Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Shah S, Husain AN. Infarct / pulmonary emboli. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumorinfarct.html. Accessed April 3rd, 2025.
Definition / general
- Pulmonary embolus (PE) is a blockage of the pulmonary artery or one of its branches due to material (solid, gaseous or liquid) that has traveled through the circulation from elsewhere in the body (StatPearls: Acute Pulmonary Embolism [Accessed 5 October 2022])
Essential features
- Pulmonary embolism is the third most common acute cardiovascular condition worldwide, after myocardial infarction and stroke
- True antemortem clots and emboli display alternating darker and lighter striations due to erythrocyte and fibrin / platelet rich layers (lines of Zahn)
- Thromboembolism is then organized by migrating fibroblasts and myofibroblasts if thrombolysis does not occur within 1 to 2 days
Terminology
- Pulmonary infarct, venous thromboembolism (VTE), pulmonary embolism
ICD coding
- ICD-10: I26.99 - other pulmonary embolism without acute cor pulmonale
Epidemiology
- Third most common acute cardiovascular condition worldwide, trailing only myocardial infarction and stroke (Arterioscler Thromb Vasc Biol 2014;34:2363)
- Responsible for ~100,000 fatalities in the United States annually (Arch Intern Med 2003;163:1711)
- M > F (Arch Intern Med 2003;163:1711)
- Increased incidence with age, particularly in women, to the point that it has an incidence of > 500 per 100,000 after the age of 75 (Am J Med 2013;126:832.e13)
- Risk factors can be divided into genetic versus acquired
- Genetic factors include hypercoagulable conditions, such as factor V Leiden mutation, protein C and S deficiency, prothrombin mutations, antiphospholipid syndrome, etc.
- Acquired risk factors include but are not limited to pregnancy, hospitalization, obesity, oral contraceptive use, malignancy, long bone fracture, stroke, indwelling central venous lines, acute spinal cord injury and patients who have had joint arthroplasty or repair
Sites
- Pulmonary arteries or any of its branches
Pathophysiology
- Pathogenesis of pulmonary embolism is similar to that of thrombus formation (i.e., Virchow's triad)
