:1179)
- 52 year old man with psoriasiform plaques on his palms and soles (Case Rep Dermatol 2009;1:60)
- 52 year old man with a 4 year history of intermittent, symmetrically distributed annular red patches on his trunk and extremities (JAAD Case Rep 2017;3:288)
Treatment
- An array of treatments and clinical trials exists
- Treatment is tailored to each patient depending on clinical findings, stage, prognosis and disease comorbidities
- Comprehensive information: NIH: Mycosis Fungoides (Including Sézary Syndrome) Treatment (PDQ®) [Accessed 12 February 2018]
- Photodynamic therapy: J Am Acad Dermatol 2016;74:27
- Retinoids: J Am Acad Dermatol 2003;49:801
- Targeted therapies: Lancet 2017;390:555
- Biologic therapies: Blood 2015;125:71
- Radiation therapy: Arch Dermatol 2011;147:561
- Chemotherapies: Blood 2015;125:71
- Transplant: J Clin Oncol 2014;32:3347
Clinical images
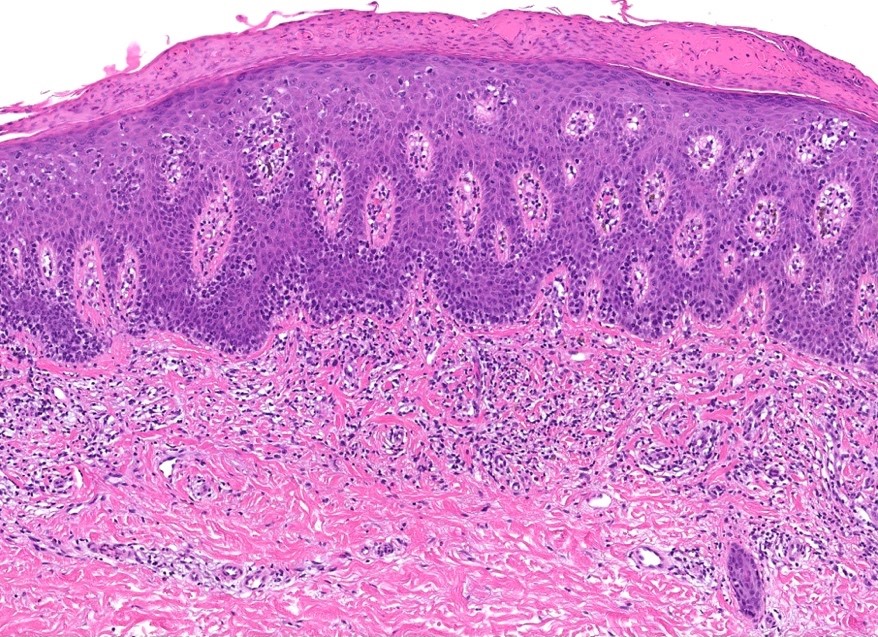
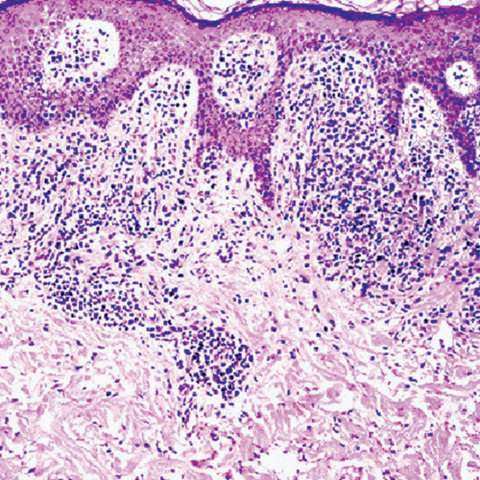
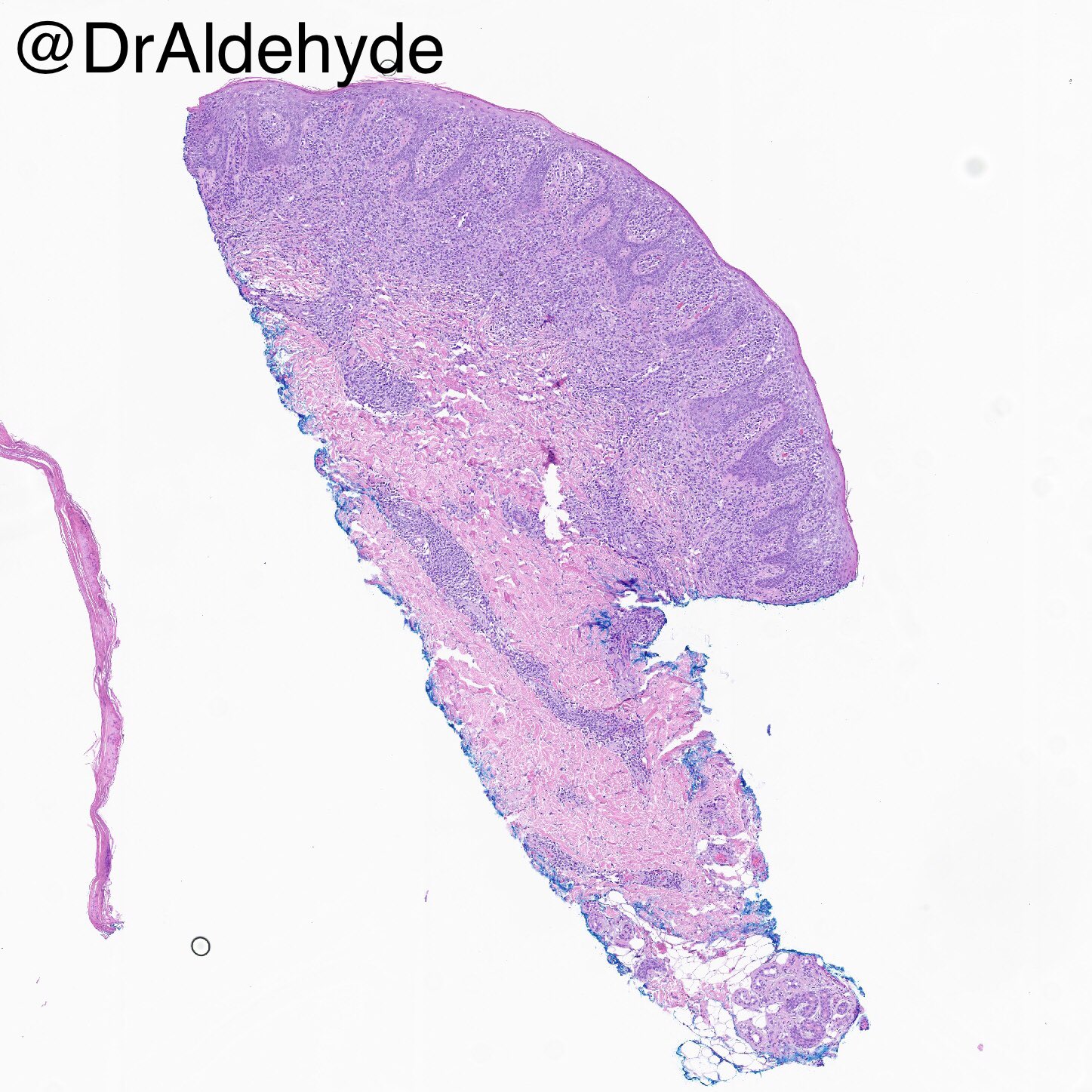
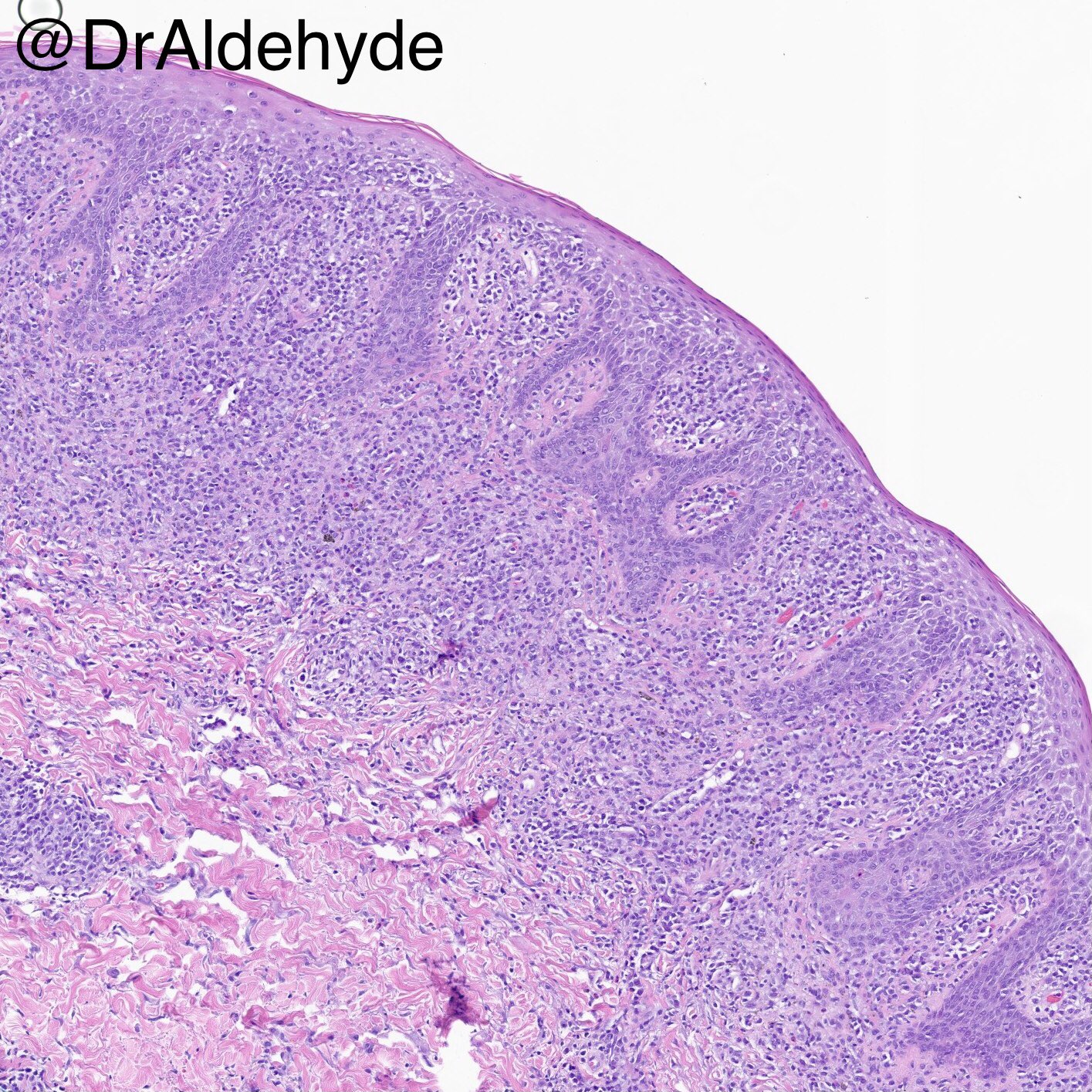
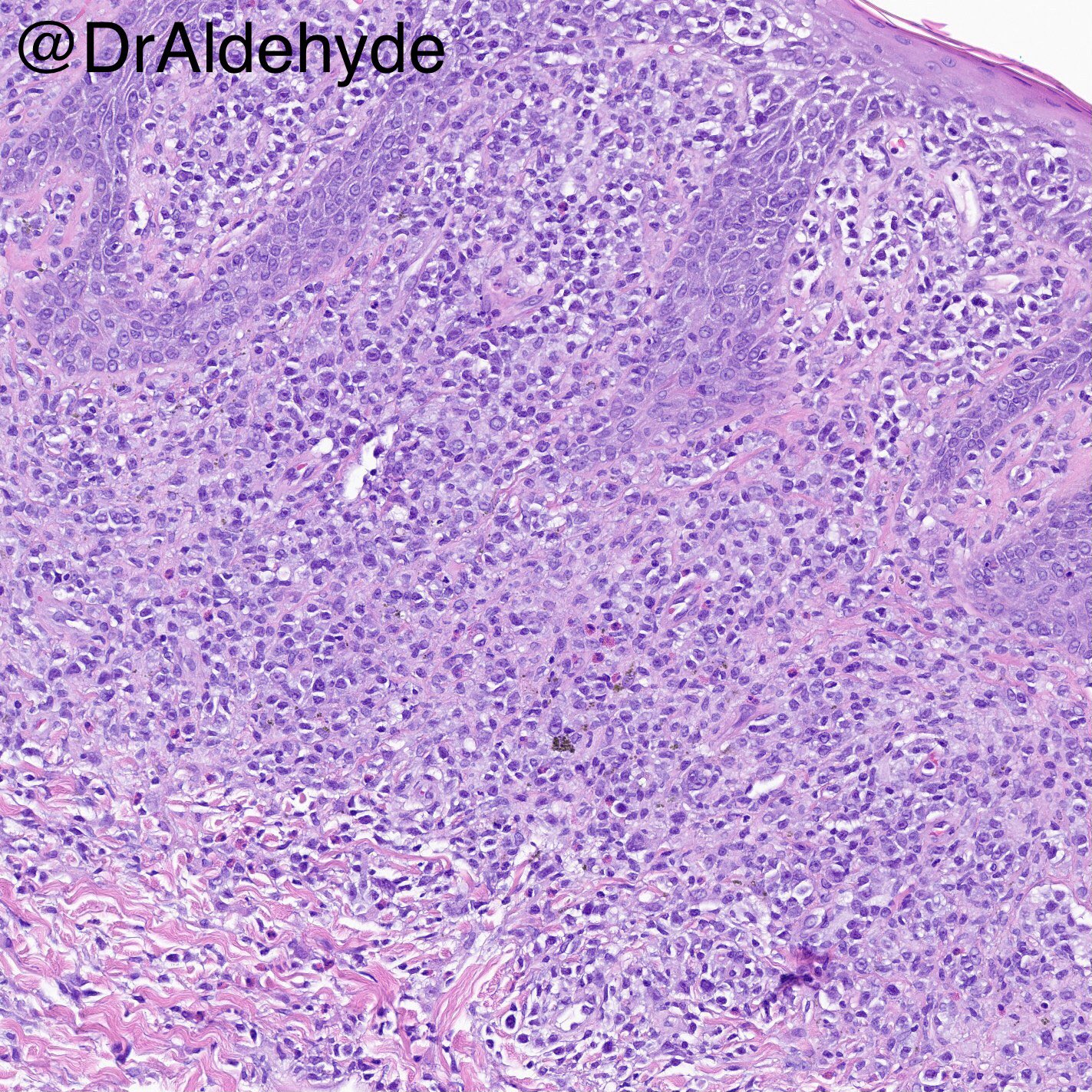
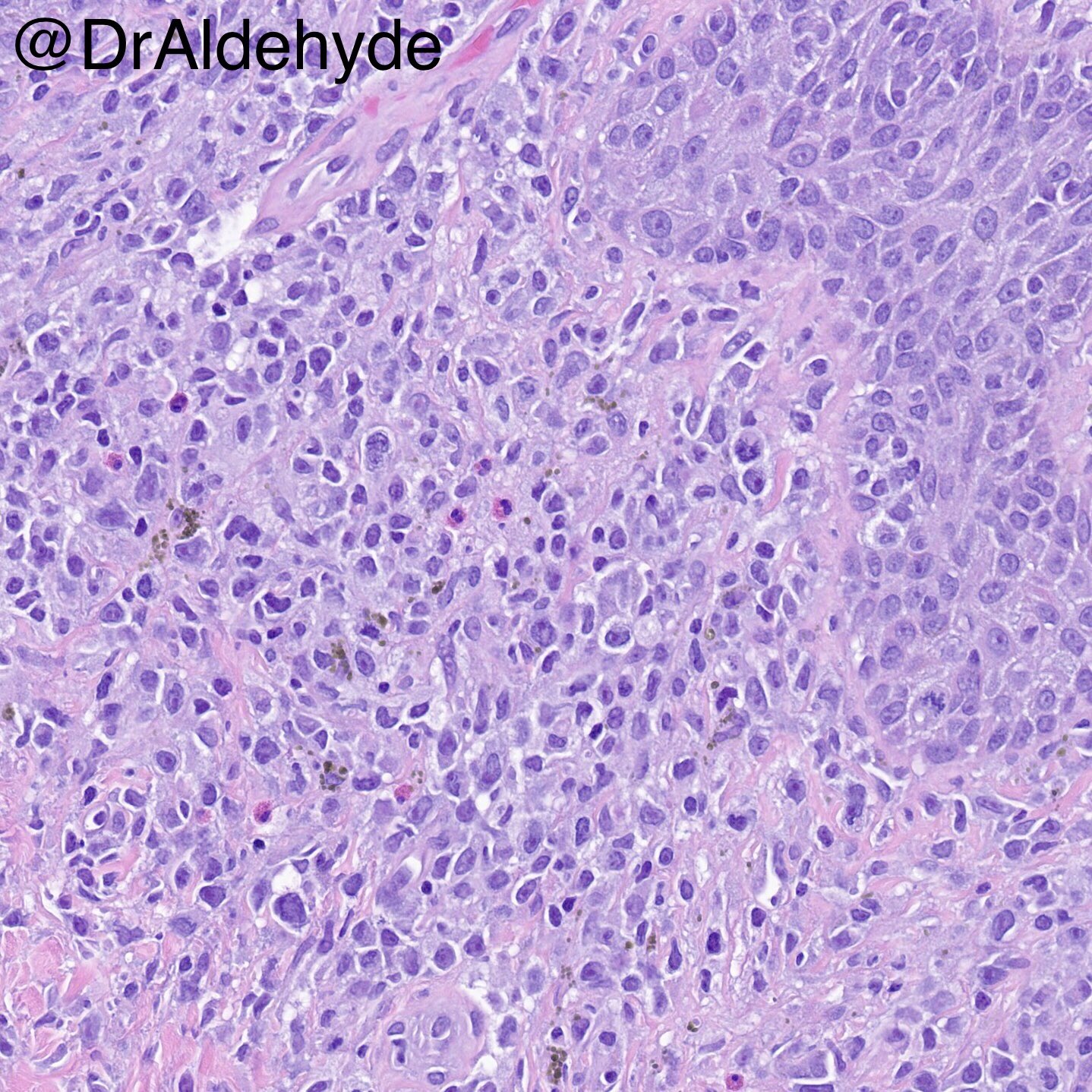
Microscopic (histologic) description
- Early lesions are sometimes histologically indistinguishable from more common inflammatory skin diseases
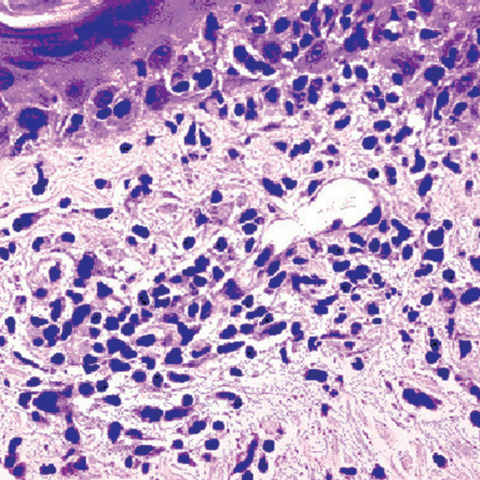
