Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Peripheral smear description | Positive stains | Negative stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Yenwongfai LN, Crane GM. Luetic lymphadenitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodessyphilis.html. Accessed March 31st, 2025.
Definition / general
- Lymph node pathology caused by Treponema pallidum (syphilis) infection
Essential features
- Lymphadenitis caused by Treponema pallidum
- Characteristic histologic features include extensive capsular fibrosis with pericapsular chronic inflammation, follicular hyperplasia with numerous plasma cells, phlebitis with endarteritis and occasional poorly formed granulomas
- Organisms stain with Warthin-Starry or specific immunohistochemical stains; confirmation by serology or PCR
Terminology
- Syphilitic lymphadenitis
ICD coding
- ICD-10: A52.79 - other symptomatic late syphilis
Epidemiology
- In 2021 there were > 171,000 cases of all stages of syphilis, representing a 68% increase from 2017 (Infect Dis Clin North Am 2023;37:195)
- Sexually transmitted infection or congenital syphilis acquired from infected mothers
- Screening recommended for men who have sex with men, in the setting of HIV and in pregnant patients
Sites
- Lymphadenitis associated with secondary syphilis (see Clinical features)
- Inguinal (most common), axillae, cervical and occipital (Br Med J 1970;4:67)
Pathophysiology
- Spread of T. pallidum organisms from the primary site of inoculation (chancre, painless ulcer with indurated margins) to regional or distant lymph nodes resulting in lymphadenopathy
- Modes of transmission include sexual contact and infection passed from mother to child
