Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Pathophysiology | Etiology | Clinical features | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Kaseb H, Hudnall SD. MGUS - non-IgM. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaMGUS.html. Accessed March 31st, 2025.
Definition / general
- The term monoclonal gammopathy of undetermined significance (MGUS) was introduced in 1978 by Robert Kyle to describe benign asymptomatic patients having an M protein that may progress to other malignancies
- By definition, no evidence of multiple myeloma, other B cell lymphoproliferative disorders or other diseases known to produce M protein
- 2 distinct types of MGUS: non-IgM MGUS (the focus of this topic) and IgM MGUS
- Non-IgM MGUS and IgM MGUS (lymphoplasmacytic lymphoma / Waldenström macroglobulinemia) are considered separate entities by the WHO / ICC classification due to the differences in cell of origin, clinical picture and disease progression (Lancet Oncol 2014;15:e538, Leukemia 2022;36:1720, Blood 2022;140:1229)
- Non-IgM MGUS (IgG, IgA, IgD or light chain MGUS) accounts for most MGUS cases and is characterized by a monoclonal plasma cell proliferation
- Light chain MGUS (a subset) has only monoclonal light chains with complete loss of heavy chain expression
- Non-IgM MGUS is a benign premalignant plasma cell disorder that is characterized by the presence of serum M protein < 30 g/L, bone marrow clonal plasma cells < 10%, absence of plasma cell myeloma related end organ damage and amyloidosis
