Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Immunohistochemistry & special stains | Electron microscopy description | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Wu R. Adenoid cystic carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumorACC.html. Accessed April 26th, 2024.
Definition / general
- #2 most common salivary gland-type carcinoma of lung
- Usually in large bronchi, may involve the trachea
- Prolonged course, but overall prognosis is poor
Essential features
- See also Salivary glands - Adenoid cystic carcinoma
- Primary pulmonary adenoid cystic carcinoma is rare, and metastasis from salivary glands must be excluded
- Morphology is similar to adenoid cystic carcinomas in other sites, with cribriform, tubular and solid patterns
- These tumors tend to arise in association with central airways and spread along neurovascular bundles
Terminology
- Formally called bronchial adenoma, but now considered malignant
ICD coding
- Use code specific for location of tumor
- C34.90 Malignant neoplasm of unspecified part of unspecified bronchus or lung
Epidemiology
- Primary pulmonary adenoid cystic carcinoma is very rare, < 0.2% of lung cancers
- Typically adults
Sites
- Usually central / endobronchial but may be peripheral
Pathophysiology
- Slow growing but persistent, with recurrences over years, potentially with metastasis to lymph nodes and distant sites
Etiology
- Unclear, probably arise from submucosal bronchial glands
Clinical features
- Obstructive symptoms, i.e., pneumonia, dyspnea, cough, wheeze, hemoptysis
- Peripheral lesions asymptomatic
Diagnosis
- Exclude metastasis from salivary glands
Radiology images
Prognostic factors
- Variable by tumor stage
Case reports
- 14 year old girl with large lung mass (BMJ Case Rep 2010 Nov 29;2010)
- 29 year old man with liver metastasis (J Thorac Oncol 2014;9:e67)
- 46 year old woman diagnosed by FNA cytology (Diagn Cytopathol 2011;39:283)
- 75 year old woman with peripheral adenoid cystic carcinoma (World J Surg Oncol 2010;8:74)
Treatment
- Complete surgical excision