- T. pallidum infection normally triggers a robust humoral and cellular immune response but may take weeks or months to gain control of infection which is often incomplete with common infectious relapses (PLoS Negl Trop Dis 2012;6:e1717)
- Macrophages appear to be the primary means of bacterial killing in the skin (PLoS Negl Trop Dis 2012;6:e1717)
- Spirochetal membrane, including lipoproteins, is key in interacting with the host immune system, first triggering an innate immune response
- Spirochetal lipoproteins, such as outer surface protein B (OspB), may inhibit neutrophil function and prevent oxidative burst; others may activate neutrophils, induce neutrophil extracellular traps and activate monocytes / macrophages and dentritic cells through CD14 and Toll-like receptor signaling pathways resulting in a proinflammatory response and cytokine production (Front Immunol 2017:8:364, PLoS Negl Trop Dis 2012;6:e1717)
- However, the outer membrane of T. pallidum is unique with limited exposed lipoproteins and antigenic variation within the population in lipoprotein expression, resulting in overall poor reaction with antibodies present in syphilitic sera and enabling T. pallidum to evade the immune system (Infect Immun 2010;78:5178)
- Secondary syphilis occurs as a result of T. pallidum’s ability to escape immune recognition while causing inflammation (PLoS Negl Trop Dis 2012;6:e1717)
- T. pallidum may also trigger systemic immunologic abnormalities (PLoS Negl Trop Dis 2012;6:e1717)
- Syphilis infection increases the likelihood of HIV infection; may increase HIV viral load and decrease CD4 count in HIV infected patients (Neurol Clin Pract 2014;4:114)
Etiology
- Treponema pallidum (gram negative spirochete) infection
Clinical features
- Primary syphilis
