Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Qiao JH. Pulmonary placental transmogrification. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumorplacentaltrans.html. Accessed December 14th, 2024.
Definition / general
- Pulmonary placental transmogrification is a rare lesion, characterized by cystic lesions of the lung
- First described in 1979 by McChesney (Lab Invest 1979;40:245)
Essential features
- Placental transmogrification or placentoid bullous lesion of the lung is an unusual condition in which the alveoli develop a peculiar villous configuration that resembles placental villi at low microscopic magnification
- Villous appearance probably results from the development of edema and fibrosis in the residual strands of alveolar tissue present in the enlarged airspaces of severe emphysema
- Placental transmogrification of the lung has been described in patients with severe emphysema induced by cigarette smoking, congenital giant bullous emphysema and fibrochondromatous hamartomas of the lung
Terminology
- Pulmonary placental transmogrification, bullous emphysema, placentoid bullous lesion
ICD coding
- ICD-10: J98.4 - Other disorders of lung
Epidemiology
- Usually occurs in men aged 20 - 50
- 48% have a history of smoking
Sites
- Lung parenchyma, usually subpleural and unilateral
Etiology
- Etiology and pathogenesis remains unclear
- Hypotheses
- Variant of giant bullous emphysema
- Initial clear cell proliferation followed by emphysema-like cystic change; uncertain if proliferation is clonal (Hum Pathol 2004;35:517)
- Congenital hamartomatous malformation
- Can have fatty infiltration (Mod Pathol 1997;10:846)
- May be the result of metaplastic mesenchymal differentiation
- Occasionally, pulmonary lipomatosis is reported as a variant of placental transmogrification
Clinical features
- Patients might be asymptomatic or present with dyspnea, chronic obstructive lung disease, pneumothorax or a combination of these
- Chest tightness, cough and chest pain
Radiology description
- CT or MRI shows unilateral localized emphysematous bulla with soft tissue and fat composition / density (Korean J Radiol 2013;14:977, AJR Am J Roentgenol 2004;183:99)
Prognostic factors
- A few patients with incomplete resection of pulmonary bullae have recurrent disease
Case reports
- 14 year old boy with right middle and lower lobe involvement (Int J Surg Pathol 2017;25:716)
- 30 year old woman with a high density shadow of the lower lung and 59 year old man with chest tightness (Medicine (Baltimore) 2017;96:e7733)
- 31 year old woman with cough and dyspnea (Korean J Radiol 2013;14:977)
- 32 year old man with Swyer-James (MacLeod) syndrome (Arch Pathol Lab Med 2005;129:686)
- 38 year old man with no risk factor for emphysema (Indian J Chest Dis Allied Sci 2006;48:147)
- 39 year old man with case presenting as emphysema and a lung mass (Ann Thorac Surg 2009;87:615)
