Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Aqil B. HIV. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodeshiv.html. Accessed April 19th, 2024.
Definition / general
- Human immunodeficiency viruses (HIV) include HIV1 and HIV2, which belong to Lentivirus (a subgroup of retrovirus)
- HIV1 causes acquired immunodeficiency syndrome (AIDS), a condition characterized by progressive failure of the immune system leading to opportunistic infections and cancers (PLoS One 2016;11:e0162704)
- World Health Organization (WHO) defines advanced HIV disease as CD4 cell count < 0.2 x 109/L or patient has disease manifestations of WHO stage 3 or 4 in adults and adolescents (WHO: HIV and AIDS [Accessed 29 February 2024])
Essential features
- HIV infection is classified into different stages: 3 stages per The U.S. Centers for Disease Control and Prevention (CDC) and 4 stages per WHO
- Viral load and CD4+ T cell count is useful for disease follow up
- Per WHO, an estimated 39.0 million (33.1 - 45.7 million) people were living with HIV (LWH) at the end of 2022
- In 2022, estimated that 630,000 (480,000 - 880,000) people died from HIV related causes and 1.3 million (1.0 - 1.7 million) people acquired HIV (WHO)
ICD coding
Epidemiology
- HIV1 is the most common subtype and the most common subtype associated with AIDS throughout most of the world
- HIV2 is less common and is found mostly in Western Africa (J Gen Virol 2002;83:1253)
- Clinical AIDS defining conditions include some of the following (refer to the complete list in MMWR Recomm Rep 2014;63:1)
- Kaposi sarcoma
- Lymphomas: Burkitt, immunoblastic, CNS
- Cervical carcinoma, invasive
- Encephalopathy, HIV related
- Wasting syndrome, HIV related
- Recurrent pneumonia
- Opportunistic infections caused by the following: Candida, Cryptococcus, Cryptosporidium, Histoplasma, herpes simplex virus, Mycobacterium, Pneumocystis, Toxoplasma, etc.
- HIV infection has been classified into different stages per the CDC and WHO (MMWR Recomm Rep 2014;63:1, Virtual Mentor 2010;12:202)
CDC Stage 0 Negative HIV test within 6 months of the first HIV diagnosis and remains 0 until 6 months after diagnosis Stages Age specific CD4+ T cell testing < 1 year 1 - 5 years 6 years - adult Cells/µL % Cells/µL % Cells/µL % 1 ≥ 1,500 ≥ 34 ≥ 1,000 ≥ 30 ≥ 500 ≥ 26 2 750 - 1,499 26 - 33 500 - 999 22 - 29 200 - 499 14 - 25 3 < 750 > 26 < 500 < 22 < 200 < 14 Unknown stage CD4 test results are missing
WHO Stage 1 Asymptomatic or generalized lymphadenopathy of at least 2 sites for longer than 6 months Stage 2 Unexplained weight loss of < 10% of body weight and recurrent respiratory / skin infections Stage 3 Unexplained weight loss of > 10% of body weight, diarrhea (> 1 month), pulmonary tuberculosis (TB), mucocutaneous and systemic bacterial infections Stage 4 AIDS defining illnesses, HIV wasting syndrome, pneumocystis pneumonia, recurrent severe bacterial pneumonia, extrapulmonary TB, Kaposi sarcoma, CNS toxoplasmosis, HIV encephalopathy, others
Pathophysiology
- HIV is a spherical virus that attaches to the host cells with glycoproteins; the virus then integrates its chromosomal material into the host's cell, leading to generation of viral proteins and genetic material (StatPearls: Acquired Immune Deficiency Syndrome [Accessed 13 December 2023])