- Painless chancre with or without regional lymphadenopathy typically within 3 - 6 weeks of inoculation of spirochete in the site of infection (Sex Transm Dis 1997;24:185, CMAJ 2011;183:2015)
- Secondary syphilis
- Disseminated skin rash (maculopapular or with pustular scales) or localized to the palms and soles of the feet, typically within 4 - 10 weeks after the appearance of the chancre (Genitourin Med 1989;65:1)
- Cutaneous well demarcated hypertrophic papules or plaques (condyloma lata) (JAAD Case Rep 2021;10:18)
- May also be associated with diffuse lymphadenopathy, hepatosplenomegaly, hepatitis or nephrotic syndrome (Am J Case Rep 2018;19:238)
- Tertiary syphilis
- Occurs 10 - 20 years post infections in untreated patients
- Cardiovascular syphilis (aneurysm or aortic insufficiency), granulomatous lesions invading and causing tissue destruction (gummas) and neurosyphilis (Infect Dis Clin North Am 2023;37:195)
- Latent syphilis
- Lack of clinical symptoms
Diagnosis
- Darkfield examinations and molecular tests for detecting T. pallidum directly from lesion exudate or tissue are the definitive methods for diagnosing early syphilis and congenital syphilis (CDC: Syphilis [Accessed 11 October 2023])
- 2 types of serologic test for syphilis are classified based on the type of antigen to which they are directed and are required for presumptive diagnosis (Neurol Clin Pract 2014;4:114, CDC: Syphilis [Accessed 11 October 2023])
- Treponemal tests detect antibody to T. pallidum proteins (reactive versus nonreactive); may show false positive in inflammatory diseases
- Treponemal tests include microhemagglutination assay, particle agglutination, hemagglutination assay, fluorescent treponemal antibody absorbed (FTA ABS) test, chemoluminescence immunoassays and enzyme immunoassays