- Virchow's triad includes venous stasis, endothelial damage and hypercoagulability
- Range of pathophysiologic reactions can occur when an embolus lodges in the lung:
- Pulmonary infarction due to tiny thrombi that lodge distally in segmental and subsegmental arteries in ~10% of people (Chest 1991;100:598)
- Ventilation perfusion mismatch (V/Q mismatch) in the lung is caused by insufficient perfusion, resulting in hypoxemia
- Hypotension due to increased pulmonary vascular resistance (PVR) (Clin Chest Med 1984;5:403)
- PVR increases due to the presence of thrombi and hypoxic vasoconstriction of lung capillaries
- Increased PVR, in turn, obstructs right ventricular outflow, resulting in right ventricular dilatation and flattening or bending of the intraventricular septum
- Both decreased right ventricular flow and right ventricular dilation decrease left ventricular preload, reducing cardiac output
Etiology
- Most emboli originate in the proximal veins of the lower extremities (iliac, femoral and popliteal)
- At the time of presentation, more than half of patients with proximal deep vein thrombosis have concurrent pulmonary embolism (Am J Respir Crit Care Med 2001;164:1033)
- Most thrombi form in lower extremity veins at regions of diminished flow, such as valve cusps or bifurcations
Clinical features
- Common symptoms at presentation include (Chest 1991;100:598)
- Dyspnea at rest or with exertion
- Pleuritic pain
- Cough
- Orthopnea
- Wheezing
- Hemoptysis
- Calf or thigh pain or swelling
- Common presenting symptoms found on examination include (Am J Med 2007;120:871)
- Tachypnea
- Tachycardia
- Calf or thigh swelling, erythema, edema, tenderness, palpable cords
- Rales
- Accentuated pulmonic component of the second heart sound
- Decreased breath sounds
- Jugular venous distension
- Fever, mimicking pneumonia
Diagnosis
- Pretest probability for pulmonary embolism should always be calculated using a validated pretest probability score or approximated clinically if pulmonary embolism is suspected (e.g., Wells score, modified Wells score or modified Geneva score)
- Criteria for Wells and modified Wells score (JAMA 2006;295:172):
