Table of Contents
Definition / general | Terminology | Embryology | Age related changes | Diagrams / tables | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy imagesCite this page: Sangle N, Pernick N. Anatomy & histology-lymph nodes. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodesanatomy.html. Accessed January 3rd, 2025.
Definition / general
- A secondary lymphoid organ, where B and T cells proliferate in response to exogenous antigen; primary lymphoid organs are bone marrow and thymus
- Other secondary lymphoid organs are spleen and Peyer patches
- Tertiary lymphoid organs are tissues with few lymphocytes that recruit more when inflammation is present
- Lymph nodes are organized to detect and inactivate foreign antigens present in lymph fluid that drains skin, GI tract and respiratory tract, the major organs in contact with the environment
Terminology
- Afferent lymph vessels:
- Penetrate capsule, enter marginal sinus, communicate with intranodal sinuses, then become efferent vessels, which lack an endothelial lining
- Intranodal vessels contain littoral cells or histiocytes with phagocytic properties
- Capsule:
- Thin fibrous connective tissue covering of lymph node
- May be thicker at hilus
- Connected to fibrous trabeculae which penetrate the node
- Capsule may contain smooth muscle cells (Anat Rec 1975;183:517)
- Cortex:
- Subcapsular portion of node with largest number of follicles (primary or secondary)
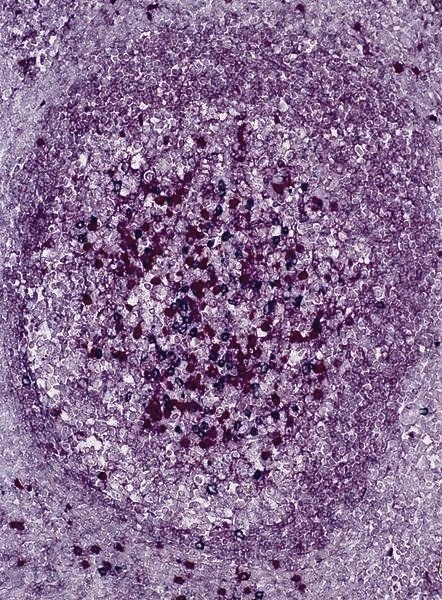