- 41 year old man and 51 year old man with smoking history, one with giant bulla and the other with cystic nodule (Hum Pathol 2004;35:517)
- 44 year old man with case presenting as giant bullae with soft fatty components (Eur J Cardiothorac Surg 2008;33:124)
- 45 year old man with case presenting as tension pneumothorax (J Thorac Cardiovasc Surg 2008;136:778)
- 72 year old man whose clinical presentation mimicked lung carcinoma (Asian Cardiovasc Thorac Ann 2016;24:811)
Treatment
- Surgical resection, including video assisted thoracoscopic surgery (VATS), pneumonectomy or lobectomy
- Surgical resection is usually curative and leads to successful improvement of symptoms and quality of life
- Lymph node dissection is unnecessary
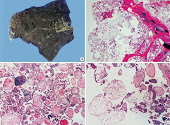
Gross description
- Resembles cystic lesions with variable amounts of intracystic papillary proliferation
- Affected areas are replaced or filled by gelatinous tissues described as bubbly, vesicular, grape-like or sponge-like
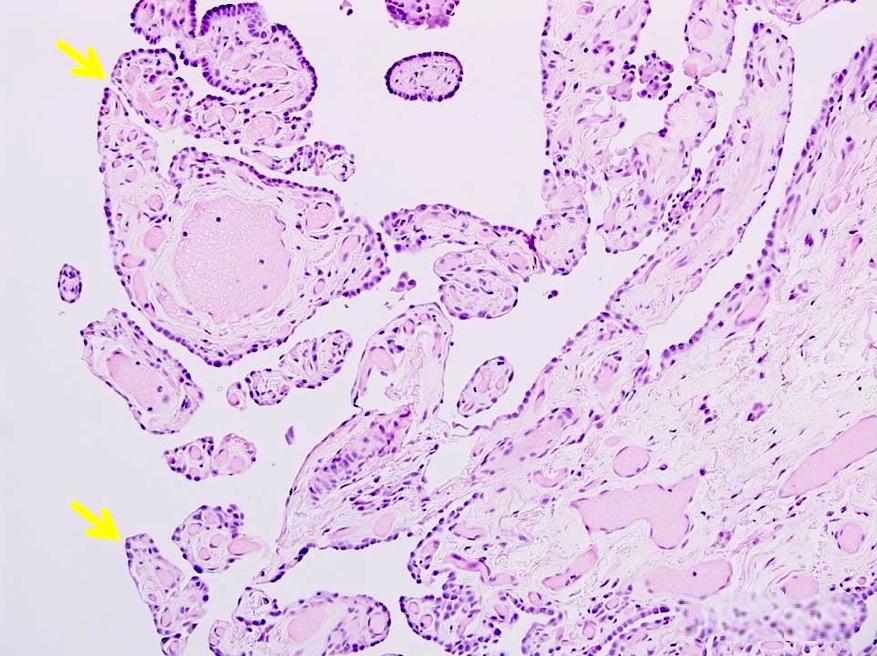
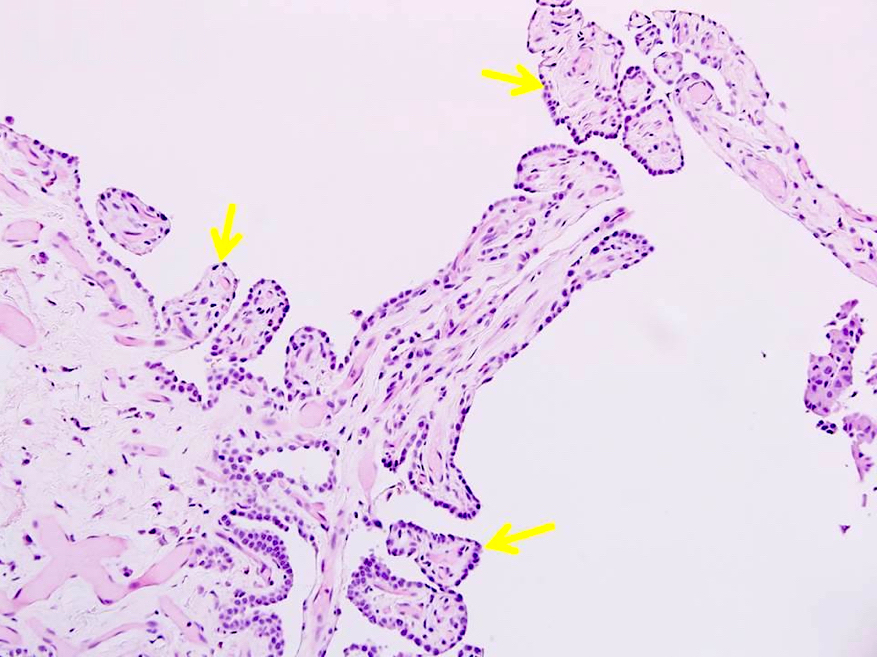
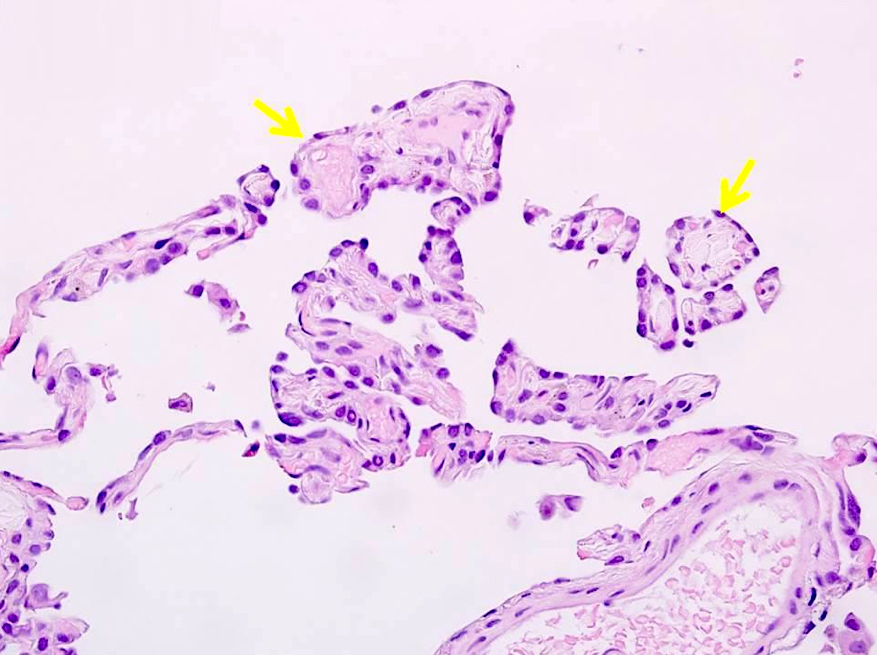
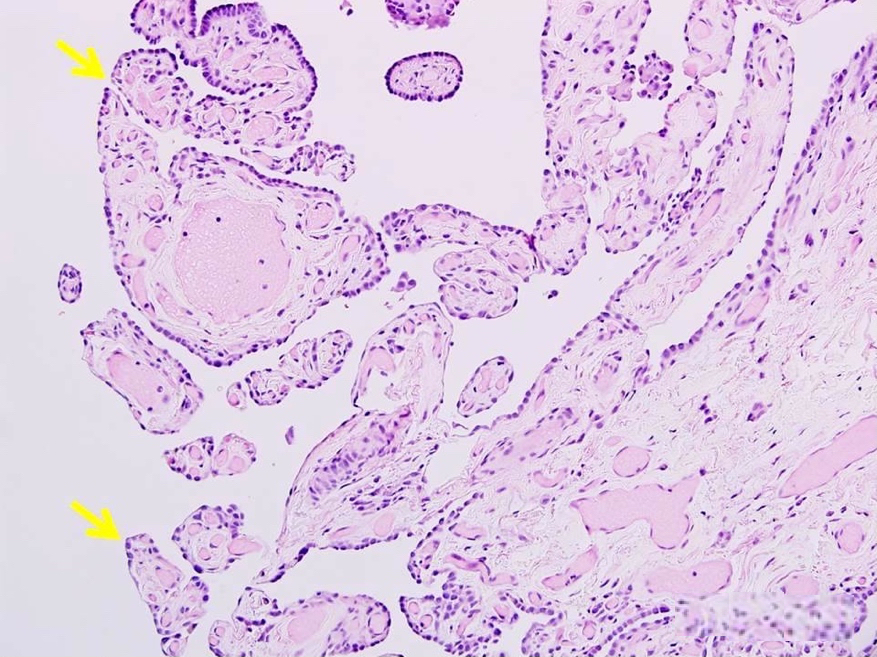
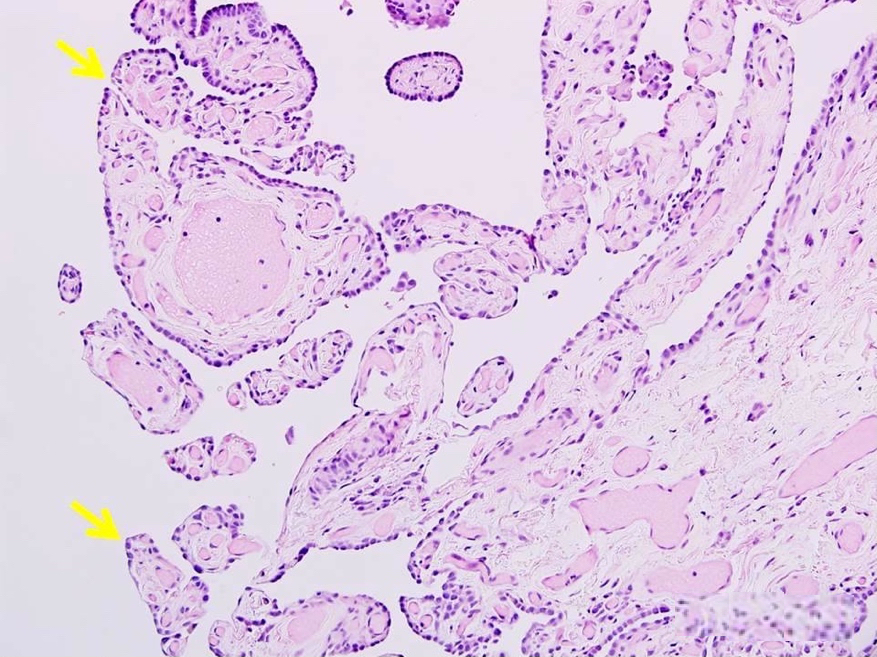
Microscopic (histologic) description
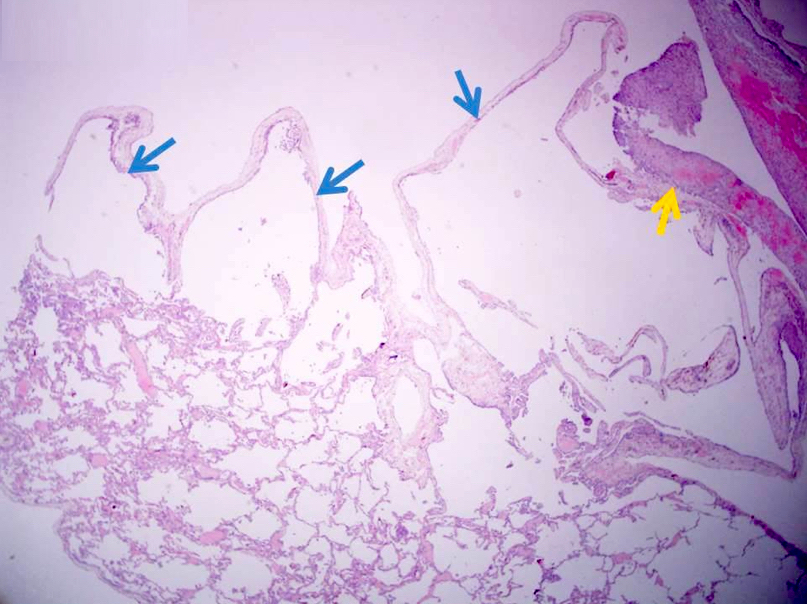
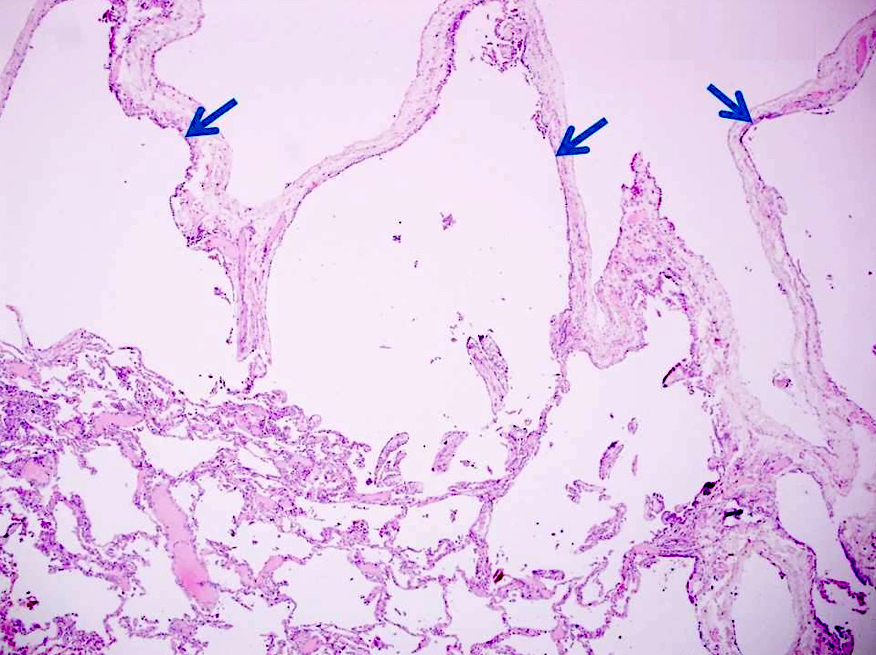
- Bullous emphysema / cystically dilated airspaces, usually subpleural