- Clinical signs and symptoms of deep vein thrombosis = 3
- Alternative diagnosis is less likely than pulmonary embolism = 3
- Heart rate > 100 = 1.5
- Immobilization for ≥ consecutive days or surgery in the previous 4 weeks = 1.5
- Previously diagnosed with pulmonary embolism or deep vein thrombosis = 1.5
- Hemoptysis = 1
- Malignancy (on treatment, treatment in the last 6 months or palliative) = 1
- Interpretation of Wells and modified Wells score:
3 tier 2 tier - 0 - 1: low risk
- 2 - 6: moderate risk
- > 6: high risk
- ≤ 4: unlikely
- ≥ 4.5: likely
- Computed tomographic pulmonary angiography (CTPA) or magnetic resonance pulmonary angiography (MRPA): a filling defect in any branch of the pulmonary artery (main, lobar, segmental, subsegmental) that becomes evident after contrast enhancement is diagnostic of pulmonary embolism
- CTPA, MRPA: very sensitive and specific, fast and readily available imaging study to rule pulmonary embolism in or out; has essentially replaced conventional angiography
- Chest Xray: wedge shaped infarct after 12 - 36 hours
- Nuclear scan: macroaggregates of labeled albumin with perfusion lung scanning; angiography is the most definitive diagnostic test
Laboratory
- D dimer testing is an excellent validated screening test for thromboembolic disease; a negative result essentially rules out pulmonary embolism
- Laboratory tests are not diagnostic but they can raise clinical suspicion for pulmonary embolism, confirm the presence of other illnesses and offer prognostic information if pulmonary embolism is diagnosed
- These include a complete blood count and serum chemistries, arterial blood gases and D dimer
- Electrocardiogram (ECG) abnormalities are common but nonspecific in those with suspected pulmonary embolism
- The most prevalent findings are tachycardia and nonspecific ST segment and T wave changes (70%) (Eur Respir J 2005;25:843)
Radiology description
- CT scan findings (Insights Imaging 2019;10:114):
- Polo mint sign: the appearance of the polo mint sign inside the pulmonary artery refers to a blood clot surrounded by contrast material