- Nontreponemal tests detect antibodies (IgM or IgG) against lipoidal antigens, damaged host cells and possibly from treponemes and are semiquantitative, reflecting disease activity (Neurol Clin Pract 2014;4:114)
- Nontreponemal tests include rapid plasma reagin (RPR), the venereal disease research laboratory (VDRL) test and the toluidine red unheated serum test
- No single test is sufficient with both tests being used to confirm infection or determine disease activity
- Treponemal tests detect antibody to T. pallidum proteins (reactive versus nonreactive); may show false positive in inflammatory diseases
Laboratory
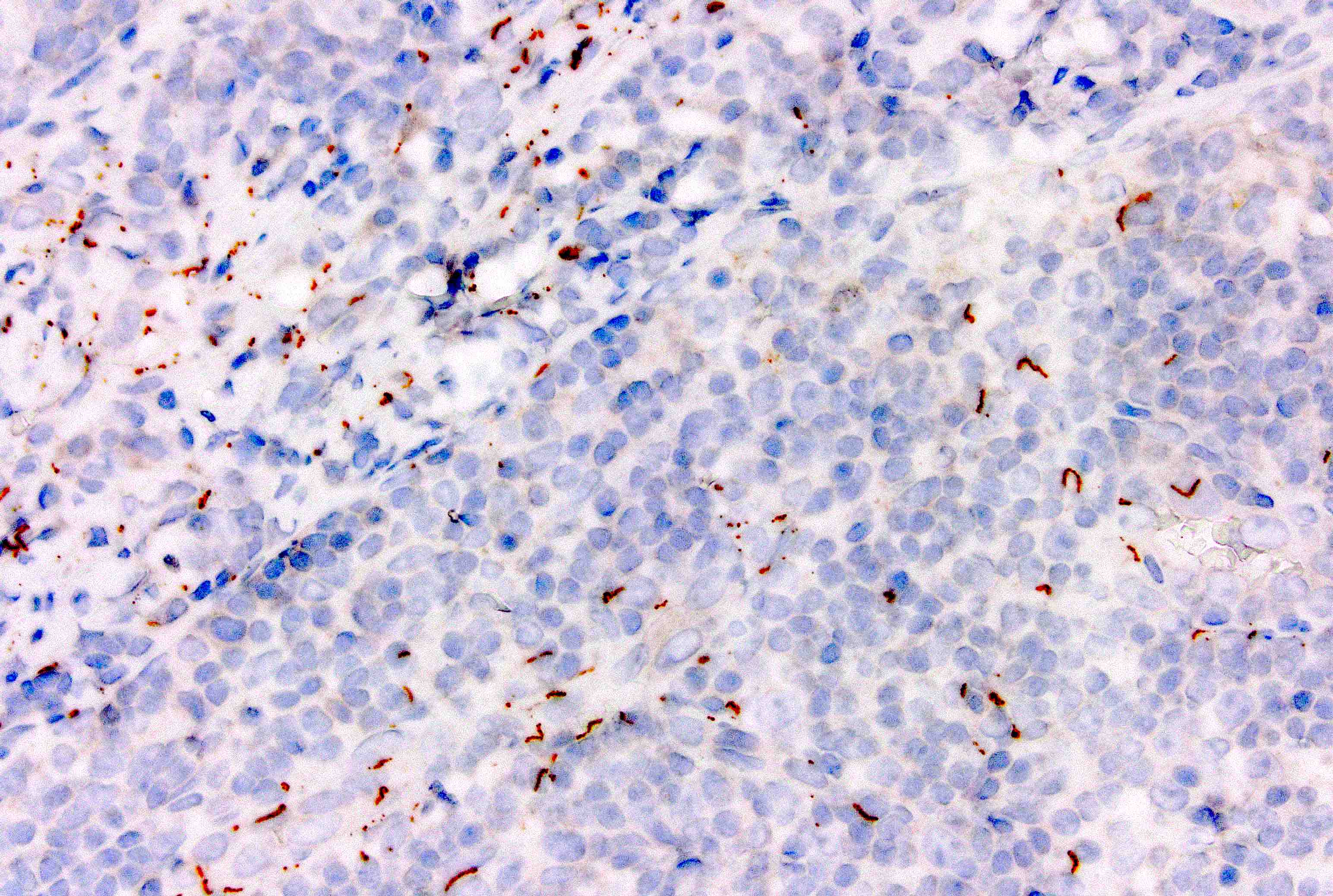
- Histology and immunohistochemical staining (J Biol Chem 1988;263:6363, J Invest Dermatol 2007;127:2345)
- Silver stain (Warthin-Starry) or antibodies to identify spirochetes in formalin fixed paraffin
- Embedded tissues from primary or secondary syphilis infections
- PCR (J Biol Chem 1988;263:6363)
- Complimentary test to serology in the diagnosis of early syphilis or congenital syphilis
- Dark field microscopy (Toxicol Sci 2004;81:3)
- Immunofluorescence is required for diagnosis but has the ability to distinguish between Treponema pallidum from nonpathogenic treponemes
- Culture (Can J Infect Dis Med Microbiol 2005;16:45)
- Technically impractical for routine diagnosis
Radiology description
- Lymphadenopathy, regional or distant sites
Prognostic factors
- Favorable prognosis with appropriate antibiotic treatment
Case reports
- 23 year old man with painless enlarged inguinal lymph node (Hum Pathol 2018;13:9)
- 27 year old man with right sided neck mass (Am J Case Rep 2018;19:238)