- Cells in the lymph nodes that are infected include monocytes, macrophages and follicular dendritic cells
- Progressive loss of CD4+ T cells occurs during the course of disease
- B cell activation during early disease leads to hypergammaglobulinemia, autoimmune phenomenons and later decreased antibody production
- Natural killer cell activity is also progressively decreased
Etiology
- There are 4 modes of acquiring HIV infection
- Sexual contact with an infected partner
- Parenteral drug use
- Exposure to infected blood or blood products
- Perinatal exposure
Clinical features
- Acute retroviral syndrome
- Headache, fever, rash, fatigue noted with initial HIV infection
- Occurs 1 - 3 weeks after infection and may last for 1 - 2 weeks
- Generalized lymphadenopathy
- Early / asymptomatic HIV disease
- Latency period that may last for years
- Advanced symptomatic HIV disease
- AIDS defining conditions
- References: World Health Organization: WHO Case Definitions of HIV for Surveillance and Revised Clinical Staging and Immunological Classification of HIV Related Disease in Adults and Children [Accessed 5 January 2024], MMWR Recomm Rep 2014;63:1
Diagnosis
- Screening test: performed on peripheral blood or body fluids
- Detection of antibodies to HIV glycoproteins by enzyme linked immunoassay (EIA) (J Infect Dis 2012;205:521, Curr Opin HIV AIDS 2012;7:125, J Infect Dis 2010;202:S270)
- Positive in about 2 - 4 weeks after infection
- Confirmatory tests: antibodies to HIV through enzyme linked immunoassay fourth generation (15 - 20 days from infection) or HIV viral load test cutoff 50 copies/mL (10 - 15 days) or ultrasensitive cutoff 1 - 5 copies/mL (5 days from infection)
- Latest recommendations: testing with immunoassay (both HIV1 and HIV2 antibodies) and p24 antigen
- Negative result: rules out infection within specific ranges of exposure and test sensitivity
- Positive result may have 4 scenarios
- HIV1+ & HIV2-: HIV1 antibodies present
- HIV1- & HIV2+: HIV2 antibodies present
- HIV1+ & HIV2+: both HIV1 and HIV2 antibodies present
- HIV1- or indeterminate & HIV2-: in this case nucleic acid test is done to identify the presence or absence of HIV1 acute infection
- Once tested positive, viral load and CD4+ T cell counts are performed (Internist (Berl) 2016;57:773)
Laboratory
- Anemia, neutropenia or thrombocytopenia
- If the white blood cell and lymphocyte counts are within the reference ranges, then the CD4 count is most likely normal
- If the absolute lymphocyte count is < 0.95 x 109/L, then a CD4 count < 0.2 x 109/L is likely (Acad Emerg Med 2011;18:385)
- Based on the symptoms and organ involvement, different tests are performed
- Complete metabolic profile: baseline renal and hepatic function
- EKG, cardiac biomarkers and echocardiography
- Chest radiography, computed tomography of chest
- Arterial blood gas analysis
- Testing for tuberculosis (TB)
- Esophagogastroduodenoscopy, colonoscopy
- Testing for ova, parasites, bacteria and C. difficile toxins
- Computed tomography of the head and lumbar puncture with cerebrospinal fluid (CSF) analysis
- Positron emission tomography (PET)