- Railway sign: the railway track sign is used in chest radiography or CT to refer to the presence of contrast in the pulmonary artery surrounding a partial filling defect in the setting of acute pulmonary embolism
- Radiograph findings (Radiopaedia: Pulmonary Embolism [Accessed 5 October 2022]):
- Fleischner sign: enlarged pulmonary artery
- Hampton hump: peripheral wedge of airspace opacity and implies lung infarction
- Westermark sign: regional oligemia and the highest positive predictive value
- Pleural effusion
- Palla sign: enlarged right descending pulmonary artery
- Chang sign: dilated right descending pulmonary artery with sudden cutoff
- Knuckle sign: abrupt tapering or cutoff of a pulmonary artery secondary to a pulmonary embolus
Prognostic factors
- Pulmonary embolism fatalities decreased from 12.8 per 100,000 to 6.6 per 100,000 between 2000 and 2015, as per research that used data from the World Health Organization (WHO) mortality database (Lancet Respir Med 2020;8:277)
- The first 7 days have the highest risk of events; mortality and morbidity are usually caused by shock and recurrent pulmonary embolism during this time
- Variables that predict poor prognosis for individuals with pulmonary embolism:
- Shock and right ventricular dysfunction (Am J Cardiol 1959;4:611)
- Right ventricle thrombus (J Am Coll Cardiol 2003;41:2245)
- Deep vein thrombosis (Am J Respir Crit Care Med 2010;181:983)
- Hyponatremia (< 130 mmol/L) and indicators of renal dysfunction (Heart 2012;98:1221)
- Older age ≥ 65 years (Am J Cardiol 2015;115:681)
- Right heart thrombus (Chest 2017;151:409)
- Poor adherence to guidelines (Eur Respir J 2018;51:1800445)
Case reports
- 37 year old woman with no previous medical history presented with chest discomfort, acute coronary syndrome was suspected and was later determined to be a case of pulmonary embolism (BMC Pulm Med 2019;19:44)
- 40 year old woman developed pulmonary embolism following a 1.5 meter stair fall with a craniothoracic impact point (Ann Med Surg (Lond) 2022;78:103868)
- 51 year old woman with progressive pain in her left shoulder for 6 months developed an asymptomatic pulmonary embolism after shoulder arthroscopy (Orthop Surg 2021;13:1119)