- Band-like papillary dermal lymphoid infiltrate
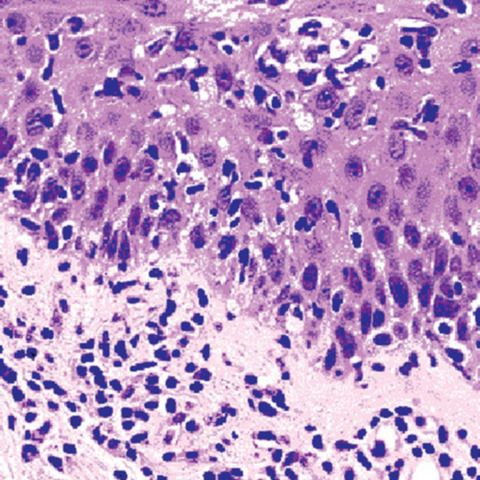
- Intraepidermal lymphocytes out of proportion with spongiosis (epidermotropism) ± Pautrier microabscesses
- Lymphocytes tagging the junction and within the epidermis may have haloes and can show variable nuclear pleomorphism, nuclear contour irregularity (cerebriform cytomorphology can be difficult to appreciate on biopsies) and hyperchromasia
- Dermal reticular fibroplasia with space between single lymphocytes
- Absences of features that would otherwise suggest a diagnosis of spongiotic dermatitis, drug hypersensitivity reaction, psoriasis or interface dermatitis