Radiology description
- Chest imaging: consolidation, ground glass opacity, cystic lesions, nodules and mass (AJR Am J Roentgenol 2012;198:1295)
- Brain imaging: ring enhancing lesions, encephalitis and mass (Jpn J Radiol 2021;39:1023)
- PET / CT: generalized lymphadenopathy, PET avid lesions in other organs
Prognostic factors
- Prognosis of adults with HIV or AIDS is now approaching that of the general population; however, it depends on the effectiveness of combination antiretroviral therapy (cART) (J Hosp Med 2015;10:608, JAMA 2008;300:51)
- Factors associated with poor prognosis from AIDS related conditions (Public Health Rep 2015;130:468, J Infect Dis 2009;199:991, J Int Assoc Physicians AIDS Care (Chic) 2011;10:5, HIV Clin Trials 2014;15:133)
- African American or mixed races
- Opportunistic infections
- Poor functional and nutritional status
- Anemia
- Substance abuse
- Low CD4+ count
- High HIV viral load
- Type of malignancy also plays an important role in overall survival and progression free survival
Case reports
- 25 year old man presented with sudden onset of psychotic symptoms associated with fever, cough and general asthenia (Front Immunol 2021:12:669723)
- 40 year old man was diagnosed HIV positive in 2008 but his viral load estimation every year since then had always been below lower detection limit and he remained healthy without treatment (Case Rep Infect Dis 2018:2018:5279595)
- 40 year old man with a history of HIV on cART presented with dyspnea and hypertension (SAGE Open Med Case Rep 2020:8:2050313X20965423)
- 46 year old man with HIV infection on cART presented with fever off and on, splenomegaly, lymphadenopathy and severe thrombocytopenia (Int J STD AIDS 2021;32:286)
- 78 year old woman of African descent from Mtwara Region, south of Tanzania presented for evaluation of leukopenia and anemia (J Med Case Rep 2021;15:341)
Treatment
- All individuals should be offered antiretroviral therapy (ART), regardless of the CD4 count or viral load
- Treatment results in sustained suppression of HIV RNA, improved cellular immunity (i.e., CD4 count), reduced HIV immune activation (e.g., proinflammatory cytokines, chronic inflammation and T cell activation) and decreased HIV transmission to others; however, access to care and treatment outcomes can differ depending upon demographic and psychosocial factors
- cART / ART: includes reverse transcriptase inhibitors (RTIs), integrase inhibitors (IIs) and protease inhibitors (PIs) (Br J Haematol 2001;112:900, AIDS 2014;28:881, Cold Spring Harb Perspect Med 2012;2:a007161)
- Latency reversing agents (LRAs): target the process of cell death via virus mediated cytolysis or immune associated clearance (Cell Host Microbe 2018;23:14, Nature 2012;487:482, PLoS Pathog 2014;10:e1004473)
- Gene therapy: works by inserting a healthy gene into the cells, which acts by repressing the mutant RNA or correcting the mutant gene (Einstein (Sao Paulo) 2017;15:369)
- Treatment of opportunistic infections and malignancies
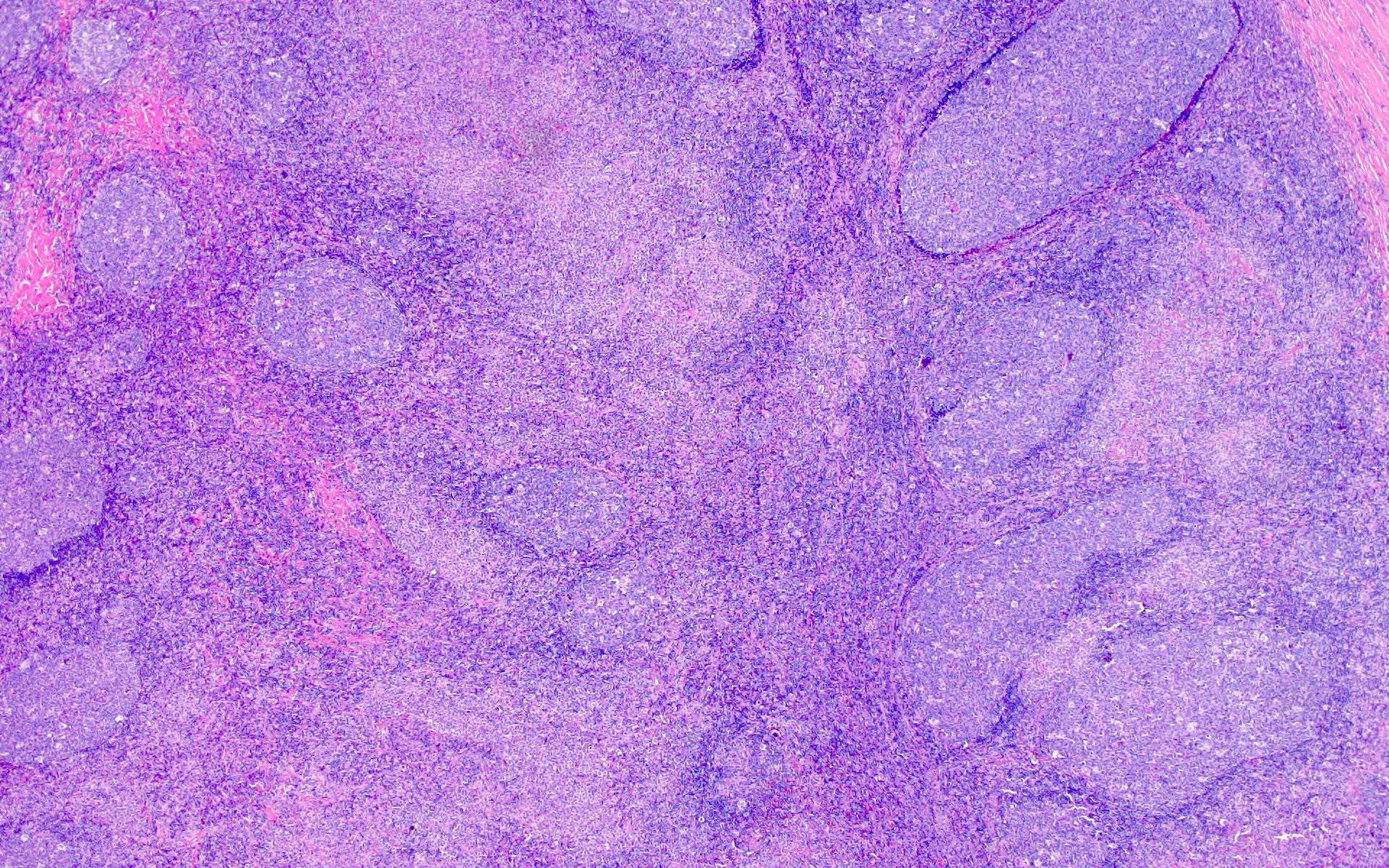
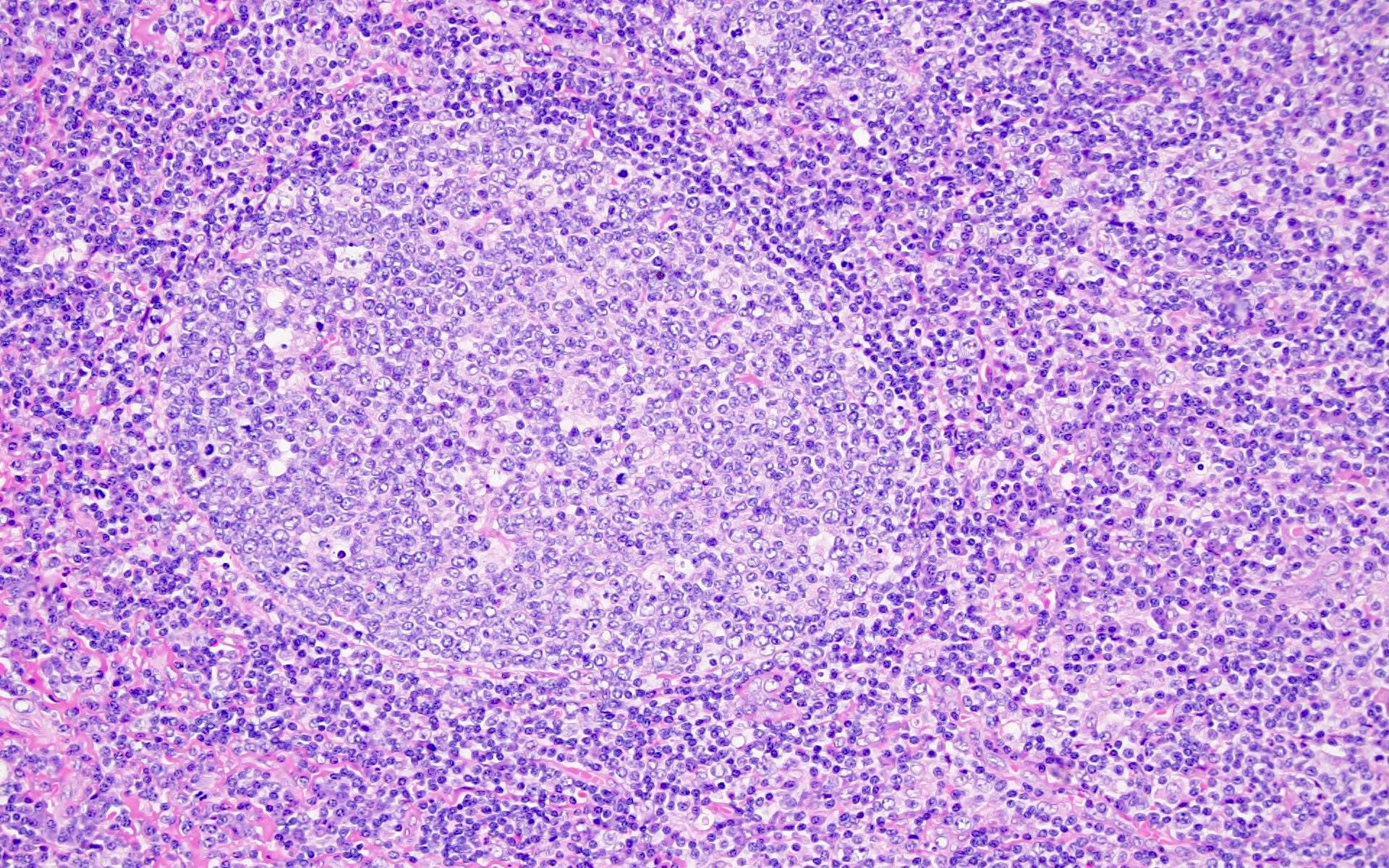
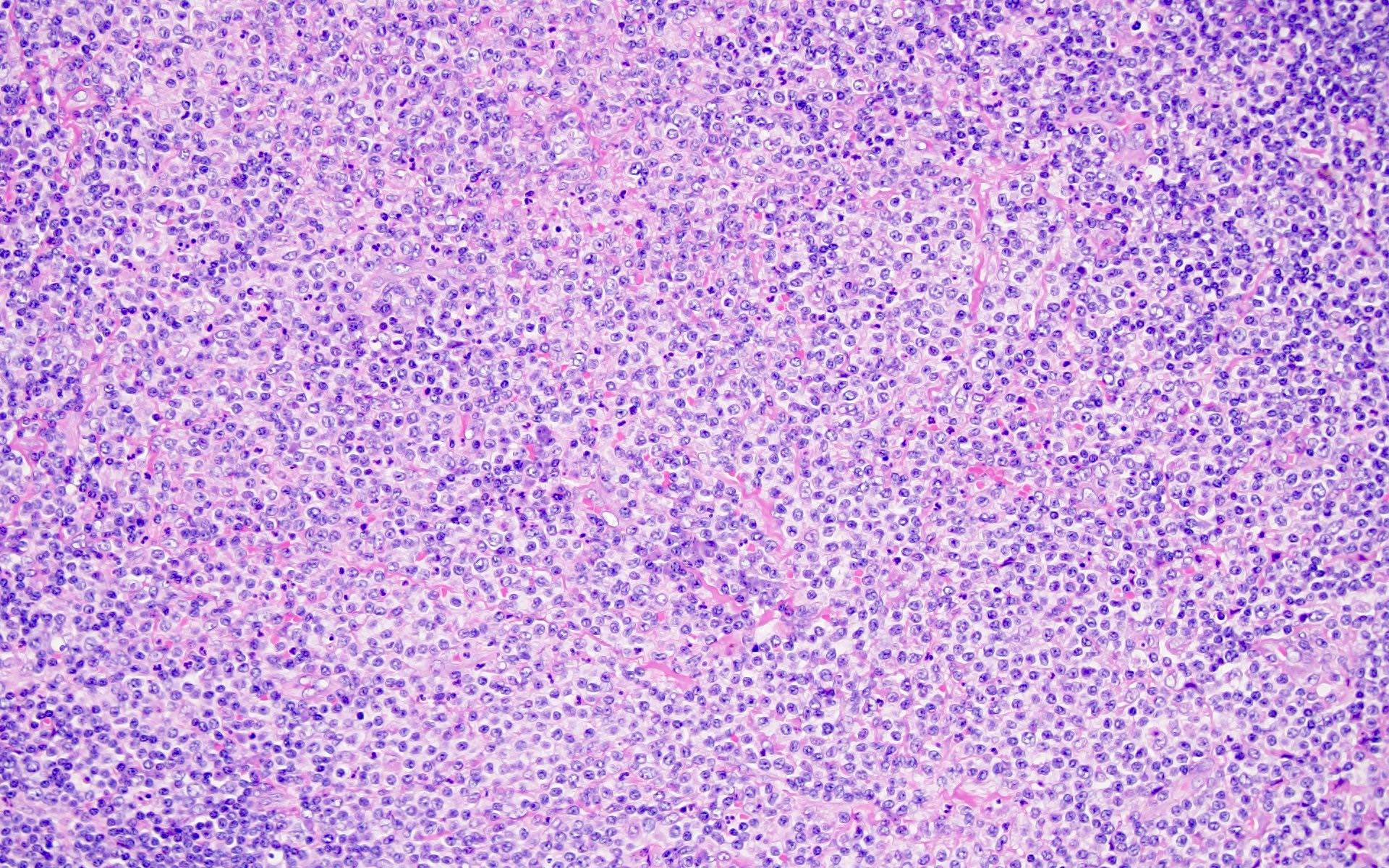
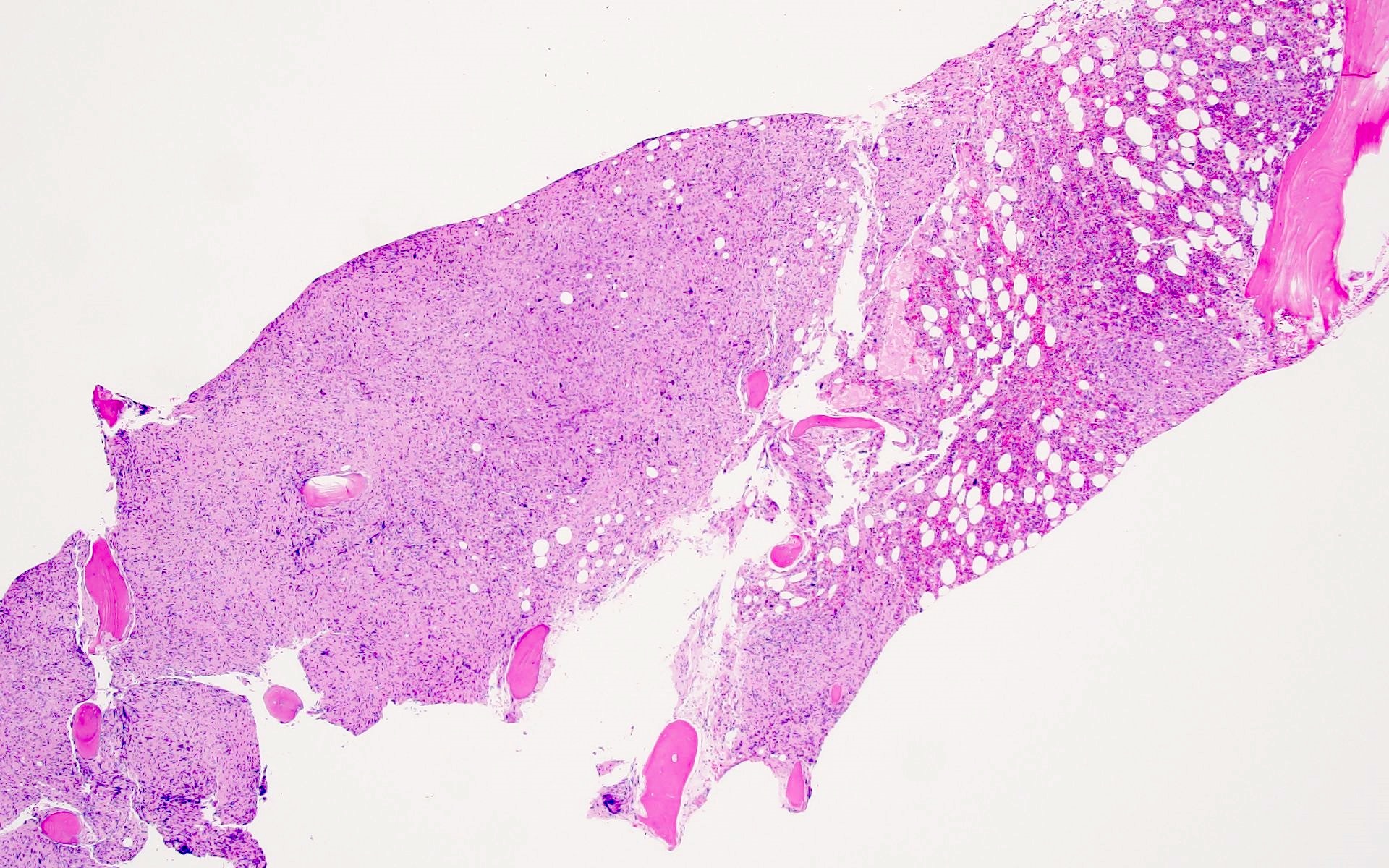
Microscopic (histologic) description