- 55 year old woman was admitted to the acute medical unit with fluctuations in consciousness and in a septic state (BMJ Case Rep 2014;2014:bcr2013201320)
- 61 year old man presented with chest pain, difficulty breathing, hemoptysis and general discomfort and was found to have a massive pulmonary embolism along with S1Q3T3 ECG findings (BMC Cardiovasc Disord 2021;21:224)
Treatment
- Stabilize the patient until a clinical examination and conclusive diagnostic tests are performed
- Start anticoagulation even before establishing the diagnosis of pulmonary embolism if the risk/benefit ratio between the suspicion of pulmonary embolism and the risk of bleeding appears favorable
- Inferior vena cava (IVC) filters should be placed in most pulmonary embolism patients for whom anticoagulation is contraindicated or when the risk of bleeding is high
- For patients who present with hemodynamic instability, thrombolytic therapy, embolectomy and catheter directed modalities like ultrasound assisted thrombolysis are potentially acceptable treatment options
- Elastic graded compression stockings, frequent ambulation and IVC filters are adjunct therapies that can be used in addition to anticoagulation in patients with pulmonary embolism
- References: Am J Cardiol 1959;4:611, Circulation 2005;112:e28
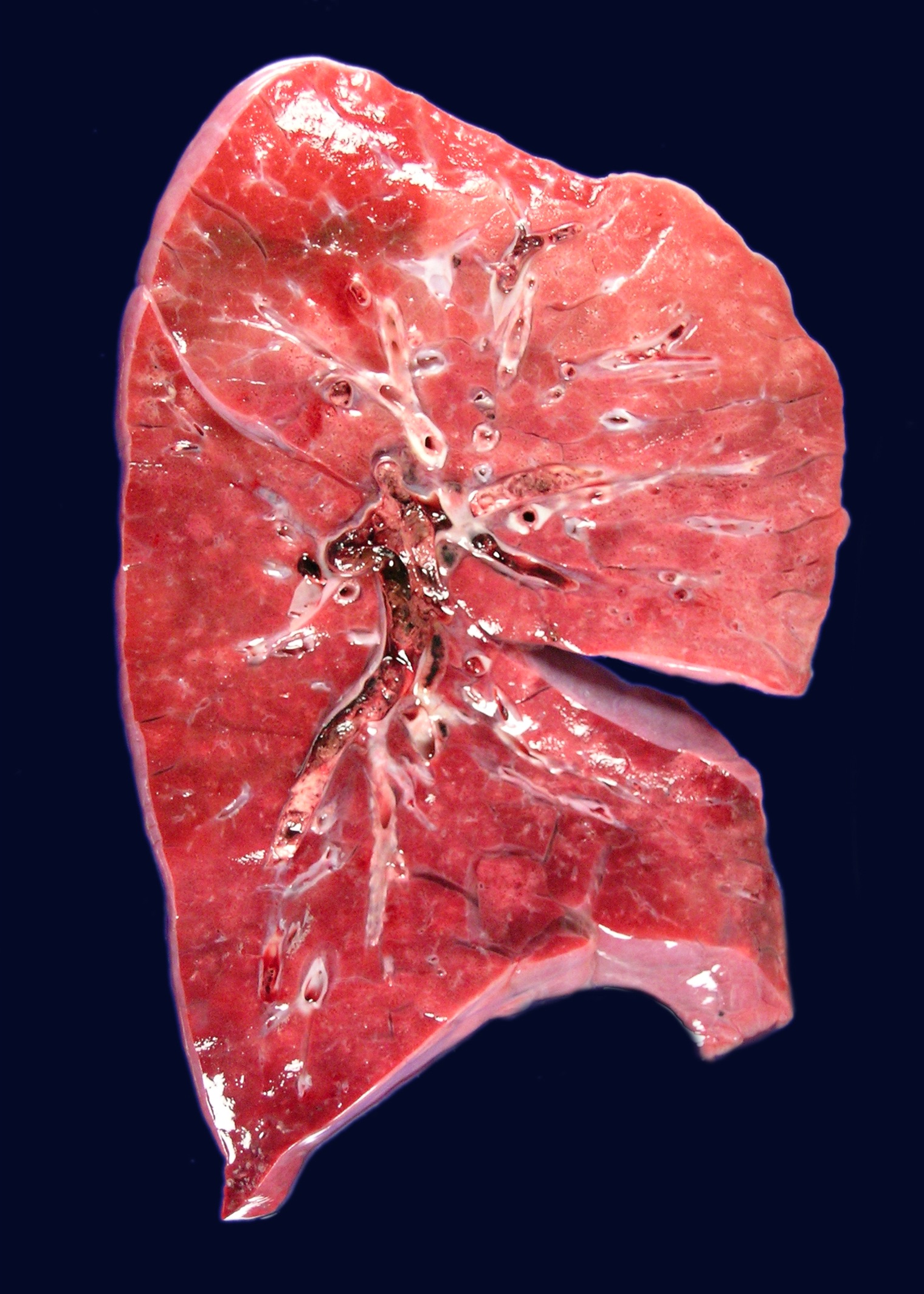
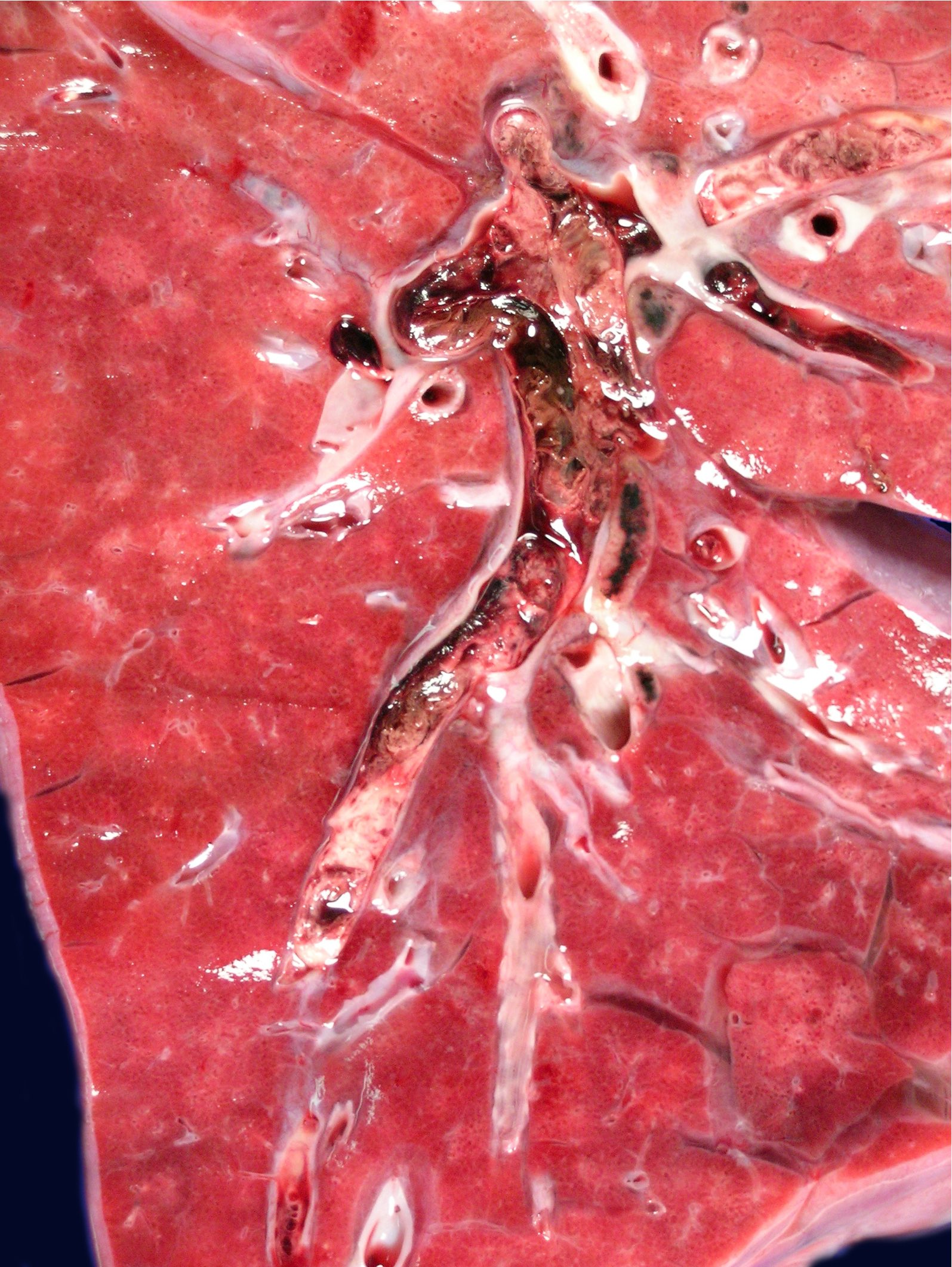
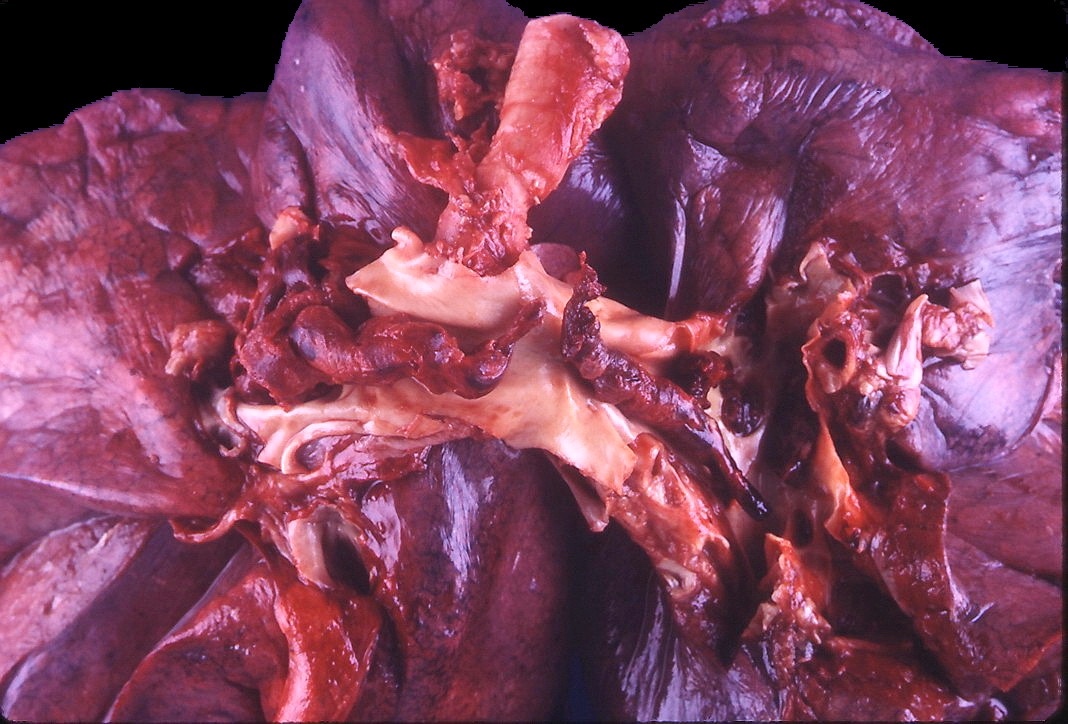
Gross description
- Early stages of pulmonary infarct are often red-blue and have a raised appearance
- Fibrinous exudate covers the apposed pleural surface
- Within 48 hours, the infarct grows paler and finally red-brown as hemosiderin is produced
- Fibrous replacement begins at the margins as a gray-white peripheral zone and gradually transforms the infarct into a contracted scar
- Saddle embolus arises when a large emboli lodges in the main pulmonary artery or one of its major branches or at the bifurcation
- Smaller emboli can induce bleeding or infarction in more peripheral arteries
- References: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020, Husain: Thoracic Pathology - High Yield Pathology, 1st Edition, 2012
Gross images