- Radiation therapy (Ann Thorac Surg 2016;101:294)
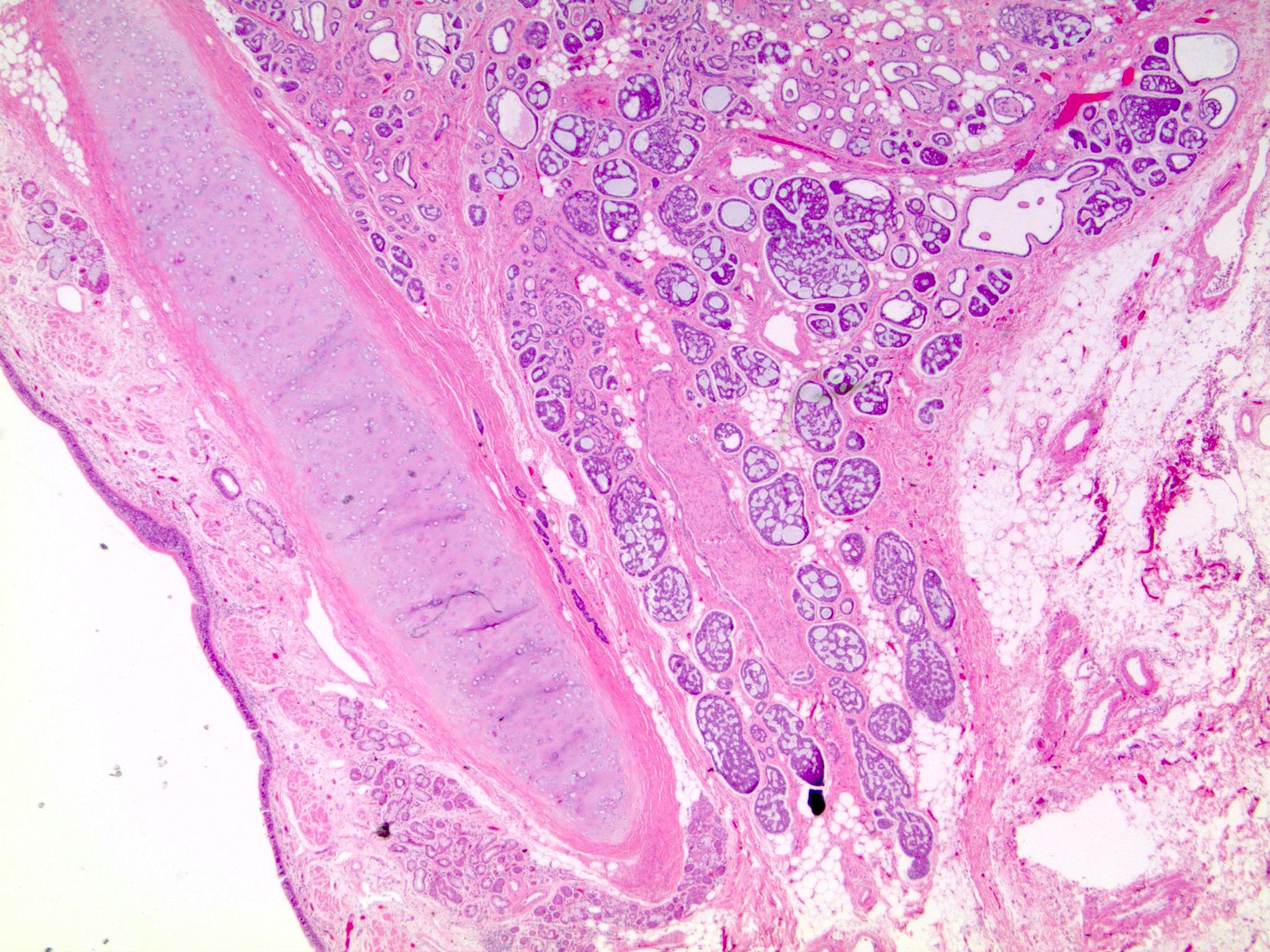
Gross description
- Large, centrally located, polypoid, intrabronchial mass
- May grow along bronchi (subepithelial) causing thickened bronchial wall
- Circumscribed, soft, yellowish white
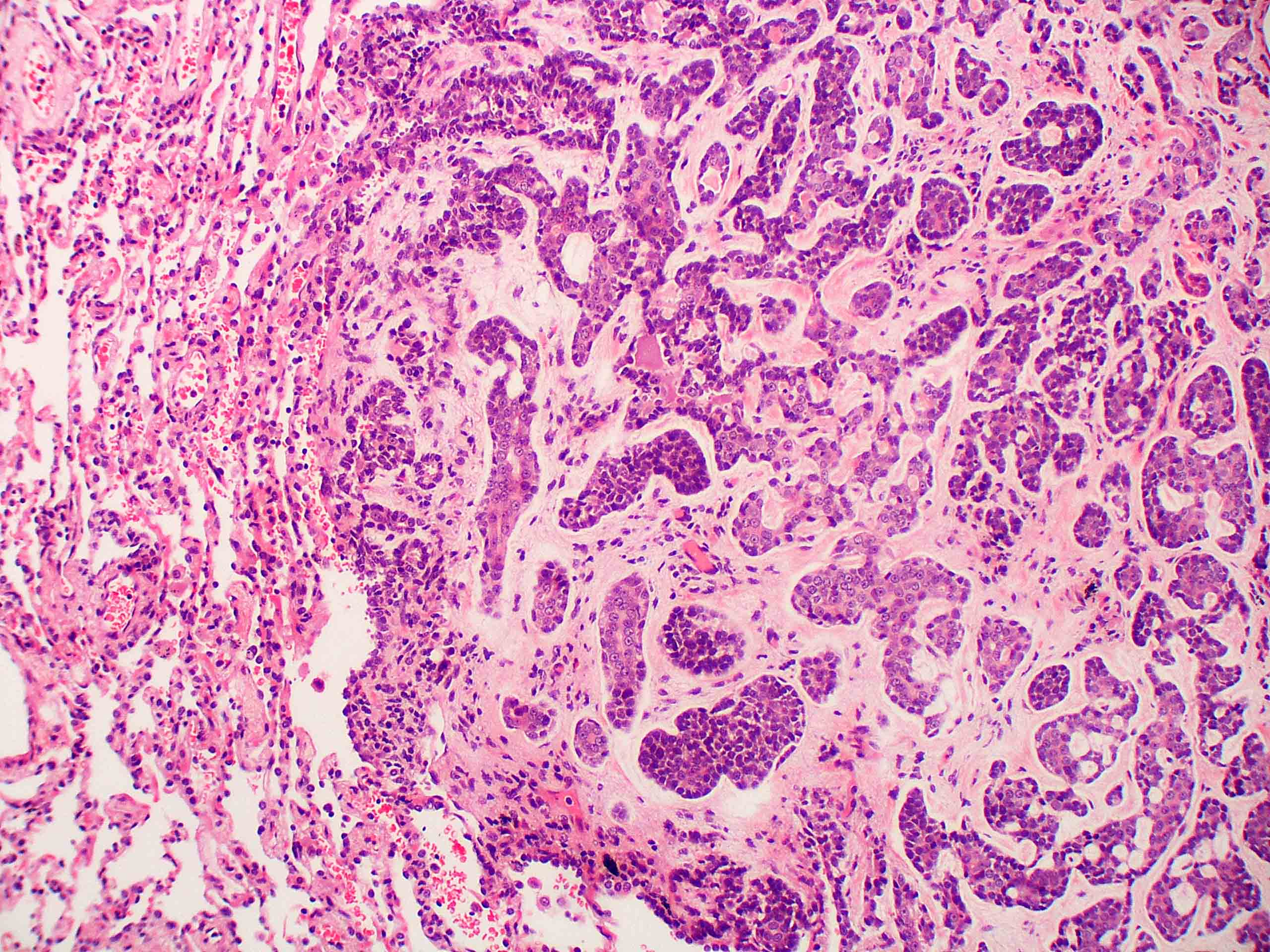
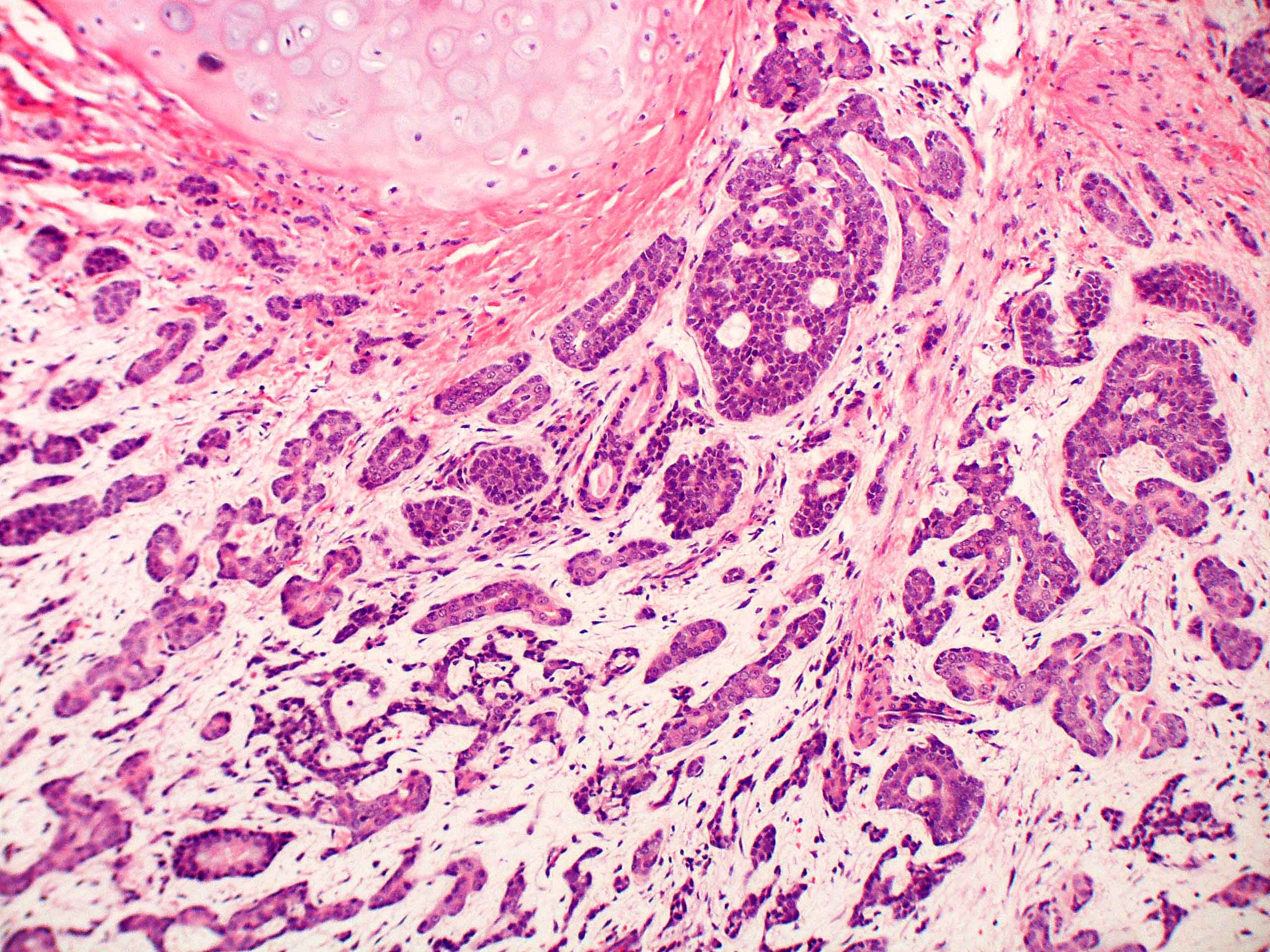
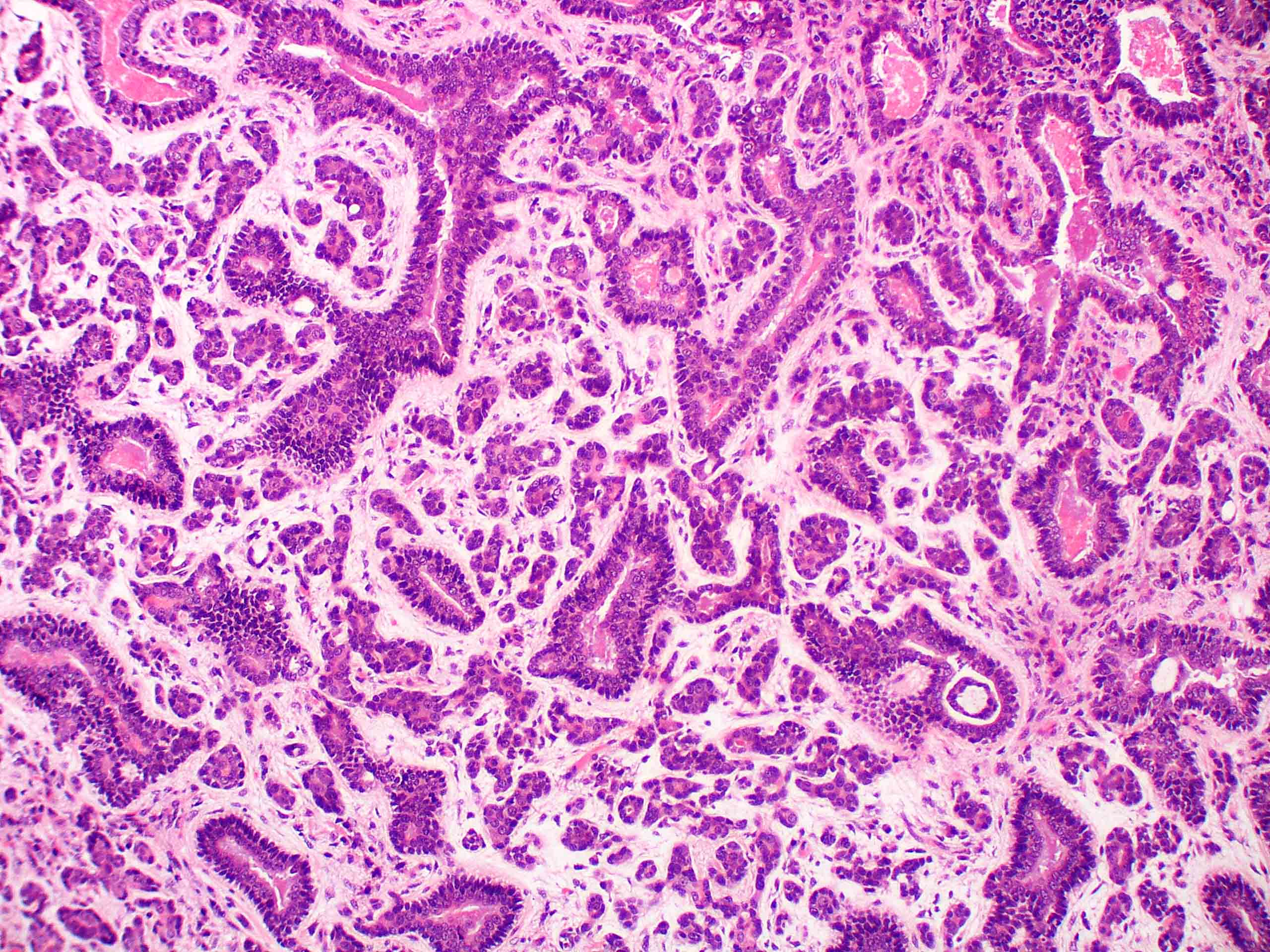
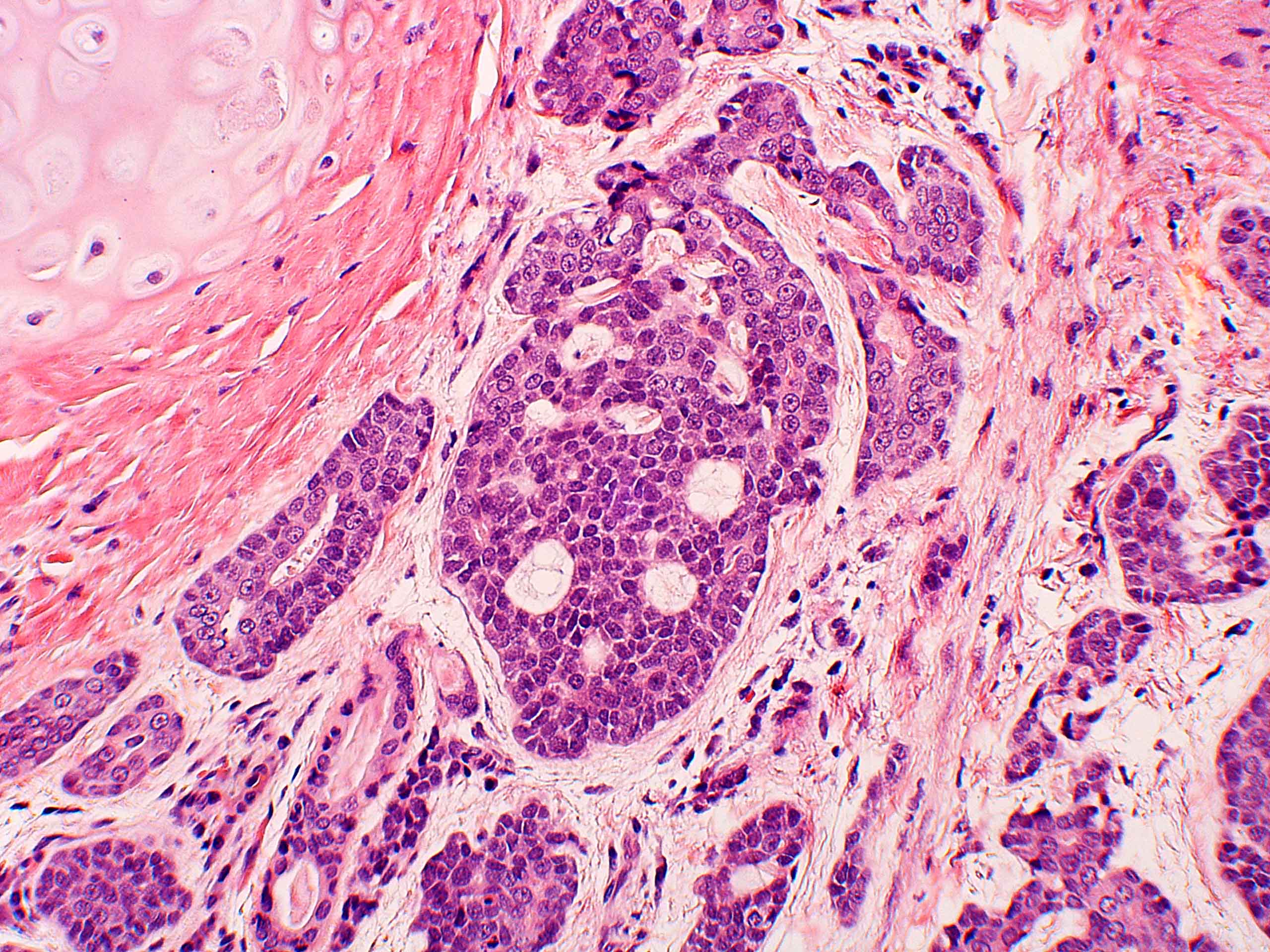
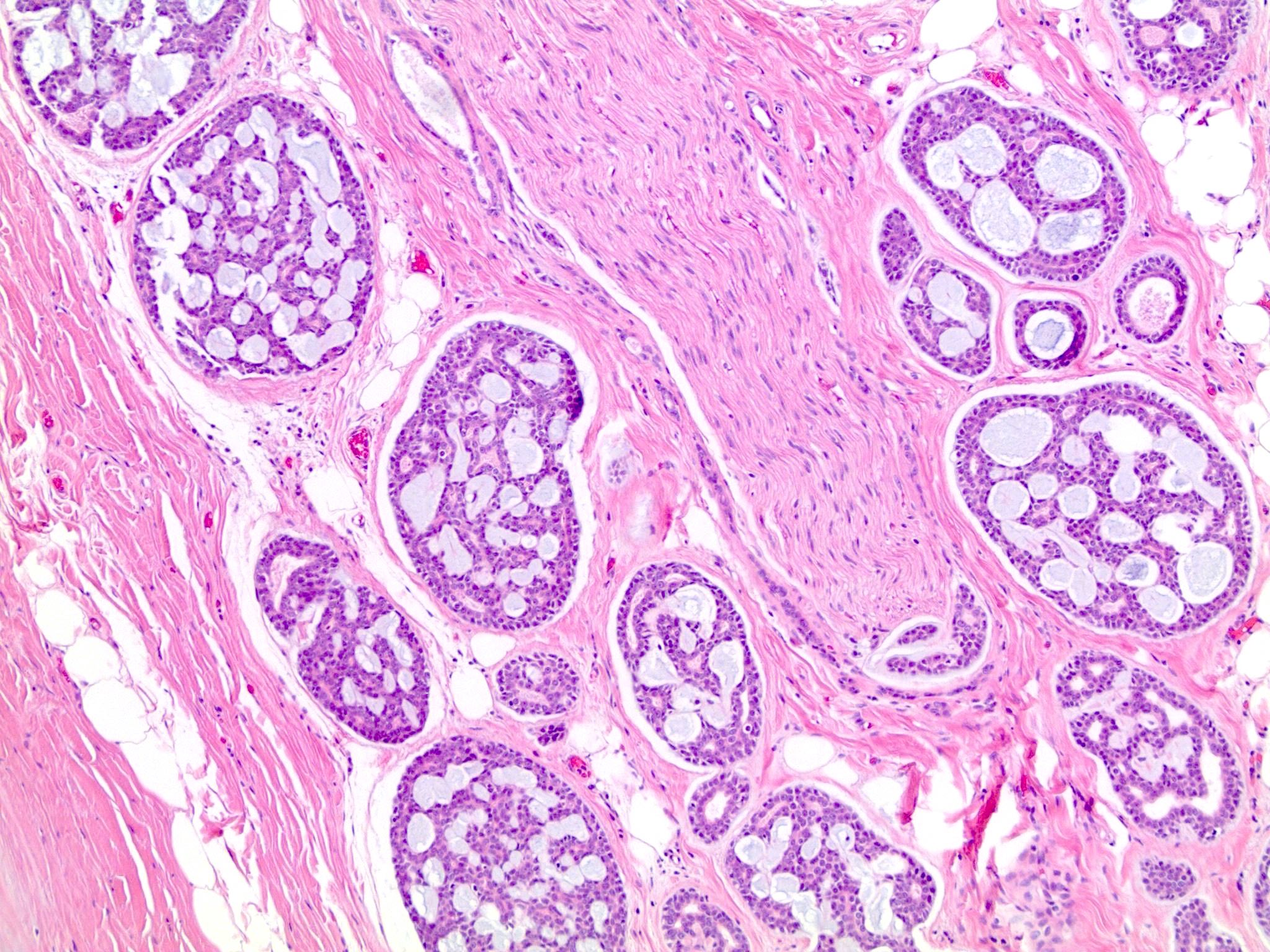
Microscopic (histologic) description
- Propensity for tracking along nerves and cartilaginous plates → bronchial margins more often positive than in other lung cancers