- Non-IgM MGUS is usually asymptomatic; conditions with symptoms should be categorized as monoclonal gammopathy of renal significance (MGRS) or monoclonal gammopathy of clinical significance (MGCS) based on symptoms (Blood 2022;140:1229)
- Rarely, plasma cell MGUS produces an IgM M protein (1% of cases)
Essential features
- Non-IgM MGUS is a benign, asymptomatic premalignant plasma cell disorder that is characterized by the presence of serum M protein < 30 g/L, bone marrow clonal plasma cells < 10% and absence of plasma cell myeloma related end organ damage or amyloidosis
- Non-IgM MGUS may progress to a malignant plasma cell neoplasm (rate of 1% per year)
ICD coding
- ICD-10: D47.2 - monoclonal gammopathy of undetermined significance (MGUS)
Epidemiology
- Most common plasma cell neoplasm (Blood 2009;113:5412)
- Incidence increases with age and is found in ~2 - 3% of adults over age 50 and 5% of adults over age 70 (N Engl J Med 2018;378:241)
- More common than multiple myeloma (1 million versus 13,000 cases/year in the U.S.)
- More prevalent in African Americans than in Caucasians (2 - 3 fold) (Leukemia 2014;28:1537)
- More common in men than women (1.5:1)
- Median age at diagnosis: 70 years
- Non-IgM MGUS represents up to 85% of MGUS cases
Pathophysiology
- Originates from clonal mature plasma cells residing in the bone marrow that harbor somatic hypermutation errors or IgH class switched variable regions; these events occur during antigen selection in germinal centers
- Most non-IgM MGUS cases are IgG, followed by IgA, biclonal and IgD