- Tumors can show an absence of epidermotropism and can involve the fibroadipose tissue
- Large cell transformation should always be reported when present and is defined as cells ≥ 4x size of a small lymphocyte comprising > 25% of total infiltrate
Microscopic (histologic) images
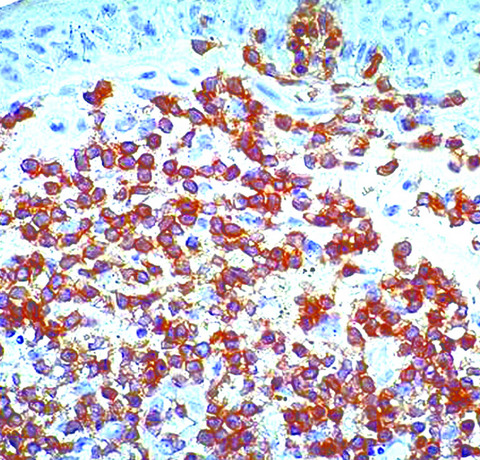
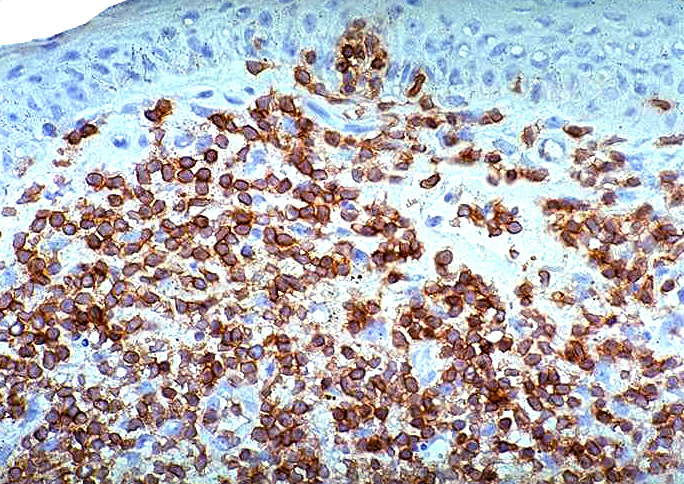
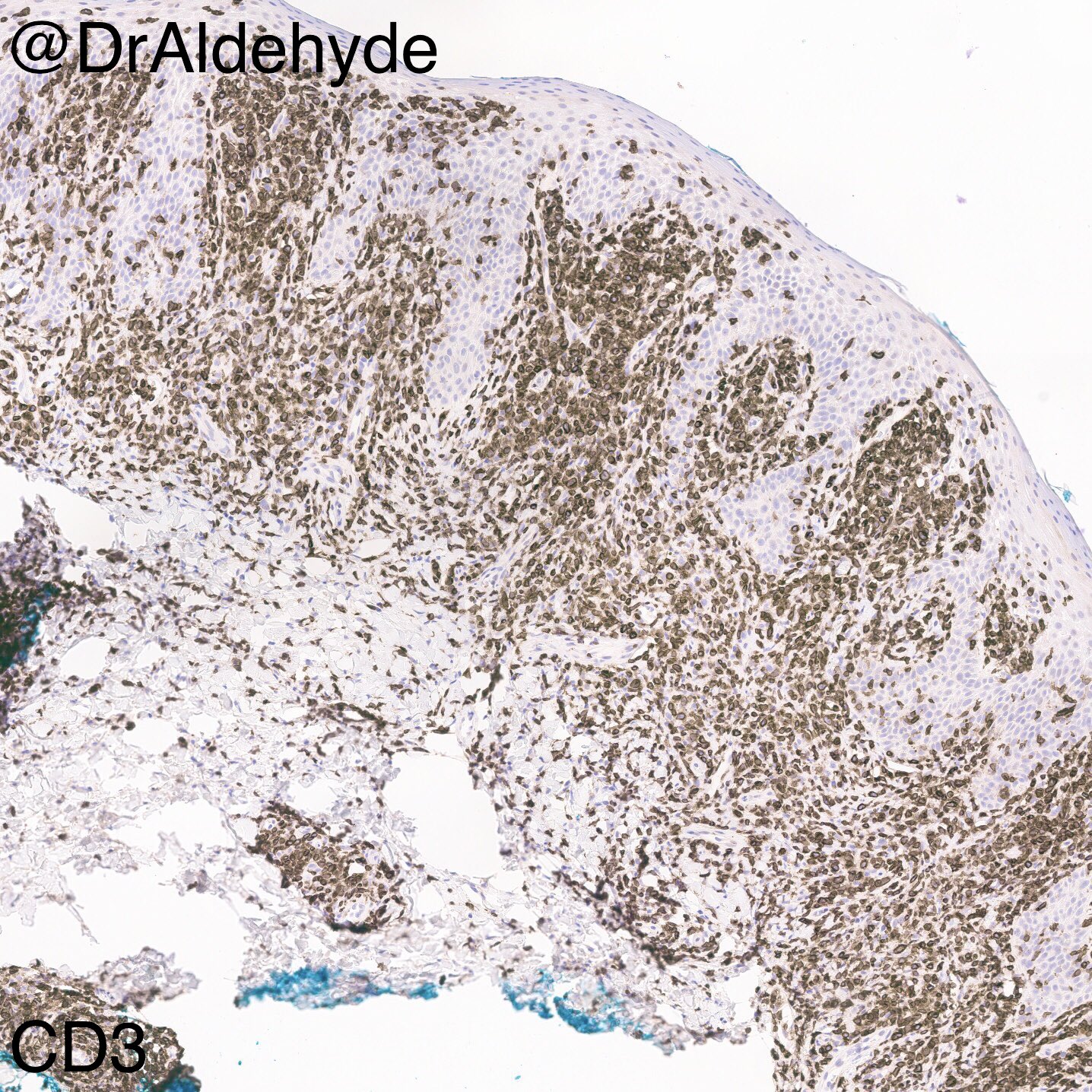
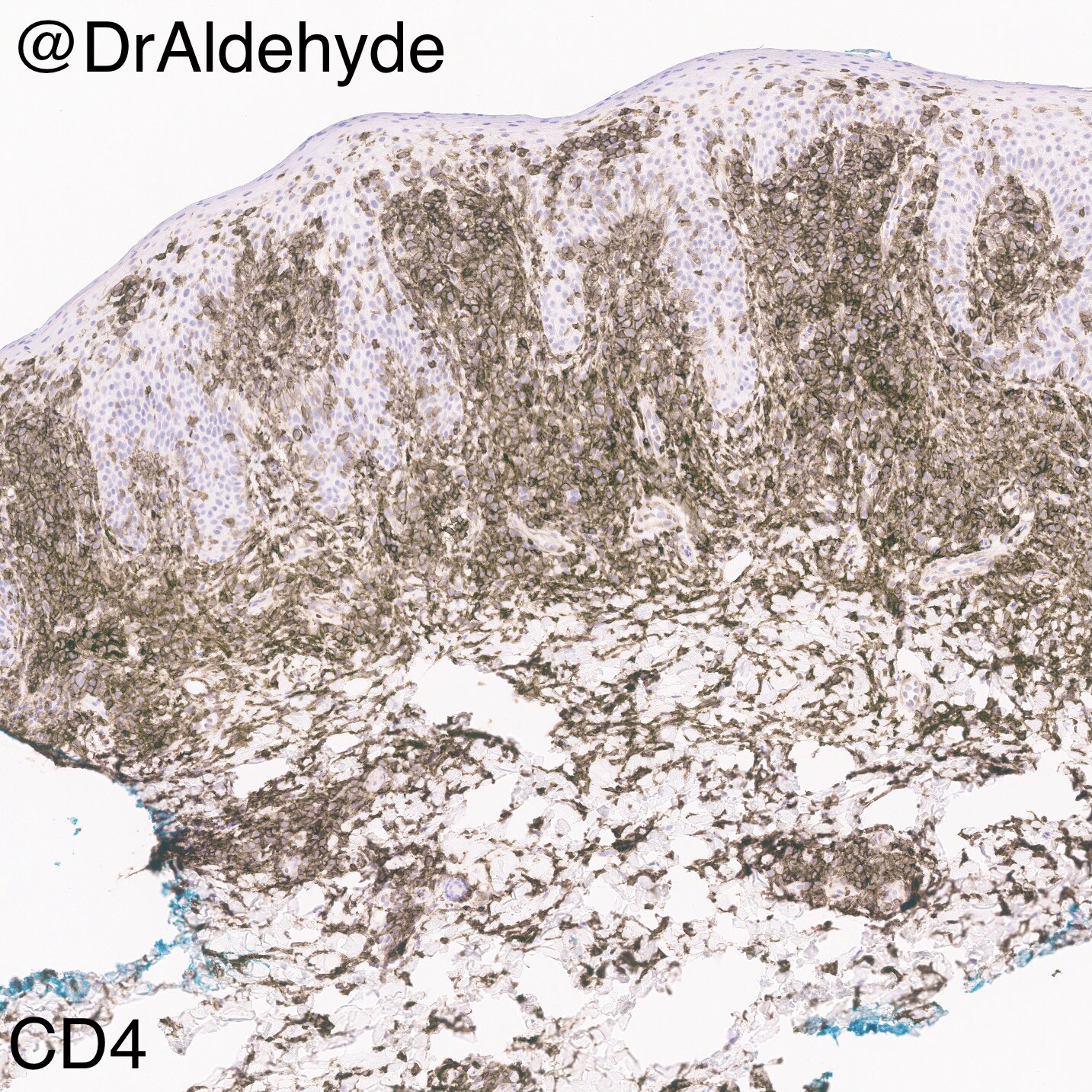
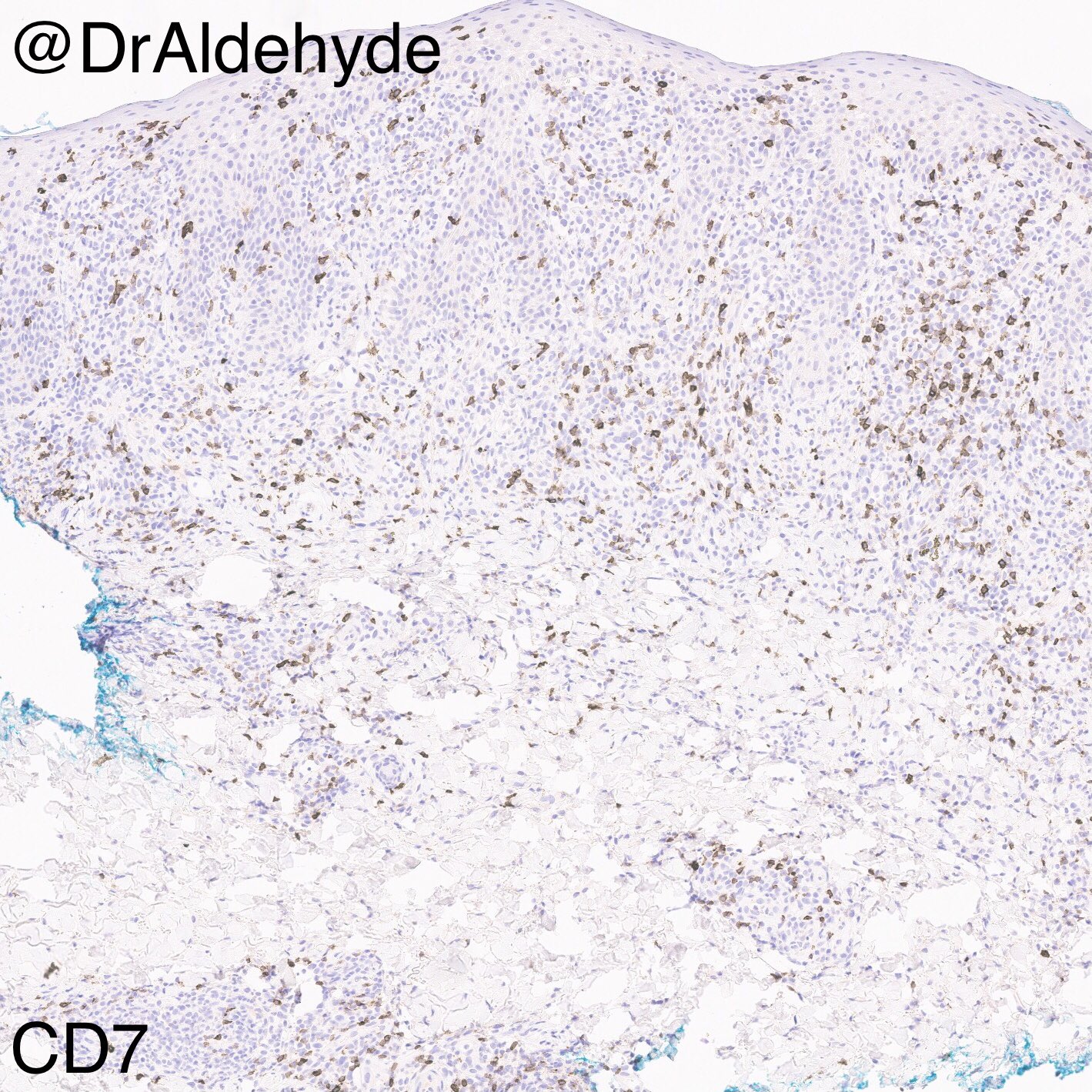
Positive stains
- In general, immunohistochemistry is more helpful to exclude other lymphomas than to confirm a diagnosis of mycosis fungoides
- Immunophenotype is variable and can change with large cell transformation and stage progression