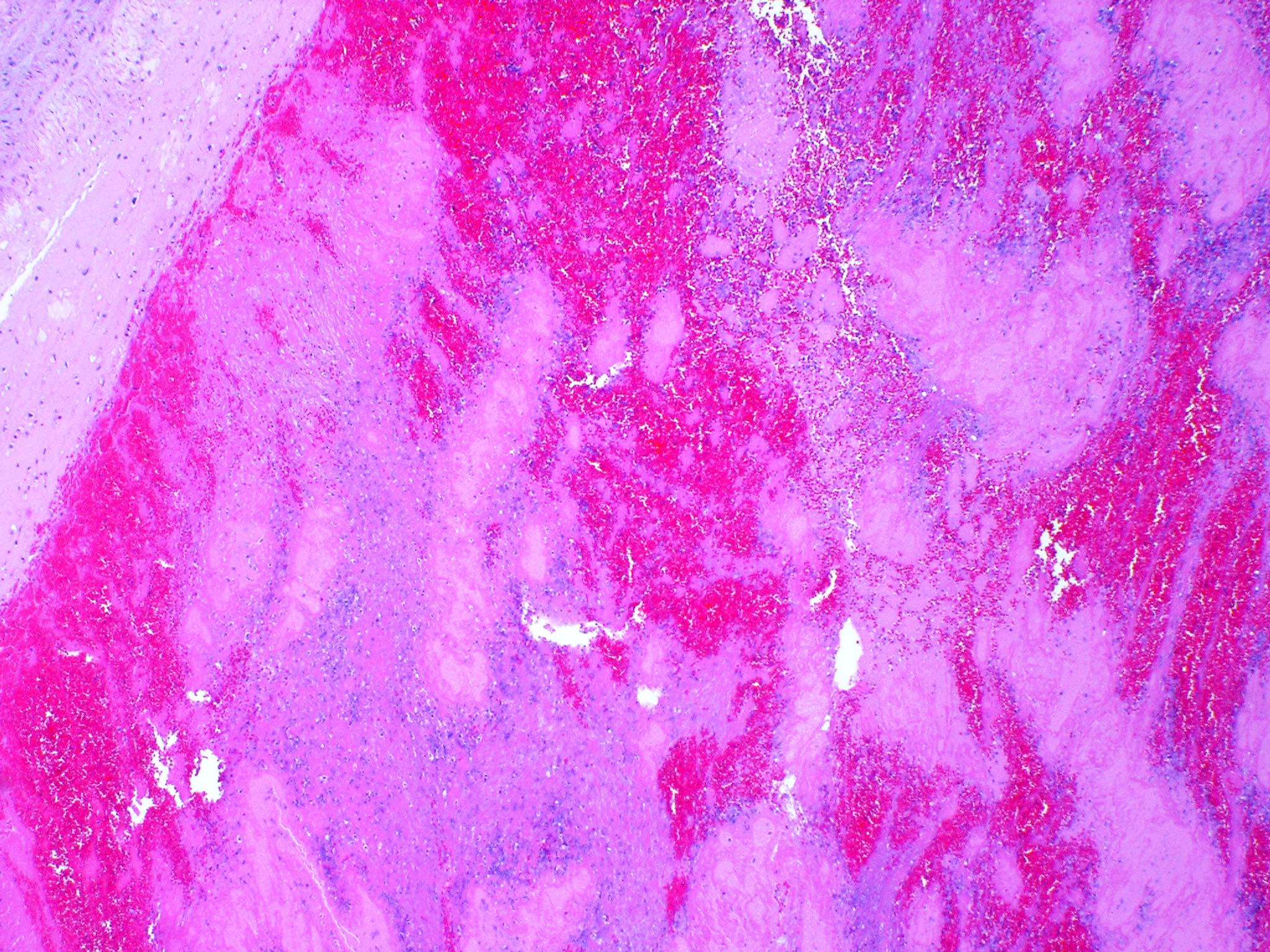
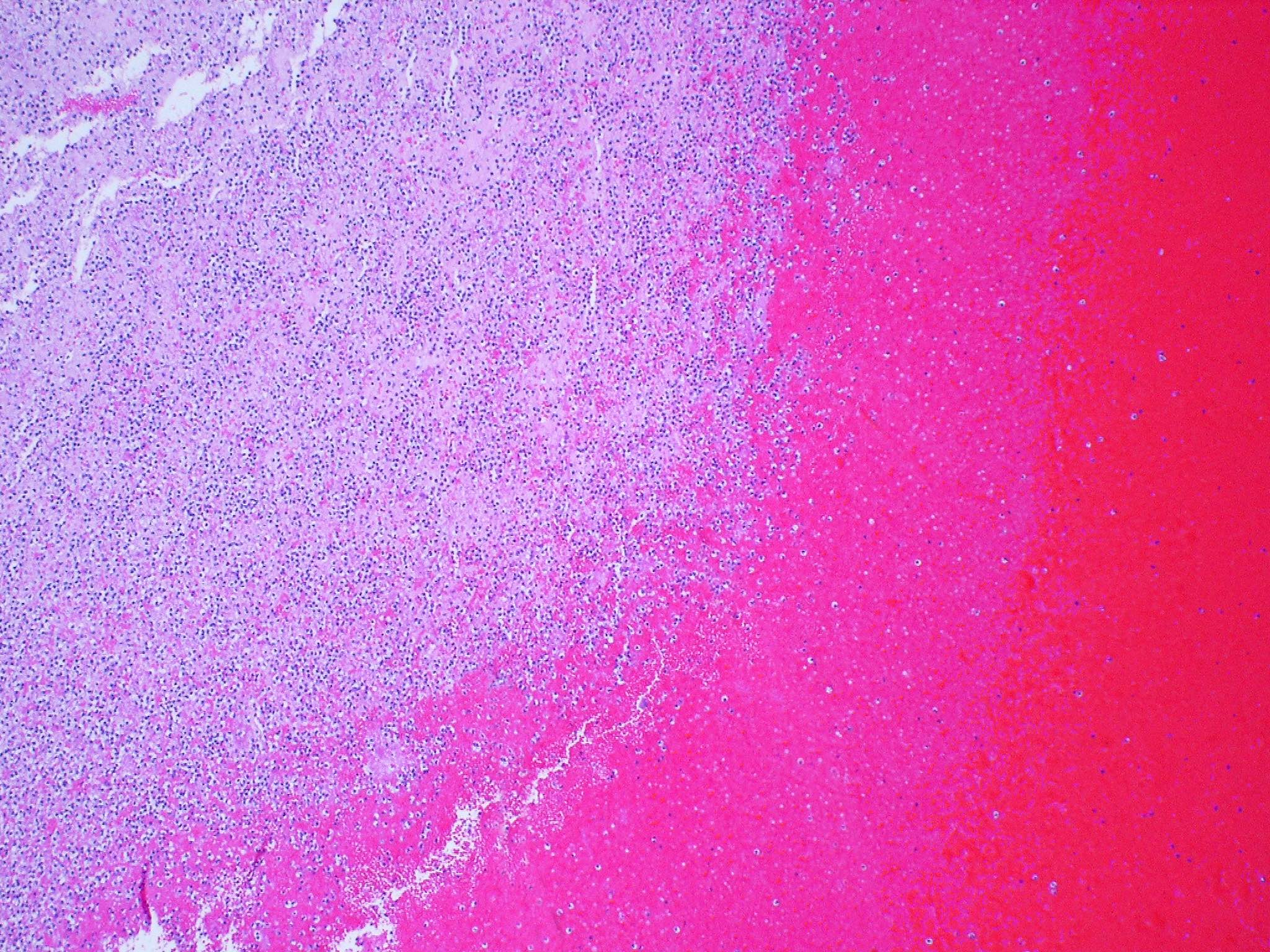
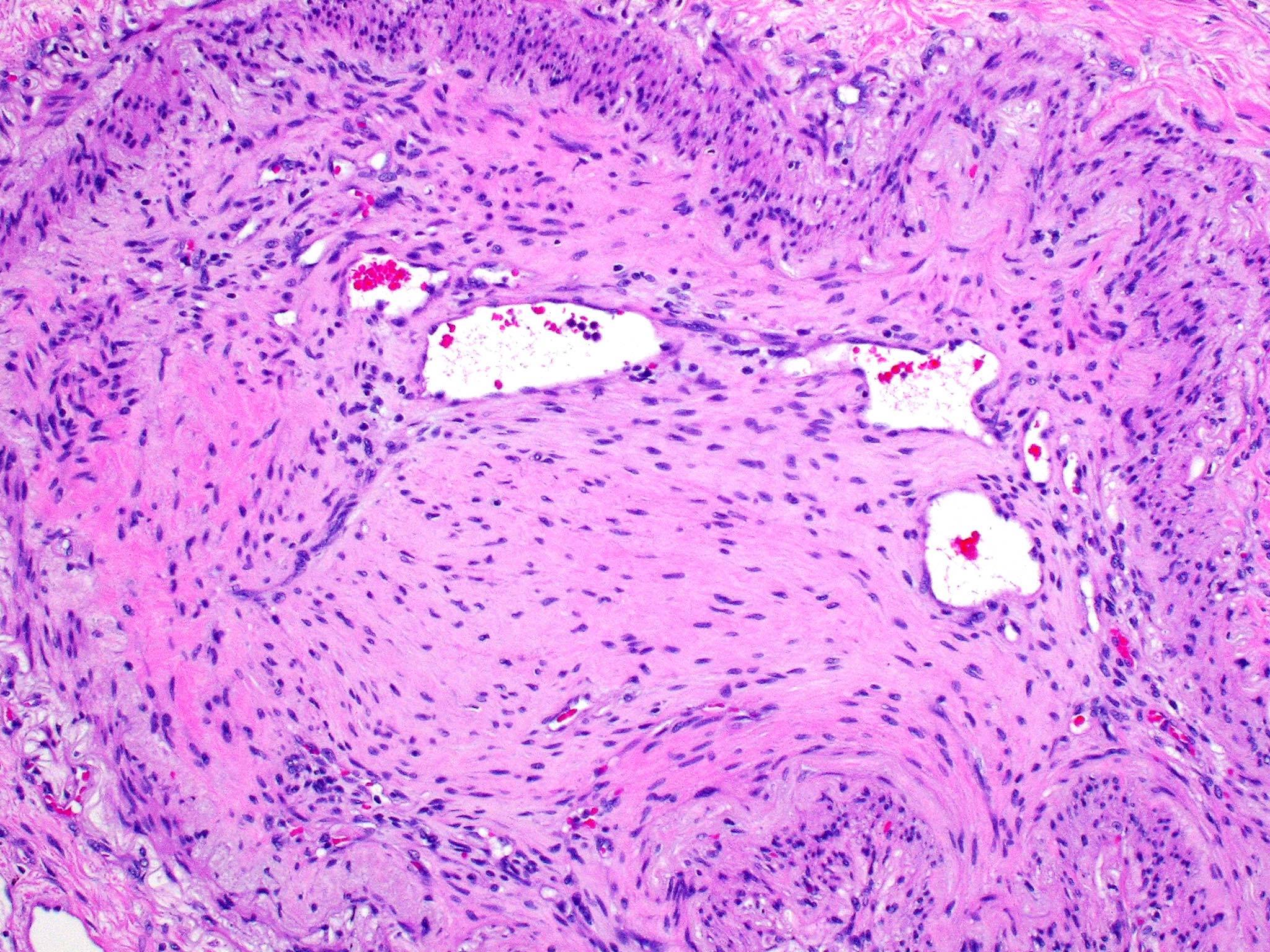
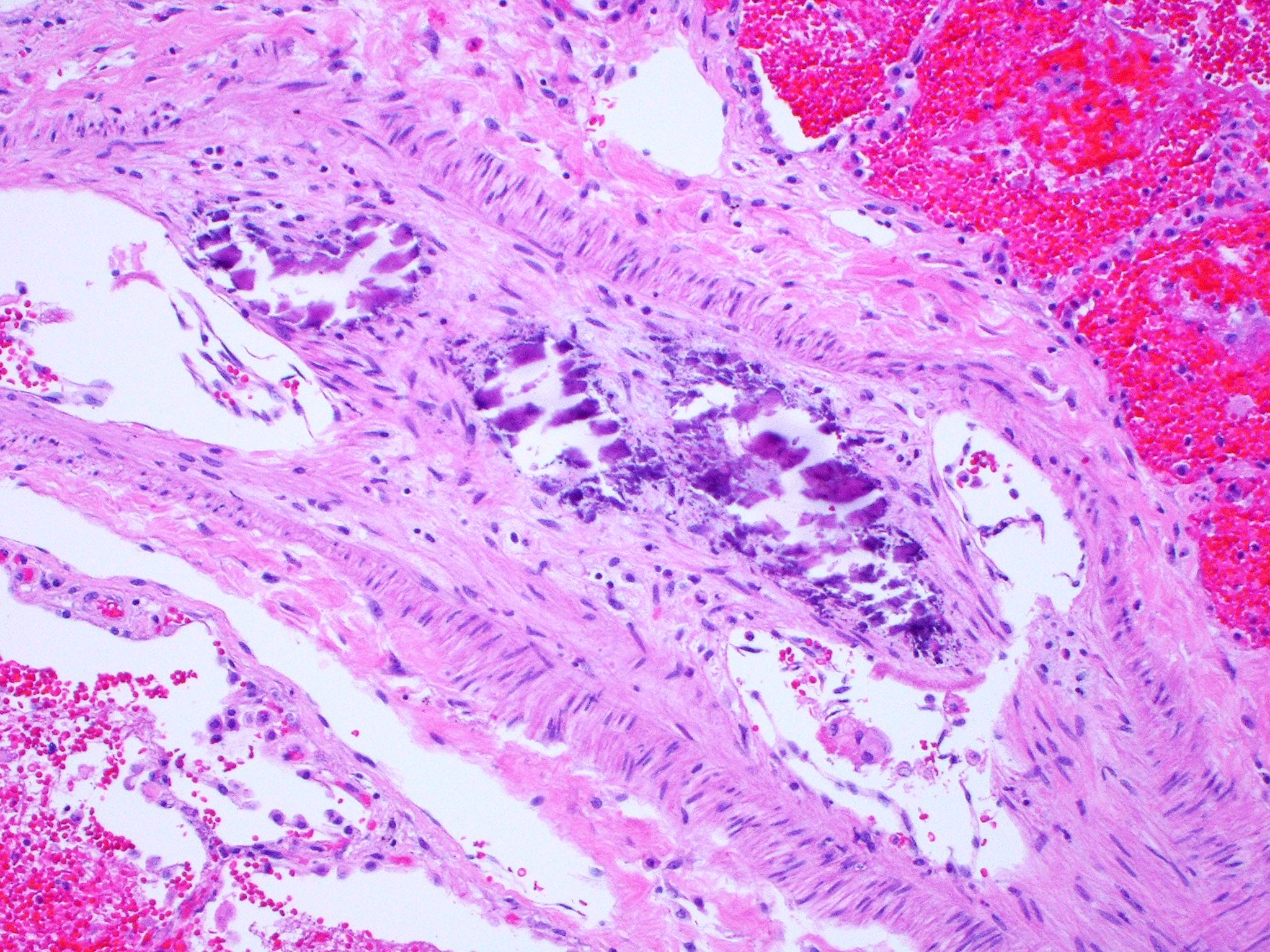
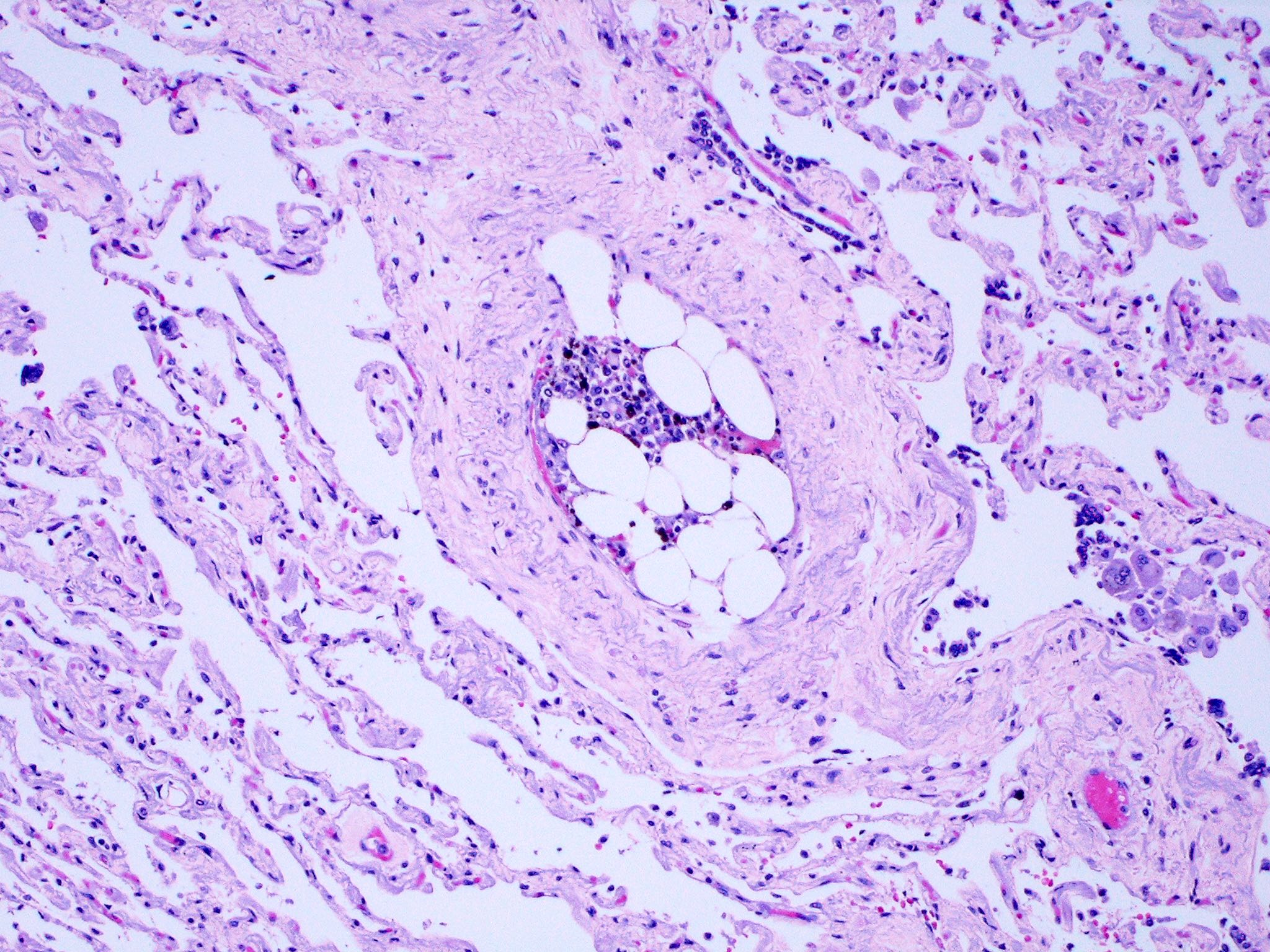
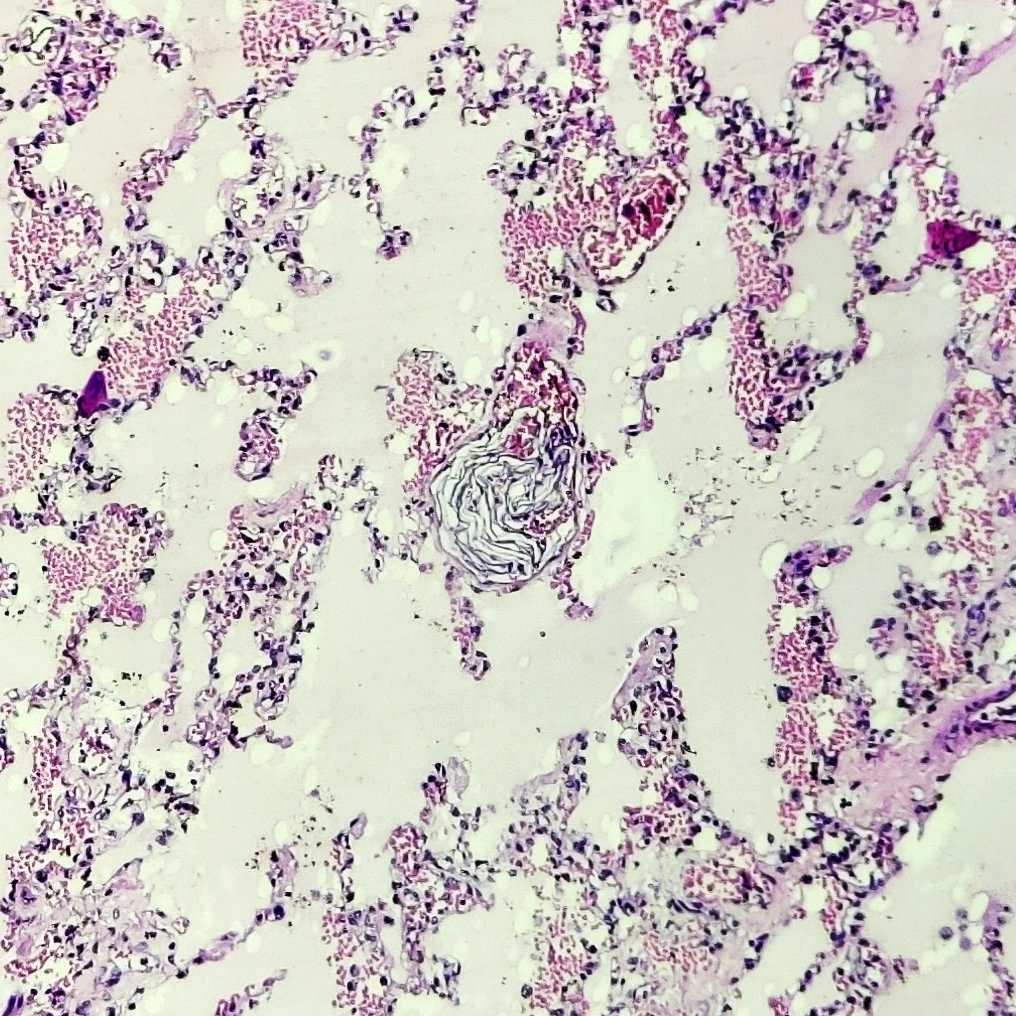
Microscopic (histologic) description
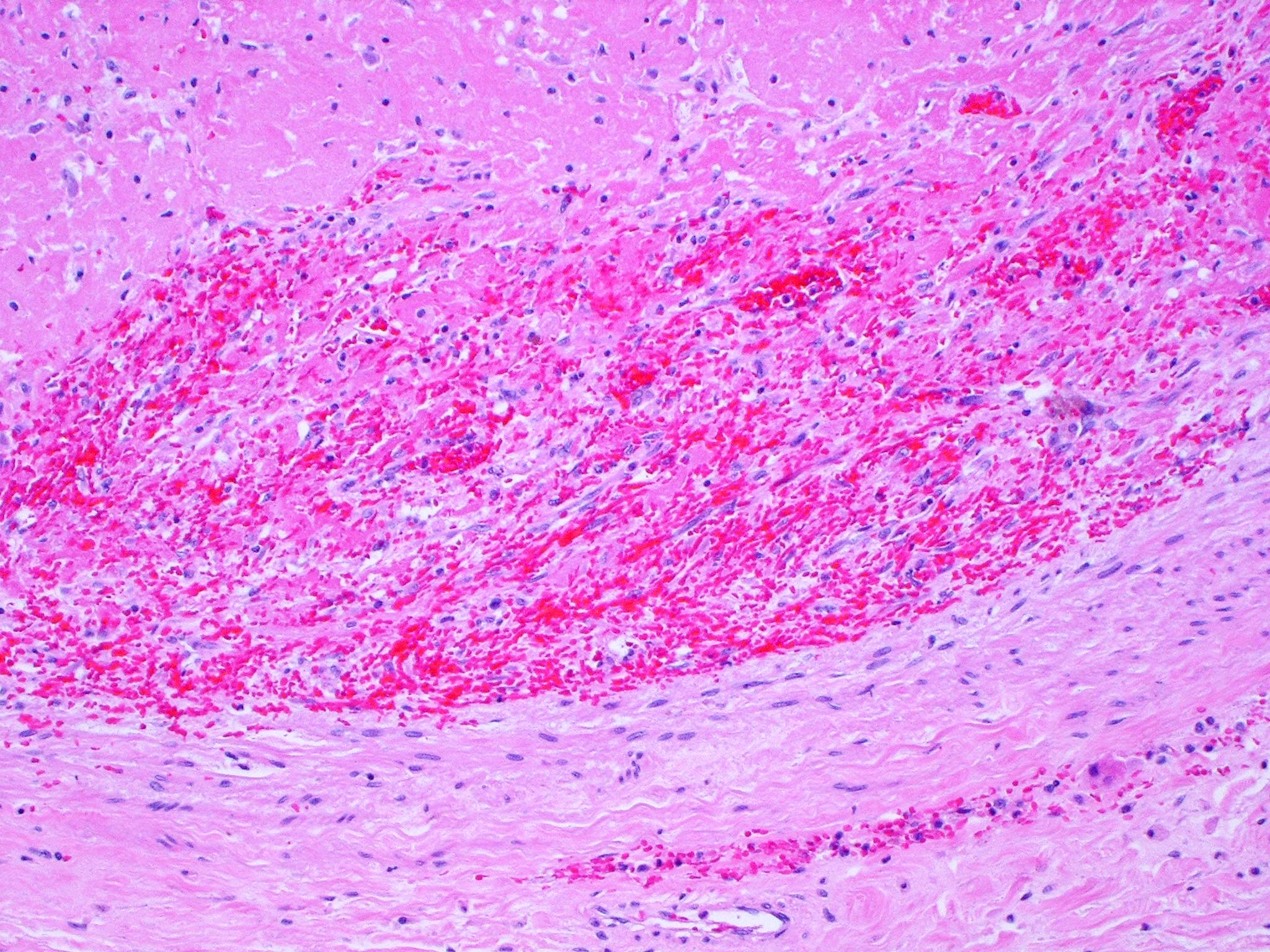
- Antemortem clots display erythrocyte and fibrin layering
- Because of erythrocyte and fibrin / platelet rich layers, true ante mortem clots and emboli exhibit alternating darker and lighter striations (lines of Zahn)
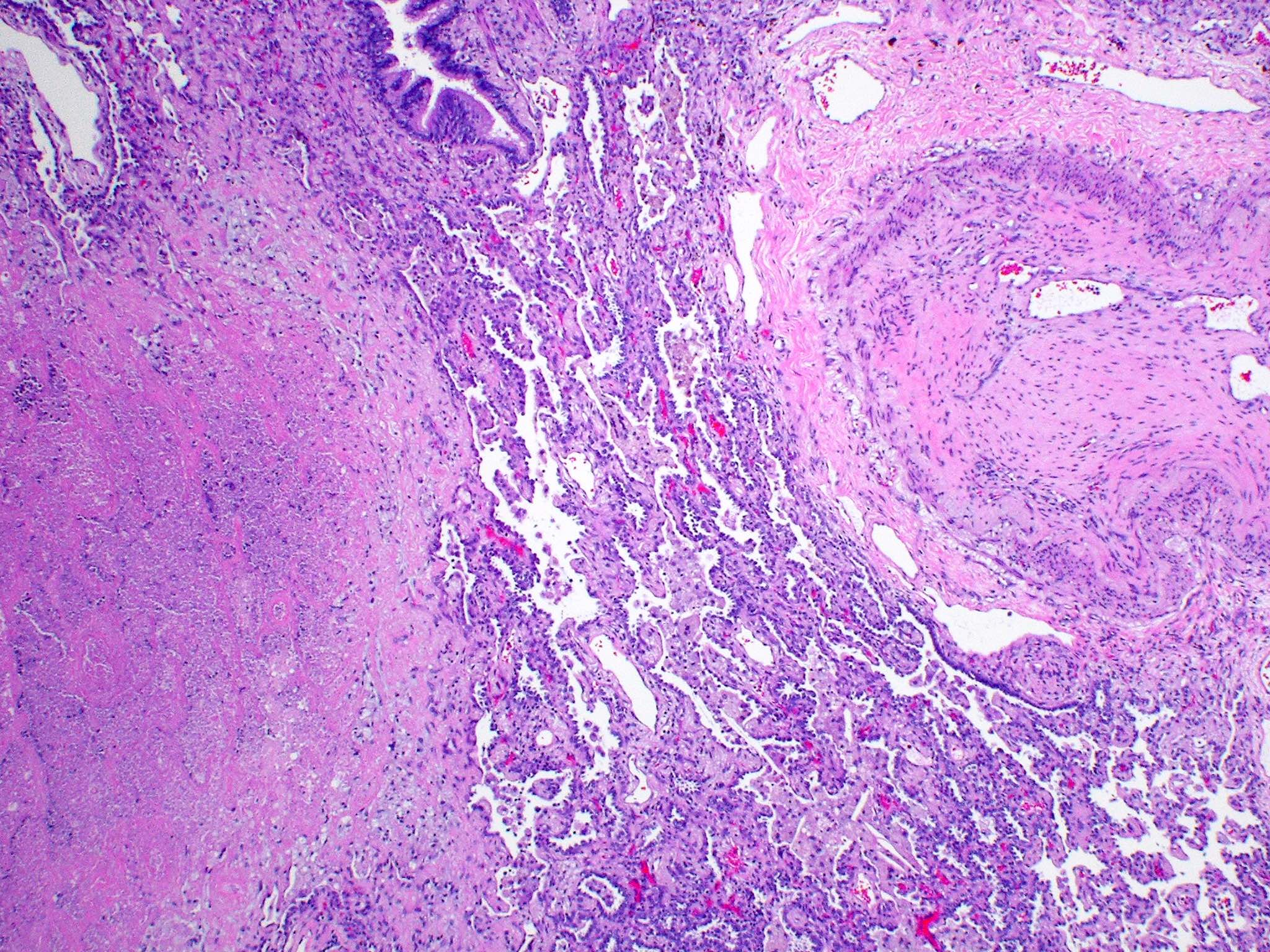
- Thromboembolus is then organized by migrating fibroblasts and myofibroblasts if thrombolysis does not take place within 1 to 2 days
- Clot organization develops from the periphery to the center
- These migratory cells combine with granulation tissue in large arteries and cause clot contraction to one side, resulting in an eccentric thickening of the affected vessel
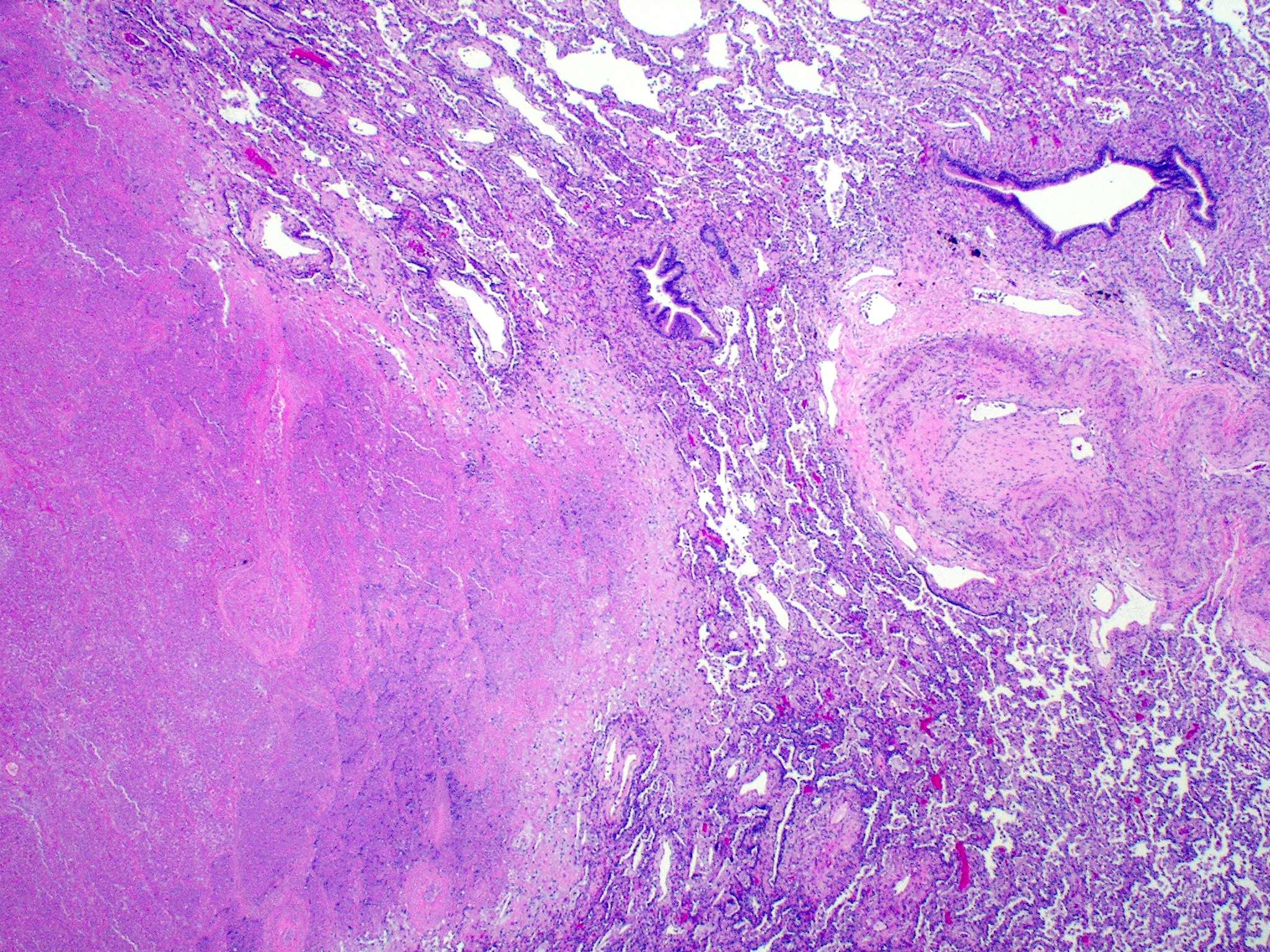
- Hemorrhagic area exhibits ischemic necrosis of the alveolar walls, bronchioles and arteries
- Infarction results in the loss of alveolar nuclei and eventual fibrosis
- Infected embolus causes a septic infarct with a significant neutrophilic response
- Fat embolism / bone marrow embolus: the presence of fat cells with or without marrow elements in the pulmonary circulation
- Most cases are due to long bone and pelvic fractures
- Rounded clear cells can be observed in the pulmonary vessel
- Pulmonary infarcts may present in several ways:
- Typical textbook description is a wedge shaped subpleural zone of hemorrhage with coagulative necrosis
- However, it is essential to remember that various configurations, such as geographical, spherical and mixed forms, can be seen at low magnification
- All of them have coagulative necrosis and significant hemorrhage in the lung parenchyma
- Geographic form is marked by coagulative necrosis in the subpleural region with a serpentine distribution and patches of healthy lung parenchyma frequently encircled by large areas of eosinophilic necrosis
