Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: McGeough A, Sharma D. Squamous cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumorscc.html. Accessed December 23rd, 2024.
Definition / general
- Malignant tumor arising from epithelial cells with squamous differentiation demonstrated either immunohistochemically or morphologically, with the presence of keratinization or intercellular bridges
- Can be keratinizing or nonkeratinizing and subtypes include solid, cystic, papillary, pseudoglandular, alveolar filling and sarcomatoid / spindle cell change
Essential features
- Morphologically identified with keratinization, keratin pearls and intercellular bridges
- Poorly differentiated lesions may lose morphologic features of squamous differentiation and require IHC to separate from other non-small lesions, p40 positivity will help
- Primary and metastatic tumors have an overlapping morphology and immunohistochemical profiles; in most cases it is not possible to determine the primary site of squamous cell carcinoma
Terminology
- Epidermoid carcinoma: historical and no longer recommended
ICD coding
Epidemiology
- Strong association with history of tobacco smoking (80% of men and 90% of women) (Thorax 1973;28:354)
- Primarily in patients over 50 years of age
- 85% of primary lung cancers are non-small cell carcinomas and squamous cell makes up 30% of these cases (Clin Cancer Res 2012;18:2443)
Sites
- Can present in any site of the lungs or bronchus but is more commonly central
- Metastasis is frequently observed (Ann Oncol 2018;29:iv192)
- Mediastinal lymph nodes are the primary site
- Hematogenous spread to distant organs
- Bone is the most common
- Liver is the second most common
Pathophysiology
- Squamous cells lining the respiratory tract transformed from carcinogen exposure, most frequently smoking
- Occupational heavy metal exposure has also been reported (Int Arch Occup Environ Health 2009;82:867)
- Extrapulmonary squamous cell carcinoma is also possible
Etiology
- See Pathophysiology
Clinical features
- Wide range of nonspecific pulmonary symptoms reported including cough, chest pain, shortness of breath, hemoptysis, wheezing, weight loss, recurrent infections, loss of appetite and fatigue (StatPearls: Squamous Cell Lung Cancer [Accessed 31 May 2023])
- If the mass compresses the recurrent laryngeal nerve it may also present with hoarseness
Diagnosis
- Can be made on biopsy or cytology specimen, though a lack of keratinization or in poorly differentiated cases immunohistochemical testing may be required (Thorax 2016;71:177)