Reactive and opportunistic infection
KSHV / HHV8 associated multicentric Castleman disease
Polymorphic lymphoproliferative disorder arising in HIV
HIV associated lymphomas
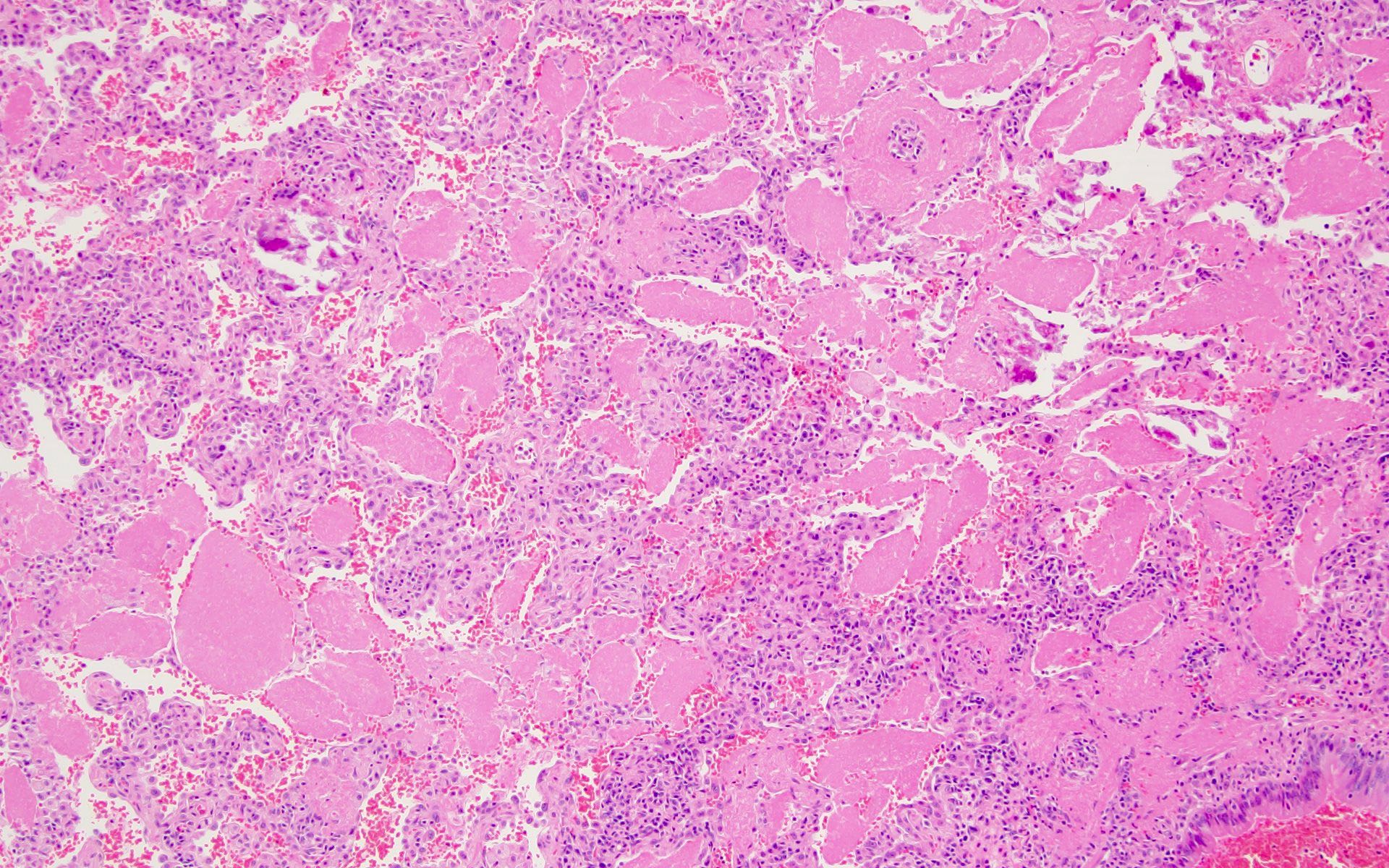
- HIV patients with CD4+ cell counts < 0.2 x 109/L, are prone to a wide variety of bacterial, viral, fungal and protozoal infections, which include
- Toxoplasma gondii, Pneumocystis jirovecii (previously Pneumocystis carinii), Cryptococcus neoformans, Mycobacterium avium, Mycobacterium tuberculosis, cytomegalovirus, herpes simplex viruses and Histoplasma capsulatum infections (StatPearls: HIV-1-Associated Opportunistic Infections [Accessed 13 December 2023])
- Pathological findings depend on the organ involved and the type of infection
- Most have lymphadenopathy, which includes florid follicular hyperplasia, paracortical hyperplasia, monocytoid B cell proliferation, granulomatous inflammation and necrosis
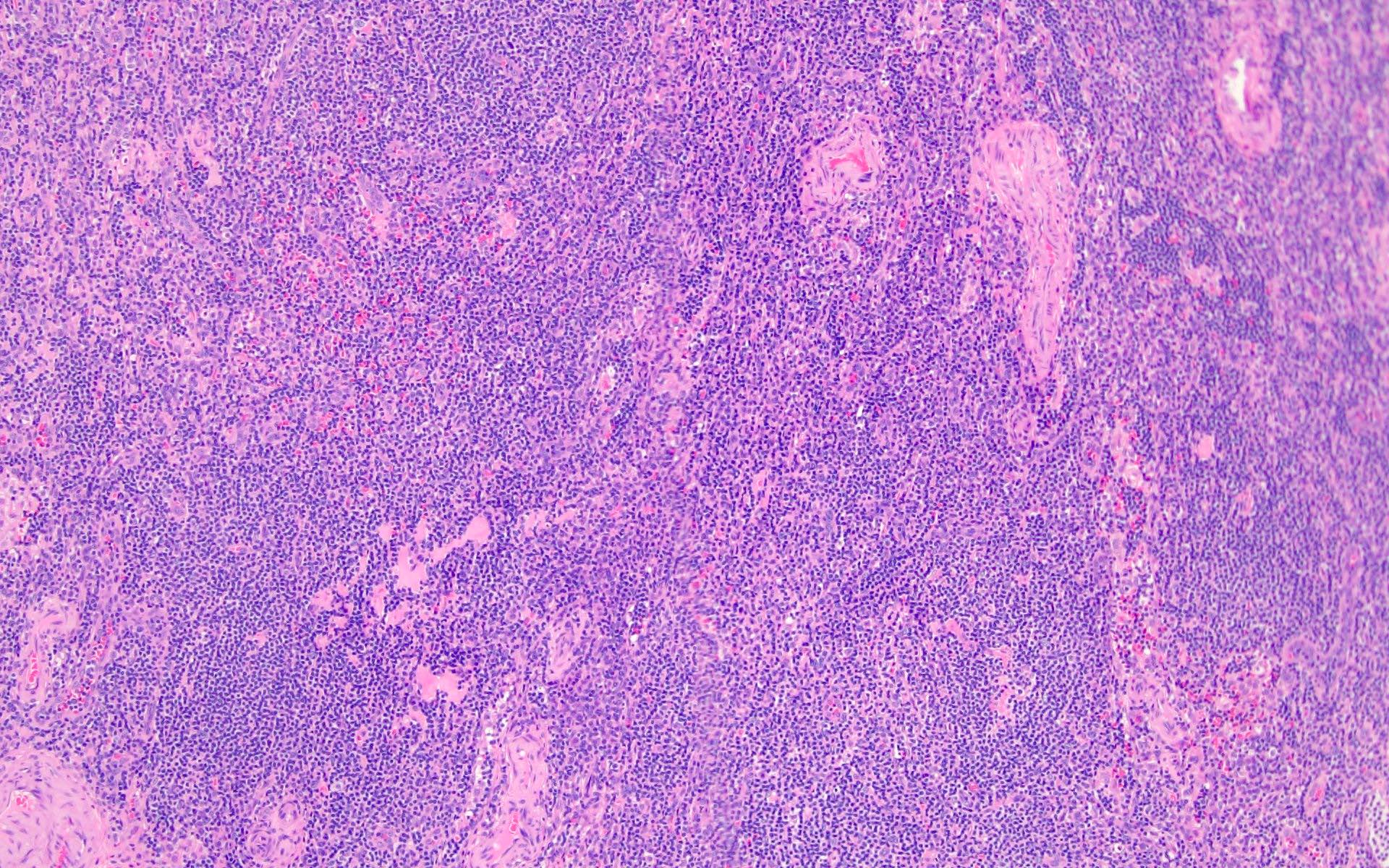
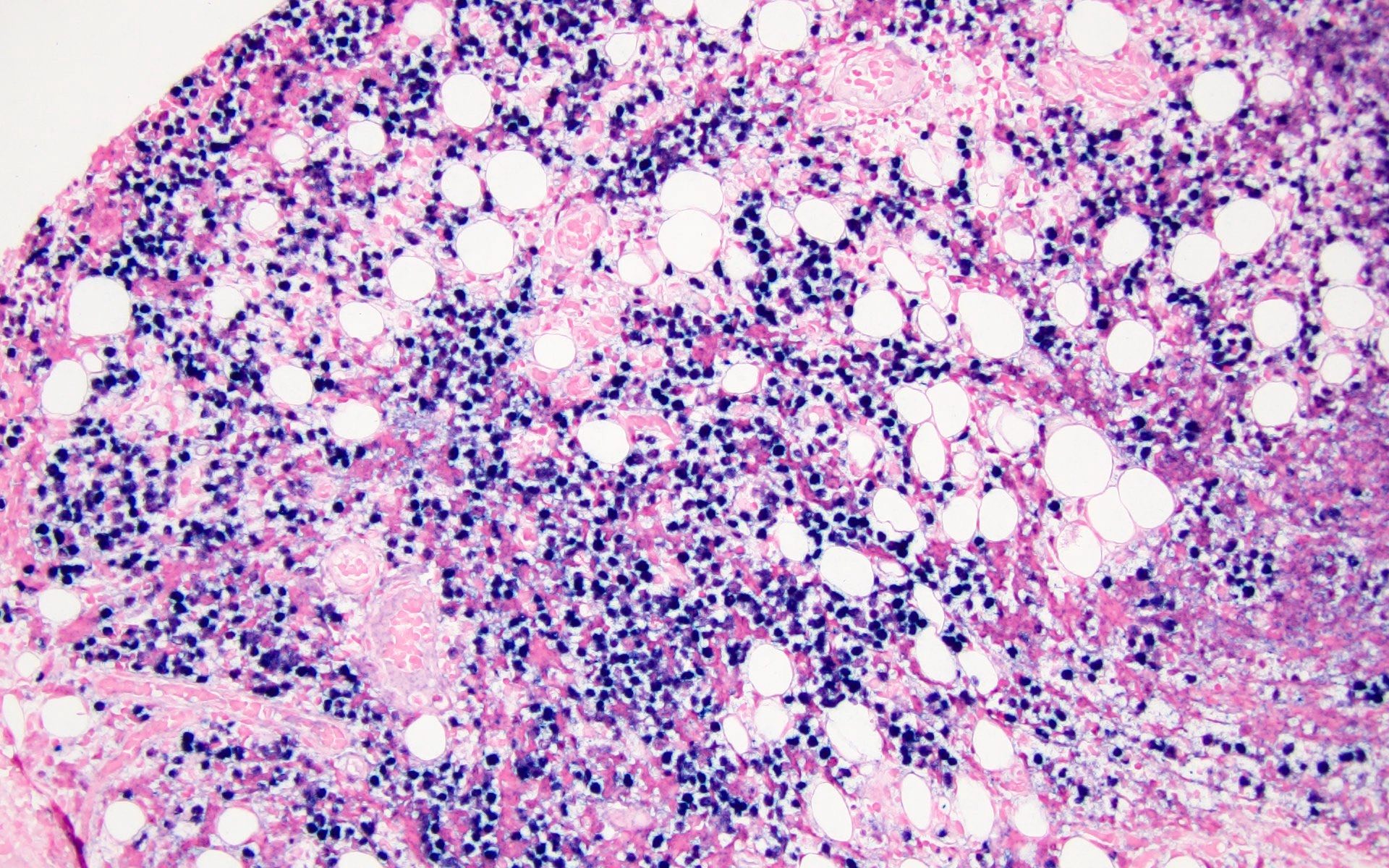
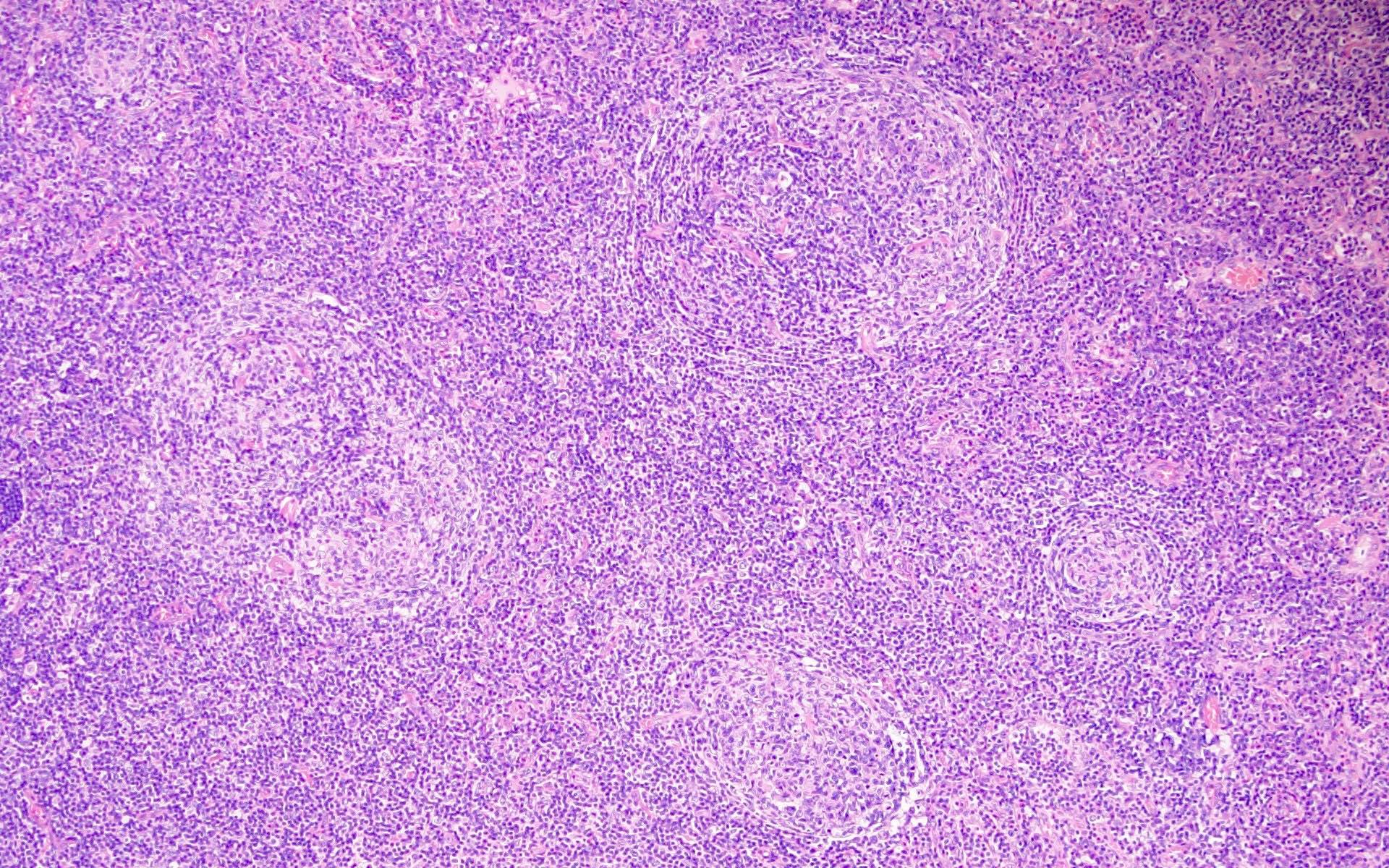
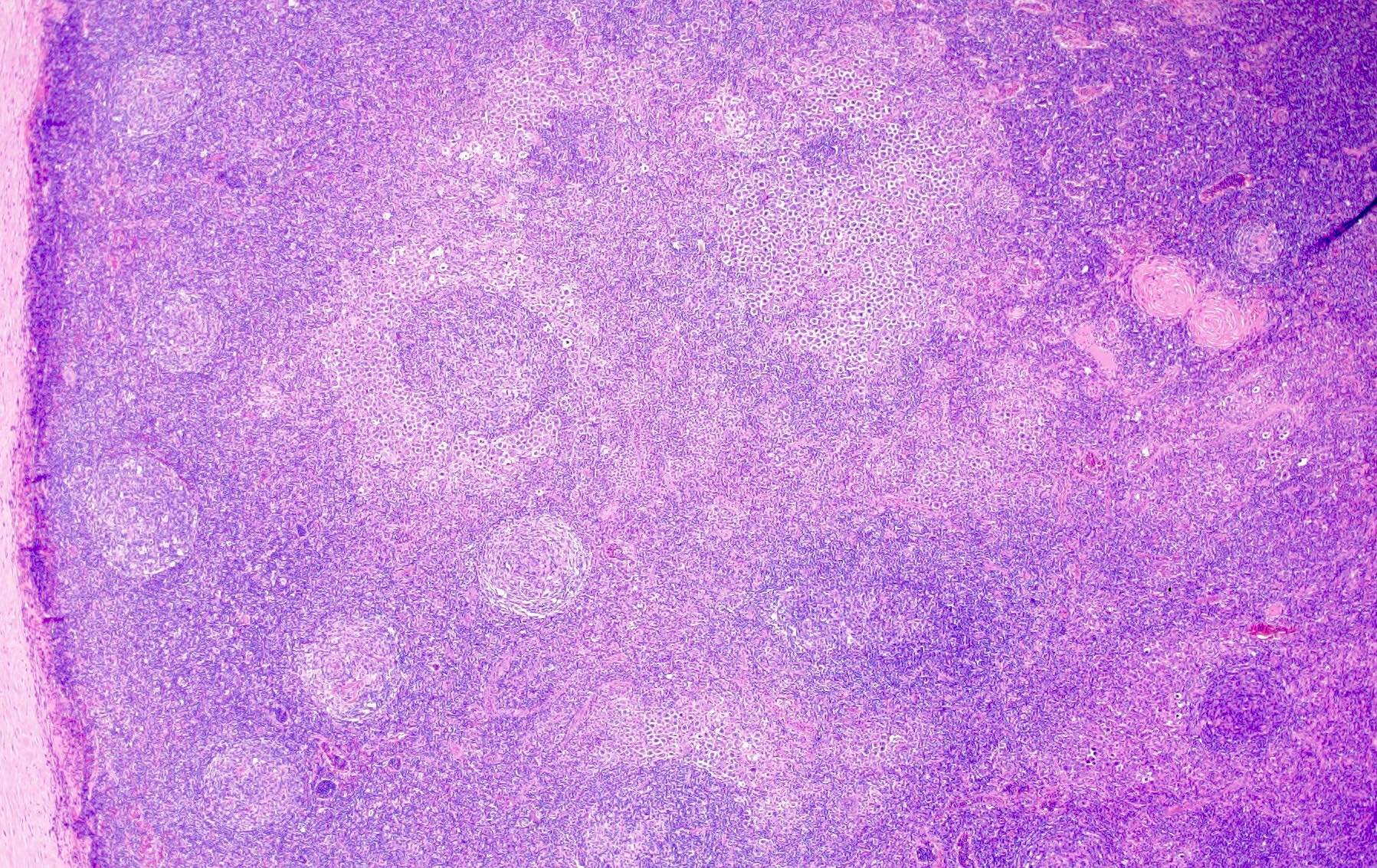
- HIV lymphadenitis has 3 histologic patterns, which correspond to clinical stages: acute, chronic and burnout (Medeiros: Ioachim's Lymph Node Pathology, 5th Edition, 2021)
- Pattern A
- Enlarged reactive follicles
- Hyperplastic germinal centers
- Diminished / absent mantle zones
- Folliculolysis - disruption of germinal centers by small lymphocytes
- Aggregates of monocytoid cells
- Pattern B
- Disruption of follicular dendritic cell meshwork
- Effacement of follicles
- Involution of germinal centers
- Increased plasma cells
- Depletion of lymphocytes
- Vascular proliferation
- Pattern C
- Atrophic follicles
- Hyalinized germinal centers
- Excessive plasma cells
- Marked loss of lymphocytes
- Fibrosis
- Pattern A
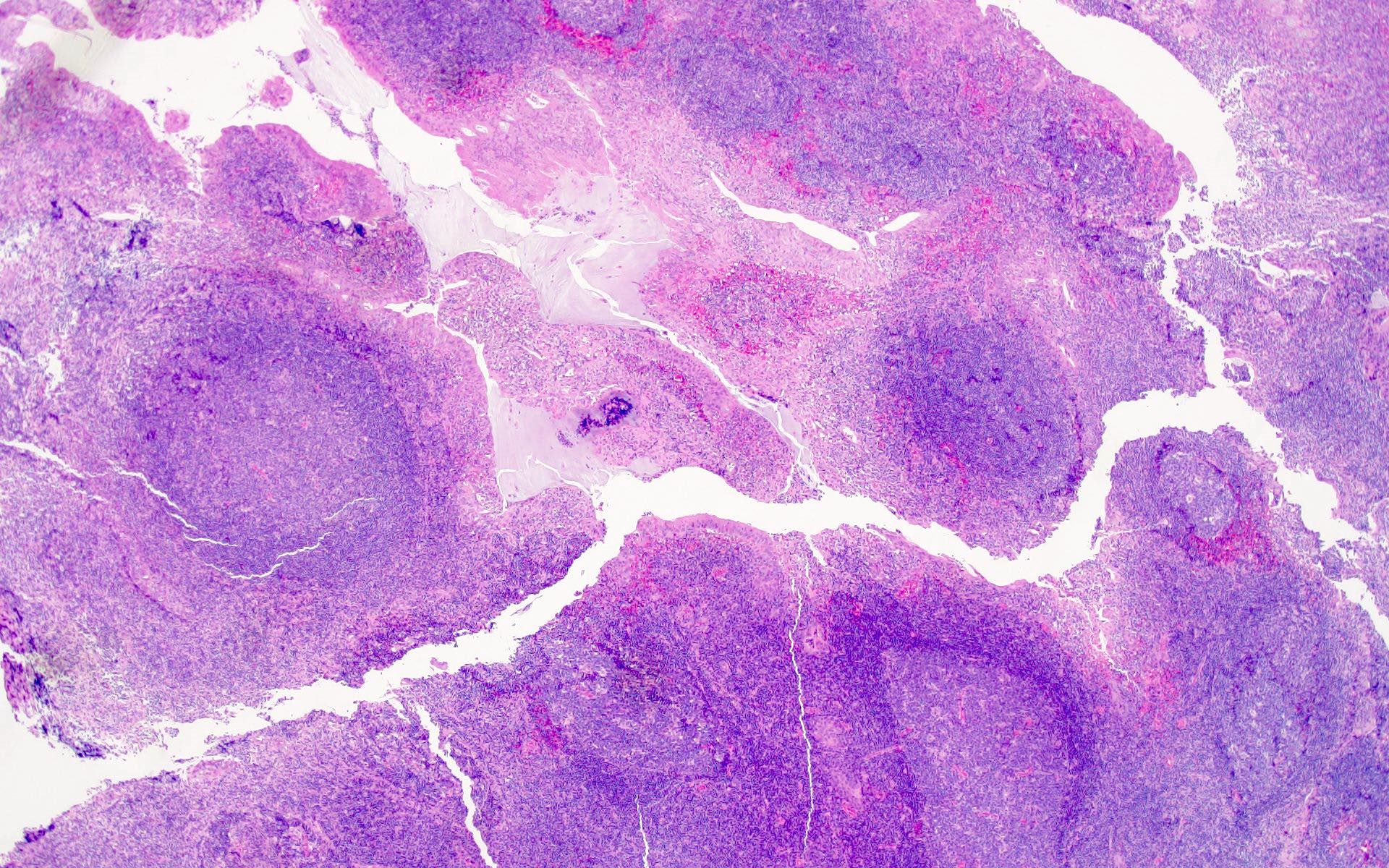
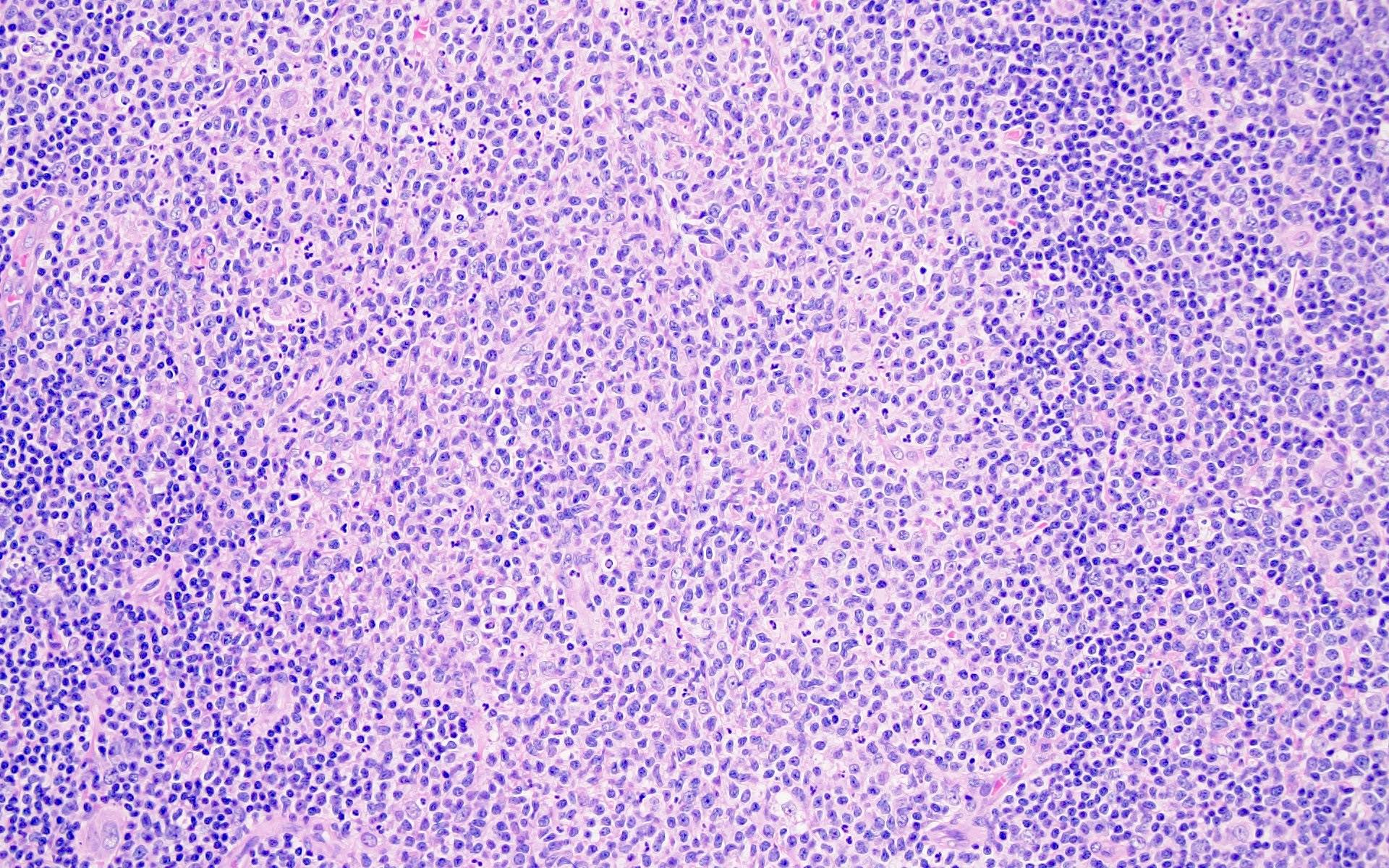
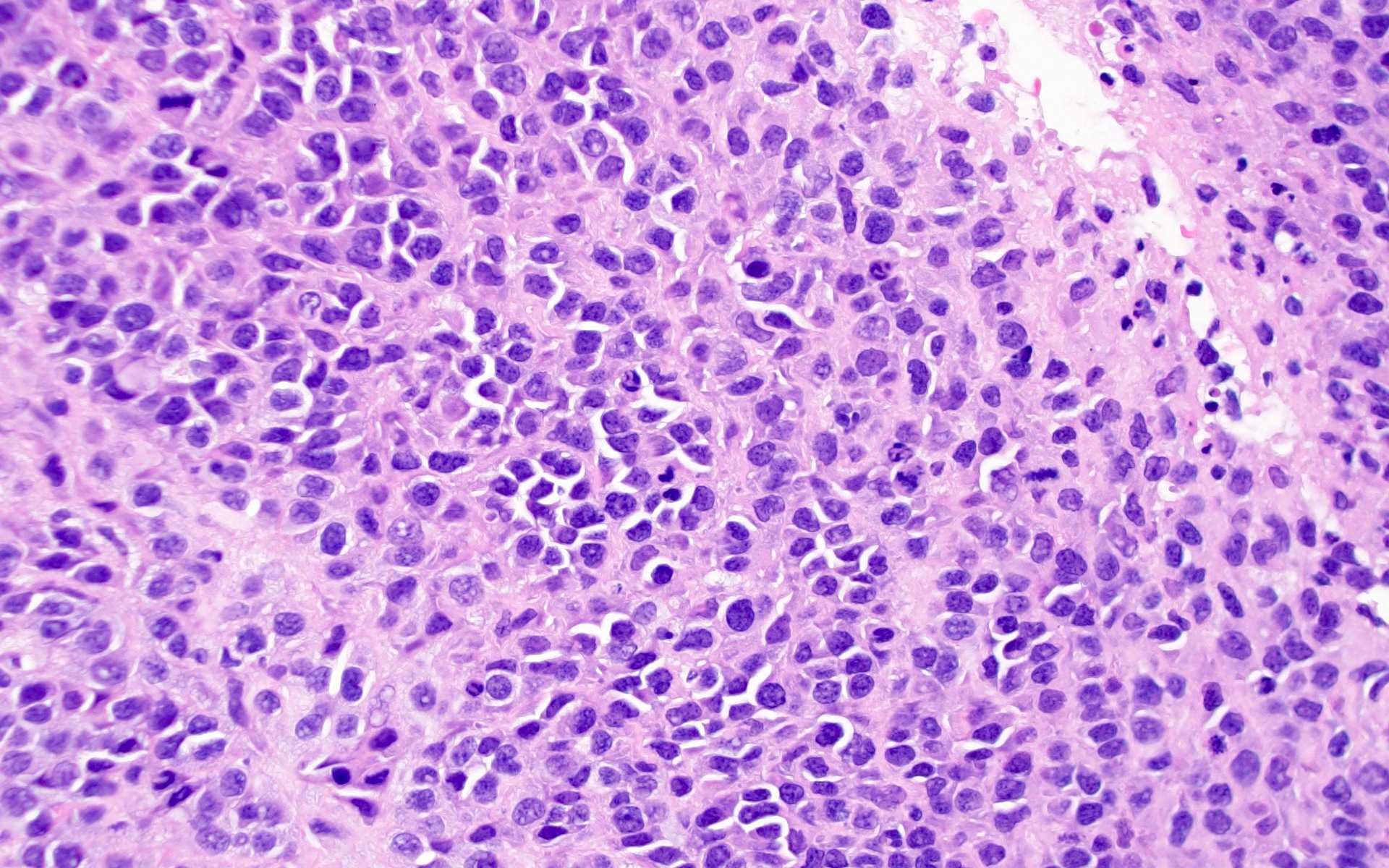
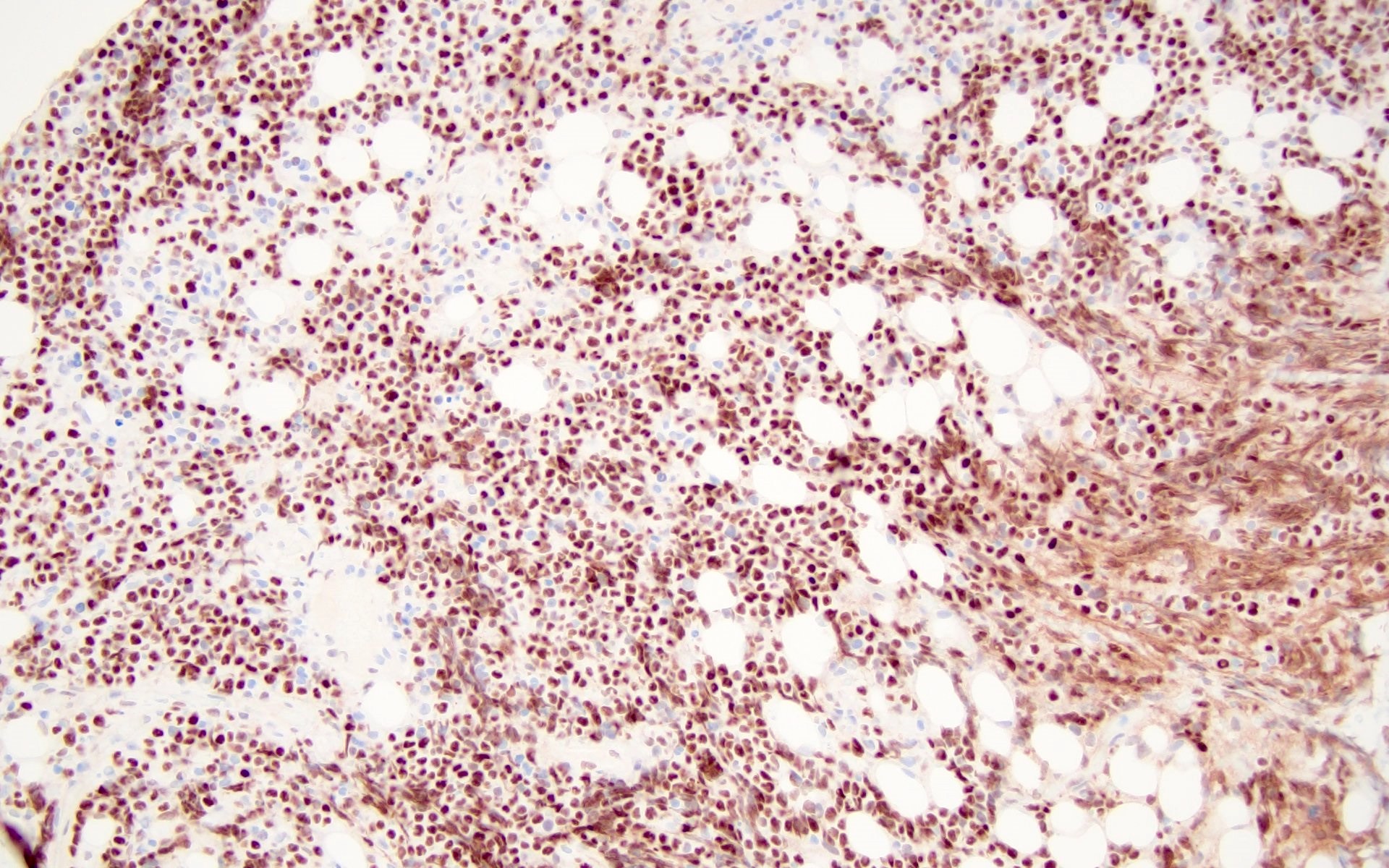
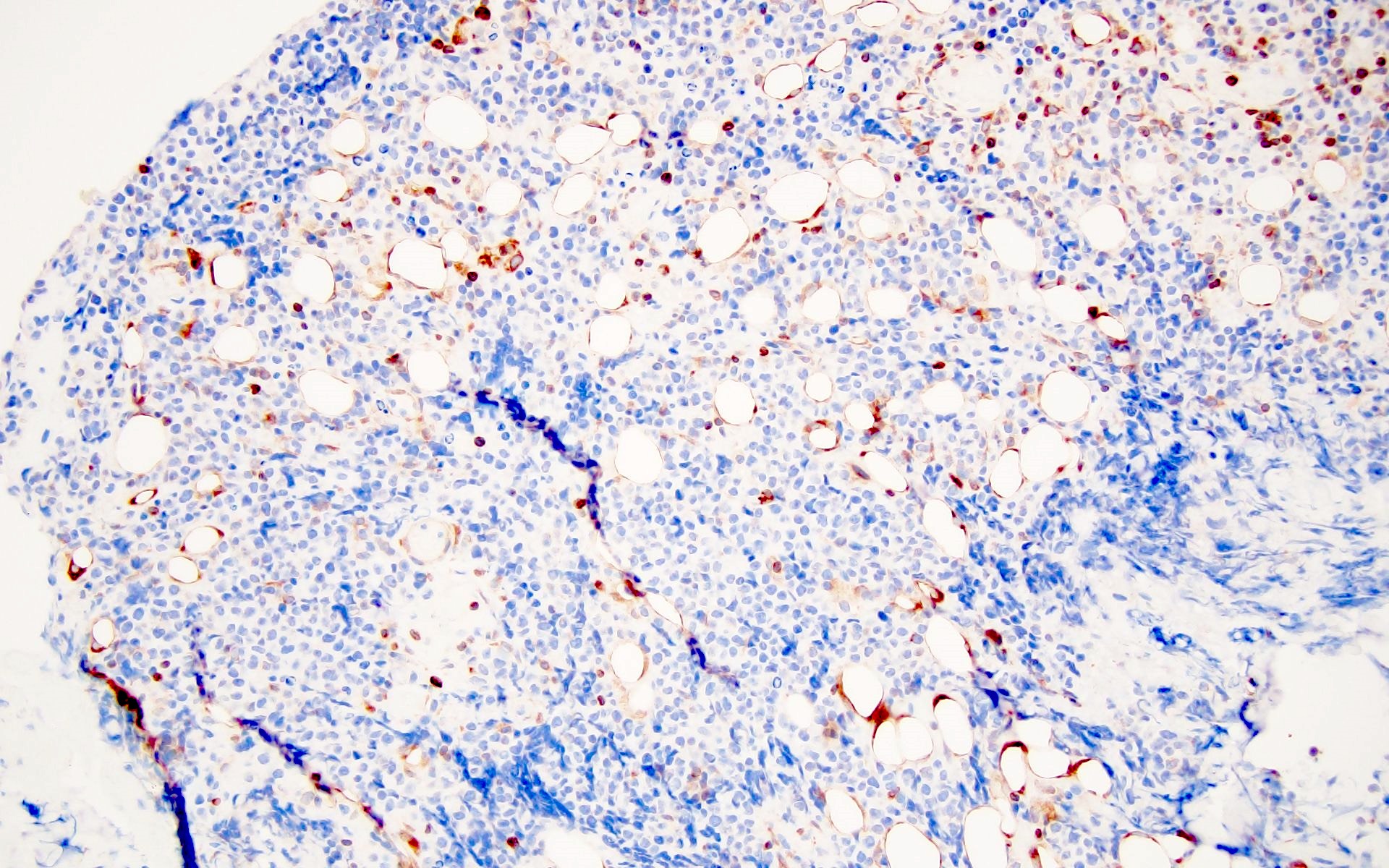
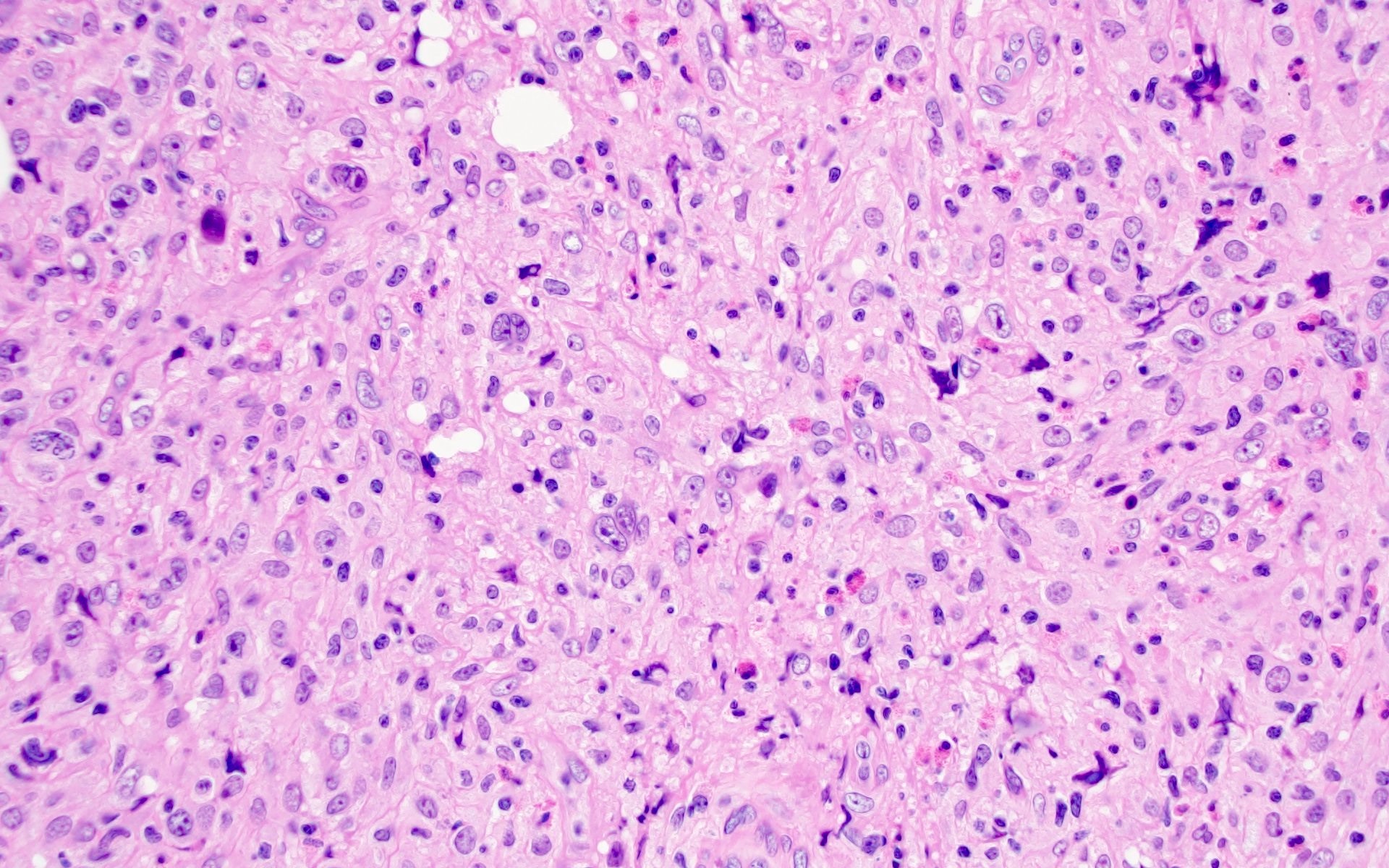
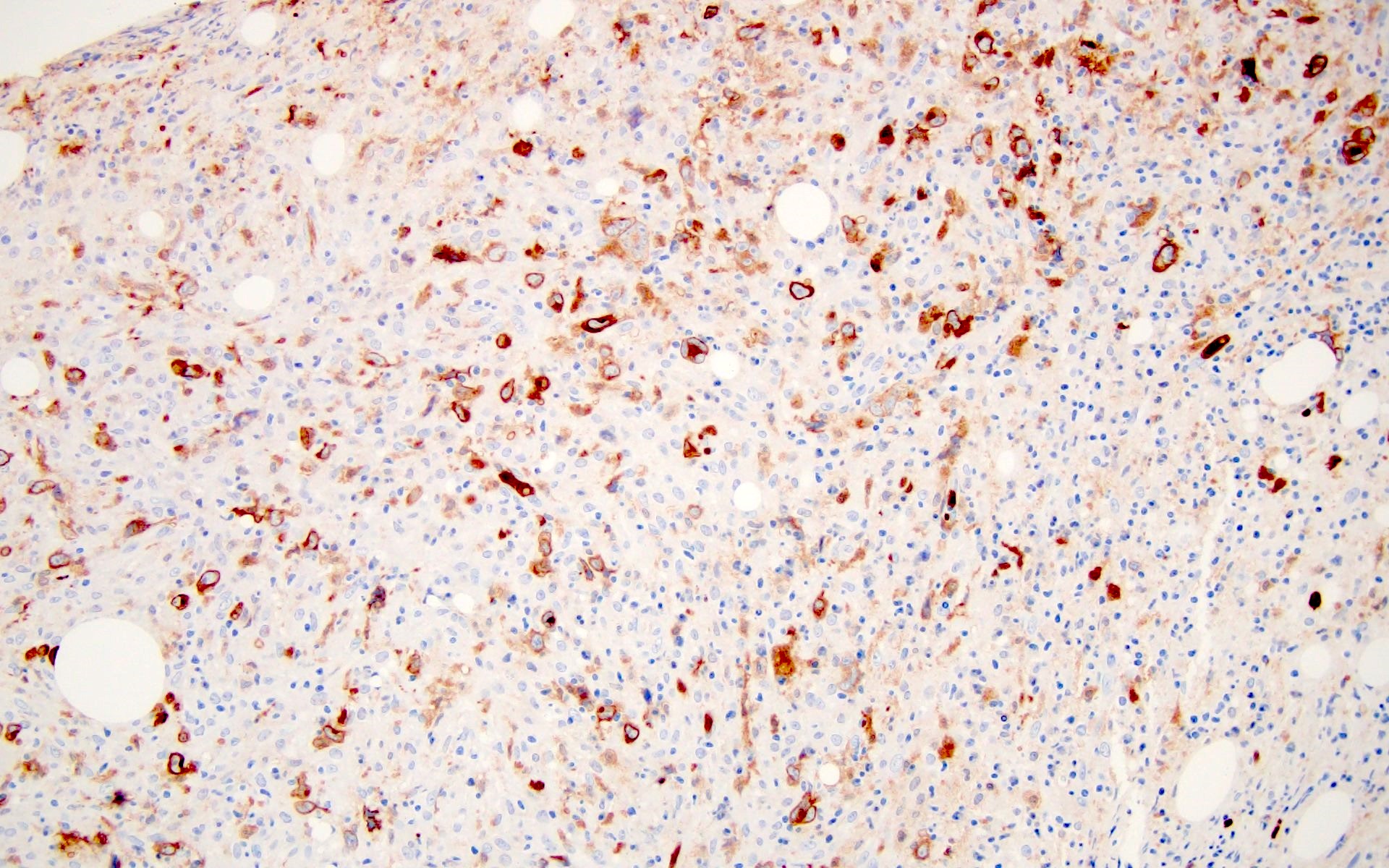
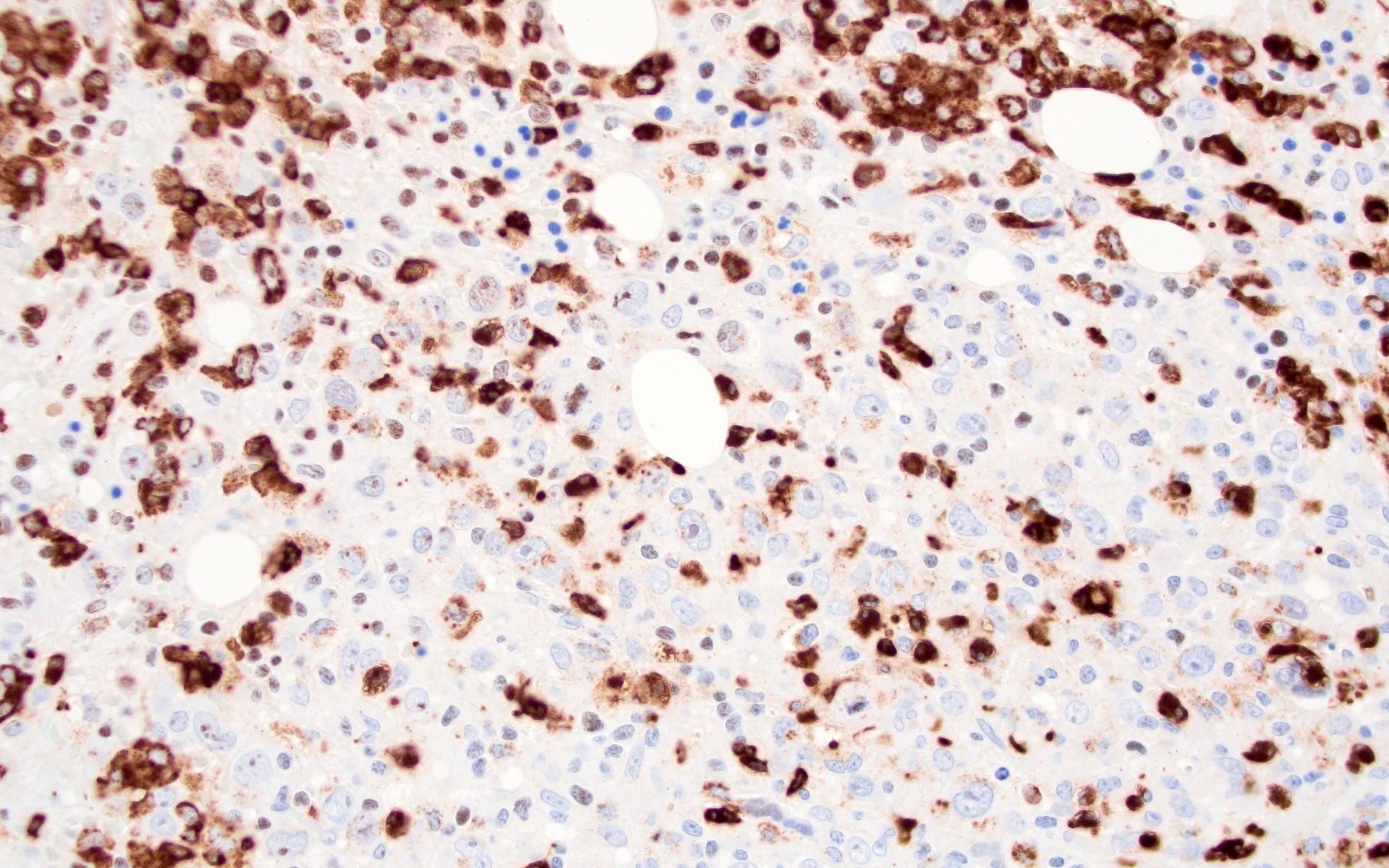
KSHV / HHV8 associated multicentric Castleman disease
- Associated with 80% of HIV+ patients (Neth J Med 2015;73:202)
- Seen in cases with low HIV viral load and median CD4 count (between 0.15 and 0.3 x 109 cells) (J Clin Oncol 2011;29:2481, Blood 2011;118:3499, Blood 2013;122:4189)
- Predominantly lymphadenopathy is noted with classic features
- Regressed follicles along with plasmacytosis
- Presence of plasmablasts in the mantle zones, which are medium to large cells with 1 - 2 nucleoli and a moderate amount of amphophilic cytoplasm
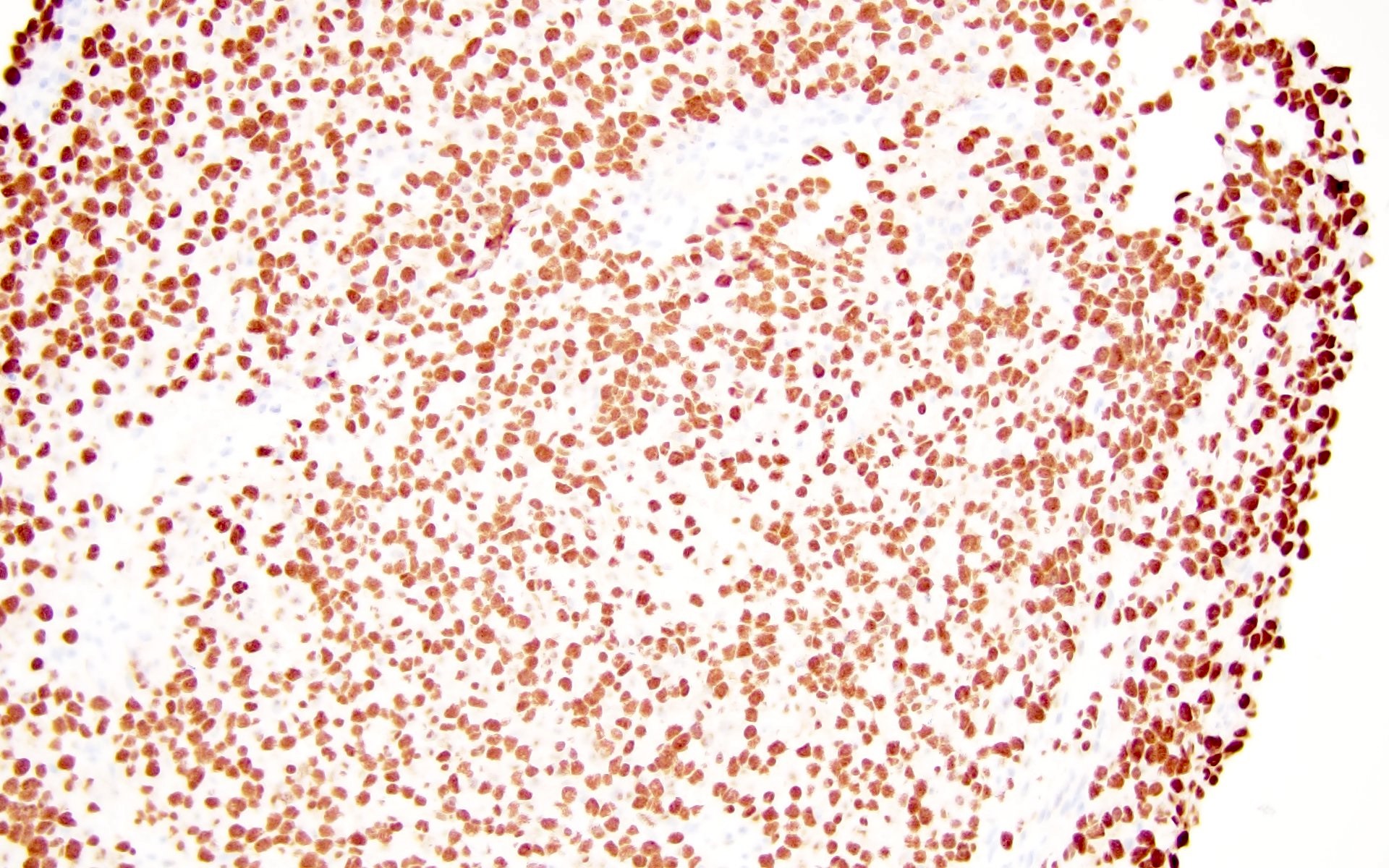
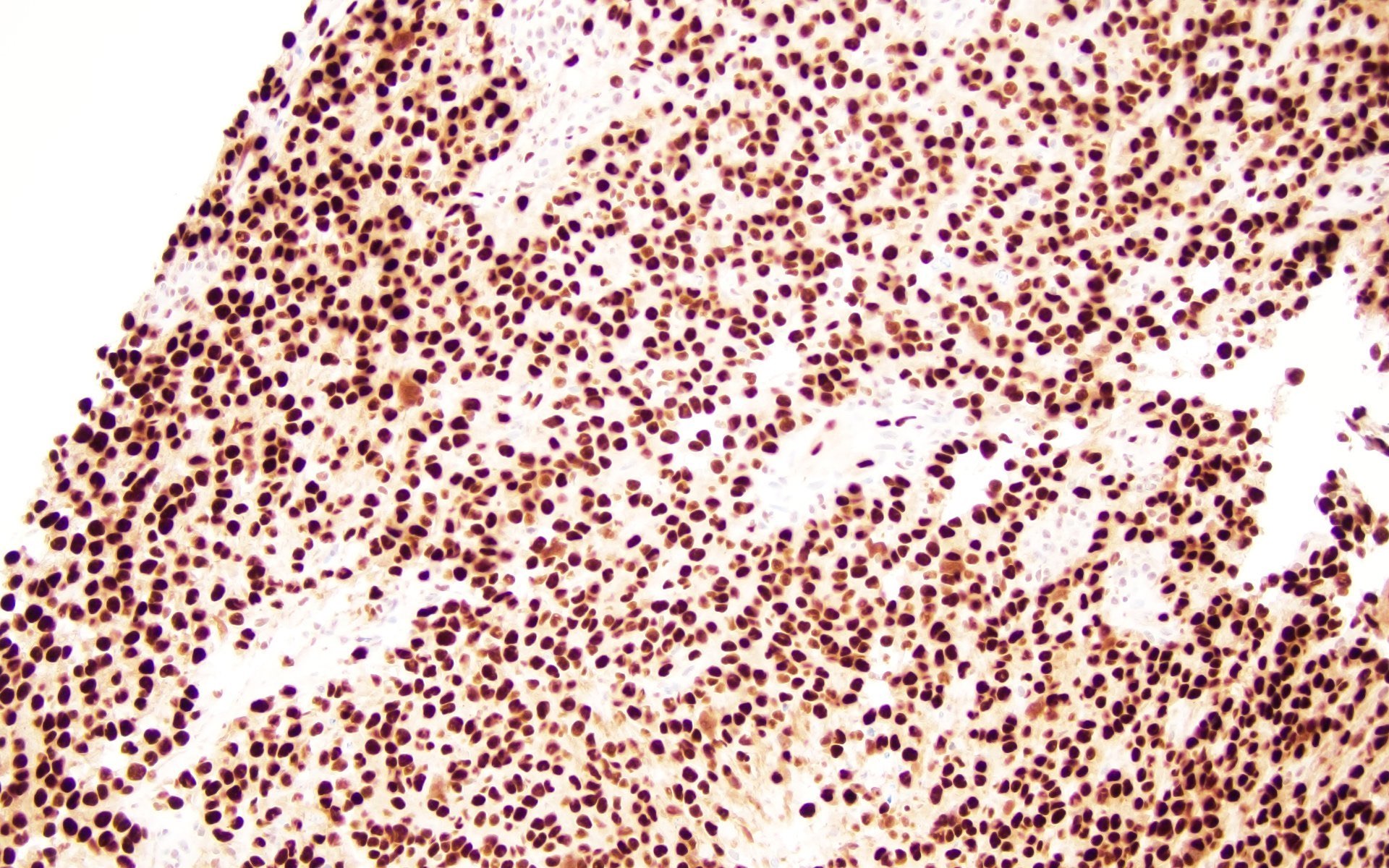
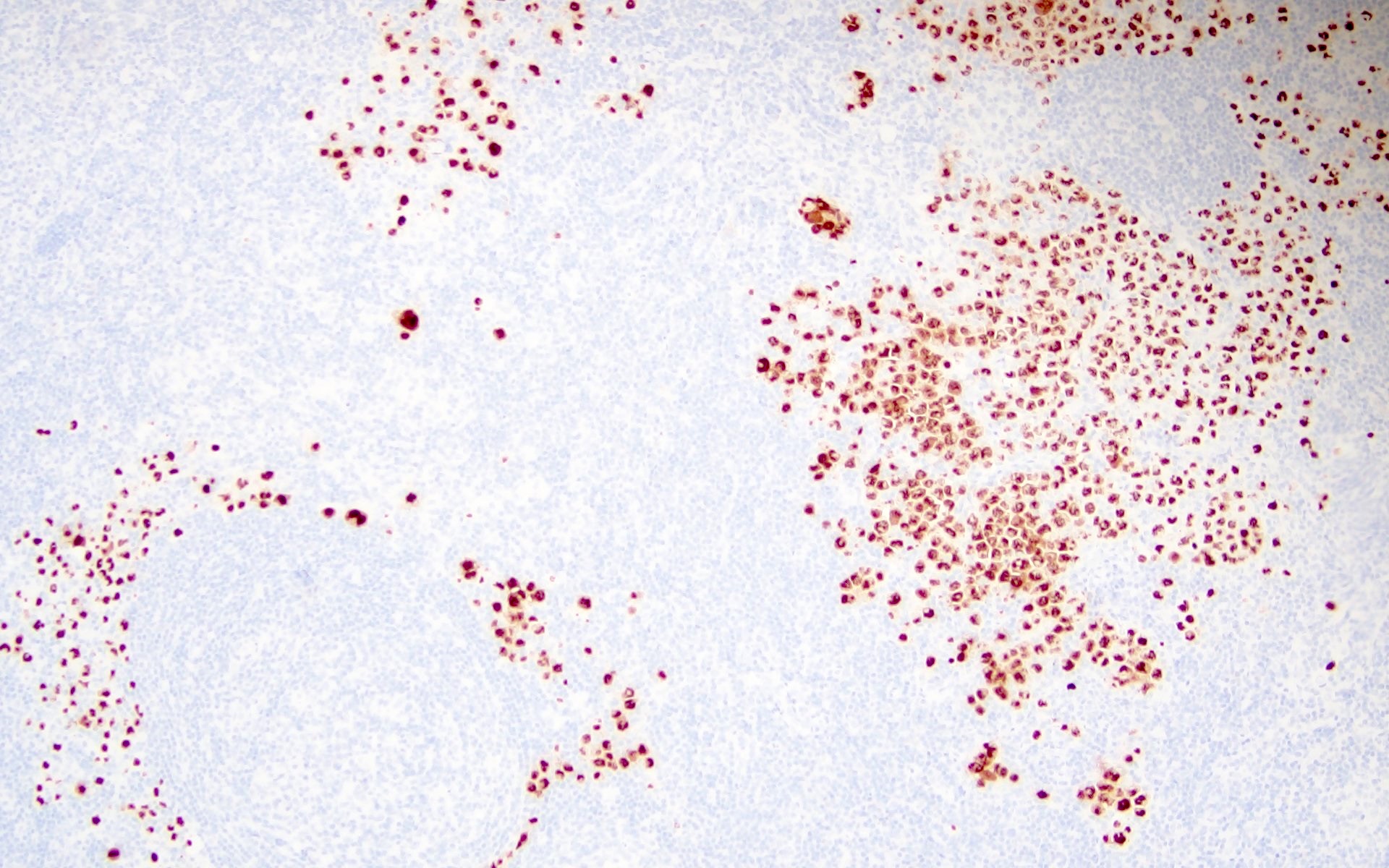
- Plasmablasts display negative to dim levels of CD20, positive expression for MUM1 and latency associated nuclear antigen (LANA) (a gene product of KSHV / HHV8 ORF73) and express cytoplasmic IgM lambda (Histopathology 2008;53:513, Blood 2001;97:2130)
- Foci of Kaposi sarcoma may be seen (Blood 2000;95:1406, Am J Pathol 1997;151:1517, AIDS Rev 2008;10:25)
- Increased risk of developing lymphoma
Polymorphic lymphoproliferative disorder arising in HIV