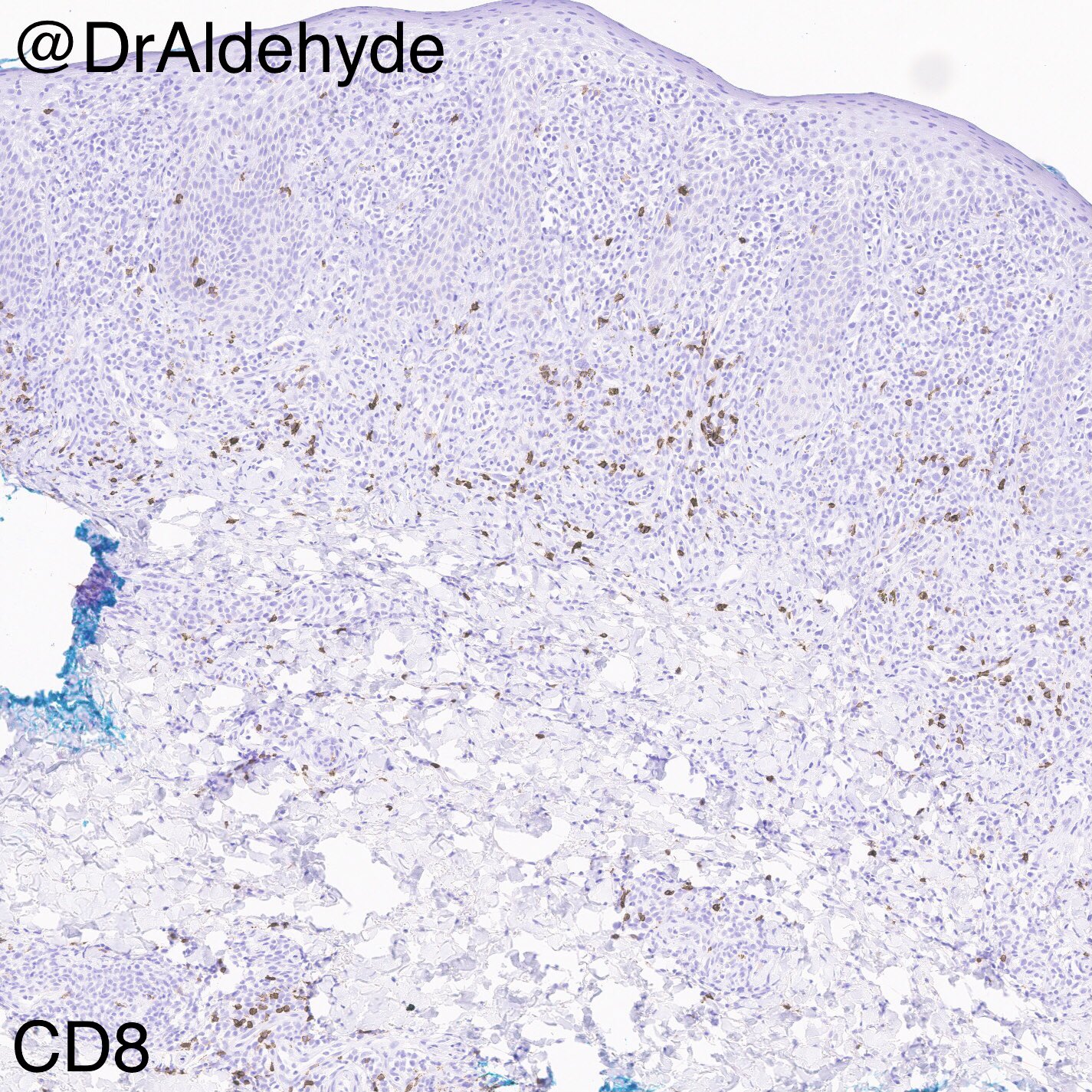
- Mature T cell phenotype (CD45RO+, TCR β+, CD2+, CD3+, CD4+ [frequent], CD8+ [infrequent], CD5+, CD7+) is most commonly observed
- Loss of CD2 or CD5 favors mycosis fungoides over inflammatory diseases such as eczema and psoriasis
- Partial loss of CD7 is common; however, this equivocal finding is also present in benign dermatoses
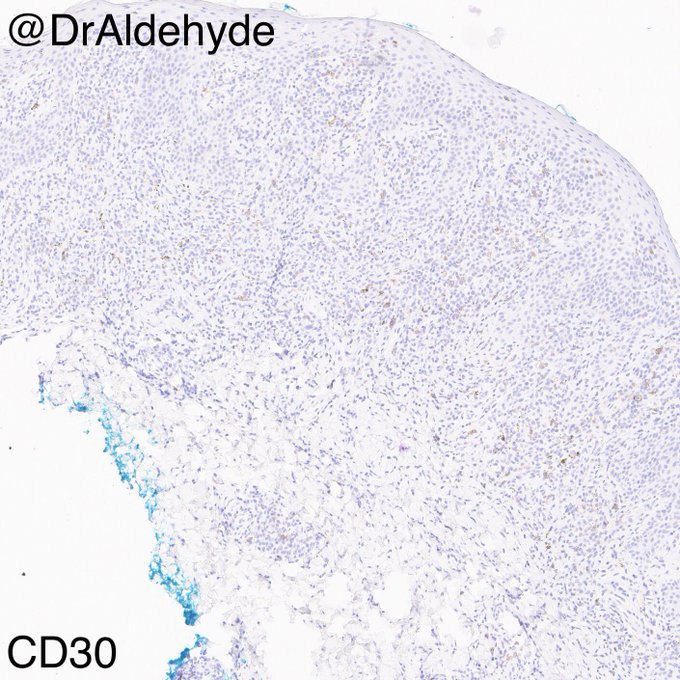
Negative stains
- TCR γ staining should raise consideration for gamma delta T cell lymphoma; however, there are clinically annotated cases of mycosis fungoides that have exhibited this immunophenotype
- CD8 and cytotoxic marker (TIA1, granzyme) expression should raise consideration for primary cutaneous CD8+ aggressive epidermotropic T cell lymphoma
- EBER staining of lesional cells should raise consideration for extranodal NK / T cell lymphoma, nasal type
Molecular / cytogenetics description
- Clonal rearrangement of the T cell receptor can be helpful if histology is nonspecific and clinical findings are strongly suggestive, but identification of clonality in a single biopsy is considerably less specific than identification of the same clone in multiple biopsies taken at different times or from different sites
- Clones can persist in pityriasis lichenoides spectrum disease and other T cell dyscrasias that do not behave as lymphoma
Sample pathology report
- Skin, left flank, punch biopsy:
- Epidermotropic T-cell infiltrate, suspicious for mycosis fungoides (see comment)
- Comment: This lesion has Pautrier-type microabscesses comprised of CD4+ T-cells that express TCR-beta and show a loss of CD2 expression. Background features of clinically considered psoriasis are not identified, and a PASd stain is negative for intracorneal fungal elements. No folliculotropism is identified. No evidence of large cell transformation is identified. Correlations with clinical and laboratory findings are essential to confirm the above impression.