- 29 year old woman with painful unilateral neck swelling (Cureus 2023;15:e36065)
- 35 year old man with cervical syphilis with Pringer-Kuchinka-like lymphadenitis (Br J Oral Maxillofac Surg 2014;52:e141)
- 40 year old man with syphilitic cervical lymphadenitis with abscess formation (Blood 2018;131:707)
- 48 year old woman with acute onset of bilateral inguinal enlargement (Histopathology 2010;56:656)
- 48 and 72 year old men with nontender, progressively enlarging neck masses (J Int Med Res 2012;40:1988)
- 56 year old man with a firm enlarged inguinal lymph node and histologic features mimicking lymphogranuloma venereum (S Afr Med J 2016;106:49)
- 71 year old with primary syphilis and painful inguinal lymphadenopathy without cutaneous manifestations (Radiol Case Rep 2022;18:280)
- 2 brothers presented with isolated unilateral cervical lymphadenitis (J Infect 2009;58:76)
Frozen section description
- Similar findings to microscopic with reactive follicles and increased plasma cells
- Organisms can be seen on Giemsa stains (Intern Med 2017;56:2083)
Frozen section images
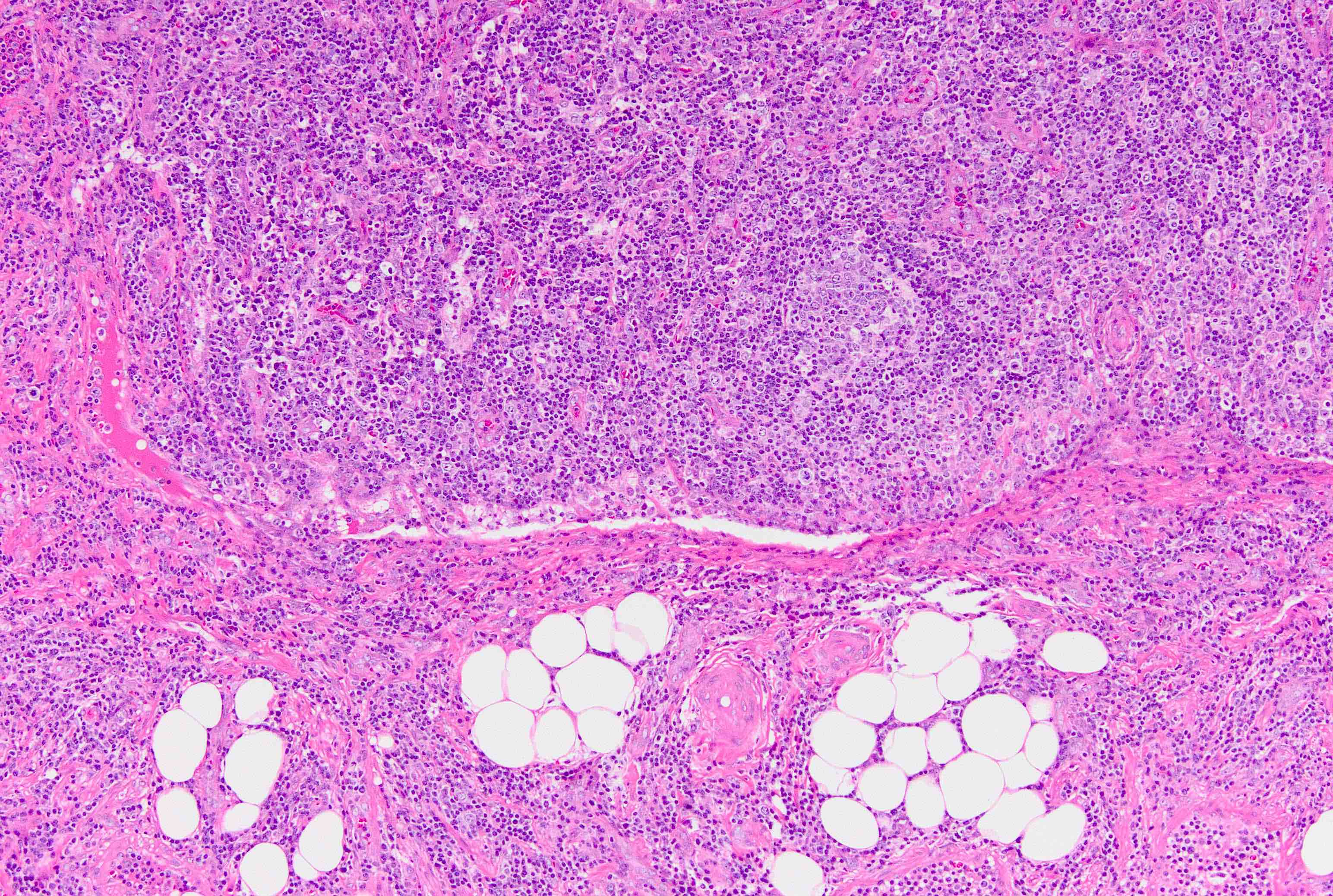
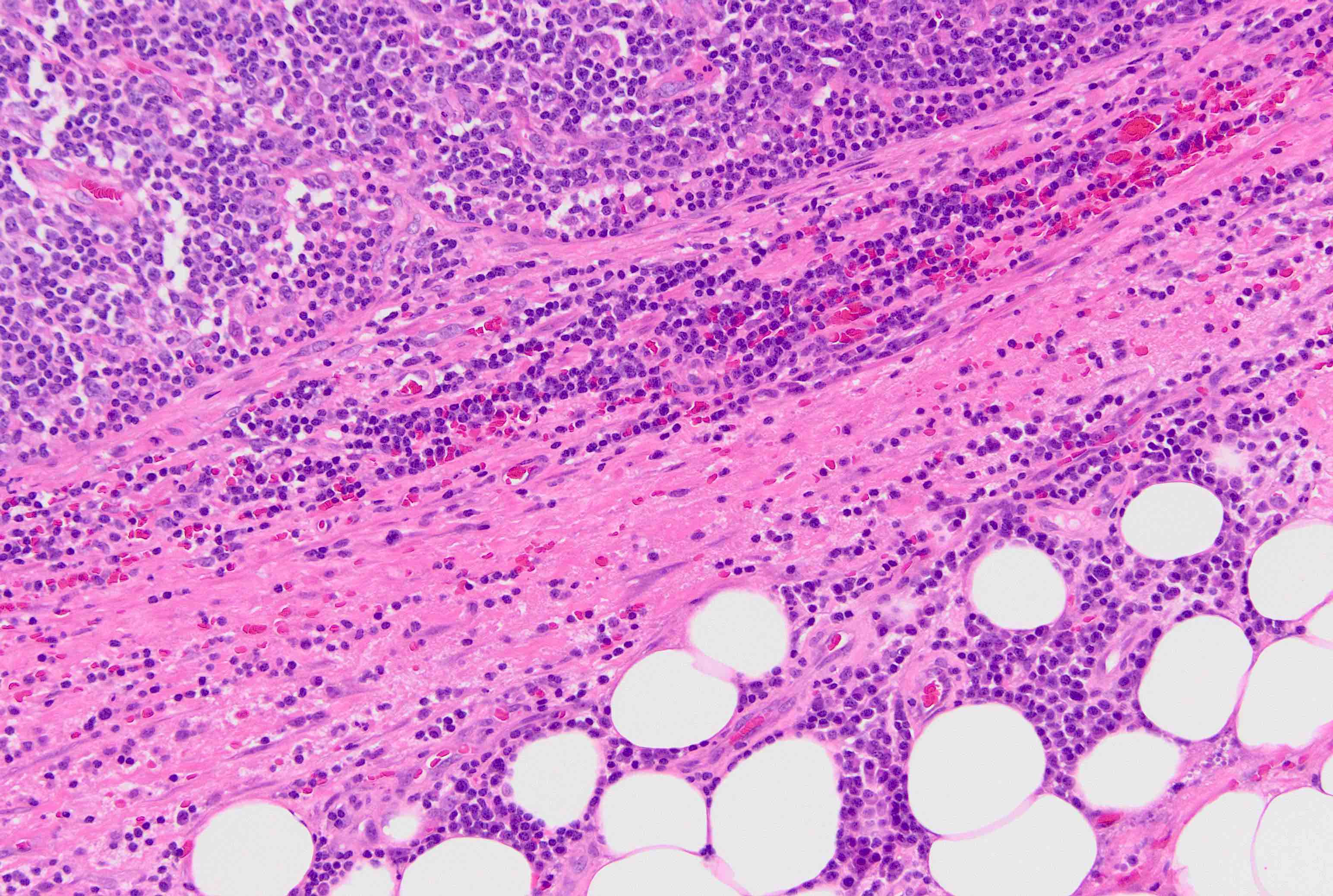
Microscopic (histologic) description
- Preserved or partial architectural distortion of lymphoid architecture (Pathol Int 2016;66:142)
- Thickened capsule with pericapsular chronic inflammation, plasma cells and extensive fibrosis (Histopathology 2010;56:656)
- Marked follicular hyperplasia with interfollicular, sinusoidal, perinodal and perivascular plasmacytosis (Arch Otolaryngol Head Neck Surg 1992;118:757)
- Phlebitis with endarteritis in the capsule and nodular tissue
- Variable histiocytes, noncaseating granulomas may be present (Pathol Int 2016;66:142, Am J Clin Pathol 1970;53:304)