- Primary follicle:
- Round aggregates of small, dark staining inactive (naïve) B lymphocytes, usually near the capsule, within a network of follicular dendritic cell processes
- No germinal center present
- Secondary follicle:
- Arises from primary follicle that develops germinal centers (see below) due to antigenic stimulation of B cells and production of antibodies
- Contains pale staining germinal center which may be polarized towards site of antigen entry
- Surrounded by mantle zone and marginal zone lymphocytes
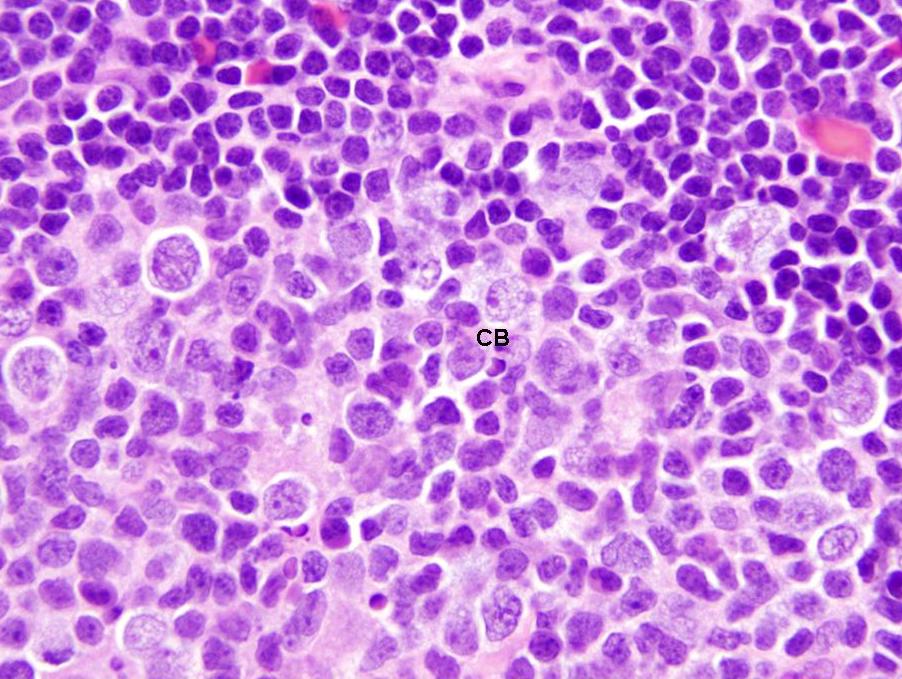
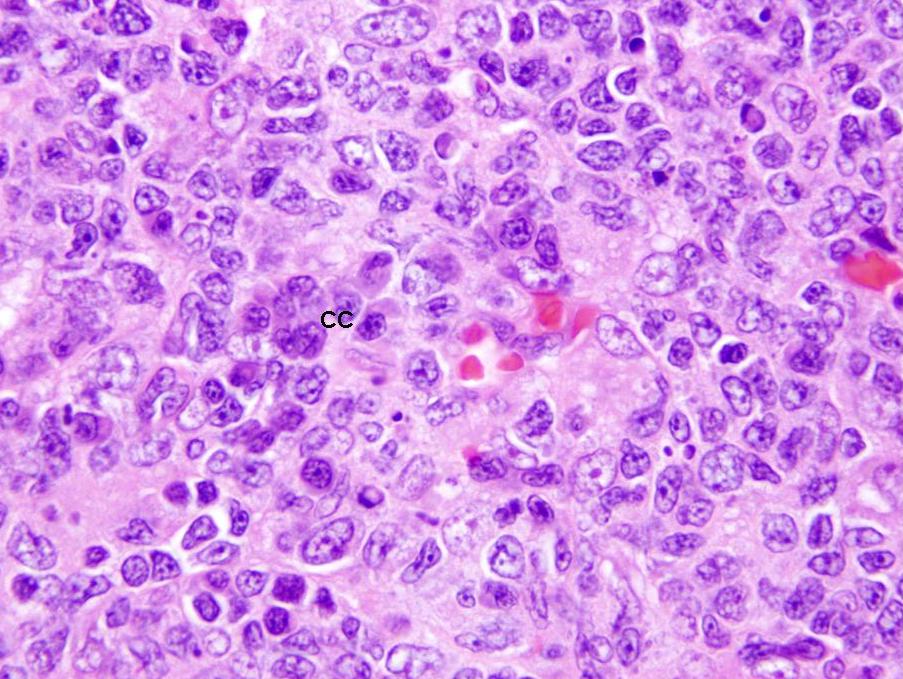
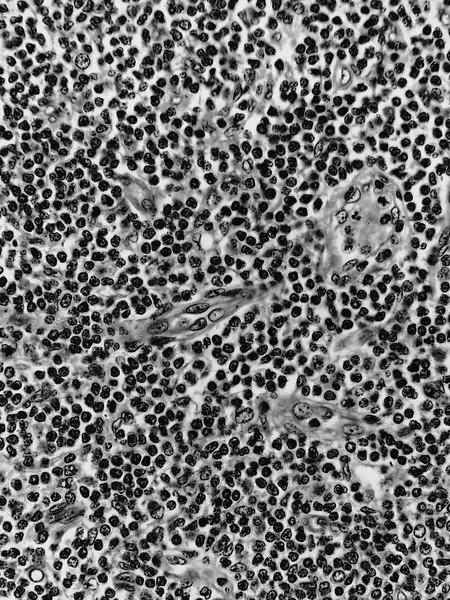
- Germinal center:
- Contains predominantly B lymphocytes (including centroblasts and centrocytes) and scattered follicular T helper cells and T regs
- Also tingible body macrophages and follicular dendritic cells
- Mantle zone:
- Tightly packed small B lymphocytes of the primary follicles, pushed aside by the germinal centers
- Marginal zone:
- Less packed small B lymphocytes with more cytoplasm
- Light zone on outer rim of mantle zone
- Contains a mix of post-follicular memory B cells derived after stimulation of recirculating cells from T cell dependent antigen and naïve B cells
- Often not well developed in lymph nodes
- Paracortex:
- Tissue between cortical follicles and medulla (see below)