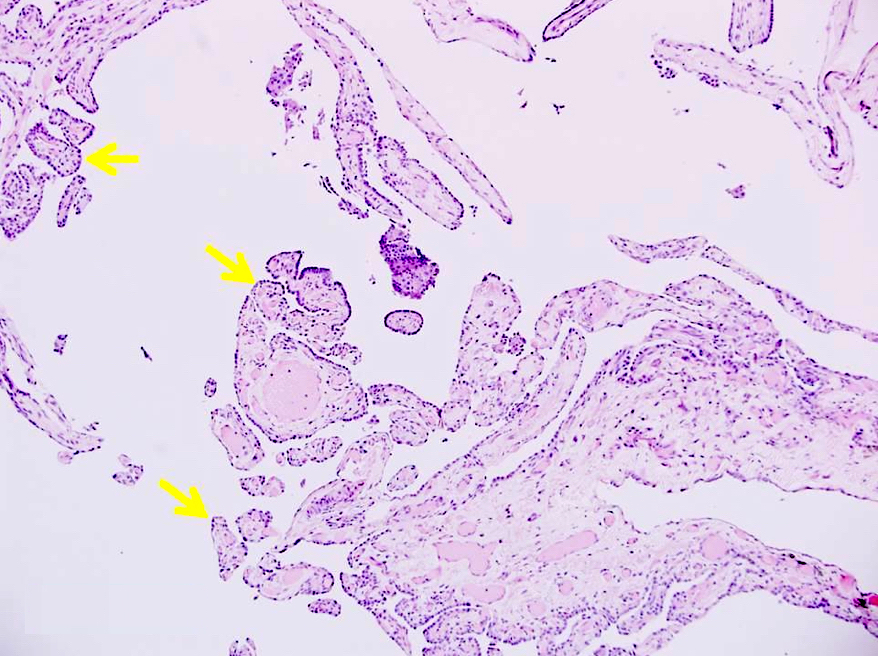
- Intracystic proliferation of variable sized papillary structures, which are morphologically similar to mature chorionic villi
- Cores of papillary / villous structures contain congested capillary sized vessels
- Papillary / villous lesions are surrounded by hyperplastic alveolar pneumocytes
- Infiltration of mature adipocytes is sometimes identified in papillary / villous lesions
- Pleural reactive changes are present and usually secondary to pneumothorax, including granulation proliferation, acute hemorrhage and infiltration of eosinophils
Microscopic (histologic) images
Positive stains
Molecular / cytogenetics description
- Interstitial clear cells were dissected by laser capture microdissection in 2 cases, DNA of interstitial clear cells were extracted and used for studies of 19 microsatellites by PCR (polymerase chain reaction) and automatic sequencer (Hum Pathol 2004;35:517)
- Microsatellite alterations were observed in 13 markers in case 1 and in 8 markers in case 2
- Loss of heterozygosity (LOH) was found in 1 chromosomal region in case 1 and none of the tested regions in case 2
Differential diagnosis
- Intralobar pulmonary sequestration:
- Mass of abnormal pulmonary tissue that does not communicate with the tracheobronchial tree and is supplied by an anomalous systemic artery (J Pediatr Surg 1993;28:802)
- Lesion is solid rather than cystic; in addition, there is no villous papillary proliferation