Laboratory
- Humoral hypercalcemia of malignancy secondary to paraneoplastic syndrome is seen in up to 10% of cases and is associated with a poor prognosis (World J Clin Oncol 2014;5:197)
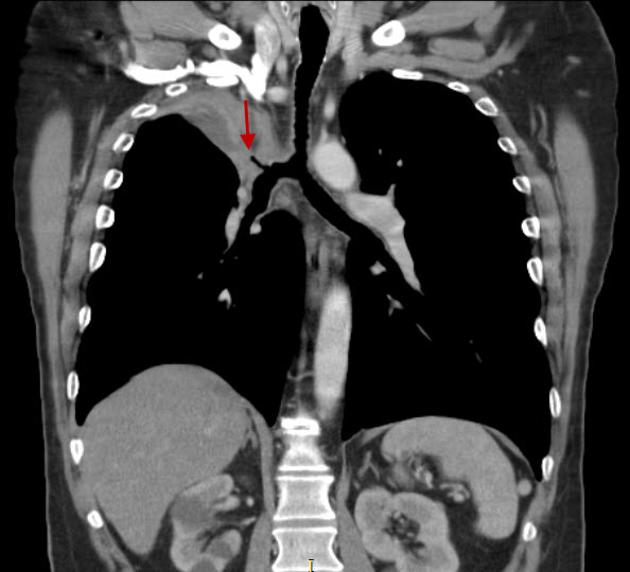
Radiology description
- CT is the imaging of choice for lung cancer evaluation and demonstrates a nonspecific mass with irregular borders, often with central cavitation
- Centrally located tumors are more common and often cause obstruction with associated pneumonitis or lung collapse
- Squamous cell carcinoma cannot be distinguished definitively from radiological findings as other lesions may have the same radiologic appearance
- Reference: Radiopaedia: Squamous Cell Carcinoma of the Lung [Accessed 31 May 2023]
Radiology images
Prognostic factors
- Stage at time of diagnosis is the best predictor of prognosis
Case reports
- 52 year old woman with lung cancer responding to alectinib (BMC Cancer 2017;17:471)
- 56 year old man with primary lung cancer and metastasis to tongue (Medicine (Baltimore) 2017;96:e8208)
- 60 year nonsmoking woman with lung cancer treated with osimertinib (Intern Med 2021;60:1067)
Treatment
- Primary treatment is surgical excision through wedge resection, lobectomy or pneumonectomy (J Natl Compr Canc Netw 2022;20:497)