- Round configuration has a thick fibrous capsule that encases a nearly spherical zone of necrosis, while the mixed pattern has segments with both rounded and geographical arrangements
- Granulation tissue covers the airspaces around the necrotic zone and is bordered by thicker interstitium
- Foamy macrophages and histiocytes may also surround the coagulative necrosis
- Squamous metaplasia is also commonly found in pulmonary infarcts and frequently demonstrates substantial reactive changes that lead to a differential diagnosis of cancer
- It may also manifest with vascular inflammation, frequently leading to a differential diagnosis of vasculitis
- References: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020, Husain: Thoracic Pathology - High Yield Pathology, 1st Edition, 2012, Mod Pathol 2009;22:679
Microscopic (histologic) images
Positive stains
- On frozen sections, oil red O or Sudan black stains help to highlight fat emboli
- Elastic stains demonstrate collapsed, intertwined elastic fibers inside a collagenous stroma in organized infarcts
- References: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020, Husain: Thoracic Pathology - High Yield Pathology, 1st Edition, 2012
Sample pathology report
- Lung, left lower lobe, wedge biopsy:
- Organized pulmonary artery thromboembolism with associated infarct (see comment)
- Comment: An irregular intimal plaque with fibrosis is evident within the artery, along with recanalization of the vessel and the presence of small lumina, suggesting a previous clot. Areas of calcification are present within the fibrosis in the pulmonary artery. In addition, necrosis of alveolar walls with loss of nuclei in the neighboring alveoli represents an area of infarction.
Differential diagnosis
- Plexiform lesions of primary pulmonary arterial hypertension
- Postmortem blood clot:
- Weak or no attachment to the wall
- Rubbery and gelatinous
- Appearance of currant jelly on chicken fat
- Absence of lines of Zahn: red blood cells and coagulated serum are mixed in 2 separate layers
- References: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020, Husain: Thoracic Pathology - High Yield Pathology, 1st Edition, 2012
Board review style question #1