- Congenital cystic adenomatoid malformation (CCAM) / congenital pulmonary airway malformation (CPAM):
- Uncommon in adults (Diagn Pathol 2012;7:37)
- Cysts are lined by ciliated columnar type epithelium, not pneumocytes
- Bronchogenic cysts:
- Closed sacs considered to be the result of an abnormal budding of the respiratory system
- Lined by ciliated epithelium and have focal areas of hyaline cartilage, smooth muscle and bronchial glands within their walls (Ann Thorac Surg 1991;52:6)
- Ciliated bronchial cells are CK7+ and CK20-
- Cystic lung carcinoma:
- Cystic airspaces preceded by nodules can evolve into non small cell lung carcinoma
- Wall thickening or mural nodularity may develop
- Location in the periphery of the upper lobes, emphysema, additional cystic lesions or ground glass nodules, lymphadenopathy and prior lung carcinoma should further increase suspicion (J Thorac Imaging 2017;32:176)
- Histologic sections and cytology smears will show malignant tumor cells
Additional references
- Am J Surg Pathol 1995;19:563, Ann Thorac Surg 1997;64:226, Pneumologie 1997;51:550, J Thorac Cardiovasc Surg 1999;118:966, J Thorac Imaging 2005;20:233, Am J Respir Crit Care Med 2014;190:e1, Lung 2015;193:855, Thorax 2017;72:284, Autops Case Rep 2017;7:44, Medicine (Baltimore) 2018;97:e0661, Semin Diagn Pathol 2019;36:2
Board review style question #1