- Infiltrative growth, cribriform / cylindromatous (islands and nests, with luminal matrix), tubular (gland-like spaces) or solid (insular, with scant matrix) - usually a mix of patterns are seen
- Defining features are pseudocysts (rounded extracellular space containing basal lamina), intercellular spaces, basal lamina and true glandular lumens (Hum Pathol 1982;13:916)
- Monotonous, polygonal, basaloid cells
- Absence of mitoses, nuclear pleomorphism, necrosis and hemorrhage in most cases; solid type may show more mitoses
Microscopic (histologic) images
Cytology description
- Cylinders or spheres of myxochondroid matrix within epithelial groups
- Diagnosis more difficult if matrix is scarce, as in solid type
- Cellular uniformity, distinct nucleolus, granular cytoplasm, distinct cell border, organoid cluster, hyaline globule and hyaline basement membrane material (J Pathol Transl Med 2015;49:511)
Immunohistochemistry & special stains
- Usually not necessary for diagnosis
- Luminal cells: c-kit/CD117+, p63-, actin-
- Basal (myoepithelial) cells: c-kit/CD117-, p63+, actin+
- Tumor cells are usually positive for keratin and S100, and negative for neuroendocrine markers
- Basement membrane material is positive for collagen type IV or laminin
Electron microscopy description
- May show evidence of partial myoepithelial differentiation
Molecular / cytogenetics description
- t(6;9) MYB rearrangement in 41% of pulmonary adenoid cystic carcinomas, not associated with clinical features or prognosis (J Thorac Oncol 2015;10:1570)
- Generally do not have similar mutations as primary adenocarcinoma (Diagn Pathol 2015;10:161)
Differential diagnosis
- Basal cell adenocarcinoma: distinction from solid adenoid cystic carcinoma may be impossible
- Basaloid squamous cell carcinoma: may have adenoid cystic carcinoma-like pattern of microcystic spaces containing mucin, surrounded by small tumor cells
- Epithelial-myoepithelial carcinoma
- Metastatic disease
- Well differentiated adenocarcinoma of the lung: larger cells with more prominent nucleoli
Additional references