- Incidence in HIV is < 5% (Am J Surg Pathol 2003;27:293, Virchows Arch 2012;461:93)
- Architectural distortion by polymorphous infiltrate consisting of spectrum of B cells, including small lymphocytes, plasmacytoid cells, plasmablasts and immunoblasts along with T cells and histiocytes
- May have Reed-Sternberg-like cells
- Epstein-Barr virus (EBV) expression seen in both small and large cells
- Responds well to cART
HIV associated lymphomas
- Lymphomas arising in HIV+ patients now are classified under lymphomas arising in immune deficiency / dysregulation per 2022, WHO classification
- HIV+ patients present with advanced clinical stage, bulky disease with a high tumor burden
- Lymphomas arising in HIV+ patients include the following
- B cell lymphomas
- Diffuse large B cell lymphoma (DLBCL)
- Burkitt lymphoma
- Extranodal marginal zone lymphoma
- Primary effusion lymphoma
- Plasmablastic lymphoma
- KSHV / HHV8 positive diffuse large B cell lymphoma
- T cell lymphomas
- Peripheral T cell lymphoma, not otherwise specified
- Anaplastic large cell lymphoma
- Nodal T follicular helper cell lymphoma, angioimmunoblastic type (nTFHL AI)
- Hepatosplenic T cell lymphoma (HSTCL)
- Mycosis fungoides
- Extranodal NK / T cell lymphoma (ENKTCL)
- Classic Hodgkin lymphoma
- B cell lymphomas
- Large B cell lymphoma in CNS (PCNS lymphoma) and diffuse large B cell lymphoma (DLBCL) are associated with low CD4+ T cell count
- Burkitt lymphoma (BL) and classic Hodgkin lymphoma (CHL) noted in more immunocompetent patients (Adv Clin Path 1997;1:13, Blood 2001;98:2339, Lancet HIV 2020;7:e641)
- Plasmablastic lymphoma, KSHV / HHV8 associated lymphomas such as primary effusion lymphomas (PEL) and KSHV / HHV8+ DLBCL occur predominantly in HIV+ patients
- With the advent of cART, the incidence of PCNS lymphoma and DLBCL have declined, while CHL cases have increased and BL incidence has been stable (Blood 2001;98:2339, AIDS 2006;20:1645, J Natl Cancer Inst 2007;99:962, J Acquir Immune Defic Syndr 2016;72:177, AIDS Patient Care STDS 2013;27:259)
- Most of the lymphomas are usually indistinguishable from their counterparts that arise in immunocompetent patients with some of the following differences
Lymphoma Histologic features of lymphomas affecting HIV+ patients BL - More variation in size and shape (pleomorphism)
- Plasmacytoid differentiation: eccentric nucleus, single central nucleolus and abundant cytoplasm (Ann Oncol 1991;2:289)
- Stronger EBV association (Semin Diagn Pathol 2017;34:352)
DLBCL - Extranodal or disseminated presentation
- Immunoblastic / plasmablastic morphology more common
CHL - Nodular sclerosis type comprises 50% of CHL cases in people living with HIV
- Lymphocyte depleted type specifically seen
- Effective cART has negated the impact of HIV related prognostic factors and has led to better therapy for most of the aggressive lymphomas, contributing to better survival outcomes comparable to lymphoma occurring in the general population (Br J Haematol 2015;168:806, Blood 2015;125:1226, Ann Oncol 2015;26:958, Blood 2015;126:160, Blood Adv 2021;5:2852)
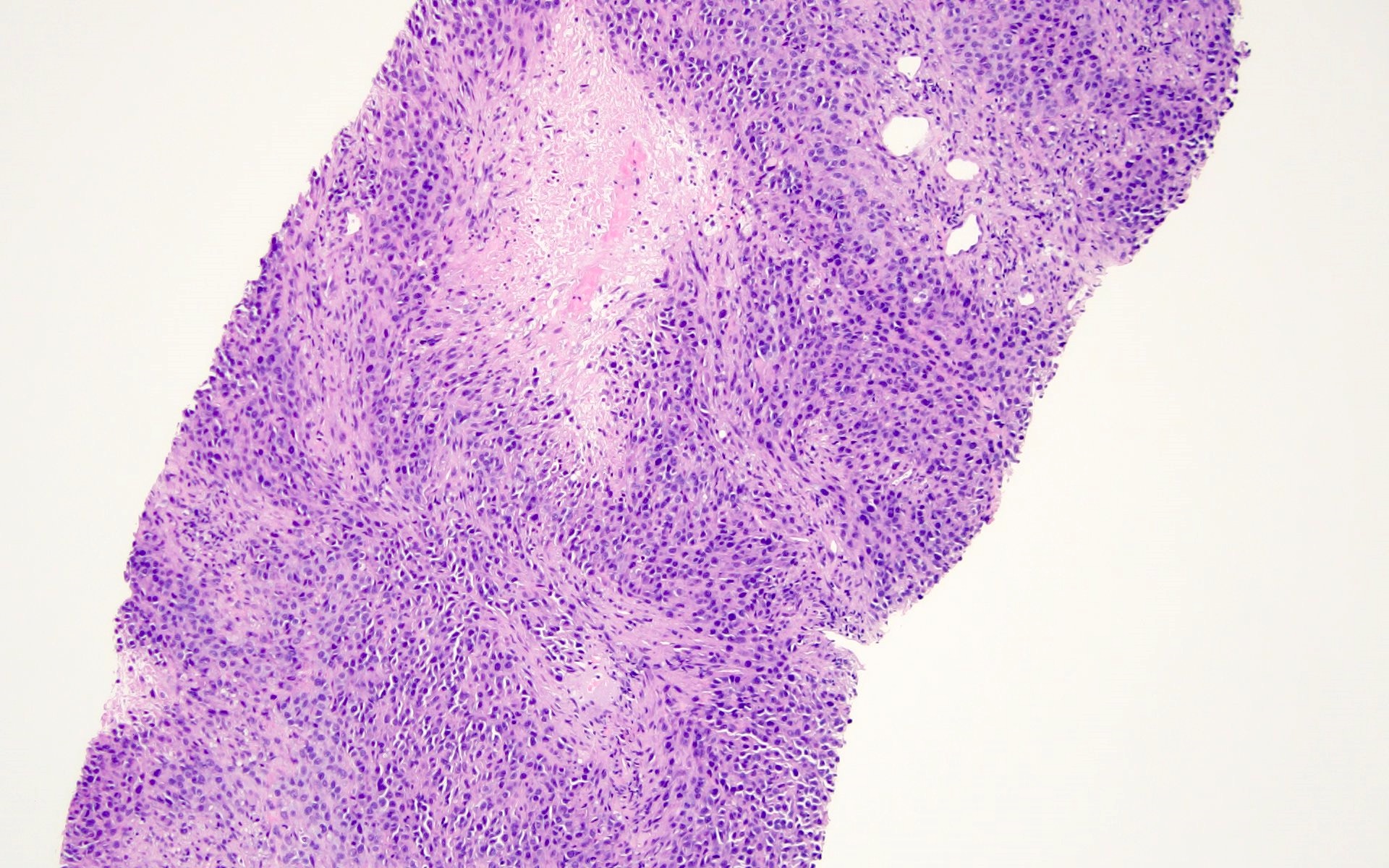
Microscopic (histologic) images
Contributed by Barina Aqil, M.D.