- Contains predominantly dark staining mature T cells, B immunoblasts, interdigitating dendritic cells, plasmacytoid dendritic cells, histiocytes and high endothelial venules (postcapillary venules lined by plump endothelial cells that express leukocyte adhesion molecules and contain intraluminal lymphocytes)
- Expands during cell mediated immunological reactions
- Has coarse network of reticulin fibers
- Medulla:
- Portion of node closest to hilum
- Contains the medullary cords, sinuses and vessels but minimal number of follicles
- Medullary cords:
- Found in hilar region between the sinuses, composed mostly of small B and T lymphocytes, plasmacytoid lymphocytes, plasmablasts and plasma cells
- Sinuses:
- Carry lymph from afferent to efferent lymphatics
- Subcapsular sinus is below capsule and partially lined by endothelium
- Becomes "medullary" as it approaches the hilum and is lined by macrophages
- Also contains mast cells and plasma cells
- Vessels:
- Blood enters and leaves lymph node at hilus
Embryology
- Develop from lateral plate mesoderm (on either side of intermediate mesoderm)
- First, lymphatic sacs arise from endothelial outgrowths of large central veins at week 5
- Second, lymphatic plexus develops from lymphatic sacs
- Third, plexuses are invaded by mesenchymal cells that proliferate and aggregate to form lymph nodes
- Small collections of lymphoblasts are present by first trimester
- By second trimester, cortex is distinguishable from medulla and primary follicles are present
- References: Martini: Human Anatomy, 9th Edition, 2017
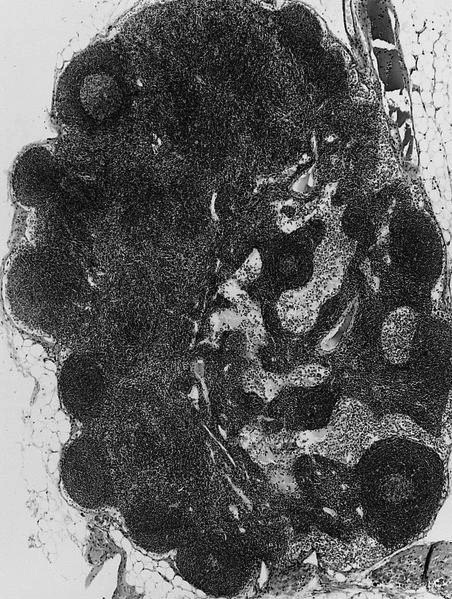