- Random secondary genetic alterations have been associated with increased risk of progression to plasma cell myeloma
- Reference: Clin Lymphoma Myeloma Leuk 2023;23:e195
Etiology
- No specific cause has been identified; however, a gene - environment interaction is possible (Hematol Oncol Clin North Am 2014;28:775)
- Associated with
- Connective tissue disorders, peripheral neuropathies, dermatological diseases (such as acquired C1 esterase inhibitor deficiency [angioedema]), endocrine diseases and liver infections (such as hepatitis C and HIV liver disease)
- Radiation, pesticides and obesity (Blood 2009;113:6386, Blood 2009;113:1639, Blood 2010;116:1056)
- First degree relatives have higher incidence (Blood 2012;119:4608)
- Risk increased by polymorphisms at 2p23.3, 3p22.1, 3q26.2, 6p21.33, 7p15.3, 17p11.2 and 22q13.1 (Blood 2014;123:2513)
Clinical features
- Most patients are asymptomatic
- Usually diagnosed as an incidental finding on protein electrophoresis performed to evaluate peripheral neuropathy, vasculitis, hemolytic anemia, skin rashes, hypercalcemia or elevated erythrocyte sedimentation rate
- Diagnosis should be established only if the disease persists and is not transient (CMAJ 2013;185:1345)
- Paraprotein incidence: 70% IgG, 15% IgM, 12% IgA, 3% biclonal, 1% IgD, 1% IgE; monoclonal light chain in urine in 33% of cases; 20% with only light chain (N Engl J Med 2006;354:1362)