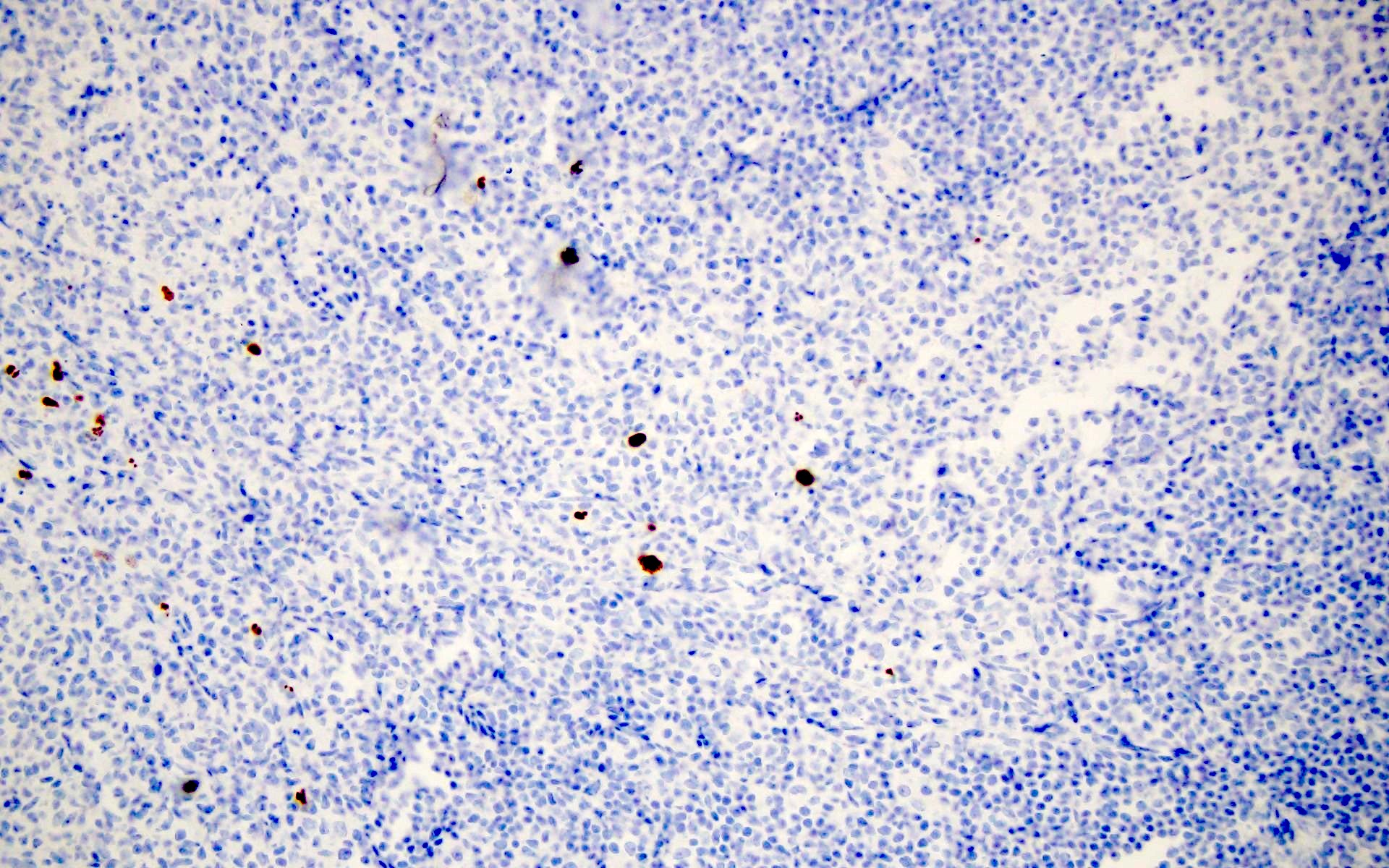
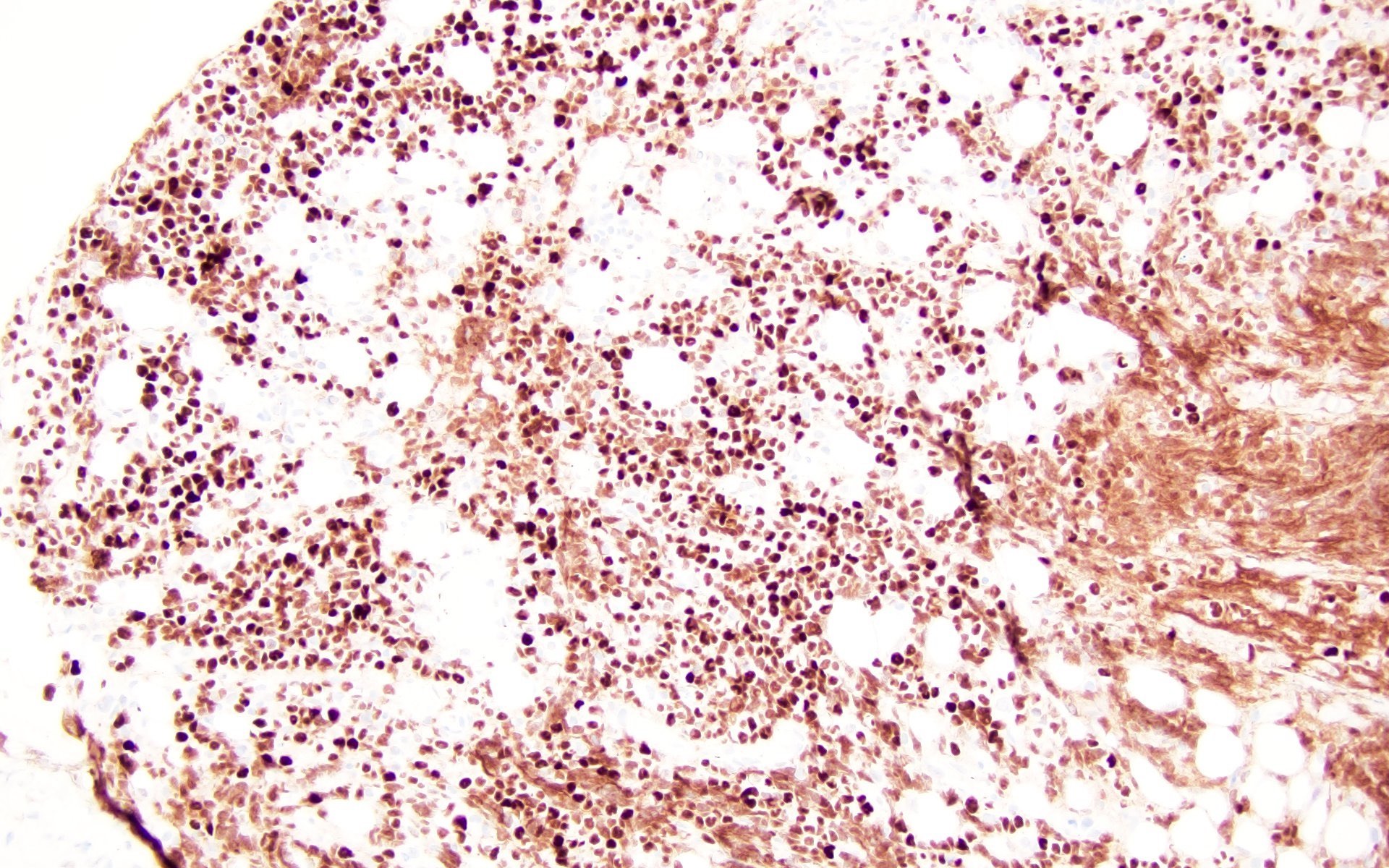
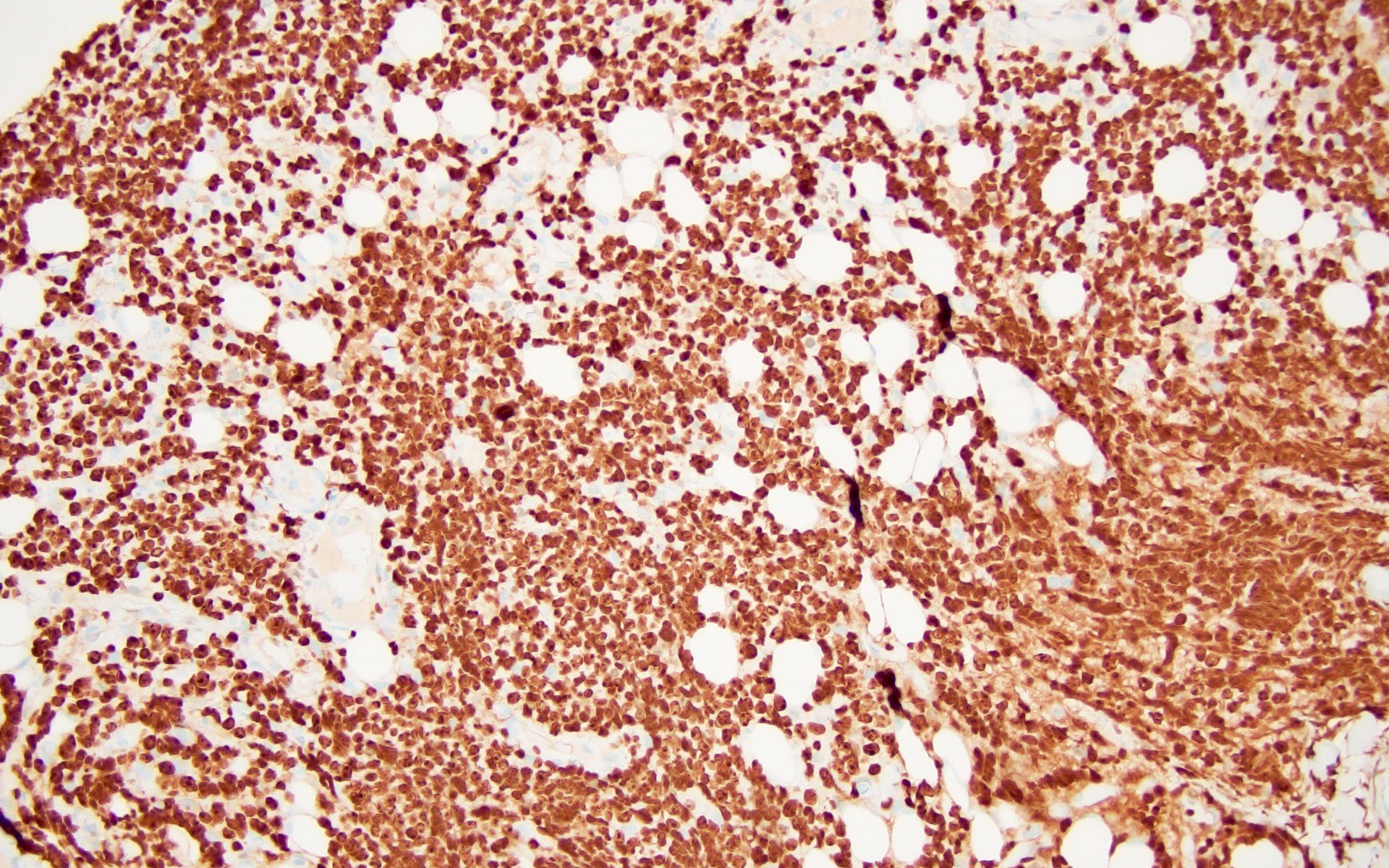
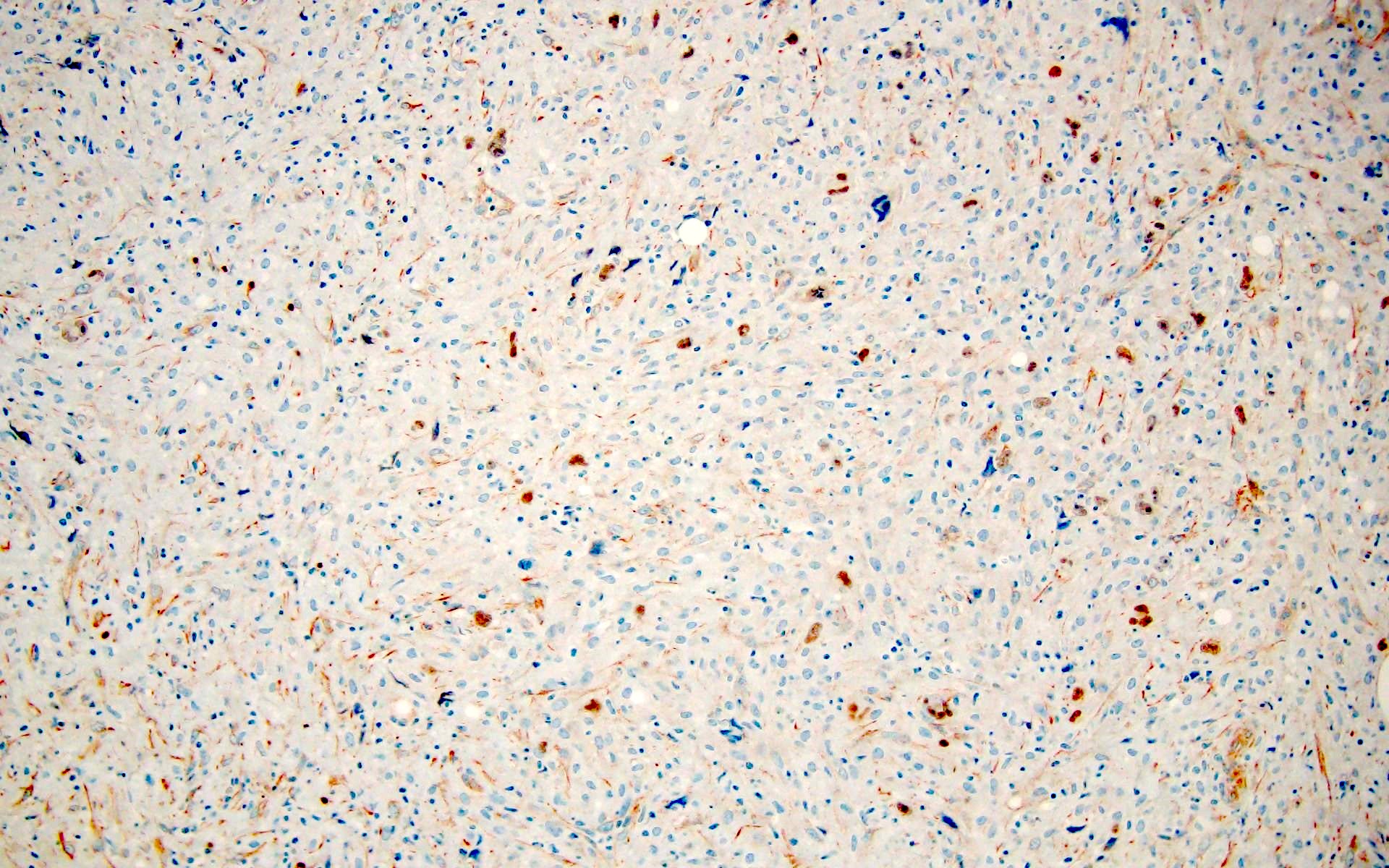
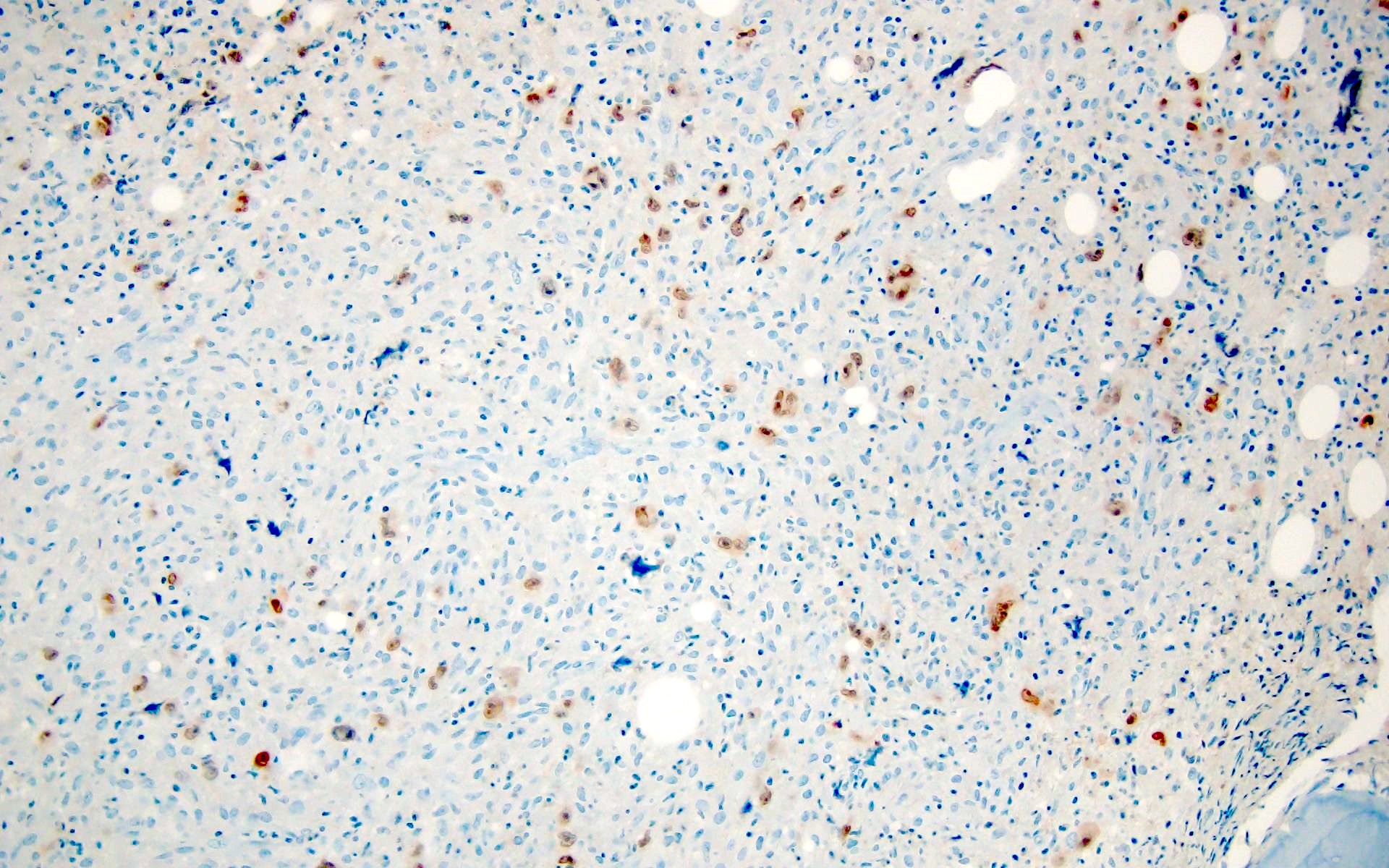
Positive stains
- p24 (Histopathology 2010;56:530)
- Antibody to HIV core protein
- Localized in reactive germinal centers along follicular dendritic cell processes
- p15 and p17 (Am J Pathol 1988;133:516)
- Staining of follicular dendritic cells
- Radiolabeled HIV RNA in situ hybridization (J Infect Dis 1991;164:1051)
- Found in high concentrations in germinal centers
Sample pathology report
- Lymph node, left supraclavicular, needle core biopsy:
- Classic Hodgkin lymphoma, EBV+ arising in an HIV+ patient
- Flow cytometric analysis performed on the left supraclavicular lymph node biopsy reveals a polytypic B cell population and a T cell population without evidence of immunophenotypic abnormality based on the markers assayed
- Microscopic description: Histologic sections show cylindrical cores of lymphoid tissue with scattered large mononuclear cells with prominent macronucleoli in the background of histiocytes, small lymphocytes, plasma cells and eosinophils. Rare mummified cells are noted.
- Immunohistochemistry results: CD3- in large atypical cells (shows numerous small T cells), CD20- in large atypical cells (shows scattered small B cells), PAX5+ with strong staining in background B cells (dim in large atypical cells), CD30+ in large atypical cells, CD15+ in large atypical cells, MUM1+ in large atypical cells, EBER+ in scattered large atypical cells
Differential diagnosis
- Infectious mononucleosis:
- Similarly reactive follicles as in HIV acute pattern
- Serologic testing positive for EBV
- Negative HIV antibodies
- Cytomegalovirus, measles and varicella lymphadenitis:
- CMV inclusions seen in CMV infection
- Giant multinucleated cells (Warthin-Finkeldey) seen in both measles and HIV; so serologic testing is required
- Toxoplasma lymphadenitis:
- Monocytoid hyperplasia noted in Toxoplasma as well as in HIV infection
- Perifollicular and intrafollicular clusters of epithelioid cells only noted in Toxoplasma
- Castleman lymphadenopathy:
- Mimics pattern B and C of HIV lymphadenopathy
- Lacks depletion of lymphocytes
- Negative for HIV antibodies
- Nodal TFH cell lymphoma, angioimmunoblastic type:
- Paracortical expansion with vascular proliferation and effaced follicles reminiscent to HIV chronic and burnout patterns
- No depletion of lymphocytes
- Proliferation of immunoblasts
Additional references