A 78 year old man was brought to the emergency room with complaints of shortness of breath, chest discomfort and cough. He died as the medical team was attempting to revive him. The family requested a postmortem examination to determine the cause of death. On investigation, a clot was found lodged in the right main pulmonary artery. Which one of the following characteristics of the clot will help identify if it formed antemortem and contributed to his death?
- Appearance of currant jelly on chicken fat
- Gelatinous, soft and rubbery appearance on gross examination
- Presence of lines of Zahn
- Red blood cells and coagulated serum mixed in 2 separate layers
Board review style answer #1
C. The presence of lines of Zahn or lighter layers of platelets and fibrin alternating with darker layers of red blood cells in a clot indicates that it was formed before the patient died.
Comment Here
Reference: Infarct / pulmonary emboli
Comment Here
Reference: Infarct / pulmonary emboli
Board review style question #2
A 62 year old woman presents to the emergency room with a right femoral fracture. 3 hours later, she develops sudden shortness of breath and altered mental status. On physical examination, she is tachycardic and a red petechial rash can be observed on her chest. A Doppler ultrasound is performed and there are no signs of a deep venous thrombosis. Which of the following best describes what the pulmonary artery histology would demonstrate?
- Atypical cells with a high N:C ratio
- Foamy macrophages and fibrin deposits
- Presence of neutrophils in a clot
- Rounded clear cells with hematopoietic elements are observed in the pulmonary vessel
Board review style answer #2
D. Rounded clear cells with hematopoietic elements are observed in the pulmonary vessel. Bone marrow embolism is defined by the presence of fat cells and hematopoietic elements in the pulmonary circulation, as seen in the image. Hypoxemia, neurologic problems and petechial rash are the characteristic triad for patients experiencing fat embolism syndrome (FES); however, none of these characteristics are unique to FES.
Comment Here
Reference: Infarct / pulmonary emboli
Comment Here
Reference: Infarct / pulmonary emboli