- No myeloma related organ or tissue impairment, such as hypercalcemia (> 1 mg/dL higher than the upper limit of normal or > 11 mg/dL), renal insufficiency (Cr clearance < 40 mL/min or serum Cr > 2 mg/dL), anemia (Hb > 20 g/L below lower limit of normal or > 100 g/L) or bone lesions (≥ 1 by skeletal radiography, CT or PET / CT) (= CRAB features of myeloma)
- 3 diagnostic criteria
- Serum monoclonal protein < 30 g/L
- < 10% clonal plasma cells in the bone marrow
- Absence of end organ damage attributable to the plasma cell disorder (CRAB features) and absence of amyloidosis
- Light chain only MGUS diagnostic criteria: abnormal light chain ratio (< 0.26 or > 1.65), urinary light chain must be < 0.5 g/24 h, < 10% plasma cells, end organ damage or amyloidosis
Laboratory
- Need thorough investigation to exclude other plasma cell neoplasms
- Complete blood count / peripheral smear: usually normal but some cases show rouleaux formation
- Plasma cells are associated with high risk MGUS
- Bone marrow with < 10% clonal plasma cells
- Plasma cells are usually mature with an interstitial distribution
- Serum calcium and creatinine: important in differentiating non-lgM MGUS from plasma cell myeloma
- Serum protein electrophoresis and immunofixation, serum free light chains, urine protein electrophoresis and immunofixation assay, quantitation of IgM
- Complete blood count / peripheral smear: usually normal but some cases show rouleaux formation
- Quantification of M protein is useful to monitor disease course (Hematol Oncol Clin North Am 2014;28:775)
- Serum protein electrophoresis can be performed on agarose gel or capillary zone electrophoresis