Gross description
- Ovoid with gray-tan cut surface
Microscopic (histologic) description
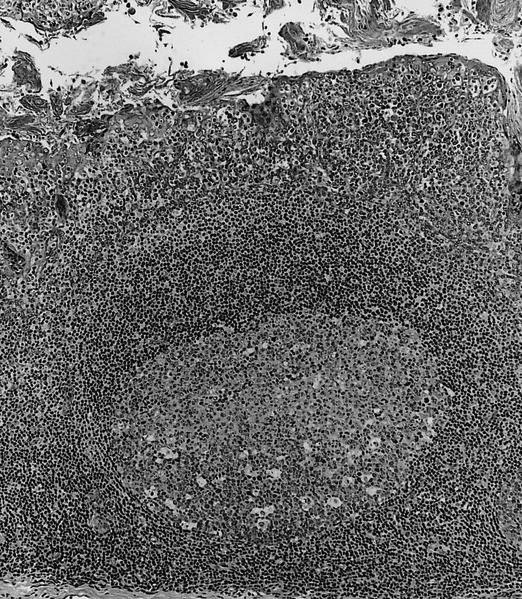
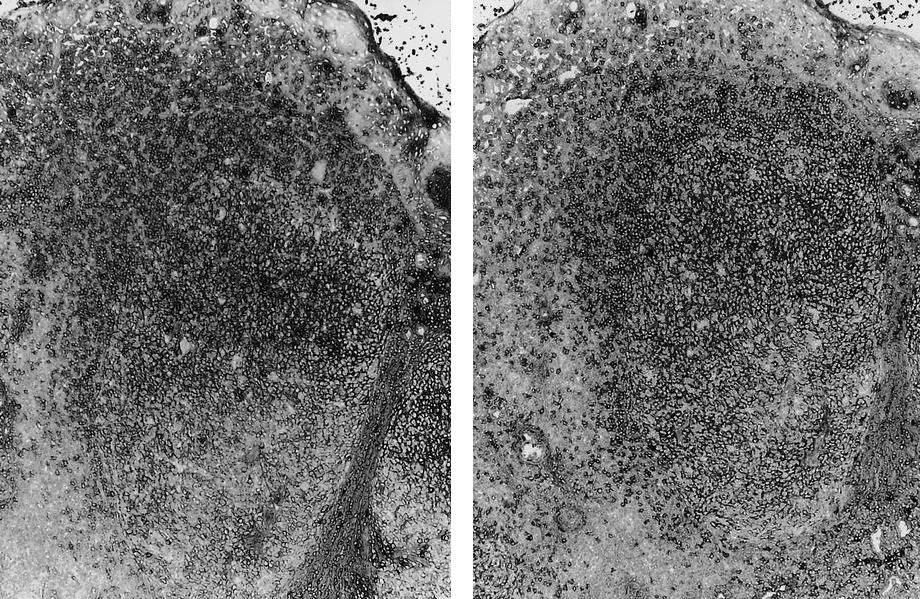
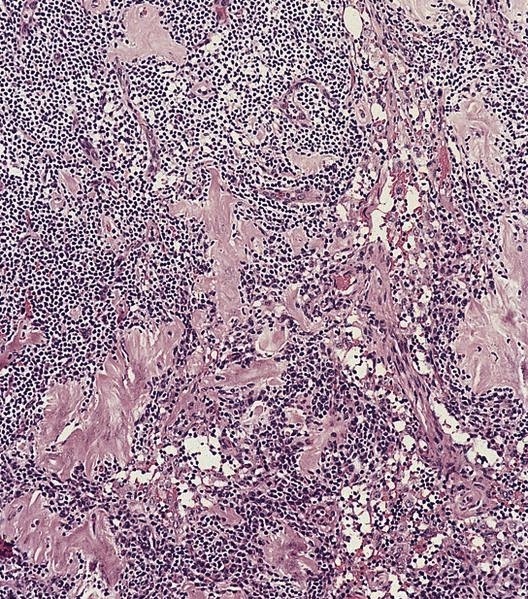
- At low power, lymph node structures are capsule, cortex and medulla, follicles, paracortex, sinuses
- Germinal center: round / oval zone containing pale staining cells, surrounded by darker cells
- Mantle zone: small unchallenged B cells surrounding pale staining germinal centers
- Marginal zone: light zone surrounding follicles; contains postfollicular memory B cells derived after stimulation of recirculating cells from T cell dependent antigen; named "marginal cells" due to location at interface of lymphoid white pulp and nonlymphoid red pulp in the spleen; however, marginal zone is rarely seen except in mesenteric nodes (APMIS 2002;110:325)
- Sinuses: direct the flow of lymph from the afferent lymphatics, to the subcapsular sinus, to the trabecular sinus, to the medullary sinus, to the efferent lymphatics (see diagrams) (Toxicol Pathol 2006;34:409)
- Centroblasts:
- Large noncleaved follicular center cells (B cells) with moderate amounts of basophilic cytoplasm, large round nuclei, open chromatin, multiple peripheral nucleoli
- Frequent mitotic figures
- Centrocytes:
- Large and small cleaved follicular center cells (B cells) with scant cytoplasm and inconspicuous nucleoli
- Immunoblasts:
- Large B cells scattered throughout the paracortex