Differential diagnosis
- Erythroderma:
- Acute graft versus host disease: subtle interface dermatitis with satellite cell necrosis
- Adult T cell leukemia / lymphoma: distinction often requires correlations with clinical history and serologic studies
- Atopic dermatitis: lymphocyte exocytosis proportionate to the degree of spongiosis; however, intraepidermal edema with eosinophils also can be present in mycosis fungoides so paired clonality studies may be helpful
- Chronic actinic dermatitis: clinical history, paired clonality studies
- Erythrodermic drug reaction: clinical correlation is necessary
- Paraneoplastic erythroderma: clinical correlation is necessary
- Pemphigus: an unusual cause of erythroderma; however, an absence of acantholysis and direct / indirect immunofluorescence findings could exclude this unlikely possibility
- Pityriasis rubra pilaris: clinical correlations can be extremely helpful and additionally, PRP can show alternating ortho and parakeratosis, thickening of suprapapillary plates, follicular plugs and focal acantholysis
- Psoriasis: dilated and tortuous papillary dermal vessels, attenuation of the suprapapillary plates, confluent parakeratotic crust with neutrophils and attenuation of the granular layer are helpful features but close clinical correlations and paired clonality testing are sometimes necessary
- Sézary syndrome: clinical correlations are necessary
- T cell prolymphocytic leukemia: clinical correlations would exclude mycosis fungoides (MF)
- Patch / plaque:
- Adult T cell leukemia / lymphoma: clinical correlations, HTLV1 serology
- Chronic actinic dermatitis: photodistribution should raise doubts about MF; however, paired clonality studies may be necessary in some cases
- Extranodal NK / T cell lymphoma nasal type: EBER+, angiodestructive
- Interface dermatitis: vacuolar degenerative changes, keratinocyte necrosis
- Lichenoid interface dermatitis: colloid body formations
- Mycosis fungoides-like drug reaction: clinical correlations are required
- Pityriasis rubra pilaris: clinical correlations can be extremely helpful and additionally, PRP can show alternating ortho and parakeratosis, thickening of suprapapillary plates, follicular plugs and focal acantholysis
- Primary cutaneous CD8+ aggressive epidermotropic cytotoxic T cell lymphoma: ulcerated plaques and tumors; furthermore, histology will show dense epidermotropic infiltrates of enlarged CD8 positive cells filling the epidermis without Pautrier microabscesses
- Primary cutaneous gamma delta T cell lymphoma: violaceous and sometimes ulcerated plaques and tumors comprised of TCR gamma+ lymphocytes
- Some show a predominantly epidermotropic pattern reminiscent of MF
- Another, potentially more aggressive variant shows adipotropism mimicking tumor stage / large cell MF and subcutaneous panniculitis-like T cell lymphoma
- Psoriasis: dilated and tortuous papillary dermal vessels, attenuation of the suprapapillary plates, confluent parakeratotic crust with neutrophils and attenuation of the granular layer are helpful features but close clinical correlations and paired clonality testing are sometimes necessary
- Secondary cutaneous involvement by an extracutaneous peripheral T cell lymphoma: clinical correlations are required
- Secondary syphilis: vacuolar interface changes, conspicuous endothelial swelling and a preponderance of plasma cells; immunohistochemistry or silver stain may highlight treponemes
- Spongiotic dermatitis: lymphocyte exocytosis proportionate to the degree of spongiosis; however, intraepidermal edema with Langerhans cells also can be present in mycosis fungoides so paired clonality studies may be helpful
- T cell prolymphocytic leukemia: clinical correlations would exclude MF
- Dermatophyte: PASd+ hyphae and yeast present in the stratum corneum
- Tumor:
- Lymphomatoid papulosis: clinical correlations (waxing and waning course), diffuse CD30 expression (this can also be seen in large cell MF) and paired clonality testing
- Primary cutaneous anaplastic large cell lymphoma: clinical correlations, diffuse CD30 expression (this can also be seen in large cell MF) and paired clonality testing
- Primary cutaneous CD4+ small / medium sized pleomorphic T cell lymphoproliferative disorder: clinical correlations (solitary lesion with no history of mycosis fungoides), polymorphous T cell infiltrate with T follicular helper immunophenotype (this immunophenotype can also be seen in MF), PD1+ rosettes, low Ki67 expression with positive cells distributed evenly throughout the lesion
- Primary cutaneous gamma delta T cell lymphoma: violaceous and sometimes ulcerated plaques and tumors comprised of TCR gamma+ lymphocytes
- Some show a predominantly epidermotropic pattern reminiscent of MF
- Another, potentially more aggressive variant shows adipotropism mimicking tumor stage / large cell MF and subcutaneous panniculitis-like T cell lymphoma
- Secondary cutaneous involvement by an extracutaneous peripheral T cell lymphoma: clinical correlations are required
- Subcutaneous panniculitis-like T cell lymphoma: clinical correlation can exclude MF; SPTCL can demonstrate epidermotropism but not to the extent of MF, CD8+ phenotype, Ki67 hotspots in the fat comprised of cytotoxic T cells rimming adipocytes
Additional references
- General mycosis fungoides: Clin Lab Med 2017;37:527, Am J Hematol 2016;91:151, Sci Transl Med 2015;7:308ra158, J Clin Oncol 2015;33:3766, J Cutan Pathol 2001;28:174
- Pediatric mycosis fungoides: Pediatr Dermatol 2017;34:547, Actas Dermosifiliogr 2017;108:564
- Folliculotropic mycosis fungoides: J Am Acad Dermatol 2016;75:347, Arch Dermatol 2008;144:738
- Hypopigmented mycosis fungoides: Int J Dermatol 2018;57:306, J Eur Acad Dermatol Venereol 2017;31:808
- Palmoplantar mycosis fungoides: Arch Dermatol 2007;143:109, Dermatology 2002;205:239
Board review style question #1
Which of the following studies best distinguishes mycosis fungoides from adult T cell leukemia / lymphoma?
- Biopsy revealing Pautrier microabscesses
- History of cutaneous patches at disease onset
- HTLV1 serology
- Immunohistochemistry with CD25
Board review style answer #1
C. HTLV1 serology. A clinical history, positive HTLV1 serology and a subsequent clinical staging could potentially distinguish mycosis fungoides from adult T cell leukemia / lymphoma. These diseases can show significant clinical and histologic overlap. Both can show CD25 expression.
Comment Here
Reference: Mycosis fungoides
Comment Here
Reference: Mycosis fungoides
Board review style question #2
Which of the following findings best distinguishes mycosis fungoides from Sézary syndrome?
- History of cutaneous patches at disease onset
- Involvement of the bone marrow
- Presence of atypical lymphocytes on peripheral smear
- Presence or absence of epidermotropism from the biopsy
Board review style answer #2
A. History of cutaneous patches at disease onset. The history of patch stage disease preceding the erythroderma distinguishes mycosis fungoides from Sézary syndrome. The remaining options can be seen with both diseases, although involvement of the bone marrow is rare.
Comment Here
Reference: Mycosis fungoides
Comment Here
Reference: Mycosis fungoides