- Serum free light chains: measures κ and λ light immunoglobulin chains that circulate unbound to heavy chains in the serum; the normal ratio for κ/λ is 0.26 - 1.65
- Light chain MGUS: no immunoglobulin heavy chain on immunofixation electrophoresis
Radiology description
- Bone survey of skull, spine and pelvis (Xray, CT, MRI and PET with differing sensitivities)
- Important in differentiating non-lgM MGUS from other plasma cell neoplasm entities and other B cell lymphoproliferative disorders
- Osteolytic bone destruction (≥ 5 mm in size) on imaging is considered positive for bone involvement of plasma cell myeloma or plasmacytoma (Lancet Oncol 2014;15:e538)
Prognostic factors
- Considered a preneoplastic condition with an annual risk of progression of ~1%
- May progress to multiple myeloma, amyloidosis, Waldenström macroglobulinemia, solitary plasmacytoma or other lymphoproliferative disorder (Lancet Oncol 2014;15:e538)
- Risk of progression of non-IgM MGUS is lower than IgM MGUS (N Engl J Med 2018;378:241)
- Risk assessment based on serum M protein < 1.5 g/dL, IgG subtype, normal FLC ratio (0.26 - 1.65) (N Engl J Med 2002;346:564)
- Light chain MGUS: lower rate of progression (0.3% per year)
Case reports
- 49 year old man with polycythemia and renal failure (Nephrol Dial Transplant 2012;27:448)
- 61 year old man with dystrophic plasma cells (Eur J Haematol 2012;88:461)
- 70 year old woman with Good syndrome (BMJ Case Rep 2012;2012:bcr2012007601)
- 74 year old woman with leukocyte cytoplasmic inclusions associated with cryoglobulinemia (Eur J Haematol 2011;86:550)