- Systemic chemotherapy including PDL1 immunotherapy (if applicable) and radiation therapy (Transl Lung Cancer Res 2018;7:S198)
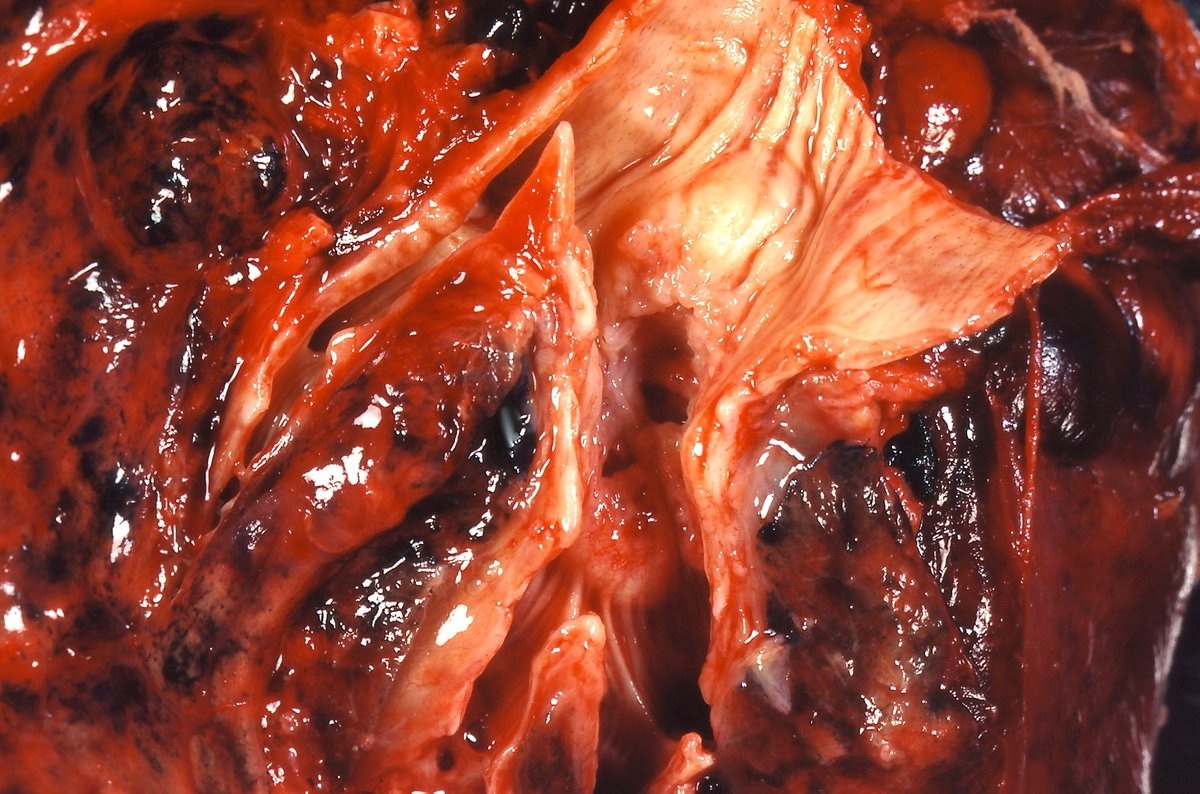
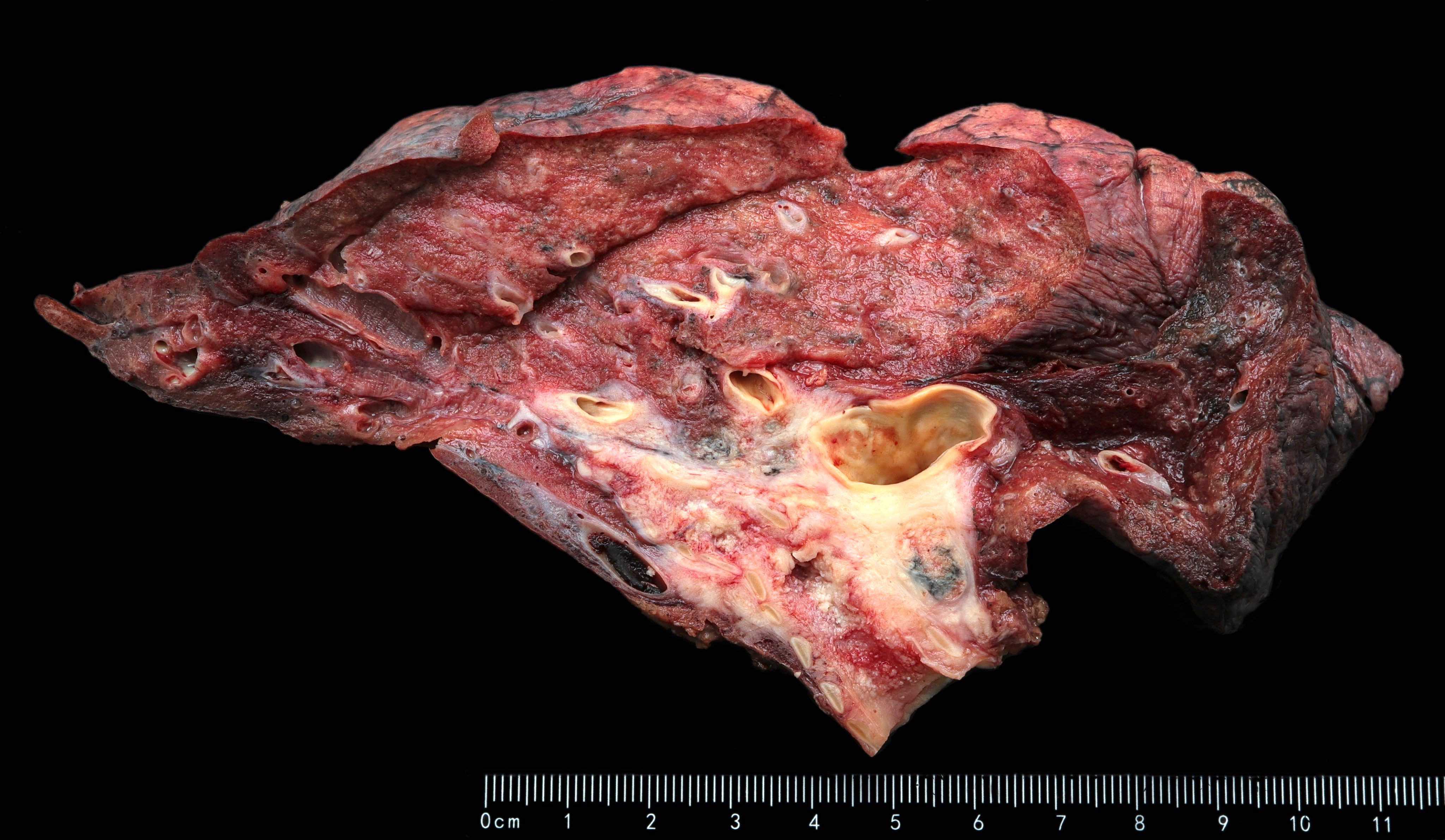
Gross description
- Often cavitary mass with white, smooth cut surfaces that frequently contain hemorrhage and necrosis
- Mass is more often central than peripheral and may be within the bronchus
Gross images
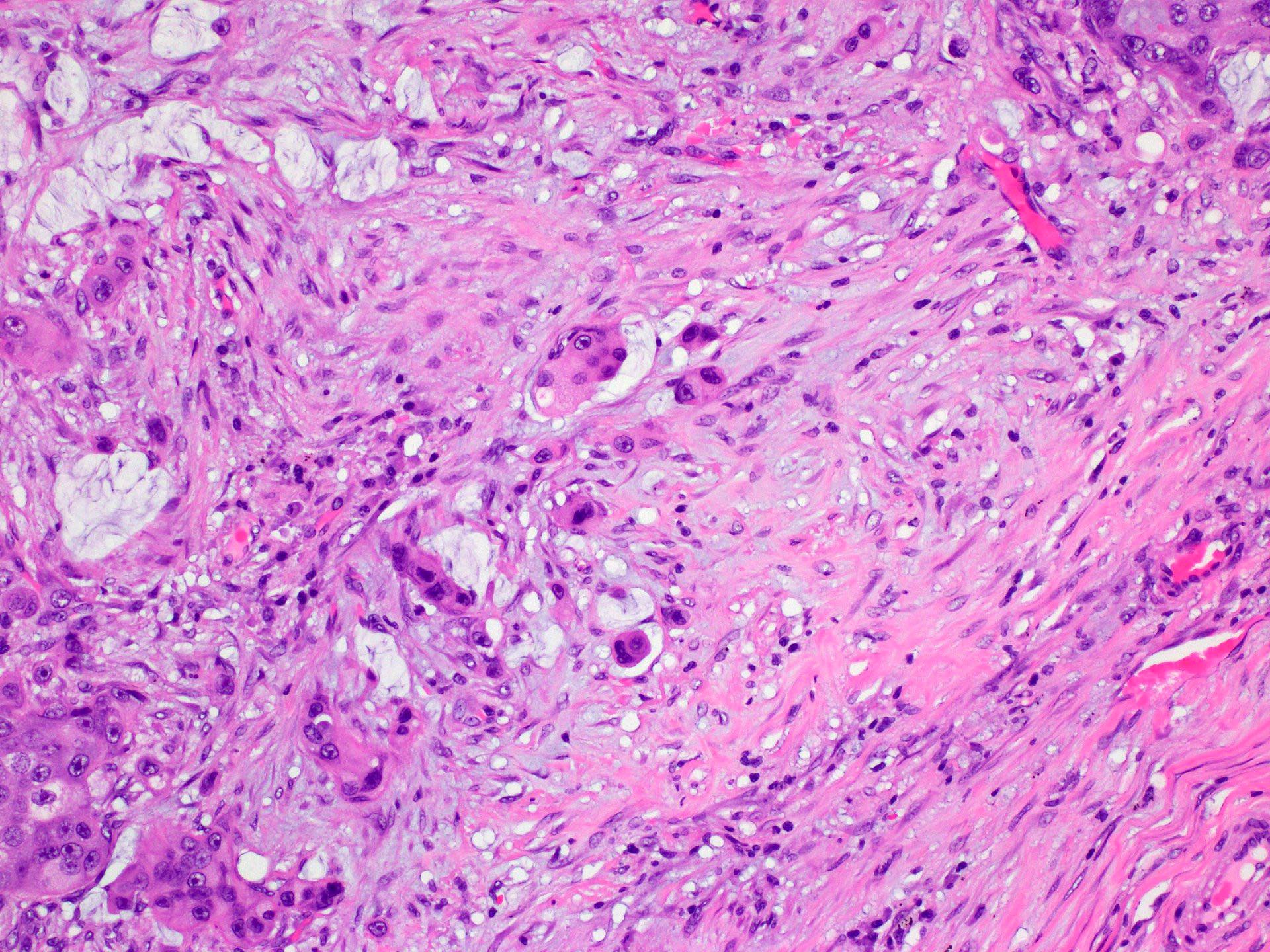
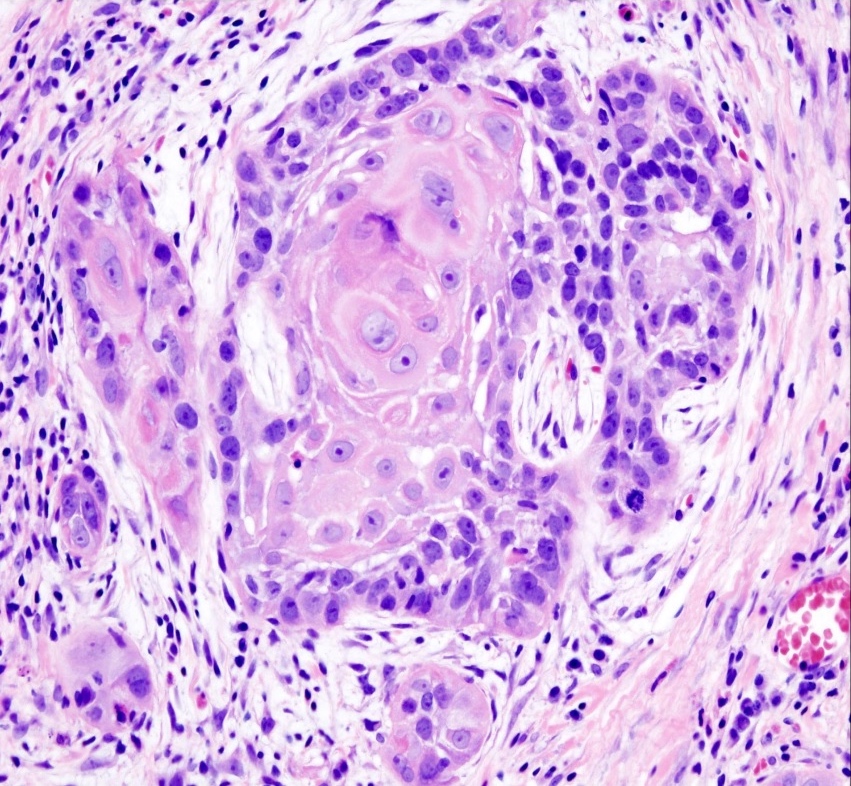
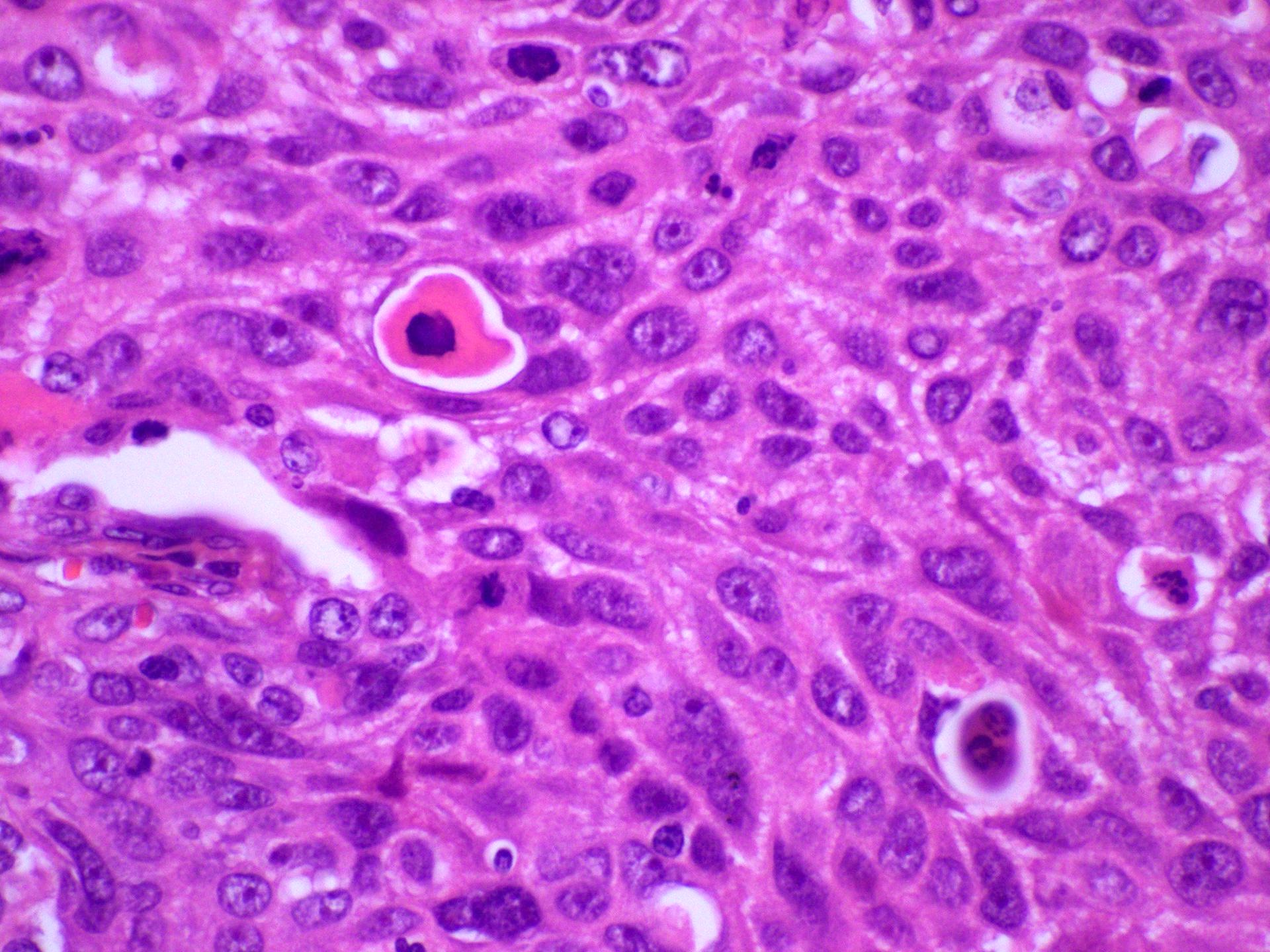
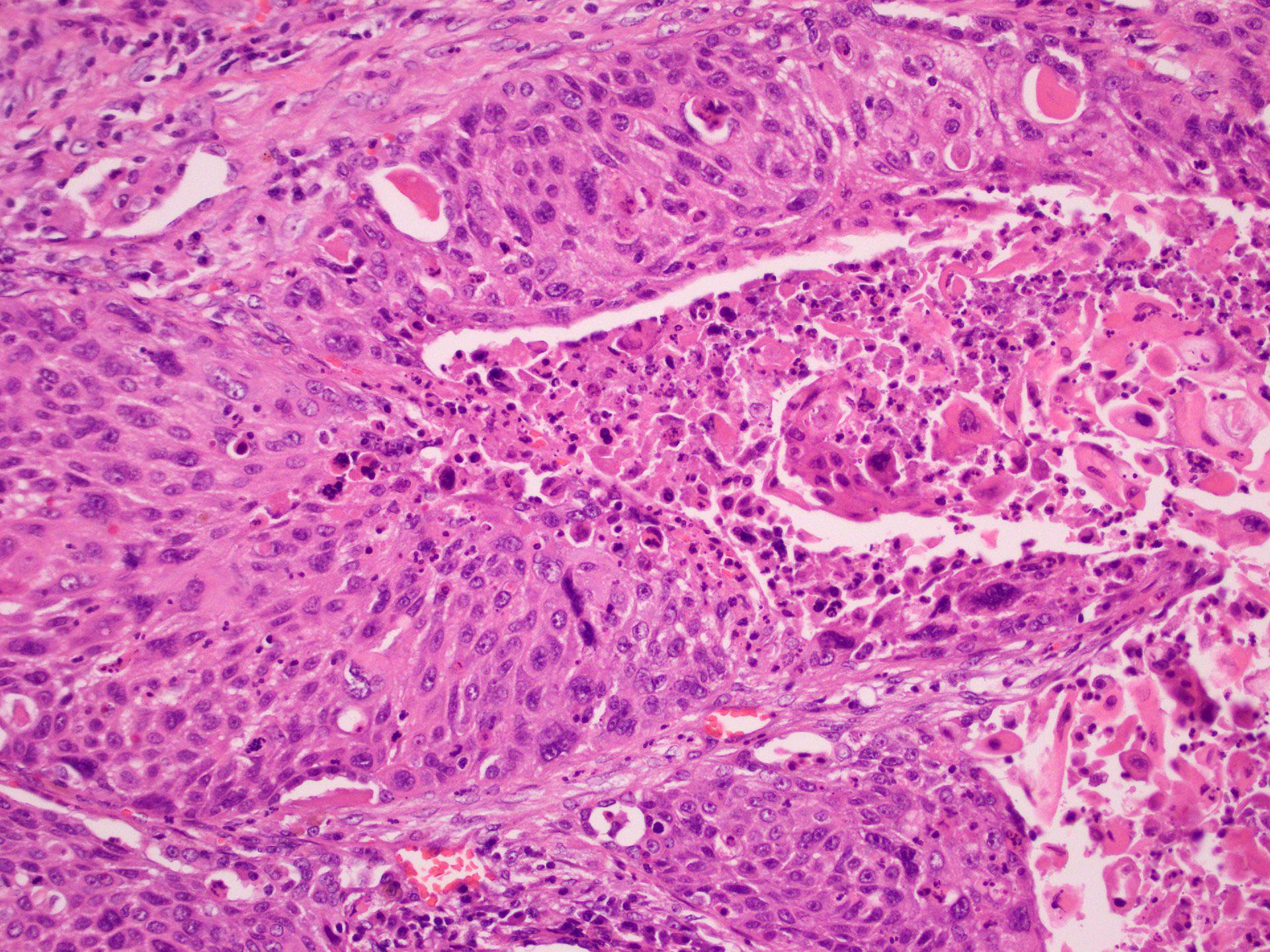
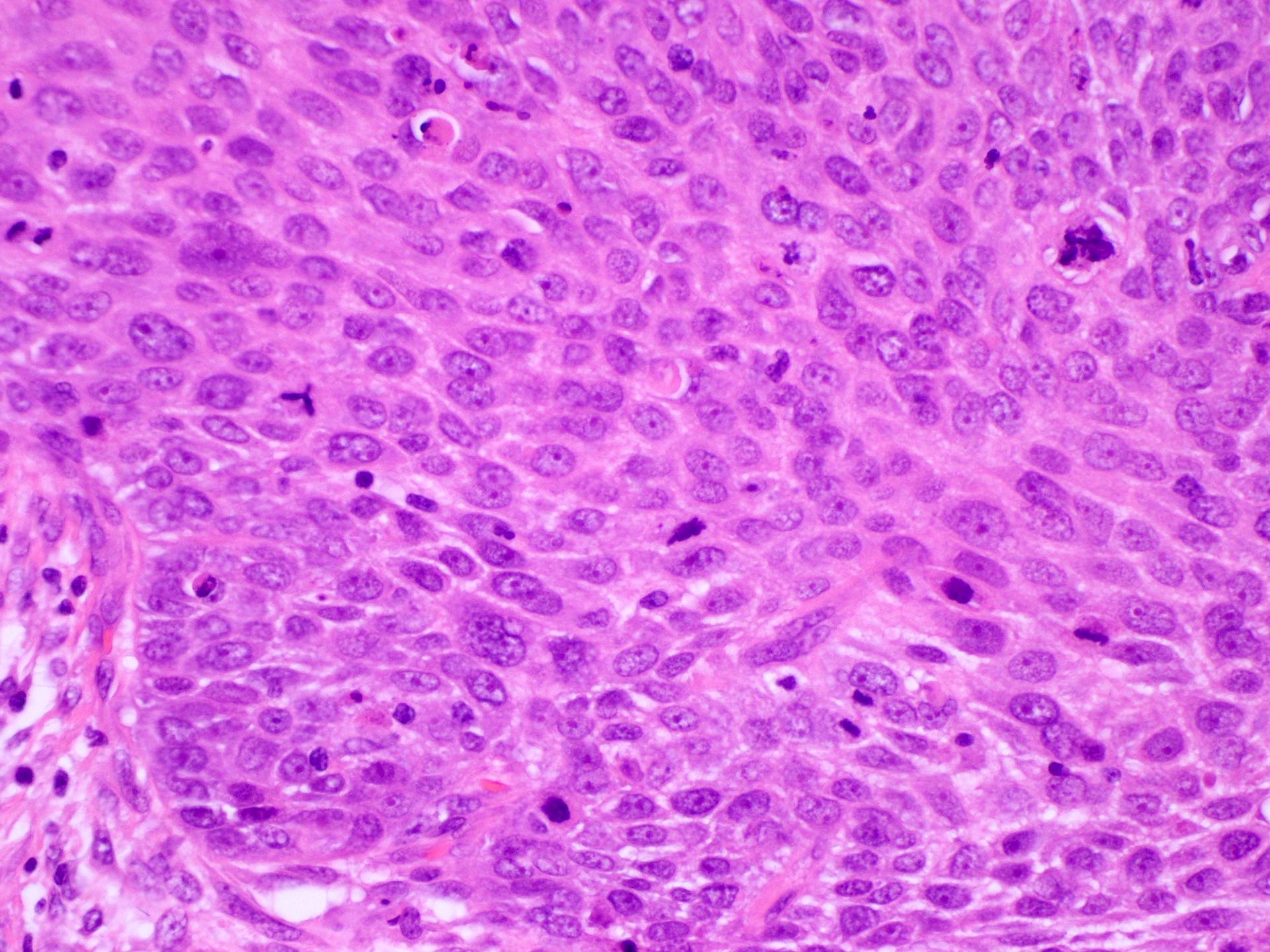
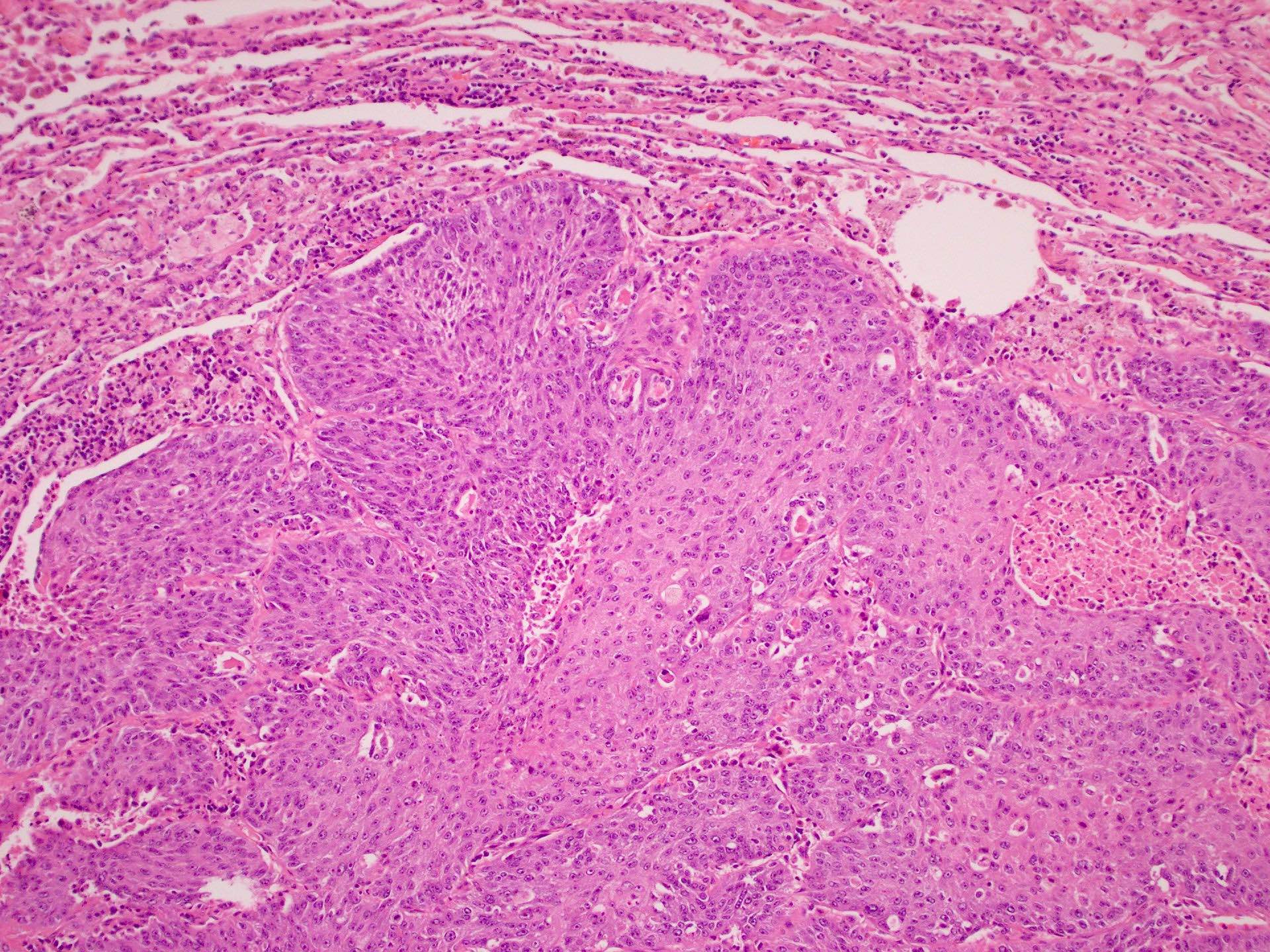
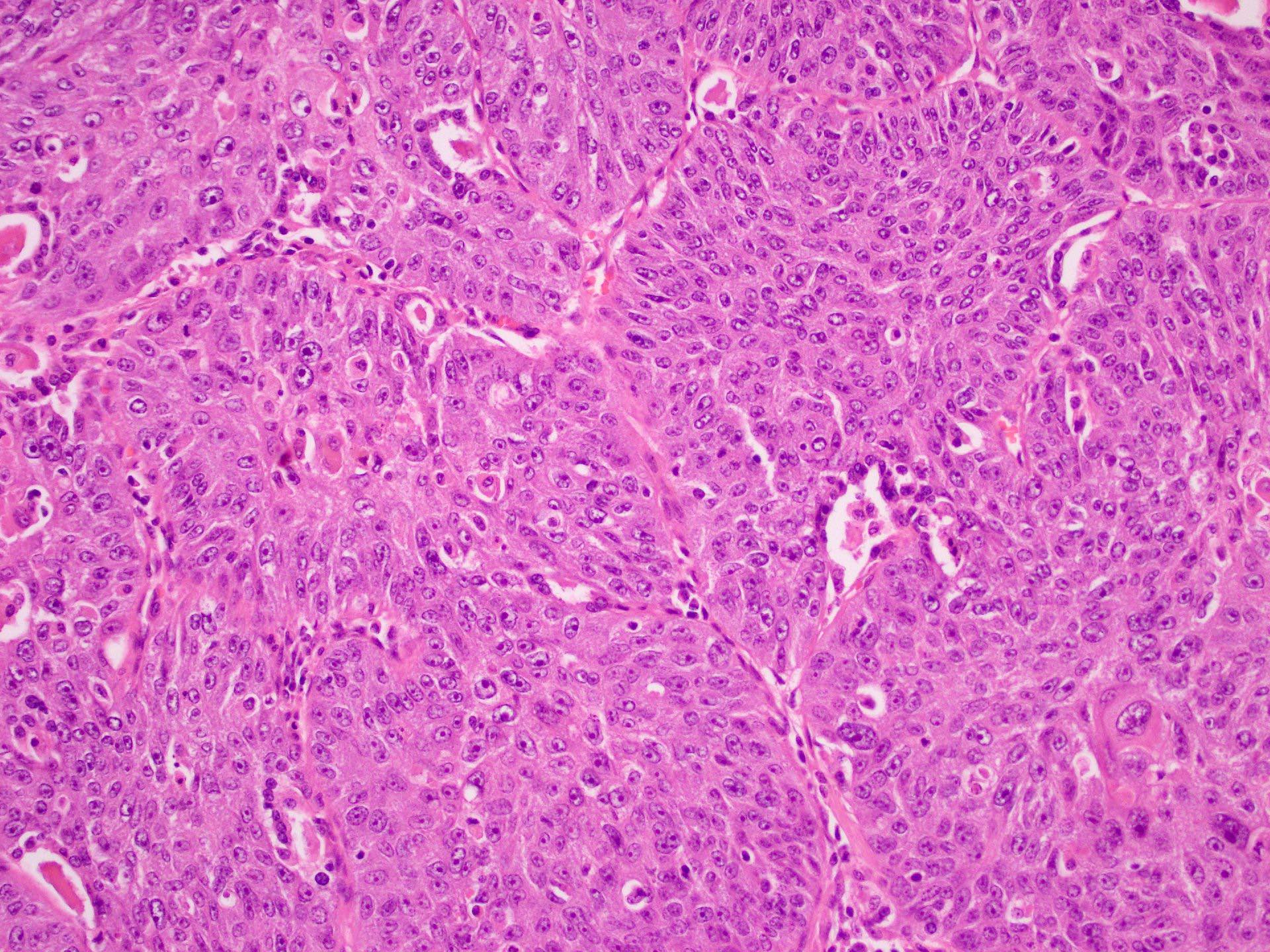
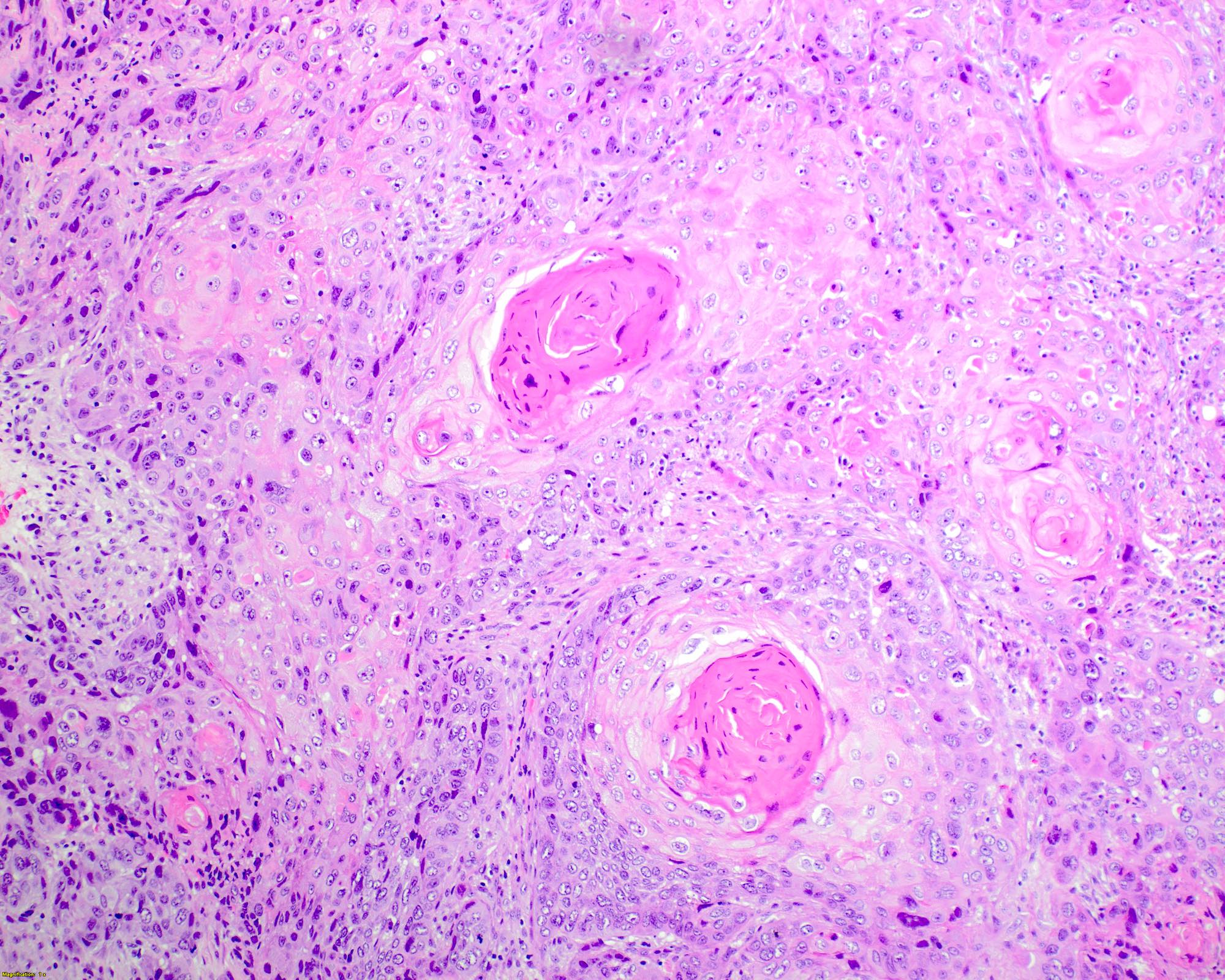
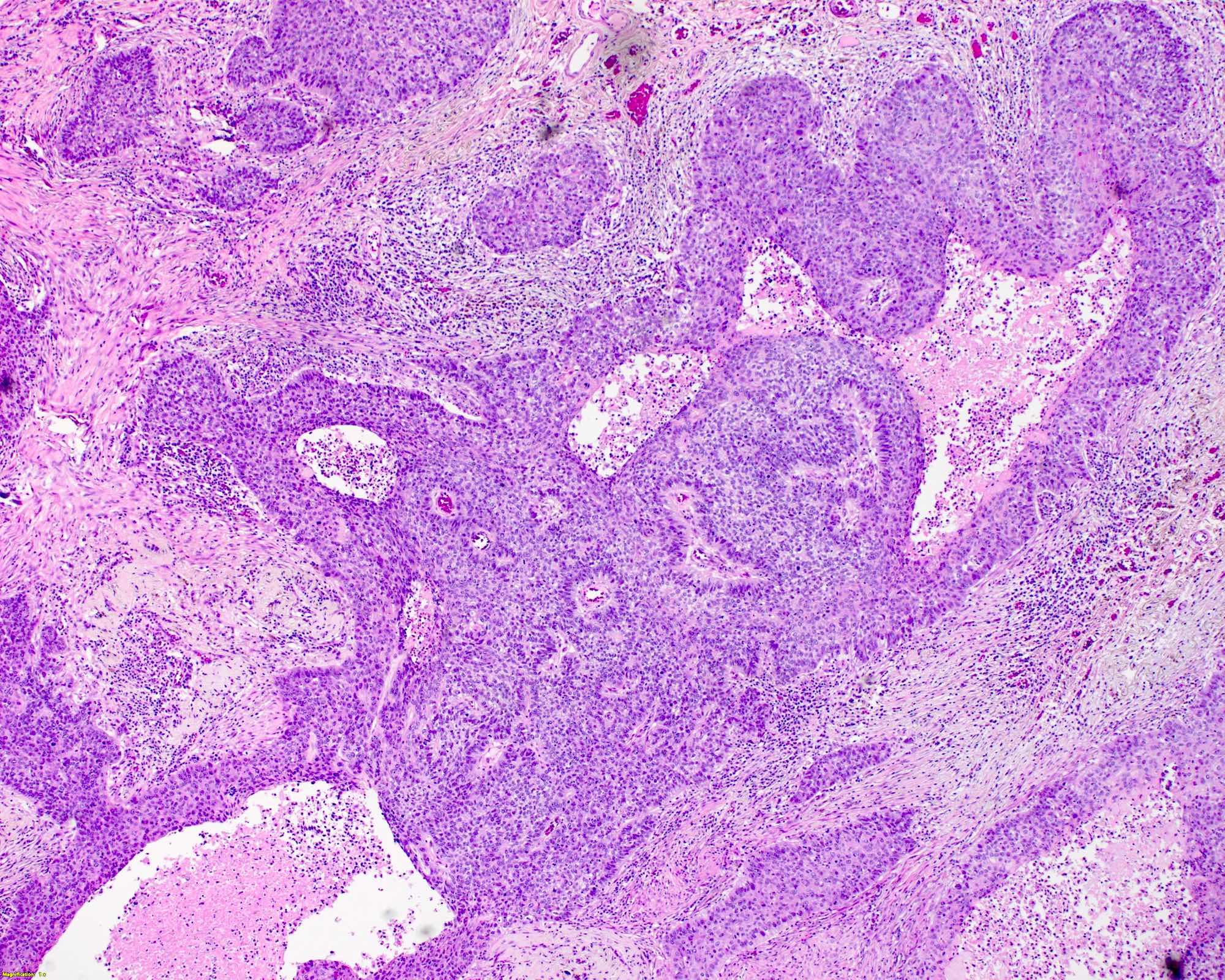
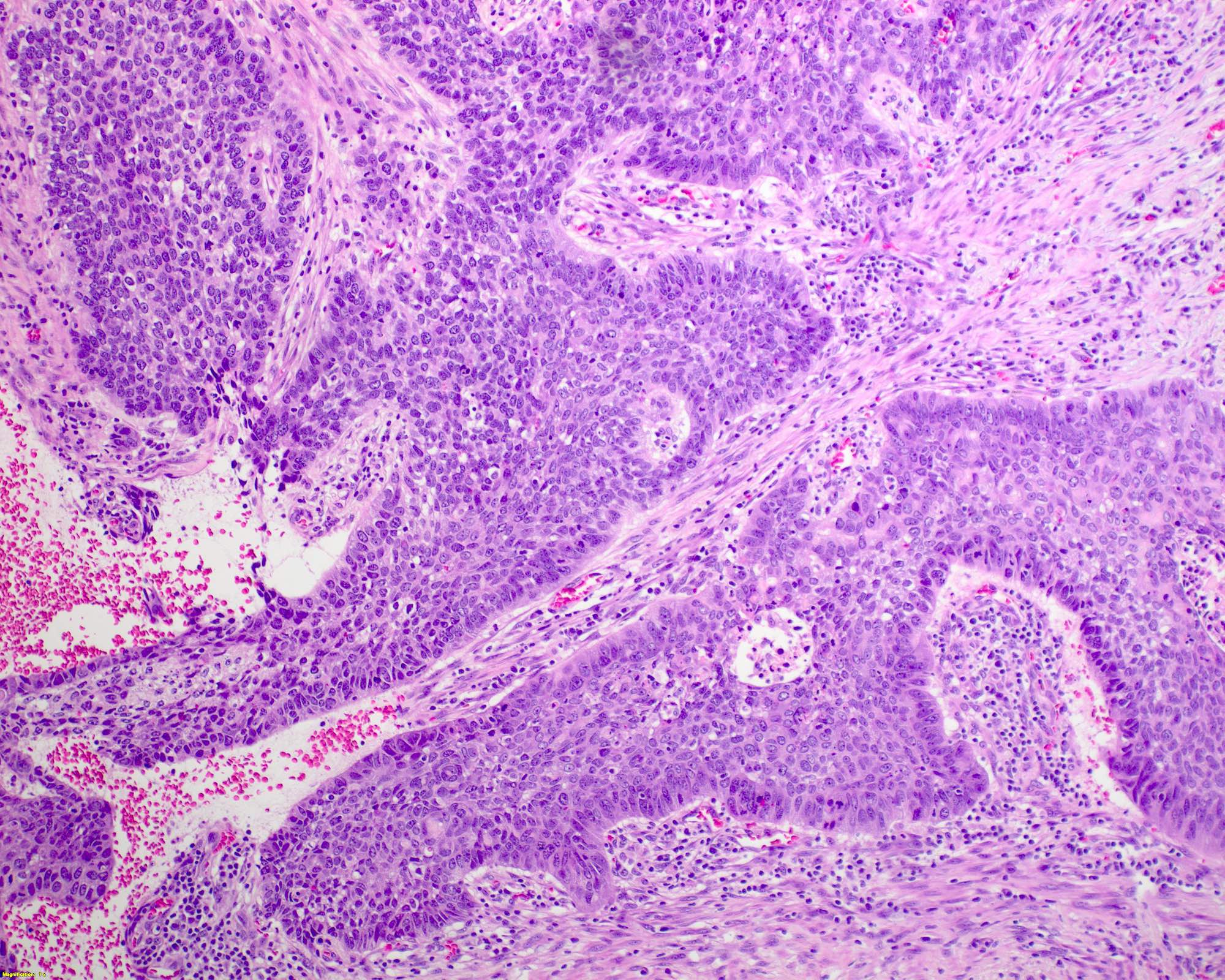
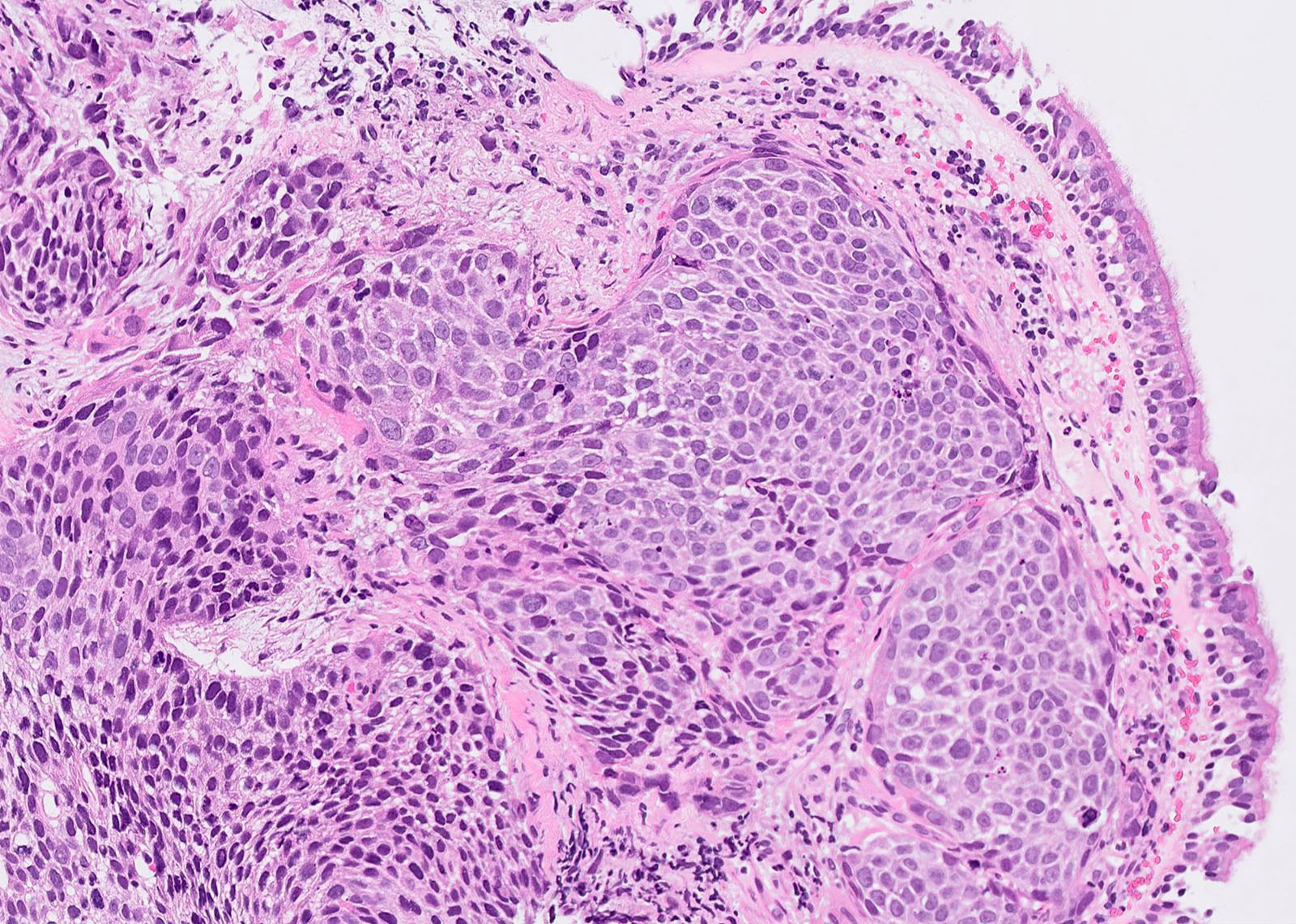
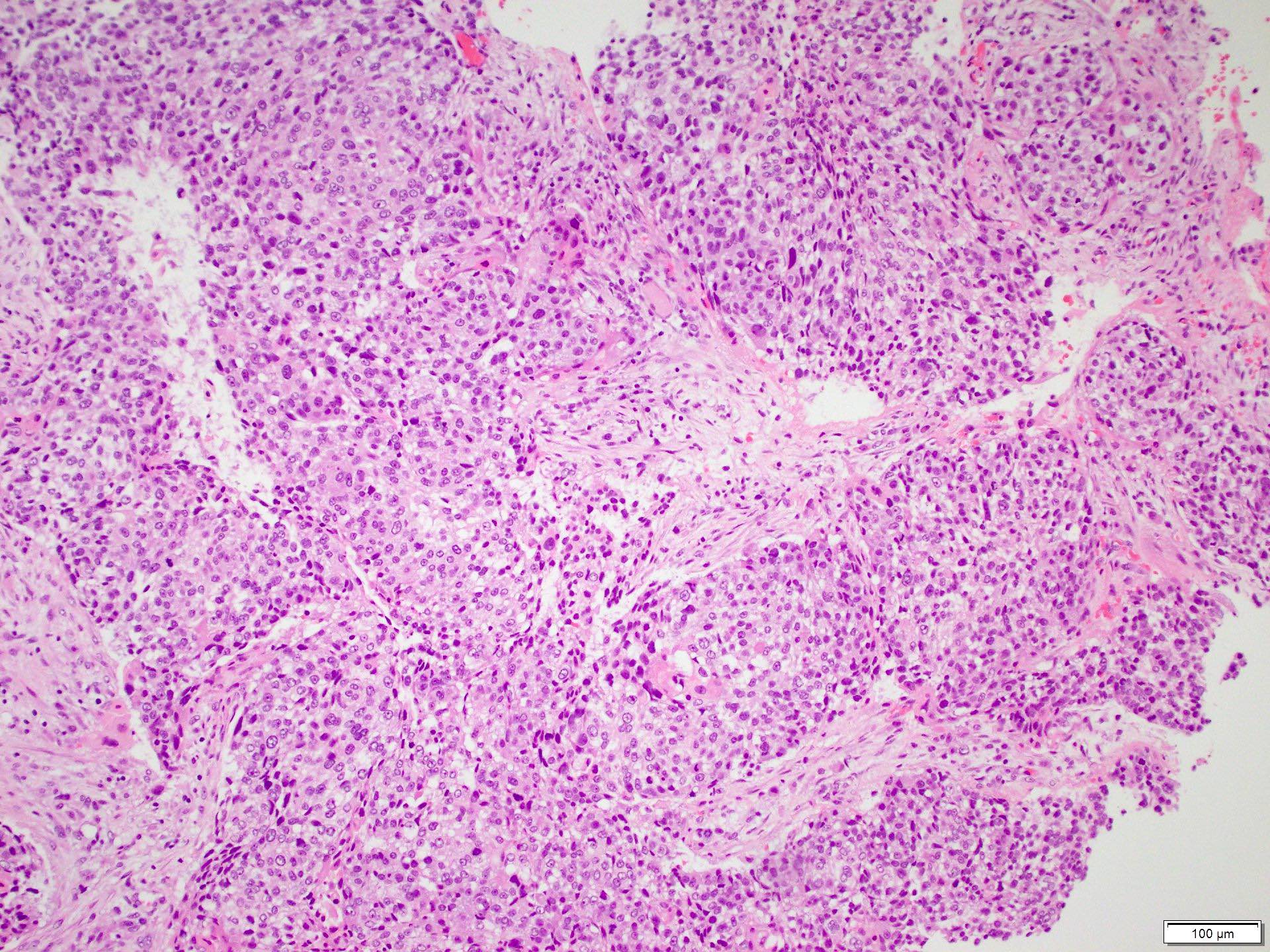
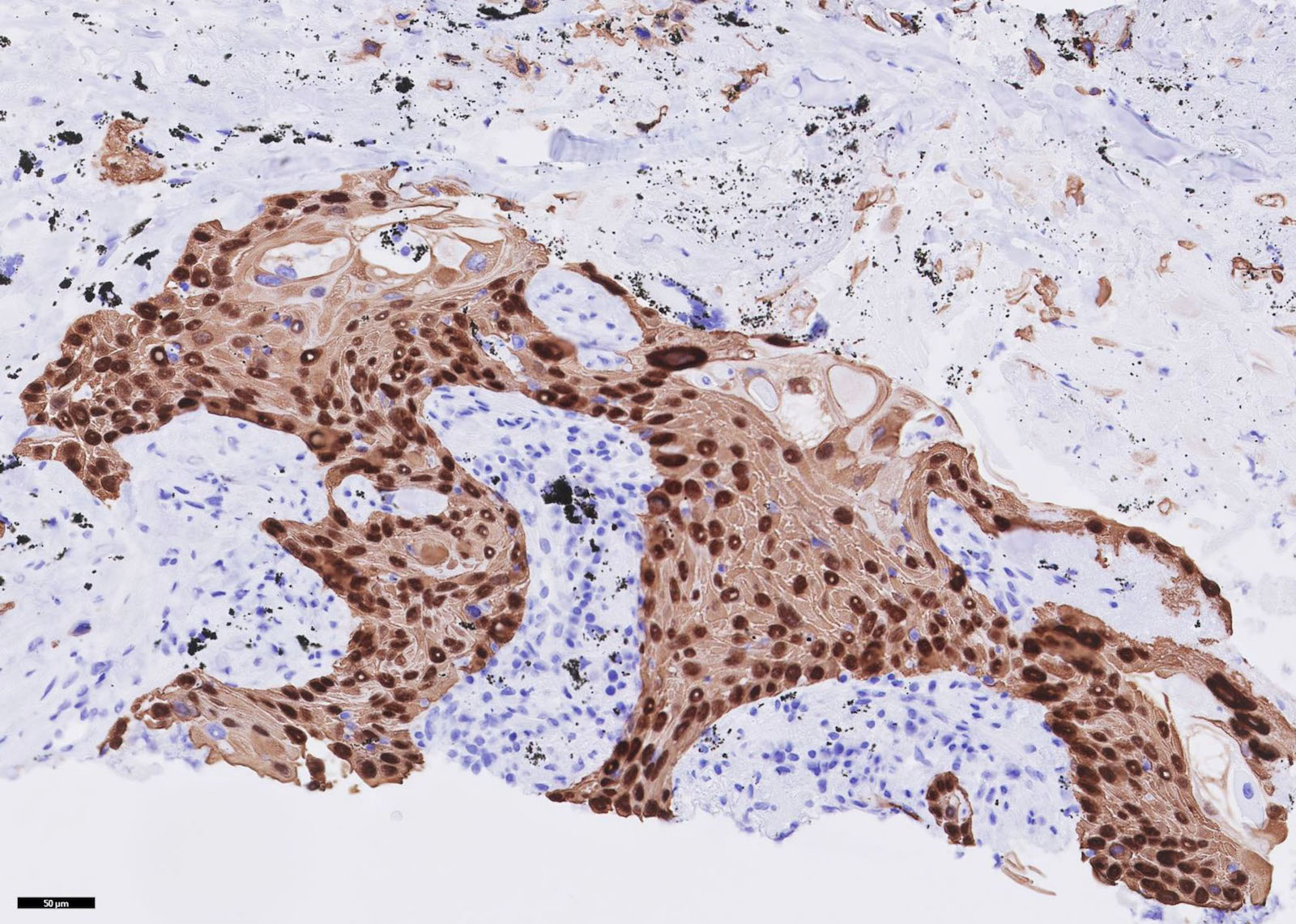
Microscopic (histologic) description
- Presence of keratinization including keratin pearls, intercellular bridging, abundant inflammation and necrosis are all frequent but not required for diagnosis