- Intermediate between small B cell and a plasma cell
- Prominent single nucleoli
- Express B cell markers (CD20, CD79a, PAX5) and CD30
- Macrophages:
- Process antigens via phagocytosis
- Related to circulatory monocytes
- Are present throughout the lymph node
- May contain thyroglobulin in lymph nodes draining thyroid tumors (J Clin Pathol 2001;54:314)
- Abundant cytoplasm with medium to large nuclei with vesicular chromatin
- Tingible body macrophages have clear cytoplasm and contain apoptotic bodies, which gives node a starry sky pattern
- Mast cells:
- Present in T cell areas (World J Surg Oncol 2003;1:25)
- Difficult to detect
- Distinct cytoplasmic boundaries, faintly granular cytoplasm, large pale nuclei
- Some cells are elongated and resemble fibroblasts
- NK cells:
- Distinct group of non T, non B lymphocytes (5 - 10% of peripheral blood lymphocytes) with large granular lymphocyte morphology on Wright-Giemsa stains
- NK cells derive from a common lymphoid progenitor with T cells
- First line of defense against various infections, by recognizing and killing target cells and producing cytokines, particularly interferon-gamma, which enhance the innate immune response
- Capable of lysing certain target cells (virally infected and tumor cells) without prior activation or major histocompatibility complex restriction (hence named "natural killers" that are part of "innate" immune system) (Wikipedia: Natural killer cell [Accessed 26 March 2021])