- 81 year old woman with crystalline keratopathy (Br J Haematol 2012;159:258)
- 82 year old man with von Willebrand disease and IgG MGUS (Blood Coagul Fibrinolysis 2014;25:631)
- 86 year old woman with blue finger syndrome (BMJ Case Rep 2013;2013:bcr2012007966)
Treatment
- Management requires an understanding of the risk of progression
- Follow up of MGUS patients depends on the risk assessment
- Risk stratification (Blood 2005;106:812)
- Serum monoclonal protein level ≥ 15 g/L
- Non-IgG MGUS (i.e., IgA, IgM and IgD MGUS)
- Abnormal serum free light chain ratio
- Patients are categorized by number of risk factors present
- 3 risk factors: high risk MGUS
- 2 risk factors: high intermediate risk MGUS
- 1 risk factor: low intermediate risk MGUS
- 0 risk factors: low risk MGUS
- Despite close observation, can progress abruptly to plasma cell myeloma
- Follow up
- Low risk MGUS: every 2 - 3 years without laboratory testing (CMAJ 2013;185:1345)
- Intermediate and high risk MGUS: clinical and laboratory follow up every 6 months (Hematol Oncol Clin North Am 2014;28:775)
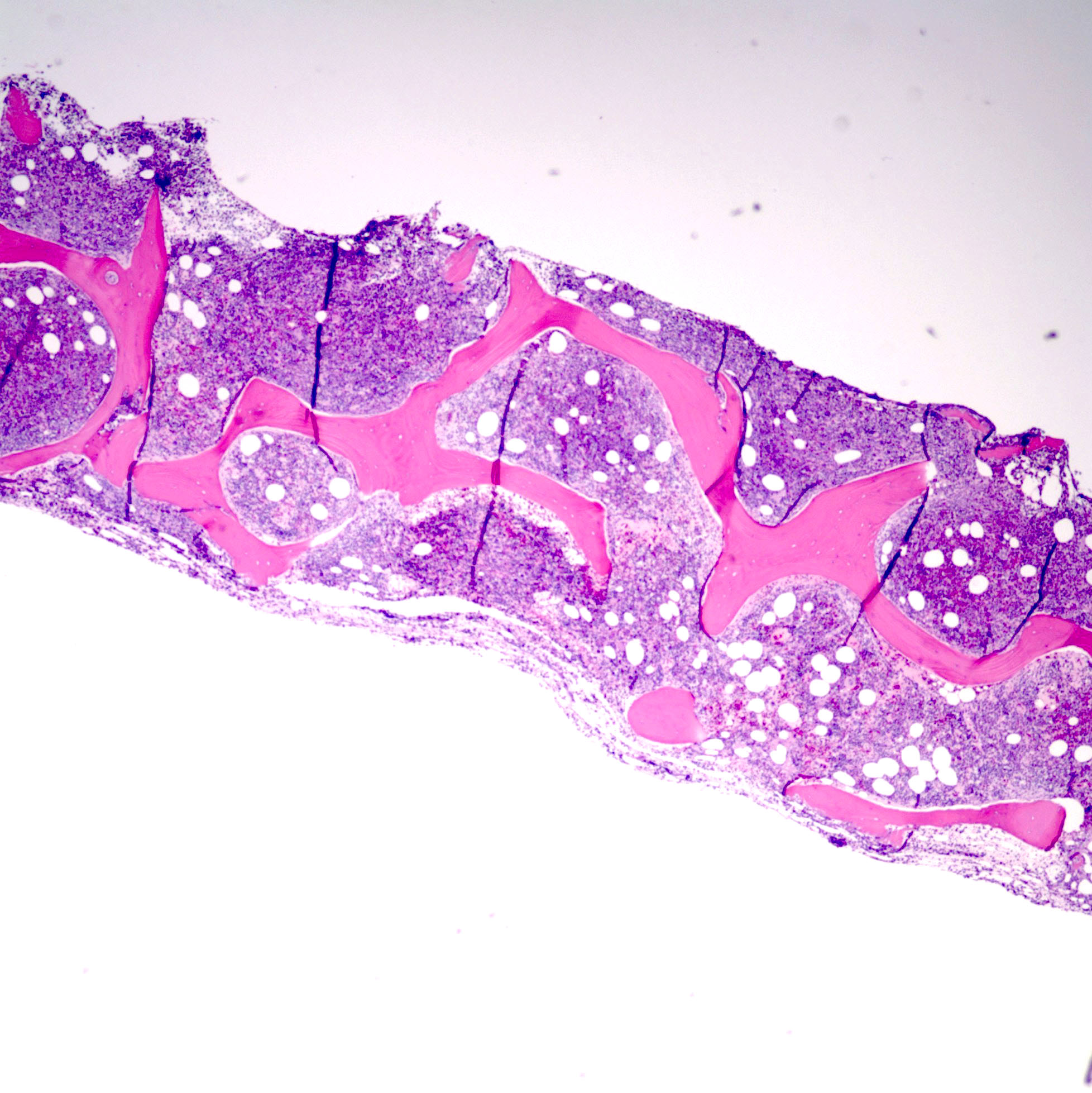
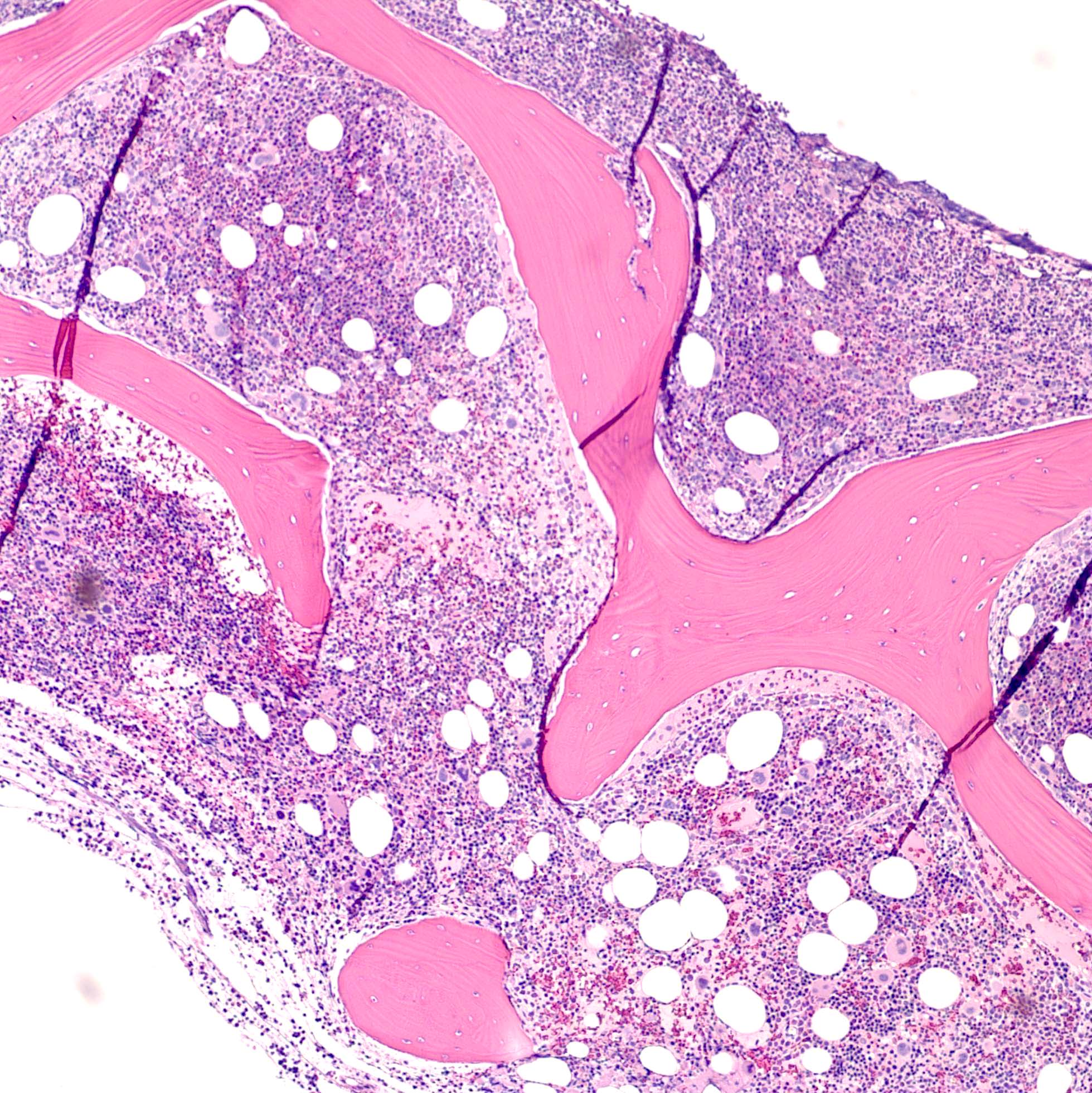
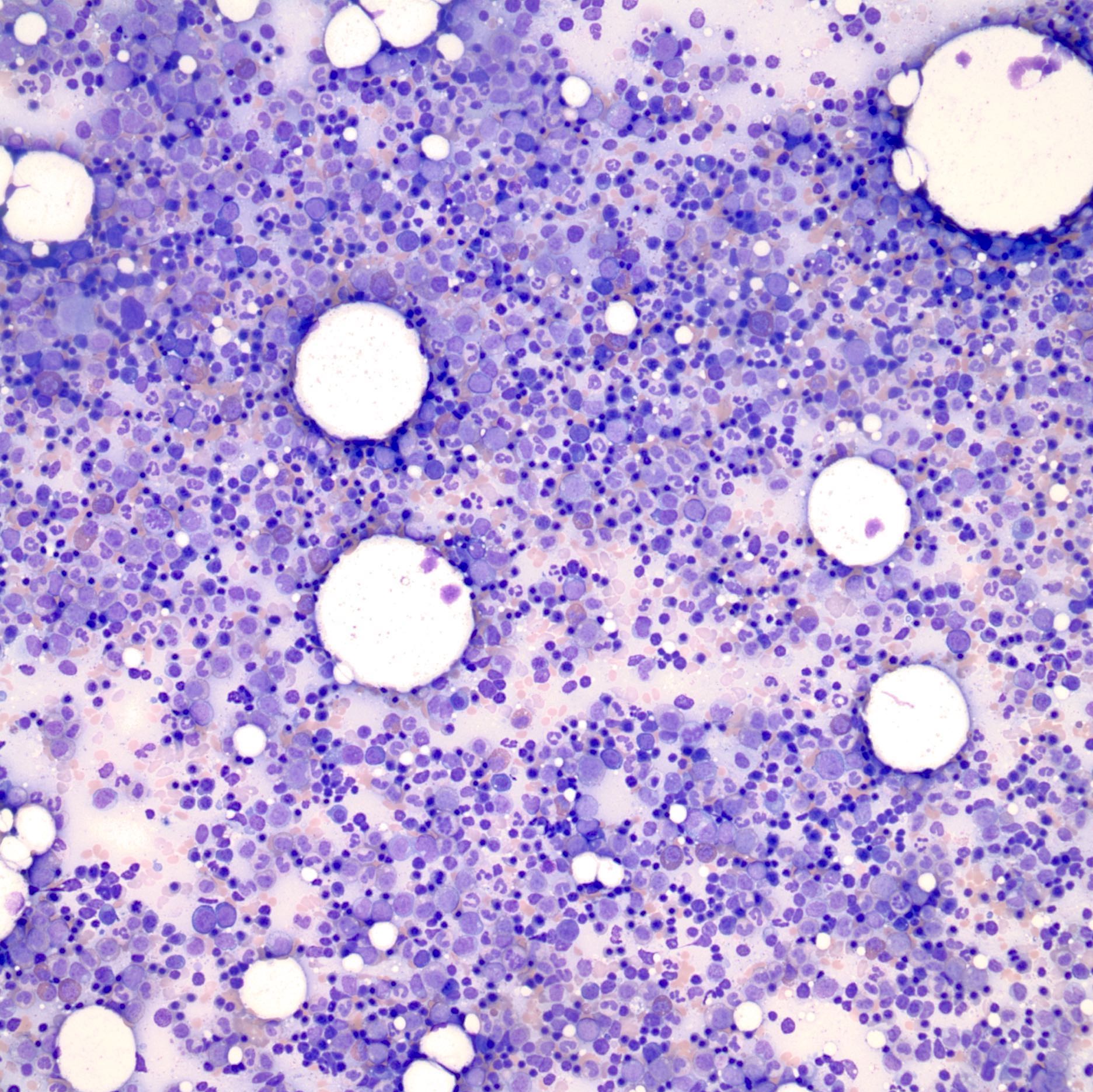
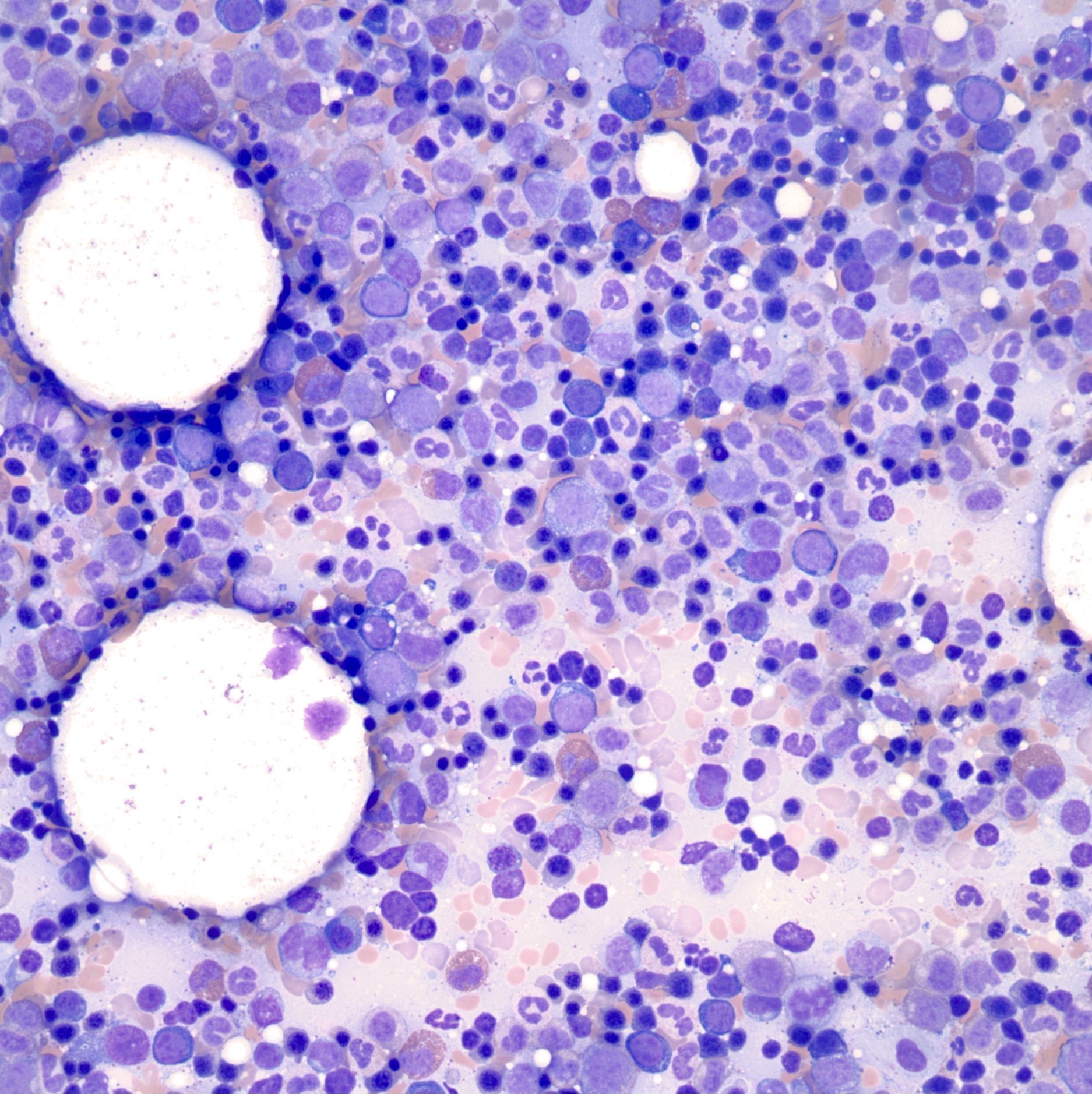
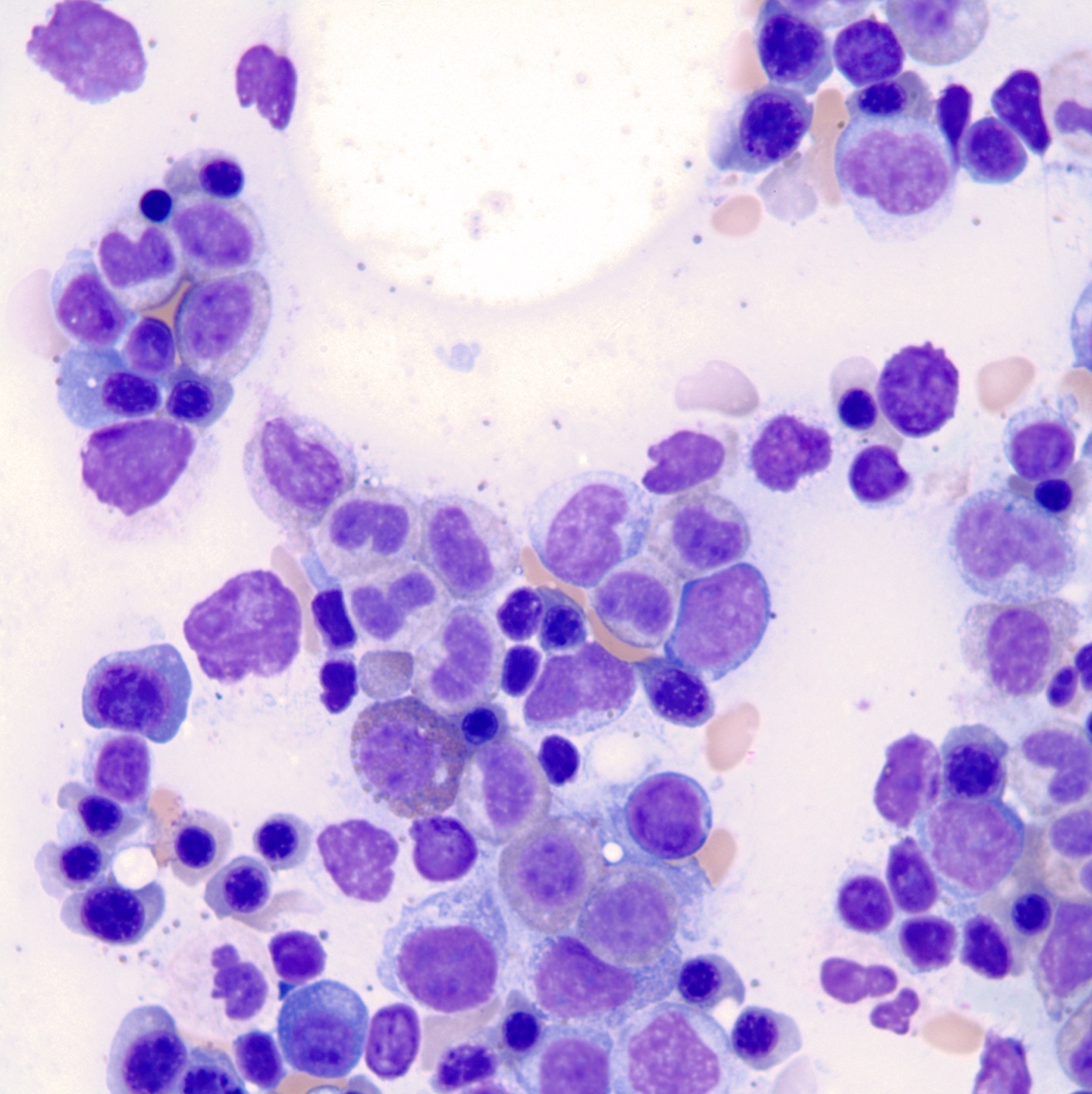
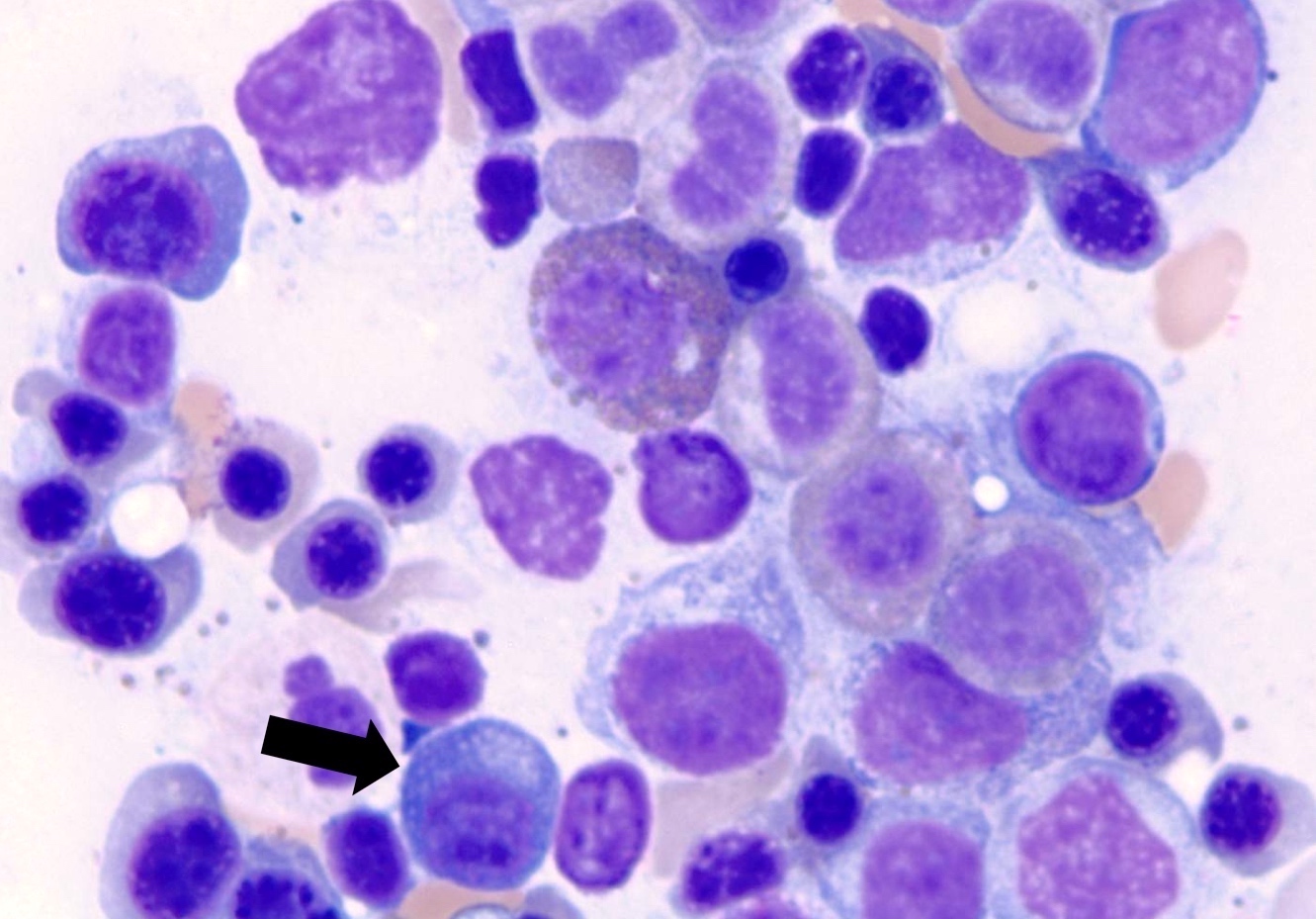
Microscopic (histologic) description
- < 10% clonal plasma cells in bone marrow aspirate / biopsy
- Plasma cells evenly scattered or in occasional small clusters
- Plasma cells lack nucleoli