- CDC: About HIV [Accessed 14 December 2023], CDC: PrEP (Pre-exposure Prophylaxis) [Accessed 14 December 2023], Bennett: Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, 9th Edition, 2019, Goldman: Goldman-Cecil Medicine, 27th Edition, 2023, Clinicalinfo: Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV [Accessed 14 December 2023]
Board review style question #1
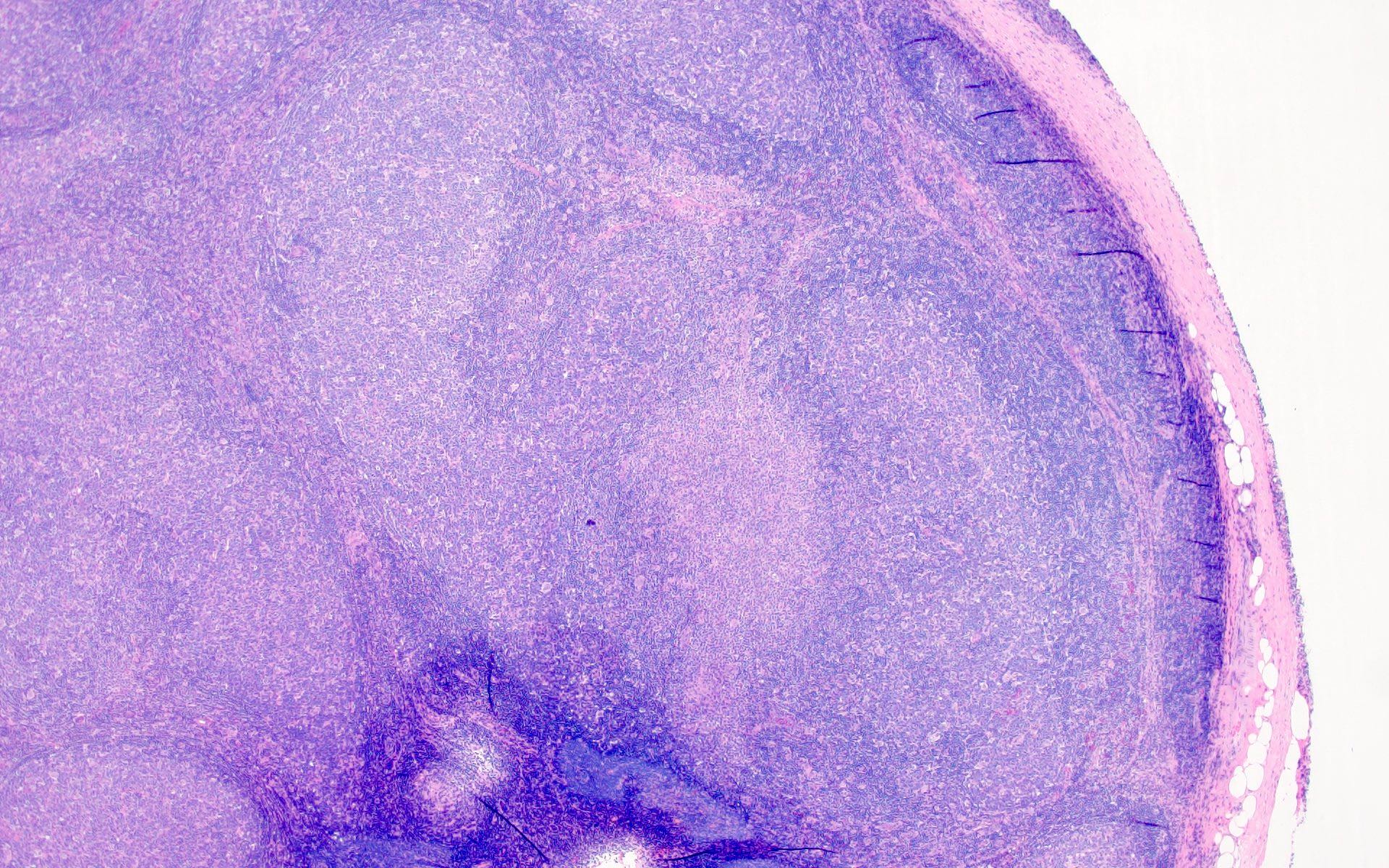
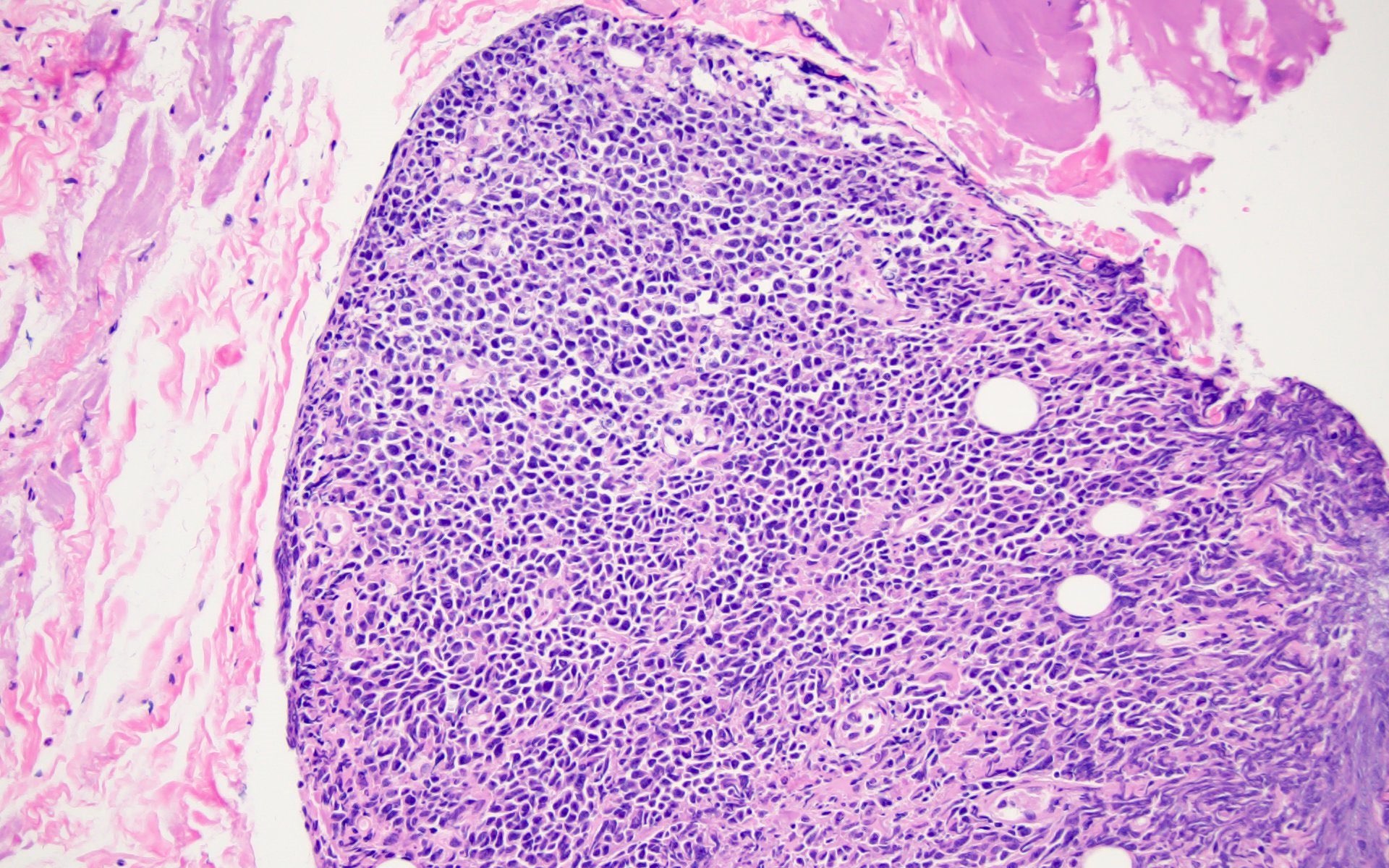
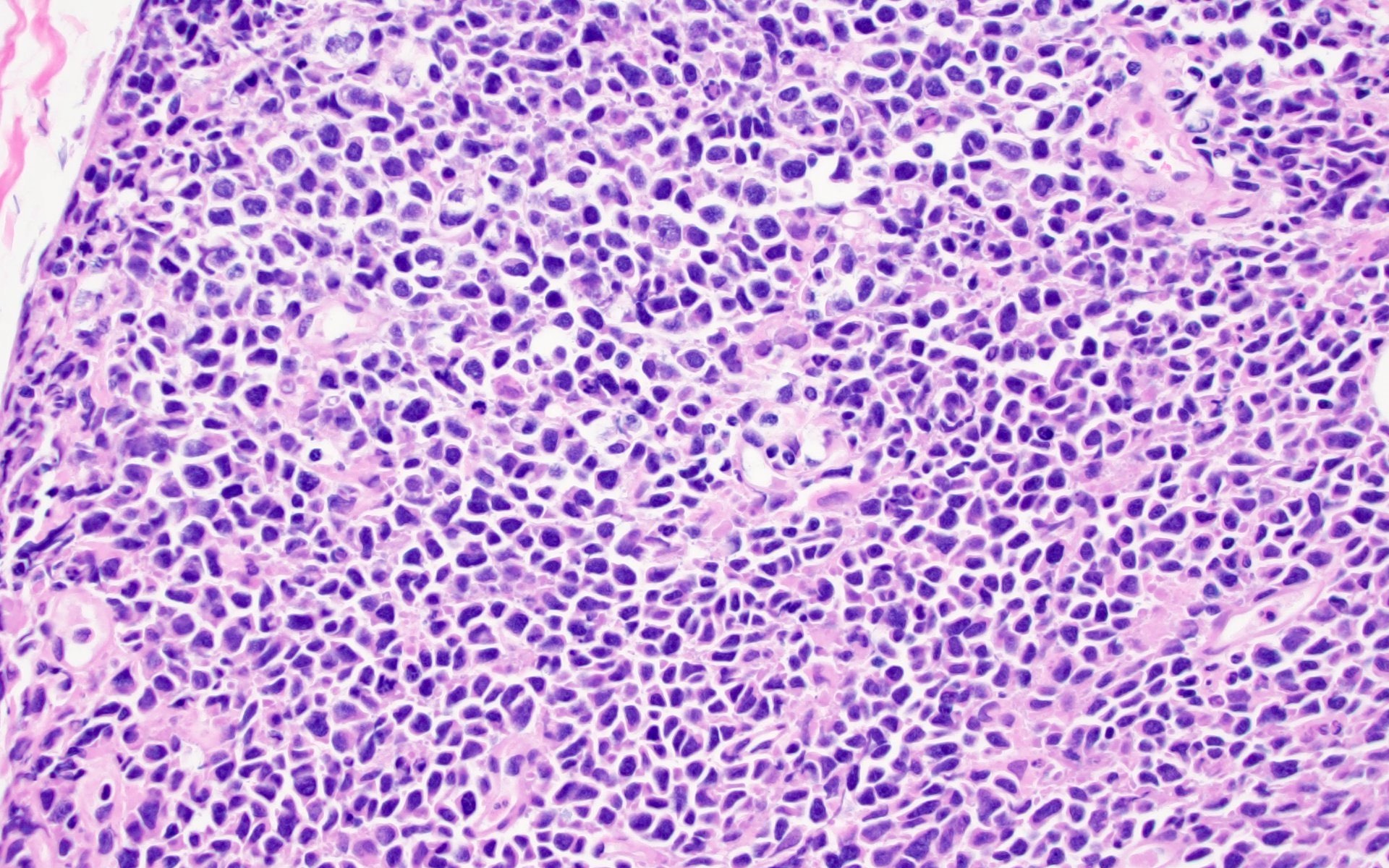
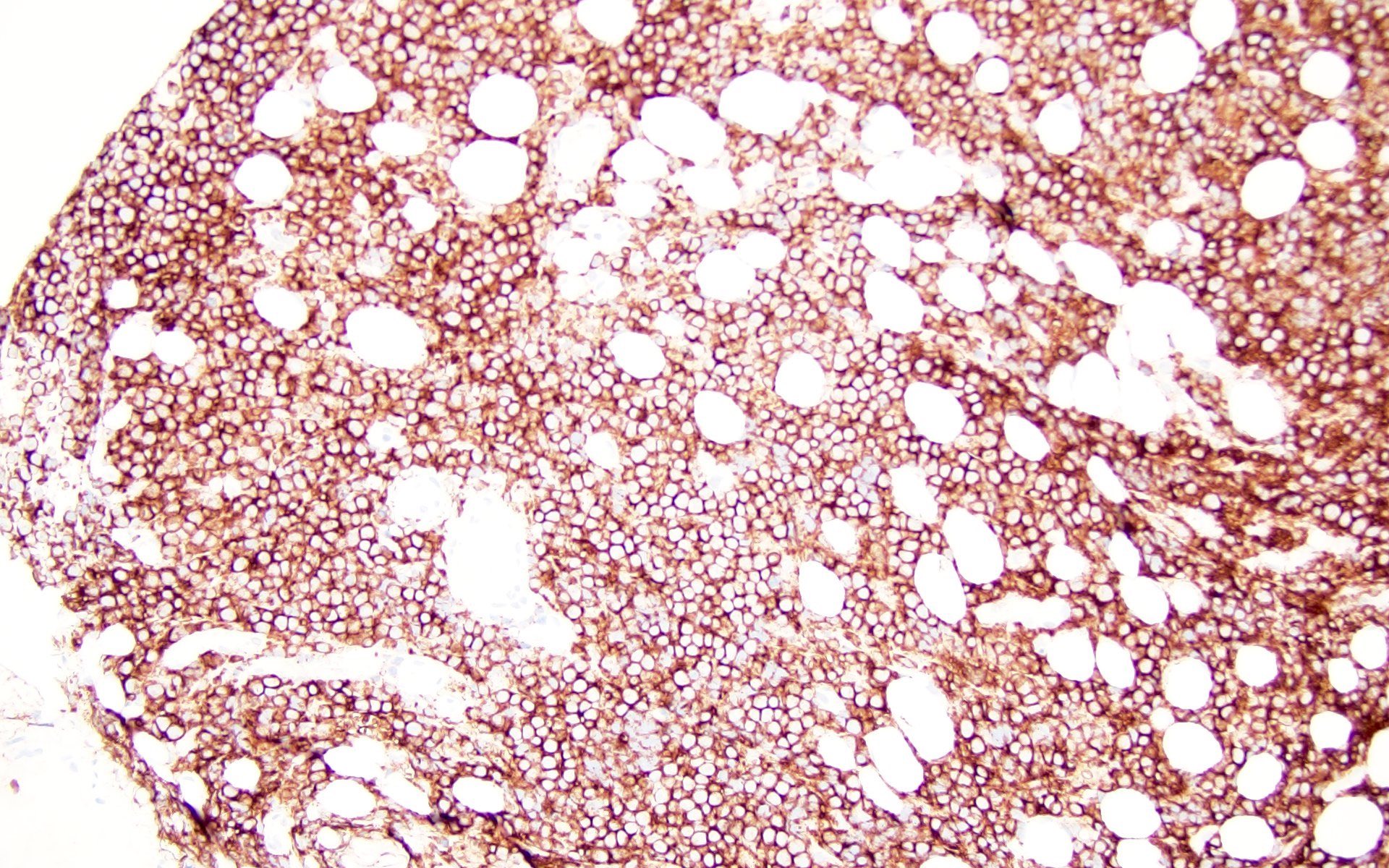
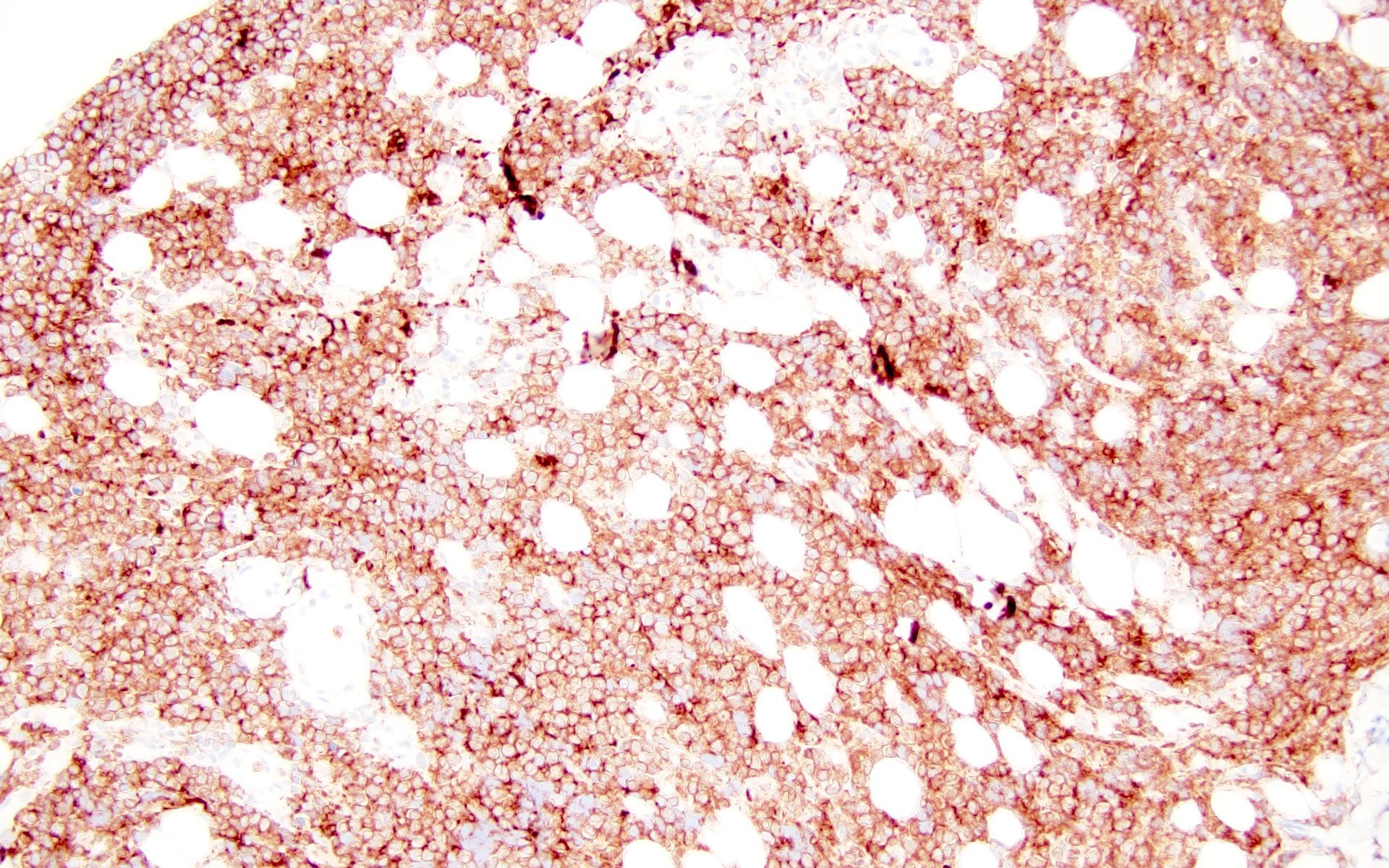
The patient is a 42 year old man who presented with fever, cough and weight loss. Imaging showed diffuse lymphadenopathy. An excisional lymph node biopsy was performed that showed the above morphology (H&E stains and LANA immunohistochemistry). What is the diagnosis?
- Burnout pattern of HIV lymphadenitis
- Diffuse large B cell lymphoma (DLBCL)
- KSHV / HHV8 associated multicentric Castleman disease
- Toxoplasma lymphadenitis
Board review style answer #1
C. KSHV / HHV8 associated multicentric Castleman disease. The lymph node showed regressed germinal centers with hyalinized arterioles, vascular proliferation and plasmablasts in the mantle zones. The plasmablasts are positive for CD138, MUM1, LANA and negative for B cell markers (CD20, PAX5, etc.).
Answer D is incorrect because toxoplasmosis has reactive follicles, monocytoid hyperplasia and perifollicular / intrafollicular clusters of epithelioid histiocytes. Answer A is incorrect because later stages of HIV lymphadenitis (patterns B and C) show markedly attenuated follicles with vascular proliferation and loss of lymphocytes. Answer B is incorrect because DLBCL has diffuse infiltrate of large neoplastic B cells, which can have variable cellular morphology, including centroblastic, immunoblastic or anaplastic. The neoplastic cells retain B cell markers and are LANA negative.
Comment Here
Reference: HIV
Answer D is incorrect because toxoplasmosis has reactive follicles, monocytoid hyperplasia and perifollicular / intrafollicular clusters of epithelioid histiocytes. Answer A is incorrect because later stages of HIV lymphadenitis (patterns B and C) show markedly attenuated follicles with vascular proliferation and loss of lymphocytes. Answer B is incorrect because DLBCL has diffuse infiltrate of large neoplastic B cells, which can have variable cellular morphology, including centroblastic, immunoblastic or anaplastic. The neoplastic cells retain B cell markers and are LANA negative.