- Do not rearrange their receptor genes, as B / T cells do but rely on a fixed number of NK cell receptors (inhibitory and activating) that recognize MHC class I and class I-like molecules and other ligands
- Appear to have capability for memory-like responses (EMBO Rep 2009;10:1103)
- Important for immunomodulation and regulation of hematopoiesis
- Plasma cells:
- Abundant basophilic cytoplasm (due to high content of rough endoplasmic reticulum) with paranuclear hof (highlighted by Giemsa stain, due to Golgi apparatus)
- Have eccentrically placed nucleus with spoke wheel (clock face) chromatin due to small clumps of chromatin on nuclear membrane in an otherwise round and clear nucleus
- May have Russell bodies (intracytoplasmic PAS+ globules)
Microscopic (histologic) images
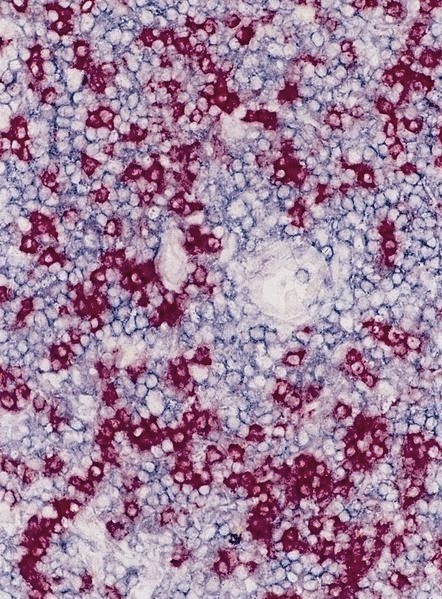
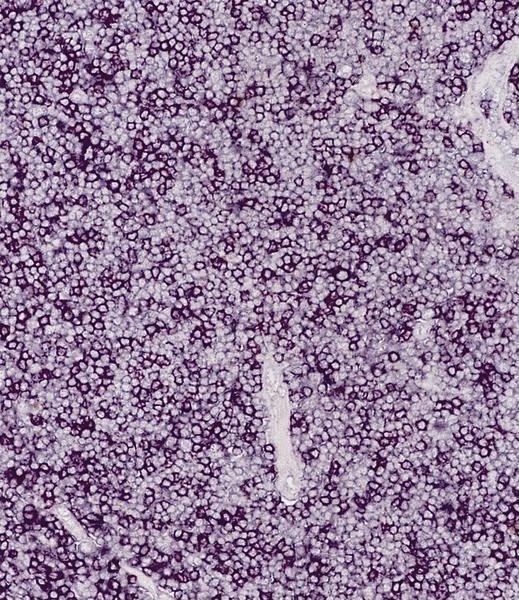
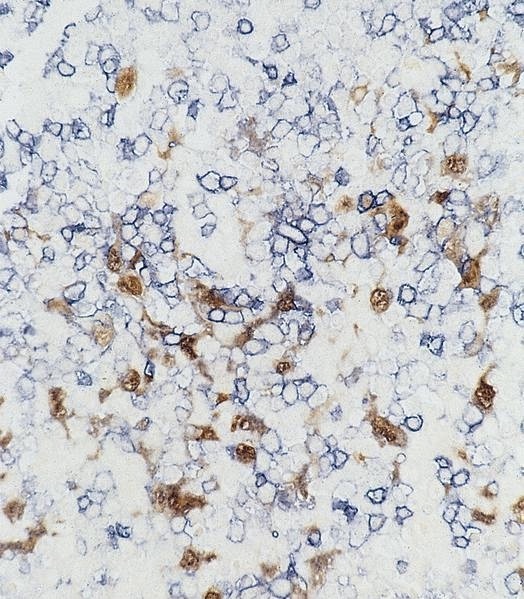
Positive stains
- B cells: CD19, CD20, CD22, CD79
- T cells: CD2, CD3, variable CD4 and CD8
- Follicular helper T cells: C3, CD4, CD57, PD1 or CD279
- T regs: CD4, CD25 and FOXP3
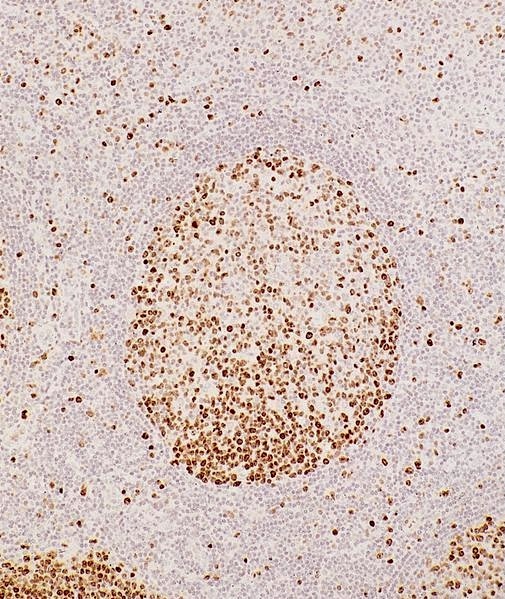
- Premature B and T cells: TdT (terminal deoxynucleotidyl transferase)
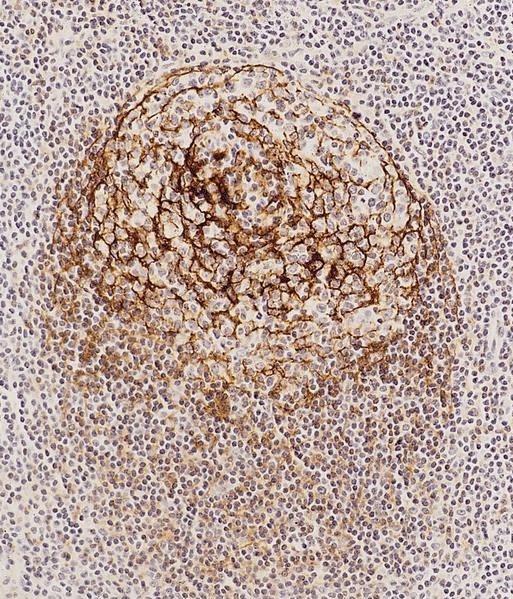
- Follicular dendritic cells: CD21, CD23, CD35
- Macrophages: CD68, lysozyme
- NK cells:
- Germinal centers have strong dense BCL6 and CD10 expression
Negative stains
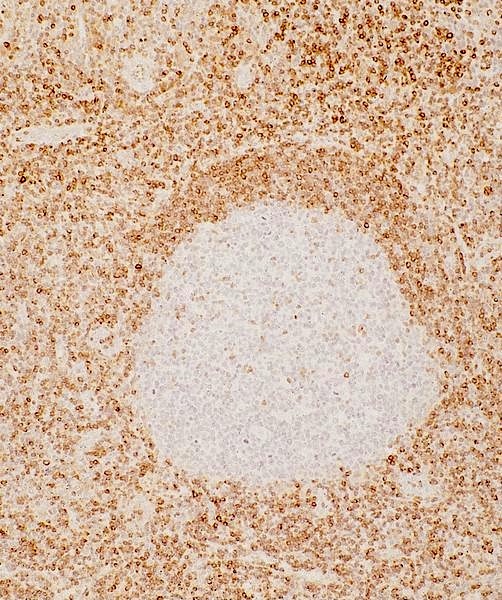
- bcl2 (not expressed in germinal center B lymphocytes)