- Reference: Clin Lymphoma Myeloma Leuk 2023;23:e195
Microscopic (histologic) images
Positive stains
Negative stains
- CD19 (in contrast to normal plasma cells)
Flow cytometry description
Molecular / cytogenetics description
- Usually shows a normal karyotype because of the relatively small number of plasma cells
- Possible chromosomal alterations include t(11;14), t(4;14), t(14;16), deletions of 13q and hyperdiploidy; no clinical correlation for these genetic alterations have been found in non-IgM MGUS
- Reference: Clin Lymphoma Myeloma Leuk 2023;23:e195
Sample pathology report
- Bone marrow, biopsy and aspirate:
- Plasma cell neoplasm with 5% plasma cells (see comment)
- Comment: This is a 70 year old man with a medical history of MGUS, currently presenting with congestive heart failure and anemia. The bone marrow shows increased plasma cells (5%); these cells show monotypic kappa light chain restriction by immunohistochemistry. Flow cytometry studies show 0.1% of the total events consistent with kappa restricted plasma cells. Further classification of plasma cell neoplasms requires correlation with clinical, laboratory and radiologic findings.
Differential diagnosis
- Smoldering plasma cell myeloma:
- Serum M protein ≥ 3 g/dL, bone marrow plasma cells ≥ 10% (but < 60%) and absence of CRAB features
- Waldenström macroglobulinemia (smoldering or symptomatic):
- IgM on immunofixation
- Light chain monoclonal gammopathy of undetermined significance (LC MGUS):
- Monoclonal protein that lacks the immunoglobulin heavy chain component