Which of the following statements applies to current practice in pulmonary placental transmogrification?
- Complete mediastinal or hilar lymph node dissection is necessary
- It usually occurs in women aged 20 - 50
- Lesion is negative for TTF1
- No patients had a history of smoking
- Surgical resection is the treatment of choice
Board review style answer #1
E. Surgical resection is usually curative and leads to successful improvement of symptoms and quality of life.
Comment Here
Reference: Pulmonary placental transmogrification
Comment Here
Reference: Pulmonary placental transmogrification
Board review style question #2
A young man with pneumothorax and pleural blebs had a VATS lung wedge biopsy performed. Microscopic examination revealed a subpleural emphysematous lesion with the following papillary lesions in dilated airspaces. What is your diagnosis?
- Bronchogenic cyst
- Congenital cystic adenomatoid malformation
- Cystic non small cell lung cancer
- Intralobar pulmonary sequestration
- Pulmonary placental transmogrification
Board review style answer #2
E. Pulmonary placental transmogrification. Papillary lesions are morphologically identical to mature chorionic villi of placental tissue. When these papillary / villous lesions present in dilated airspaces of resected lung, it is diagnostic for pulmonary placental transmogrification
Comment Here
Reference: Pulmonary placental transmogrification
Comment Here
Reference: Pulmonary placental transmogrification