- Unusual formation of abscess containing spirochetes may occur (Blood 2018;131:707, Am J Clin Pathol 1970;53:304)
Microscopic (histologic) images
Virtual slides
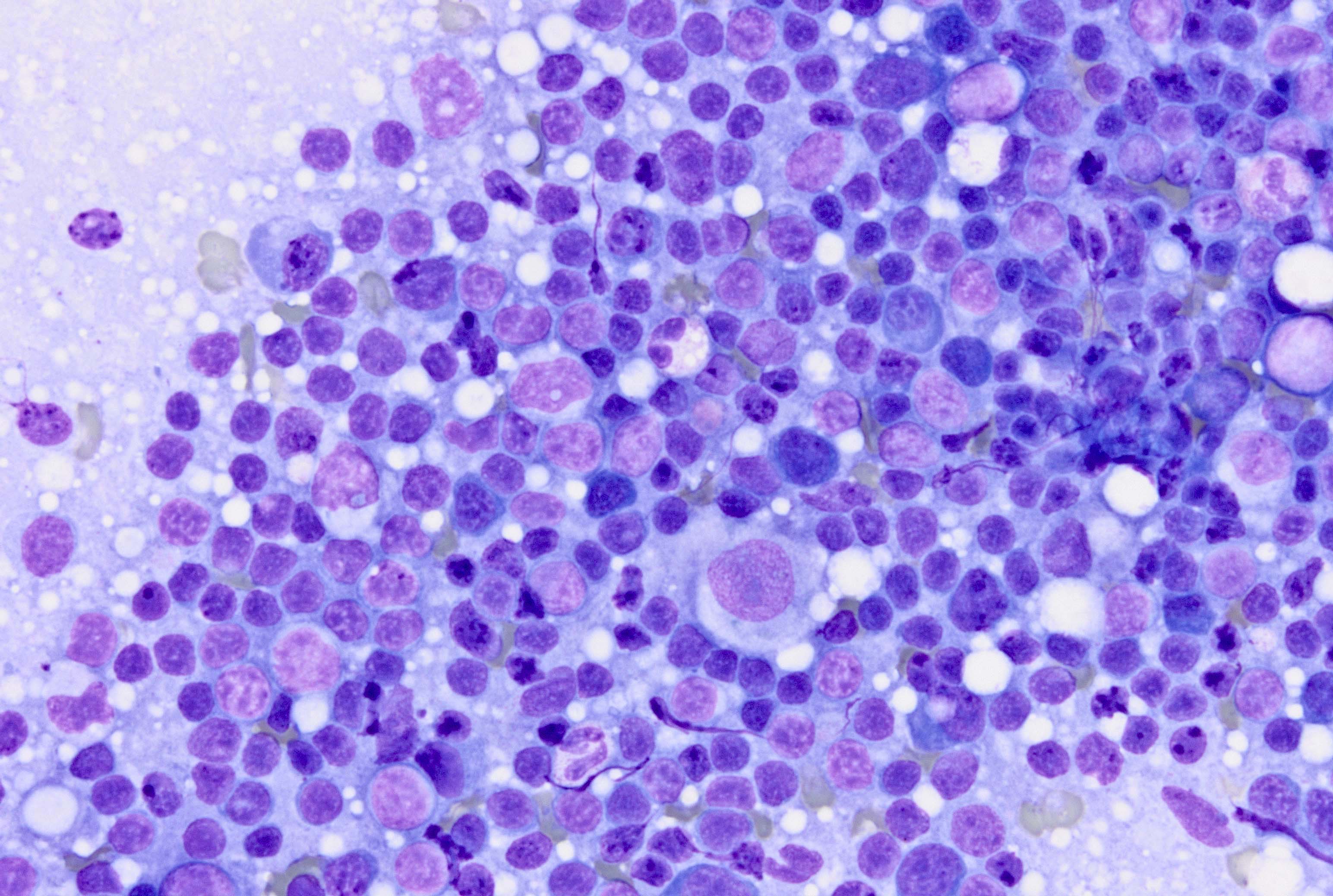
Cytology description
- Branching / arborizing vessels with perivascular plasma cell cuffing, presence of neutrophils and granulomas (Diagn Cytopathol 2023;51:E199)
Peripheral smear description
- Leukocytosis, anemia and thrombocytopenia especially in neonates in the setting of congenital acquired syphilis (AJP Rep 2017;7:e167)
Positive stains
- Warthin-Starry silver stain or modified Steiner stain highlights spirochetes (Hum Pathol 2018;13:9)
- T. pallidum IHC (Hum Pathol 2018;13:9)
- Giemsa stain (Intern Med 2017;56:2083)
Negative stains
- Difficult to visualize with Gram stain (Intern Med 2017;56:2083)
- Acid fast stain (Medeiros: Ioachim's Lymph Node Pathology, 5th Edition, 2021)
Electron microscopy description
- Complex structure with 2 layered outer wall (Bull World Health Organ 1966;35:223)
Sample pathology report
- Inguinal lymph node, excisional biopsy:
- Reactive follicular hyperplasia with increased plasma cells, capsular thickening and fibrosis (see comment)
- Positive for T. pallidum consistent with syphilitic lymphadenitis
- Comment: The patient is a 60 year old man presenting with an indurated inguinal mass. Concurrent flow cytometry demonstrates no evidence of a monoclonal B cell or aberrant T cell population. The morphologic findings together with the organisms visualized by a special stain for T. pallidum are consistent with syphilitic (luetic) lymphadenitis. Correlation with clinical presentation and history are recommended. Confirmation with serologic or molecular studies can be considered if clinically indicated.