- Monoclonal gammopathy of renal significance:
- Meets diagnostic criteria for MGUS as well as renal insufficiency and monoclonal immunoglobulin deposits in the kidney by immunofluorescence (Blood 2012;120:4292)
- Light chain smoldering multiple myeloma (idiopathic Bence Jones proteinuria):
- Presence of monoclonal light chains in the urine (Bence Jones proteinuria) and no immunoglobulin heavy chain expression in the serum or urine
- Primary (amyloid light chain) amyloidosis and light chain deposition disease:
- Plasma cell neoplasm associated with the pathologic deposition of monoclonal light chains in tissue
- Presence of amyloid in tissue and evidence of plasma cell neoplasm
- Other B cell lymphoproliferative disorders:
- Diagnosis of the specific entity is based on biopsy, IHC, cytogenetics and molecular studies
Additional references
Board review style question #1
What is the rate of progression of non-IgM monoclonal gammopathy of uncertain significance (MGUS) to more advanced disease?
- 0.5% per year
- 1% per year
- 1.5% per year
- 2% per year
Board review style answer #1
Board review style question #2
Board review style answer #2
D. M protein of 15 g/L. The risk stratification (Blood 2005;106:812) for non-IgM MGUS includes serum monoclonal protein level ≥ 15 g/L, non-IgG MGUS (i.e., IgA, IgM and IgD MGUS) and abnormal serum free light chain ratio. Generalized lymphadenopathy and type of light chain restriction are not considered as risk factors for non-IgM MGUS.
Comment Here
Reference: MGUS - non-IgM
Comment Here
Reference: MGUS - non-IgM