- There is currently no established grading system for squamous cell carcinoma of the lung and cases and intuitively graded based on the degree of perceived differentiation
- Poorly differentiated squamous cell carcinoma exhibits severe cellular and nuclear atypia, abundant mitosis and often requires IHC studies to differentiate from other poorly differentiated lesions
- Reference: Acad Pathol 2017;4:2374289517705950
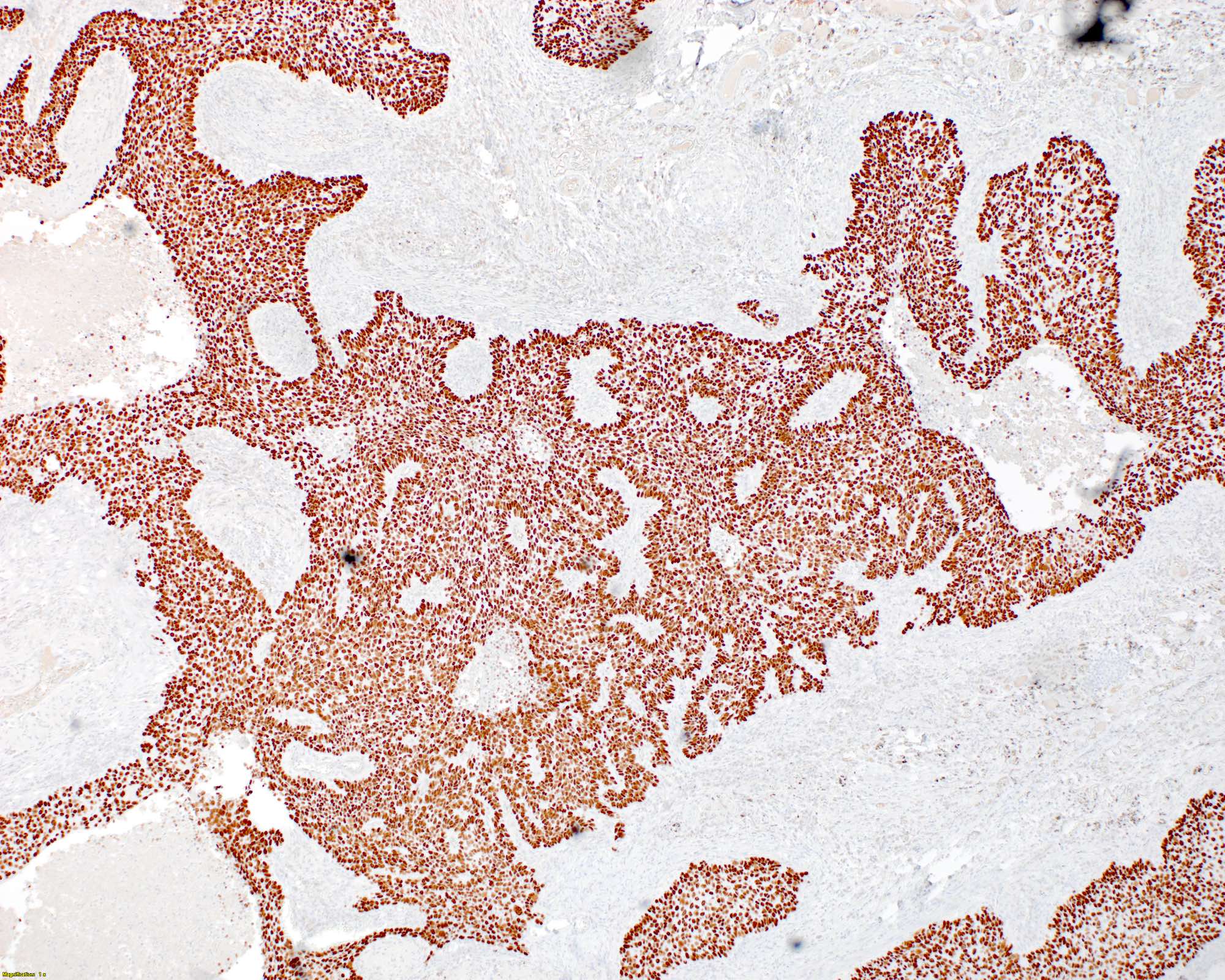
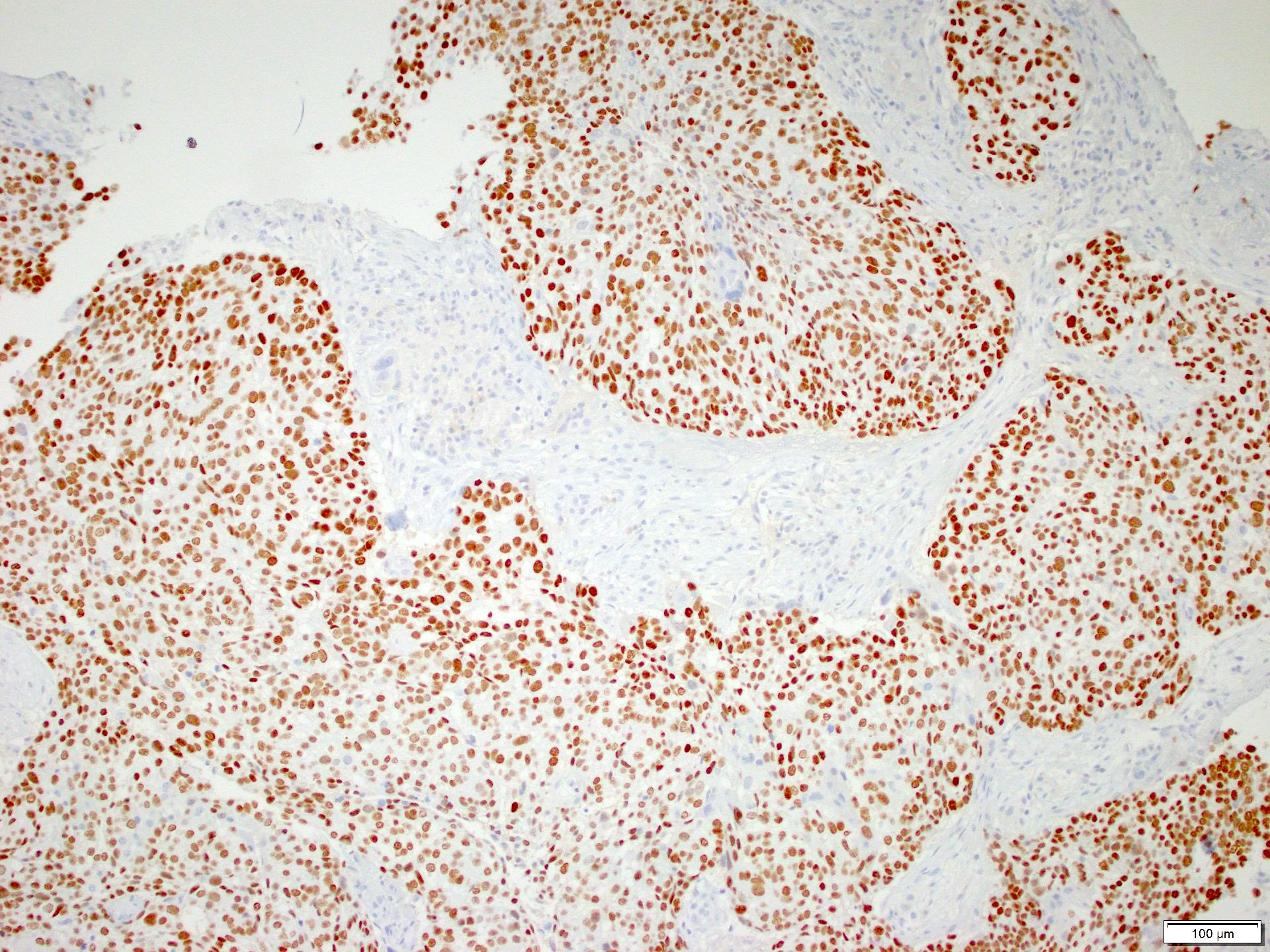
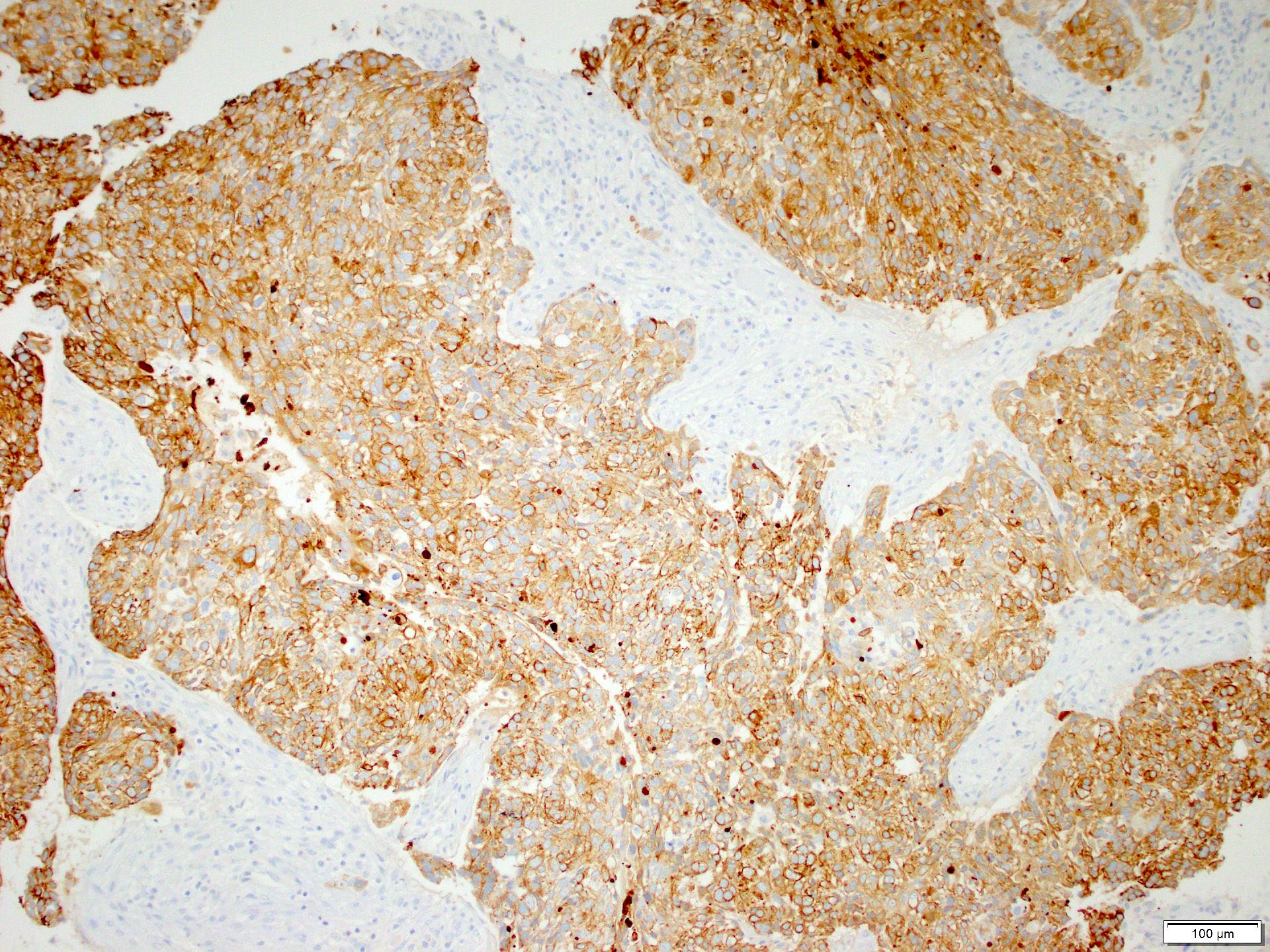
Microscopic (histologic) images
Contributed by Alex McGeough, M.D. and Andrey Bychkov, M.D., Ph.D.
Cytology description
- Atypical cells with keratinization are seen in well differentiated cases
- Higher grade lesions may have similar cytologic appearance to adenocarcinoma and IHC studies can be performed on the cell block to differentiate
- Often demonstrates stretching of the cytoplasm referred to as tadpole cells
- Reference: Int J Clin Exp Pathol 2010;3:367
Positive stains
- p40, p63 are strongly and diffusely positive and are more specific for squamous differentiation; however, p63 is less specific so p40 is preferred
- CK7, high molecular weight keratins, pankeratins and CK5/6 are positive in the majority of cases but will also stain adenocarcinoma (J Pathol 2002;198:100)