Comment Here
Reference: HIV
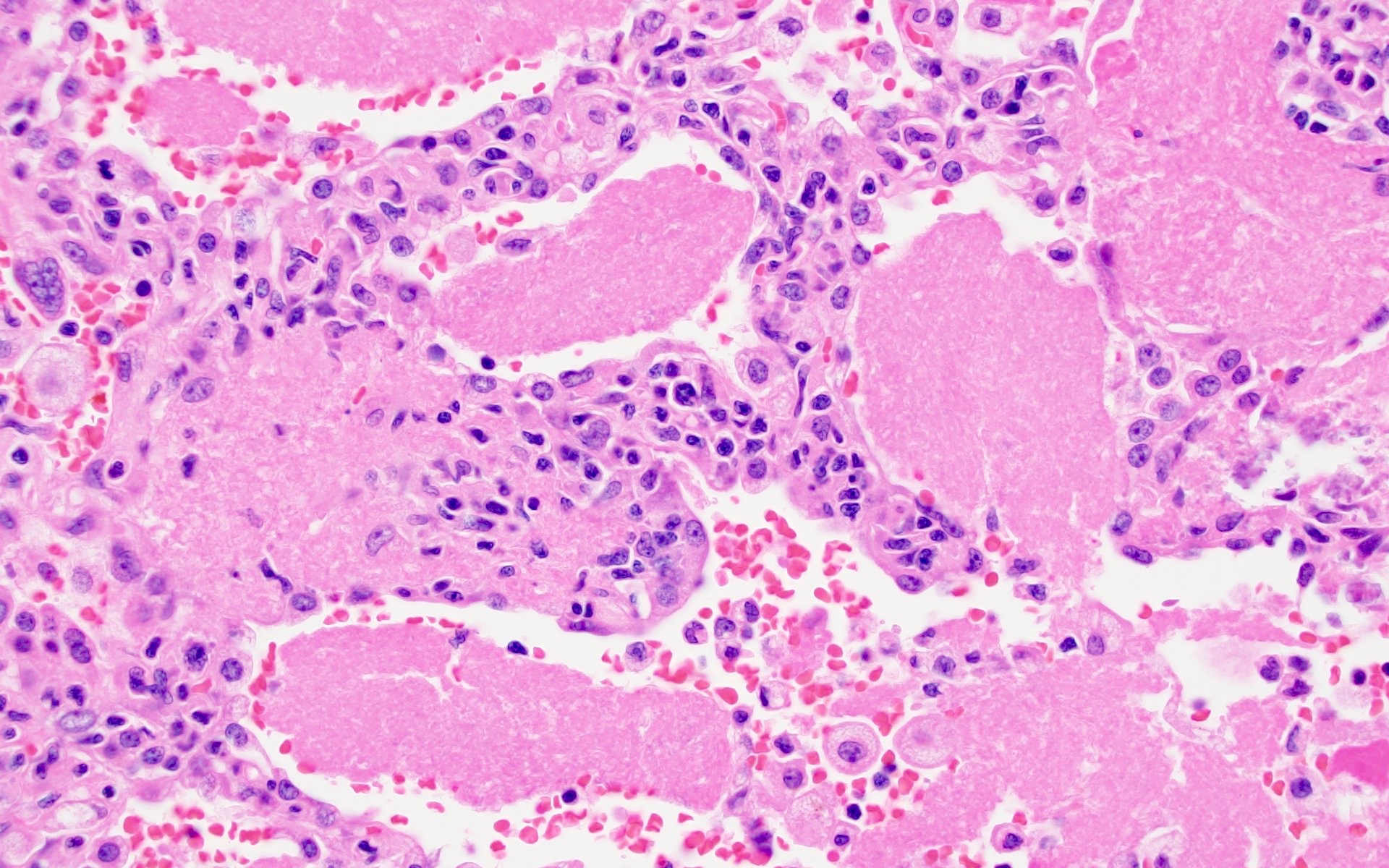
Board review style question #2
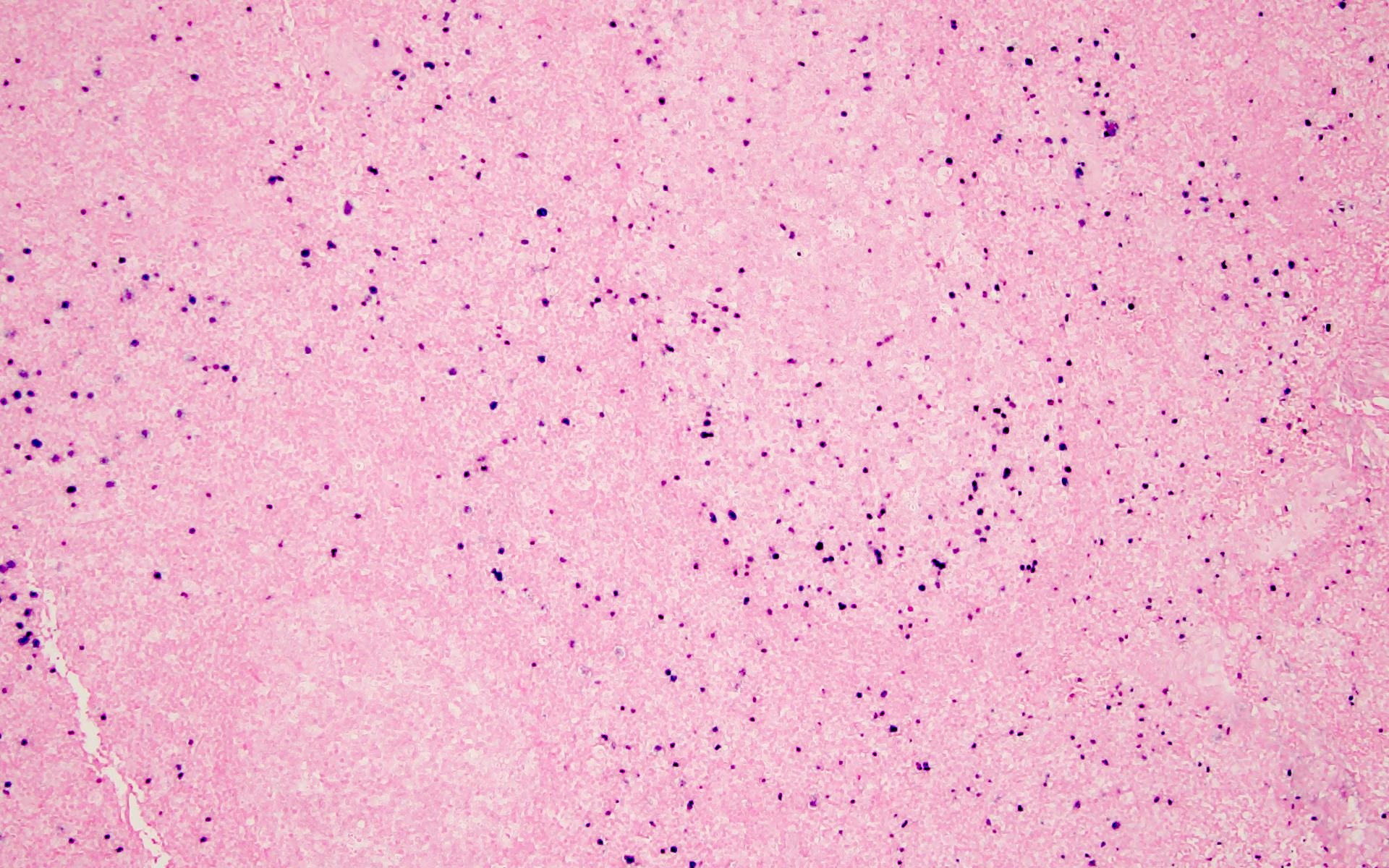
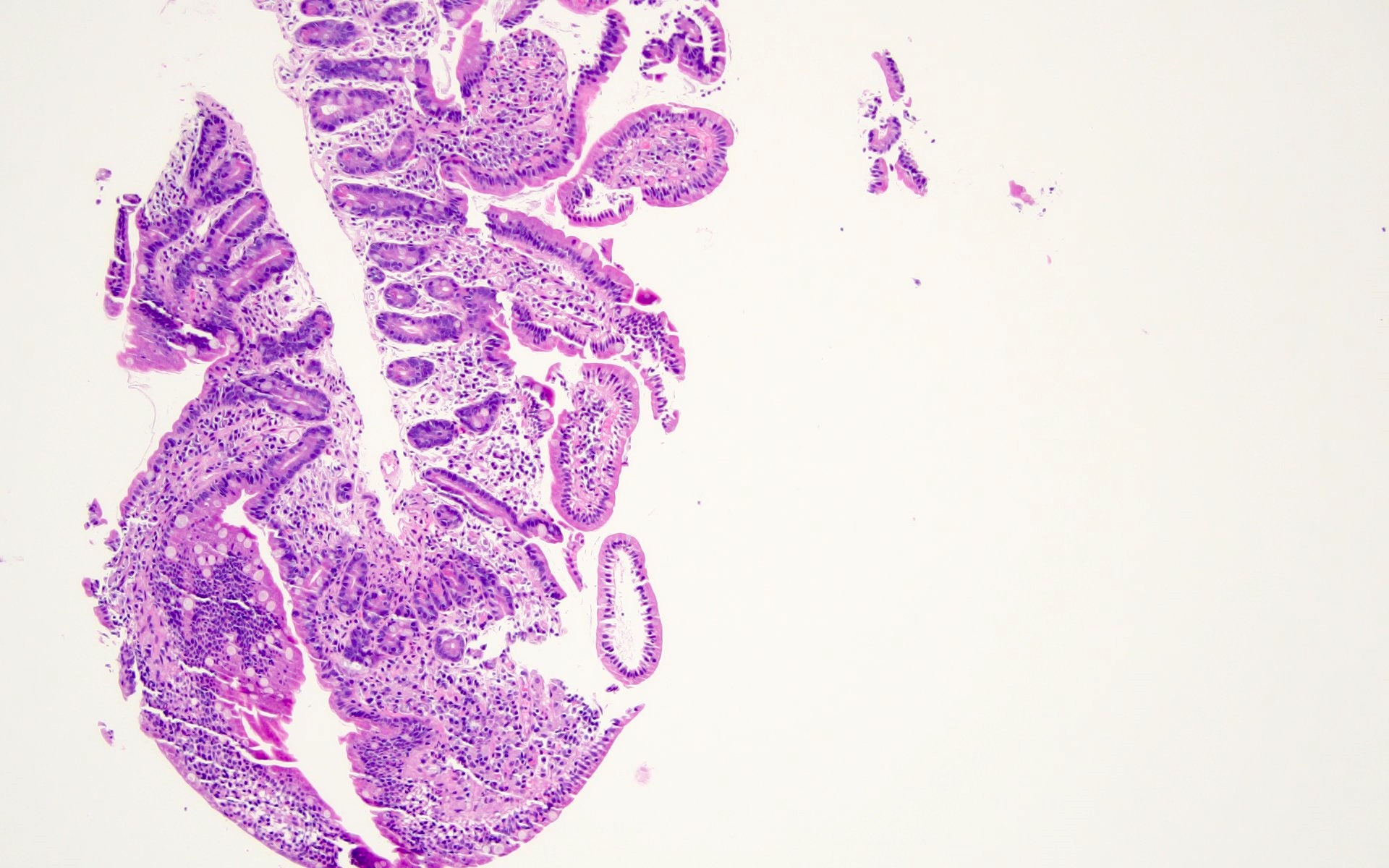
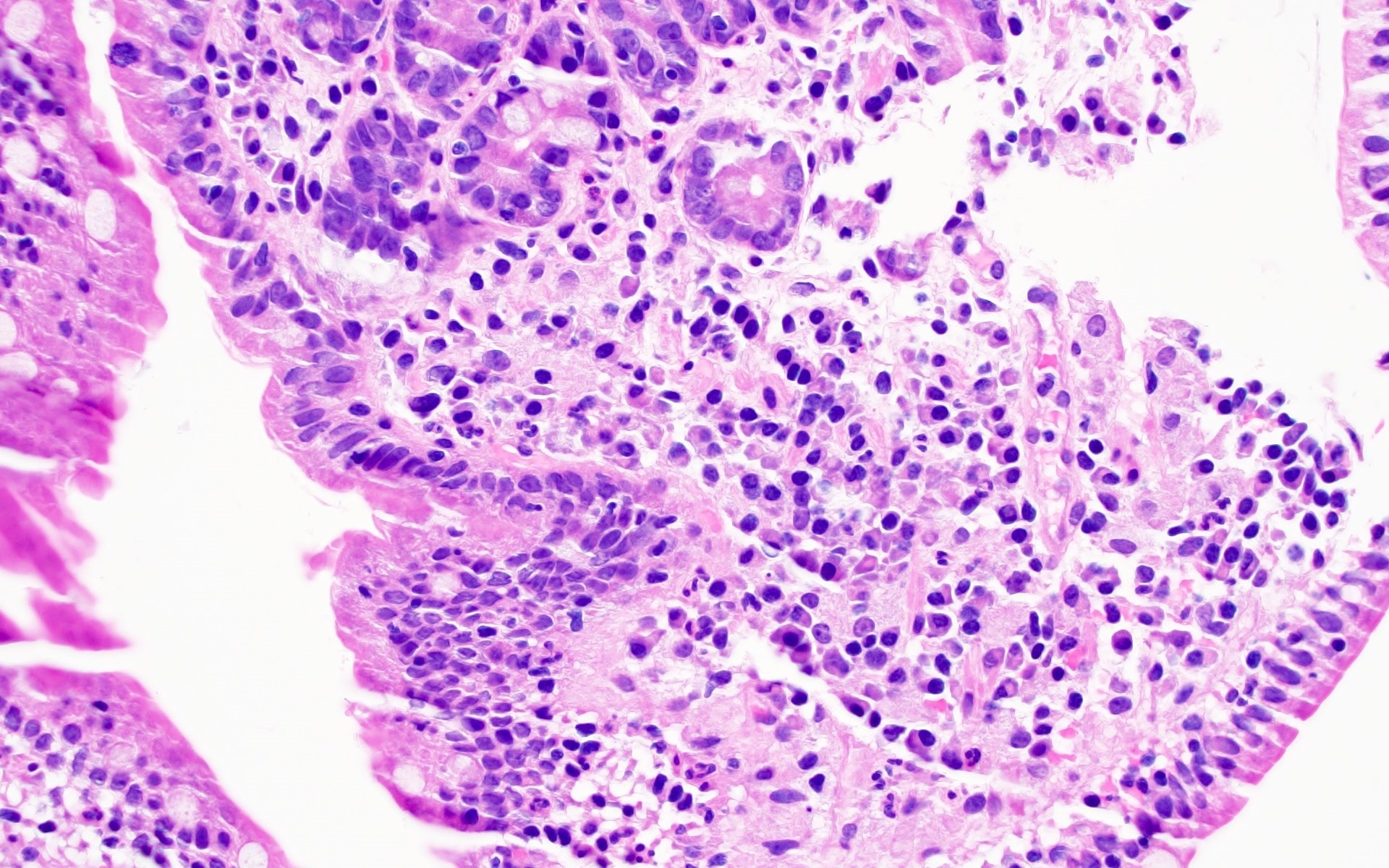
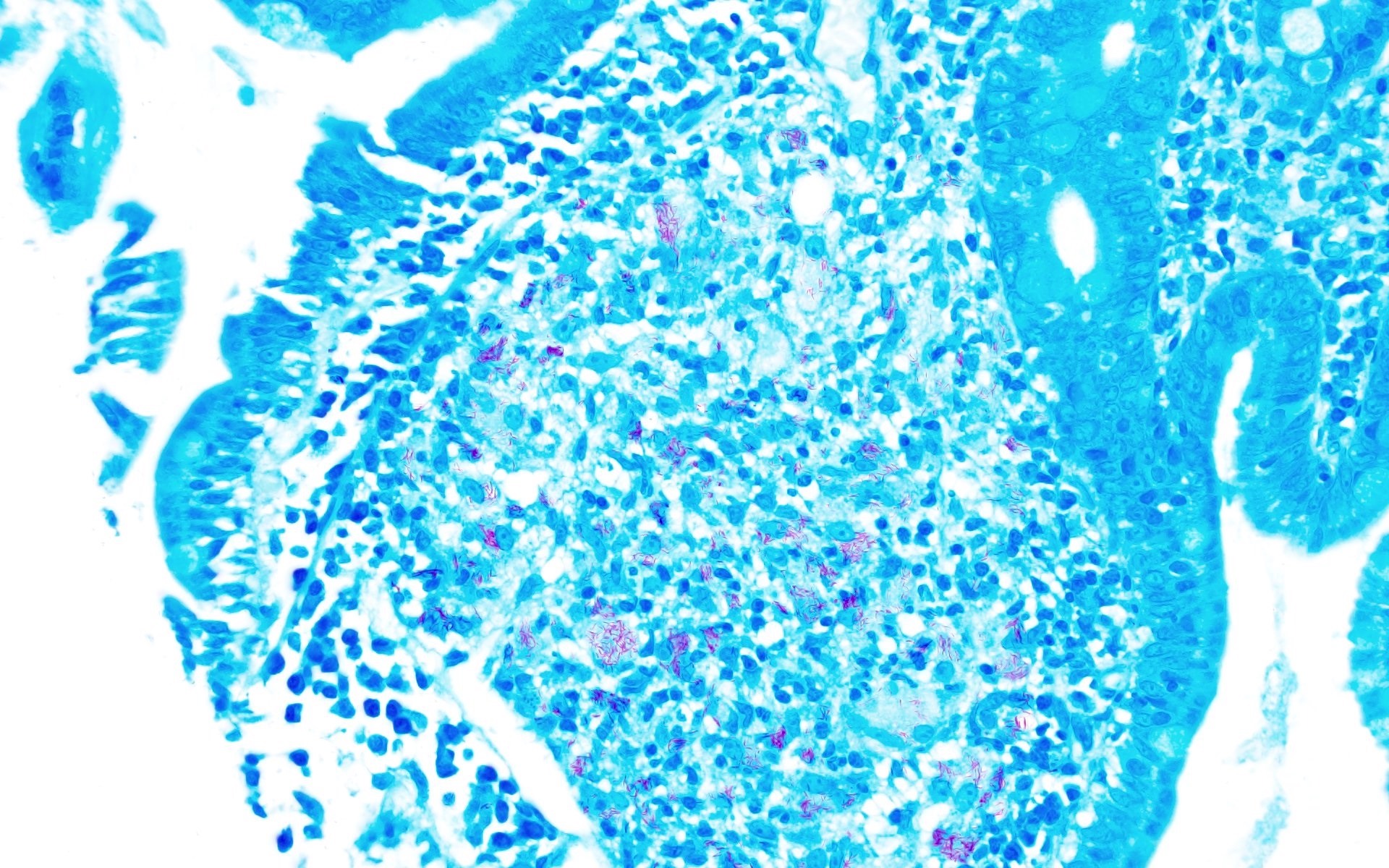
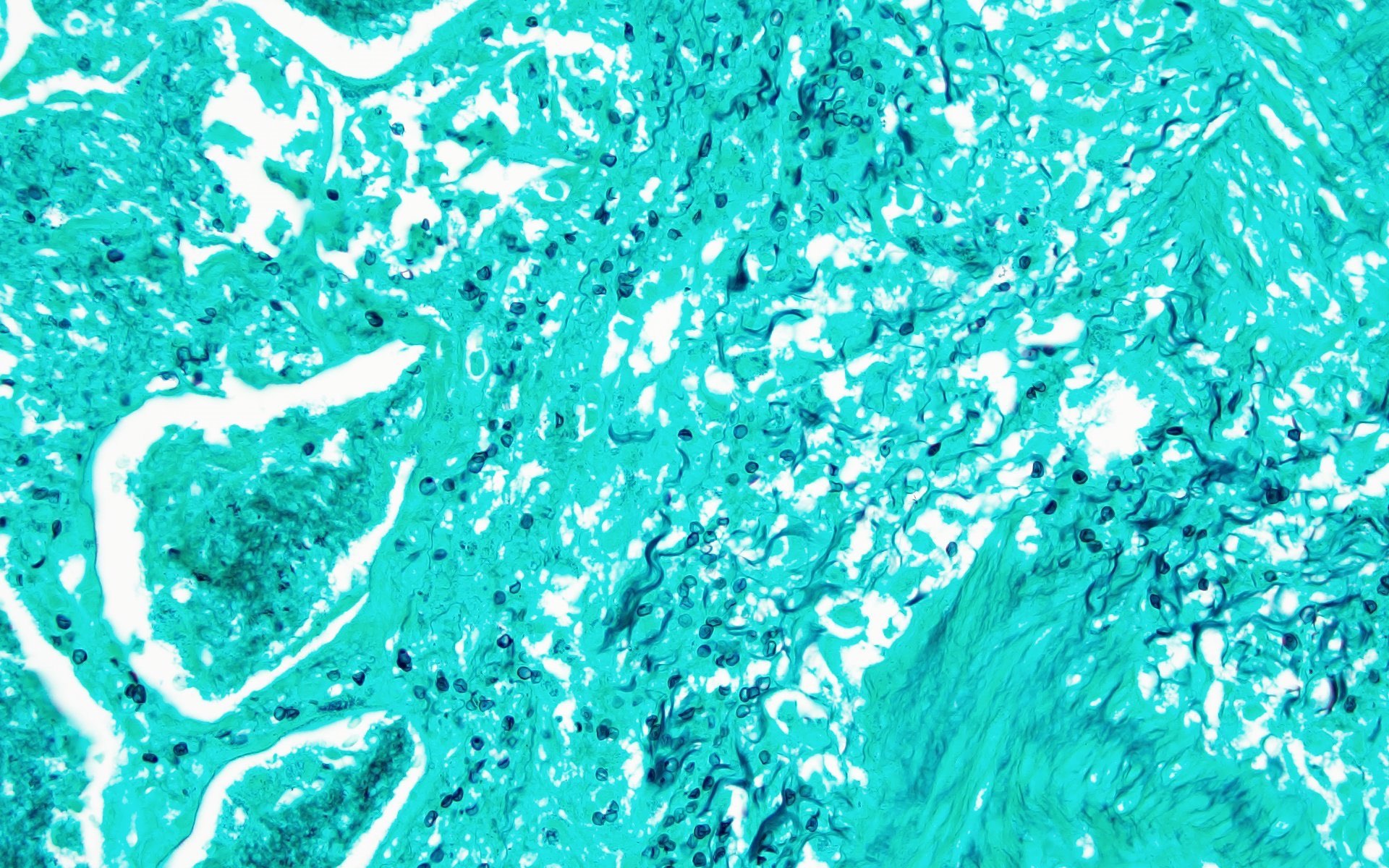
The patient is an adult who was found unresponsive at the bus stop and brought over to the emergency department by the paramedics. HIV serologies were positive. Imaging showed generalized lymphadenopathy, pulmonary infiltrates and bilateral pleural effusion. Lung sampling showed the above morphology (H&E stains and Gomori methenamine silver). What is the diagnosis?
- Alveolar proteinosis
- Blastomycosis
- Mycobacterium avium intracellulare (MAI)
- Pneumocystis jirovecii infection
Board review style answer #2
D. Pneumocystis jirovecii infection is a fungal infection seen in immunocompromised patients. Lung specimen shows pink foamy amorphous material within the alveolar spaces and the GMS (Grocott-Gomori methenamine silver) reveals thin walled, oval, round and crescentic yeast forms about the size of red blood cells (7 μm) with a small central dot.
Answer A is incorrect because intra-alveolar PAS (periodic acid Schiff) positive and GMS negative material is noted in alveolar proteinosis. Answer B is incorrect because blastomycosis is also a fungal infection characterized by granulomatous inflammation and GMS shows 12 μm spherical yeast forms with broad based buds. Answer C is incorrect because MAI is a bacterial infection that may have necrotizing granulomas or just foamy histiocytes with red stained acid fast bacilli seen on special stain (AFB).
Comment Here
Reference: HIV
Answer A is incorrect because intra-alveolar PAS (periodic acid Schiff) positive and GMS negative material is noted in alveolar proteinosis. Answer B is incorrect because blastomycosis is also a fungal infection characterized by granulomatous inflammation and GMS shows 12 μm spherical yeast forms with broad based buds. Answer C is incorrect because MAI is a bacterial infection that may have necrotizing granulomas or just foamy histiocytes with red stained acid fast bacilli seen on special stain (AFB).
Comment Here
Reference: HIV