Differential diagnosis
- Lymphogranuloma venereum:
- Sexually transmitted disease caused by Chlamydia trachomatis
- Diagnosis may be complicated by coinfection with T. pallidum
- Hyperplastic lymphoid follicles with increased plasma cell infiltrates and suppurative lymphadenitis which often involves the lymph node capsule and surrounding tissues
- Stellate abscesses are characteristic but not specific (S Afr Med J 2016;106:49)
- PCR for chlamydial DNA or complement fixation with titers > 1:256
- No commonly available stain for the tissue identification of C. trachomatis (Histopathology 2021;78:392)
- Necrotizing granulomatous lymphadenitis:
- Lymphadenitis characterized by acute inflammatory cells and necrosis with giant cells and granulomas
- Clinical conditions include tuberculosis, cat scratch disease, histoplasmosis and leprosy
- Etiologic agents can be determined through serology, specific antibodies or identification of specific antigens using PCR
- Inflammatory pseudotumor:
- Etiology unknown
- Prominent benign lymphadenopathy affecting 1 or several nodes
- Reactive node with mixed inflammation, vascular proliferation with phlebitis and varying degrees of storiform sclerosis
- Negative stains: Warthin-Starry or anti-Treponema pallidum antibodies, ALK and HHV8
- Cat scratch lymphadenitis:
- Caused by Bartonella henselae acquired from arthropod vector or inoculation by scratch from infected cat
- Lymph nodes show follicular hyperplasia with deposition of amorphous intercellular proteinaceous material in follicles and characteristic stellate necrotizing granulomas (Am J Clin Pathol 1962;38:513)
- Positive stain with Warthin-Starry (rod shape rather than spiral)
- Monoclonal anti-B. henselae on paraffin fixed tissue or PCR analysis of bacterial DNA
- Toxoplasma lymphadenitis:
- Lymphadenitis caused by Toxoplasma gondii
- Preserved lymph node architecture, with no capsular involvement
- Characteristic triad of florid follicular hyperplasia, monocytoid B cell hyperplasia and epithelioid histiocytes and microgranulomas
- Difficult to identify organisms in nodes but infection can be confirmed by serology for IgM and IgG antibodies against T. gondii cell wall antigens
- Highly sensitive and specific Sabin-Feldman dye test (mainly used by reference laboratories)
- HIV lymphadenitis:
- Similar patient population and may co-occur
- Prominent follicular hyperplasia
- Capsular fibrosis is not a characteristic feature
- Distinguished by a lack of detectable organisms, serology
- Reference: Medeiros: Ioachim's Lymph Node Pathology, 5th Edition, 2021
Board review style question #1
A 40 year old man presents with a right sided inguinal lymphadenopathy several weeks after a new sexual encounter. No monoclonal B cell or aberrant T cell populations are detected by flow cytometry. Histologic sections of a lymph node and an IHC stain are shown. Which of the following is most consistent with the timing, region and morphologic features of this process?
- Lymphogranuloma venereum
- New HIV infection
- Primary syphilis
- Secondary syphilis
- Tertiary syphilis
Board review style answer #1
D. Secondary syphilis. The findings are most suggestive of syphilitic lymphadenitis, which is associated with secondary syphilis. Answer B is incorrect because while this may overlap with an HIV infection, acute HIV will typically show robust follicular hyperplasia without increased capsular fibrosis and without identifiable organisms. Answer A is incorrect because lymphogranuloma venereum may show some overlapping features but typically shows more suppurative features. Overlapping conditions may occur and so clinical correlation and serologic studies are recommended. Answers C and E are incorrect because timing and clinical features described are not consistent with primary or tertiary syphilis.
Comment Here
Reference: Luetic lymphadenitis
Comment Here
Reference: Luetic lymphadenitis
Board review style question #2
Which morphologic feature is least characteristic of syphilitic (luetic) lymphadenitis?
- Ability to visualize organisms by special stains
- Acute inflammation with necrotizing granulomas
- Increased plasma cells
- Reactive follicular hyperplasia
- Thickened, fibrotic capsule
Board review style answer #2
B. Acute inflammation with necrotizing granulomas. Answers A and C - E are incorrect because syphilitic lymphadenitis is characterized by follicular hyperplasia, increased plasma cells, thickened fibrotic capsule and the ability to visualize organisms by silver stain or IHC for T. pallidum. Granulomatous inflammation can also be seen but necrotizing granulomas with acute inflammation are more characteristic of cat scratch lymphadenitis. Toxoplasma lymphadenitis may show follicular hyperplasia, epithelioid granulomas and increased monocytoid cells along vessels. Toxoplasma organisms are not usually well visualized by special stains in affected lymph nodes.
Comment Here
Reference: Luetic lymphadenitis
Comment Here
Reference: Luetic lymphadenitis