- PDL1 expression is variable and is scored using tumor proportion score (Lung Cancer 2017;104:7)
Electron microscopy description
- Abundant tonofilaments, complex desmosomes, basal lamina
Molecular / cytogenetics description
- Abundant molecular alterations are present and testing does not have the prognostic value seen in adenocarcinoma
- Molecular testing for targetable driver mutations is recommended in cases of adenosquamous carcinoma
- EGFR and ALK targetable variants can occur in squamous cell carcinoma; as such, molecular testing may be considered in young or nonsmoking patients
Sample pathology report
- Lung, right upper lobe, wedge resection:
- Invasive, moderately differentiated, keratinizing squamous cell carcinoma (1 cm greatest dimension) (see synoptic report)
- Pathologic tumor stage: pT1a, pN0, pMX
- Margins of resection are free of tumor (4 cm bronchial margin of resection)
Differential diagnosis
- Solid pattern adenocarcinoma:
- High grade small cell carcinoma:
- Usually strongly positive for neuroendocrine markers and may express TTF1
- Also look for precursor lesion
- Melanoma:
- Adenosquamous carcinoma:
- Will have > 10% adenocarcinoma component
- Important to identify as it allows for molecular testing, which may impact prognosis
- NUT carcinoma:
- Positive for NUT IHC or have rearrangements detected by FISH or NGS testing
- Squamous cell metaplasia:
- Arises secondary to lung damage and will not have an associated mass on imaging
- Large cell neuroendocrine carcinoma:
- Mucoepidermoid carcinoma:
- Most often has mucocytes present and lacks keratinization and squamous cell carcinoma in situ
- Lymphoepithelial carcinoma:
- Dense lymphocyte predominant inflammation present
- Not strongly associated with smoking history
- May have positive EBV ISH
- Large cell carcinoma:
- Pleomorphic carcinoma:
- Squamous cell carcinoma elements can be seen admixed with cases of pleomorphic (sarcomatoid carcinoma)
- If there is > 10% spindle or giant cells admixed with squamous cell carcinoma, the WHO recommends classification as a pleomorphic (sarcomatoid) carcinoma
- SMARCA4 deficient undifferentiated tumor
Board review style question #1
Board review style answer #1
B. Intercellular bridges. Intercellular bridging can be easily appreciated between adjacent tumor cells, which is a defining histologic feature of squamous cell carcinoma. Answers A, C and D are incorrect because these are nonspecific findings and can be seen in other lung lesions.
Comment Here
Reference: Lung - Squamous cell carcinoma
Comment Here
Reference: Lung - Squamous cell carcinoma
Board review style question #2
What molecular testing is routinely recommended in squamous cell carcinoma of the lung?
- EGFR
- KRAS
- PDL1
- PTEN
Board review style answer #2
C. PDL1. PDL1 is the correct answer as PDL1 expression assessed by the tumor proportion score (TPS) may predict response to immunotherapy. Answers A and B are incorrect because EGFR and KRAS are only routinely recommended in lung adenocarcinoma. Answer D is incorrect because PTEN is associated with colorectal cancer and thyroid cancer.
Comment Here
Reference: Lung - Squamous cell carcinoma
Comment Here
Reference: Lung - Squamous cell carcinoma
Board review style question #3
Board review style answer #3
C. p40 is the stain of choice for the identification of squamous cell carcinoma and will help demonstrate squamous differentiation. Answers A and B are incorrect because while CK7 and CK5/6 would also both be positive in this lesion, they would not prove squamous differentiation, as they are positive in the majority of lung carcinomas. Answer D is incorrect because TTF1 would support neuroendocrine or adenocarcinoma differentiation instead of squamous.
Comment Here
Reference: Lung - Squamous cell carcinoma
Comment Here
Reference: Lung - Squamous cell carcinoma